
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 22 July 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.941198
This article is part of the Research Topic Adaption to Change and Coping Strategies: New Resources for Mental Health View all 29 articles
Introduction: Community-acquired pneumonia (CAP) is an important cause of hospitalization and death in patients with mental disorders. It is critical to understand the risk factors of CAP and determine prevention strategies to reduce CAP. The aim of this study is to explore the characteristics of inpatients with mental disorders who have CAP and analyze the risk factors.
Methods: This retrospective study included 16,934 inpatients with mental disorders who were admitted for the first time to a tertiary general hospital between January 2017 and July 2021 (excluding January 2020–May 2020). Risk factors for CAP were identified by logistic regression analysis after propensity score matching (PSM, 1:4) for age, gender, and BMI.
Results: The CAP rate of inpatients with mental disorders was 1.78%. Inpatients who had CAP had a significantly prolonged hospital stay, and were more often admitted to a closed ward or the ICU. After PSM, the multivariable analysis revealed that clozapine use (OR = 3.212, 95% CI = 1.744–5.915, P < 0.001), schizophrenia spectrum disorder (OR = 2.785, 95% CI = 1.684–4.607, P < 0.001), alcohol consumption (OR = 2.549, 95% CI = 1.586–4.096, P < 0.001), cardiovascular disease (OR = 2.299, 95% CI = 1.362–3.879, P = 0.002), Charlson comorbidity index (CCI) ≥ 3 (OR = 2.092, 95% CI = 1.342–3.260, P = 0.001), organic mental disorder (OR = 1.941, 95% CI = 1.194–3.156, P = 0.007), antipsychotic drug use (OR = 1.886, 95% CI = 1.312–2.711, P = 0.001), unmarried status (OR = 1.720, 95% CI = 1.164–2.541, P = 0.006) and junior high school education (OR = 1.591, 95%CI = 1.010–2.508, P = 0.045) were independent risk factors for CAP in inpatients with mental disorders.
Conclusion: CAP was common in inpatients with mental disorders. Patients with mental disorders have unique risk factors for CAP. Further research is required to explore the relationship and mechanism between different mental disorders, antipsychotic drugs and CAP.
Mental disorders are a group of diseases that manifest as cognitive, emotional, and behavioral disturbances. The global burden of mental disorders has increased in recent years (1). Mental disorders account for 14.3% of all deaths worldwide, and around 8 million people with mental disorders die each year (2). Most of the reductions in life expectancy in people with mental disorders appear to be due to somatic comorbidities or other natural causes of death such as cardiovascular disease (CVD) and pneumonia (3).
Community-acquired pneumonia (CAP), which develops in people outside of healthcare settings, is a serious disease with a potentially poor long-term prognosis. CAP is particularly prevalent in developing countries and is associated with high morbidity, hospitalization, and mortality rates (4). Epidemiological studies have found that patients with mental disorders have a significantly increased risk of developing CAP (5). CAP is an important cause of hospitalization and death in patients with mental disorders (6). Patients with mental disorders such as schizophrenia and depression have a generally poorer prognosis after developing CAP, such as higher occupancy rates in the intensive care unit (ICU) (7).
Risk factors for CAP in the general population include advanced age, male gender, smoking, alcoholism, respiratory disease, dementia, and various comorbidities (8). People with mental disorders are more likely to use antipsychotic drugs, have unhealthy lifestyles, show poor adherence to treatment, and have poor access to medical services (3). All of these factors may affect the occurrence of CAP. To date, few published studies have evaluated the epidemiology of CAP and the risk factors for CAP in inpatients with mental disorders. A retrospective analysis of 2,209 patients with schizophrenia hospitalized in Tokyo, Japan, found that 101 patients (4.6%) were diagnosed with pneumonia on admission (9). Furthermore, advanced age (≥50 years-old), body mass index (BMI) <18.5 kg/m2, smoking, use of atypical antipsychotic drugs, and high-dose antipsychotic drugs were risk factors for pneumonia on admission in patients with schizophrenia (9). The above study mainly focused on patients in specialized psychiatric hospitals and on schizophrenia. There are few reports describing the epidemiological characteristics of CAP among inpatients with mental disorders in general hospitals.
