
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 05 July 2022
Sec. Aging Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.944154
This article is part of the Research TopicEpidemiology and Clinical Researches on Neuropsychiatric Disorders in AgingView all 10 articles
Background: The relationship between diet and psychological disorders in older adults has attracted considerable attention as the global trend of aging. This study examines the relationship between Dietary inflammatory index (DII) and the risk of depression and suicide in older adults using the National Health and Nutrition Examination Survey (NHANES) as a large cross-sectional study.
Methods: The data were extracted from NHANES from 2005 to 2018, and cross-sectional studies were conducted on older adults (age ≥ 60 years). According to their median DII, participants were classified into High-DII (DII ≥ 1.23) and Low-DII (DII < 1.23) groups. Depression was the primary outcome, and suicidal ideation was a secondary outcome. Utilizing multi-factor logistic regression to correlate DII with outcomes.
Results: There were 10,956 elderly participants included in the analysis. In comparison to Low-DII group, High-DII group exhibited a higher rate of depression (8.9% vs. 6.7%; P < 0.001) and higher ideation to commit suicide (3.7% vs. 3.0%; P = 0.039). Moreover, in terms of gender ratio, men accounted for 44% of the High-DII group, which was significantly lower than 56.2% of the Low-DII group (P < 0.001). Furthermore, logistic regression revealed that High-DII group had a higher risk of depression in the previous 2 weeks (OR = 1.358, 95% CI: 1.180–1.564; P < 0.001) and a higher risk of suicidal ideation (OR = 1.244, 95% CI: 1.010–1.532; P = 0.040). Additionally, after adjusting for demographic covariates such as age, gender and race, High-DII group still had a higher risk of depression (OR = 1.293, 95% CI: 1.121–1.493; P < 0.001) and suicidal ideation (OR = 1.261, 95% CI: 1.021–1.55; P = 0.031). Furthermore, after adjusting for various covariates like demographic, social factors, and comorbidities, the High-DII group remained at higher risk for depression (OR = 1.178, 95% CI: 1.019–1.363; P = 0.027), and the risk of comorbid suicidal ideation remained high (OR = 1.136, 95% CI: 0.917–1.408), but the difference was not significant (P = 0.243).
Conclusion: In older adults, high levels of DII are associated with depression and suicidal ideation. Multiple factors affect the mental health of older adults, and it is unknown to what extent a pro-inflammatory diet contributes to depression and suicidal thoughts in older adults. Nonetheless, daily dietary management in older adults should be emphasized.
The mental health of the elderly is gradually becoming a critical global public health issue as the global aging trend develops. As of 2013, nearly 10% of the world’s population (approximately 615 million) suffers from a psychiatric disorder, with more than 20% of the older population over the age of 60 suffering from a psychiatric disorder, of which depression is one of the most common (1). Many factors, including widowhood, living alone, reduced intergenerational communication, declining physical function, and various chronic diseases, are increasing the elderly’s mental health risks, seriously impacting their daily lives, and lowering their quality of life in their later years (2, 3). The most frequent mental illness in the elderly is depression (4). Research conducted in Germany (5). According to a population-based survey, it is reported that 28.7% of older adults had depressive symptoms, among them, 6.6% were severe depression, and the older the person, the higher the prevalence of depressive symptoms. Another study (6) conducted in Greece found that 34.4% of older adults had impaired cognitive functions, and 32.3% experienced depressive symptoms. In addition, a large cross-sectional study (7) from China indicated that the prevalence of somatic symptom disorders in older adults was 63.2%, significantly higher than in the non-elderly population (45.3%); similarly, the risk of depression or anxiety was 3.7 times that of the general population. Furthermore, patients with chronic depressive symptoms are prone to suicidal thoughts, with up to 15% of depressed patients reportedly preferring suicide ideation (8).
