
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 14 September 2022
Sec. Anxiety and Stress Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.947945
This article is part of the Research Topic Assessing and Evaluating the Impact Of The Covid 19 Pandemic on Anxiety And Stress: A Global Perspective View all 16 articles
Background: Social support is an important factor affecting individual mental health. However, the relationship between social support and mental health in frontline healthcare workers (FHW) during the coronavirus disease 2019 (COVID-19) pandemic has garnered less attention. In this study, we aimed to investigate the level of social support and the prevalence of depression and anxiety in FHW during the COVID-19 pandemic and determine the factors affecting the relationship between social support, depression, and anxiety.
Methods: A cross-sectional study using an online survey was conducted to collect data from FHW between 15 February and 31 March 2020 in China. The data included demographic factors, Self-rated Depression Scale (SDS), Self-rated Anxiety Scale (SAS), and Social Support Rate Scale (SSRS). Spearman correlation test was performed to determine the correlation among SAS, SDS, and SSRS scores. Multiple linear regression analysis was performed to determine the relationship among demographic factors, social support, depression, and anxiety in FHW.
Results: Of all 201 participants, 44 (21.9%) had depressive symptoms and 32 (15.9%) had anxiety symptoms. The average total SSRS scores among FHW were lower than that of the norms of the Chinese general population (37.17 ± 7.54 versus 44.38 ± 8.38, P < 0.001). Marital status positively affected the SSRS score (β = 7.395, P < 0.01). Age over 40 years old negatively affected the SSRS score (β = −5.349, P = 0.017). The total SSRS score, subjective social support score, objective social support score, and support utilization score among FHW negatively correlated with the SAS score and SDS score (P < 0.05). A lower support utilization score was significantly associated with high anxiety and depressive symptoms (β = −0.869, P = 0.024; β = −1.088, P = 0.035, respectively).
Conclusion: During the COVID-19 pandemic, FHW experienced depression, anxiety, and inadequate social support. The marital status and age had a major impact on social support. Social support was inversely associated with depression and anxiety. Improving the mental health of FHW by strengthening social support is crucial. Future studies are needed to investigate how to improve the level of social support and mental health condition of FHW facing public health emergencies in the future.
Since its outbreak in December 2019 in Wuhan, coronavirus disease 2019 (COVID-19) has posed a huge challenge to the healthcare system of China. On 29 January 2020, all 31 Chinese provinces declared public health emergencies and initiated lockdown policies in affected areas (1). As of 31 March 2020, 81,518 cases and 3,187 deaths were reported in China (2).
Amidst the development of the COVID-19 pandemic, frontline healthcare workers (FHW) globally were under tremendous pressure, and many suffered from psychological disorders (3), such as anxiety, depression, psychological stress response, and sleep disorders (4). When this online survey was conducted, the COVID-19 pandemic in China was still serious, with more than 2,400 confirmed cases and 139 deaths every day (5). FHW had to simultaneously prevent and treat the infection of COVID-19. The exhaustive work and risk of being infected by the virus caused a heavy psychological burden on FHW. Wearing protective equipment can relatively limit the communication of FHW. These factors can induce the presence of anxiety and depression among FHW during the COVID-19 pandemic. A cross-sectional study performed in the early stages of the COVID-19 outbreak reported that a significant proportion of FHW in China reported symptoms of depression (50.4%), anxiety (44.6%), insomnia (34.0%), and distress (71.5%) (6). Furthermore, anxiety symptoms can compromise work and frontline activities that can negatively affect private and social leisure activities (7). Previous studies focusing on the mental health reactions of healthcare workers during the acute phase of the COVID-19 pandemic reported that post-traumatic stress disorder, anxiety, and depression were associated with impairment in both work and social functioning (8, 9). FHWs are the direct providers of hospital services and are a key factor in controlling the pandemic (10). These psychological disorders affect the quality of life and health of FHW and also their professional performance, which greatly reduce their work efficiency and negatively affect the control of the COVID-19 pandemic.
Social support, which refers to the social connections, social integration, and major group relationships for individuals, is an important part of social psychology (11). Social support can enhance the protection of self-consciousness and effectively relieve the psychological disorders of individuals (12, 13). Lau proposed that social support is a crucial factor in alleviating stressful events and reducing their negative effects on the physical and mental health of individuals (14). Social support is associated with depression among health workers in developed countries (15, 16). Similarly, Chinese physicians had a higher prevalence of depressive symptoms and lower social support than the Chinese general population (17). A cross-sectional survey of Chinese doctors reported that social support is an important protective factor for the psychology of doctors. The more social support provided to doctors, the lower their depressive and anxiety symptoms (18). Another study also revealed that sufficient social support and training on positive coping skills can reduce anxiety in medical staff during the COVID-19 pandemic (19). Although these studies investigated the association between social support, depression, and anxiety among health workers, the relationship between social support and mental health among FHW during the COVID-19 pandemic was not investigated. The studies on psychological disorders of FHW in China mostly focused on epidemiological surveys (6, 20, 21). However, the relationship between social support and mental health among FHW during the COVID-19 pandemic has garnered less attention. The factors affecting the relationship between social support and mental health among FHW remains is yet to be investigated, which limits us from taking effective measures to help reduce psychological disorders, such as depression and anxiety, among FHW.
