- 1Health Promotion Division, Public Health Foundation of India, New Delhi, India
- 2Health Related Information Dissemination Amongst Youth (HRIDAY), New Delhi, India
- 3Los Angeles County Department of Public Health, Los Angeles, CA, United States
- 4Madras Diabetes Research Foundation & Dr. Mohan’s Diabetes Specialities Centre, Chennai, Tamil Nadu, India
- 5Centre for Chronic Conditions and Injuries (CCCI), Public Health Foundation of India & Centre for Chronic Disease Control, New Delhi, India
- 6Hubert Department of Global Health, Emory University, Atlanta, GA, United States
- 7King’s College London, London, United Kingdom
- 8Department of Endocrinology, All India Institute of Medical Sciences, National Capital Territory of Delhi, New Delhi, India
Background: The world witnessed a highly contagious and deadly disease, COVID-19, toward the end of 2019. India is one of the worst affected countries. We aimed to assess anxiety and depression levels among adult tobacco users and people who recently quit tobacco during COVID-19 lockdown in India.
Materials and methods: The study was conducted across two Indian cities, Delhi and Chennai (July-August, 2020) among adult tobacco users (n = 801). Telephonic interviews were conducted using validated mental health tools (Patient Health Questionnaire-PHQ-9 and Generalized Anxiety Disorder-GAD-7) to assess the anxiety and depression levels of the participants. Descriptive analysis and multiple logistic regression were used to study the prevalence and correlates of depression and anxiety.
Results: We found that 20.6% of tobacco users had depression symptoms (3.9% moderate to severe); 20.7% had anxiety symptoms (3.8% moderate to severe). Risk factors associated with depression and anxiety included food, housing, and financial insecurity.
Conclusion: During COVID-19 lockdown, mental health of tobacco users (primarily women) was associated with food, housing and financial insecurity. The Indian Government rightly initiated several health, social and economic measures to shield the most vulnerable from COVID-19, including a ban on the sale of tobacco products. It is also necessary to prioritize universal health coverage, expanded social security net, tobacco cessation and mental health services to such vulnerable populations during pandemic situations.
Introduction
The novel Coronavirus or SARS CoV-2, which began in late 2019, has infected more than 25 million people worldwide thus far and still increasing (1). Besides the massive human toll and economic burden on the Indian healthcare system, the pandemic also posed a myriad of challenges for the country’s public health system. As the primary preventive strategy, India went under a nationwide lockdown in March 2020 (2). Strict lockdown regulations and, most importantly, the forced social confinement, disrupted the supply chain of essential commodities, affecting the nation’s mental health as a whole (3, 4). Fear, anxiety, depression, and insomnia were a few common mental health issues detected in the population during the lockdown (5, 6). COVID-19 Mental Disorders Collaborators concluded that the pandemic led to a 27⋅6% increase in cases of major depressive disorders and 25⋅6% increase in cases of anxiety disorders, globally (7). There is a complex relationship between COVID-19 and smoking. Tobacco users are at increased risk of adverse outcome like death and severity of COVID-19 infection (8). Considering this, the Government of India issued several advisories to prohibit the use and spitting of tobacco in public places (9). Subsequently, more stringent tobacco control measures were implemented in India such as banning the sale and use of tobacco products in public places to prevent spitting during COVID-19 (10). A cross-sectional study found that nearly half of the users couldn’t easily access tobacco products during this period (11). There are complex and often bidirectional dynamics between substance abuse and mental health problems (12, 13) which are often believed to co-exist (14).
A study conducted following the outbreak of COVID-19, suggested increased mental health problems during the pandemic was associated with increased tobacco use as well (15). However, there is conflicting as well scant scientific literature regarding mental health disorders among tobacco users in India, particularly considering the realities of the pandemic.
While we are trying to cope and adapt to the new normal with all the focus on containing the pandemic, the mental health impact due to the unprecedented situation created during these times remains unaddressed. These challenges pose even a more significant threat, especially in tobacco consumer groups, especially when there is no capacity and networks for provision of psychosocial support during these vulnerable times. The research evidence reveals significant associations were observed between different smoking behavior groups and psychosocial factors (15). Therefore, there is an urgent requirement to understand and address the psychological burden of tobacco users as well. Hence, this cross-sectional study was conducted to assess the prevalence and correlates of anxiety and depression among adult tobacco users during the COVID-19 restrictions in India.
Materials and methods
Study design, setting, and participants
A cross-sectional study was conducted in New Delhi and Chennai (India) between July and August 2020. The study was conducted with adult tobacco users (n = 801), both males (n = 722) and females (n = 79). The inclusion criteria being participant’s consent to participate, aged 20 years or above, people who can understand Hindi, English, and Tamil, and be a current tobacco user (any form of tobacco). The participants who were institutionalized, unable to respond the survey, not speak or understand Hindi, English, or Tamil and not willing to provide or record verbal consent were excluded from the study. The participants who used tobacco in any form in the past one month (from the onset of the survey, i.e, July 2020) or have quit tobacco during past three months (from the onset date of the survey) were included in the survey. The study participants were recruited from the pre-existing cohort of the CARRS study (”Centre for Cardiometabolic Risk Reduction in South Asia-CARRS), a model surveillance system for cardio-metabolic diseases (16). Considering the large target population (over 1 million), assuming a 5% margin of error, with a 95% confidence level, we estimated a minimum sample size of ∼800 for our study.
Data collection
The study data were collected through telephonic interviews, administered by a trained research team, using a standardized protocol. The telephonic interview technique was adopted for data collection to counter the spread of COVID-19 and protect all individuals associated. The questionnaires were administered in English, Hindi, or Tamil, based on the participants’ preferences. Team of researchers were skilled to conduct interviews in the respective languages. Those eligible to participate were then asked for informed consent. The verbal consent was audio-recorded following the Indian Council of Medical Research’s revised guidelines for obtaining consent for biomedical and health research during the COVID-19 pandemic (17). This method was approved by the Ethics Committee. Prior ethics approval for the research involving human subjects was obtained from the Centre for Chronic Disease Control’s Institutional Ethics Committee (Reference # CCDC_IEC_04_2018).
