Abstract
Background:
Exposure to coronavirus disease 2019 (COVID-19) can cause severe mental health problems, the dynamics of which remain unclear. This study evaluated the mental status of frontline health care workers (FHWs) and suspected infected patients (SIPs) during different periods of the COVID-19 outbreak.
Materials and methods:
Demographic and psychological data were collected through a cross-sectional survey of 409 participants in a hospital from 20 January to 7 August 2020. COVID-19 outbreaks were divided into three periods owing to the time, place, and scale, including the national outbreak period (a nationwide pandemic period from 20 January to 8 April 2020), sporadic period (a stable period from 9 April to 10 June), and local epidemic period (a local pandemic in Beijing from 11 June to 7 August 2020). Acute psychological disorders (APDs), including symptoms of anxiety and depression, were assessed using the Zung Self-Rating Anxiety/Depression Scale (SAS/SDS).
Results:
A total of 206 FHWs and 203 SIPs completed the electronic questionnaire. Overall, the prevalence rates of anxiety and depression among SIPs were 3.9 and 19.4%, respectively, while significantly higher prevalence rates (17.7 and 25.1%) were found among FHWs, P-value < 0.05. Psychological status among SIPs did not differ significantly across the three periods. The FHWs were more vulnerable, as their SAS and SDS scores and almost all the dimension scores were significantly higher during the local epidemic period than during the national outbreak and sporadic periods (all P-values < 0.001). The prevalence of anxiety (34.41%) and depression (41.94%) was significantly higher during the local epidemic period (P < 0.001). Logistic and linear mixed models showed that age, sex, and doctor-patient ratio especially, independently influenced most dimension scores of SAS and SDS among FHWs (P < 0.05).
Conclusion:
Compared to the COVID-19 epidemic at the national level, the local epidemic had a greater influence on FHWs’ mental health. More attention should be given to the workload of FHWs.
Introduction
Coronavirus disease 2019 (COVID-19) currently represents an unprecedented threat to human health worldwide (1, 2). The first cases of this novel coronavirus (3, 4) were reported in Wuhan, the capital city of Hubei Province, China, in December 2019. Subsequently, the virus was identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the World Health Organization. The disease has a very strong infectious ability, such that it rapidly spread within a few months and finally became a worldwide health threat. The World Health Organization announced that as of 30 March 2021, 126,372,442 cases had been diagnosed, and 2,769,696 persons had died from COVID-19 due to the high mortality rate and lack of effective treatment (5). The primary routes of transmission include short-distance person-to-person contact, respiratory droplets, and aerosols. The pandemic has relentlessly affected normal social order, caused social panic, and seriously influenced public mental health (6), especially for those frequently exposed to high-risk environments.
Frontline health care workers (FHWs) are the most important force in preventing the spread of COVID-19 and protecting public health (7). However, due to factors such as direct exposure to infectious individuals, a shortage of protective equipment, prolonged separation from family and friends, and even stigmatization (8), FHWs often experience acute psychological disorders (APDs), such as anxiety and depression (9–11). As early as May 2020, the International Council of Nurses reported that more than 90,000 medical workers had been infected with COVID-19. This figure is likely to be conservative because countries were busy combatting the pandemic. Studies (12, 13) have shown that during the outbreak of SARS and Middle East respiratory syndrome (MERS), many frontline staff were infected in their workplaces, which often provoked their loss of emotional control and finally the emergence of APDs.
The effective control of the COVID-19 outbreak in Wuhan was followed by a short period of tranquility. However, the calm soon ended in June 2020 with a local outbreak in the Xinfadi Agricultural Wholesale Market in Fengtai District, Beijing. At this time, increasing numbers of medical staff devoted themselves to handling the drastically increasing number of suspected infected patients (SIPs). The state of the spread of COVID-19 worldwide is not positive. Such a serious situation requires not only effective treatment programs but also more medical staff on the frontlines to combat the pandemic. Although doctor-patient mental health is a concern among scholars, the periods covered in most studies are relatively short (3, 14). Therefore, this study investigated the dynamic changes in APDs caused by the COVID-19 pandemic among health care workers and inpatients over a relatively long period, with the main purpose of providing important evidence for psychological interventions.
Materials and methods
Study design, participants, and data collection
This study was a cross-sectional survey conducted from 20 January to 7 August 2020, to observe the different psychosocial status of FHWs and SIPs during outbreaks of COVID-19 (Figure 1). During this time, a total of 503 FHWs were sent to isolation wards to combat the COVID-19 epidemic, each of whom worked in a totally closed environment for 3 weeks. According to the COVID-19 prevention policy, 914 consecutive SIPs were hospitalized in the isolation ward for a definitive diagnosis. A total of 41% of FHWs and 29% of SIPs in our hospital during this period were sampled for the psychological health status survey. All the data were collected by questionnaire on a professional online assessment platform.1 Participants completed anonymous self-evaluation forms in the Mini Program provided by WeChat APP linked to the survey website using their own cell phones with each patient submitting questionnaire only once. The exclusion criteria included old age (80 years or above), blurred vision, communication disorders, illiteracy, non-use of cell phones, or refusal to cooperate. All participants were enrolled from isolation wards in Beijing Friendship Hospital, which is a third-level grade A general hospital in Beijing affiliated with Capital Medical University. During the COVID-19 outbreak period, the isolation wards mainly received patients with suspected infection from fever clinics. SIPs were screened by throat swab nucleic acid tests at least twice with an interval of 24 h. The results were reviewed by the team of chief examiners. If COVID-19 infection was confirmed, the infected patients were transferred to a designated hospital for further treatment. The other patients were released from the isolation wards. All the enrolled participants signed informed consent forms, and the study was approved by the Ethics Committee of Beijing Friendship Hospital (2020-P2-161-01).
FIGURE 1
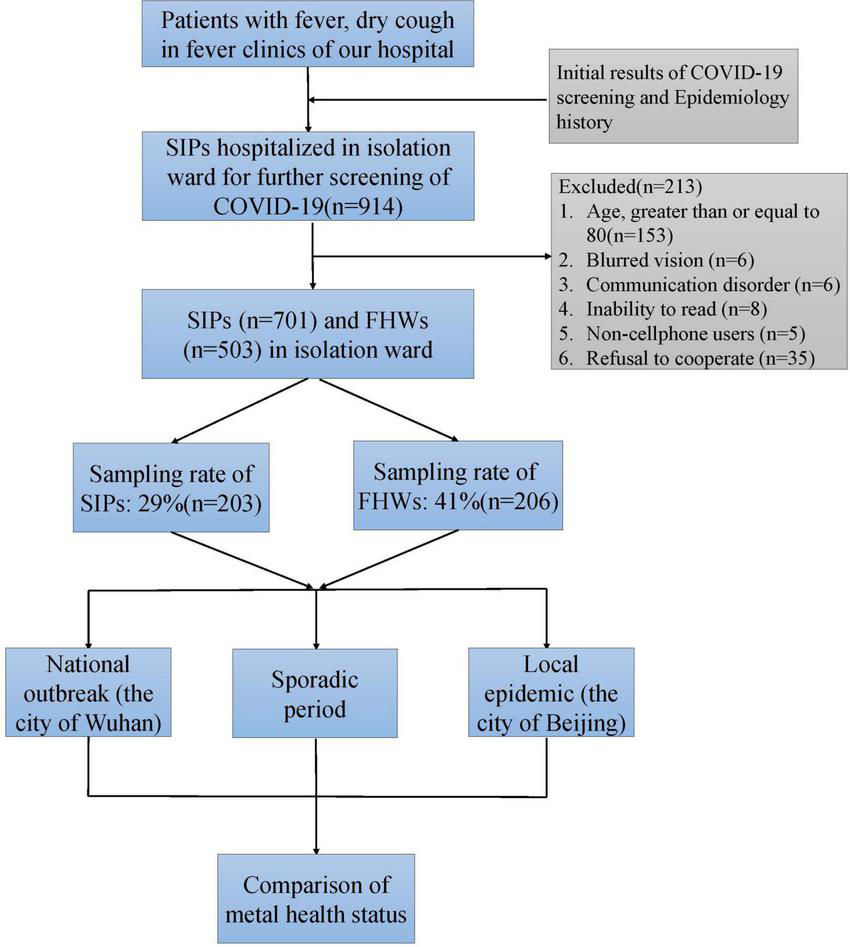
Consolidated Standards of Reporting Trials (CONSORT) diagram of the study. COVID-19, coronavirus disease 2019; FHWs, frontline health care workers; SIPs, suspected infected patients.