There is research evidence that depression is significantly associated with chronic systemic inflammation (9). Chronic inflammation can mediate a permanent reorganization of inflammatory neurotransmitter pathways, resulting in the transition from acute to chronic pain and promoting depression, anxiety, and sleep disturbances (10–12). The association between diet and chronic systemic inflammation is quite close, and an inappropriate dietary structure or pattern is a significant source of chronic systemic inflammation in the organism (13). Dietary inflammatory index (DII) is a novel tool for assessing the subversive potential of the diet and the amount of pro-inflammatory food components in an individual’s dietary composition (14). DII is strongly associated with mental illness, compared to controls, patients with schizophrenia appeared to have higher DII scores (1.99 ± 1.39 vs. 1.60 ± 1.38; P = 0.009), and each unit increase in DII score was associated with a 62% increase in the odds of developing schizophrenia (OR = 1.62; 95% CI 1.17–2.26) (14). Chronic systemic inflammation can significantly increase with high levels of DII (15). Several studies (16, 17) have found that pro-inflammatory dietary patterns are significantly associated with an elevated risk of depression in adults, as high levels of DII increase the risk of depressive symptoms. Nonetheless, these studies have been limited to specialized populations, like medical personnel. However, these were only single-center studies on specific people, such as medical personnel (18). Furthermore, the relationship between suicide and DII has not been clarified.
There is a scarcity of direct and robust evidence between DII to an increased risk of depression and suicide in the elderly population. Data from large-scale demographic surveys are still required, given the potential economic burden and adverse effects of psychological disorders in older adults on an individual and societal level and the guiding significance of a rational daily dietary pattern. It is essential to investigate the relationship between psychological disorders and nutritional habits in the elderly, emphasizing daily dietary interventions.
The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional survey conducted by the National Center for Health Statistics and the Centers for Disease Control and Prevention, utilizing data from a nationally representative sample of the U.S. civilian population. This study’s dataset was constructed using NHANES public data files from 2005 to 2018, and the study population comprised all NHANES respondents.
The key exposure variable in this study was DII, and the types and amounts of food and beverages consumed by the participants in 24 h were extracted. As documented in the literature (19), DII was calculated and briefly explained as follows: DII for each nutrient or dietary ingredient = [(daily intake of that nutrient or dietary ingredient - global per capita daily intake of that nutrient or dietary ingredient)/that nutrient or dietary ingredient Standard deviation of global per capita daily intake] × inflammatory effect index of that nutrient or dietary ingredient, and the sum of DII of each nutrient or dietary ingredient was the total DII score of individual study subjects (see Supplementary Table 1 for specific nutrients and their inflammation indexes). According to the median DII of all included subjects, the participating population was classified into a High-DII group (DII ≥ median) and a Low-DII group (DII < median).
This study’s primary outcome was depression. NHANES questionnaire yielded Patient Health Questionnaire-9 (PHQ-9) data. They consisted of nine clinical depression symptom items for the past 2 weeks, with scores ranging from zero to three for each item, with zero indicating no symptoms during the period, one suggesting a few days of symptoms, two showing more than half of the days with symptoms, and three describing symptoms almost every day. The cumulative PHQ-9 score was used to determine the presence and severity of clinical depressive symptoms in the previous 2 weeks. According to prior studies (20), when the total PHQ-9 score = 10, there was good sensitivity and specificity for major depression. Therefore, the study participant population with PHQ-9 < 10 was considered non-depressed patients and PHQ-9 ≥ 10 as depressed patients.
Even though the proportion of elderly suicides is relatively low compared to depressive symptoms, it is important to focus on the study of suicidal ideation in the elderly, considering that suicide is mainly secondary to severe depressive symptoms and the heavy burden on society. Consequently, suicidal ideations were chosen as the secondary outcome in this study, and item nine of the PHQ-9 (Scoring rules are in Supplementary Table 2) explicitly asked respondents if they had had suicidal thoughts in the past 2 weeks, which was demonstrated to be a valid predictor of future attempted or completed suicide (21).