To bridge this gap, in this study, we aimed to investigate the level of social support and the prevalence of depression and anxiety among FHW during the COVID-19 pandemic and determine the factors affecting the relationship between social support, depression, and anxiety. We hope that our research can help us better understand the psychological needs of FHW during the pandemic and provide a basis for government health departments to formulate effective psychological rehabilitation intervention policies.
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine (No. ZE2020-036). This trial has been registered at the Chinese Clinical Trial Registry (No. ChiCTR2000029815). All participants provided their informed consent prior to their participation in the electronic questionnaire (with a “yes or no” question) to confirm their willingness to participate in this study. The data was stored on a cloud server accessible only to the main author.
This cross-sectional study was conducted from 15 February to 31 March 2020 in China after the COVID-19 outbreak has been declared as a public health emergency of international concern. As the Chinese government advised the public to reduce their face-to-face interactions and tightened restrictions on the flow of people, potential participants were invited to complete an anonymous online questionnaire. The online questionnaire was developed using the SurveyStar1 (Changsha Ranxing Information Technology Co., Ltd., Changsha, China). Next, we shared the questionnaire on the social media, including WeChat and Tencent QQ. The responses to the questionnaire were automatically collected into an EXCEL spreadsheet by the SurveyStar for further data analyses.
The inclusion criteria for the participants were as follows: (1) being a FHW; (2) age >18 years; (3) Chinese resident; (4) no history of mental illness; (5) submitted only one survey using the same IP address; and (6) volunteered to participate in this study. The exclusion criteria included the following: (1) working time on the frontline of COVID-19 prevention and control <1 week; (2) trainee, interns, external hired, or dispatched personnel; (3) refusal to participate in the survey; and (4) the time to complete the questionnaire being <5 min.
To determine the practicability of the online questionnaire, the constituent instruments were pilot-tested beforehand on a group of 20 FHW, and these individuals were excluded from the main study.
Demographic and social data were self-reported by the participants, which included their age, gender, marital status (married or single), educational level (master’s degree or above, bachelor’s degree or lower), profession (doctor or nurse), seniority (primary, intermediate, or senior), and the number of days working at the frontline since COVID-19 outbreak (7–28, >28 days). The participants were asked whether they were currently working in one of the following three departments: fever clinics, isolation ward for suspected cases, and treatment ward for confirmed cases. The respondents who answered with a “yes” were defined as FHW and those who answered with a “no” were defined as second-line healthcare workers. The latter were excluded from this study.
Depressive symptoms of FHW were assessed by the well-established Self-rated Depression Scale (SDS) (22). SDS is a widely recognized tool for evaluating depressive disorder (23). The score of each item was added and then multiplied by 1.25 as a total score ranged from 25 to 100, with a higher score indicating more depressive symptoms. The severity rating index for SDS were as follows: normal (25–52), mild (53–62), moderate (63–72), and severe (73–100). We categorized FHW with an SDS score ≥53 as having depressive symptoms. In this study, the Cronbach’s alpha of SDS was 0.886.
Anxiety symptoms were assessed by using the Self-rated Anxiety Scale (SAS) (24, 25). An aggregate score of 20 items was multiplied by 1.25, with a higher score indicating more severe levels of anxiety. Anxiety score of <50 was considered normal, that of 50–60 was considered mild, that of 61–70 was considered moderate, and that >70 was considered severe. We set the cutoff point of SAS at 50 to suggest anxiety symptoms. In this survey, the Cronbach’s alpha of SAS was 0.806.
Social support was assessed by using the Social Support Rate Scale (SSRS), which was designed to determine how much support respondents received from their family, friends, and social contexts (26, 27). SSRS consists of three subscales: subjective support (four items on the number of friends who offered assistance, relationship with neighbors, relationship with colleagues, and the level of support from family members), objective support (three items on the living conditions in the past year, problem-solving channels in emergency situations, and the sources of psychological comfort in the event of stress or resistance), and support utilization (three items on the way one expresses when in trouble, the way in which one seeks help when in trouble, and the willingness of participation in group activities). The total SSRS score is the sum of these three subscales scores, with a higher score indicating higher levels of social support (28). In this study, the Cronbach’s alpha value of SSRS was 0.844.
The dataset was entered and analyzed using the statistical package for the social sciences (SPSS) version 25.0 (IBM Corp., Armonk, NY, United States). The following descriptive statistics were used, including frequencies (n), percentages (%), means, and standard deviations (SD).
Shapiro–Wilk test was performed to examine the normality. Reliability was assessed with Cronbach’s alpha. One-sample mean test was performed to identify the difference in the SSRS score between FHW and the norms of Chinese general population. One-way analysis of variance was conducted to identify the difference in the SDS, SAS, and SSRS of the FHW based on the demographic factors. Spearman correlation analyses were performed to examine the relationship among the scores of SAS, SDS, and SSRS.