The demographic characteristics included age, sex, area of residence (Fengtai District or other districts), education status (high school or below, bachelor’s degree, master’s degree, and doctoral degree), marital status (single, married, and divorced), and number of children in the participant’s family (no children, one or more children). Participants were classified into three groups according to the enrolment date: national outbreak period, sporadic period and local epidemic period (Figure 2). The COVID-19 outbreak in Wuhan lasted from 20 January to 8 April 2020, and the number of local infected cases in Beijing increased during this period, which was defined as the national outbreak period. From 9 April to 10 June 2020, the epidemic in Wuhan was effectively controlled, and the number of local confirmed cases in Beijing remained stable, without a remarkable increase. This period was defined as the sporadic period. From 11 June to 7 August 2020, a new COVID-19 outbreak occurred in the Xinfadi Agricultural Wholesale Market in Fengtai District, Beijing, and the number of cases increased rapidly. This period was called the local epidemic period.
FIGURE 2
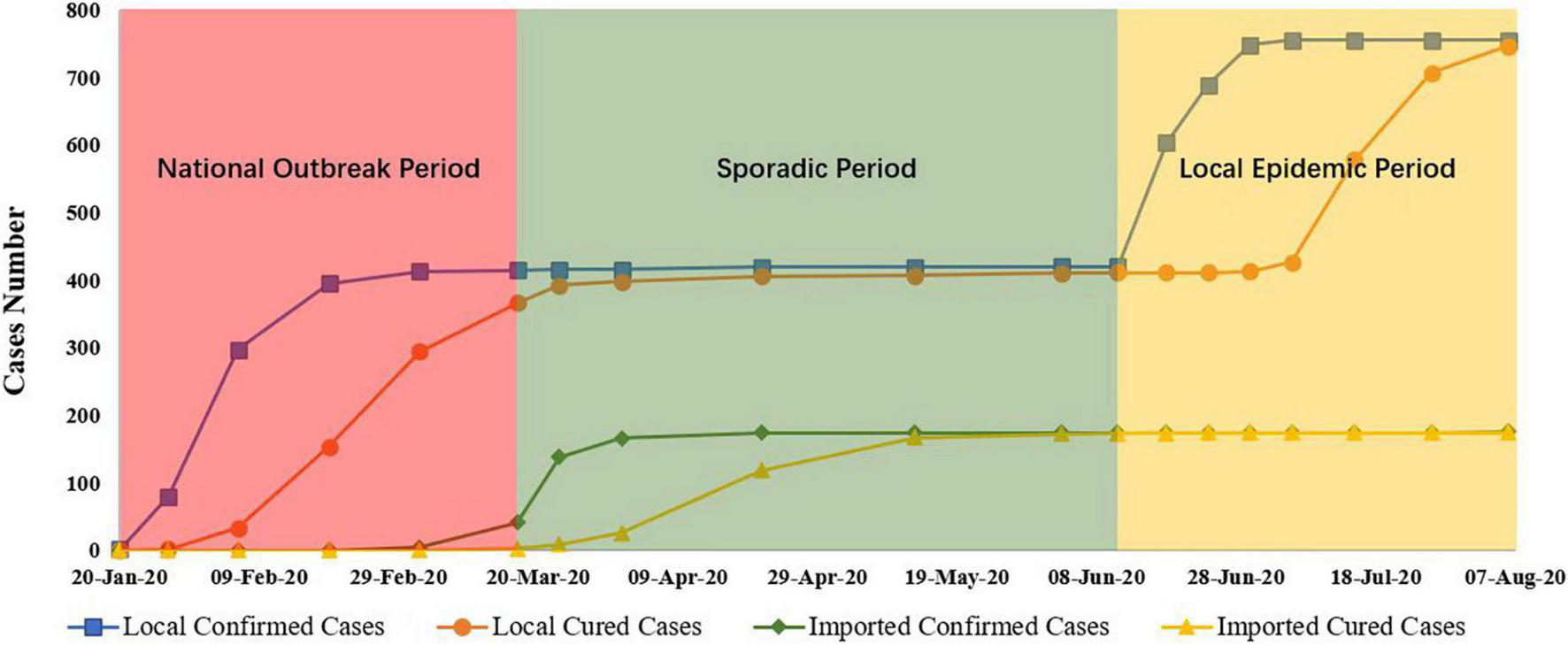
COVID-19 cases during the national outbreak, sporadic, and local epidemic periods in Beijing. Data were obtained from the Beijing Municipal Health Commission (available at http://wjw.beijing.gov.cn/). COVID-19, coronavirus disease 2019.
Assessment criteria
The symptoms of anxiety and depression were assessed with the Zung Self-Rating Anxiety/Depression Scale (SAS/SDS) (15, 16). These scales have been widely applied in clinical practice and scientific research, showing good reliability and convincing results in the Chinese population (17–19). The SAS and the SDS both include 20 items, with each item scored on a scale from 1 to 4, indicating none or a little of the time, some of the time, a good part of the time, and most or all of the time. The participants responded according to their psychological and physical symptoms within the past week. According to convention in China, the threshold score of anxiety on the self-reported scale is 50. Scores in the range of 50–59 indicate slight anxiety, scores from 60 to 69 indicate moderate anxiety, and scores above 70 indicate severe anxiety. For depression, the cut-off score is 53, with scores in the range of 53–62 implying slight depression, scores ranging from 63 to 72 indicating moderate depression, and scores above 73 indicating severe depression.
Physical symptoms of anxiety and depression can manifest in multiple systems, such as the cardiovascular, digestive, respiratory, skeletal and muscle, urinary, and reproductive systems. The related physical complaints are often composed of factors in several dimensions. The SAS/SDS includes only the abovementioned physical symptoms. Therefore, the SAS/SDS is an appropriate instrument for dimensional analysis and theoretically supports the detection of the cause of mental disease.