Covariates were chosen to influence depression-related factors that have previously been reported. Age, gender, and race, for example, were included as demographic characteristics. Social factors include education level, marital status, household income up to the poverty level, health insurance coverage, and data on everyday health-related behaviors such as smoking and alcohol consumption. In addition, medical comorbidity variables such as Body mass index (BMI), diabetes, and cancer were collected.
Quantitative data were examined using the t-test or Analysis of Variance, and data for categorical variables were analyzed using the χ2 test for differences in cohort characteristics between exposure groups. The preliminary analysis employed multi-factor logistic regression to determine the relationship between the exposure group and the outcome variable. All descriptive studies were assessed for significance using two-sided tests at the P < 0.05 level of energy. Eventually, a Generalized additive model was employed to test for non-linear relationships between the outcome variables and exposure factors. All data analyses were performed utilizing Empower Stats software1 (X&Y solutions, Inc., Boston MA, United States) and R.3.5.2.2
First, initial survey data were obtained from 70,190 participants. After eliminating individuals who lacked outcome, exposure, or covariate data (with the exceptions noted above), the analysis included 10,956 older participants (Figure 1).
All elderly subjects’ median DII was calculated to be 1.23. As a result, the subjects were classified into the High-DII group (DII ≥ 1.23) and Low-DII group (DII < 1.23), with 5,478 participants in each group. Table 1 depicts the distribution of cohort characteristics stratified by DII level. In the preliminary analysis, the average age of participants in the High DII group was (70.0 ± 7.0) years, whereas the average age of participants in the Low-DII group was (69.9 ± 7.0) years. There was no statistically significant difference between the groups (P > 0.05). Furthermore, regarding gender ratio, males accounted for 44% of the High-DII group, significantly lower than 56.2% of the Low-DII group (P < 0.001), indicating that men tend to have a lower DII. Similarly, in terms of social factors, the High-DII group had a higher proportion ratio of family income to poverty ≤ 2.9,” “Married or living with a partner,” and “Never married” compared to the Low-DII group (P < 0.05). Furthermore, the differences in BMI, hypertension, diabetes and tumor history were statistically significant (P < 0.05).
The High-DII group had 487 (8.9%) participants with comorbid depression and 205 (3.7%) with comorbid suicidal ideation, while the Low-DII group had 367 (6.7%) participants with comorbid depression and 166 (3.0%) with comorbid suicidal ideation. Therefore, depression and suicidal ideation were higher in the High-DII group than in the Low-DII group, and the differences were statistically significant (P < 0.05).
As indicated in Table 2, in an unadjusted multivariate logistic regression analysis, high DII was an independent risk factor for depression (OR = 1.358, 95% CI: 1.180–1.564; P < 0.001) and suicidal ideation (OR = 1.244, 95% CI: 1.010–1.532; P = 0.040) in the previous 2 weeks. After adjusting for demographic covariates like age, sex, and race, high DII was still associated with a higher risk of depression (OR = 1.293, 95% CI: 1.121–1.493; P < 0.001) and suicidal ideation (OR = 1.261, 95% CI: 1.021–1.55; P = 0.031). In addition, after adjusting for various covariates like demographic, social factors, and comorbidities, high DII remained an independent risk factor for depression (OR = 1.178, 95% CI: 1.019–1.363; P = 0.027). However, it was not a risk factor for suicidal ideation (OR = 1.136, 95% CI: 0.917–1.408; P = 0.243).
Moreover, subgroup logistic regression analyses by gender revealed that women with high DII were more likely to have comorbid suicidal ideation (OR = 1.355, 95% CI: 1.004–1.829; P = 0.047), while men were not (Table 3).

Table 3. Subgroup multi-factor logistic regression analysis for the association between DII high-level and outcomes.