Multiple linear regression analysis was performed to examine the association between social support and demographic factors. The dependent variable was the total SSRS score, and the independent variables included age, marital status, and seniority. We also conducted multiple linear regression analysis to identify the relation among social support and the SDS and SAS scores. The dependent variable was the SDS and SAS scores. The independent variables included subjective social support score, objective social support score, support utilization score, and the total SSRS score. The regression model was statistically significant (P < 0.05), indicating a linear correlation between the dependent and independent variables. All tolerance values were >0.1, and the VIF value was <10, which indicated that no data had multicollinearity (29). Regression coefficient estimates (β), standard error (SE) of β, 95% confidence intervals (CIs) of β, and P-values were also analyzed. P < 0.05 was considered to indicate statistical significance.
A total of 211 participants answered questionnaires in the survey, of which 201 fulfilled the study inclusion criteria, giving an effective response rate of 95.3%. Of the 201 participants (mean age = 33.31 years, SD = 7.12 years), 100% worked on the frontline during the COVID-19 pandemic, 43.3% were between the ages of 30 and 39, 74.6% were women, 58.2% were married, and 82.1% had a bachelor’s degree or lower. In terms of professionally, 63.2% were registered nurses, 55.2% held a primary professional title, 47.8% of healthcare workers were affiliated with the suspected case isolation ward unit, and 73.6% worked on the frontline for 7–28 days. The socio-demographic and clinical characteristics of the participants are presented in Table 1.
Among 201 FHW, the mean scores of SAS and SDS were 40.98 (SD = 8.20) and 43.30 (SD = 11.38), respectively. A total of 44 (21.9%) participants self-reported depressive symptoms, and 32 (15.9%) participants self-reported anxiety symptoms (Table 1).
In terms of depression and anxiety, the participants were distributed across the three levels of severity. Based on the data of this survey, 44 participants reported depressive symptoms, 32 (72.7%) reported mild depression, 9 (20.5%) reported moderate depression, and 3 (6.8%) reported severe depression. Of 32 participants with anxiety symptoms, 29 (90.6%) reported mild anxiety, 2 (6.3%) reported moderate anxiety, and 1 (3.1%) reported severe anxiety (Figure 1).
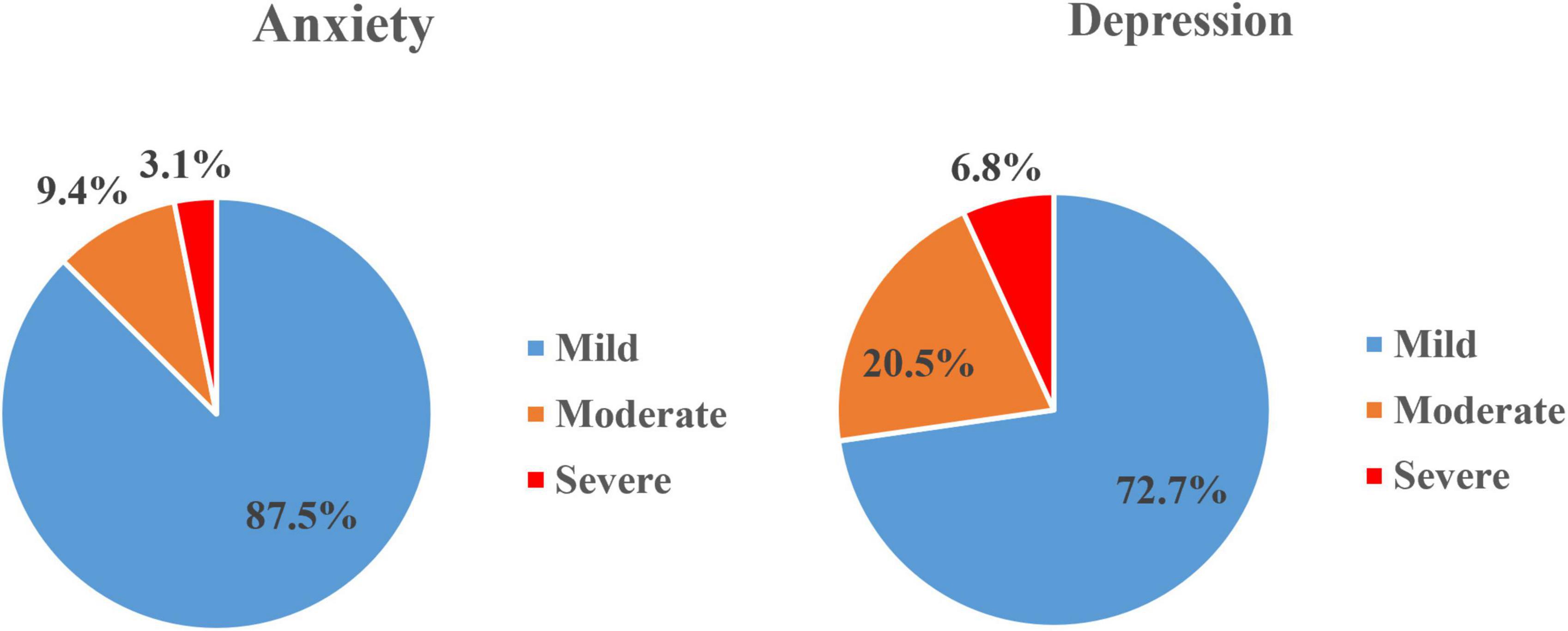
Figure 1. The distribution of levels of severity on depression and anxiety (prevalence of depressive and anxiety symptoms based on a cutoff score of 53 on SDS and 50 on SAS, respectively. Of 201 participants, 44 participants self-reported with mild-severe depressive symptoms and 32 participants self-reported with mild-severe anxiety symptoms).