A four-factor structure of the SAS/SDS (20, 21), which is generally stable and significantly correlated with relevant variables, was adopted in this study. The SAS contained four factors: anxiety and panic (items 1, 2, 3, 4, 18), somatic control (items 5, 9, 13, 17, 19), vestibular sensations (items 6, 10, 11, 12, 14), and gastrointestinal/muscular sensations (items 7, 8, 15, 16, 20). The SDS also consisted of four dimensions: core depression (items 1, 3, 6, 14, 17, 18, 19, 20), cognitive depression (items 10, 11, 12, 16), anxiety (items 4, 13, 15), and somatic control (items 5, 7, 9). Items 2 and 8 were not included.
Statistical analysis
The independent continuous variables, including age, SAS score, SDS score and dimension score, were described as means with standard deviations (SDs) and analyzed by ANOVA tests among the three-period groups. Categorical variables, including sex, area of residence, education status, marital status, and the number of children, were described as frequencies (%) and analyzed by the chi-square test or Fisher’s exact test. Bonferroni-adjusted tests were used for multiple comparisons. Univariate and stepwise multivariate logistic regression models were used to calculate the factors influencing anxiety and depression status. All the collected characteristics were entered into the multivariate logistic regression models, and only significant variables remained in the final models. Odds ratios and 95% CIs were calculated for each variable. Linear mixed models were used to calculate the influencing factors with the SAS score, SDS score and dimension score. SAS statistical software version 9.4 (SAS Institute Inc.) was used for statistical analysis. All statistical analyses were tested at a significance level of 0.05 (two-sides).
Results
Demographic characteristics of the enrolled health care workers and patients
A total of 203 health care workers assigned to isolation wards during the COVID-19 pandemic period from January to August were enrolled and completed the survey. The demographic characteristics of the enrolled FHWs are shown in Table 1. Across the three periods (national outbreak period, sporadic period, and local epidemic period), there was no significant difference among the medical staff assigned to the isolation wards in terms of age, with most staff being approximately 30 years old (F = 0.724, P = 0.696). The number of female workers was almost double the number of male workers (P = 0.801). The FHWs surveyed in the local epidemic period had lower education levels than those surveyed in the previous periods, with 34.41% of FHWs having a master’s degree or higher vs. 54.10 and 57.14% in the national outbreak period and sporadic period, respectively (P = 0.011). The FHWs surveyed in different periods showed no significant differences regarding other demographic characteristics, including marital status, number of children in the participant’s family, and area of residence. Notably, the workload differed significantly across the three periods and presented an upward trend. The doctor-patient ratio was only 0.75 during the national outbreak period and rose to 4.21 during the local epidemic period, which meant that medical resources were so limited that one doctor had to treat 4–5 patients in the isolation wards during the local epidemic period. A total of 206 SIPs in the isolation wards were enrolled and completed the survey. As shown in Table 1, the demographic characteristics of patients in the isolation wards were similar among patients surveyed during the national outbreak period, sporadic period and local epidemic period (all P-values > 0.05).
TABLE 1
| National outbreak period | Sporadic period | Local epidemic period | F/χ2 value | P-value | |
| FHWs | n = 61 | n = 49 | n = 93 | ||
| Age | 31.30 ± 4.41 | 30.78 ± 4.24 | 31.83 ± 5.79 | 0.724 | 0.696 |
| Sex | |||||
| Male | 20 (32.79) | 14 (28.57) | 26 (27.96) | 0.443 | 0.801 |
| Female | 41 (67.21) | 35 (71.43) | 67 (72.04) | ||
| Area of residence | |||||
| Fengtai district | 10 (16.39) | 4 (8.16) | 14 (15.05) | 1.777 | 0.411 |
| Other district | 51 (83.61) | 45 (91.84) | 79 (84.95) | ||
| Education level | |||||
| Bachelor’s or below | 28 (45.90) | 21 (42.86) | 61 (65.59) | 9.093 | 0.011 |
| Master’s or above | 33 (54.10) | 28 (57.14) | 32 (34.41) | ||
| Marital status | |||||
| Not married | 21 (34.43) | 16 (32.65) | 31 (33.33) | 0.040 | 0.980 |
| Married or divorced | 40 (65.57) | 33 (67.35) | 62 (66.67) | ||
| Children | |||||
| None | 33 (54.10) | 29 (59.18) | 40 (43.01) | 3.875 | 0.144 |
| 1 or more | 28 (45.90) | 20 (40.82) | 53 (56.99) | ||
| Doctor-patient ratio | 0.75 | 1.37 | 4.21 | 202 | <0.001 |
| Patients | n = 33 | n = 35 | n = 138 | ||
| Age | 38.09 ± 11.80 | 37.46 ± 12.00 | 39.92 ± 14.00 | 0.446 | 0.800 |
| Sex | |||||
| Male | 14 (42.42) | 20 (57.14) | 73 (52.90) | 1.627 | 0.443 |
| Female | 19 (57.58) | 15 (42.86) | 65 (47.10) | ||
| Area of residence | |||||
| Fengtai district | 10 (30.30) | 14 (40.00) | 43 (31.16) | 1.803 | 0.582 |
| Other district | 23 (69.70) | 21 (60.00) | 95 (68.84) | ||
| Education level | |||||
| Bachelor’s or below | 29 (87.88) | 27 (77.14) | 127 (92.03) | # | 0.060 |
| Master’s or above | 4 (12.12) | 8 (22.86) | 11 (7.97) | ||
| Marital status | |||||
| Not married | 12 (36.36) | 10 (28.57) | 39 (28.26) | 0.861 | 0.650 |
| Married or divorced | 21 (63.64) | 25 (71.43) | 99 (71.74) | ||
| Children | |||||
| None | 15 (45.45) | 11 (31.43) | 45 (32.61) | 2.118 | 0.347 |
| 1 or more | 18 (54.55) | 24 (68.57) | 93 (67.39) | ||
The demographic characteristics of enrolled health care workers and patients during the national outbreak period, sporadic period and local epidemic period.
#Fisher’s exact test. FHWs, Health care workers.
The psychological status of participants in the isolation ward during the COVID-19 pandemic
The psychological status of health care workers in the isolation wards was significantly poor during the local epidemic period (Table 2). The SAS and SDS scores and the scores for almost all the dimensions of the SAS/SDS, except for the second dimension of the SDS (P = 0.09), were higher in the local epidemic period than in the national outbreak and sporadic periods (all P-values < 0.001). The health care workers assigned to isolation wards during the local epidemic period had SAS and SDS scores of 44.14 ± 14.32 and 50.53 ± 13.36, respectively, which were 8–10 points higher than the scores in the national outbreak and sporadic periods (Figure 3A). Furthermore, the proportion of health care workers with anxiety (34.41%) and depression (41.94%) was higher during the local epidemic period (P < 0.001). The prevalence of anxiety and depression in FHWs during the national outbreak period and sporadic period was 1.6 and 13.1% and 6.1 and 8.1%, respectively. The overall incidence of anxiety and depression in FHWs was 17.7 and 25.1%, respectively.