Study instruments and measures
A validated mental health tool, i.e., Patient Health Questionnaire-9 (PHQ-9), was used in our study to assess the symptoms of depression and anxiety among tobacco users (18, 19). Participants assigned each indicator (e.g., little interest or pleasure in doing things) a value based on the frequency of symptoms they experienced over the preceding two weeks, on a 4-point scale – 0 (not at all), 1 (several days), 2 (more than half the days) and 3 (nearly every day). The total score ranged from zero to 27. The participants were categorized for the severity of depression based on cumulative scores. A score of 4 or lower was dismissed for signs of depression, 5 to 9 fell into mild, 10 to 14 reflected moderate depression, 15 to 19 was moderately severe depression, and anything beyond 20 was severe depression (18). These scores were further re-coded for analysis; scores 4 or lower were coded as 0 or “having no symptoms of depression,” and scores ≥ 5 were coded as 1 or “with depression symptoms” (20).
Likewise, Generalized Anxiety Disorder-7 (GAD-7) was used to assess self-reported symptoms of anxiety (21). The study participants ranked each item (e.g., not being able to stop or control worrying) based on the recurrence of symptoms in the previous two weeks on a 4-point scale – 0 (not at all), 1 (several days), 2 (more than half the days) and 3 (nearly every day). The aggregate score ranged from 0 to 21. Scores of 4 or lower reflected no anxiety, 5 to 9 represented mild anxiety, 10 to 14 indicated moderate anxiety, and 15 to 21 indicated severe anxiety (22). During analysis, scores 0 to 4 were coded as 0 or “having no symptoms of anxiety,” and scores ≥ 5 were coded as 1 or “with symptoms of anxiety.”
Additional demographic information, namely age, sex, education level, employment status, were gathered. Particulars about the participants’ pre-existing comorbidities (e.g., diabetes, hypertension, stroke, cancer) were obtained from the CARRS database. Additional information on variable definitions is presented in Supplementary Table 1.
Statistical analysis
Chi-square test and Fisher’s Exact test were used to determine univariate associations between the socio-demographic characteristics and depression, and anxiety. Unpaired (two-sample) t-test was used to compare the mean score of depression and anxiety among male and female participants. The threshold for significance was set at p < 0.05. The data are displayed as a mean score ± (SD), proportions, and percentages. Multiple logistic regression analysis was