
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 01 December 2022
Sec. Digital Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.971896
 Tobias Rohrmann1†
Tobias Rohrmann1† Peter Praus1†
Peter Praus1† Tanja Proctor2†
Tanja Proctor2† Anastasia Benedyk1
Anastasia Benedyk1 Heike Tost1
Heike Tost1 Oliver Hennig1
Oliver Hennig1 Andreas Meyer-Lindenberg1
Andreas Meyer-Lindenberg1 Anna-Sophia Wahl1,3,4*
Anna-Sophia Wahl1,3,4*Background: During the COVID-19 pandemic telemedicine became essential in maintaining diagnostic procedures and treatment in psychiatry. However, it is still an open question if telemedicine is a feasible treatment option for all groups of psychiatric patients alike. This prospective monocentric observational trial was conducted to assess the general applicability of telemedical treatment in a naturalistic psychiatric outpatient cohort and to identify groups of disorders and clusters of psychopathology that respond particularly well to telemedical treatment considering sociodemographic characteristics and patients' perspectives.
Methods: Patients were recruited April 2020–April 2021 and asked to fill out the WHO-5 and the SCL-90R at baseline, after 4–6 and 8–12 weeks and a feedback-survey. Additionally, medical records, psychopathology, psychosocial functioning, and socio-demographic data were analyzed. Primary outcomes were well-being, psychopathology and functioning during treatment. Secondly, diagnostic groups and psychopathology linked to a superior treatment-response were determined with respect to patients' subjective experiences.
Results: Out of 1.385 patients, 254—mostly with hyperkinetic (35.3%) and depressive disorders (24.6%)—took part. Well-being and SCL-90R total scores improved substantially (both p < 0.001). CGI and GAF scores were worse in depressed subjects (both p < 0.05). Improvement was mainly seen in depressed patients; chronic disorders experienced a decline in well-being. Sociodemographic characteristics could not explain this difference. Particularly female (r = 0.413) patients found telepsychiatry equivalent to conventional treatment. The more virtual sessions participants attended the more likely they were to find telepsychiatry equal to conventional treatment (r = 0.231).
Conclusion: Telemedicine is an effective treatment for patients with depression under naturalistic conditions. Telemedical consultations are a simple and reliable way of monitoring symptom severity and directing treatment choices during the treatment of depressive disorders. Patients with depression benefited more from telemedical treatment compared to participants with chronic non-episodic psychiatric disorders. Future research needs to concentrate on improving telemedical treatment options suited for the latter conditions. Psychiatric telemedicine yielded overall high degrees of satisfaction among users.
Already at early stages of the coronavirus disease 19 (COVID-19) pandemic it became evident that an accelerated transition from face-to-face services to virtual interventions would automatically impose a plethora of critical questions concerning the adequacy and quality of such treatment options on healthcare providers, caregivers and patients alike (1). Telemedicine—in contrast to conventional psychiatric care—solely relies on the exclusive administration of mental health services via technological devices such as phone or video calls or other platforms (2) without face-to-face contact. Pre-pandemic investigations had substantially focused on the applicability and potential benefits of telemedical mental health services in the context of equalizing access to these services under conditions of shortage, mainly targeting symptoms of depressive or anxiety disorders (3, 4). The rapid expansion of telemedical interventions related to the COVID-19 pandemic raised the question of their comparability with conventional treatment options, hitherto mainly relying on personal relationships in the field of psychiatry and psychotherapy. Until 2020, the available data showed a steadily growing dissemination of telemedical practice, albeit only accounting for a relatively small proportion of the entirety of medical services in the U.S. (5). With the pandemic surge of COVID-19 infections in 2020, sudden changes in legislation and reimbursement practices allowed for an unprecedented expansion of telemedical treatment services in the field of psychiatry (6, 7).
Besides of general advantages of telemedical treatment such as greater geographical and temporal flexibility, the reduction of age-, gender-, and ethnicity-specific treatment barriers (8) and cost effectiveness (9), telemedical interventions were an essential tool in maintaining the continuity of community-based treatment paths for patients with severe mental health conditions like schizophrenia-spectrum disorders during the COVID-19 pandemic (10). Telemedical interventions also promoted the involvement of peers and relatives at multiple stages of diagnostic and treatment procedures (11).
Despite these advantages, there are some valid concerns about possible tool-related limitations of the reliability and reproducibility of telemedical assessments and categorical diagnostics under the conditions of telemedical consultations compared to traditional face-to-face evaluations (12). In particular, there is only limited evidence on the question which mental health conditions might respond optimally to exclusive telemedical treatment and which mental disorders require face-to-face appointments, respecting patients' personal preferences. On a larger scale, telemedical interventions alone might not be suited to mitigate or overcome gross disparities in health status and access to mental health services, rather calling for thorough systematic implementation of telemedical services without marginalizing patient groups with less developed digital literacy (13).
In this longitudinal observational study, the authors aimed to elucidate the applicability, reliability, and safety of telemedical assessment and treatment provided via telephone or video calls in a naturalistic sample of psychiatric outpatients during the COVID-19 pandemic. In this line, the purpose of this study was to identify a cluster of mental disorders and patient related features (e.g., sociodemographic characteristics) that potentially indicate a favorable response to telemedical treatment under these conditions and to determine the comparability of telemedical interventions to conventional treatments from a patient-perspective.
The study was designed during the first enforced Germany-wide lockdown (starting from March 22 2020) due to the COVID-19 pandemic. Most services of the outpatient clinic at the Central Institute of Mental Health, Mannheim (CIMH) at the University of Heidelberg, Germany, had to be transformed into telemedical treatment options in order to maintain provision of psychiatric consultations for patients with mental health issues despite severe contact restrictions. The goal of the study was (1) to observe how psychiatric symptoms of patients with mental health problems develop during the course of telepsychiatry; (2) if patient cohorts could be identified which benefit more or less from telemedical psychiatric treatment, (3) if sex-, age or sociodemographic factors with an impact on the effectiveness of telepsychiatric treatment could be revealed and (4), how patients experienced telepsychiatric consultations compared to conventional treatment face to face with professional mental health experts.
Participants were recruited between April 2020 and April 2021. Patients received information about the study during the scheduling of their first telemedical psychiatric counseling. All individuals who had not received regular treatment by the general psychiatric outpatient services of the CIMH prior to the study period were invited to take part in the study. Due to the observational nature of the study there were no other exclusion criteria except the exclusion of children and adolescents (patients under 18 years of age). The aims and purpose of the study were explained either by members of the study team who contacted interested patients or by the psychiatrist or psychologist who provided the first telemedical session. Telemedical treatment was administered via phone or video calls (Table 4), according to patients' preferences, technical equipment as well as individual and legal data safety concerns. For initial telemedical appointments past and medical history of patients including current medical complaints as well as a history of psychiatric symptoms, treatments, medication, secondary diagnoses and social history were recorded comparable to an initial appointment in person except for the physical examination. During the following telemedical consultations, patients received psychiatric counseling with optimization of psychopharmacological treatment and/or psychotherapy. Between telemedical psychiatric consultations patients received scheduled appointments with strictly limited personal contact for blood tests, therapeutic drug monitoring (TDM), and physical as well as radiological examinations (e.g., MRI scans), if required. Patients who gave informed consent to participate were asked to complete three surveys during the course of the study: Before the first telemedical consultation, participants agreed that their medical record, which would be created during telemedical treatment, could be used for further analysis (see below) as part of the study. Subjects were also asked to fill out the WHO-5 wellbeing index [WHO-5 (14)] and the symptom check-list-90-R [SCL-90R (15)], which were provided paper-based. 4–6 and 8–12 weeks after the first telemedical session, participants could choose to take part in the second and third survey, if they preferred an interview via phone call or online surveys using REDCap (https://www.project-redcap.org/), a secure web application for building and managing online surveys for research studies and operations supported by the National Institutes of Health (NIH/NCATS UL1 TR000445). N = 254 participants returned the first paper-based survey (including 9 anonymous study subjects). N = 94 participated in the second survey via RedCap and N = 50 via telephone. N = 68 study subjects also completed the third survey via RedCap, while N = 48 were interviewed via telephone. During all surveys, patients were asked to fill out the WHO-5 questionnaire repeatedly, whereas they were only requested twice to complete the SCL90-R (1st and 2nd survey, see Supplementary Figure S3 for the number of subjects who completed all inquiries, as well as drop out cases or subjects just responding to one inquiry). Either during the second or the third survey patients could evaluate the telemedical psychiatric treatment (see details below).