Figure 2 depicts the dose-response relationship between DII and outcome indicators. DII was positively associated with the risk of depressive symptoms, and the overall risk of depression in older adults tended to increase progressively with increasing DII (Figure 2A). Similarly, the relationship between DII and the risk of comorbid suicidal ideation also increased progressively with DII levels (Figure 2B).
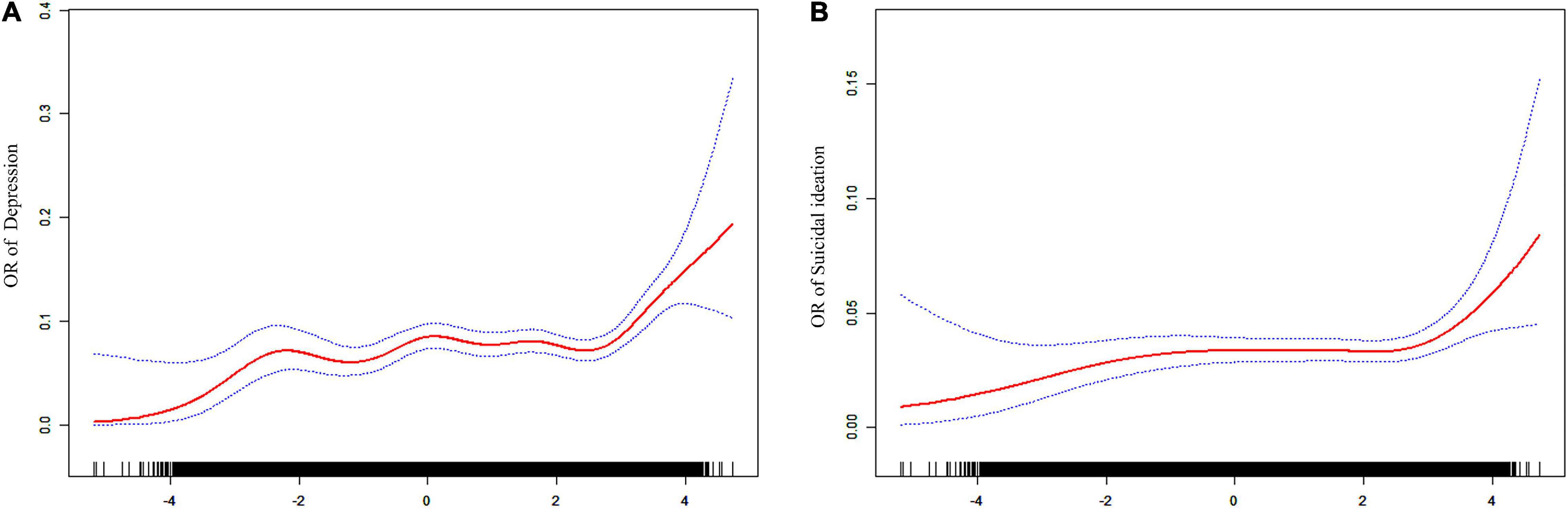
Figure 2. Dose-response association between (A,B) OR of depression and suicidal ideation and DII (adjusted for age, sex, race, smoker, alcohol user, glucocorticoid user, hypertension, cancer, and diabetes).
Using a nationally representative cross-sectional study of older adults, this study demonstrated a significant relationship between high levels of DII and depression in older adults and a relationship with suicidal ideation in the past 2 weeks.
