- 1Psychiatry Unit, Department of Health Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy
- 2Department of Psychiatry, University of Perugia, Perugia, Italy
- 3Psychiatry Unit, Department of Medical and Surgical Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy
Introduction: Dissociative symptoms have been recently related to bipolar disorder (BD) symptomatology. Moreover, the disease burden carries on a share of perceived self-stigma that amplifies the BD impairment. Internalized stigma and dissociative symptoms often seem overlapping, leading toward common outcomes, with reduced treatment seeking and poor adherence. We hypothesize a potential relationship between dissociation and self-stigma in patients suffering from BD.
Materials and methods: In this cross-sectional study we enrolled a total of 120 adult clinically stable BD outpatients. All participants completed the Internalized Stigma of Mental Illness (ISMI), Dissociative Experiences Scale-II (DES-II), and Manchester Short Assessment of Quality of Life (MANSA).
Results: Average age and age at BD (BD-I n = 66, 55%; BD-II n = 54, 45%) onset were 46.14 (±4.23), and 27.45 (±10.35) years, with mean disease duration of 18.56 (±13.08) years. Most participants were female (n = 71; 59.2%) and 40 (33%) of them experienced lifetime abuse, with an average of 1.05 (±0.78) suicide attempts. DES scores (mean 31.8, ±21.6) correlated with ISMI total-score, with significant association with spikes in Alienation (13.1, SD±3.1) (p < 0.001) and Stereotype (13.8, SD±3.9) (p < 0.001). Linear regression analysis has shown a significant association between DES total score and alienation (p < 0.001), stereotype (p < 0.001) and MANSA total-score (p < 0.001).
Discussion: For the first time, our data suggests that self-stigma is associated to dissociative symptoms, reducing overall quality of life in BD. The early identification of at-risk patients with previous lifetime abuse and high perceived stigma could lead the way for an ever more precise tailoring of treatment management.
Introduction
Bipolar disorder (BD) is a severe psychiatric disorder characterized by shifts of emotions, energy and thought, as well as changes in concentration and sleep need, with impairment in the ability to carry out day-to-day tasks, which mainly occur during biphasic mood episodes of mania or hypomania and depression, and are expressed as recurrent episodes of changes in energy levels and behavior, with a negative impact on patients' overall quality of life (1, 2).
The lifetime prevalence is around 1% worldwide, and, usually, the onset is in the late second or early third decade of life (1, 3). The chronic episodic course negatively affects several aspects of patients' life, including interpersonal relationships and occupational functioning, and can also lead to severe outcomes, including death by suicide (4, 5). Recently, dissociative symptoms have been related to BD symptomatology and phenotype characterization suggesting a role in the etiology and clinical course of the disease, thus representing a new area of study both for research and for the clinic, with the aim of a more precise tailoring of patients' treatment management (6).
Frequently, not recognizing the mood shift and poor insight can delay treatment initiation and a worsening of the clinical course (7, 8). Indeed, these two aspects of BD could be due to a considerable heterogeneity of clinical presentation and the patients' fear of being stigmatized in case of seeking help (9). However, both reduced treatment-seeking and the worst clinical course can lead to a severe outcome and frequently are associated with social withdrawal, functional impairment and alienation (4, 5). Consequentially, stigma is a critical issue in BD because it leads to poor treatment adherence and more severe symptomatology (10). This is an important concern because the chronic mood shift could represent a risk factor for psychosis, traumatic events, and cognitive impairment, and all those aspects were correlated to dissociative symptomatology (11, 12).
Moreover, several studies highlight that patients suffering from affective disorders present dissociation as a preferred coping strategy (13, 14), and dissociative experience disrupts wholeness in the stream of mind. Dissociation also prevents the integration of experiences and information and leads to amnesia, depersonalization, and derealization (15, 16). Additionally, internalized stigma and dissociative symptoms seem to overlap, sharing features such as alienation, isolation, functional impairment and disease burden, often leading to common outcomes with reduced treatment-seeking and poor adherence (17).
In recent years, some advances have been made regarding the knowledge concerning stigma in BD, and, according to our current understanding, there are mainly three kinds of stigma. The most well-studied concept is the internalized or self-stigma, which explains the subjective appreciation of negative experiences and perceptions of the patients themselves, leading to identity transformation and stereotype endorsement (18). The second entity is perceived stigma, namely the patients' subjective experience of being stigmatized by other agencies (19, 20). This is mostly contributed by endorsing various discriminatory traits deep-rooted in the disease process. Structural or systemic stigma is the third and probably a minor studied entity. It refers to institutional policies and practices surrounding a person that creates inequality by restricting opportunities for people suffering from mental illness (21, 22). Stigma also involves perceiving patients with BD with a negative outlook and attributing stereotypes, thus further leading to interference in community participation. However, the debate on developing effective interventions to fight stigma related to BD or other general medical and psychiatric diseases is still ongoing (23).
We hypothesize a potential relationship between internalized stigma and dissociative phenomena in patients affected by BD, potentially leading to a peculiar negative clinical course and a worsening quality of life. Therefore, the present work aimed to assess the correlation between self-stigma, dissociative symptoms, and quality of life in a clinical sample of patients suffering from BD with a cross-sectional study design, and to test if the dissociative symptomatology may be related to a specific subthreshold of internalized stigma and/or to quality of life.