TABLE 2
| National outbreak period | Sporadic period | Local epidemic period | F/χ2 value | P-value | |
| FHWs | n = 61 | n = 49 | n = 93 | ||
| SAS scores | 32.52 ± 6.08 | 34.59 ± 7.62 | 44.14 ± 14.32* | 34.211 | <0.001 |
| 1 | 60 (98.36) | 46 (93.88) | 61 (65.59) | 33.084 | <0.001 |
| ≥2 | 1 (1.64) | 3 (6.12) | 32 (34.41) | ||
| F1 | 7.73 ± 1.75 | 8.06 ± 2.09 | 10.47 ± 4.29* | 19.736 | <0.001 |
| F2 | 9.04 ± 2.87 | 9.49 ± 2.89 | 14.35 ± 4.90* | 57.31 | <0.001 |
| F3 | 6.84 ± 0.98 | 7.53 ± 1.87 | 8.53 ± 3.08** | 15.507 | <0.001 |
| F4 | 8.61 ± 2.36 | 9.13 ± 2.71 | 10.42 ± 3.88** | 8.846 | 0.012 |
| SDS scores | 42.28 ± 10.06 | 42.51 ± 9.01 | 50.53 ± 13.36* | 20.851 | <0.001 |
| 1 | 53 (86.89) | 45 (91.84) | 54 (58.06) | 26.142 | <0.001 |
| ≥2 | 8 (13.11) | 4 (8.16) | 39 (41.94) | ||
| D1 | 15.41 ± 4.80 | 15.48 ± 4.27 | 18.21 ± 5.62* | 13.289 | 0.001 |
| D2 | 10.64 ± 2.72 | 10.28 ± 2.86 | 11.37 ± 3.37 | 4.812 | 0.09 |
| D3 | 5.29 ± 1.93 | 5.43 ± 1.68 | 7.06 ± 2.87* | 19.391 | <0.001 |
| D4 | 5.49 ± 1.86 | 5.48 ± 1.80 | 7.50 ± 2.86* | 27.354 | <0.001 |
| D5 | 5.10 ± 1.55 | 5.43 ± 1.26 | 6.01 ± 1.80** | 11.648 | 0.003 |
| SIPs | n = 33 | n = 35 | n = 138 | ||
| SAS scores | 32.18 ± 7.18 | 31.29 ± 6.79 | 34.42 ± 8.83 | 4.969 | 0.083 |
| 1 | 33 (100.00) | 33 (94.29) | 132 (95.65) | # | 0.490 |
| ≥2 | 0 | 2 (5.71) | 6 (4.35) | ||
| F1 | 7.73 ± 1.75 | 7.21 ± 1.69 | 8.36 ± 2.77 | 5.797 | 0.055 |
| F2 | 9.85 ± 3.81 | 9.57 ± 3.05 | 10.73 ± 3.99 | 2.77 | 0.25 |
| F3 | 6.63 ± 0.80 | 6.71 ± 1.64 | 7.03 ± 1.66 | 5.1 | 0.078 |
| F4 | 7.65 ± 1.92 | 7.43 ± 1.71 | 7.93 ± 2.41 | 0.555 | 0.758 |
| SDS scores | 43.97 ± 10.80 | 39.69 ± 8.41 | 43.22 ± 11.39 | 2.611 | 0.271 |
| 1 | 26 (78.79) | 32 (91.43) | 108 (78.26) | 3.175 | 0.205 |
| ≥2 | 7 (21.21) | 3 (8.57) | 30 (21.74) | ||
| D1 | 17.20 ± 6.21 | 15.07 ± 3.59 | 16.98 ± 5.23 | 2.244 | 0.326 |
| D2 | 10.30 ± 3.42 | 9.32 ± 3.57 | 9.69 ± 3.72 | 1.454 | 0.483 |
| D3 | 5.76 ± 2.02 | 5.32 ± 2.21 | 5.59 ± 2.19 | 1.406 | 0.495 |
| D4 | 4.85 ± 1.55 | 4.75 ± 1.24 | 5.54 ± 1.95 | 6.466 | 0.039 |
| D5 | 5.49 ± 1.17 | 4.79 ± 1.41 | 5.01 ± 1.62 | 4.574 | 0.102 |
Depression and anxiety status and scores for the enrolled health care workers and patients.