used to determine Odds Ratios (OR) and 95% Confidence Intervals (95% CI) for associations between dependent variable depression (coded 1 = depression present, 0 = depression absent) and other predictor variables. Participant’s location, sex, age, education, employment status, and other variables like financial status during the lockdown, food, and housing insecurity were treated as independent variables. Similarly, for the other dependent variable, anxiety (coded, 1 = anxiety present, 0 = anxiety absent), the same independent variables were used in the regression model. All tests were considered significant at the 0.05 level. The independent variables were examined for multicollinearity. The VIF values were less than ten, indicating no evidence of multicollinearity (18). The data were analyzed using STATA 13.0 (StataCorp, LP, Texas) (23).
Results
Study participants’ characteristics
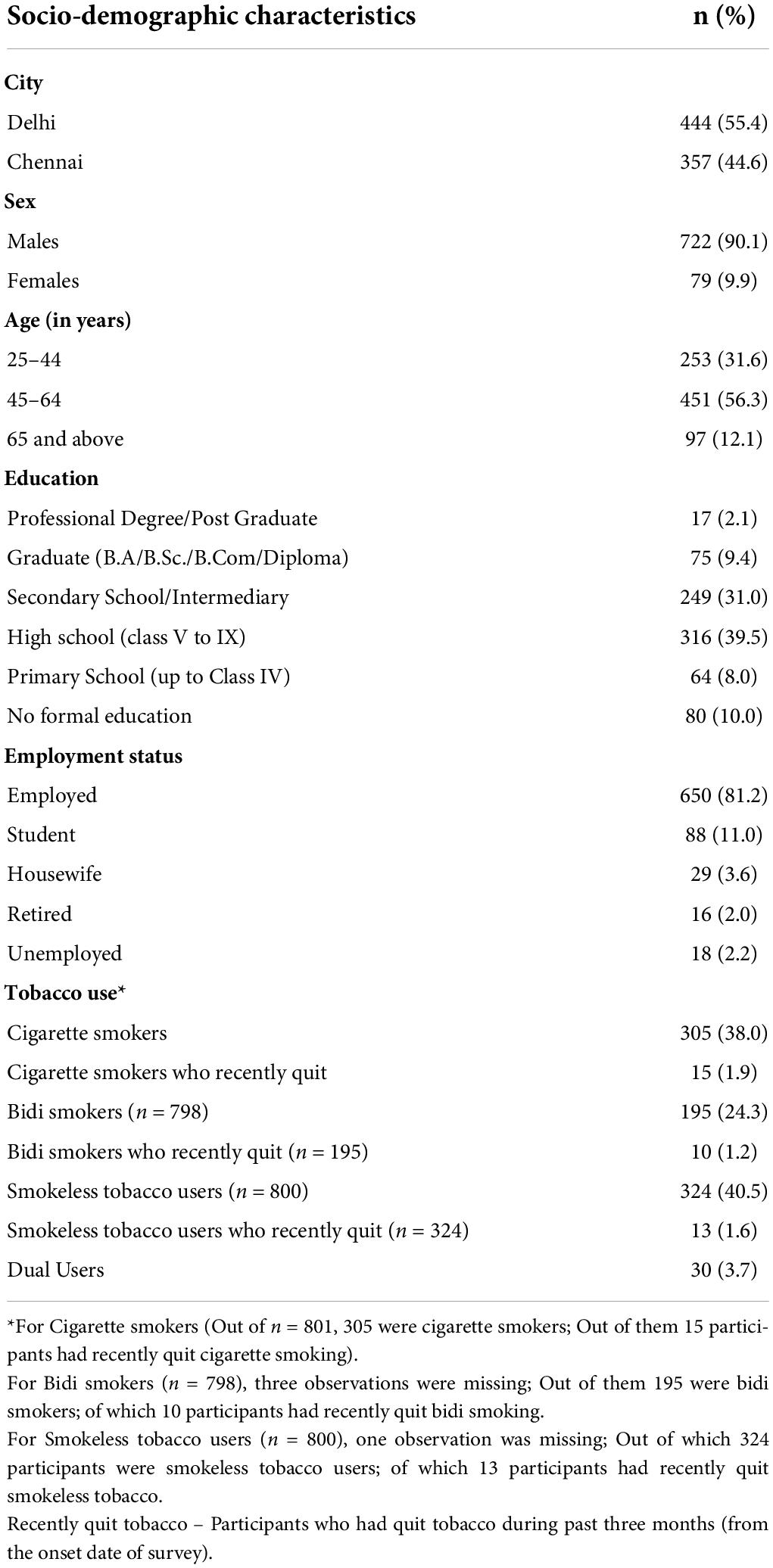
In total, 2,505 adult tobacco users from Delhi (n = 1365) and Chennai (n = 1140) were approached to participate in our study. A total of 801 tobacco users participated in the survey out of whom, 444 (55.4%) were from Delhi while 357 (44.6%) from Chennai. As the survey was conducted telephonically, a disposition table is used to explain the response rates [Supplementary Tables 2, 3]. The gross response rate for the study was 48.4%, the basic response rate was 85.3% and the response rate calculated using the CASRO Estimator (24) was 60.9%. Roughly 90% of the adult tobacco users were males, and 87.9% were in the age group of 25-64 years. The majority (81.2%) were employed, and 11.5% had a bachelor’s degree and above. The study participants’ mean age was 50.5 years, with a range from 25 to 90 years. The majority of tobacco users were smokeless tobacco users (40.5%), followed by cigarette smokers (38.0%) and bidi smokers (24.3%) (Table 1).
Prevalence of depressive symptoms among tobacco users
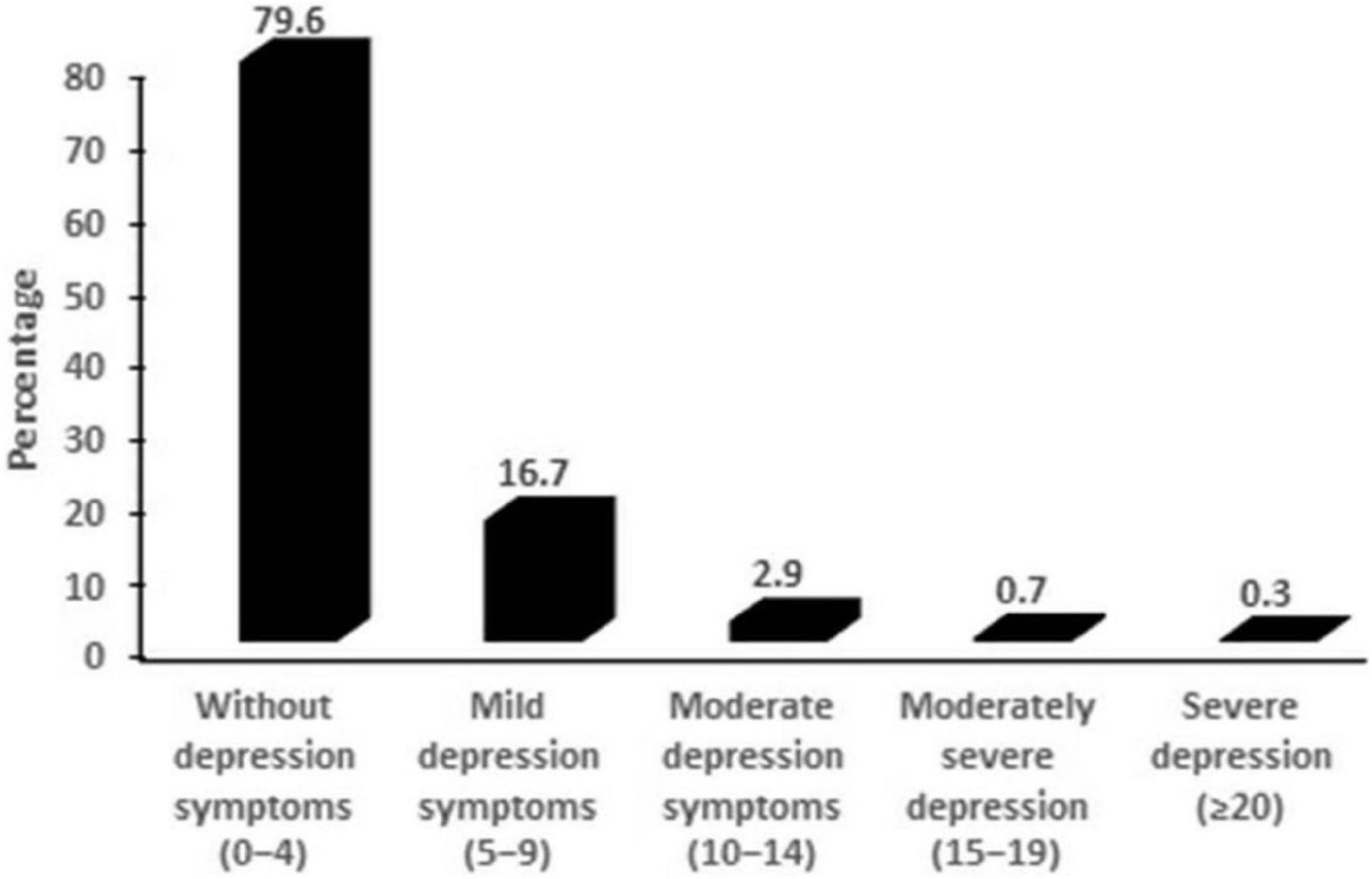
The mean PHQ-9 score for the study participants was 2.5 ± (3.4). Of the 763 complete responses, 20.6% of tobacco users were found to have depression symptoms (PHQ-9 score > 4). About 16.7% of participants reported mild depression symptoms (PHQ-9 score between 5 and 9), 2.9% experienced moderate depression (PHQ-9 score between 10 and 14), 0.7% had moderately severe depression (PHQ-9 score 15–19), and 0.3% had severe depression (PHQ-9 score 20–27) (Figure 1). The mean depression score for females was 3.2 ± (3.1), which was significantly higher than that for males 2.4 ± (3.4). (p = 0.02).