Materials and methods
Participants and procedures
This study was designed as a naturalistic and uncontrolled cross-sectional observational study at the outpatients' Psychiatry unit of the University Hospital Mater Domini of Catanzaro (Italy) and was conducted between May 2020 and January 2022. All consecutive potentially candidate patients were screened for eligibility and invited to participate in the study, where applicable. Participants were screened and diagnosed by a clinical interview conducted by experienced clinicians through the Structured Clinical Interview for DSM-5 (SCID-5 CV) (24). The interviewers were experienced psychiatrists who work in clinical research, were trained in administering neuropsychiatric tools, and used these tests in their daily clinical practice.
We included all patients fulfilling the following inclusion criteria: (1) aged between 18 and 70 years and able to read and understand the informed consent form; (2) capability to answer self-report questionnaires; (3) diagnosed with BD type-I (BD-I) or type-II (BD-II) according to the Diagnostic and Statistical Manual of Mental Disorders-fifth edition (DSM-5) (24); (4) clinically stable, if at the time of enrollment the Clinical Global Impression for Bipolar Patients (CGI-BP) (25) scored ≤2 at item 1 (severity of illness). We did not set any other inclusion criteria, with the goal to achieve a real-world clinical sample, as routinely visited in daily clinical activity. Regarding exclusion criteria, we excluded patients if: (1) with recent (≤6 months) or uncertain BD diagnosis or with a medical history that was implausible or undocumented; (2) with comorbid psychiatric diagnosis (i.e., schizophrenia spectrum disorders, major depressive disorder, post-traumatic stress disorder); (3) affected by dementia or intellectual disability from mild to severe according to DSM-5 (corresponding to IQ <70); (4) with alcohol or drug abuse in the previous 6 months and dependence for 12 months according to DSM-5 diagnostic criteria; (5) suffering from another severe medical condition related with psychiatric symptoms (e.g., temporal lobe epilepsy, multiple sclerosis, brain trauma, malignant disease).
According to the Ethical Committee, participants were provided with a complete description of the study aims and methods and gave written informed consent to participate in the study before any procedure took place. The study protocol was submitted and approved by the Ethical Committee of University Hospital Mater Domini at Catanzaro (n. 307/2020), and the study procedures were carried out in accordance with the ethical principles set out in the revised version of the Helsinki Declaration (26).
Assessments
We collected patients' demographics and clinical (i.e., psychopharmacological therapy) information through an ad hoc schedule. In detail, we used a semi-structured interview collecting data on age, sex, civil status, years of education, current occupation, family history of psychiatric diseases, psychiatric and general medical comorbidity, onset, and longitudinal course of the disorder (e.g., number of depressive/hypo/manic episodes, mixed and anxious features, and psychotic symptoms), number of previous suicidal attempts and psychiatric hospitalizations, and current prescribed treatments.
Then, all participants were evaluated by means of the following Italian versions of assessment scales:
• The Clinical Global Impression for Bipolar Patients (CGI-BP) (25) is a modified version of the original CGI specifically developed to assess global illness severity and change in patients affected by bipolar disorder, and already used with Italian clinical samples (27). It is divided into two sections, severity of illness and global improvement, and both range between a minimum of one (“normal, not ill at all”) to a maximum of seven (“among the most extremely ill patients”), while 0 denotes the impossibility to assess the score.
• The Internalized Stigma of Mental Illness (ISMI) scale (28) is a 29-item self-administrated questionnaire measuring self-stigma in the population suffering from mental disorders. It has been structured to quantity the subjective experience of stigma, with subscales measuring Alienation (six items), Stereotype Endorsement (seven items), Perceived Discrimination (five items), Social Withdrawal (six items) and Stigma Resistance (five items) through 29 Likert questions with four reply options, ranging between strongly disagree (one point) and strongly agree (four points), with a total score between 29 and 116 (28). It is a widely used and validated tool whose psychometric proprieties have been comprehensively evaluated across multiple versions, cultures, and languages, including Italy (18, 29), as well as several major psychiatric disorders (e.g., depression, schizophrenia, substance abuse, eating disorders) and general medical illnesses (e.g., epilepsy, inflammatory bowel disease, leprosy) (20). It should be considered that the five stigma resistance subscale items are reverse-coded, and also serve as a validity check (28). Therefore, stigma resistance displays the same direction of correlation as the other four subscales. A high total score on the ISMI scale indicates more severe internalized stigmatization (30).
• The Dissociative Experiences Scale II (DES-II) (31), and its Italian version (32), is a largely used self-assessment measure developed to offer a feasible tool of reliably quantifying dissociative symptoms in both general and clinical populations. The scale is made up of 28 items describing dissociation features (i.e., absorption, amnesia, depersonalization, and derealization), and the user is asked to select a percentage defining how much the patient experienced the symptom, ranging from 0 (never) to 100% (always). The final score comes from the sum of all items divided by the number of total items (i.e., 28), ranging between 0 and 100. The dissociative disorder cut-off is settled with scores >30.
• The Manchester Short Assessment of Quality of Life (MANSA) has been developed as a brief, handy and innovative instrument for assessing the quality of life, focusing on satisfaction with life as a whole and with life domains (33). It includes 16 questions, four of them investigating the objective quality of life and rated by a dichotomized yes/no scale, and 12 rated on a 7-point scale and exploring satisfaction with life, job, financial situation, friendships, leisure activities, accommodation, personal safety, people that the person lives with, family and global health. Its maximum total score is 93 points. Finally, an overall subjective quality of life score may be calculated (34). The MANSA scale showed good reliability, construct validity, and internal consistency when investigating quality of the life in people affected by severe general medical and psychiatric conditions, including Italian samples (34, 35).