The average scores of SSRS, subjective support, objective support, and support utilization were 37.17 (SD = 7.54), 20.20 (SD = 3.97), 9.41 (SD = 3.47), and 7.56 (SD = 2.02), respectively. Shapiro–Wilk test showed that the total SSRS score and three subscales scores of the SSRS were normally distributed (P > 0.05). The one-sample mean test showed that the total SSRS score and three subscales scores of the SSRS among FHW were lower than that of the norms of the Chinese general population (30), respectively (P < 0.01) (Table 2).
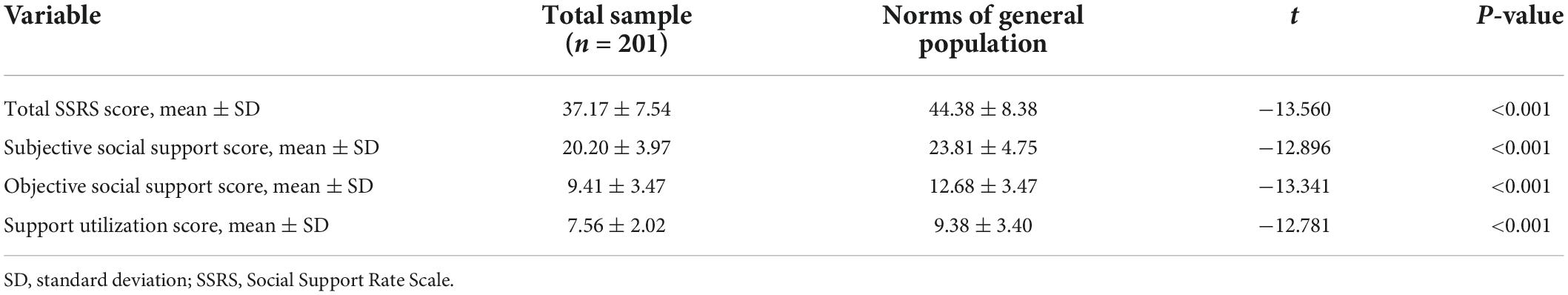
Table 2. The difference of social support scores among frontline healthcare workers and the norms of Chinese general population.
One-way analysis of variance showed no significant difference in the effect of demographic factors on depressive and anxiety symptoms (Table 3). However, a one-way analysis of variance showed that FHW within the age of 30–39 years old had a higher SSRS score compared with the younger FHW (39.22 ± 7.45 versus 34.62 ± 6.93, P < 0.01). Moreover, the total SSRS score of married FHW was higher than that of unmarried FHW (39.92 ± 6.73 versus 33.33 ± 6.93, P < 0.01). Compared with FHW with primary titles, FHW with senior titles had a lower total SSRS score (39.34 ± 7.34 versus 35.64 ± 7.72, P = 0.013), whereas FHW with intermediate titles had a higher total SSRS score than those with senior titles (38.90 ± 6.70 versus 35.64 ± 7.72, P = 0.007) (Table 3).
Multiple linear regression analysis was performed to investigate the association between social support and demographic factors. The regression model was statistically significant [F(5,195) = 11.216, P < 0.001], which suggested that a linear correlation existed between the dependent and independent variables. In this study, all tolerance values were greater than 0.1 (minimum 0.3) and the VIF was less than 10 (maximum 3.5), which indicated that all data had no multicollinearity. Multiple linear regression analysis showed that being married positively affected the SSRS score (β = 7.395, P < 0.01), and age over 40 years old negatively affected the SSRS score (β = −5.349, P = 0.017). Multiple linear regression analysis also showed that age, marital status, and seniority were associated with social support, which explained 20.3% of all variance (Table 4).
Spearman correlation test showed that the total SSRS score, subjective social support score, objective social support score, and support utilization score among FHW were all negatively correlated with the SAS score and SDS score (P < 0.05) (Table 5). Multiple linear regression analysis suggested that a lower support utilization score was respectively significantly associated with high anxiety and depressive symptoms (β = −0.869, P = 0.024; β = −1.088, P = 0.035, respectively). Multiple linear regression analysis also showed that the total SSRS score, objective social support score, and support utilization score were associated with anxiety and depressive symptoms, which explained 8.9 and 14.9% of all variance, respectively (Tables 6, 7).