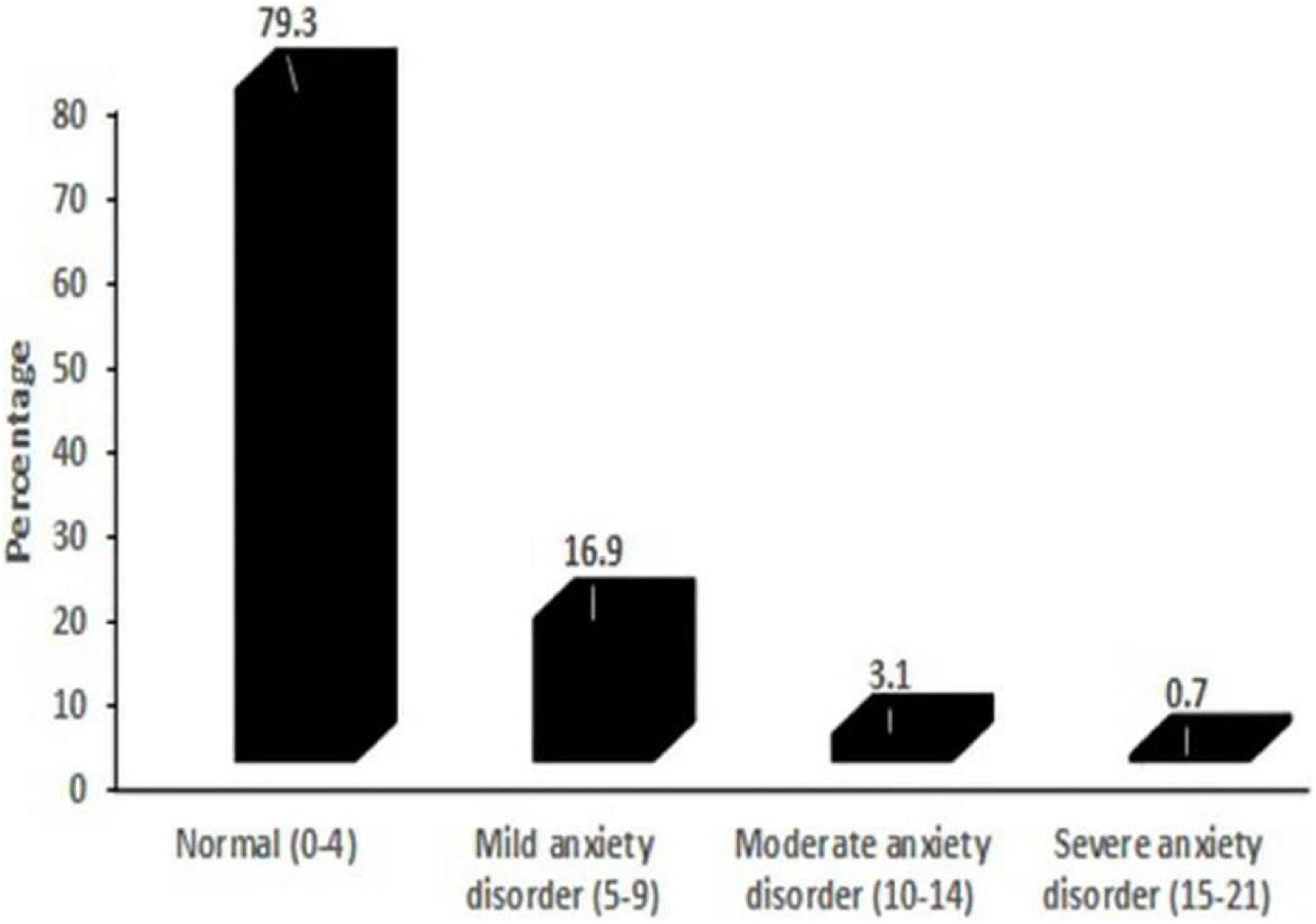
Figure 2 represents the distribution of the tobacco users according to the GAD-7 score. The mean GAD-7 score for the study participants was 2.4 (SD ± 3.2). Of the 774 respondents responding to anxiety questions, 20.7% had a GAD score greater than 4. The prevalence of mild anxiety (GAD score 5–9) was 16.9%, 3.1% had moderate anxiety symptoms (GAD score 10–14), and 0.7% had severe anxiety symptoms (GAD score 15–21). When analyzed along gender lines, the mean anxiety score for females was 3 ± (3.2), significantly higher than the mean scores for males at 2.3 ± (3.20) (p = 0.02).