Statistical analyses
Descriptive statistics were calculated for socio-demographic and clinical characteristics and other relevant assessment instruments. As appropriate, data are presented as means and standard deviations (SD) or frequencies and percentages (%). A Spearman's correlation analysis was performed to test the correlation between psychometric scale and clinical and sociodemographic variables. A linear regression model was used to describes the relationship between the DES total score as dependent variable, and ISMI subscales and MANSA total score as independent variables. Odds ratios (OR) with 95% confidence intervals were assessed for observed associations. All tolerance values in the regression analyses were >0.1 and all variance inflation factors were <10, expressing that the assumption of multicollinearity was not violated. The level of statistical significance was set at a nominal value of p ≤ 0.05. Statistical analyses were performed by using the Statistical Package for Social Sciences Version 26 (SPSS, Chicago, Illinois, USA).
Results
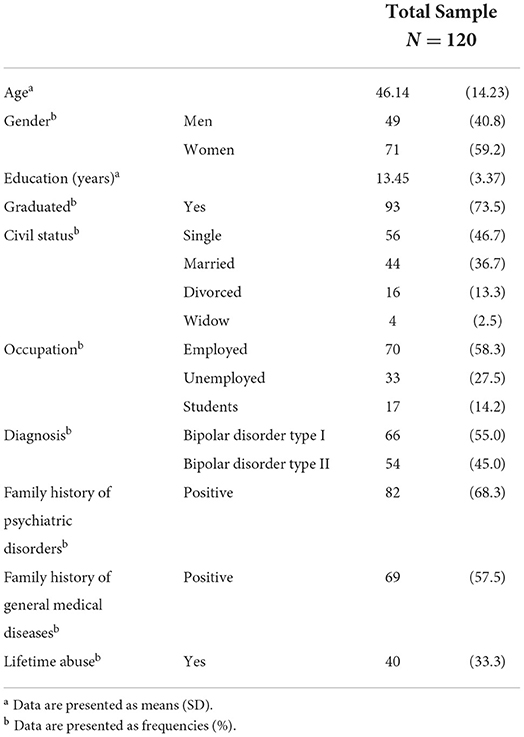
We approached a total of 138 consecutive patients fulfilling the inclusion and exclusion criteria. Of these, a total of 18 did not participate in the study due to the following reasons: refusal to complete the assessment (n = 10) or to sign the informed consent (n = 6), or other reasons (n = 2). Therefore, the final sample was made up of 120 patients, of whom 66 (55%) suffering from BD-I and 54 (45%) from BD-II. The average age (± standard deviation, SD) was 46.1 (±14.23) years, and the majority of participants were female (n = 71; 59.2%), single (n = 56; 46.7%), graduated (n = 93; 73.5%), employed (n = 70; 58.3%), with positive family history for both psychiatric (n = 82; 68.3%) and general medical (n = 69; 57.5%) disease, and 33.3% (n = 40) of them experienced lifetime abuse (Table 1).
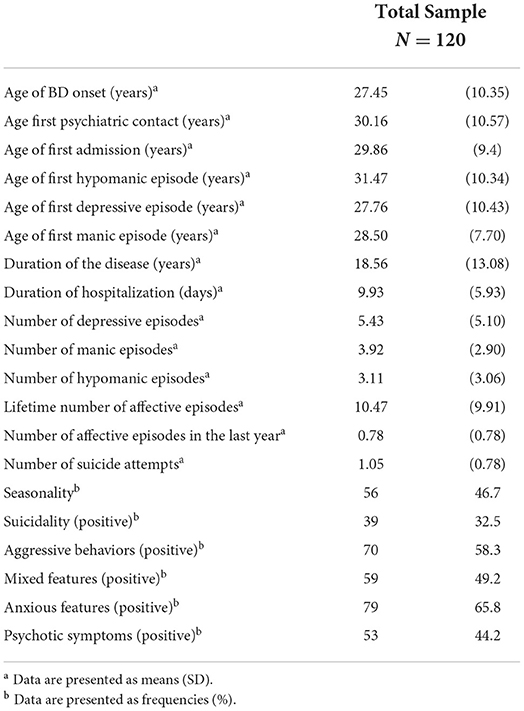
Regarding clinical features, the average age (± standard deviation, SD) at BD onset was 27.45 (±10.35), while the average disease duration was 18.56 (±13.08) years. We recorded a mean of 5.43 (±5.10) depressive, 3.92 (±2.90) maniac, and 3.11 (±3.06) hypomanic episodes, then the average number of affective episodes was 10.47 (±9.91) among patients. Most included patients presented aggressive behaviors (n = 70; 58.3%) and anxious features (n = 79; 65.8%), with also frequent mixed (n = 59; 49.2%) and psychotic (n = 53; 44.2%) symptoms. Seasonality was also very common (n = 56; 46.7%), as well as suicidality (n = 39; 32.5%), with an average of 1.05 (±0.78) suicide attempts (Table 2).