Out of all participants, 182 subjects (71.7%) gave informed consent to acquire sex, age and sociodemographic data as well as their psychiatric history and standardized professional ratings of psychopathology from their medical records. All mental health experts providing telepsychiatric services in our outpatient clinic were instructed to use a highly structured computerized rating of psychopathology provided by the electronic documentation system of our clinic (ORBIS, SAP, Walldorf Germany) during the first interview. Patients were screened for current psychiatric symptoms, psychiatric diagnoses according to the ICD-classification of the WHO (version 10), past psychiatric history and sociodemographic data such as current living situation, education, professional training and labor situation, debts and history of criminal assaults. All psychiatrists and psychologists of our outpatient clinic were also requested to score patients on initial appearance according to the global assessment of functioning scale [GAF (16)] and the clinical global impression scale [CGI (17)]. During subsequent data analysis electronic medical records were systematically queried for the number of telemedical treatment sessions participants received and possible hospitalizations during the course of the study. Medical records were additionally scrutinized for the number of in- and outpatient treatments and days of hospitalization during the year before March 2020, when outpatient psychiatric care was still provided personally.
For assessment of overall wellbeing over the course of telepsychiatric counseling the WHO-5, a short self-administered measure of wellbeing over the last two weeks (18), was used. The WHO-5 consists of five positively worded items that are rated on a 6-point Likert scale, ranging from 0 (at no the time) to 5 (all of the time). We transformed the raw scores to a score from 0 to 100 (raw data*4), where lower scores indicated worse wellbeing. A score of ≤50 was considered as poor wellbeing and a score of 28 or below indicative of depression.
The SCL-90-R by Derogatis (19) measures the subjective perception of physical and mental symptoms a person has experienced during the past seven days. All 90 symptoms are scored on a Likert scale consisting of 5 steps, ranging from 0 (no symptom at all) to 4 (very strong impairment due to the symptom). We analyzed the data gained in two surveys of the SCL-90-R according to the instructions provided by Derogatis/Franke, German Version, 2nd Edition, Beltz Test, 2000. T-Values equal to and above 60 were considered as a relevant mental detraction from the respective symptom or global score.
While the WHO-5 and the SCL-90-R are self-report questionnaires on the subjective perception of overall wellbeing and different symptom domains, the GAF and CGI were used as clinician-rated scales to document the global impairment due to patients' (mental) health conditions. The CGI scores the severity of the symptoms, ranging from 1 to 7 [1= normal/not at affected; 7 = very severely ill (17)]. The GAF indicates the global functioning of a patient taking into account the psychiatric, social and professional level of functioning. The scale is ranging from 0 (very sick) to 100 (healthy) (16).
One hundred and twelve individuals (44.1% of all participants) completed an evaluation questionnaire asking for feedback concerning technical details (e.g., if patients decided for phone call or video conference or both and if interruptions occurred due to technical problems) and the overall experience with the telepsychiatric consultations. Participants were asked how helpful they found the telemedical interventions during the study period and if they were comparable to conventional face-to face consultations. Patients were also requested to state their preference about using telepsychiatry in the future again. Participants could also document pros and cons of the telemedicine and their wishes for future improvements.
All data acquired during surveys and from the medical records were entered into an Excel master file and then translated to SPSS Version 27 and R Version 4.1.1. for further analysis. The descriptive statistics of the sample were computed for the sociodemographic characteristics, consisting of frequencies and percentages for categorical values and mean and standard deviations (SD) for scale variables. Differences between two groups of patients (depressive and suffering from other psychiatric diseases) were assessed using the Mann-Witney test for the different non-parametric clinical scale variables. The differences in these scales over time for the single patients were assessed with an ANOVA test and a post-hoc Bonferroni test.
A paired Wilcoxon signed-rank test was used to assess differences in the levels of mental health variables such as e.g.: WHO-5 or SCL 90 comparing the results of the three inquiries. For this only data from subjects were included where subjects had participated in all inquiries (“complete cases,” Supplementary Figure S3). Bivariate associations between WHO-5 and SCL90-R, CGI and GAF were analyzed using linear regression models and between mental x and y (continuous variable) were assessed via Spearman's correlation coefficient r. For all tests, a p-value of < 0.05 was considered statistically significant.
Written informed consent was obtained from all subjects who participated in our study, except for 9 cases where patients returned the paper-based WHO-5 and SCL90-R questionnaires of the first survey anonymously. These data could not be used for further evaluation. The study design and data acquisition were presented to the ethics committee II at the medical faculty Mannheim, University of Heidelberg and approved (No. 2020-562N).
During the first year of the Covid-19 pandemic (April 2020–April 2021) 8.235 telemedical treatment sessions were provided to 1.385 patients via phone or video call by the psychiatrists and psychologists of the outpatient clinic at the Central Institute of Mental Health (CIMH) in Mannheim, Germany. Two hundred and fifty four (18.3%) of these patients gave their informed consent to participate in the study and to use their medical record generated during telemedical treatment for further systematic analysis. Out of 239 patients who engaged in the first survey at baseline, 140 patients responded to the second, and 103 patients to the third survey 4–6 and 8–12 weeks after the first telemedicine session, respectively.
In total, electronic medical records of 174 patients could be evaluated revealing sociodemographic characteristics as presented in Table 1: Our study population consisted of younger adults, 38.6 ± 13.1 years old with more women (56.7%, 39.9 ± 13.3 years old) than men (37,8%, 37.0 ± 12.6 years old) participating. Most patients had a partner (55.3%), but no children (82.8%) and were living alone (53.6%). Almost half of the study population (48.8%) was well educated with at least 12 years of school education while more than half (53.8%) had also successfully completed apprenticeship. 53.3% were employed during the time of telemedicial treatment and most patients (63.9%) lived in a stable financial situation without significant debts.