To the best of our knowledge, this is the first study to investigate the relationship between the levels of social support and the prevalence of depression and anxiety among FHW during the COVID-19 pandemic in China. FHW are the direct providers of hospital services and the main force in controlling COVID-19. Understanding their level of social support and the relationship between psychological impact and social support can help Chinese hospital management and health policymakers take effective measures to further improve the mental health well-being of FHW, thus improving their professional performance and work efficiency.
This study showed that during the COVID-19 pandemic, the prevalence of depressive and anxiety symptoms among FHW was 21.9 and 15.9%, respectively. However, using the same measurement as in our study, the prevalence of depressive and anxiety symptoms among FHW in the early stages of the COVID-19 pandemic was 35.8 and 22.4% (31), respectively, which was significantly higher than the population surveyed in our study. This is most likely associated with the deployment of psychological assistance services by the Chinese government. On 26 January 2020, the Ministry of Health of the Chinese Government issued a guideline for emergency psychological crisis intervention and counseling (32). On 2 February 2020, the state council of China set up a nationwide psychological assistance hotline to help people suffering from psychological disorders due to the epidemic (33). These programs are not only for patients with COVID-19 and the general public but also for all healthcare workers. Participants in this study received psychological assistance services before submitting questionnaires, which can reduce the prevalence of depression and anxiety.
Our findings showed that no significant difference was found in the effect of demographic factors (such as age, gender, seniority, and education level) on depression and anxiety symptoms. The main reasons can be related to the small sample size of this study and the relatively low proportion of FHW with depression and anxiety. Many FHW experiencing symptoms of anxiety and depression had mild degrees of depression and anxiety in our study. Among all the participants, only 12 (27.3%) had moderate and severe depression, and 3 (9.4%) had moderate and severe anxiety. A previous study reported that the anxiety levels in health workers did not vary significantly with age, education, and marital status (34). However, a recent meta-analysis revealed the prevalence of anxiety and depression was higher among females and nursing staff than among males and doctors during the COVID-19 pandemic (3). Nurses, FHW, female, young, and intermediate seniority were associated with a severe degree of depression and anxiety (6, 35). Furthermore, a significant causal relationship was found between depression and age and working on the frontline (36). Another study reported that working in an isolation ward or fever clinic was an independent risk factor for depression and anxiety among frontline pediatric nurses, whereas age and education level did not have any significant effect on depression and anxiety (37). The effect of demographic factors on depression and anxiety is controversial and more rigorously designed studies are required to further clarify this issue.
Our study revealed that the total SSRS score of FHW was significantly lower than that of the general population. The three dimensions of social support (namely subjective social support, objective social support, and support utilization) of FHW were all significantly lower than the Chinese general population. In SSRS, subjective social support refers to the support received from family, friends, and colleagues. During the COVID-19 pandemic, the government-imposed quarantine policies and increased workloads limited the time that FHW could spend with family members and friends. Objective support refers to any type of visible or actual social support, especially economic assistance, received from any source, including the government, non-governmental organizations, religious groups, and local communities (38). The low social status of healthcare workers in China can limit their access to objective social support beyond family members (39). The lockdown policies imposed by the government can also limit their participation in community activities, which made it difficult for them to obtain community help. Support utilization refers to the degree of willingness to seek social support. Fear of stigma can make FHW reluctant to seek outside support (40). Moreover, excessive workloads and minimal vacations can also lead to extreme fatigue for FHW, which can limit their willingness to join in social interactions during breaks (41).
We also found a negative correlation between the levels of social support and the severity of depressive and anxiety symptoms. The participants in our study who reported higher levels of social support were less likely to have symptoms of depression and anxiety, which indicated that social support is an important protective factor for the mental health of FHW. This was consistent with the results from previous studies (42, 43).
Subjective social support reflects the personal experience and feelings of social support (44). People with higher subjective social support score indicates that they receive adequate support, understanding, and respect from their family, friends, and colleagues. High subjective social support can help individuals to reduce loneliness and build a positive self-image, self-efficacy, and self-esteem, thus bringing more understanding, respect, courage, and professional achievements to themselves (45), which has a positive effect on reducing depression and anxiety of FHW.
Objective social support emphasizes the existence of visible social support (46). Those who scored higher on objective social support indicated that they received more visible help and support from the government, local communities, and non-governmental organizations. It also means they have extensive social networks. A high level of objective social support helps individuals to reduce the stress in work and life, and maintain good mental health, which can decrease the depressive and anxiety symptoms in FHW. Moreover, a wide social network can decrease the perceived threat of stressful events among FHW and reduce the physical reactions induced by stress, which also has a positive effect on reducing anxiety and depressive symptoms (47).
High social support utilization indicates a greater willingness to seek social support. This usually manifests as an emotional outpouring to family or friends or seeking help by participating in activities organized by the local community or religious groups. In our study, the higher the social support utilization of FHW, the less likely they were to have symptoms of depression and anxiety. This is consistent with the finding that a better connection with others can mitigate the harmful effects of stressful life events (48).
