
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 30 August 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.954857
Background: Living alone is one of the most common psychosocial factors that may have an impact on lifestyle management and health status. Although many previous cross-sectional studies have found that living alone increases the risk of depression. However, this risk has rarely been assessed on the basis of longitudinal studies. Therefore, we will explore this relationship on the basis of longitudinal studies.
Methods: We systematically searched Pubmed, Embase, and Cochrane databases up to May 2022. Adjusted odds ratios (ORs), and 95% confidence intervals (CIs) were pooled by a random-effects model using an inverse variance method.
Results: Seven studies (six cohort studies and one case-control study) were included in our study. A total of 123,859 without a history of psychosis individuals were included, and the proportion of females was 65.3%. We applied a random-effects model to minimize the heterogeneity. Overall, the pooled data suggest that people living alone are associated with an increased risk of depression compared to those who do not live alone (OR 1.42, 95%CI 1.19–1.70).
Conclusion: Compared to people who live with others, living alone increases the risk of depression. Only cross-sectional studies and a few longitudinal studies currently support this association; more high-quality studies will be required in the future to confirm this causal association.
With declining birth rates and an overall increase in average life expectancy, the world’s population has been aging in recent years. Social living arrangements have changed significantly, particularly with the increasing number of single-person households (1), with around 30% of people in Western countries living alone and a significantly higher proportion of middle-aged and older people than previously (2, 3). Due to the global COVID-2019 epidemic, the impact of social isolation disadvantages has been rising in recent years (4). Social isolation is a substantial risk factor for physical health, cardiovascular disease, stroke, and premature mortality in studies (5–7). Living alone is also a prevalent psychosocial issue and an essential component of negative social variables. Living alone increases the chances of social isolation. Living alone may be harmful to one’s mental health, especially among older people. Previous research has found that persons who live alone have poorer mental health and a lower quality of life than those who live with others. Additionally, loneliness can contribute to depression (8). Unfavorable socioeconomic situations are determinants of social health, and poor social conditions (living alone, low income, little social interaction, and a lack of care) raise the risk of depression in the population, particularly among the elderly (9–11). Depression, one of the main causes of disability worldwide, is a mental health disorder characterized by chronic sorrow, loss of interest or pleasure in formerly valued or pleasant activities, sleep and eating difficulties, exhaustion, and poor concentration (12, 13). A meta-analysis reported that the prevalence of late-life depression in China was 22.7% (14). According to research, depression is linked to the incidence of cardiovascular illness, stroke, coronary heart disease, gastrointestinal problems, hypertension, asthma, arthritis, disability, suicide, and self-harm. Depression not only harms the health of older folks but also lowers the quality of life for individuals and their families (15–17). Many previous cross-sectional studies have found that living alone increases the risk of developing depression. A meta-analysis that included cross-sectional studies showed that living alone increased the risk of depression by 44% (18). However, previous studies have some limitations: (a) the majority of them are cross-sectional studies with methodological limitations; (b) meta-analyses that included cross-sectional studies did not include longitudinal studies, including cohort studies and RCT studies, which failed to truly reflect the causal relationship between solitary living and depression; and (c) the results are controversial; based on these limitations, we will include longitudinal studies to further explore this relationship.
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) project was used to conduct this meta-analysis and systematic review (19). We did not need to obtain ethical approval because the results of the studies included in this meta-analysis were already published. We systematically searched the electronic databases PubMed, Embase, and Cochrane for relevant studies reporting the relationship between living alone and the risk of diabetes until May 2022. The search strategy used the Boolean operators ‘and’ in combination with two search terms: (1) social isolation OR living alone OR living status OR living arrangement (2) depression OR mental health problems. We did not apply language restrictions in the literature search. To ensure the comprehensiveness of the literature search, we screened the reference lists of the retrieved studies to identify additional reports.
The following studies were included: (1) The study included participants who did not have depression. (2) Comparison: living alone versus living with others (3) Outcome: risk of depression (4) Study design: randomized controlled trials or cohort studies (5) Estimates of effect: adjusted odds ratios (ORs) and 95 percent confidence intervals (CIs). We excluded publications that did not include effect estimates, such as reviews, case reports, case series, editorials, letters, cross-sectional studies, guidelines, and conference abstracts. If subjects from different studies came from the same data source, the study with the longest duration or largest sample size was included.