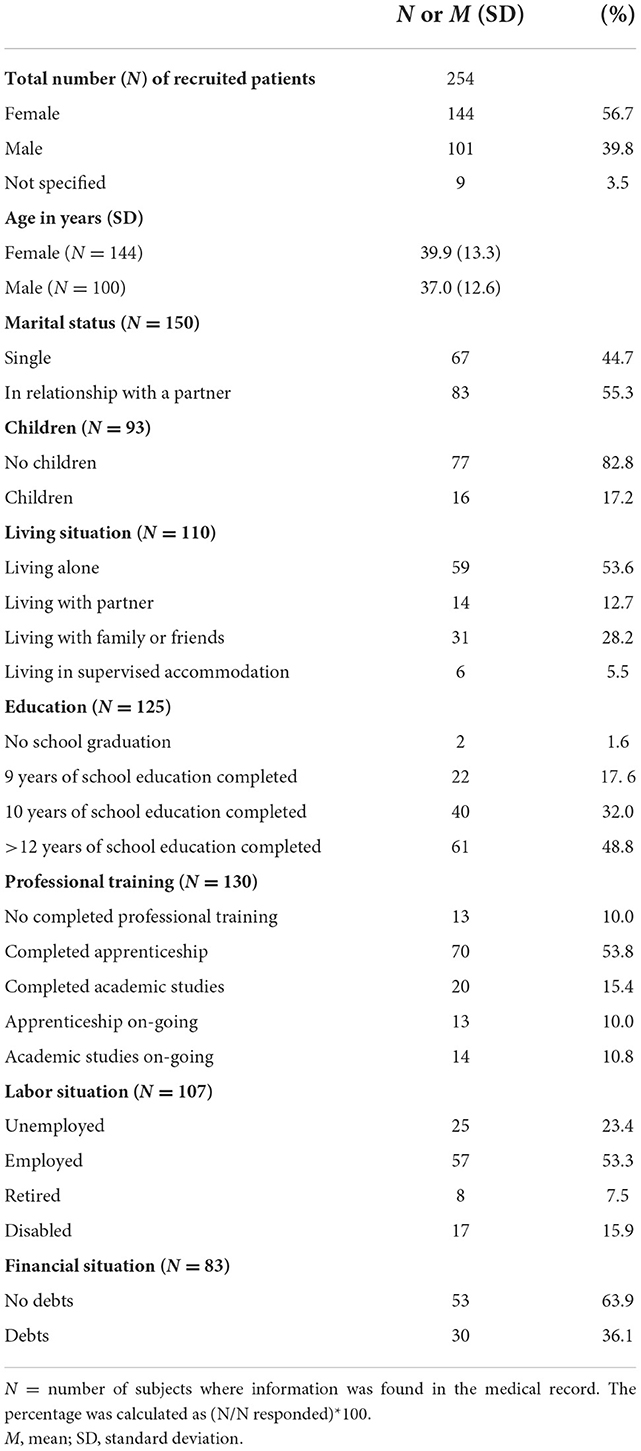
Table 1. Sociodemographic characteristics of the study population assessing sex, age, marital status, children, living situation, education, professional training, labor, and financial situation.
All patients included in the study were diagnosed with at least one psychiatric disorder (Table 2): The largest group (35.3%) consisted of patients with hyperkinetic and tic disorders, while almost a quarter of the study population (24.6%) was primarily diagnosed with a depressive episode or recurrent depressive disorder according to the ICD-10 classification. In addition, for 32 patients (12.6%) a depressive or recurrent depressive disorder was noted as secondary diagnosis. Schizophrenia was only diagnosed in 3 cases (1.3%) as the main psychiatric disorder currently requiring psychiatric treatment. Matching with this preponderance of affective and neurodevelopmental disorders, most patients presented with psychopathological symptoms (Supplementary Table S1) typical of affective and hyperkinetic disorders such as attention (51.9%) and concentration deficits (67.6%), abnormal thought processes (71.7%), changes in mood (84.0%), reduced ability to experience joy (52.9%), lack of drive (56.9%), anxiety (64.4%) and sleep disturbances (69.4%). Orientation, Mnestic functioning as well as illness insight were undisturbed in almost all patients (see Supplementary Table S1), while symptoms typical of an episode of psychosis such as abnormal thought content, hallucinations or intrusions were almost absent (Supplementary Table S1). Among the patients who gave full particulars of their psychiatric medical records (71.7%, Supplementary Table S3), 29.2% reported a history of attempted suicide. Three quarters of participants (74.3%) had already been referred to psychiatric treatment in the past, while only a minority (25.8%) received psychiatric treatment for the first time.
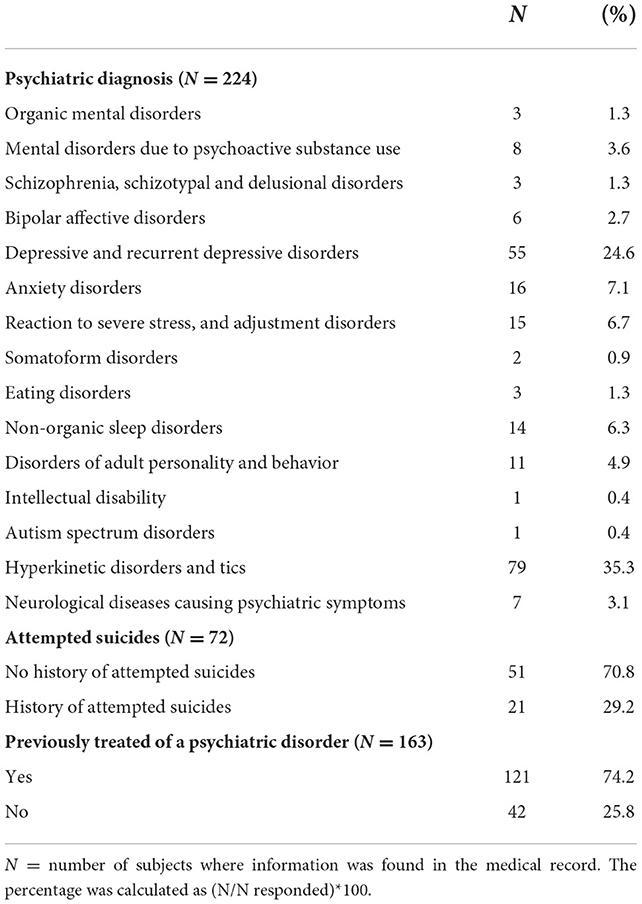
Table 2. Table depicting the psychiatric history of subjects including the leading psychiatric diagnosis documented in the medical record, as well as attempts of suicides and previous psychiatric treatments.
Most patients (93.7%, Table 3) had not been in contact with the outpatient clinic within 12 months before the pandemic. During the course of the study patients had on average 4 (4.26 ± 5.45) psychiatric appointments. At least 3 (3.05 ± 3.58) appointments were provided via telemedicine (phone or video call). For comparison, the 16 patients that had already been in psychiatric outpatient treatment before the pandemic had also had 4 (4.56 ± 5.89) face to face appointments during the course of 12 months before the pandemic. Only a small number of participants (n = 13, 5.12%) required hospitalization during the study period. These 13 patients spent on average 74.54 ± 46.67 days on a psychiatric ward (Table 3), while four participants had stayed in hospital more than 4 months (128 ± 62.20) in the year prior to the pandemic.