In the present study, the level of social support for FHW positively correlated with age. One possible reason could be that healthcare workers over 30 years are more likely to have experienced severe acute respiratory syndrome (SARS) and middle east respiratory syndrome (MERS) outbreaks; therefore, they have more experience in seeking social support in the COVID-19 pandemic (49). Moreover, being older also means they have a wider social network and more access to social support than younger people (less than 30 years old). Individuals who had more social support generally had better mental health than those who had less (50).
Our findings also showed that being single was associated with a low level of social support among FHW. One possible reason is that married healthcare workers have higher quality and wider social networks than single healthcare workers because they can receive additional social support from their spouse and spouse’s family (51). These results are consistent with the study by Jaffar Abbas to some extent (52).
Interestingly, despite previous research showing differences in social support between male and female healthcare workers (17), our study showed that gender does not affect the level of social support. This can be because both male and female healthcare workers have longer working hours during the COVID-19 pandemic. Therefore, they did not have sufficient time to participate in family and social activities to seek social support (53). This may also explain why no difference was found in the social support between nurses and doctors in this study.
The results of this study showed that the department where FHW work and how long they worked on the frontline did not affect their social support because FHW feel so exhausted during the COVID-19 pandemic that they were reluctant to seek social support through social and family activities (54).
Previous studies have reported that healthcare workers with high education levels and seniority will receive more social support from patients and the social environment because of their high professional level and rich experience (55). However, the result of the present study showed that education level and seniority do not affect the social support of FHW. Further study is required to explain this phenomenon.
Based on our findings, during COVID-19 pandemic, policy makers should: (1) reduce the working hours and workload of FHW and give them more time to participate in social and family activities; (2) pay more attention to the mental health of unmarried and young FHW and extend more help to alleviate the symptoms of depression and anxiety.
This study has several limitations. First, this study used self-report measures, hence there was a risk of information bias. Second, our study was a cross-sectional study that limited our ability to make statements on causality. In the absence of further follow-up studies, caution should be exercised regarding causality. Third, the income level and religious belief of FHW were not considered in this study, which has a certain relationship with social support. Further prospective and longitudinal studies with a large sample size are needed to assess the impact of social support levels on the mental health in the context of COVID-19 pandemic.
In this study, we showed that 21.9 and 15.9% of FHW had depressive and anxiety symptoms, respectively. There was lower social support among FHW in comparison to the Chinese general population during the COVID-19 pandemic. The marital status and age had a major effect on social support. Social support was inversely associated with depression and anxiety. These findings signify that social support plays an important role in mental health, and health policymakers should pay more attention to the psychological status of FHW. Efforts should also be made to address their low level of social support, to reduce adverse psychological outcomes among FHW. More studies are required to determine how to improve the level of social support and mental health condition of FHW facing public health emergencies in the future.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of Guangdong Provincial Hospital of Chinese Medicine (No. ZE2020-036). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
JZ and LL designed the study. JZ, LZ, and HC were responsible for the development and distribution of questionnaire. XY and XW were responsible for data auditing and data cleaning. JZ, CC, and LL analyzed and interpreted the data. CC and JZ revised the manuscript on the basis of comments from other authors. All authors have read and approved the final manuscript.
This study was funded by the special project of Science and Technology of Traditional Chinese Medicine of Guangdong Provincial Hospital of Chinese Medicine (No. YN2020QN23), China Postdoctoral Science Foundation (No. 2021M700906), special project of “Lingnan modernization of traditional Chinese medicine” in 2019 Guangdong Provincial R&D Program (No. 2020B1111100008), and the Chinese Medicine Innovation Team Project of the State Administration of Traditional Chinese Medicine. The funders had no influence on study design, data collection and analysis, decision to publish, or preparation of the manuscript.
We would like to thank all participants who have been involved in this study and the Changsha Ranxing Information Technology Co., Ltd. for providing us a platform of electronic questionnaires. Changsha Ranxing Information Technology Co., Ltd. was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication. We also thank MJEditor (www.mjeditor.com) for English language editing.
The authors declare that this study received support from Changsha Ranxing Information Technology Co., Ltd. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. The People’s Government of Tibet Autonomous Region. Tibet Launched A Level I Response to A Major Public Health Emergency. (2020). Available online at: http://www.xizang.gov.cn/xwzx_406/xw_tp/202001/t20200130_131210.html (accessed May 1, 2022).
2. National Health Commission of the People’s Republic of China. The Latest Situation of New Coronavirus Pneumonia By 24:00 on 31 March. (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/202003/ec2689b0e716468fbfff7cf890c74bb7.shtml (accessed May 1, 2022).
3. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
4. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public -A systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
5. National Health Commission of the People’s Republic of China. The Latest Situation of New Coronavirus Pneumonia By 24:00 on 14 February. (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/202002/50994e4df10c49c199ce6db07e196b61.shtml (accessed May 1, 2022).
6. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
7. Carmassi C, Pedrinelli V, Dell’Oste V, Bertelloni CA, Cordone A, Bouanani S, et al. Work and social functioning in frontline healthcare workers during the covid-19 pandemic in Italy: role of acute post-traumatic stress, depressive and anxiety symptoms. Riv Psichiatr. (2021) 56:189–97. doi: 10.1708/3654.36346
8. Carmassi C, Pedrinelli V, Dell’Oste V, Bertelloni CA, Grossi C, Gesi C, et al. PTSD and depression in healthcare workers in the italian epicenter of the COVID-19 outbreak. Clin Pract Epidemiol Ment Health. (2021) 17:242–52. doi: 10.2174/1745017902117010242
9. Carmassi C, Dell’Oste V, Barberi FM, Bertelloni CA, Pedrinelli V, Dell’Osso L. Mental health symptoms among general practitioners facing the acute phase of the COVID-19 pandemic: detecting different reaction groups. Int J Environ Res Public Health. (2022) 19:4007. doi: 10.3390/ijerph19074007
10. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian J Psychiatr. (2020) 51:102119. doi: 10.1016/j.ajp.2020.102119
11. Finfgeld-Connett D. Clarification of social support. J Nurs Scholarsh. (2015) 37:4–9. doi: 10.1111/j.1547-5069.2005.00004.x
12. Sarason BR, Pierce GR, Shearin EN, Sarason IG. Perceived social support and working models of self and actual others. J Pers Soc Psychol. (1991) 60:273–87.
13. Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry. (2007) 4:35–40.
14. Lau EYH, Chan KKS, Lam CB. Social support and adjustment outcomes of first-year university students in Hong Kong: self-esteem as a mediator. J Coll Stud Dev. (2018) 59:129–34.
15. Tomioka K, Morita N, Saeki K, Okamoto N, Kurumatani N. Working hours, occupational stress and depression among physicians. Occup Med. (2011) 61:163–70. doi: 10.1093/occmed/kqr004
16. Song J, Cheng TC. How do gender differences in family responsibilities affect doctors’ labour supply? Evidence from Australian panel data. Soc Sci Med. (2020) 265:113475. doi: 10.1016/j.socscimed.2020.113475
17. Fu C, Wang G, Shi X, Cao F. Social support and depressive symptoms among physicians in tertiary hospitals in China: a cross-sectional study. BMC Psychiatry. (2021) 21:217. doi: 10.1186/s12888-021-03219-w
18. Sun J, Sun R, Jiang Y, Chen X, Li Z, Ma Z, et al. The relationship between psychological health and social support: evidence from physicians in China. PLoS One. (2020) 15:e0228152. doi: 10.1371/journal.pone.0228152
19. Zhu W, Wei Y, Meng X, Li J. The mediation effects of coping style on the relationship between social support and anxiety in Chinese medical staff during COVID-19. BMC Health Serv Res. (2020) 20:1007. doi: 10.1186/s12913-020-05871-6
20. Ni MY, Yang L, Leung CMC, Li N, Yao XI, Wang Y. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment Health. (2020) 7:e19009. doi: 10.2196/19009
21. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
22. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
23. Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. (2020) 133:110102. doi: 10.1016/j.jpsychores.2020.110102
24. Zung WW, Magruder-Habib K, Velez R, Alling W. The comorbidity of anxiety and depression in general medical patients: a longitudinal study. J Clin Psychiatry. (1990) 51:77–80.
25. Hu HH, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Hum Hypertens. (2015) 29:198–203. doi: 10.1038/jhh.2014.58
26. Xiao SY. Theoretical basis and application in research of Social Support Rating Scale. J Clin Psychiatry. (1994) 4:98–100. doi: 10.1186/s12913-016-1423-5
27. Dai W, Chen L, Tan H, Wang J, Lai Z, Kaminga AC, et al. Association between social support and recovery from post-traumatic stress disorder after flood: a 13-14 year follow-up study in Hunan, China. BMC Public Health. (2016) 16:194. doi: 10.1186/s12889-016-2871-x
28. Wang XD, Wang XL, Ma H. Manual of Mental Health Rating Scale. Beijing: China Mental Health Magazine (1999). p. 82–122.
29. Yang WC, Lin CH, Wang FC, Lu MJ. Factors related to the improvement in quality of life for depressed inpatients treated with fluoxetine. BMC Psychiatry. (2017) 17:309. doi: 10.1186/s12888-017-1471-3
30. Zhang MY. Psychiatric Rating Scale Manual. 2nd ed. Changsha: Hunan Science and Technology Press (1993). p. 35–42.
31. Guo JM, Liao LM, Wang BG, Li XQ, Guo LR, Tong Z, et al. Psychological effects of COVID-19 on hospital staff: a national cross-sectional survey in mainland China. Vasc Invest Ther. (2021) 4:6–11.
32. The Ministry of Health of China. A Notification on the Issuance of Guidelines for Emergency Psychological Crisis Intervention in Novel Coronavirus Outbreaks of Pneumonia. (2020). Available online at: http://www.gov.cn/xinwen/2020-01/27/content_5472433.htm (accessed May 1, 2022).