#Fisher’s exact test. *The variables in the local epidemic period were significantly different from those in both the national outbreak period and the sporadic period. **The variables in the local epidemic period were significantly different from those in the national outbreak period. SAS: F1, anxiety and panic (items 1, 2, 3, 4, 18); F2, somatic control (items 5, 9, 13, 17, 19); F3, vestibular sensations (items 6, 10, 11, 12, 14); F4, gastrointestinal/muscular sensations (items 7, 8, 15, 16, 20). SDS: D1, core depressive factor (items 1, 3, 6, 14, 17, 18, 19, 20); D2, cognitive factor (items 10, 11, 12, 16); D3, anxiety factor (items 4, 13, 15); D4, somatic factor (items 5, 7, 9); D5, (items 2, 8).
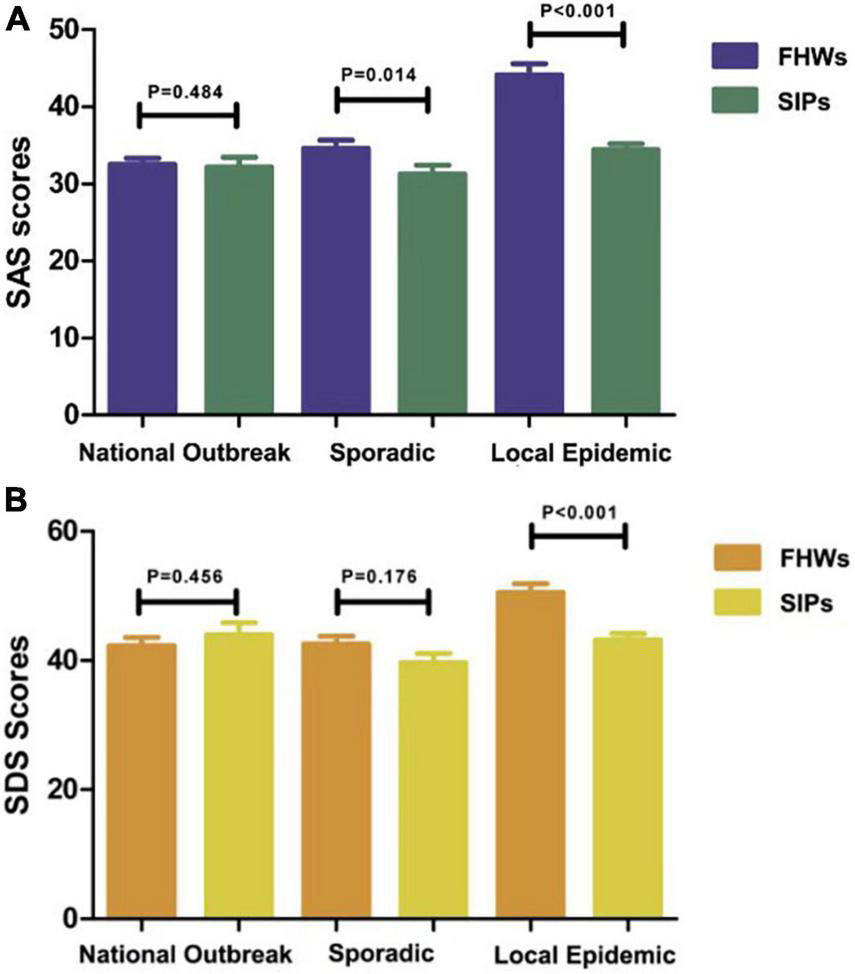
FIGURE 3
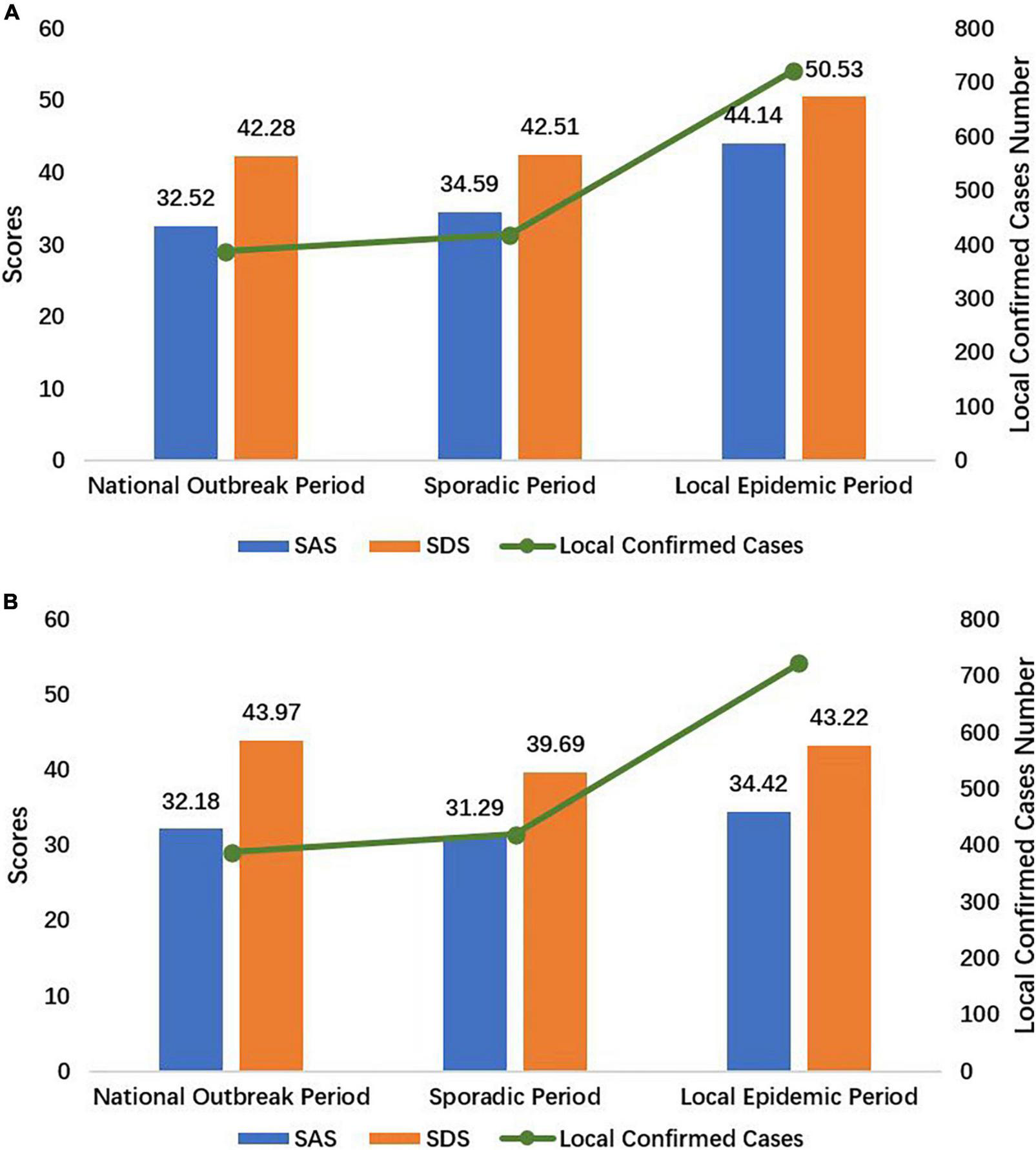
The SAS and SDS scores of FHWs (A) and SIPs (B) during the national outbreak, sporadic and local epidemic periods. SAS, the Zung Self-Rating Anxiety Scale; SDS, the Zung Self-Rating Depression Scale; FHWs, frontline health care workers; SIPs, suspected infected patients.
The psychological status of the patients in the isolation wards was stable overall (Figure 3B) and showed no significant differences across the three periods (Table 2). The prevalence of anxiety and depression among the SIPs was 0 and 21% during the national outbreak period, 5.7 and 8.6% during the sporadic period, and 4.4 and 21.7% during the local epidemic period, respectively. The average incidence of anxiety and depression among the SIPs was 3.9 and 19.4%, respectively.
There were evident changes in health care workers’ and patients’ psychological status across the three periods (Figure 4). A comparison of the SAS and SDS scores of the patients in the isolation wards showed an approximately equilateral triangle indicating similar values in each period. In contrast to the patients, the health care workers in the isolation wards scored much higher during the local epidemic period, with skewness in the triangle.
FIGURE 4
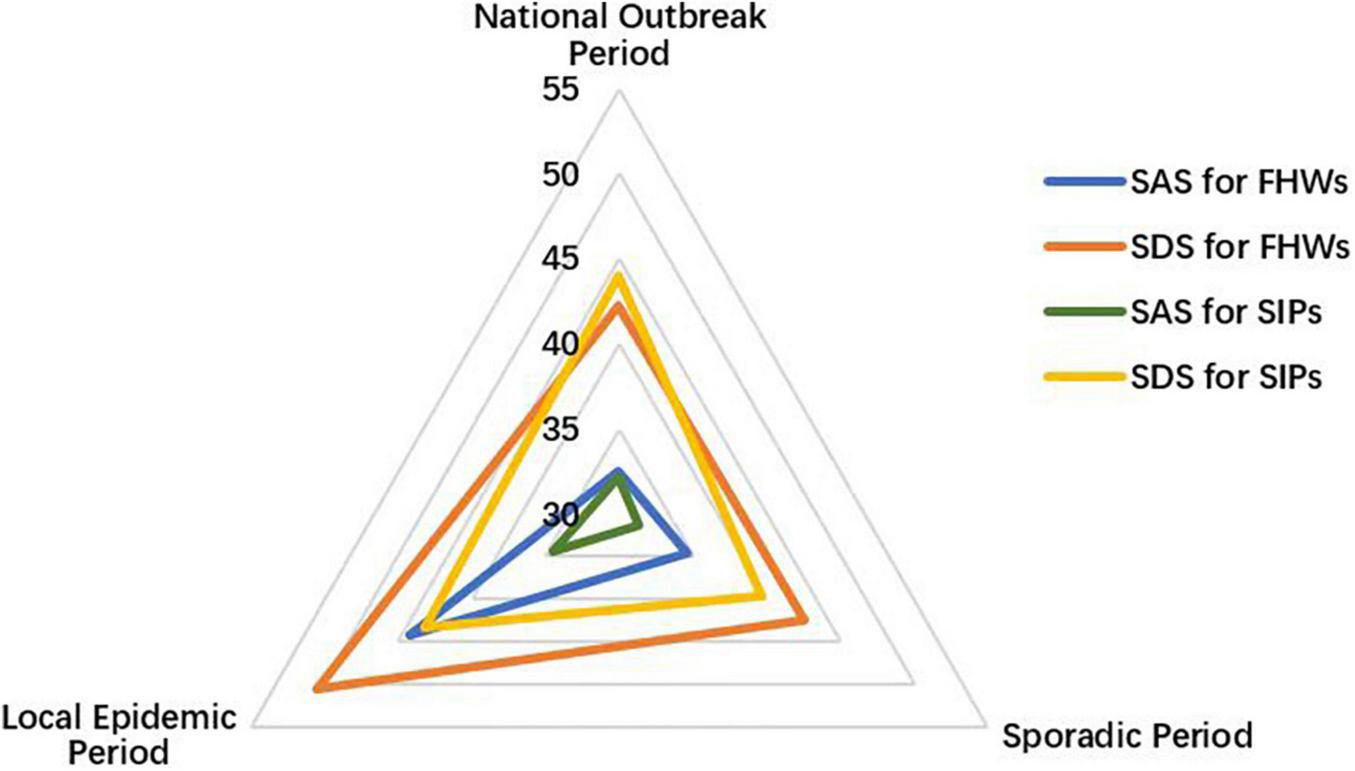
The SAS and SDS scores for frontline health care workers (FHWs) and suspected infected patients (SIPs). SAS, the Zung Self-Rating Anxiety Scale; SDS, the Zung Self-Rating Depression Scale.