Two independent authors reviewed all of the retrieved literature (DL-W and FW-L). Based on pre-defined criteria, we read the titles and abstracts of potentially eligible studies before reviewing them in depth. Negotiation was used to settle disagreements between the two authors. We collected information on the following topics for each study: first author; year of publication; study design; study site; data source; follow-up time; primary baseline information; and adjusted ORs, adjusted for confounders. If a study reported adjusted ORs in multiple models, only the most adjusted model was used.
To measure study quality, we employed a modified Newcastle-Ottawa Scale (NOS). This scale has three components: cohort selection, cohort comparability, and outcome evaluation. studies with NOS scores < 6 were defined as low quality, and studies with NOS scores ≥ 6 were defined as moderate to high quality (20).
Review Manager 5.3 software was used for all statistical analyses (the Nordic Cochrane Center, Rigshospitalet, Denmark). The Cochrane Q test and the I2 statistic were the two most often used statistical techniques to quantify heterogeneity, with P < 0.1 and I2 > 50% indicating significant heterogeneity, respectively. The natural logarithm of the OR and standard errors of the included studies were determined and then pooled using an inverse variance random effects model.
Supplementary Table 1 depicts the procedure of doing a literature search. Electronic searches in the PubMed, Embase and Cochrane databases yielded 2056 studies. Through titles and abstracts, full text reading, and reference to predetermined criteria, we finally included seven studies (Supplementary Figure 1). All of the included studies had NOS values ranging from moderate to high (Supplementary Table 2). The baseline characteristics of the included studies are shown in Table 1. The meta-analysis includes six cohort studies (21–26) and one case-control study (27). We gathered baseline characteristics from the included studies, such as authors, study type, data source, geographic region, sample size, study population, mean age, male proportion, length of follow-up, and adjusted confounders. There were 123,859 people without a history of psychosis in the study, with 65.3 percent of them being female. To reduce heterogeneity, we used a random-effects model. Overall, the pooled data showed that living alone was associated with a higher risk of depression than not living alone (OR 1.42, 95% CI 1.19–1.70) (Figure 1).
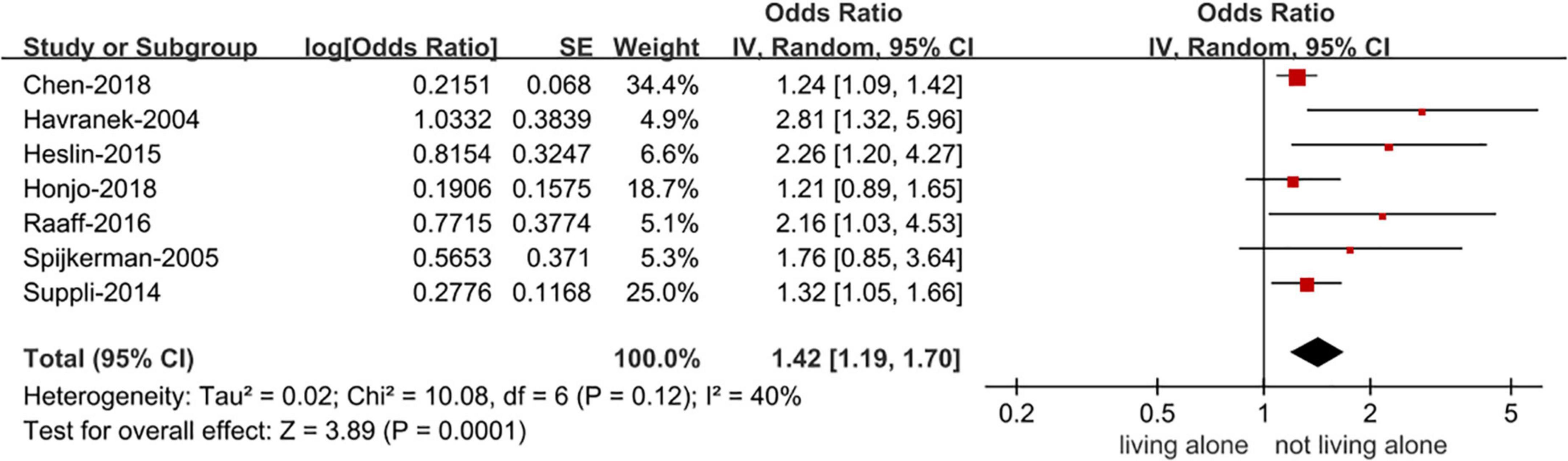
Figure 1. Forest plot for the association of living alone with the risk of depression. CI, confidence interval; SE, standard error; IV, inverse of the variance.