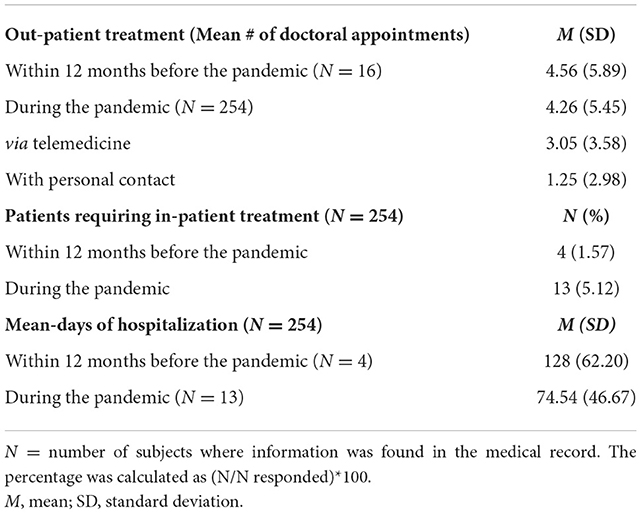
Table 3. Table revealing the amount of psychiatric counseling, hospitalization requirements, and days of hospitalization in a specialized psychiatric unit 12 months before the pandemic and during the course of the study in the COVID-19 pandemic.
Participants were requested to report current mental wellbeing by completing the WHO-5 wellbeing Index [WHO-5, (18)] before, as well as 4–6 and 8–12 weeks after the beginning of telepsychiatric treatment. Two hundred thirty-seven patients (93.3%) participated in the first self-report, scoring 31.65 ± 20.11 (range 0–100, Figure 1A). The prevalence of poor wellbeing [WHO-5 score ≤ 50, (20)] was 81.9% (n = 194) and that of depression (WHO-5 score ≤ 28) was 55.3% (n = 131) before the start of the telemedical treatment. One Hundred Thirty-one (51.6%) and 98 (38.5%) of the initial 254 participants also responded to the second and third survey, respectively. Patients reported a significant improvement of wellbeing 4–6 and in particular 8–12 weeks after the start of the telemedical appointments (WHO-5 4–6 weeks 39.60 ± 21.61; WHO-5 8–12 weeks 41.47 ± 21.26; p < 0.001, the Wilcoxon test was used for comparison with the initial WHO-5 self-report). 8–12 weeks after initiation of the telemedical treatment only 32% (n = 33) revealed very poor wellbeing, indicative of severe depressive symptoms (WHO-5 score ≤ 28).
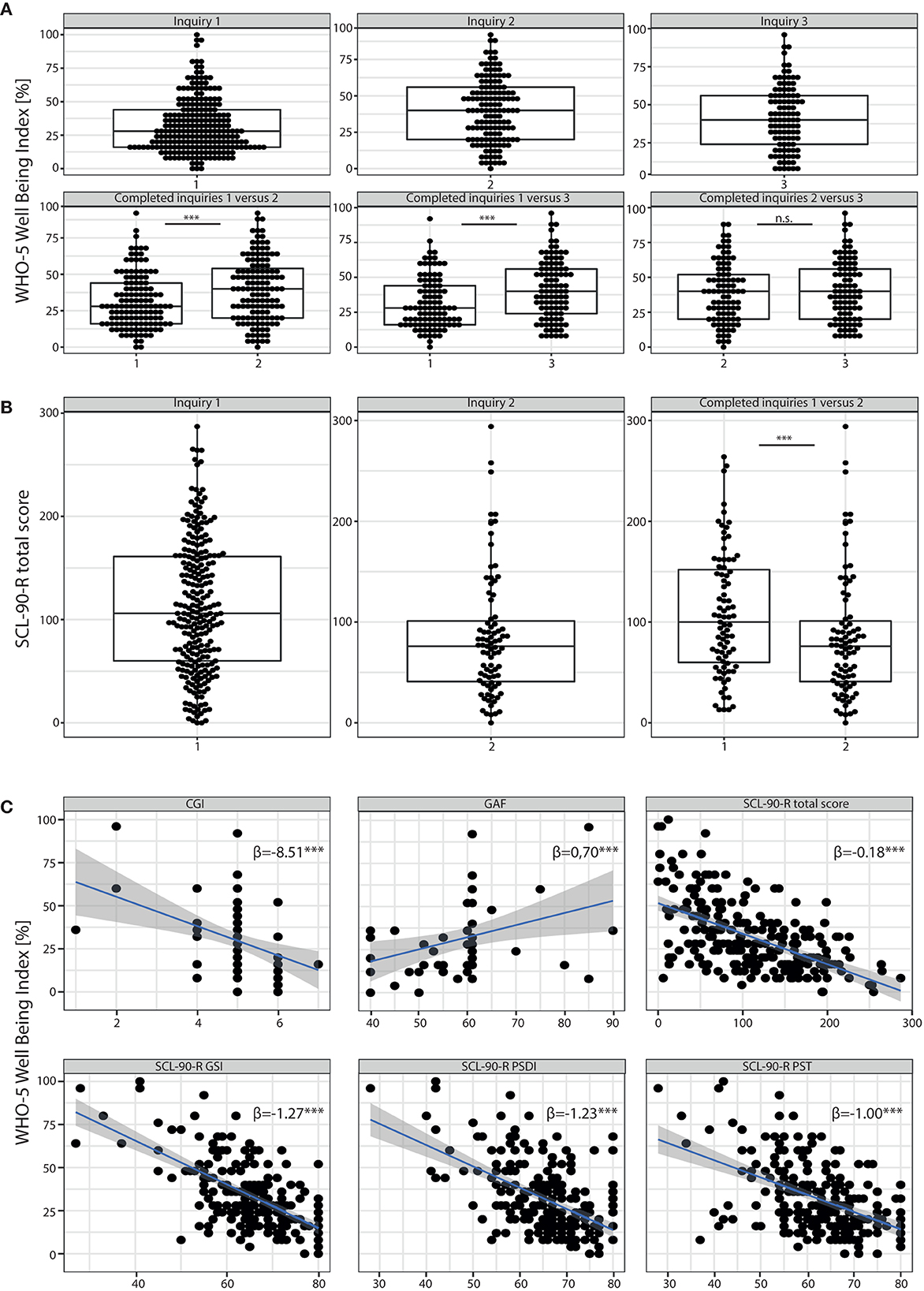
Figure 1. Results of self-report assessment using WHO-5 and SCL90-R. (A) Results of the WHO-5 Wellbeing Index: Boxplots with scoring details of all individuals participating in the different surveys (inquiry 1 = survey before the beginning of the telemedical treatment; inquiry 2 and 3 = surveys 4–6 and 8–12 weeks after start of the telemedical counseling, respectively) are shown in the upper panel. In the lower panel we compared the results of subjects who participated at least in the first and one consecutive survey. We found a significant improvement of WHO5 scores during the course of telemedical treatment (inquiry 1 vs. 2, p < 0.001, Wilcoxon-test). Results of individual study subjects are shown in percentage where 0% reflects very impaired wellbeing while 100% represents perfect wellbeing. (B) Results of the SCL90-R depicting data points of individual study participants. High scoring rates represent severe detraction of psychiatric symptoms. Those participants that completed the survey twice (before and 4–6 weeks after start of the telemedical psychiatry) reported a significant improvement of psychopathological symptoms (significant decrease of total scores for inquiry 2 vs. 1, p < 0.001, Wilcoxon-test). (C) Results of the WHO-5 (in %) correlated to clinical scores such as the CGI and the GAF as well as to all three global indices of distress of the SCL90-R such as the GSI, PSDI and PST (A linear regression analysis was performed, β = regression coefficient). ***p < 0.001. n.s. = non-significant.