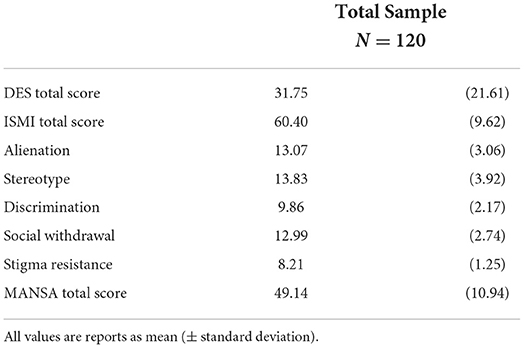
The DES mean (± standard deviation, SD) score was higher than the settled cut-off of 30 points (i.e., 31.8 (±21.6), with spikes shown especially in Alienation (13.1, ±3.1), Stereotype (13.8, ±3.9) and Social distancing (13.0, ±2.7) items. As for the MANSA scale, participants scored an average total of 49.1 (±10.9) out of 93 total points, while ISMI mean score was 60.4 (±9.6) out of a tool range between 29 and 116 (Table 3).
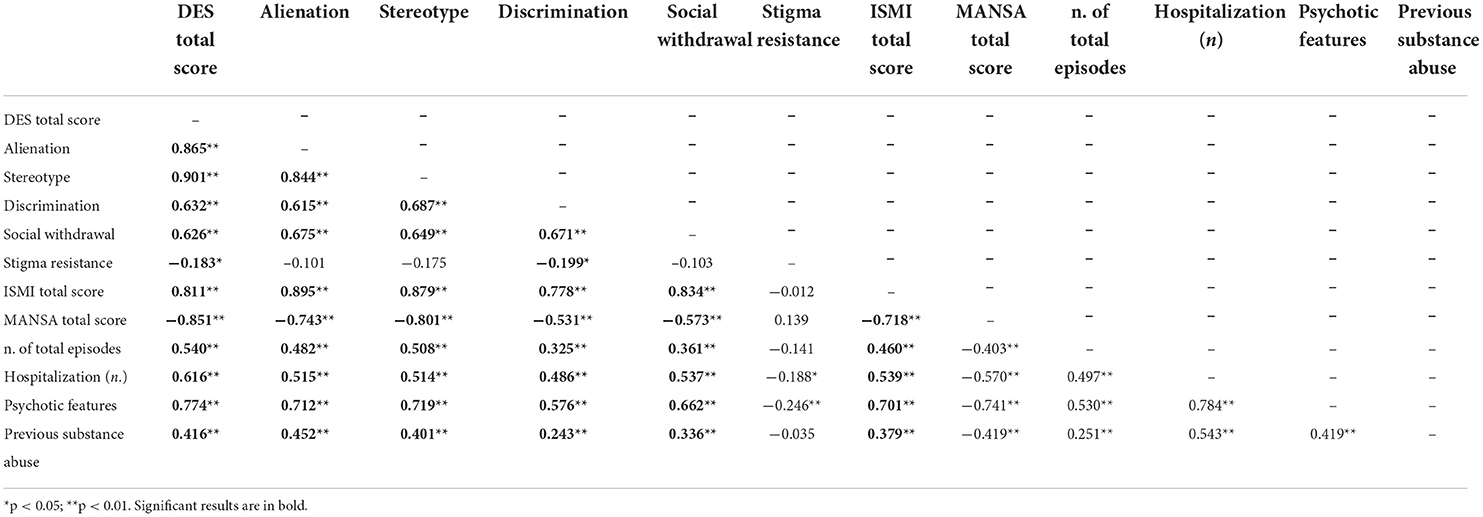
Table 4 includes the results of Spearman's correlations between DES-II total score, ISMI-specific subdomains, ISMI total score and MANSA total score and clinical features (i.e., number of total episodes, hospitalization, psychotic features, and previous substance abuse). Several significant correlations emerged for almost all variables, particularly between DES total score, ISMI subdomains and ISMI total score.
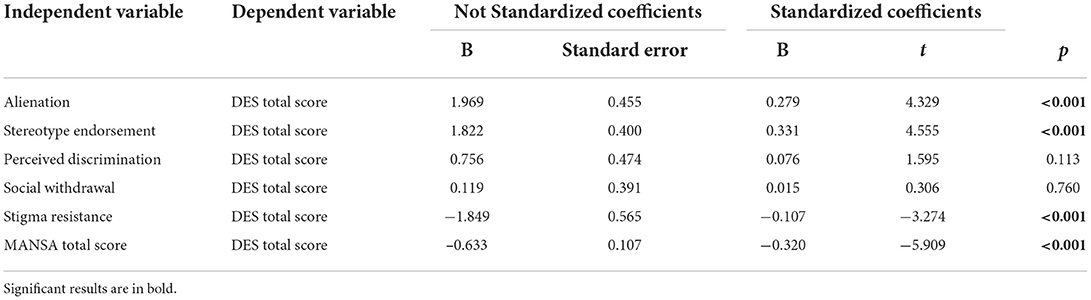
A linear regression with DES total score as dependent variable was performed to assess the association between dissociative symptomatology and ISMI total score, ISMI sub-domains, and MANSA. A significant association was found between Alienation (B = 0.279; t = 4.329; p < 0.001), Stereotype (B = 0.331; t = 4.555; p < 0.001) and MANSA total score (B = –0.320; t = –5.909; p < 0.001) (Table 5).