Our hospital is a tertiary general hospital with the largest number of psychiatric beds in China (350 beds, including 225 beds on open wards and 125 beds on closed wards). Our hospital also has high-level respiratory, infectious disease, intensive care medicine, and radiology departments, which allows patients with suspected CAP to be diagnosed and treated in a timely manner. The aim of this cross-sectional study was to investigate the epidemiological characteristics of CAP among inpatients with mental disorders admitted to a general hospital in China.
This retrospective study included inpatients diagnosed with mental disorders at Renmin Hospital of Wuhan University between January 2017 and July 2021. The Ethics Committee of Renmin Hospital of Wuhan University approved this study (WDRY2021-KS069) and waived the requirement for informed consent due to the retrospective nature of the analysis.
The inclusion criteria were as follows: (1) admitted to the hospital with a primary diagnosis of a mental disorder or a mental disorder with pneumonia/pulmonary infection; (2) hospitalized for >48 h; and (3) aged ≥ 18 years-old. The diagnoses of the mental disorders were made in accordance with the tenth revision of the International Classification of Mental Disorders (ICD-10, codes F00–F99) (WHO, 1992). Patients were excluded from the final analysis if any of the following criteria were met: (1) hospital-acquired pneumonia (HAP); (2) died or discharged from the hospital within 48 h of admission; (3) admitted during the COVID-19 pandemic (January 2020–May 2020); (4) readmitted after a first admission during the study period; and (5) incomplete data.
The following baseline data were extracted from the medical records: age, gender, education level, marital status, smoking history, history of alcohol consumption, history of mental disorder (including type, age at onset, disease course, and current treatment strategy), BMI, comorbidities, type of ward admitted to (closed or open), the requirement for ICU admission, the requirement for mechanical ventilation, duration of hospitalization and survival.
The inpatients with mental disorders were divided into a CAP group and a non-CAP group according to whether comorbid CAP was present. The diagnosis of CAP was made if the patient met all three of the following criteria (10): (1) onset in the community; (2) any one of the following pneumonia-related clinical manifestations: (i) newly developed cough or expectoration or exacerbation of existing respiratory disease symptoms with or without purulent sputum, chest pain, dyspnea, or hemoptysis; (ii) fever; (iii) signs of pulmonary consolidation and/or moist rales; (iv) peripheral blood leukocytes > 10 × 109/L or <4 × 109/L with or without a left shift; (3) chest imaging demonstrated new patchy infiltrates, lobar or segmental consolidation, ground-glass opacities, or interstitial changes with or without pleural effusion. They were excluded if other lung diseases (such as pulmonary tuberculosis, lung tumor, non-infectious pulmonary interstitial disease, pulmonary edema, atelectasis, pulmonary embolism, pulmonary eosinophilic infiltration, or pulmonary vasculitis) were present.
The data were analyzed using SPSS 22.0 (IBM Corp., Armonk, NY, USA). Measurement data were tested for normality using the Kolmogorov-Smirnov method (sample size ≥ 50) or the Shapiro-Wilk method (sample size < 50). Normally-distributed measurement data are presented as the mean ± standard deviation (SD) and were compared between groups using the t-test for independent samples. Non-normally-distributed measurement data are shown as median [interquartile range (IQR)] and were compared between groups using the Mann–Whitney U test. Non-normally-distributed data were compared between multiple groups using the Kruskal–Wallis test. Count data are presented as frequency (percentage) and were analyzed using the chi-squared test or Fisher's exact test. Propensity score matching (PSM) was carried out using R 4.1.1 software (R Foundation for Statistical Computing, Vienna, Austria), and 1:4 matching was performed using variables such as age, gender, and BMI. Factors associated with CAP in patients with mental disorders were explored using univariate and multivariable logistic regression analyses. The presence or absence of CAP was used as the outcome variable, and the demographic/laboratory indicators were used as the independent variables. Variables with a p < 0.05 in the univariate analysis were entered into the multivariate analysis (enter method). Odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated. Multicollinearity was considered if Tolerance was <0.2 or the variance inflation factor (VIF) was >10. No multicollinearity was observed in the multivariable model. P < 0.05 was considered statistically significant.