Participants were also asked to fill out the Symptom Checklist-90 Revised (SCL90-R) at baseline, and 4–6 weeks after the start of the telemedical treatment. The mean SCL90 total score for n = 83 (32.68%) participants was 107.9 ± 60.86 at baseline (1st inquiry, Figure 1B) with a decline to a mean score of 85.08 ± 61.22 in the second survey (2nd inquiry, Figure 1B), indicating a significant improvement of psychopathological symptoms after 4–6 weeks (p < 0.001 with a paired Wilcoxon test to compare the SCL90 total scores of patients who participated in both inquiries). For patients who participated in both inquiries (n = 83), the means of all three global indices of distress in the first inquiry were above the critical threshold (T ≥ 60, Supplementary Figure S2). The Global Severity Index (GSI) was 66.61 ± 10.31. 77% (n = 83) of the study population who participated in both inquiries scored with a T ≥ 60 suggesting “psychologically measurable distressed cases” (21). In addition, the Positive Symptom Distress Index (PSDI) and the Positive Symptom Total (PST) were evaluated as global measures of symptom intensity and number of psychiatric symptoms with significant burden. Means of both indices revealed T ≥ 60 (PSDI 65.12 ± 8.23; PST 62.02 ± 8.45) substantiating significant mental distress. Furthermore, all mean values of the nine primary symptom dimensions (Supplementary Figure S2) exceeded T-values of 60. In particular the subscales for obsessive-compulsive symptoms and depression scored even above a T ≥ 65 (Mean obsessive-compulsive 67.55 ± 10.77; Mean depression 67.08 ± 10.61, Supplementary Figure S1), revealing a significant burden within the study population (T ≥ 1½ SD of mean T-values in a healthy norm group, Franke 2001). All global scales and nine primary dimension scores were markedly decreased in the second inquiry (p < 0.001); a Wilcoxon test was used for the comparison of the results of patients with both inquiries completed (Supplementary Figure S2). In particular T-Values were below 60 for the PSDI (59.45 ± 10.67) and for 5 out of nine primary dimension scores (anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism, Supplementary Figure S2), indicating a reduction of psychopathological burden for these dimensions to the range of a healthy norm group.
The correlations of the WHO-5 self-assessments with the SCL90-R global scores are displayed in Figure 1C. With regard to well-established clinical scales, relationships between the response and explanatory variables were obtained; for the Clinical Global Impressions Scale (CGI), WHO-5 decreased by 8.51 per CGI increase to measure the severity of psychopathology and for the Global Assessment of Functioning scale (GAF), the WHO-5 increased by 0.70 points per GAF point increase.
Next, the development of patients diagnosed with a depressive episode under telepsychiatric treatment was investigated, as these patients were significantly more severely affected based on clinical judgment than patients with other psychiatric disorders: The CGI was significantly higher for patients diagnosed with depression (4.98 ± 0.89) than for those without (4.70 ± 0.92, p < 0.05, Mann-Whitney test, Figure 2A). In addition, GAF scores were significantly lower for depressive participants (57.46 ± 10.77) than for those participants with other psychiatric issues (62.18 ± 10.77, p < 0.05, Mann-Whitney test, Figure 2B). Depressive patients also scored significantly lower in the WHO-5 in the first inquiry before the start of telepsychiatric treatment [Figure 2C, depressive patients 18.80 ± 14.57 vs. others 30.92 ± 22.00, p < 0.001, two-way repeated measures analysis of variance (ANOVA) with post-hoc Bonferroni]. However, during the course of telepsychiatric treatment WHO-5-scores improved for depressed patients to a level comparable to patients with other psychiatric disorders, who were clinically less severely ill at the beginning of treatment (Figure 2C, p = 0.22 for inquiry 2 comparing patients with and without depression and p > 0.99 for inquiry 3, ANOVA with post-hoc Bonferroni). In particular, patients with depression reported an improvement of >20% on the WHO-5, while subjects with chronic disorders like personality disorders or hyperkinetic disorders, who completed the 2nd and 3rd survey of the WHO-5, indicated a decline in mental wellbeing (Figure 2D). Also, potentially protective or supportive sociodemographic characteristics of depressed patients that were lacking in other patient groups and potentially facilitated their recovery were investigated. However, when examining life and labor situation, education and professional training, children and living situation, as well as debts and the history of criminal assaults, no significant differences were found (Figure 2E).

Figure 2. Based on clinical judgment using the clinical scores, CGI (A) and GAF (B) patients diagnosed with depression were significantly sicker than subjects with other psychiatric entities (for both CGI and GAF Mann-Whitney test was used to compare participants with and without a diagnosis of depression). For the CGI the following scale was used to rate the severity of psychopathology: 1 = normal, not at all ill; 2 = borderline mentally ill; 3 = mildly ill; 4 = moderately ill; 5 = markedly ill; 6 = severely ill; 7 = among the most extremely ill patients. The GAF scale measures how much a person‘s symptoms affect their day-to- day life on a scale of 0–100 (with 100 = not affected at all, 0 = severely affected). (C) Although depressive patients scored lower in the WHO-5 than patients with other psychiatric entities (results inquiry 1 of depressive patients vs. others, p < 0.001, ANOVA with post-hoc Bonferroni), overall wellbeing of this patient cohort improved in such a way, that during the 2nd and 3rd inquiry, WHO-5 total scores significantly raised (inquiry 1 vs. 2, p < 0.05; inquiry 1 vs. 3, p < 0.001, ANOVA with post-hoc Bonferroni) to the same levels as found in patients without a diagnosis of depression. Results are presented in percentage with 0% reflecting very impaired wellbeing and 100% representing perfect wellbeing. (D) Table depicting the number of participants diagnosed with different psychiatric entities and how many of these subjects reported a decline or improvement in wellbeing according to the WHO-5 during the course of the telemedical counseling. (E) Violin plots showing sociodemographic characteristics for the two cohorts (subjects diagnosed with depression and those without). Using the same different subcategories as described in Table 1 (Children: 1 = no children, 2 = children; history of criminal assaults: 1 = no criminal assaults, 2 = criminal assaults, 3 = not specified; education: 1 = no school graduation, 2 = 9 years of school education completed, 3 = 10 years of school education completed, 4 = >12 years of school education completed; Debts: 1 = no debts, 2 = debts; labor situation: 1 = unemployed, 2 = employed, 3 = retired, 4 = disabled; living situation: 1 = living alone, 2 = living with a partner, 3 = living with family or friends, 4 = living in supervised accommodation; marital status: 1 = single, 2 = in relationship with a partner; professional training: 1 = no completed professional training, 2 = completed apprenticeship, 3 = completed academic studies, 4 = apprenticeship on-going, 5 = academic studies on-going), we did not find a significant difference between the distribution of sociodemographic characteristics. Results are presented in mean ± SEM; *P < 0.05, **P < 0.01, ***P < 0.001.
At the end of the study period, patients were asked to evaluate the telepsychiatric treatment they had received. Most consultations were arranged via phone (89.29%, Table 4 vs. 10.71% via video call) and technical problems were rarely an issue (87.50%). More than 80% of participants (81.48%, Table 4) were satisfied with telemedical treatment. 49.07% (Table 4) of subjects experienced telepsychiatric treatment as effective as face-to-face treatment. Almost half of the patients (49.54%, Table 4) considered using telemedicine in the future again. In particular female patients rated telemedical treatment as equivalent to personal appointments (r = 0.413, Spearman‘s correlation) and expressed their wish to use telemedicine in the future again (r = 0.342, Spearman‘s correlation). The more telepsychiatric sessions subjects attended the more likely they were to experience telepsychiatry as equal to conventional psychiatric outpatient treatment (r = 0.231, Spearman‘s correlation). When participants were asked to describe pros and cons of telepsychiatry, half of the participants providing feedback (102 statements) missed the personal atmosphere when talking face to face, while a quarter even reported to have missed substantial information of the conversations due to missing gestures and body language. 16.7% could not describe any disadvantage at all. 46.1% found telepsychiatry much more comfortable compared to conventional treatment, as it was secure to prevent any kind of infection (10.8%) and required less time. A substantial proportion of patients (27.4%) reported to feel less stressed during telepsychiatric treatment when providing intimate details of their biography while sitting in a familiar environment at home.
