- 1Applied Neurosciences for Technological Advances in Rehabilitation Systems (ANTARES) Joint Lab, Clinica Psichiatrica ed SPDC, Largo Rosanna Benzi, Genoa, Italy
- 2Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), Section of Psychiatry, University of Genoa, Genoa, Italy
- 3IRCCS Ospedale Policlinico San Martino, Genoa, Italy
- 4U-VIP Unit for Visually Impaired People, Fondazione Istituto Italiano di Tecnologia, Genoa, Italy
Since the outbreak of the COVID-19 pandemic, reading facial expressions has become more complex due to face masks covering the lower part of people's faces. A history of psychiatric illness has been associated with higher rates of complications, hospitalization, and mortality due to COVID-19. Psychiatric patients have well-documented difficulties reading emotions from facial expressions; accordingly, this study assesses how using face masks, such as those worn for preventing COVID-19 transmission, impacts the emotion recognition skills of patients with psychiatric disorders. To this end, the current study asked patients with bipolar disorder, major depressive disorder, schizophrenia, and healthy individuals to identify facial emotions on face images with and without facial masks. Results demonstrate that the emotion recognition skills of all participants were negatively influenced by face masks. Moreover, the main insight of the study is that the impairment is crucially significant when patients with major depressive disorder and schizophrenia had to identify happiness at a low-intensity level. These findings have important implications for satisfactory social relationships and well-being. If emotions with positive valence are hardly understood by specific psychiatric patients, there is an even greater requirement for doctor-patient interactions in public primary care.
Introduction
The impact and social consequences of the COVID-19 pandemic varied depending on factors such as social inequalities (1), age, gender (2), and the presence of medical (3) and psychiatric (4) conditions. Moreover, among individuals with mental health conditions, COVID-19 presents higher rates of complications, hospitalization, and mortality (5). The history of psychiatric illness confers a heightened vulnerability to disaster-related conditions (6).
Owing to the outbreak of the COVID-19 pandemic, the use of face masks has become somewhat widespread depending on different state laws and people's subjective attitudes (7). Although different beliefs about the effectiveness of this personal protective equipment, face mask has been widely adopted to reduce disease transmission (8, 9). Wearing face masks significantly impacts the human capacity to read facial expressions [for a comprehensive review, see (10)], making it more difficult to recognize people's emotions and their intensity (7, 11–14). The ancestral origin and crucial phylogenetic importance of the facial emotion recognition process in social interactions has been apparent since Darwin's first observations 150 years ago in his book “The Expression of the Emotions in Man and Animals” (15). His intuition has received further confirmations to date, due in particular to Paul Ekman's work (16). Reading facial expressions is an essential component of non-verbal communication in humans, together with head orientation (17), posture, body language (7) or characteristics of voice (18). While understanding affective expressions is a key social ability, its deficit is associated with severe difficulties in human interactions (19). Before the pandemic, studies reported that people had difficulty reading facial emotions when others were wearing some objects that cover parts of the face, for example: cardboard (20), a cap, or a scarf (21). More recently, studies on face masks reported that covering the lower part of the face altered the facial emotion reading (22), probably due to the constraint of focusing on the eye region compared to the mouth region (23, 24).
Mental illness conditions are often characterized by a different magnitude of impairments in social functioning and interpersonal interactions (25), linked to significant impairments in emotional expression reading. Participants with psychiatric disorders showed different degrees of impairment in facial emotion recognition (26). Such impacts on the emotional reading of faces mainly depend on shared alterations of dimensions such as mood (27), social cognition (28), or metacognition (29) among mental illnesses. Given the well-known disadvantages in social interactions of participants who present with a mental illness (Wild and Kornfeld 2021), the current study aims to assess how the widespread use of face masks impacts the emotion recognition skills in patients with psychiatric disorders.
For this purpose, we asked a group of participants with bipolar disorder (BD), major depressive disorder (MDD), schizophrenia (SZ), and a healthy control (HC) group to identify facial emotions on images with and without face masks. Our study tested varying intensities of facial expressions to investigate mild levels of impairment and recall more realistic facial configurations.
Methods
Sample
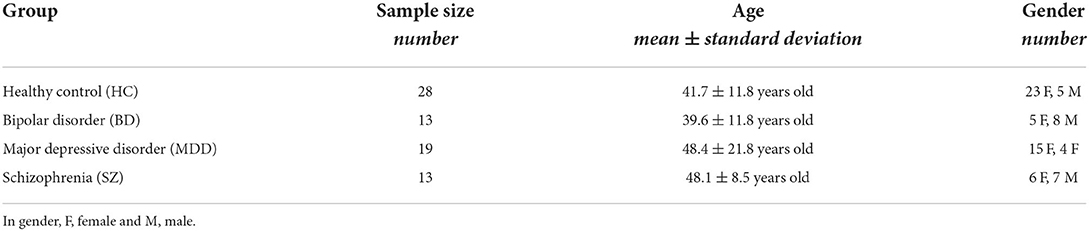
The current study recruited twenty-eight HC, 15 participants with BD, 20 participants with MDD, and 13 participants with SZ (see Table 1). The study excluded one participant with MDD and two participants with BD from the analyses because they were identified as outliers (i.e., a score in at least one task differing more than two standard deviations from the group's mean score). Thus, the remaining group was comprised of 28 HC (mean age ± standard deviation = 41.7 years old ± 11.8; females = 23), 13 participants with BD (39.6 years old ± 11.8; females = 5) 19 participants with MDD (48.4 years old ± 21.8; females = 15), and 13 participants with SZ (48.1 years old ± 8.5; females = 6). Groups were age-matched (F(3, 69) = 1.5, p > 0.05). The study included a power analysis based on previously published studies testing participants' ability to recognize emotion with and without masks among healthy adults (22), indicating a minimum of 13 participants was necessary to reach a power of 0.85 (two-tailed t-test, Cohen's d = 1.2, α = 0.05).