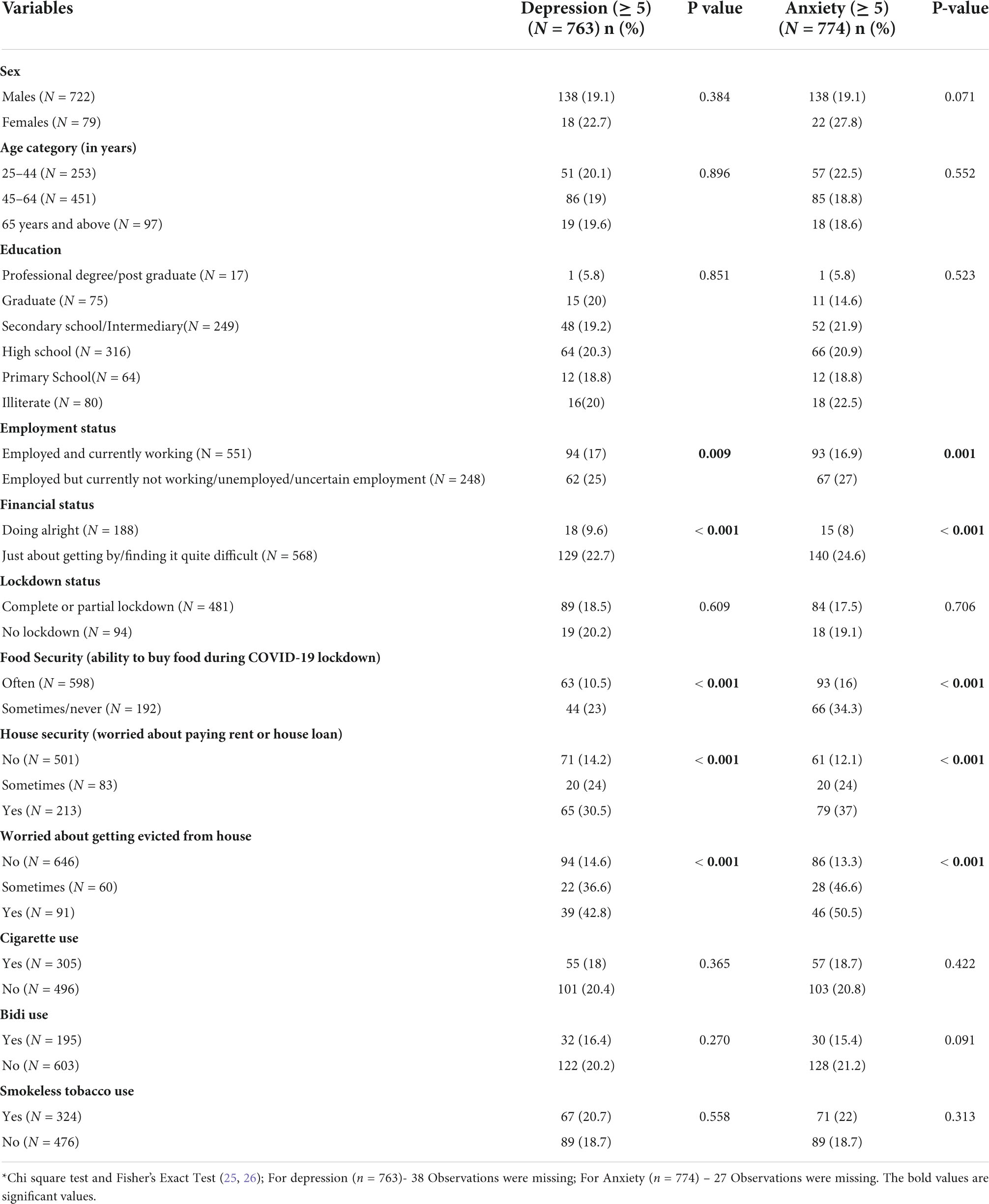
Table 2 shows the univariate associations of depression and anxiety with the socio-demographic as well as other independent variables. The symptoms of anxiety appeared in 27% and depression in 25% of the study participants, who were employed but currently not working, unemployed, or had uncertain employment status. In contrast, among the individuals who were employed and currently working, 17% experienced depression and 16.9% anxiety.
Individuals experiencing poor financial status displayed a marked distinction in depression (22.7%) and anxiety symptoms (24.6%) when compared to those who claimed to be financially secure and stable during the pandemic-depression (9.6%) and anxiety (8%). Tobacco users who reported the ability to buy food sometimes or never during COVID-19 lockdown had significantly higher rates of depression (23%) and anxiety symptoms (34.3%) as opposed to (10.5%) and (16%) in people who could often buy food during the pandemic. Of the individuals who were worried about paying house rent or loans, 30.5% claimed to have depression, and 37% reported anxiety symptoms, starkly distinguished from individuals who were not worried had depression (14.2%) and anxiety (12.1%) respectively. The participants who worried about being evicted from homes were significantly more depressed (42.8%) as compared to those who were not worried (14.6%) and reported anxiety symptoms in 50.5% of participants as compared to those who were not worried (13.3%). We observed that the prevalence of depression and anxiety symptoms did not change with the presence of lockdown restrictions or by type of containment zones (P > 0.05).
We observed that the presence of depression and anxiety symptoms did not change with the type of tobacco use and did not differ significantly between single and dual/multiple tobacco product users. The people who had recently quit tobacco did not display marked distinction in depression and anxiety symptoms than current tobacco users.