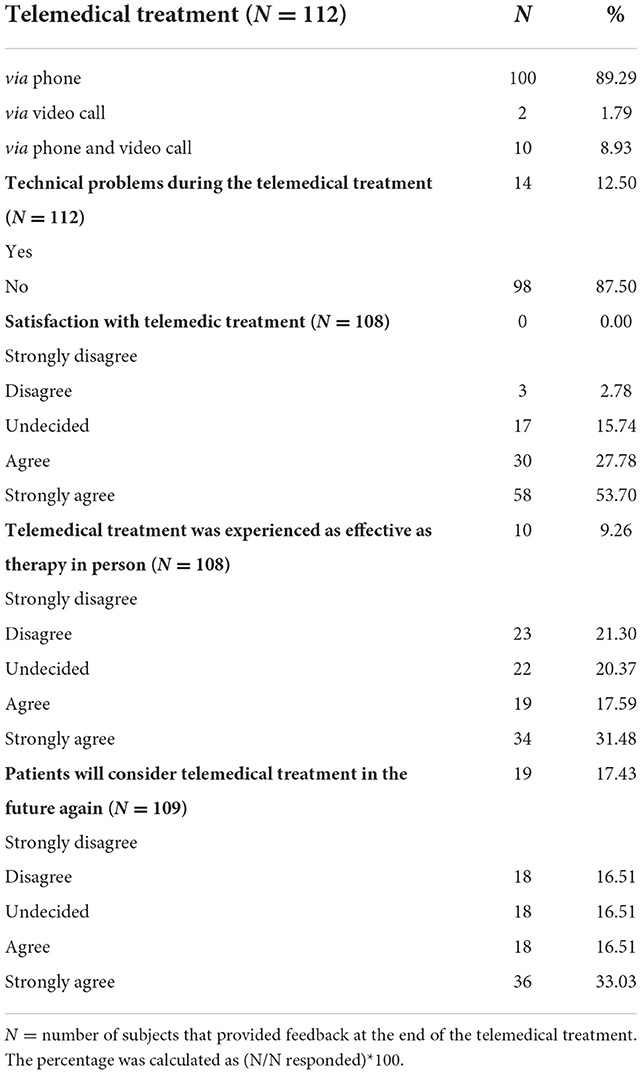
Table 4. Results of the evaluation of the telemedical psychiatric counseling by the study participants requesting feedback considering the mode of telemedical treatment, problems that emerged during telemedical treatment, overall satisfaction and if subjects are willing to use telemedical offers in the future.
The current study aimed at longitudinally investigating the applicability and effectiveness of telemedical treatment in a naturalistic monocentric sample of psychiatric outpatients during the first waves of the COVID-19 pandemic in Germany. A secondary aim was to identify clusters of psychopathology and determine sociodemographic features that were indicative of a favorable response to telemedical psychiatric outpatient treatment. Lastly, the study addressed patients' perceptions of telemedical treatment.
More than one third of participants was diagnosed with a hyperkinetic disorder, mostly attention deficit hyperactivity disorder (ADHD) or attention deficit disorder (ADD), probably due to the professional specialization of general psychiatric outpatient services at the CIMH. Almost a quarter of participants was diagnosed with a depressive episode as the main diagnosis during the treatment interval of concern. However, psychopathology in the entire sample, as rated by clinicians, was dominated by symptoms of depression and anxiety in a majority of participants at the onset of telemedical treatment. This is consistent with earlier findings concerning psychological distress linked to the outbreak of the COVID-19 pandemic (22).
Most participants reported poor wellbeing and high rates of depression before the onset of telemedical psychiatric outpatient treatment on the WHO-5 and showed significant improvement 8–12 weeks after the initiation of telemedical treatment. Furthermore, the study population showed a significant degree of psychological distress as measured by the SCL 90-R, both on a global scale (GSI) as well as concerning symptom intensity (PSDI) and quantitative symptom load (PST). In this line, participants' self-assessments via the SCL 90-R revealed a significant burden in all nine primary symptom dimensions of the SCL 90-R, centering around the subscales for depressive and obsessive-compulsive symptoms at baseline. After 4–6 weeks a significant reduction of psychopathology, as measured by the SCL 90-R, was observed, partly equivalent to the range of a healthy norm group. Generally, patients' self-assessment via the WHO-5 and the SCL 90-R correlated well with observer-rated impressions on more generic measures of clinical functioning and disorder-severity (CGI, GAF). Thus, the specific conditions of telepsychiatric assessment and treatment did not impede the validity and reproducibility of diagnostic procedures in the study sample. This corroborates earlier findings that the implementation of patient reported outcome measures via telemedicine is a viable way of assessing psychiatric symptoms and psychosocial functioning as well as monitoring clinical changes in order to improve treatment outcomes (23).
Overall, participants diagnosed with depressive disorders during telemedical treatment were significantly more affected by a deterioration of wellbeing and functioning than participants suffering from other mental disorders. Yet, during the treatment process, patients with depressive disorders showed a pronounced improvement, whereas individuals with chronic or non-episodic disorders like ADHD and personality disorders did not benefit likewise and—somewhat counterintuitively—showed a decline in mental wellbeing on the WHO-5 during the study period. Specific sociodemographic traits derived from patients' electronic medical records were not associated with this remarkable difference in treatment outcomes, although it could be speculated that chronically impaired individuals might be exposed to more challenging social and environmental conditions (e.g., societal isolation, job insecurity, downward social mobility). Patients with ADHD and other neurodevelopmental disorders may generally be more vulnerable to a variety of negative health outcomes and increased mortality (24). ADHD symptom severity predicted adherence to preventive measures during the pandemic and higher psychological distress (25). Yet, it is unknown if the ADHD patients in our sample experienced higher or equal levels of distress and higher levels of wellbeing before the pandemic. Thus, variance and oscillations of psychopathology in neurodevelopmental disorders, that are predominantly chronic by nature, could not be effectively influenced during the study period by telemedical treatment in our sample. In contrast, available data concerning the telemedical treatment of chronic somatic diseases points at an overall positive effect of telemedicine on the management of these conditions (25). Lastly, these results corroborate findings from an online survey conducted in Russia during early stages of the COVID-19 pandemic that reported elevated stress levels and a more acute response in participants with self-reported affective or anxiety disorders (26). Conversely, this was not accompanied by increased suicide rates in 21 high- and upper-middle-income countries on a global scale (27), although concerns about rising suicide rates in vulnerable individuals, e.g., patients suffering from depression, seemed well founded initially.
Overall, a vast majority of participants reported high satisfaction with and robust acceptance of the telemedical treatment administered during the study period. Roughly 50% of participants, predominantly female, rated telemedical treatment equivalent to treatment provided face to face. This finding seems to be of particular interest as almost 75% of all participants had undergone psychiatric treatment at some point before their participation in this study. Remarkably, patients' satisfaction with telemedical treatment seemed to increase with the number of telemedical consultations. This is in line with findings from a current nationwide multicentric study from Germany where overall good experiences with the telemedical treatment of affective, stress related and somatoform disorders were reported (28).