All psychiatric patients were recruited from the Psychiatric Unit of San Martino Hospital in Genoa, and they were hospitalized while testing was occurring. The study recruited typical participants from the general population using advertising on social media and personal newsletters. Moreover, they underwent a clinical interview to exclude the presence of lifetime or current psychiatric disorders. Participants did not receive incentives of any kind for participating in the study. The Ethical Committee of IRCCS Ospedale Policlinico San Martino approved the study, and all participants gave their written informed consent.
Experimental paradigm
To investigate how face masks affect emotion recognition in psychiatric patients during hospitalization, we administered an internet-based questionnaire via smartphone. The questionnaire required participants to identify facial emotions on images with and without facial masks. Specifically, we replicated the paradigm that researchers previously used to test the effects of face masks on emotion recognition during childhood (22). This consisted of a standardized verbal-response test based on selecting an emotion's label (forced-choice) as a means to describe static pictures of human facial configurations. Such a choice favored the repeatability of the task and simplified the test administration to overcome the difficulties related to hospitalization and social distancing rules.
The task was structured in sequential blocks, showing first a block of pictures with facial masks, followed by a block of mask-free images. A total of 40 adult face pictures were presented in randomized order, including four repetitions of four facial emotions (happiness, sadness, fear, anger) with two levels of intensity (Low, High), in addition to a neutral facial expression that was presented 8 times to each participant. Figure 1 offers example images of happiness, sadness, fear and anger, with a low level of intensity. The original and modified pictures were obtained from the ER-40 color emotional stimuli database (30, 31), developed for the validated ER-40 test for facial emotion recognition (32, 33). A web designer modified pictures from the original database ad hoc, creating and adding realistic face masks for the set of images containing masks. We asked participants to identify their facial emotions by choosing five possible randomized options: happy, sad, fearful, angry, and neutral (see Figure 2).

Figure 1. Examples of low-intensity facial configuration with and without face masks for happiness, anger, sadness, and fear. Face images were obtained with permission from the ER-40 color emotional stimuli public database (30, 31).
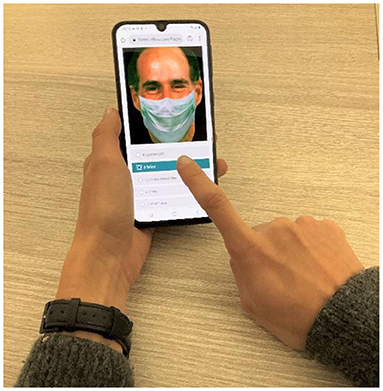
Figure 2. Experimental procedure. We asked participants to identify the correct facial emotion by choosing between five possible randomized options: happy, sad, fearful, angry, and neutral. Each face was displayed on the screen of personal smartphones for as long as it took to respond by holding an index finger against the touch screen. The study obtained face images with permission from the ER-40 color emotional stimuli public database (30, 31).
To control for face mask exposure, the test occurred one year following the first lockdown's end in Italy (May 2021). Patients performed the test autonomously under the supervision of a clinical doctor, while typical participants performed it without supervision (the participants received specific written instructions, including the instruction to perform the task without any help). We did not impose time limits to provide answers.
Data analyses
For data analysis, we calculated performance as a percentage of correct responses with and without the masks. Performance was not normally distributed for one group (Shapiro-Wilk normality tests: HC: W = 0.91, p < 0.01; BD: W = 0.95, p > 0.05; MDD: W = 0.96, p > 0.05; SZ: W = 0.97, p > 0.05); we then ran ANOVAs based on permutation tests and permutation t-tests. We used the aovp function (lmPerm package) and the perm.t.test function (MKinfer package) in R to compute the analysis. First, for each emotion separately (i.e., Happiness, Sadness, Fear, Anger), we ran an ANOVA based on permutation tests with mask presence (i.e., Mask, NoMask) and intensity level of emotions (i.e., Low, High) as within-subject factors and group (i.e., HC, BD, MDD, SZ) as between-subject factors. Considering there were no significant interactions between mask presence x intensity x group for anger, fear, and sadness but only for happiness, we focused subsequent analyses on emotional valence. We marked happiness as positive emotional valence, while grouping sadness, fear and anger into negative emotional valence. We thereby ran an ANOVA based on permutation tests with group (i.e., HC, BD, MDD, SZ) as between-subject factor, condition (i.e., Mask, NoMask), the intensity level of emotions (i.e., Low, High) and valence (i.e., Positive, Negative) as within-subject factors. We carried out follow-up ANOVAs using permutation tests and post hoc comparisons, applying Bonferroni correction to the results.
The intensity was absent as a variable for neutral faces. For the neutral expression, we performed a separate ANOVA based on permutation tests that considered only mask presence (i.e., Mask, NoMask) and group (i.e., HC, BD, MDD, SZ). Moreover, we computed confusion matrices to investigate the response distribution among different emotions with masks for each group.