A total of 25,891 patients with mental disorders were admitted during the study period. After the exclusion of patients under the age of 18 years-old (n = 3,853), patients with a hospital stay of <48 h (n = 449), patients with HAP (n = 194), repeat admissions (n = 4,419) and patients with incomplete pre-admission clinical data (n = 42), the final analysis included 16,934 patients. The baseline clinical characteristics of the study participants before PSM are shown in Supplementary Table 1. The 301 patients (168 men, 55.81%) in the CAP group had a median age of 50.00 (IQR, 33.00–62.00) years, and the 16,633 patients (7,063 men, 42.46%) in the non-CAP group had a median age of 31.00 (IQR, 24.00–48.00) years.
The incidence rate of CAP was 1.78% overall, 8.44% in patients with organic mental disorders, 2.80% in patients with schizophrenia spectrum disorders, 1.04% in patients with mood-affective disorders, and 1.28% in patients with other mental disorders. The incidence rate of CAP increased with age (1.06% for those aged 18–44 years-old, 2.68% for those aged 45–64 years old, and 6.86% for those aged ≥ 65 years-old), was higher in men than in women (2.32 vs. 1.37%) and higher in patients with a BMI ≤ 18.5 kg/m2 than in those with a BMI > 18.5 kg/m2 (3.90 vs. 1.65%).
The propensity score-matched data consisted of 1,495 patients and included 299 patients with CAP and 1,196 patients without CAP. There were significant differences in education, smoking, alcohol consumption, type of mental disorder, age at onset of the mental disorder, duration of the mental disorder, duration of treatment for the mental disorder, duration of treatment with antipsychotic drugs, use of antipsychotic drugs, use of clozapine, use of cholinesterase inhibitors, CCI and incidences of comorbid diseases (cerebrovascular disease, CVD, diabetes mellitus) between the CAP group and non-CAP group after PSM (Table 1).
The patient outcomes were analyzed after PSM. Inpatients with mental disorders who had comorbid CAP had a significantly prolonged hospital stay, were more often admitted to a closed ward or the ICU, and were more often treated with mechanical ventilation than those without CAP (P < 0.001 for all parameters). However, there was no significant difference in mortality rate between the two groups (Table 2).
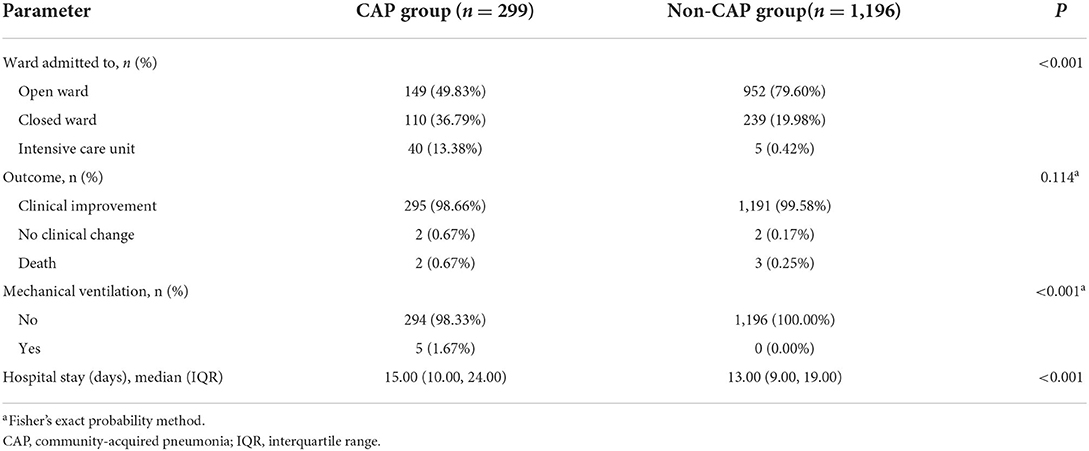
Table 2. Ward of admission and outcomes of inpatients with mental disorders stratified according to the presence/absence of comorbid community-acquired pneumonia.