There are some limitations concerning the above mentioned results that warrant further discussion. Firstly, the study sample might not be fully representative of the entirety of patients that underwent telemedical treatment during the COVID-19 pandemic at the general psychiatric outpatient services of the CIMH. The study sample could be enriched for individuals with an above average willingness to partake in an observational study with repeated surveys. Consequently, severely and extremely mentally ill patients who experience difficulties filling out questionnaires and checklists repeatedly might have been excluded. An earlier study found that older patients and patients with more severe disorders (e.g., schizophrenia) were less likely to use telemedicine, whereas female patients with anxiety and depressive disorders as well as post-traumatic stress disorder (PTSD) more frequently used telemedicine (29). Additionally, the study cohort was enriched with general psychiatric patients, omitting patients seeking treatment in more specialized departments at the CIMH (e.g., the Department of addictive behavior and the Memory Clinic). Therefore, possible selection effects need to be taken into account with regard to the interpretation of the data. Furthermore, participants were not screened for their cultural or ethnic background. Therefore, it cannot be excluded that language or cultural barriers prevented potential participants from being included into the study cohort as described before in a sample of African American patients from North America (7). There is no information regarding the degree of digital literacy in the study sample although it is characterized by a relatively high degree of education. Previous studies demonstrated that healthcare providers' degrees of experience with digital technologies are associated with the willingness to use these technologies and the way they are judged by their users (30). Likewise, the acceptance of telemedicine by its users is shaped by the perceived usefulness of the technologies applied, social influence and personal attitude (31).
Furthermore, nine participants indicated that they did neither identify with the female nor the male gender or felt a mismatch between their gender and their biological sex at baseline (Table 1). Therefore, the authors chose to include these individuals into a third category of gender “not specified,” even if individual patient records indicated an allocation to a specific biological sex. However, these participants were not given the opportunity of further specification later during the study period. Thus, this group of participants is not appropriately represented in our study sample and should be more decidedly addressed by future research.
It cannot be ruled out that the significant improvement in psychopathology and functioning observed in individuals with depressive disorders during telemedical treatment merely corresponds to the naturalistic course of a group of disorders that is generally characterized by an episodic course. Furthermore, a decrease in distress among the study population during the observation period might be partially linked to the gradual suspension of lockdown measures during spring/summer 2020 and spring 2021 as a confounding factor. It has been shown that an escalation of lockdown measures during the COVID-19 pandemic and the rapid spreading of the novel coronavirus reliably lead to a deterioration of mental health in the general population within different cultural backgrounds around the world (32–35). However, more recent studies hint at a persistence of distress and burden of psychopathology independent from periodic intensifications of lockdown measures (6). In our study cohort, there was a marked difference in the decrease of symptom load between participants with episodic, mostly depressive disorders and chronic disorders like ADHD, strengthening the hypothesis that a significant part of the psychopathological improvement experienced by a distinct group of participants in our study truly represents a treatment effect.
Lastly, due to the naturalistic design of the study, there were neither a healthy control group nor placebo or sham treatments included. The latter might in any case have raised serious ethical concerns during a global pandemic. Nevertheless, it could be speculated that the participants in our study were generally more affected by psychological distress compared to the general population since the severity of their symptomatology crossed the threshold for diagnosing one of the above mentioned disorders and was eligible for psychiatric treatment within the German insurance system. However, the precise pre-pandemic level of psychopathology at baseline is not known. Since a majority of patients that enrolled in the study had received psychiatric treatment at some time, however not immediately before the beginning of the study, they might have been at a greater risk for developing clinically relevant psychopathology during the COVID-19 pandemic, a finding that is also supported by results from a French cohort focusing on individuals with a history of depressive episodes (36). After all, it needs to be pointed out the results of this study are not sufficient to assume any causal connection between the psychopathology observed and the COVID-19 pandemic and associated public measures per se. The study population consisted merely of individuals seeking psychiatric counseling and receiving telemedical treatment during the first stages of the COVID-19 pandemic in Germany.
Psychiatric telemedical treatment is an effective treatment option for patients with depressive disorders that yielded overall favorable outcomes in the observed group of patients. Although individuals diagnosed with depression in our sample had a higher load of psychopathology in the beginning, they profited most from telemedical treatment compared to participants with chronic neurodevelopmental disorders like ADHD who experienced an additional decline of wellbeing. The latter finding indicates that future research needs to concentrate on improving telemedical treatment options suited for chronic psychiatric conditions. Our study demonstrated a good match between patient-reported standardized measures of psychopathology and clinicians' assessments during telemedical treatment, indicating that telemedical consultations could be a simple, economic and cost-effective but nevertheless reliable way of monitoring symptom severity and directing treatment choices during the treatment of depressive disorders. This is complemented by the overall high satisfaction of participants with the telemedical treatment they received. Therefore, current research on other, more specific monitoring and treatment tools, e.g., ecological momentary assessment (EMA), seems to open a promising new avenue toward personalized psychiatric telemedical treatment in the near future.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The study design and data acquisition were presented to the Ethics Committee II at the medical faculty Mannheim, University of Heidelberg and approved (No. 2020-562N). The patients/participants provided their written informed consent to participate in this study.
A-SW and PP designed the study. TR, PP, and A-SW acquired data and wrote the manuscript with the help of all authors. AB developed the online survey tool. TR, TP, and A-SW analyzed data. OH, HT, and AM-L advised and discussed data. All authors have read and approved the manuscript.
A-SW was a recipient of the Branco Weiss Society in Science Fellowship and of the Wrangell Habilitation Scholarship. Otherwise, this research did not receive a specific grant from any funding agency in the public, commercial, or non-profit sectors.
The authors thank the service and telephone team of the outpatient clinic at the Central Institute of Mental Health Mannheim, Germany, under the lead of Volker Nitschke for their help with the recruitment of study subjects as well as Gerhard Kühne for the help with the analysis of data from the electronic medical records.