Results
Results showed that face masks always negatively impact the human ability to recognize emotions from facial configurations, but in the current study, this was particularly true for patients with MDD and SZ who were asked to recognize low-intensity images with positive valence. Indeed, the ability of patients with MDD and SZ to infer happiness when happy facial configurations were relatively subtle is drastically influenced by face masks.
When considering each emotion separately, the interaction between mask presence x intensity x group appeared significant only for happiness, which offered the opportunity to group fear, anger and sadness and analyse them together based on their negative valence. Specifically, the interaction was insignificant for anger [F(3, 207) = 0.1, p > 0.05, Iter = 51], sadness [F(3, 207) = 0.7, p > 0.05, Iter = 556], and fear [F(3, 207) = 0.2, p > 0.05, Iter = 424]. Subsequently, the ANOVA considering mask presence, group, valence and level of intensity demonstrated a significant main effect of mask presence [F(1, 1, 067) = 54.7, p < 0.01, Iter = 5,000], group [F(3, 69) = 6.5, p < 0.01, Iter = 5,000], valence [F(1, 1, 067) = 184.7, p < 0.01, Iter = 5,000] and level intensity [F(1, 1, 067) = 54.7, p < 0.01, Iter = 5,000]. Moreover, this analysis revealed a significant interaction between the involved factors [mask presence x group x valence x level of intensity: F(3, 1067) = 2, p < 0.01, Iter = 5,000].
Concerning the emotion with positive valence (i.e., happiness, Figure 3 top), the follow-up analyses demonstrated a significant interaction between mask presence x group x level of intensity [F(3, 276) = 4.8, p < 0.05, Iter = 5,000], allowing us to separately analyse the two levels of intensity. For high-intensity emotions with positive valence (Figure 3A) only a significant main effect of mask presence emerged [F(1, 69) = 3.8, p < 0.01, Iter = 2,865], while there was no significant effects for group [F(3, 69) = 2.1, p > 0.05, Iter = 724] and the interaction mask presence x group [F(3, 69) = 1.6, p > 0.05, Iter = 1,377]. Instead, for low-intensity emotions with positive valence (Figure 3B), the interaction between mask presence and group was statistically significant [F(3, 69) = 6.6, p < 0.01, Iter = 5,000]. Post hoc permutation t-tests showed masks' presence reduced a participant's ability to recognize emotions with positive valence for HC [t(37.8) = −2.2, p < 0.01, Iter = 5,000], MDD patients [t(18) = −5.9, p < 0.01, Iter = 5,000], and SZ patients [t(16.4) = −3.5, p < 0.01, Iter = 5,000], but not BD patients [t(24) = 0.0001, p > 0.05, Iter = 5,000]. Moreover, while patients and control participants performed similarly without masks [for HC vs. BD: t(20.2) = 0.3, p > 0.05, Iter = 5,000; for HC vs. MDD: t(27) = −1.8, p > 0.05, Iter = 5,000; for HC vs. SZ: t(20.2) = 0.4, p > 0.05, Iter = 5,000; for BD vs. MDD: t(12)= 1.5, p > 0.05, Iter = 400; for BD vs. SZ: t(24) = 0.0001, p > 0.05, Iter = 5,000; for MDD vs. SZ: t(12) = 1.5, p > 0.05, Iter = 400], analyses showed some differences between groups when masks covered half of one's face. Specifically, MDD patients performed worse than HC participants [t(35.5) = 2.8, p < 0.01, Iter = 5,000], and BD patients [t(27.5) = −4.3, p < 0.01, Iter = 5,000]. Similarly, SZ patients performed worse than HC [t(19.4) = 2.4, p < 0.01, Iter = 5,000] and BD patients [t(16.4) = 3.5, p < 0.01, Iter = 5,000]. HC participants and BD patients had similar performance with masks [t(37.8) = −1.6, p > 0.05, Iter = 5,000], as did MDD and SZ patients [t(24.1) = 0.08, p > 0.05, Iter = 5,000].