Discussion
This study found a strong relationship between internalized stigma and dissociative phenomena in patients suffering from BD, which may lead to a peculiar negative clinical course and a worsening quality of life. To the best of our knowledge, this is the first time internalized stigma was explored concerning its role in dissociation symptoms in BD, with consequences on quality of life. Further, as shown by Spearman's correlation analysis, internalized stigma is correlated to several clinical variables predictive of poor clinical outcomes in BD. ISMI total score correlates to a higher number of total episodes, hospitalization, psychotic features, and previous substance abuse, highlighting its impact on those factors predictive of a higher psychopathological burden. Such results are easily explained due to the impact of stigma on the life of psychiatric patients, especially those suffering from BD (36, 37). A growing body of literature focused on the sociodemographic and clinical variables correlated to the stigma, and our results are in line with them except for the age of onset, which was poorly investigated before (38, 39). Stigma has a significant impact on people with BD, linked to negative stereotypes, prejudice and discrimination (8).
Usually, one of the most explored findings resulting from studies using ISMI is the relationship between internalized stigma and more severe psychopathology, lower self-esteem, reduced treatment adherence, and greater symptom severity (40–42). Pilot studies exploring ways to reduce internalized stigma are promising and warrant further investigation (20). In addition, a negative correlation is reported with the perceived quality of life. Initial studies on ways to reduce internalized stigma are promising but need further investigation (43, 44). Research has focused on the relationship between internalized stigma and self-esteem and how this implies negative evaluations (45, 46). An issue underlying this hypothesis is the influence that different processes have on self-esteem: one of the most critical concerns is the response of others. Many authors suggest that patients affected by mental illness tend to have dissociative symptoms that lead to alienation, discrimination, and negative representation even before being diagnosed. Due to this, several negative consequences occur, including the tendency to social isolation and a reduction in interpersonal relationships. This maladaptive schema worsens the patient's quality of life (47, 48). To date, little research has focused on the phenomenon of internalized stigma and the negative aspects related to it. The results obtained in the present study confirm our hypothesis, according to which there is a direct effect between dissociation and internalized stigma, particularly in the alienation and stereotype fields. Alienation is widespread among patients with bipolar disorder, especially those with higher psychopathological burdens, and refers to a sense of self-estrangement and poor social connection (49). The phenomenon of alienation represents an essential indicator of mental well-being and is often associated with depressed mood, dissociative symptoms, and psychological distress, even in other severe psychiatric disorders (50). According to our results, patients with a high level of dissociative symptoms and low self-esteem attribute a high level of stigma to themselves.
Further, previous research indicates alienation as a maladaptive coping strategy in psychiatric patients facing traumatic experiences (51, 52). This field might explain the strong connection resulting in the linear regression between alienation and dissociation. Moreover, a significant association was found between dissociation and stereotype. These results support the hypothesis that mental illness stereotypes still may represent a cultural barrier. Indeed, patients affected by chronic severe psychiatric disorders could experience social stigma feeling it as a trauma, thus rising maladaptive coping strategies, including dissociation (53).
Consequently, both self-stigma and dissociative symptoms represent two elements of greater severity of BD that potentially worsen its clinical outcome lowering treatment adherence and deteriorating the prognosis (54, 55). Previous research has focused on the difference in internalized stigma in different cohorts of psychiatric patients, highlighting the major level of internalized stigma in bipolar disorder rather than non-affective psychotic disorders (56, 57). Another expected result in line with the literature is the negative relationship between internalized stigma and quality of life. Several studies have been conducted on this topic. The explanation is that internalized stigma is associated with adverse psychological outcomes such as depressive symptoms, lower self-esteem and reduced self-efficacy, which a poorer outcome will reflect on the psychological domain (58–60).
Moreover, results presented in our study should be interpreted in the light of both some limitations and strengths. Indeed, although the clinical sample involved was recruited in a naturalistic setting, adequate to describe the general population and similar to several analogous studies (8, 61, 62), the inconspicuous final sample size as well as the lack of hypothesis-driven sample size estimation and the absence of confounders addressed in the linear regression model represent the main study limitations which preclude drawing causal conclusions; therefore, we foresee the implementation of the sample size together with a prospective study design to confirm the results obtained. Secondly, the cross-sectional design using self-administered evaluations represents a structural limitation regarding the assembly and reliability of the data, which must be considered in any generalization of the results. Finally, the enrolled patients were clinically stabilized as inclusion criteria, so a mirror evaluation in patients with acute BD may result differently. Hence, the need to replicate similar protocols on larger samples with perspectives capable of acquiring designs at different stages of the disease. On the other hand, this was the first attempt to evaluate the role and implications of internal stigma in BD, taking into account its relationships to demographics, history of the disease, clinical features, quality of life, and dissociative symptoms. Thus, the results presented in this study open a new perspective on the role that self-stigma and dissociative symptoms play in BD. Indeed, future studies could shed the light on the causal and temporal relationship existing between internalized-stigma and dissociation, opening new and interesting frontiers in both clinical and research fields.
Conclusion
Recently, dissociative symptoms have been studied concerning their impact on BD clinical course and treatment response, while perceived stigma is already well-known to interfere with clinical outcomes. However, the relationship between dissociative symptoms, self-stigma and quality of life in patients suffering from BD is still far from being fully understood and has been explored in this study.