Comparison of the Zung self-rating anxiety scale and the Zung self-rating depression scale scores between frontline health care workers and suspected infected patients during the periods
Figure 5 and Table 2 show the differences between the scores of FHWs and SIPs during the COVID-19 pandemic. There was no significant difference between FHWs and SIPs during the national outbreak period (P = 0.484 and P = 0.456). In the sporadic period, the SAS scores of the FHWs (34.59 ± 7.62) were higher than those of the SIPs (31.29 ± 6.79), with a p-value of 0.014. There was no significant difference in SDS scores between FHWs and SIPs during the sporadic period (P = 0.176). In the local epidemic period, the SAS and SDS scores of the FHWs were both higher than those of the SIPs (P < 0.001).
FIGURE 5
Comparison of SAS (A) and SDS (B) scores of frontline health care workers (FHWs) and suspected infected patients (SIPs) during different periods.
The anxiety rate in FHWs was 17.7%, which was higher than that in SIPs (3.9%) (χ2 = 20.430, P < 0.001). The depression rates in SIPs and FHWs were 19.4 and 25.1%, respectively (χ2 = 1.924, P = 0.165).
Factors influencing anxiety and depression among doctors in isolation wards during the COVID-19 pandemic
The multivariate logistic regression models (Table 3) showed that age (OR = 0.248, 95% CI: 0.068–0.905) and the doctor-patient ratio (OR = 2.434, 95% CI: 1.705–3.476) were independent factors of anxiety, while for depression, only the doctor–patient ratio was an independent factor (OR = 1.718, 95% CI: 1.369–2.156).
TABLE 3
| Univariate logistic regression model | Multivariate logistic regression model | |||||
| OR | 95% CI | P | OR | 95% CI | P | |
| Anxiety | ||||||
| Age | 0.384 | 0.111–1.330 | 0.131 | 0.248 | 0.068–0.905 | 0.035 |
| Sex | ||||||
| Male | Ref | Ref | Ref | |||
| Female | 2.389 | 0.938–6.084 | 0.068 | |||
| Area of residence | ||||||
| Fengtai district | Ref | Ref | Ref | |||
| Other district | 0.99 | 0.349–2.807 | 0.985 | |||
| Education level | ||||||
| Bachelor’s degree or below | Ref | Ref | Ref | |||
| Master’s degree or above | 0.531 | 0.249–1.131 | 0.101 | |||
| Marital status | ||||||
| Not married | Ref | Ref | Ref | |||
| Married or divorced | 0.751 | 0.357–1.581 | 0.451 | |||
| Children | ||||||
| None | Ref | Ref | Ref | |||
| 1 or more | 1.012 | 0.492–2.080 | 0.974 | |||
| Doctor-patient ratio | 2.338 | 1.644–3.326 | <0.001 | 2.434 | 1.705–3.476 | <0.001 |
| Depression | ||||||
| Age | 0.287–1.728 | 0.444 | ||||
| Sex | ||||||
| Male | Ref | Ref | Ref | |||
| Female | 1.009 | 0.503–2.024 | 0.979 | |||
| Area of residence | ||||||
| Fengtai district | Ref | Ref | Ref | |||
| Other district | 0.814 | 0.335–1.982 | 0.651 | |||
| Education level | ||||||
| Bachelor’s degree or below | Ref | Ref | Ref | |||
| Master’s degree or above | 0.962 | 0.509–1.820 | 0.906 | |||
| Marital status | ||||||
| Not married | Ref | Ref | Ref | |||
| Married or divorced | 1.285 | 0.645–2.558 | 0.476 | |||
| Children | ||||||
| None | Ref | Ref | Ref | |||
| 1 or more | 1.63 | 0.857–3.098 | 0.136 | |||
| Doctor-patient ratio | 1.718 | 1.369–2.156 | <0.001 | 1.718 | 1.369–2.156 | <0.001 |
Factors influencing anxiety and depression status in univariate and multivariate logistic regression models.
OR: odds ratio.
The linear mixed models (Table 4) showed that age influenced the total SAS (P = 0.011), total SDS (P = 0.029), F1 (P = 0.007), F2 (P = 0.011), F3 (P = 0.026), D1 (P = 0.038), and D4 (P = 0.014) scores. Sex also independently influenced the total SAS (P = 0.030), F2 (P = 0.037), F3 (P = 0.040), and F4 (P = 0.049) scores. The doctor-patient ratio independently influenced most of the dimension scores, including total SAS and SDS, F1, F2, F3, F4, D1, D3, D4, and D5 scores (all P < 0.005).
TABLE 4
| Mixed model | |||
| β | P | ||
| SAS | Age | −0.475 | 0.011 |
| Sex | 4.129 | 0.030 | |
| Doctor-patient ratio | 3.480 | <0.001 | |
| F1 | Age | −0.149 | 0.007 |
| Doctor-patient ratio | 0.858 | <0.001 | |
| F2 | Age | −0.172 | 0.011 |
| Sex | 1.434 | 0.037 | |
| Doctor-patient ratio | 1.615 | <0.001 | |
| F3 | Age | −0.090 | 0.026 |
| Sex | 0.844 | 0.040 | |
| Doctor-patient ratio | 0.469 | <0.001 | |
| F4 | Sex | 1.123 | 0.049 |
| Doctor-patient ratio | 0.527 | <0.001 | |
| SDS | Age | −0.436 | 0.029 |
| Doctor-patient ratio | 2.732 | <0.001 | |
| D1 | Age | −0.182 | 0.038 |
| Education level | 1.718 | 0.043 | |
| Doctor-patient ratio | 1.014 | <0.001 | |
| D2 | NA | NA | NA |
| D3 | Doctor-patient ratio | 0.546 | <0.001 |
| D4 | Age | −0.100 | 0.014 |
| Doctor-patient ratio | 0.631 | <0.001 | |
| D5 | Area of residence | −0.740 | 0.025 |
| Doctor-patient ratio | 0.236 | 0.001 | |
Influencing factors in SAS scores, SDS scores, and dimension scores in the linear mixed model.