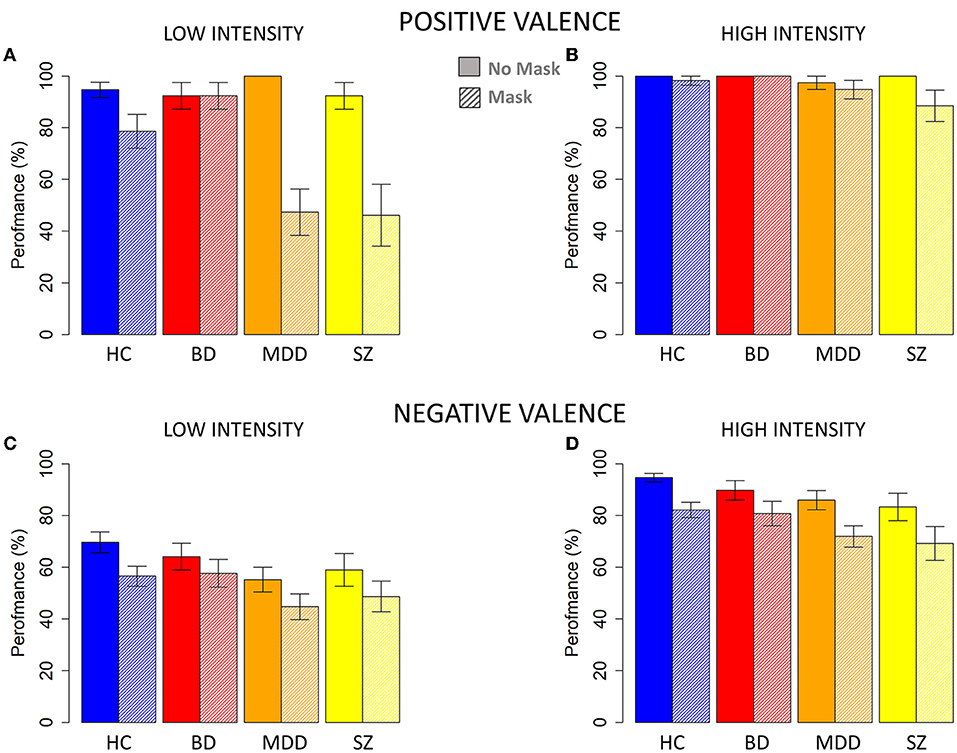
Figure 3. Percentage of correct responses without and with face masks for each group. (A) Performance for images with low-level positive valence. (B) Performance for images with high-level positive valence. (C) Performance for images with low-level negative valence. (D) Performance for images with high-level negative valence. HC, healthy control; BD, patients with bipolar disorder; MDD, patients with major depressive disorder; SZ, patients with schizophrenia. Filled and shaded color bars represent images without and with face masks, respectively. The standard error of the mean (SEM) is reported.
For emotions with negative valence (Figure 3 bottom), the interaction mask presence x group x level of intensity was insignificant [F(3, 791) = 0.07, p > 0.05, Iter = 51]. The analysis showed an overall decrease of performance correlated with mask presence [F(1, 791) = 54.7, p < 0.01, Iter = 5,000], low level of intensity [F(1, 791) = 184.7, p < 0.01, Iter = 5,000] and group [F(3, 69) = 6.5, p < 0.01, Iter = 5,000]. As Figures 3C,D indicate, the percentage of corrected responses gradually decreased independent of intensity level among HC participants, patients with BD, patients with MDD, and patients with SZ.
When analyzing neutral expressions, we observed that masks similarly affected the performance of all participants, with no differences between groups. Indeed, a main effect of mask presence emerged from the ANOVA on performance [F(1, 69) = 8.5, p < 0.01, Iter = 4,913] but not a main effect of group [F(3, 69) = 1.9, p > 0.05, Iter = 432] or an interaction between mask presence and group [F(1, 69) = 1.9, p > 0.05, Iter = 962].
Figure 4 presents response distribution among different emotions with masks, indicating the matrices of confusion for low and high levels of intensity emotions for HC, BD, MDD, and SZ individuals, respectively. We excluded the responses to neutral expressions as they do not involve two levels of intensity. All participants confused the correct emotion with other emotions more often when the mask was present. For all groups, confusion increased in the low-intensity condition, and this was especially true for MDD and SZ patients. The most challenging emotion to recognize was anger in line with (30, 33), which participants typically recognized as a neutral expression or sadness. Participants regularly misrecognized happy faces covered with masks as neutral expressions, while also confusing sad faces covered with masks with neutral expressions and all the other emotions.
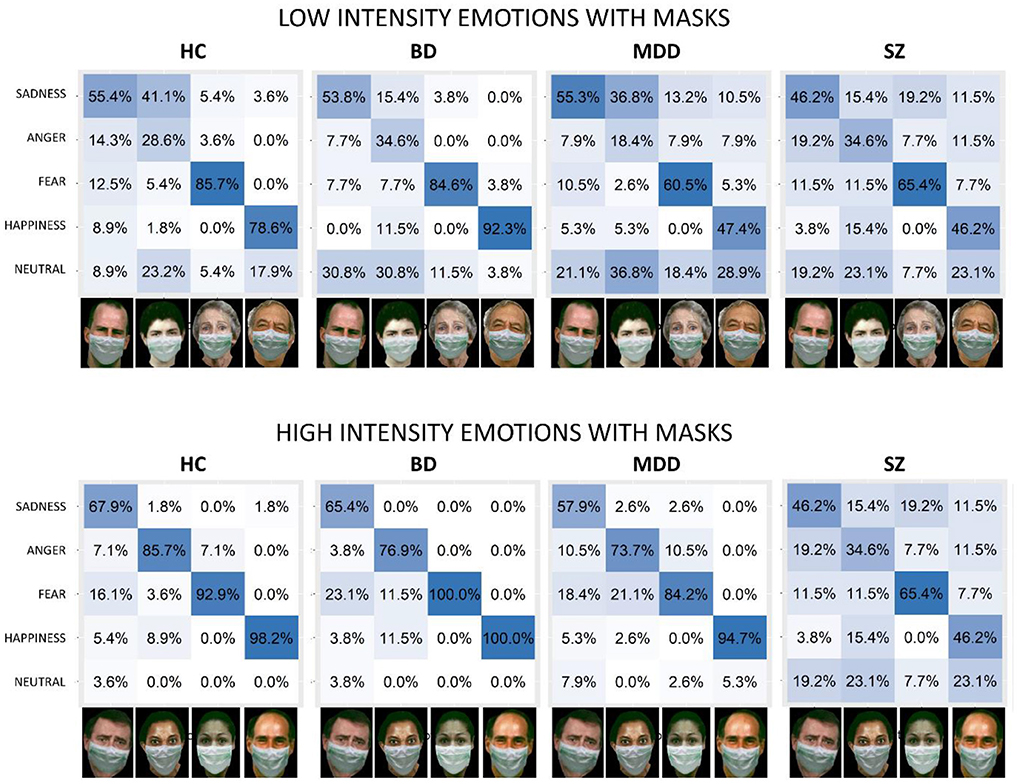
Figure 4. Confusion matrices for emotion inference from low-intensity (bottom) and high-intensity (top) facial configurations with face masks for all groups. The x-axis shows the presented stimuli. The y-axis shows the emotions perceived by participants. Columns report the percentage of responses for each emotion. HC, healthy control; BD, patients with bipolar disorder; MDD, patients with major depressive disorder; SZ, patients with schizophrenia. Face images were obtained with permission from the ER-40 color emotional stimuli public database (30, 31).