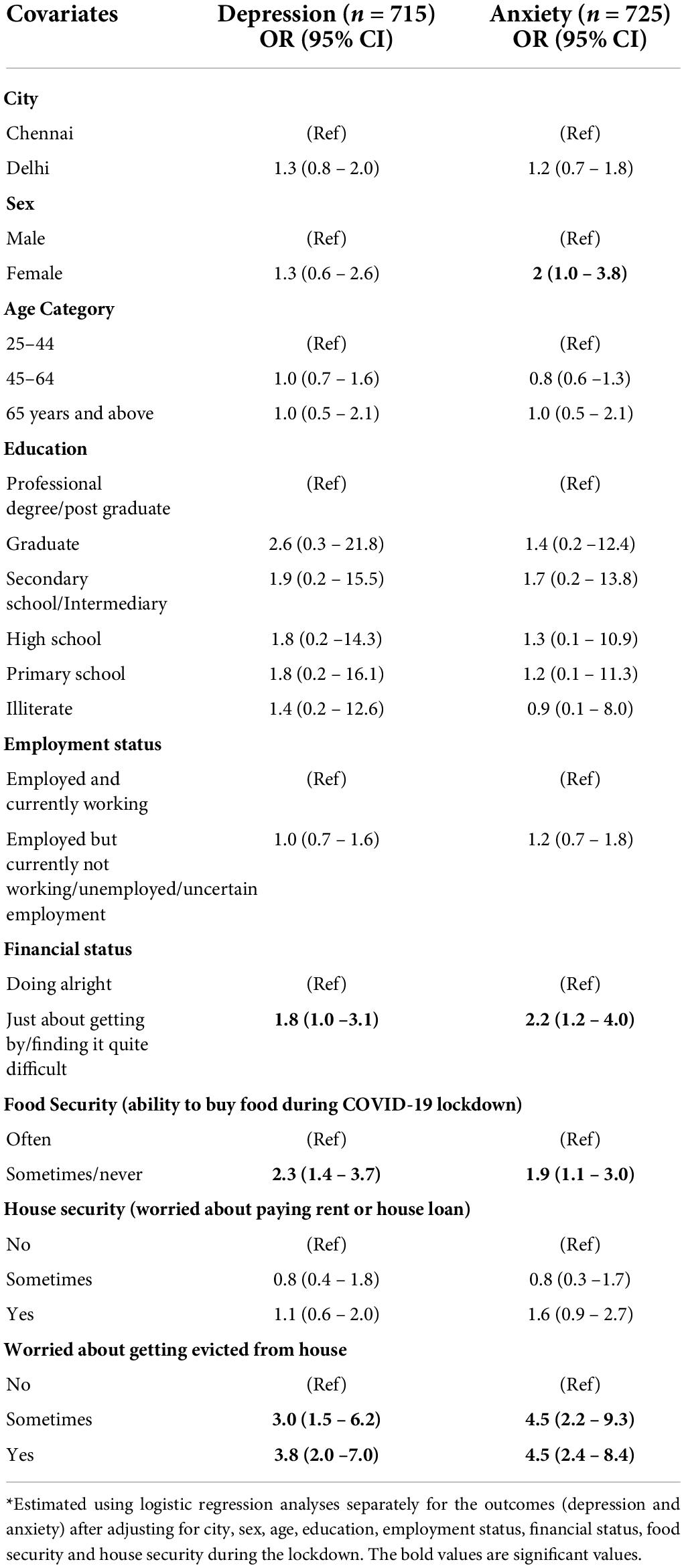
Table 3 represents findings from the logistic regression analysis assessing predictors of depression and anxiety in adult tobacco users during COVID-19. In females, the odds of anxiety were twice that in males (OR = 2, 95% CI 1.0–3.8). The risk of depression was 1.8 times and anxiety 2.2 times among participants who were financially just about getting by or finding it quite difficult as compared to those who were financially doing all right (OR = 1.8, 95% CI 1.0 −3.1 and OR = 2.2, 95% CI 1.2-4.0, respectively). The risk of being depressed was 2.3 times and being anxious, 1.9 times higher in people who could buy food only sometimes or never than in the people who could buy food often during the lockdown (OR 2.3, 95% CI 1.4 – 3.7 and OR 1.9, 95% CI 1.1 – 3.0), respectively.
For participants who were only ‘sometimes worried about getting evicted from the house’, the risk of depression was 3 times and anxiety was 4.5 times more than those who were not worried (OR 3, 95% CI 1.5 – 6.2 and OR 4.5,95% CI 2.2 – 9.3). Furthermore, people who were regularly worried about getting evicted had higher odds of depression (3.8 times) and anxiety (4.5 times) than those who did not worry about evictions (OR 3.8, 95%CI 2.0 –7.0 and OR 4.5, 95% CI 2.4 – 8.4, respectively).
Discussion
The COVID-19 pandemic has caused unprecedented changes around the globe in a very short time, affecting all the facets of people’s lives. This study assessed the levels of psychological distress measured in terms of depression and anxiety in tobacco users and who had recently quit tobacco during the COVID-19 pandemic in India. We found that, 20.5% of study participants had symptoms of depression with the majority experiencing mild depression, and 3.9% experienced moderate to severe depression. Similarly, anxiety was present in 20.7% of tobacco users, with 3.7% experiencing moderate to severe symptoms. The prevalence of anxiety and depression was lower in our study as compared to the other studies conducted among the general population in India and globally during the COVID-19 times (27–29). This could be because our study was limited to tobacco users and people who had recently quit tobacco in two large metropolitan cities of India and was conducted at much later stage of the COVID-19, when gradual easing of lockdown was in process. This was the period when there was relaxation in restrictions which might have led to a relative sense of normalcy. We did not find any association between tobacco use and anxiety and depression symptoms, which could be attributed to the fact that there was limited illegal availability of tobacco products during the ban (11).
The findings of our study showed an association between depression and anxiety symptoms (score ≥ 5) with the present unemployment, financial, food and housing insecurity. Similar findings were observed in an online study conducted in India during the pandemic among the general population where the financial status of the family and ability to access essential supplies were seen to be linked with anxiety and depression (30).
When the depression and anxiety scores were analyzed along gender lines, women had significantly higher scores than males. These findings although cannot be generalized because female population in our sample was skewed.