Among the patients with CAP, hospital stay was significantly longer in those with schizophrenia or mood-affective disorder than in those with organic mental disorders or other types of mental illness (P = 0.039) (Table 3). Prognosis and length of hospital stay were comparable between patients admitted to open wards, closed wards, and the ICU. However, only patients admitted to the ICU received mechanical ventilation (Table 4).
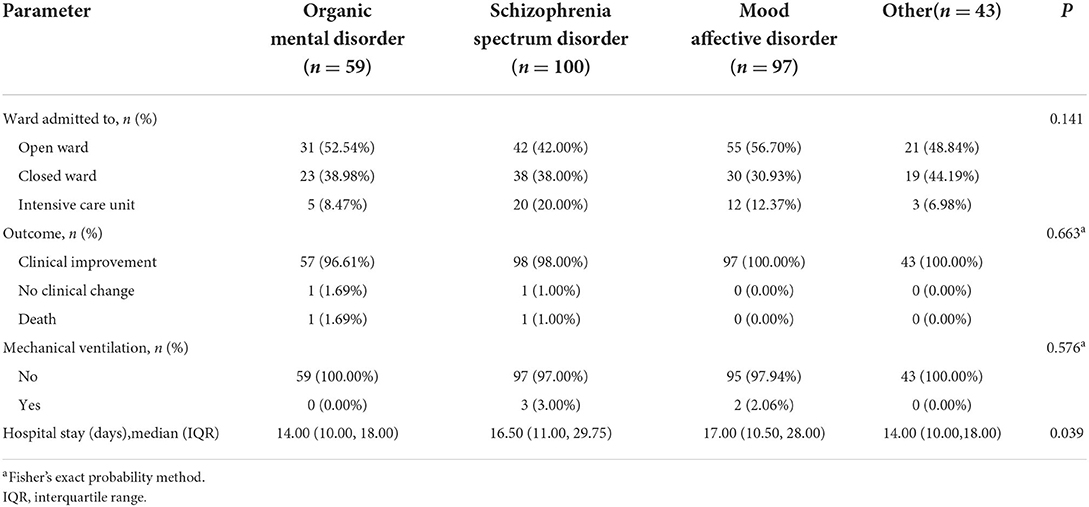
Table 3. Ward of admission and outcomes of inpatients with mental disorders and community-acquired pneumonia stratified according to the type of mental disorder.
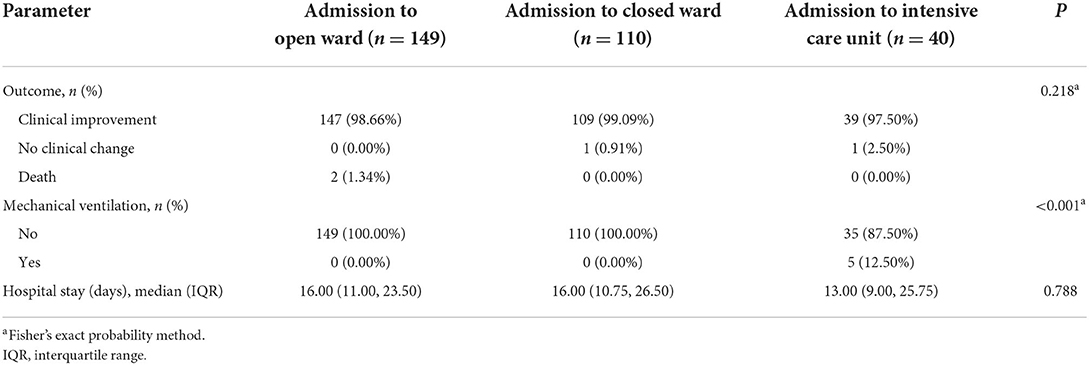
Table 4. Outcomes of inpatients with mental disorders and community-acquired pneumonia stratified according to ward of admission.