Discussion
In this study, we investigated whether psychiatric patients, and particularly those affected by BD, SZ, and MDD, have more difficulties than healthy people recognizing facial emotions with a part of the face covered by a face mask. We demonstrated that using face masks overall reduces recognition performance across all individuals. Moreover, hiding the lower part of the face with face masks specifically impairs the recognition of subtle happy faces for SZ and MDD.
We replicated literature findings of a negative effect in recognizing facial expressions due to face masks (14, 22, 34). As expected, in specific cases, the difficulty is much higher for psychiatric patients. Indeed, impairment is particularly intense for positive faces with low-intensity emotional valence: face masks critically altered the chances of MDD and SZ participants recognizing happiness when it is slight. These results further confirm the importance of the mouth region in recognizing this emotion (23, 35). The reason for the drop in performance in MDD and SZ individuals when they must recognize low-intensity happy faces with masks may result from the negative symptoms these groups of patients share. An inverse association has been shown between the accuracy in recognizing happy expressions and depression severity (36). As well, depression drives people to bias facial expressions toward negative emotions like sadness, thus under-recognizing happy facial expressions in comparison with healthy participants (36). Given the crucial importance of the mouth to infer the facial expression of happiness (37), it is reasonable to hypothesize that when a mask covers this region there results in a real struggle to recognize happiness in the presence of negative symptoms. A ceiling effect for low-intensity happiness without masks might also underly the lack of differences between the two groups of patients and, if this is the case, this limits the generalizability of our results to real-life situations. Indeed, for high-intensity positive emotions with and without masks, and low-intensity positive without masks, we did not observe significant differences between the groups (SZ, MDD, BD, and HC). The lack of differences between patients and controls in these conditions is likely due to the dataset of images that involves very clear stimuli concerning positive emotions, evoking ceiling effects (33). In contrast to the commonly used emotion recognition tasks, we chose to use an easier task to emphasize the difference between the masked vs. non-masked conditions. Another non-mutually exclusive hypothesis is that the presence of masks during the year of COVID-19 before our experiment helped patients in their overall ability to recognize emotions. We can speculate that focusing only on the eyes during the pandemic improved skills to recognize facial expressions; when only half the face is available, patients generally had to learn to be more responsive to eye cues. If this is the case, patients still face difficulties when masks cover part of the face but became more similar to HC when the whole face was visible. Further research is necessary to validate this latter hypothesis. The fact that the performance drastically decreases when low-intensity happy expressions are covered with masks stresses the importance of the mouth region in recognizing happiness when negative symptoms are present.
As for emotion with negative valence (i.e., fear, anger, and sadness), we observed that the presence of masks similarly impacted the performance of all participants. We hypothesize that the deficit associated with the mask is present in all groups but not particularly impairing. This is because recognizing anger and fearful expressions largely requires information from the eyes (38–40). In line with previous results, performance significantly decreases with reduced intensity (33) and, independent of intensity level, the percentage of corrected responses was higher for HC and decreased for BD, followed by MDD and SZ. This agrees with the overall difficulty of psychiatric patients in reading facial emotions. For instance, a recent review by Krause et al. (36) stresses the existence of a broad facial emotion recognition deficit in individuals suffering from MDD. Among participants affected with BD, available evidence accounted for a global or selective facial expression recognition deficit in euthymic participants, or during the active phase of illness in nearly 2/3 of the available studies (41). Patients affected with BD are significantly less accurate when it comes to recognizing facial emotions but particularly fear (42, 43). Since the first episode, psychotic patients displayed a global impairment in recognizing facial affective expressions, and in particular negative emotions like fear and anger (28). Similarly, participants with SZ are generally insensitive or misrecognized negative emotions such as sadness, fear, and anger (44) while also being more likely to misinterpret happy faces (45). In SZ patients, the abnormal face processing seems to depend on a faulty structural encoding of faces (45, 46) and on the tendency to visually scan features of the face that are not important in the expression of a specific emotion (47).
Regarding neutral expressions, our study agrees with previous findings that reported a certain difficulty in recognizing the neutral expression, a difficulty accentuated when the face mask is worn (39, 48).