SAS: F1, anxiety and panic (items 1, 2, 3, 4, 18); F2, somatic control (items 5, 9, 13, 17, 19); F3, vestibular sensations (items 6, 10, 11, 12, 14); F4, gastrointestinal/muscular sensations (items 7, 8, 15, 16, 20). SDS: D1, core depressive factor (items 1, 3, 6, 14, 17, 18, 19, 20); D2, cognitive factor (items 10, 11, 12, 16); D3, anxiety factor (items 4, 13, 15); D4, somatic factor (items 5, 7, 9); D5, (items 2, 8); NA, not applicable.
Discussion
A total of 409 participants were included in this study, including FHWs and patients from the isolation wards of Beijing Friendship Hospital in Beijing, China. Overall, the incidence of anxiety and depression among FHWs was 17.7 and 25.1%, respectively, which was significantly higher than the incidence among SIPs (3.9 and 19.4%). Furthermore, the occurrence of APDs in patients was basically stable during the three different periods, but the figures for FHWs fluctuated drastically across periods. The scores in the local epidemic period were significantly higher than those in the previous two periods. In addition, age, sex, and doctor-patient ratio were independent risk factors for APDs. It is worth noting that the doctor-patient ratio was the strongest influencing factor for almost all dimensions of the SAS and SDS (only the cognitive dimension in the SDS was not related).
Theoretically, the closeness of contact with COVID-19 determines the risk of being infected and the degree of APD occurrence (22, 23). A recent study (24) based on 43 investigations showed that anxiety and depression were more frequent in FHWs than in non-FHWs. Previous studies (25) showed that anxiety and depression rates were 20.8 and 29.2%, respectively, in infected patients. Among FHWs, the anxiety and depression rates ranged from 38.5 to 44.6% and 21.7 to 50.4%, respectively (22, 26). In our study, the prevalence was consistent with previous studies. It was reported that the reasons for the higher prevalence of APD among FHWs were sociodemographic factors, current and past medical history, psychological and social factors, and job-related factors (24).
The brain is the central organ of stress adaptation that is responsible for sensing and judging the degree of stress and reacting accordingly physiologically and behaviorally (27). Acute and chronic stress can lead to imbalances in the neural circuits of cognition, anxiety and emotion, which in turn affect the physiology and behavior of the whole body through neuroendocrine, autonomic nerve, immune, and metabolic mediators (27, 28). Therefore, when the experience of tension and danger goes beyond the body’s short-term adaptive capability, neural circuits become blocked, which results in mental disorders, such as schizophrenia, anxiety, and depression (28). This can explain why the occurrence of anxiety, depression and other psychological disorders was significantly higher among FHWs than among SIPs and other groups. FHWs were continuously exposed to health-damaging circumstances (29), while SIPs could be discharged after a short stay in the hospital when they tested negative.
In the present study, we found that the doctor-patient ratio was the strongest risk factor influencing the occurrence of APDs among FHWs by affecting various dimensions of the SAS and SDS, including anxiety and panic, somatic control, vestibular sensations, gastrointestinal/muscular sensation factors, core depression, anxiety, and somatic factors (20, 21). A higher doctor-patient ratio implied that FHWs had to care for and manage more patients. In addition, the high proportion of older individuals among SIPs meant that FHWs wearing protective clothing had to be more careful and perform more communication, medical documentation and complex treatments. Simultaneously, the increasing number of SIPs led to higher working hours and workload, causing FHWs to suffer higher psychological and physical pressures (30–33).
In the early periods of COVID-19, Chinese government and hospitals took effective measures to address mental health problems, for example, adopting the psychological protection measures provided by the International Guidelines for Psychological Crisis Intervention, establishing psychological expert groups in hospitals and creating network mental health consulting services (6). Necessary training regarding professional knowledge, mental health, and protective equipment can build the confidence of health care workers, help them overcome the panic linked to the pandemic, and reduce nosocomial infections, thus reducing the occurrence of APDs (23). Above all, the findings suggest that in the long-term fight against COVID-19, more attention should be given to the workload of FHWs, including the doctor-patient ratio, working hours, and night duty arrangements. In addition, the establishment of critical care isolation wards is particularly important.
One strength of this study is that it tracked the dynamic changes in mental health status among participants in different periods. As a result, it provided objective and reliable results regarding the mental health impacts of the COVID-19 pandemic. A self-rating scale, the Zung Self-Rating Anxiety/Depression Scale (SAS/SDS), was adopted in this study. In addition, an in-depth dimensional analysis was conducted to show the main symptoms of anxiety and depression. However, several limitations exist in this study. First, the mental changes experienced by FHWs before and after isolation could not be followed up on due to the cross-sectional survey design of this study. Second, the convenience sampling methods and limited sample size might lead to selection bias. Third, the SAS and SDS have no diagnostic efficacy, even though they have been used in many psychological studies worldwide.
Conclusion
The present study reveals that FHWs have a much higher chance of experiencing APDs than do SIPs. Furthermore, the prevalence of anxiety and depression among SIPs remained relatively stable, while the prevalence among FHWs fluctuated drastically, with the highest incidence of anxiety and depression occurring during the local epidemic period. Analysis of the related risk factors proved that age, sex, and especially the doctor–patient ratio were independent risk factors for APDs. Our findings suggest that psychological assistance measures should be implemented not only in the anti-epidemic period but also before and after exposure to COVID-19. In addition, more concern and attention should be given to the workload of FHWs.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Beijing Friendship Hospital (2020-P2-161-01). The patients/participants provided their written informed consent to participate in this study.
Author contributions
YT and QZ collected the questionnaires and clinical data. QZ analyzed the data. YT and XD wrote the manuscript with input from all authors. XD and YC designed the study and reviewed the final manuscript. All authors participated in designing various parts of the study and the interpretation of the results.
Funding
This work was supported by the Research Foundation of Beijing Friendship Hospital, Capital Medical University (No. yyqdkt2020-22) and Wu Jieping Medical Foundation (No. 320.6750.2020-17-4).
Acknowledgments
We thank all patients and health care workers involved in our study for their impartial contributions. We also thank the Research Foundation of Beijing Friendship Hospital and Wu Jieping Medical Foundation for financial support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The reviewer JZ declared a shared parent affiliation with the authors to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
- APDs
acute psychological disorders
- COVID-19
coronavirus disease 2019
- FHWs
frontline health care workers
- MERS
Middle East respiratory syndrome
- SARS
severe acute respiratory syndrome
- SAS
the Zung Self-Rating Anxiety Scale
- SDS
the Zung Self-Rating Depression Scale
- SIPs
suspected infected patients.
Footnotes
References
1.
WHO.Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). (2020). Available online at: https://www.who.int/news-room/detail/30-01-2020-statement-on-thesecond-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed Feb 15, 2020).
2.
CucinottaDVanelliM. WHO declares COVID-19 a pandemic.Acta Bio Med. (2020) 91:157–60.
3.
ZhuNZhangDWangWLiXYangBSongJet alA novel coronavirus from patients with pneumonia in China, 2019.N Engl J Med. (2020) 382:727–33. 10.1056/NEJMoa2001017
4.
ZhouPYangXLWangXGHuBZhangLZhangWet alA pneumonia outbreak associated with anew coronavirus of probable bat origin.Nature. (2020) 579:270–3.