India’s mental health care system, which is a part of the general health care system, has suffered from sub-optimal investment and was already over-extended and under-resourced even before the advent of the pandemic. It is mostly curative in nature concentrating on providing tertiary care. COVID-19 has caused widespread social and economic turmoil across the globe. Although the Government of India has taken several initiatives to protect the most vulnerable population, there are definite gaps in its reach, nature as well level of protection it offers. Financial insecurities take a definite toll on the mental health of individuals as seen in our study. The pandemic has accentuated the need for a comprehensive social security net now more than ever. This crisis should be seen as an opportunity to rebuild a strong resilient health system to broaden the canopy of universal health coverage. Easy access to tobacco cessation services must be provided as it is crucial for both the physical and mental health of tobacco users.
Strengths and limitations of the study
The strength of our study lies in the fact that it tries to explore the effect of life altering situations during the COVID-19 pandemic on mental health among tobacco users in India. Our questionnaire was designed based on previously validated STOP survey (31). There is a dearth of literature on mental health among tobacco users in the country. Possible limitations of this study include use of telephonic interviews for data collection. This did not allow building up of rapport with the participants which is especially crucial in sensitive topics like mental health. This may not have characterized mental health status of the people with accuracy of structured face to face interviews. There is also the possibility of recall bias because participants may not accurately recall having depression and anxiety symptoms in preceding two weeks. There is also a possibility of depression and anxiety among the participants due to some other reasons not captured through our survey. There are predictive limitations because the study is cross-sectional so causal inferences cannot be drawn. We did not have pre-COVID data on depression and anxiety levels of the study participants to compare. We did not have control group of non-tobacco users so could not assess if tobacco use was one of the correlates of mental health status. The study was conducted across two cities of India namely, Delhi and Chennai and hence, the study findings may not be generalized to entire Indian population. We tried to encompass equal number of males and females, due to societal taboo or other reason a smaller number of females agreed to be part of our study. Hence, it does not generalize our results. However, we able to study the objective of our study despite the limitations. We were not able to use a specific definition of ‘serious illness’ to exclude participants due to the multiplicity of such serious health conditions, however, these excluded participants were deemed to be ill enough so as not to be able to respond to the telephonic survey.
Conclusion
Just over 20% of tobacco users in our study had symptoms of depression or anxiety. We did not find any association between types/number of tobacco products used and depression/anxiety. Financial, food and housing insecurity among tobacco users was associated with higher depression and anxiety levels. The measures enforced by the Government of India to reduce access to tobacco products during the nationwide COVID-19 lockdown may have led to the creation of an enabling environment for existing tobacco users to limit their tobacco use through reduced access and expenditure on these products. There is also an urgent need to prioritize universal health coverage, expanded social security net, tobacco cessation and mental health services as we increasingly face such emergency lockdown situations.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Centre for Chronic Disease Control’s Institutional Ethics Committee (Reference # CCDC_IEC_04_2018). Informed consent was sought from eligible participants. A verbal consent was audio-recorded following the Indian Council of Medical Research’s revised guidelines for obtaining consent for biomedical and health research during the COVID-19 pandemic. Participants who were suffering from any severe illness, institutionalized, unable to respond the survey, and not willing to provide or record verbal consent were excluded from the study. All data was collected in accordance with guidelines, protocols and methods approved by the CCDC’s Ethics Committee. All the necessary measures to safeguard participants’ anonymity and confidentiality of information were respected. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MA, GN, and SB conceptualized the study. SB and GN led the data collection efforts and contributed to study administration. SB, GN, NJ, NS, and AP contributed to data management, analysis, interpretation of results, and drafting the manuscript. MD, SM, SP, MKA, AM, NT, DP, and MA provided technical inputs on data analysis, interpretation of results, and reviewed the manuscript critically for intellectual contents. All authors approved the final version of the manuscript and are accountable for the accuracy and integrity of any part of the work.
Funding
The activities and results presented in this publication were supported by the following grants: COVID-19 and Tobacco Project, funded from the University of Edinburgh’s Scottish Funding Council Global Challenges Research Fund (GCRF) allocation and the Tobacco Control Capacity Programme (MR/P027946/2) supported by UK Research and Innovation (UKRI) with funding from the Global Challenges Research Fund.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.964949/full#supplementary-material
Abbreviations
PHQ 9, Patient Health Questionnaire-9; GAD 7, Generalized Anxiety Disorder-7; SD, Standard deviation; CI, Confidence interval; OR, Odds ratio.
References
1. World Health Organization [WHO]. WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard. (2022). Available online at: https://covid19.who.int/ (accessed August 4, 2022).
2. Suri M, Gupta S, Kottasová I. India, Population 1.3 billion, Orders “Complete” Coronavirus Lockdown. Atlanta: CNN (2020).
3. Sharma AJ, Subramanyam MA. Psychological impact of Covid-19 lockdown in India: Different strokes for different folks. medRxiv [Preprint]. (2020) Availble online at: https://doi.org/10.1101/2020.05.25.20111716 (accessed May 26, 20220).
4. Dalal PK, Roy D, Choudhary P, Kar SK, Tripathi A. Emerging mental health issues during the COVID-19 pandemic: an Indian perspective. Indian J Psychiatry. (2020) 62(Suppl 3):S354. doi: 10.4103/psychiatry.IndianJPsychiatry_372_20
5. Roy A, Singh AK, Mishra S, Chinnadurai A, Mitra A, Bakshi O. Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry. (2020) 67:587–600. doi: 10.1177/0020764020950769
6. Walter D. Implications of Covid-19 for labour and employment in India. Indian J Labour Econ. (2020) 63:47–51. doi: 10.1007/s41027-020-00255-0
7. Daly M, Robinson E. Depression and anxiety during COVID-19. Lancet. (2022) 399:518. doi: 10.1016/S0140-6736(22)00187-8
8. Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction. (2020) 11:1319–68. doi: 10.1111/add.15276
9. News18. Don’t Consume or Spit Smokeless Tobacco Products in Public Places: ICMR. (2020). Available online at: https://www.news18.com/news/india/dont-consume-or-spit-smokeless-tobacco-products-in-public-places-icmr-2564739.html (accessed on May 14, 2020).