Author A-SW is a recipient of the Margarete Wrangell habilitation fellowship and the Branco Weiss Society in Science Fellowship.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.971896/full#supplementary-material
1. Sood S, Mbarika V, Jugoo S, Dookhy R, Doarn CR, Prakash N, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed e-Health. (2007) 13: 573–90. doi: 10.1089/tmj.2006.0073
2. Siegel A, Zuo Y, Moghaddamcharkari N, McIntyre RS, Rosenblat JD. Barriers, benefits and interventions for improving the delivery of telemental health services during the coronavirus disease 2019 pandemic: a systematic review. Curr Opin Psychiatr. (2021) 34:434–43. doi: 10.1097/YCO.0000000000000714
3. Bashshur RL, Shannon GW, Bashshur N, Yellowlees PM. The empirical evidence for telemedicine interventions in mental disorders. Telemed e-Health. (2016) 22:87–113. doi: 10.1089/tmj.2015.0206
4. Fu Z, Burger H, Arjadi R, Bockting CLH. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. (2020) 7:851–64. doi: 10.1016/S2215-0366(20)30256-X
5. Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005–2017. JAMA. (2018) 320:2147–9. doi: 10.1001/jama.2018.12354
6. Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Int Med. (2021) 181:388–91. doi: 10.1001/jamainternmed.2020.5928
7. Xue Y, Saeed SA, Liang H, Jones K, Muppavarapu KS. Investigating the Impact of COVID-19 on telepsychiatry use across sex and race: a study of north carolina emergency departments. Telemed e-Health. (2022) 28:1431–9. doi: 10.1089/tmj.2021.0549
8. Basit SA, Mathews N, Kunik ME. Telemedicine interventions for medication adherence in mental illness: a systematic review. General Hospital Psychiatr. (2020) 62:28–36. doi: 10.1016/j.genhosppsych.2019.11.004
9. Guaiana G, Mastrangelo J, Hendrikx S, Barbui C. A systematic review of the use of telepsychiatry in depression. Community Ment Health J. (2021) 57:93–100. doi: 10.1007/s10597-020-00724-2
10. Bessonova L, et al. Clinical management of patients with schizophrenia treated with long-acting injectable antipsychotics and telepsychiatry use during COVID-19 pandemic. CNS Spectr. (2022) 27:230. doi: 10.1017/S1092852922000256
11. Fortier CB, Currao A, Kenna A, Kim S, Beck BM, Katz D, et al. Online telehealth delivery of group mental health treatment is safe, feasible, and increases enrollment and attendance in post-9/11 U.S. veterans. Behav Ther. (2022) 53:469–80. doi: 10.1016/j.beth.2021.11.004
12. Barnett P, Goulding L, Casetta C, Jordan H, Sheridan-Rains L, Steare T, et al. Implementation of telemental health services before COVID-19: rapid umbrella review of systematic reviews. J Med Internet Res. (2021) 23:e26492. doi: 10.2196/26492
13. Lyles CR, Wachter RM, Sarkar U. Focusing on digital health equity. JAMA. (2021) 326:1795–6. doi: 10.1001/jama.2021.18459
14. Primack BA. The WHO-5 Wellbeing index performed the best in screening for depression in primary care. ACP J Club. (2003) 139:48. doi: 10.1136/ebm.8.5.155
15. Peveler RC, Fairburn CG. Measurement of neurotic symptoms by self-report questionnaire: validity of the SCL-90R. Psychol Med. (1990) 20:873–9. doi: 10.1017/s0033291700036576
16. Grootenboer EMV, Giltay EJ, van der Lem R, van Veen T, van der Wee NJA, Zitman FG. Reliability and validity of the Global Assessment of Functioning Scale in clinical outpatients with depressive disorders. J Eval Clin Pract. (2012) 18:502–7. doi: 10.1111/j.1365-2753.2010.01614.x
17. Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry. (2007) 4:28–37.
18. WHO Regional Office for Europe. Wellbeing Measures in Primary Health Care. Report on a WHO Meeting, Stockholm, Sweden (1998).
19. Derogatis L, Savitz K. The SCL-90-R, brief symptom inventory, and matching clinical rating scales. In: The use of psychological testing for treatment planning and outcomes assessment (2nd Edn.). Lawrence Erlbaum Associates Publishers (1999).
20. Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 wellbeing index: a systematic review of the literature. Psychother Psychosom. (2015) 84: 84:167–76. doi: 10.1159/000376585
21. Franke GH. Möglichkeiten und Grenzen im Einsatz der Symptom-Checkliste SCL-90-R. Verhaltenstherapie und psychosoziale Praxis. (2001) 33:475–85.
22. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
23. Kablinger AS, Gatto AJ, O'Brien VC, Ko H, Jones S, McNamara RS, et al. Effects of COVID-19 on patients in adult ambulatory psychiatry: using patient-rated outcome measures and telemedicine. Telemed e-Health. (2022) 28:1421–30. doi: 10.1089/tmj.2021.0642
24. Catalá-López F, Hutton B, Page MJ, Driver JA, Ridao M, Alonso-Arroyo A, et al. Mortality in persons with autism spectrum disorder or attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. JAMA Pediatrics. (2022) 176:e216401. doi: 10.1001/jamapediatrics.2021.6401
25. Pollak Y, Shoham R, Dayan H, Gabrieli-Seri O, Berger I. Symptoms of ADHD predict lower adaptation to the covid-19 outbreak: financial decline, low adherence to preventive measures, psychological distress, and illness-related negative perceptions. J Atten Disord. (2022) 26:735–46. doi: 10.1177/10870547211027934
26. Sorokin MY, Kasyanov ED, Rukavishnikov GV, Khobeysh MA, Makarevich OV, Neznanov NG. Determinants of stress levels and behavioral reactions in individuals with affective or anxiety disorders during the COVID-19 pandemic in Russia. Front Sociol. (2022) 7:870421. doi: 10.3389/fsoc.2022.870421
27. Pirkis J, John A, Shin S, DelPozo-Banos M, Arya V, Analuisa-Aguilar P, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. (2021) 8:579–88. doi: 10.1016/S2215-0366(21)00091-2
28. Wiegand HF, Bröcker AL, Fehr M, Lohmann N, Maicher B, Röthke N, et al. Changes and challenges in inpatient mental health care during the first two high incidence phases of the COVID-19 pandemic in Germany - results from the COVID PSI psychiatry survey. Front Psychiatry. (2022) 13:855040. doi: 10.3389/fpsyt.2022.855040
29. Ainslie M, Brunette MF, Capozzoli M. Treatment interruptions and telemedicine utilization in serious mental illness: retrospective longitudinal claims analysis. JMIR Ment Health. (2022) 9:e33092. doi: 10.2196/33092
30. Wilczewski H, Paige SR, Ong T, Barrera JF, Soni H, Welch BM, et al. Perceptions of telemental health care delivery during COVID-19: a cross-sectional study with providers, February–March 2021. Front Psychiatry. (2022) 13:855138. doi: 10.3389/fpsyt.2022.855138
31. Harst L, Lantzsch H, Scheibe M. Theories predicting end-user acceptance of telemedicine use: systematic review. J Med Int Res. (2019) 21:e13117. doi: 10.2196/13117
32. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
33. Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. J Epidemiol Community Health. (2021) 75. doi: 10.1136/jech-2020-215060
34. Pandey D, Bansal S, Goyal S, Garg A, Sethi N, Pothiyill DI, et al. Psychological impact of mass quarantine on population during pandemics-The COVID-19 Lock-Down (COLD) study. PLoS ONE. (2020) 15:e0240501. doi: 10.1371/journal.pone.0240501
35. Wang C, Song W, Hu X, Yan S, Zhang X, Wang X, et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatr. (2021) 21:99. doi: 10.1186/s12888-021-03108-2
Keywords: telemedicine, psychiatry, depression, wellbeing, chronic disorders
Citation: Rohrmann T, Praus P, Proctor T, Benedyk A, Tost H, Hennig O, Meyer-Lindenberg A and Wahl A-S (2022) Patients with affective disorders profit most from telemedical treatment: Evidence from a naturalistic patient cohort during the COVID-19 pandemic. Front. Psychiatry 13:971896. doi: 10.3389/fpsyt.2022.971896
Received: 17 June 2022; Accepted: 04 November 2022;
Published: 01 December 2022.
Edited by:
Oswald David Kothgassner, Medical University of Vienna, AustriaReviewed by:
Grigory Rukavishnikov, St.Petersburg V.M. Bekhterev Psychoneurological Research Institute, RussiaCopyright © 2022 Rohrmann, Praus, Proctor, Benedyk, Tost, Hennig, Meyer-Lindenberg and Wahl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna-Sophia Wahl, QW5uYVNvcGhpYS5XYWhsQG1lZC51bmktbXVlbmNoZW4uZGU=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.