To conclude, the outcome of our work is that wearing a face mask makes each facial expression much more complex to recognize, regardless of the underlying psychological disorder. However, when the face mask is on, difficulties in recognizing happy facial emotions become even more severe for SZ and MDD patients. Nevertheless, this study has some limitations for which to account when interpreting the results: samples were relatively small and unequal in terms of the number of participants; the visual input includes different positions of the head, head tilt, etc. beyond information about facial emotions; all patients were hospitalized at the moment of testing, questioning the generalizability of results when it comes to applying them to non-hospitalized people suffering from mental health conditions; the experimental setup challenges the ecological validity of a computerized test vs. real-life situations. Furthermore, future studies should address possible effects resulting from a lack of gender-matched samples. Indeed, emotion recognition is gender specific, with females known to better perform (49–51), and females predominated our sample of MDD in line with the skewed gender ratio for this psychiatric condition (51). Females also predominated the HC group because we purposefully matched it with the gender bias of the MDD group. Moreover, we cannot completely rule out other potential confounds, such as visual acuity, previous experience with this kind of paradigm, or personality traits. Although further research is necessary, our findings retain important clinical implications. They may explain why the use of portrait photos with smiling faces positively affects patients' perceptions of healthcare staff (52). Additionally, the impairment of positive implicit communication might contribute to misinterpretation of other intentions and emotions during social relationships (53), with negative consequences on clinical interactions with patients of mental health workers such as psychiatrists, psychologists, psychiatric rehabilitation technicians, or nurses. Moreover, recognizing emotions with positive valence is crucial for the patient's social interactions and well-being in general.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Committee of IRCCS Ospedale Policlinico San Martino. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AE, MBA, DE, and BP collected the data and organized the database. MBA performed the statistical analysis. AE, MBA, and AR wrote the first draft of the manuscript. AT helped to revised the manuscript. All authors contributed to the conception and design of the study, revising, reading, and approving the submitted version.
Funding
This research was supported by the joint lab ANTARES between the Unit for Visually Impaired People (IIT) and the Section of Psychiatry of the Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI) of the University of Genoa. This work was developed within the DINOGMI Department of Excellence of MIUR 2018-2022 (Law 232; 2016).
Acknowledgments
We thank all participants who took part in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Magesh S, John D, Li WT, Li Y, Mattingly-App A, Jain S, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw open. (2021) 4:e2134147. doi: 10.1001/jamanetworkopen.2021.34147
2. Barek MA, Aziz MA, Islam MS. Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: a meta-analysis with 55 studies and 10,014 cases. Heliyon. (2020) 6:e05684. doi: 10.1016/j.heliyon.2020.e05684
3. Thakur B, Dubey P, Benitez J, Torres JP, Reddy S, Shokar N, et al. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Rep. (2021) 11:8562. doi: 10.1038/s41598-021-88130-w
4. Campion J, Javed A, Lund C, Sartorius N, Saxena S, Marmot M, et al. Public mental health: required actions to address implementation failure in the context of COVID-19. Lancet Psychiatry. (2022) 9:169. doi: 10.1016/S2215-0366(21)00199-1
5. Hassan L, Peek N, Lovell K, Carvalho AF, Solmi M, Stubbs B, et al. Disparities in COVID-19 infection, hospitalisation and death in people with schizophrenia, bipolar disorder, and major depressive disorder: a cohort study of the UK biobank. Mol Psychiatry. (2021) 27:1248–55. doi: 10.1038/s41380-021-01344-2
6. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
7. Carbon CC. Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol. (2020) 11:566886. doi: 10.3389/fpsyg.2020.566886
8. Baxter-King R, Brown JR, Enos RD, Naeim A, Vavreck L. How local partisan context conditions prosocial behaviors: Mask wearing during COVID-19. Proc Natl Acad Sci U S A. (2022) 119:e2116311119. doi: 10.1073/pnas.2116311119
9. Collis A, Garimella K, Moehring A, Rahimian MA, Babalola S, Gobat NH, et al. Global survey on COVID-19 beliefs, behaviours and norms. Nat Hum Behav. (2022) 1–8. doi: 10.1038/s41562-022-01347-1. [Epub ahead of print].