These outcomes are consistent with earlier studies (16) on the relationship between diet and depression; a high intake of pro-inflammatory foods significantly increases the risk of depressive symptoms. Those at the highest risk for depression had significantly lower consumption of meat, fish, and eggs, higher consumption of added sugars, and relatively lower consumption of fruits, vegetables, and fiber (16, 18). Furthermore, a study of medical personnel (18) found a significant positive correlation between high PHQ-9 scores and high DII levels when gender, psychiatric diagnosis, physical activity, and mental exercise were all taken into account (P < 0.01). Another study (22) of residential female undergraduates discovered that higher DII was significantly associated with an increased likelihood of stress symptoms (OR = 1.41, 95% CI: 1.12–1.77; P = 0.003) and anxiety symptoms (OR = 1.35, 95% CI: 1.07–1.69; P = 0.01). The relationship between dietary patterns and depression remains significant, and strong epidemiological evidence proposes that poor diet may hurt mental health disorders (23). However, after adjusting for marriage, education, and family poverty to income ratios, the significance of DII concerning the risk of suicide in older patients decreased significantly. Diet may have a lesser impact on suicidal ideation than social factors. Indeed, according to earlier surveys, unhappy marriages, inadequate education, and economic poverty are significant social factors contributing to older adults’ suicide (24, 25).
Furthermore, our gender stratification results indicate that both men and women in the High-DII group are at higher risk of developing depression than those in the Low-DII group. Women with high DII are more likely to experience suicidal ideation. The differential results for suicidal ideation may be driven primarily by the female population. Although women generally have lower rates of committing suicide than men, they have higher suicidal ideation and attempt rates, especially in women over the age of 75 (26). This could be related to the unstable nature of the female elderly, who are emotional in situations and have weak resistance to stress and a relative lack of social support. When confronted with unexpected situations, they are more prone to depression and anxiety symptoms (27, 28).
In short, the relationship between diet and mental health is complicated. Even though our observational studies reveal that high levels of DII may be related to depressive mood and suicidal ideation, there are many biological, psychological and social factors involved. As the global trend of population aging develops, numerous aspects of demographic changes increase socioeconomic pressures, and declining somatic functionality further complicates the discussion linked to mental health in the elderly population. The previous study has focused on the association between social factors and mental health in older adults.
However, there are some limitations of the present work. First, it is difficult to elaborate on the causal relationship between an inflammatory diet and depression/suicide in the present cross-sectional study. Because the NHANES study collected data at a single time point, nutritional data were recorded only once for all participants, and PHQ-9 scores, as well as suicidal ideation questionnaires, were measured only once, which resulted in some possible bias in DII scores and PHQ-9 scores. In addition, this study may also have overlooked some relevant factors that influence depression/suicidal ideation in older adults, such as the presence of major life changes, chronic pain, family atmosphere, etc. Therefore, in the future, we need to conduct a multicenter longitudinal clinical trial to confirm our findings, dynamically assess changes in each of the factors that may influence depression/suicidal ideation in older adults, and conduct a long follow-up to investigate how inflammatory diet specifically affects the onset and progression of depression in older adults.
Nonetheless, studies of dietary patterns and cognitive problems in older adults are scarce and primarily single-centered with small sample sizes. As our understanding of the factors influencing mental health in the elderly population improves, we should carefully evaluate dietary patterns’ long-term benefits and harms to mental disease in future studies and develop appropriate nutritional patterns for the elderly.
By analyzing a nationally representative sample, we discovered that high levels of DII were related to moderate to severe clinical depression and suicidal ideation in older adults. This relationship is complicated, and further studies are required to understand it fully. However, the extent to which a pro-inflammatory diet leads to significant depressive symptoms and suicidal ideation is complicated and requires further research to demonstrate this relationship.
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
Before being interviewed or examined, all survey participants provided informed consent, and the NCHS Ethics Review Board approved the data collection protocol.
YX and WH carried out the acquisition and interpretation of data and was the major contributor to drafting the manuscript and participated in drawing tables and diagrams. YX carried out the clinical data collection and analysis. WH contributed to the ideas of the article and reviewed the manuscript. Both authors provided final approval for publishing the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.944154/full#supplementary-material
Supplementary Table 1 | Forty five nutrients included in DII calculation.
Supplementary Table 2 | PHQ-9 score.
DII, dietary inflammatory index; NHANES, National Health and Nutrition Examination Survey; PHQ-9, patient health questionnaire-9; BMI, body mass index.