The multivariable analysis revealed that clozapine use, schizophrenia spectrum disorder, alcohol consumption, CVD, CCI ≥ 3 points, organic mental disorder, use of an antipsychotic drug, unmarried status, and junior high school education were independently associated with CAP in hospitalized patients with mental disorders (Table 5).
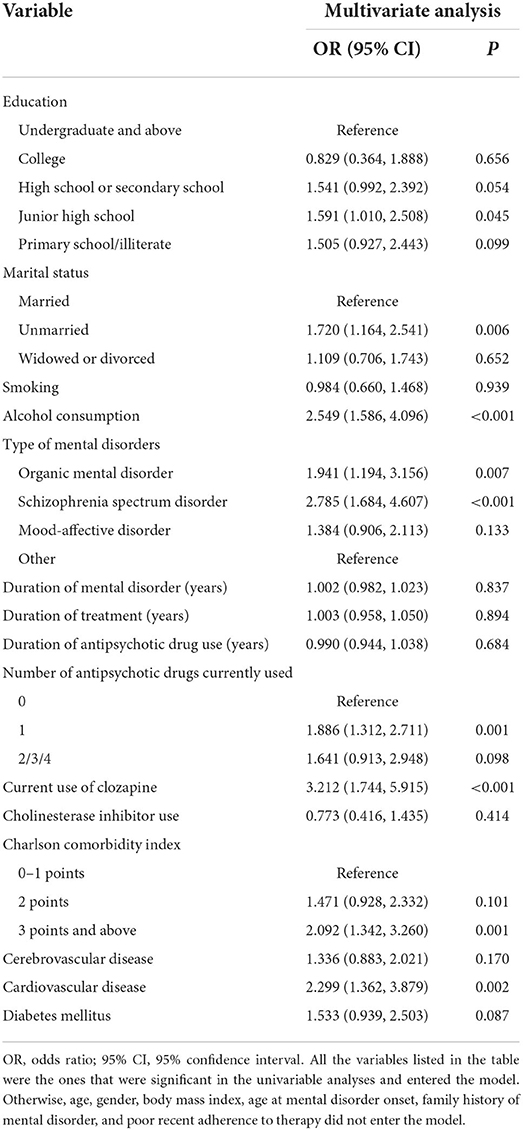
Table 5. Logistic regression analyses of factors associated with community-acquired pneumonia in inpatients with mental disorders.
As far as we know, this is the first study to investigate the occurrence, risk factor analysis, and prognosis of CAP in hospitalized patients with mental disorders in a large general hospital.
The overall incidence of CAP in the patients with mental disorders admitted to this tertiary general hospital was 1.78%, which was higher than that reported for inpatients without mental disorders (11) but lower than that in a psychiatric hospital (9). The present study found that CAP significantly increased the length of hospital stay for inpatients with mental disorders. Comorbid CAP also increased the probability of the patient being admitted to a closed ward or the ICU, as well as the probability of the patient requiring mechanical ventilation during treatment. However, comorbid CAP didn't increase the mortality rate of patients with mental disorders in this general hospital, which was different from the previous reports of psychiatric hospitals (6).
The incidence of CAP among the patients with mental disorders in this study was higher in those aged ≥ 65 years-old, males, and those with a BMI ≤ 18.5 kg/m2, which agrees well with previous findings in the general population (8). Therefore, the main analyses were performed following PSM for gender, age, and BMI. After PSM, it was found that the risk factors for CAP in patients with mental disorders admitted to this general hospital were the use of anti-psychotic drugs, especially clozapine, schizophrenia spectrum disorder, organic mental disorder, alcohol consumption, CVD, CCI index ≥ 3, unmarried status and low education level.