10. Pavlova MA, Sokolov AA. Reading covered faces. Cereb Cortex. (2022) 32:249–65. doi: 10.1093/cercor/bhab311
11. Henke L, Guseva M, Wagemans K, Pischedda D, Haynes J-D, Jahn G, et al. Surgical face masks do not impair the decoding of facial expressions of negative affect more severely in older than in younger adults. Cogn Res Princ Implic. (2022) 7:63. doi: 10.1186/s41235-022-00403-8
12. Pavlova MA, Sokolov AA. Reading language of the eyes. Neurosci Biobehav Rev. (2022) 140:104755–104755. doi: 10.1016/j.neubiorev.2022.104755
13. Proverbio AM, Cerri A. The recognition of facial expressions under surgical masks: the primacy of anger. Front Neurosci. (2022) 16:864490. doi: 10.3389/fnins.2022.864490
14. Tsantani M, Podgajecka V, Gray KLH, Cook R. How does the presence of a surgical face mask impair the perceived intensity of facial emotions? PLoS ONE. (2022) 17:e0262344. doi: 10.1371/journal.pone.0262344
15. Waller BM, Julle-Daniere E, Micheletta J. Measuring the evolution of facial “expression” using multi-species FACS. Neurosci Biobehav Rev. (2020) 113:1–11. doi: 10.1016/j.neubiorev.2020.02.031
16. Wolf K. Measuring facial expression of emotion. Dialogues Clin Neurosci. (2015) 17:457–62. doi: 10.31887/DCNS.2015.17.4/kwolf
17. Sauer A, Mothes-Lasch M, Miltner WHR, Straube T. Effects of gaze direction, head orientation and valence of facial expression on amygdala activity. Soc Cogn Affect Neurosci. (2014) 9:1246–52. doi: 10.1093/scan/nst100
18. Aviezer H, Hassin RR, Ryan J, Grady C, Susskind J, Anderson A, et al. Angry, disgusted, or afraid? Studies on the malleability of emotion perception. Psychol Sci. (2008) 19:724–32. doi: 10.1111/j.1467-9280.2008.02148.x
19. Avery SN, VanDerKlok RM, Heckers S, Blackford JU. Impaired face recognition is associated with social inhibition. Psychiatry Res. (2016) 236:53. doi: 10.1016/j.psychres.2015.12.035
20. Bassili JN. Emotion recognition: the role of facial movement and the relative importance of upper and lower areas of the face. J Pers Soc Psychol. (1979) 37:2049–58. doi: 10.1037/0022-3514.37.11.2049
21. Kret ME, Gelder de B. Islamic headdress influences how emotion is recognized from the eyes. Front Psychol. (2012) 3:110. doi: 10.3389/fpsyg.2012.00110
22. Gori M, Schiatti L, Amadeo MB. Masking emotions: face masks impair how we read emotions. Front Psychol. (2021) 12:1541. doi: 10.3389/fpsyg.2021.669432
23. Blais C, Roy C, Fiset D, Arguin M, Gosselin F. The eyes are not the window to basic emotions. Neuropsychologia. (2012) 50:2830–8. doi: 10.1016/j.neuropsychologia.2012.08.010
24. Jack RE, Blais C, Scheepers C, Schyns PG, Caldara R. Cultural confusions show that facial expressions are not universal. Curr Biol. (2009) 19:1543–8. doi: 10.1016/j.cub.2009.07.051
25. Høegh MC, Melle I, Aminoff SR, Olsen SH, Lunding SH, Ueland T, et al. Affective lability and social functioning in severe mental disorders. Eur Arch Psychiatry Clin Neurosci. (2022) 272:873–85. doi: 10.1007/s00406-022-01380-1
26. Coleman JRI, Lester KJ, Keers R, Munafò MR, Breen G, Eley TC, et al. Genome-wide association study of facial emotion recognition in children and association with polygenic risk for mental health disorders. Am J Med Genet B Neuropsychiatr Genet. (2017) 174:701–11. doi: 10.1002/ajmg.b.32558
27. Surguladze SA, Senior C, Young AW, Brébion G, Travis MJ, Phillips ML, et al. Recognition accuracy and response bias to happy and sad facial expressions in patients with major depression. Neuropsychology. (2004) 18:212–8. doi: 10.1037/0894-4105.18.2.212
28. Tripoli G, Quattrone D, Ferraro L, Gayer-Anderson C, La Cascia C, La Barbera D, et al. Facial emotion recognition in psychosis and associations with polygenic risk for schizophrenia: findings from the multi-center EU-GEI case-control study. Schizophr Bull. (2022) 48:1104–14. doi: 10.1093/schbul/sbac022
29. Lysaker PH, Chernov N, Moiseeva T, Sozinova M, Dmitryeva N, Alyoshin V, et al. The association of metacognition with emotion recognition and perspective taking in a Russian sample with psychosis. J Clin Psychol. (2021) 77:1034–44. doi: 10.1002/jclp.23076
30. Gur RC, Sara R, Hagendoorn M, Marom O, Hughett P, Macy L, et al. A method for obtaining 3-dimensional facial expressions and its standardization for use in neurocognitive studies. J Neurosci Methods. (2002) 115:137–43. doi: 10.1016/S0165-0270(02)00006-7
31. Pinkham AE, Sasson NJ, Calkins ME, Richard J, Hughett P, Gur RE, et al. The other-race effect in face processing among African American and Caucasian individuals with schizophrenia. Am J Psychiatry. (2008) 165:639–45. doi: 10.1176/appi.ajp.2007.07101604
32. Carter CS, Barch DM, Ruben G, Raquel G, Pinkham A, Ochsner K. CNTRICS final task selection: social cognitive and affective neuroscience-based measures. Schizophr Bull. (2009) 35:153–62. doi: 10.1093/schbul/sbn157
33. Kohler CG, Turner TH, Gur RE, Gur RC. Recognition of facial emotions in neuropsychiatric disorders. CNS Spectr. (2004) 9:267–74. doi: 10.1017/S1092852900009202