Although burdened by several limitations and by a cross-sectional study design which avoids a generalization, our findings correlate self-stigma reported by patients affected by BD to experienced dissociative symptoms, resulting in a reduced overall quality of life. Therefore, the study of this network may represent an area of clinical research interest for the future, with the goal of reaching a more patients' focused clinical practice to anticipate a precise diagnosis, manage personalized treatment, and improve prognosis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee of University Hospital Mater Domini at Catanzaro (Italy) (n. 307/2020), and the study procedures were carried out in accordance to the ethical principles set out in the revised version of the Helsinki Declaration. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LS: conceptualization and formal analysis. RdF and LS: methodology and writing the original draft preparation. RdF, MD'A, and LS: investigation and data curation. RdF, GM, EC, AT, PD, and LS: writing and review and editing. All authors read and approved the final manuscript.
Acknowledgments
The authors are grateful to patients who took part in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Smith DJ, Whitham EA, Ghaemi SN. Bipolar disorder. In: Handbook of Clinical Neurology, vol 106. (2012). p. 251-63
2. Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Prim. (2018) 4:18008. doi: 10.1038/nrdp.2018.8
3. Miller TH. Bipolar Disorder. Prim Care Clin Off Pract. (2016) 43:269–84. doi: 10.1016/j.pop.2016.02.003
4. Müller JK, Leweke FM. Bipolar disorder: clinical overview. Med Monatsschr Pharm. (2016) 39:363–9.
5. Greenberg PE, Fournier A-A, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. (2015) 76:155–62. doi: 10.4088/JCP.14m09298
6. Steardo L, Carbone EA, Ventura E, de Filippis R, Luciano M, Segura-Garcia C, De Fazio P. Dissociative symptoms in bipolar disorder: impact on clinical course and treatment response. Front Psychiatry. (2021) 12: doi: 10.3389/fpsyt.2021.732843
7. Uher R, Mantere O, Suominen K, Isometsä E. Typology of clinical course in bipolar disorder based on 18-month naturalistic follow-up. Psychol Med. (2013) 43:789–99. doi: 10.1017/S0033291712001523
8. Uher R, Pallaskorpi S, Suominen K, Mantere O, Pavlova B, Isometsä E. Clinical course predicts long-term outcomes in bipolar disorder. Psychol Med. (2019) 49:1109–17. doi: 10.1017/S0033291718001678
9. Ellison N, Mason O, Scior K. Public beliefs about and attitudes towards bipolar disorder: testing theory based models of stigma. J Affect Disord. (2015) 175:116–23. doi: 10.1016/j.jad.2014.12.047
10. Dubreucq J, Plasse J, Franck N. Self-stigma in serious mental illness: a systematic review of frequency, correlates, and consequences. Schizophr Bull. (2021) 47:1261–87. doi: 10.1093/schbul/sbaa181
11. Kehyayan V, Mahfoud Z, Ghuloum S, Marji T, Al-Amin H. Internalized stigma in persons with mental illness in Qatar: a cross-sectional study. Front Public Heal. (2021) 9:685003. doi: 10.3389/fpubh.2021.685003
12. Gomes DRAS, Zanetti ACG, Miasso AI, Castro FFS, Vedana KGG. Internalized stigma in people with mood disorders. J Nerv Ment Dis. (2021) 209:54–8. doi: 10.1097/NMD.0000000000001257
13. Levenson JC, Wallace ML, Fournier JC, Rucci P, Frank E. The role of personality pathology in depression treatment outcome with psychotherapy and pharmacotherapy. J Consult Clin Psychol. (2012) 80:719–29. doi: 10.1037/a0029396
14. O'Leary D, Costello F. Personality and outcome in depression: an 18-month prospective follow-up study. J Affect Disord. (2001) 63:67–78. doi: 10.1016/S0165-0327(00)00159-2
15. Pastucha P, Prasko J, Grambal A, Latalova K, Sigmundova Z, Tichackova A. Dissociative disorder and dissociation - comparison with healthy controls. Neuro Endocrinol Lett. (2009) 30:769–73.
16. Dell P, O'Neil J. Dissociation and the Dissociative Disorders: DSM-V and Beyond. New York, NY: Routledge. (2009).
17. Prasko J, Ociskova M, Grambal A, Sigmundova Z, Kasalova P, Marackova M, et al. Personality features, dissociation, self-stigma, hope, and the complex treatment of depressive disorder. Neuropsychiatr Dis Treat. (2016) 12:2539–52. doi: 10.2147/NDT.S117037
18. Boyd JE, Adler EP, Otilingam PG, Peters T. Internalized Stigma of Mental Illness (ISMI) Scale: a multinational review. Compr Psychiatry. (2014) 55:221–31. doi: 10.1016/j.comppsych.2013.06.005
19. Koumaki D, Efthymiou O, Bozi E, Katoulis AC. Perspectives on perceived stigma and self-stigma in patients with hidradenitis suppurativa. Clin Cosmet Investig Dermatol. (2019) 12:785–90. doi: 10.2147/CCID.S180036
20. Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. (2016) 18:11. doi: 10.1007/s11920-015-0654-1
21. Hatzenbuehler ML. Structural stigma: research evidence and implications for psychological science. Am Psychol. (2016) 71:742–51. doi: 10.1037/amp0000068
22. Mitchell UA, Nishida A, Fletcher FE, Molina Y. The long arm of oppression: how structural stigma against marginalized communities perpetuates within-group health disparities. Heal Educ Behav. (2021) 48:342–51. doi: 10.1177/10901981211011927
23. Ransing R, Ramalho R, de Filippis R, Ojeahere MI, Karaliuniene R, Orsolini L, et al. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: Drivers, facilitators, manifestations, and outcomes across the world. Brain Behav Immun. (2020) 89:555–8. doi: 10.1016/j.bbi.2020.07.033
24. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association (2013).
25. Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. (1997) 73:159–71. doi: 10.1016/S0165-1781(97)00123-6
26. World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191. doi: 10.1001/jama.2013.281053
27. Perugi G, Ceraudo G, Vannucchi G, Rizzato S, Toni C. Dell'Osso L. Attention deficit/hyperactivity disorder symptoms in italian bipolar adult patients: a preliminary report. J Affect Disord. (2013) 149:430–4. doi: 10.1016/j.jad.2012.12.010
28. Boyd Ritsher J, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. (2003) 121:31–49. doi: 10.1016/j.psychres.2003.08.008
29. Brohan E, Elgie R, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr Res. (2010) 122:232–8. doi: 10.1016/j.schres.2010.02.1065
30. Tanabe Y, Hayashi K, Ideno Y. The Internalized Stigma of Mental Illness (ISMI) scale: validation of the Japanese version. BMC Psychiatry. (2016) 16:116. doi: 10.1186/s12888-016-0825-6
31. Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. (1986) 174:727–35. doi: 10.1097/00005053-198612000-00004
32. Garofalo C, Velotti P, Zavattini GC, Tommasi M, Romanelli R, Espírito Santo H, et al. Struktura czynnikowa Skali Przezyć Dysocjacyjnych: włoska wersja skali DES-II. Psychiatr i Psychol Klin. (2015) 15:4–12. doi: 10.15557/PiPK.2015.0001
33. Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (Mansa). Int J Soc Psychiatry. (1999) 45:7–12. doi: 10.1177/002076409904500102
34. Björkman T, Svensson B. Quality of life in people with severe mental illness. Reliability and validity of the Manchester Short Assessment of Quality of Life (MANSA). Nord J Psychiatry. (2005) 59:302–6. doi: 10.1080/08039480500213733
35. Petrelli F, Grappasonni I, Peroni A, Kracmarova L, Scuri S. Survey about the potential effects of economic downturn on alcohol consumption, smoking and quality of life in a sample of Central Italy population. Acta Biomed. (2018) 89:93–8. doi: 10.23750/abm.v89i1.7059
36. Pal A, Sharan P, Chadda RK. Internalized stigma and its impact in Indian outpatients with bipolar disorder. Psychiatry Res. (2017) 258:158–65. doi: 10.1016/j.psychres.2017.09.087
37. Milev R, Mileva Vazquez. Effects, experiences, and impact of stigma on patients with bipolar disorder. Neuropsychiatr Dis Treat. (2013) 31. doi: 10.2147/NDT.S38560
38. Ellison N, Mason O, Scior K. Bipolar disorder and stigma: a systematic review of the literature. J Affect Disord. (2013) 151:805–20. doi: 10.1016/j.jad.2013.08.014
39. Hawke LD, Parikh S V, Michalak EE. Stigma and bipolar disorder: a review of the literature. J Affect Disord. (2013) 150:181–91. doi: 10.1016/j.jad.2013.05.030
40. Howland M, Levin J, Blixen C, Tatsuoka C, Sajatovic M. Mixed-methods analysis of internalized stigma correlates in poorly adherent individuals with bipolar disorder. Compr Psychiatry. (2016) 70:174–80. doi: 10.1016/j.comppsych.2016.07.012
41. Post F, Pardeller S, Frajo-Apor B, Kemmler G, Sondermann C, Hausmann A, et al. Quality of life in stabilized outpatients with bipolar I disorder: associations with resilience, internalized stigma, and residual symptoms. J Affect Disord. (2018) 238:399–404. doi: 10.1016/j.jad.2018.05.055
42. Post F, Buchta M, Kemmler G, Pardeller S, Frajo-Apor B, Hofer A. Resilience predicts self-stigma and stigma resistance in stabilized patients with bipolar I disorder. Front Psychiatry. (2021) 12:1–8. doi: 10.3389/fpsyt.2021.678807
43. Çuhadar D, Çam MO. Effectiveness of psychoeducation in reducing internalized stigmatization in patients with bipolar disorder. Arch Psychiatr Nurs. (2014) 28:62–6. doi: 10.1016/j.apnu.2013.10.008
44. Keshavarzpir Z, Seyedfatemi N, Mardani-Hamooleh M, Esmaeeli N, Boyd JE. The effect of psychoeducation on internalized stigma of the hospitalized patients with bipolar disorder: a quasi-experimental study. Issues Ment Health Nurs. (2021) 42:79–86. doi: 10.1080/01612840.2020.1779881
45. Shumet S. W/Michele B, Angaw D, Ergete T, Alemnew N. Magnitude of internalised stigma and associated factors among people with bipolar disorder at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: a cross-sectional study. BMJ Open. (2021) 11:e044824. doi: 10.1136/bmjopen-2020-044824
46. Oliveira SEH, Esteves F, Carvalho H. Clinical profiles of stigma experiences, self-esteem and social relationships among people with schizophrenia, depressive, and bipolar disorders. Psychiatry Res. (2015) 229:167–73. doi: 10.1016/j.psychres.2015.07.047
47. Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. (2000) 177:4–7. doi: 10.1192/bjp.177.1.4