The observation that anti-psychotic drug use was associated with increased odds of CAP in inpatients with mental disorders is consistent with previous studies (12). Typical anti-psychotics may enhance the risk of aspiration pneumonia by causing extra-pyramidal side effects such as dyskinesia. Although atypical anti-psychotics are associated with a lower risk of extra-pyramidal side effects, they can cause dry mouth and dysphagia (due to anticholinergic effects) as well as sedation (caused by central nervous system H1 receptor blockade), which are also risk factors for pneumonia. This study found that clozapine, an atypical anti-psychotic drug, was associated with an elevated risk of CAP in inpatients with mental disorders (OR = 3.212). Several previous large-scale investigations have reported that treatment with clozapine is associated with an increased risk of pneumonia (13). Clozapine may be more likely to induce sedation and salivation (14). Clozapine is the antipsychotic drug of choice for the treatment of refractory schizophrenia (15). However, clozapine-treated patients should be monitored carefully.
This study found that inpatients with organic mental disorders or schizophrenia spectrum disorder had a higher incidence of CAP than those with other types of mental disorder. Schizophrenia is a common, chronic, and disabling mental illness (16). A 9-year follow-up study in Taiwan determined that the incidence of pneumonia in patients with schizophrenia was 10.26% and that the incidence density was 11.4/1,000 person-years (17). Many patients with schizophrenia exhibit impairments in social functioning, self-care, and self-control, which may increase the risk of pneumonia. In addition, dysphagia is common in patients with schizophrenia, and this can lead to aspiration pneumonia. Organic mental disorders may have an inherent “organic basis” and hence be associated with physical comorbidities (1), and many patients with organic mental disorders are elderly and have comorbid dementia and cerebrovascular disease, which may increase the risk of pneumonia. Dementia, in particular, is thought to elevate the risk of pneumonia (18).
Previous research showed that polymorbidity (two or more physical comorbidities) was more common in people with mental disorders than in those without mental illness (19). Compared with the general population, patients with mental disorders have a 6–8-fold increase in medical comorbidity, a shorter life expectancy, and a higher mortality (20). The present study found that a CCI index ≥ 3 was a risk factor for CAP in inpatients with mental disorders. The age- and sex-standardized incidence of CVD was found to be higher in patients with mental disorders than in those without mental illnesses (13.5/1,000 person-years vs. 6.3/1,000 person-years), and the highest CVD incidence rates were in patients with bipolar disorder and schizophrenia (21). CVD is a known risk factor for CAP (22). Thus, it is important that clinicians are aware that inpatients with mental disorders and multiple comorbidities are at particular risk of CAP.
This study found that unmarried status was closely related to CAP in inpatients with mental disorders. A population-based case-control study found that the odds of pneumonia-related hospitalization were 33% higher for unmarried people than for married people, and alcoholism-related disorders and other comorbidities appeared to explain the increased risk of pneumonia-related hospitalization in unmarried people (23). Junior high school education was also associated with CAP in inpatients with mental disorders. Prior research has yielded evidence that a higher level of education is associated with a lower risk of major psychiatric disorders and most physical disorders, independent of intelligence (24). In China, low education and being unmarried are both associated with an increased risk of serious mental illness (25). This study found that 6.03% of the inpatients with mental disorders had alcohol misuse disorder, and the consumption of alcohol was identified as a risk factor for CAP in patients with mental disorders. The sedative effects of prolonged alcohol consumption can impair cough and vomiting responses and thereby increase the risk of aspiration.
The incidence rate of CAP was 1.78% in inpatients with mental disorders. Clozapine, schizophrenia spectrum disorder, alcohol consumption, CVD, CCI index ≥ 3, organic mental disorder, use of antipsychotic drugs, unmarried status, and lower level of education were identified as independent risk factors for CAP in hospitalized patients with mental disorders. These findings provide baseline data for establishing effective prevention strategies of CAP in people with mental disorders.