5.
World Health Organization.COVID-19 Weekly Epidemiological Update. (2021). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---31-march-2021 (accessed March 30, 2021).
6.
BaoYSunYMengSShiJLuL. 2019-nCoV epidemic: address mental health care to empower society.Lancet. (2020) 395:e37–8. 10.1016/S0140-6736(20)30309-3
7.
ZhangWRWangKYinLZhaoWFXueQPengMet alMental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China.Psychother Psychosom. (2020) 89:242–50. 10.1159/000507639
8.
MaunderRHunterJVincentLBennettJPeladeauNLeszczMet alThe immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital.CMAJ. (2003) 168:1245–51.
9.
LeeAMWongJGMcAlonanGMCheungVCheungCShamPCet alStress and psychological distress among SARS survivors 1 year after the outbreak.Can J Psychiatry. (2007) 52:233–40. 10.1177/070674370705200405
10.
Van BortelTBasnayakeAWurieFJambaiMKoromaASMuanaATet alPsychosocial effects of an Ebola outbreak at individual, community and international levels.Bull World Health Organ. (2016) 94:210–4. 10.2471/BLT.15.158543
11.
PappaSNtellaVGiannakasTGiannakoulisVGPapoutsiEKatsaounouP. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis.Brain Behav Immun. (2020) 88:901–7. 10.1016/j.bbi.2020.05.026
12.
SepkowitzKAEisenbergL. Occupational deaths among healthcare workers.Emerg Infect Dis. (2005) 11:1003–8. 10.3201/eid1107.041038
13.
ElkholyAAGrantRAssiriAElhakimMMalikMRVan KerkhoveMDet alMERS-CoV infection among healthcare workers and risk factors for death: retrospective analysis of all laboratory-confirmed cases reported to WHO from 2012 to 2 June 2018.J Infect Public Health. (2020) 13:418–22. 10.1016/j.jiph.2019.04.011
14.
KangLJMaSMChenMYangJWangYLiRet alImpact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study.Brain Behav Immun. (2020) 87:11–7. 10.1016/j.bbi.2020.03.028
15.
ZungWW. A rating instrument for anxiety disorders.Psychosomatics. (1971) 12:371–9. 10.1016/S0033-3182(71)71479-0
16.
ZungWW. A self-rating depression scale.Arch Gen Psychiatry. (1965) 12:63–70. 10.1001/archpsyc.1965.01720310065008
17.
DunstanDAScottNToddAK. Screening for anxiety and depression: reassessing the utility of the Zung scales.BMC Psychiatry. (2017) 17:329. 10.1186/s12888-017-1489-6
18.
YueTLiQWangRLiuZGuoMBaiFet alComparison of hospital anxiety and depression scale (HADS) and Zung self-rating anxiety/depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis.Dermatology. (2020) 236:170–8. 10.1159/000498848
19.
ZhuJHSunLZhangLWangHFanAYangBet alPrevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu.Front Psychiatry. (2020) 11:386. 10.3389/fpsyt.2020.00386
20.
OlatunjiBODeaconBJAbramowitzJSTolinDF. Dimensionality of somatic complaints: factor structure and psychometric properties of the self-rating anxiety scale.J Anxiety Disord. (2006) 20:543–61. 10.1016/j.janxdis.2005.08.002
21.
RomeraICohenHDPerezTCaballeroLGilaberteIF. Factor analysis of the Zung self-rating depression scale in a large sample of patients with major depressive disorder in primary care.BMC Psychiatry. (2008) 8:4. 10.1186/1471-244X-8-4
22.
LaiJBMaSMWangYCaiZHuJWeiNet alFactors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019.JAMA Netw Open. (2020) 3:e203976. 10.1001/jamanetworkopen.2020.3976
23.
WangLQZhangMLiuGMNanSYLiTXuLet alPsychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study.J Psychiatr Res. (2020) 129:198–205. 10.1016/j.jpsychires.2020.07.008
24.
VindegaardNBenrosME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence.Brain Behav Immun. (2020) 89:531–42. 10.1016/j.bbi.2020.05.048
25.
ZhangJLuHPZengHPZhangSDuQJiangTet alThe differential psychological distress of populations affected by the COVID-19 pandemic.Brain Behav Immun. (2020) 87:49–50. 10.1016/j.bbi.2020.04.031
26.
WangYMaSMYangCCaiZHuSZhangBet alAcute psychological effects of coronavirus disease 2019 outbreak among healthcare workers in China: a cross-sectional study.Transl Psychiatry. (2020) 10:348. 10.1038/s41398-020-01031-w
27.
McEwenBSGrayJDNascaC. 60 Years Of neuroendocrinology: redefining neuroendocrinology: stress, sex and cognitive and emotional regulation.J Endocrinol. (2015) 226:T67–83. 10.1530/JOE-15-0121
28.
McEwenBS. Allostasis and the epigenetics of brain and body health over the life course the brain on stress.JAMA Psychiatry. (2017) 74:551–2. 10.1001/jamapsychiatry.2017.0270
29.
TaylorWDBlackfordJU. Mental health treatment for front-line clinicians during and after the coronavirus disease 2019 (COVID-19) pandemic: a plea to the medical community.Ann Intern Med. (2020) 173:574–5. 10.7326/M20-2440
30.
MoYYDengLZhangLYLangQLiaoCWangNet alWork stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic.J Nurs Manag. (2020) 28:1002–9. 10.1111/jonm.13014
31.
ZhouYJWangWJSunYPQianWLiuZWangRet alThe prevalence and risk factors of psychological disturbances of frontline medical staff in China under the COVID-19 epidemic: workload should be concerned.J Affect Disord. (2020) 277:510–4. 10.1016/j.jad.2020.08.059
32.
MoshevaMPalmorNHIlanSDMatalonNPessachIMAfekAet alAnxiety, pandemic-related stress and resilience among physicians during the COVID−19 pandemic.Depress Anxiety. (2020) 37:965–71. 10.1002/da.23085
33.
FavaGAMcEwenBSGuidiJGostoliSOffidaniESoninoN. Clinical characterization of allostatic overload.Psychoneuroendocrinology. (2019) 108:94–101. 10.1016/j.psyneuen.2019.05.028
Summary
Keywords
COVID-19, anxiety, depression, healthcare workers, mental health
Citation
Tong Y, Zhang Q, Wang X, Du Y, Chang D, Cui Y and Duan X (2022) Dynamic changes in mental health status related to the COVID-19 pandemic among health care workers and inpatients in China. Front. Psychiatry 13:956068. doi: 10.3389/fpsyt.2022.956068
Received
29 May 2022
Accepted
01 September 2022
Published
03 October 2022
Volume
13 - 2022
Edited by
Francesca Conte, Second University of Naples, Italy
Reviewed by
Siqi Ge, Beijing Tiantan Hospital, China; Jie Zhang, Capital Medical University, China; Wenjie Jiao, The Affiliated Hospital of Qingdao University, China
Updates
Copyright
© 2022 Tong, Zhang, Wang, Du, Chang, Cui and Duan.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinchun Duan, duanxinchun45@163.comYong Cui, cuiyong@ccmu.edu.cn
†These authors have contributed equally to this work
This article was submitted to Mood Disorders, a section of the journal Frontiers in Psychiatry
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.