48. Holubova M, Prasko J, Matousek S, Latalova K, Marackova M, Vrbova K, et al. Comparison of self-stigma and quality of life in patients with depressive disorders and schizophrenia spectrum disorders – a cross-sectional study. Neuropsychiatr Dis Treat. (2016) 12:3021–30. doi: 10.2147/NDT.S121556
49. Perugi G, Akiskal HS, Rossi L, Paiano A, Quilici C, Madaro D, et al. Chronic mania. Br J Psychiatry. (1998) 173:514–8. doi: 10.1192/bjp.173.6.514
50. Grover S, Avasthi A, Singh A, Dan A, Neogi R, Kaur D, et al. Stigma experienced by patients with severe mental disorders: a nationwide multicentric study from India. Psychiatry Res. (2017) 257:550–8. doi: 10.1016/j.psychres.2017.08.027
51. Regehr C, Goldberg G, Hughes J. Exposure to human tragedy, empathy, and trauma in ambulance paramedics. Am J Orthopsychiatry. (2002) 72:505–13. doi: 10.1037/0002-9432.72.4.505
52. Gilmoor A, Vallath S, Regeer B, Bunders J. “If somebody could just understand what I am going through, it would make all the difference”: conceptualizations of trauma in homeless populations experiencing severe mental illness. Transcult Psychiatry. (2020) 57:455–67. doi: 10.1177/1363461520909613
53. Levy BR, Chung PH, Slade MD, Van Ness PH, Pietrzak RH. Active coping shields against negative aging self-stereotypes contributing to psychiatric conditions. Soc Sci Med. (2019) 228:25–9. doi: 10.1016/j.socscimed.2019.02.035
54. Karidi MV, Vassilopoulou D, Savvidou E, Vitoratou S, Maillis A, Rabavilas A, et al. Bipolar disorder and self-stigma: a comparison with schizophrenia. J Affect Disord. (2015) 184:209–15. doi: 10.1016/j.jad.2015.05.038
55. Rasmussen JD, Kakuhikire B, Baguma C, Ashaba S, Cooper-Vince CE, Perkins JM, et al. Portrayals of mental illness, treatment, and relapse and their effects on the stigma of mental illness: population-based, randomized survey experiment in rural Uganda. PLoS Med. (2019) 16:e1002908. doi: 10.1371/journal.pmed.1002908
56. Sarisoy G, Kaçar ÖF, Pazvantoglu O, Korkmaz IZ, Öztürk A, Akkaya D, et al. Internalized stigma and intimate relations in bipolar and schizophrenic patients: a comparative study. Compr Psychiatry. (2013) 54:665–72. doi: 10.1016/j.comppsych.2013.02.002
57. Chang C-C, Wu T-H, Chen C-Y, Lin C-Y. Comparing self-stigma between people with different mental disorders in Taiwan. J Nerv Ment Dis. (2016) 204:547–53. doi: 10.1097/NMD.0000000000000537
58. Mashiach-Eizenberg M, Hasson-Ohayon I, Yanos PT, Lysaker PH, Roe D. Internalized stigma and quality of life among persons with severe mental illness: the mediating roles of self-esteem and hope. Psychiatry Res. (2013) 208:15–20. doi: 10.1016/j.psychres.2013.03.013
59. Picco L, Pang S, Lau YW, Jeyagurunathan A, Satghare P, Abdin E, et al. Internalized stigma among psychiatric outpatients: associations with quality of life, functioning, hope and self-esteem. Psychiatry Res. (2016) 246:500–6. doi: 10.1016/j.psychres.2016.10.041
60. Cerit C, Filizer A, Tural Ü, Tufan AE. Stigma: a core factor on predicting functionality in bipolar disorder. Compr Psychiatry. (2012) 53:484–9. doi: 10.1016/j.comppsych.2011.08.010
61. Pal A, Saxena V, Avinash P. Stigma in bipolar affective disorder: a systematic quantitative literature review of Indian studies. Indian J Psychol Med. (2021) 43:187–94. doi: 10.1177/0253717621996618
Keywords: bipolar disorder, dissociation, internalized stigma, mental health, mood disorders, psychopathology, quality of life, trauma
Citation: de Filippis R, Menculini G, D'Angelo M, Carbone EA, Tortorella A, De Fazio P and Steardo L Jr (2022) Internalized-stigma and dissociative experiences in bipolar disorder. Front. Psychiatry 13:953621. doi: 10.3389/fpsyt.2022.953621
Received: 26 May 2022; Accepted: 11 July 2022;
Published: 29 July 2022.
Edited by:
Andrew T. Olagunju, McMaster University, CanadaReviewed by:
Babatunde Fadipe, Lagos University Teaching Hospital, NigeriaOlaniyi Olayinka, University of Texas Health Science Center at Houston, United States
Copyright © 2022 de Filippis, Menculini, D'Angelo, Carbone, Tortorella, De Fazio and Steardo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renato de Filippis, ZGVmaWxpcHBpc3JlbmF0b0BnbWFpbC5jb20=
†ORCID: Renato de Filippis https://orcid.org/0000-0001-6928-1224
Giulia Menculini https://orcid.org/0000-0001-8380-1943
Elvira Anna Carbone https://orcid.org/0000-0001-5521-6552
Alfonso Tortorella https://orcid.org/0000-0002-8095-2305
Pasquale De Fazio https://orcid.org/0000-0001-5375-3565
Luca Steardo Jr. https://orcid.org/0000-0002-7077-3506
 Renato de Filippis
Renato de Filippis Giulia Menculini
Giulia Menculini Martina D'Angelo1
Martina D'Angelo1 Luca Steardo Jr.
Luca Steardo Jr.