First, this was a cross-sectional study, and subsequent readmissions and deaths after discharge were not tracked. Second, this study involved only one general hospital, so the findings will need to be further evaluated in a stratified analysis of data from multiple centers of different sizes. Third, the severity of mental disorders on admission could not be assessed in all patients due to the retrospective study design.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
JH and GW conceived and designed the experiment. JH performed the research, analyzed the results, wrote the manuscript, analyzed the data, and carried out a literature search. JH, QW, LX, and GW contributed to revising the manuscript. JH and MS collected data. JH and ZL submitted the article. All authors read and approved the final manuscript.
This study was supported by the National Natural Science Foundation of China (No. 81571325 and No. 81401117); the Medical Science Advancement Program of Wuhan University (No. TFLC2018001); Design of this study was supported by the National Natural Science Foundation of China (No. 81571325 and No. 81401117).
Thanks to DongJun Qin from Shanghai MedSci Healthcare Center for his assistance with the statistical analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.941198/full#supplementary-material
1. Chen WY, Huang SJ, Chang CK, Pan CH, Su SS, Yang TW, et al. Excess mortality and risk factors for mortality among patients with severe mental disorders receiving home care case management. Nord J Psychiatry. (2021) 75:109–17. doi: 10.1080/08039488.2020.1799431
2. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
3. Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. (2015) 72:1172–81. doi: 10.1001/jamapsychiatry.2015.1737
4. Kosar F, Alici DE, Hacibedel B, Arpinar Yigitbas B, Golabi P, Cuhadaroglu C. Burden of community-acquired pneumonia in adults over 18 y of age. Hum Vaccin Immunother. (2017) 13:1673–80. doi: 10.1080/21645515.2017.1300730
5. Schoepf D, Uppal H, Potluri R, Heun R. Physical comorbidity and its relevance on mortality in schizophrenia: a naturalistic 12-year follow-up in general hospital admissions. Eur Arch Psychiatry Clin Neurosci. (2014) 264:3–28. doi: 10.1007/s00406-013-0436-x
6. Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L. Risk of dementia and death in community-dwelling older men with bipolar disorder. Br J Psychiatry. (2016) 209:121–6. doi: 10.1192/bjp.bp.115.180059
7. Kao LT, Liu SP, Lin HC, Lee HC, Tsai MC, Chung SD. Poor clinical outcomes among pneumonia patients with depressive disorder. PLoS ONE. (2014) 9:e116436. doi: 10.1371/journal.pone.0116436
8. Hammond A, Halliday A, Thornton HV, Hay AD. Predisposing factors to acquisition of acute respiratory tract infections in the community: a systematic review and meta-analysis. BMC Infect Dis. (2021) 21:1254. doi: 10.1186/s12879-021-06954-3
9. Haga T, Ito K, Sakashita K, Iguchi M, Ono M, Tatsumi K. Risk factors for pneumonia in patients with schizophrenia. Neuropsychopharmacol Rep. (2018) 38:204–209. doi: 10.1002/npr2.12034
10. Cao B, Huang Y, She DY, Cheng QJ, Fan H, Tian XL, et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society, Chinese Medical Association. Clin Respir J. (2018) 12:1320–60. doi: 10.1111/crj.12674
11. McLaughlin JM, Khan FL, Thoburn EA, Isturiz RE, Swerdlow DL. Rates of hospitalization for community-acquired pneumonia among US adults: a systematic review. Vaccine. (2020) 38:741–51. doi: 10.1016/j.vaccine.2019.10.101
12. Papola D, Ostuzzi G, Gastaldon C, Morgano GP, Dragioti E, Carvalho AF. Antipsychotic use and risk of life-threatening medical events: umbrella review of observational studies. Acta Psychiatr Scand. (2019) 140:227–43. doi: 10.1111/acps.13066
13. de Leon J, Sanz EJ, Norén GN, De Las Cuevas C. Pneumonia may be more frequent and have more fatal outcomes with clozapine than with other second-generation antipsychotics. World Psychiatry. (2020) 19:120–1. doi: 10.1002/wps.20707
14. Cicala G, Barbieri MA, Spina E, de Leon J. A comprehensive review of swallowing difficulties and dysphagia associated with antipsychotics in adults. Expert Rev Clin Pharmacol. (2019) 12:219–34. doi: 10.1080/17512433.2019.1577134
15. National Collaborating Centre for Mental Health. National Institute for Health and Clinical Excellence: Guidance. Psychosis and Schizophrenia in Adults: Treatment and Management: Updated Edition 2014. London: National Institute for Health and Care Excellence (UK) Copyright (c) National Collaborating Centre for Mental Health. (2014).