10. The Economic Times. 28 States, UTs Ban Smokeless Tobacco Products, Spitting due to Coronavirus. (2020). Available online at: https://economictimes.indiatimes.com/news/politics-and-nation/28-states-uts-ban-smokeless-tobacco-products-spitting-due-to-coronavirus/articleshow/75657382.cms (accessed May 10, 2020).
11. Veeraiah S, Sudhakar R, Tripathy JP, Sankar D, Usharani A, Ramakrishnan S, et al. Tobacco use and quitting behaviour during COVID-19 lockdown. Int J Tuberc Lung Dis. (2020) 25:247–9. doi: 10.5588/ijtld.20.0728
12. Vorspan F, Mehtelli W, Dupuy G. Anxiety and substance use disorders?: co-occurrence and clinical issues. Curr Psychiatry Rep. (2015) 17:4. doi: 10.1007/s11920-014-0544-y
13. Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Arch Gen Psychiatry. (2002) 59:1039–44. doi: 10.1001/archpsyc.59.11.1039
14. Brose LS, Brown J, Robson D, McNeill A. Mental health, smoking, harm reduction and quit attempts - A population survey in England. BMC Public Health. (2020) 20:1237. doi: 10.1186/s12889-020-09308-x
15. Chen D. The psychosocial impact of the COVID-19 pandemic on changes in smoking behavior: evidence from a nationwide survey in the UK. Tob Prev Cessat. (2020) 6:1–5. doi: 10.18332/tpc/126976
16. Nair M, Ali MK, Ajay VS, Shivashankar R, Mohan V, Pradeepa R, et al. CARRS Surveillance study: design and methods to assess burdens from multiple perspectives. BMC Public Health. (2012) 12:701. doi: 10.1186/1471-2458-12-701
17. ICMR. ICMR National Guidelines for Ethics Committees for COVID-19 Research. (2020). Available online at: https://www.icmr.gov.in/pdf/covid/techdoc/EC_Guidance_COVID19_06052020.pdf (accessed on April 20 2020).
18. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
19. Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. J Am Med Assoc. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
20. Thour A, Das S, Sehrawat T, Gupta Y. Depression among patients with diabetes mellitus in North India evaluated using patient health questionnaire-9. Indian J Endocrinol Metab. (2015) 19:252–5. doi: 10.4103/2230-8210.149318
21. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
22. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
24. Massey JT. Estimating the Response Rate in a Telephone Survey with Screening: Proceedings of the section on survey research methods. Alexandria, VA: American Statistical Association (1995).
25. Pearson K. On the criterion that a given system of deviations from the probable in the case of a correlated system of variables is such that it can be reasonably supposed to have arisen from random sampling. Lond Edinb Dublin Philos Magaz J Sci. (1900) 50:157–75.
26. Fisher RA. “Statistical methods for research workers,” in Breakthroughs in Statistics. New York, NY: Springer (1992), 66–70.
27. Al Azdi Z, Islam K, Chowdhury AH, Ahmed HU, Alam R, Hussain AHME, et al. The magnitude of depression and anxiety during COVID 19?: an online survey among adults in Bangladesh. JMIR Preprints. (2020). Available online at: https://preprints.jmir.org/preprint/20576 [unpublished, non-peer-reviewed preprint (accessed on May 22, 2020).
28. Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during covid-19. Int J Environ Res Public Health. (2020) 17:3740. doi: 10.3390/ijerph17103740
29. Gopal A, Sharma AJ, Subramanyam MA. Dynamics of psychological responses to COVID-19 in India: a longitudinal study. Vickers K, editor. PLoS One. (2020) 15:e0240650. doi: 10.1371/journal.pone.0240650
30. Rehman U, Shahnawaz MG, Khan NH, Kharshiing KD, Khursheed M, Gupta K, et al. Depression, anxiety and stress among indians in times of Covid-19 lockdown. Commun Ment Health J. (2020) 57:42–8. doi: 10.1007/s10597-020-00664-x
Keywords: mental health, tobacco users, COVID-19, lockdown, anxiety, depression
Citation: Bassi S, Nazar GP, Joshi N, Sharma N, Pandian A, Deepa M, Mohan S, Patel SA, Ali MK, McNeill A, Tandon N, Mohan V, Prabhakaran D and Arora M (2022) Anxiety and depression among adult tobacco users during the COVID-19 restrictions in India. Front. Psychiatry 13:964949. doi: 10.3389/fpsyt.2022.964949
Received: 09 June 2022; Accepted: 01 August 2022;
Published: 23 August 2022.
Edited by:
Roy Abraham Kallivayalil, Pushpagiri Medical College, IndiaReviewed by:
Gerhard Grobler, University of Pretoria, South AfricaZvi Zemishlany, Reichman University (Inter Disciplinary Center), Israel
Copyright © 2022 Bassi, Nazar, Joshi, Sharma, Pandian, Deepa, Mohan, Patel, Ali, McNeill, Tandon, Mohan, Prabhakaran and Arora. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shalini Bassi, c2hhbGluaS5iYXNzaUBwaGZpLm9yZw==
†ORCID: Gaurang P. Nazar, orcid.org/0000-0002-7025-2946; Mohan Deepa, orcid.org/0000-0001-6348-1946; Sailesh Mohan, orcid.org/0000-0003-1853-3596; Shivani A. Patel, orcid.org/0000-0003-0082-5857; Ann McNeill, orcid.org/0000-0002-6223-4000; Viswanathan Mohan, orcid.org/0000-0001-5038-6210; Dorairaj Prabhakaran, orcid.org/0000-0002-3172-834X; Monika Arora, orcid.org/0000-0001-9987-3933
 Shalini Bassi
Shalini Bassi Gaurang P. Nazar†2
Gaurang P. Nazar†2 Sailesh Mohan
Sailesh Mohan Viswanathan Mohan
Viswanathan Mohan Monika Arora
Monika Arora