34. Grundmann F, Epstude K, Scheibe S. Face masks reduce emotion-recognition accuracy and perceived closeness. PLoS ONE. (2021) 16:e0249792. doi: 10.1371/journal.pone.0249792
35. Roberson D, Kikutani M, Döge P, Whitaker L, Majid A. Shades of emotion: what the addition of sunglasses or masks to faces reveals about the development of facial expression processing. Cognition. (2012) 125:195–206. doi: 10.1016/j.cognition.2012.06.018
36. Krause FC, Linardatos E, Fresco DM, Moore MT. Facial emotion recognition in major depressive disorder: a meta-analytic review. J Affect Disord. (2021) 293:320–8. doi: 10.1016/j.jad.2021.06.053
37. Eisenbarth H, Alpers GW. Happy mouth and sad eyes: scanning emotional facial expressions. Emotion. (2011) 11:860–5. doi: 10.1037/a0022758
38. Noyes E, Davis JP, Petrov N, Gray KLH, Ritchie KL. The effect of face masks and sunglasses on identity and expression recognition with super-recognizers and typical observers. R Soc open Sci. (2021) 8:201169. doi: 10.1098/rsos.201169
39. Smith ML, Cottrell GW, Gosselin F, Schyns PG. Transmitting and decoding facial expressions. Psychol Sci. (2005) 16:184–9. doi: 10.1111/j.0956-7976.2005.00801.x
40. Wegrzyn M, Vogt M, Kireclioglu B, Schneider J, Kissler J. Mapping the emotional face. How individual face parts contribute to successful emotion recognition. PLoS ONE. (2017) 12:e0177239. doi: 10.1371/journal.pone.0177239
41. Miskowiak KW, Seeberg I, Kjaerstad HL, Burdick KE, Martinez-Aran A, del Mar Bonnin C, et al. Affective cognition in bipolar disorder: s systematic review by the ISBD targeting cognition task force. Bipolar Disord. (2019) 21:686–719. doi: 10.1111/bdi.12834
42. Furlong LS, Rossell SL, Karantonis JA, Cropley VL, Hughes M, Van Rheenen TE, et al. Characterization of facial emotion recognition in bipolar disorder: focus on emotion mislabelling and neutral expressions. J Neuropsychol. (2021) 16:353–72. doi: 10.1111/jnp.12267
43. Rocca CCDA, Van Den Heuvel E, Caetano SC, Lafer B. Facial emotion recognition in bipolar disorder: a critical review. Rev Bras Psiquiatr. (2009) 31:171–80. doi: 10.1590/S1516-44462009000200015
44. Lee SC, Lin GH, Shih CL, Chen KW, Liu CC, Kuo CJ, et al. Error patterns of facial emotion recognition in patients with schizophrenia. J Affect Disord. (2022) 300:441–8. doi: 10.1016/j.jad.2021.12.130
45. Turetsky BI, Kohler CG, Indersmitten T, Bhati MT, Charbonnier D, Gur RC, et al. Facial emotion recognition in schizophrenia: when and why does it go awry? Schizophr Res. (2007) 94:253–63. doi: 10.1016/j.schres.2007.05.001
46. Wynn JK, Lee J, Horan WP, Green MF. Using event related potentials to explore stages of facial affect recognition deficits in schizophrenia. Schizophr Bull. (2008) 34:679–87. doi: 10.1093/schbul/sbn047
47. Kohler CG, Walker JB, Martin EA, Healey KM, Moberg PJ. Facial emotion perception in schizophrenia: a meta-analytic review. Schizophr Bull. (2010) 36:1009–19. doi: 10.1093/schbul/sbn192
48. Duncan J, Gosselin F, Cobarro C, Dugas G, Blais C, Fiset D, et al. Orientations for the successful categorization of facial expressions and their link with facial features. J Vis. (2017) 17:7. doi: 10.1167/17.14.7
49. Herlitz A, Lovén J. Sex differences and the own-gender bias in face recognition: a meta-analytic review. Vis Cogn. (2014) 21:1306–36. doi: 10.1080/13506285.2013.823140
50. Mishra MV, Likitlersuang J, Wilmer B, Cohan J, Germine S, DeGutis L, et al. Gender differences in familiar face recognition and the influence of sociocultural gender inequality. Sci Rep. (2019) 9:17884. doi: 10.1038/s41598-019-54074-5
51. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
52. Wiesmann M, Franz C, Sichtermann T, Minkenberg J, Mathern N, Stockero A, et al. Seeing faces, when faces can't be seen: wearing portrait photos has a positive effect on how patients perceive medical staff when face masks have to be worn. PLoS ONE. (2021) 16:e0251445. doi: 10.1371/journal.pone.0251445
Keywords: COVID-19, emotion recognition, face masks, psychiatric disorders, happiness
Citation: Escelsior A, Amadeo MB, Esposito D, Rosina A, Trabucco A, Inuggi A, Pereira da Silva B, Serafini G, Gori M and Amore M (2022) COVID-19 and psychiatric disorders: The impact of face masks in emotion recognition face masks and emotion recognition in psychiatry. Front. Psychiatry 13:932791. doi: 10.3389/fpsyt.2022.932791
Received: 30 April 2022; Accepted: 26 August 2022;
Published: 27 September 2022.
Edited by:
Marina A. Pavlova, University Hospital Tübingen, GermanyReviewed by:
Paola Ricciardelli, University of Milano-Bicocca, ItalyLamiece Hassan, The University of Manchester, United Kingdom
Copyright © 2022 Escelsior, Amadeo, Esposito, Rosina, Trabucco, Inuggi, Pereira da Silva, Serafini, Gori and Amore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Bianca Amadeo, bWFyaWFiaWFuY2EuYW1hZGVvQGlpdC5pdA==
†These authors share first authorship
 Andrea Escelsior
Andrea Escelsior Maria Bianca Amadeo
Maria Bianca Amadeo Davide Esposito
Davide Esposito Anna Rosina
Anna Rosina Alice Trabucco2
Alice Trabucco2 Alberto Inuggi
Alberto Inuggi Gianluca Serafini
Gianluca Serafini Monica Gori
Monica Gori Mario Amore
Mario Amore