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (DSM-5). Arlington: American Psychiatric Association. (2013).
17. Chou FH, Tsai KY, Chou YM. The incidence and all-cause mortality of pneumonia in patients with schizophrenia: a nine-year follow-up study. J Psychiatr Res. (2013) 47:460–6. doi: 10.1016/j.jpsychires.2012.12.007
18. Manabe T, Fujikura Y, Mizukami K, Akatsu H, Kudo K. Pneumonia-associated death in patients with dementia: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0213825. doi: 10.1371/journal.pone.0213825
19. Stubbs B, Koyanagi A, Veronese N, Vancampfort D, Solmi M, Gaughran F, et al. Physical multimorbidity and psychosis: comprehensive cross sectional analysis including 242,952 people across 48 low- and middle-income countries. BMC Med. (2016) 14:189. doi: 10.1186/s12916-016-0734-z
20. Plana-Ripoll O, Pedersen CB, Agerbo E, Holtz Y, Erlangsen A, Canudas-Romo V, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. (2019) 394:1827–35. doi: 10.1016/S0140-6736(19)32316-5
21. Bent-Ennakhil N, Cécile Périer M, Sobocki P, Gothefors D, Johansson G, Milea D, et al. Incidence of cardiovascular diseases and type-2-diabetes mellitus in patients with psychiatric disorders. Nord J Psychiatry. (2018) 72:455–61. doi: 10.1080/08039488.2018.1463392
22. Yeh JJ, Lin CL, Kao CH. Relationship between pneumonia and cardiovascular diseases: a retrospective cohort study of the general population. Eur J Intern Med. (2019) 59:39–45. doi: 10.1016/j.ejim.2018.08.003
23. Mor A, Ulrichsen SP, Svensson E, Berencsi K, Thomsen RW. Does marriage protect against hospitalization with pneumonia? A population-based case-control study. Clin Epidemiol. (2013) 5:397–405. doi: 10.2147/CLEP.S50505
24. Yuan S, Xiong Y, Michaëlsson M, Michaëlsson K, Larsson SC. Genetically predicted education attainment in relation to somatic and mental health. Sci Rep. (2021) 11:4296. doi: 10.1038/s41598-021-83801-0
Keywords: mental disorders, community-acquired pneumonia, general hospitals, inpatients, risk factors
Citation: Han J, Shen M, Wan Q, Lv Z, Xiao L and Wang G (2022) Risk factors for community-acquired pneumonia among inpatients with mental disorders in a tertiary general hospital. Front. Psychiatry 13:941198. doi: 10.3389/fpsyt.2022.941198
Received: 11 May 2022; Accepted: 29 June 2022;
Published: 22 July 2022.
Edited by:
María del Mar Molero Jurado, University of Almeria, SpainReviewed by:
Laura Bahlis, Clinical Hospital of Porto Alegre, BrazilCopyright © 2022 Han, Shen, Wan, Lv, Xiao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gaohua Wang, d2doNjQwMkAxNjMuY29t; Ling Xiao, MzI3NTUwMzc3QHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.