We performed sensitivity analyses by excluding one study at a time (Supplementary Table 3). ORs ranged between 1.33 and 1.58. Heterogeneity results ranged between 31 and 50%. The main results were similar to those of the main analysis using the random-effects model. Furthermore, when we re-performed the analysis using the fixed-effects model (Supplementary Figure 2), the results did not change substantially.
We did not examine publication bias since our meta-analysis comprised just six trials. It was emphasized that publication bias should not be addressed for some reported outcomes when less than ten studies were included.
Although previous meta-analyses have found that living alone increases the risk of depression, as they were only based on cross-sectional studies, with this limitation in mind, we will for the first time examine the relationship between living alone and the risk of depression from data from longitudinal studies. The main finding of our study is that living alone increases the risk of depression by 42%. This finding is consistent with the results of a previous meta-analysis (18).
At the time of statistical analysis, we found a moderate degree of heterogeneity in the findings, which may be related to the characteristics of the study populations included and residual confounding factors. a case-control study by Heslin et al. included 896 participants in London with no history of psychosis and showed that the risk of depression was 2.26 times higher in those who lived alone than in those who did not live alone (27). A Japanese cohort study that included 42,169 older adults found that living arrangements were associated with the risk of depressive symptoms in both men and women and that these associations varied by gender and level of community social cohesion. The study cautions that more attention needs to be paid to whether individuals live alone and with whom individuals live to prevent depressive symptoms in older adults (26). Patients who appear to have a disease state or history of the disease are at higher risk of developing depression compared to the general population, and the disease itself may affect the patient’s quality of life psychosocially. Two cohort studies of patients with breast cancer were included in our study, with the cohort study from Denmark finding a 70% increased risk of depression in the first year after diagnosis for living alone and a 3.09 times higher rate of antidepressant use than for non-living alone patients. The study suggested that women with co-morbidities, lymph node-positive disease, and those aged 70 years or older were at the highest risk. However, no clear association was found between the type of surgery or adjuvant treatment and the risk of depression (25). A single-center cohort study from the Netherlands showed that living alone increased the risk of depression in breast cancer patients by 2.16 times that of non-solitary patients, and previous studies have found that breast cancer reconstructive therapy reduces the risk of depression, but no such association was found in this study (22). A community-based retrospective cohort research in Taiwan discovered that glaucoma patients living alone had a considerably higher incidence of depression than the general population. Age, gender, poor income, substance usage, and living alone were all major risk factors for developing depression in glaucoma patients (21). Depressive symptoms after myocardial infarction appear to be driven primarily by the psychological and social consequences of myocardial infarction in patients prone to depression, particularly a history of depression or the risk of developing depression in patients exacerbated by the presence of vital failure (24). Another cohort study incorporating heart failure suggests that social factors and health status predict the development of depression in heart failure outpatients, prompting clinicians to identify patients at high risk for early psychosocial intervention (23).
Living alone raises the risk of developing depression, but it doesn’t stop there. Numerous previous cross-sectional studies have also discovered that this risk varies by age, gender, and location. Older people living alone are more vulnerable than younger people (28), men living alone are more vulnerable than women (29), and rural people living alone are more vulnerable than urban people (30). Unfortunately, the number of longitudinal studies currently available is insufficient to allow for subgroup analysis in our study.
As the worldwide birth rate falls and the global aging rate rises, more and more individuals are adjusting their lifestyles to accommodate. The amount of persons living alone has increased dramatically in Western countries, reaching 30%, with the older population being particularly vulnerable (2). Because of changing family arrangements and urbanization, the number of seniors living alone is continuously increasing in developed Asian nations such as Korea, Japan, and China (31). The negative impacts of living alone are becoming a major issue. Living alone leads to a lack of contact with others and atrophy of social networks, exacerbating social disconnection and leading to objective social isolation. There is growing concerned about the adverse effects of living alone, and previous research evidence suggests that social isolation is associated with an increased risk of physical (e.g., cardiovascular disease and diabetes) and mental health (e.g., anxiety and depression) disorders (32, 33). Depression is now one of the leading chronic diseases and is also considered a major public health problem, and may become the second most common cause of disability by 2020, after heart disease (34). Depression is associated with genetics (35), behavior, psychological factors (36), sleep quality (37), and health status. Social support is an important factor in depression. Living arrangements as a structural element of social support may help reduce and prevent the risk of depression in older adults. There are several possible explanations for the increased risk of depression associated with living alone: first, people who live alone have poorer economic and material conditions and less social support; second, people who live alone lack contact with others and may have poorer health habits and lower levels of mental health awareness; and third, people who live alone are at higher risk of developing diseases. More research are needed based on these factors to investigate the impact of psychosocial factors on people living alone and their prognosis, to identify at-risk patients early, and to intervene in the development of depression.