33. The State Council of China. A Notification to Set Up Nationwide Psychological Assistance Hotlines Against the 2019-nCoV Outbreak. (2020). Available online at: http://www.gov.cn/xinwen/2020-02/02/content_5473937.htm (accessed May 1, 2022).
34. Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. (2020) 148:e98. doi: 10.1017/S0950268820001107
35. Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. (2020) 290:113130. doi: 10.1016/j.psychres.2020.113130
36. Şahin MK, Aker S, Şahin G, Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J Community Health. (2020) 45:1168–77. doi: 10.1007/s10900-020-00921-w
37. Zheng R, Zhou Y, Qiu M, Yan Y, Yue J, Yu L, et al. Prevalence and associated factors of depression, anxiety, and stress among Hubei pediatric nurses during COVID-19 pandemic. Compr Psychiatry. (2021) 104:152217. doi: 10.1016/j.comppsych.2020.152217
38. Viseu J, Leal R, de Jesus SN, Pinto P, Pechorro P, Greenglass E. Relationship between economic stress factors and stress, anxiety, and depression: moderating role of social support. Psychiatry Res. (2018) 268:102–7. doi: 10.1016/j.psychres.2018.07.008
39. Wu SJ, Qiu S, Liao HC. Theory of the domestic doctor the influence of the social status of people in the health industry. J Med Theory Pract. (2015) 28:2269–71. doi: 10.19381/j.issn.1001-7585.2015.16.095
40. Lin CY, Peng YC, Wu YH, Chang J, Chan CH, Yang DY. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. (2007) 24:12–7. doi: 10.1136/emj.2006.035089
41. Watson AG, McCoy JV, Mathew J, Gundersen DA, Eisenstein RM. Impact of physician workload on burnout in the emergency department. Psychol Health Med. (2019) 24:414–28. doi: 10.1080/13548506.2018.1539236
42. Guntzviller LM, Williamson LD, Ratcliff CL. Stress, social support, and mental health among young adult hispanics. Fam Community Health. (2020) 43:82–91. doi: 10.1097/FCH.0000000000000224
43. Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. (2021) 16:e0247679. doi: 10.1371/journal.pone.0247679
44. Gyasi RM, Phillips DR, Abass K. Social support networks and psychological wellbeing in community-dwelling older Ghanaian cohorts. Int Psychogeriatr. (2018) 31:1047–1057. doi: 10.1017/S1041610218001539
45. Feng D, Su S, Wang L, Liu F. The protective role of self-esteem, perceived social support and job satisfaction against psychological distress among Chinese nurses. J Nurs Manag. (2018) 26:366–72. doi: 10.1111/jonm.12523
46. Cao M, Kan J. Influence of social support on career identification in nurses. Nurs Res. (2020) 24:380–1.
47. Gu Y, Hu J, Hu Y, Wang J. Social supports and mental health: a cross-sectional study on the correlation of self-consistency and congruence in China. BMC Health Serv Res. (2016) 16:207. doi: 10.1186/s12913-016-1463-x
48. Wilkinson A, Bowen L, Gustavsson E, Håkansson S, Littleton N, McCormick J, et al. Maintenance and development of social connection by people with long-term conditions: a qualitative study. Int J Environ Res Public Health. (2019) 16:1875. doi: 10.3390/ijerph16111875
50. Baek RN, Tanenbaum ML, Gonzalez JS. Diabetes burden and diabetes distress: the buffering effect of social support. Ann Behav Med. (2014) 48:145–55. doi: 10.1007/s12160-013-9585
51. Cairney J, Boyle M, Offord DR, Racine Y. Stress, social support and depression in single and married mothers. Soc Psychiatry Psychiatr Epidemiol. (2003) 38:442–9. doi: 10.1007/s00127-003-0661-0
52. Abbas J, Aqeel M, Abbas J, Shaher BAJ, Sundas J, Zhang W. The moderating role of social support for marital adjustment, depression, anxiety, and stress: evidence from Pakistani working and nonworking women. J Affect Disord. (2019) 244:231–8. doi: 10.1016/j.jad.2018.07.071
53. Usman N, Mamun M, Ullah I. COVID-19 infection risk in pakistani health-care workers: the cost-effective safety measures for developing countries. Soc Health Behav. (2020) 3:75–7.
54. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. (2018) 320:1131–50. doi: 10.1001/jama.2018.12777
Keywords: depression, anxiety, social support, COVID-19, frontline healthcare workers
Citation: Zhan J, Chen C, Yan X, Wei X, Zhan L, Chen H and Lu L (2022) Relationship between social support, anxiety, and depression among frontline healthcare workers in China during COVID-19 pandemic. Front. Psychiatry 13:947945. doi: 10.3389/fpsyt.2022.947945
Received: 19 May 2022; Accepted: 23 August 2022;
Published: 14 September 2022.
Edited by:
Vsevolod Konstantinov, Penza State University, RussiaReviewed by:
Virginia Pedrinelli, University of Pisa, ItalyCopyright © 2022 Zhan, Chen, Yan, Wei, Zhan, Chen and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liming Lu, bHVsaW1pbmdsZW9uQDEyNi5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.