1. Liu W, Han G, Yan X, Zhang X, Ning G, Akhmedov A, et al. The impact of mental health status on health consumption of the elderly in China. Int J Environ Res Public Health. (2021) 18:6622. doi: 10.3390/ijerph18126622
2. Xie Y, Ma M, Wu W, Zhang Y, Zhang Y, Tan X. Dose-response relationship between intergenerational contact frequency and depressive symptoms amongst elderly Chinese parents: a cross-sectional study. BMC Geriatrics. (2020) 20:349. doi: 10.1186/s12877-020-01751-0
3. Yadav U, Thapa T, Mistry S, Pokhrel R, Harris M. Socio-demographic characteristics, lifestyle factors, multi-morbid conditions, and depressive symptoms among Nepalese older adults. BMC Psychiatry. (2020) 20:261. doi: 10.1186/s12888-020-02680-3
5. Glaesmer H, Riedel-Heller S, Braehler E, Spangenberg L, Luppa M. Age- and gender-specific prevalence and risk factors for depressive symptoms in the elderly: a population-based study. Int Psychogeriatr. (2011) 23:1294–300. doi: 10.1017/S1041610211000780
6. Mantzorou M, Vadikolias K, Pavlidou E, Serdari A, Vasios G, Tryfonos C, et al. Nutritional status is associated with the degree of cognitive impairment and depressive symptoms in a Greek elderly population. Nutr Neurosci. (2020) 23:201–9. doi: 10.1080/1028415X.2018.1486940
7. Wu Y, Tao Z, Qiao Y, Chai Y, Liu Q, Lu Q, et al. Prevalence and characteristics of somatic symptom disorder in the elderly in a community-based population: a large-scale cross-sectional study in China. BMC Psychiatry. (2022) 22:257. doi: 10.1186/s12888-022-03907-1
8. Lopes R, Meyer B, Berger T, Svacina M. Effectiveness of an internet-based self-guided program to treat depression in a sample of Brazilian users: a study protocol. Braz J Psychiatry. (2020) 42:322–8. doi: 10.1590/1516-4446-2019-0582
9. Bao C, Lv J, Chen J, Wei G, Liu N, Wang Y, et al. Chronic inflammation as a potential mediator between phthalate exposure and depressive symptoms. Ecotoxicol Environ Saf. (2022) 233:113313. doi: 10.1016/j.ecoenv.2022.113313
10. Hu Y, Niu T, Xu J, Peng L, Sun Q, Huang Y, et al. Negative air ion exposure ameliorates depression-like behaviors induced by chronic mild stress in mice. Environ Sci Pollut Res Int. (2022). doi: 10.1007/s11356-022-20144-x [Epub ahead of print].
11. Benatti C, Blom J, Rigillo G, Alboni S, Zizzi F, Torta R, et al. Disease-induced neuroinflammation and depression. CNS Neurol Disord Drug Targets. (2016) 15:414–33. doi: 10.2174/1871527315666160321104749
12. Shulyak A, Gorpynchenko I, Drannik G, Poroshina T, Savchenko V, Nurimanov K. The effectiveness of the combination of rectal electrostimulation and an antidepressant in the treatment of chronic abacterial prostatitis. Cent European J Urol. (2019) 72:66–70. doi: 10.5173/ceju.2018.1719
13. Ahmad TB, Rudd D, Kotiw M, Liu L, Benkendorff K. Correlation between fatty acid profile and anti-inflammatory activity in common Australian seafood by-products. Marine Drugs. (2019) 17:155. doi: 10.3390/md17030155
14. Jahrami H, Faris MA, Ghazzawi HA, Saif Z, Habib L, Shivappa N, et al. Increased dietary inflammatory index is associated with schizophrenia: results of a case–control study from Bahrain. Nutrients. (2019) 11:1867. doi: 10.3390/nu11081867
15. Khan I, Kwon M, Shivappa N, Hébert J, Mi KK. Proinflammatory dietary intake is associated with increased risk of metabolic syndrome and its components: results from the population-based prospective study. Nutrients. (2020) 12:1196. doi: 10.3390/nu12041196
16. Ljungberg T, Bondza E, Lethin C. Evidence of the importance of dietary habits regarding depressive symptoms and depression. Int J Environ Res Public Health. (2020) 17:1616. doi: 10.3390/ijerph17051616