There are some limitations to the current study that should be highlighted. The number of includable longitudinal studies was small, and there was heterogeneity and residual confounding between studies; second, due to limited data, subgroup analyses for gender and urban-rural differences were not conducted; and third, there is a lack of relevant interventions to demonstrate a reduced risk of depression in people living alone. More long-term studies are needed in the future to validate this causal association, based on these limitations.
Compared to people who live with others, living alone increases the risk of depression. Only cross-sectional studies and a few longitudinal studies currently support this association; more high-quality studies will be required in the future to confirm this causal association.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.954857/full#supplementary-material
1. Lin H, Jin M, Liu Q, Du Y, Fu J, Sun C, et al. Gender-specific prevalence and influencing factors of depression in elderly in rural China: a cross-sectional study. J Affect Disord. (2021) 288:99–106. doi: 10.1016/j.jad.2021.03.078
2. Raymo JM. Living alone in Japan: relationships with happiness and health. Demogr Res. (2015) 32:1267–98. doi: 10.4054/DemRes.2015.32.46
3. Tamminen N, Kettunen T, Martelin T, Reinikainen J, Solin P. Living alone and positive mental health: a systematic review. Syst Rev. (2019) 8:134. doi: 10.1186/s13643-019-1057-x
4. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
5. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
6. Hawton A, Green C, Dickens AP, Richards SH, Taylor RS, Edwards R, et al. The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res. (2011) 20:57–67. doi: 10.1007/s11136-010-9717-2
7. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. (2016) 102:1009–16. doi: 10.1136/heartjnl-2015-308790
8. Peerenboom L, Collard RM, Naarding P, Comijs HC. The association between depression and emotional and social loneliness in older persons and the influence of social support, cognitive functioning and personality: a cross-sectional study. J Affect Disord. (2015) 182:26–31. doi: 10.1016/j.jad.2015.04.033
9. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. (2010) 7:e1000316. doi: 10.1371/journal.pmed.1000316
10. De Araujo AT, Costa MF. Clinical repercussion of the various states of extrinsic pulmonary granulomatoses on the bronchial tree. Bronchopneumologie. (1976) 26:285–92.
11. Vink D, Aartsen MJ, Schoevers RA. Risk factors for anxiety and depression in the elderly: a review. J Affect Disord. (2008) 106:29–44. doi: 10.1016/j.jad.2007.06.005
12. Contreras-Carreto NA, Villalobos-Gallegos L, Mancilla-Ramirez J. Epidemiological analysis of perinatal depression. Cir Cir. (2022) 90:128–32. doi: 10.24875/CIRU.20001246
13. Dubovsky SL, Ghosh BM, Serotte JC, Cranwell V. Psychotic depression: diagnosis, differential diagnosis, and treatment. Psychother Psychosom. (2021) 90:160–77. doi: 10.1159/000511348
14. Zhang L, Xu Y, Nie H, Zhang Y, Wu Y. The prevalence of depressive symptoms among the older in China: a meta-analysis. Int J Geriatr Psychiatry. (2012) 27:900–6. doi: 10.1002/gps.2821
15. Kang HJ, Bae KY, Kim SW, Shin HY, Shin IS, Yoon JS, et al. Impact of anxiety and depression on physical health condition and disability in an elderly Korean population. Psychiatry Investig. (2017) 14:240–8. doi: 10.4306/pi.2017.14.3.240
16. Verhaak PF, Dekker JH, de Waal MW, van Marwijk HW, Comijs HC. Depression, disability and somatic diseases among elderly. J Affect Disord. (2014) 167:187–91. doi: 10.1016/j.jad.2014.05.057
17. Aziz R, Steffens DC. What are the causes of late-life depression? Psychiatr Clin North Am. (2013) 36:497–516. doi: 10.1016/j.psc.2013.08.001
18. Xiu-Ying H, Qian C, Xiao-Dong P, Xue-Mei Z, Chang-Quan H. Living arrangements and risk for late life depression: a meta-analysis of published literature. Int J Psychiatry Med. (2012) 43:19–34. doi: 10.2190/PM.43.1.b
19. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
20. Chan YH, Chao TF, Lee HF, Chen SW, Li PR, Liu JR, et al. Clinical outcomes in atrial fibrillation patients with a history of cancer treated with non-vitamin k antagonist oral anticoagulants: a nationwide cohort study. Stroke. (2021) 52:3132–41. doi: 10.1161/STROKEAHA.120.033470