17. Popa T, Ladea M. Nutrition and depression at the forefront of progress. J Med Life. (2012) 5:414–9.
18. Belliveau R, Horton S, Hereford C, Ridpath L, Foster R, Boothe E. Pro-inflammatory diet and depressive symptoms in the healthcare setting. BMC Psychiatry. (2022) 22:125. doi: 10.1186/s12888-022-03771-z
19. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. (2014) 17:1689–96. doi: 10.1017/S1368980013002115
20. Williams JB, Kroenke K, Spitzer RL. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2013) 9:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
21. Rossom RC, Coleman KJ, Ahmedani BK, Beck A, Johnson E, Oliver M, et al. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J Affect Disord. (2017) 215:77–84. doi: 10.1016/j.jad.2017.03.037
22. Wang XY, Fang AP, Chen PY, Liao GC, Zhang YJ, Shivappa N, et al. High dietary inflammatory index scores are associated with an elevated risk of hepatocellular carcinoma in a case–control study. Food Funct. (2018) 9:5832–42. doi: 10.1039/c8fo01190g
23. Ahuja M, Sathiyaseelan T, Wani RJ, Fernandopulle P. Obesity, food insecurity, and depression among females. Arch Public Health. (2020) 78:83. doi: 10.1186/s13690-020-00463-6
24. Lee J, Lee A, Lee D, Jung HY, Lee SI. Suicidal ideation of the elderly according to their involvement in grandchild care. Psychiatry Investig. (2019) 16:625–8. doi: 10.30773/pi.2019.06.06
25. Zhu RT, Ma ZY, Jia CX, Zhou L. Completed suicide with violent and non-violent methods by the elderly in rural china: a psychological autopsy study. Front Psychiatry. (2021) 12:624398. doi: 10.3389/fpsyt.2021.624398
26. Vapa D, Radosavkić R, Lakić T, Maletin M, Stojanović I. Analysis of suicides in the province of vojvodina, republic of serbia, during the 2001-2015 perioD. Acta Clin Croat. (2022) 60:450–6. doi: 10.20471/acc.2021.60.03.16
27. Goodyer IM, Jones PB, Kaur SP, Neufeld SA, Jesmont C, Qiu T, et al. Age and gender effects on non-suicidal self-injury, and their interplay with psychological distress. J Affect Disord. (2022) 306:240–5. doi: 10.1016/j.jad.2022.03.021
28. Otten D, Ernst M, Tibubos AN, Brähler E, Fleischer T, Schomerus G, et al. Does social support prevent suicidal ideation in women and men? Gender-sensitive analyses of an important protective factor within prospective community cohorts. J Affect Disord. (2022) 306:157–66. doi: 10.1016/j.jad.2022.03.031
Keywords: Dietary inflammatory index, depression, suicide ideation, older adults, NHANES
Citation: Xiao Y and Huang W (2022) Association of Dietary Inflammatory Index With Depression and Suicidal Ideation in Older Adult: Results From the National Health and Nutrition Examination Surveys 2005–2018. Front. Psychiatry 13:944154. doi: 10.3389/fpsyt.2022.944154
Received: 14 May 2022; Accepted: 09 June 2022;
Published: 05 July 2022.
Edited by:
Wuxiang Xie, Peking University, ChinaReviewed by:
Guixiong Zhang, The First Affiliated Hospital of Sun Yat-sen University, ChinaCopyright © 2022 Xiao and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Huang, ZGh5eWh1YW5nd2VpQG91dGxvb2suY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.