21. Chen YY, Lai YJ, Wang JP, Shen YC, Wang CY, Chen HH, et al. The association between glaucoma and risk of depression: a nationwide population-based cohort study. BMC Ophthalmol. (2018) 18:146. doi: 10.1186/s12886-018-0811-5
22. de Raaff CA, Derks EA, Torensma B, Honig A, Vrouenraets BC. Breast reconstruction after mastectomy: does it decrease depression at the long-term? Gland Surg. (2016) 5:377–84. doi: 10.21037/gs.2016.05.02
23. Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS. Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol. (2004) 44:2333–8. doi: 10.1016/j.jacc.2004.09.034
24. Spijkerman TA, van den Brink RH, Jansen JH, Crijns HJ, Ormel J. Who is at risk of post-MI depressive symptoms? J Psychosom Res. (2005) 58:425–32. doi: 10.1016/j.jpsychores.2005.02.005
25. Suppli NP, Johansen C, Christensen J, Kessing LV, Kroman N, Dalton SO. Increased risk for depression after breast cancer: a nationwide population-based cohort study of associated factors in Denmark, 1998-2011. J Clin Oncol. (2014) 32:3831–9. doi: 10.1200/JCO.2013.54.0419
26. Honjo K, Tani Y, Saito M, Sasaki Y, Kondo K, Kawachi I, et al. Living alone or with others and depressive symptoms, and effect modification by residential social cohesion among older adults in Japan: the JAGES longitudinal study. J Epidemiol. (2018) 28:315–22. doi: 10.2188/jea.JE20170065
27. Heslin M, Desai R, Lappin JM, Donoghue K, Lomas B, Reininghaus U, et al. Biological and psychosocial risk factors for psychotic major depression. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:233–45. doi: 10.1007/s00127-015-1131-1
28. Koo JH, Son N, Yoo KB. Relationship between the living-alone period and depressive symptoms among the elderly. Arch Gerontol Geriatr. (2021) 94:104341. doi: 10.1016/j.archger.2021.104341
29. Choi JS, Kwak SH, Son NH, Oh JW, Lee S, Lee EH. Sex differences in risk factors for depressive symptoms in patients with COPD: the 2014 and 2016 Korea national health and nutrition examination survey. BMC Pulm Med. (2021) 21:180. doi: 10.1186/s12890-021-01547-x
30. Kim C, Chang EJ, Kim CY. Regional differences in the effects of social relations on depression among Korean elderly and the moderating effect of living alone. J Prev Med Public Health. (2021) 54:441–50. doi: 10.3961/jpmph.21.337
31. Lim EJ. Gender differences in the relationship between physical functioning and depressive symptoms in low-income older adults living alone. Nurs Health Sci. (2014) 16:381–6. doi: 10.1111/nhs.12119
32. Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
33. Xia N, Li H. Loneliness, social isolation, and cardiovascular health. Antioxid Redox Signal. (2018) 28:837–51. doi: 10.1089/ars.2017.7312
34. Gureje O, Kola L, Afolabi E. Epidemiology of major depressive disorder in elderly Nigerians in the Ibadan study of ageing: a community-based survey. Lancet. (2007) 370:957–64. doi: 10.1016/S0140-6736(07)61446-9
35. Ni Y, Tein JY, Zhang M, Yang Y, Wu G. Changes in depression among older adults in China: a latent transition analysis. J Affect Disord. (2017) 209:3–9. doi: 10.1016/j.jad.2016.11.004
36. Harvey SB, Overland S, Hatch SL, Wessely S, Mykletun A, Hotopf M. Exercise and the prevention of depression: results of the HUNT cohort study. Am J Psychiatry. (2018) 175:28–36. doi: 10.1176/appi.ajp.2017.16111223
Keywords: living alone, depression, longitudinal studies, systematic review, meta-analysis
Citation: Wu D, Liu F and Huang S (2022) Assessment of the relationship between living alone and the risk of depression based on longitudinal studies: A systematic review and meta-analysis. Front. Psychiatry 13:954857. doi: 10.3389/fpsyt.2022.954857
Received: 27 May 2022; Accepted: 11 August 2022;
Published: 30 August 2022.
Edited by:
Aliya Naheed, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), BangladeshReviewed by:
Mir Nabila Ashraf, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), BangladeshCopyright © 2022 Wu, Liu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fuwei Liu, Z3psaXVmdXdlaUAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.