- Department of Applied Social Sciences, The Hong Kong Polytechnic University, Hong Kong, Hong Kong SAR, China
As studies on the mental health status of university students during the COVID-19 pandemic are almost non-existent in Hong Kong, we examined four research questions in this paper: What is the prevalence of depressive symptoms in university students in Hong Kong? What are the socio-demographic correlates of depressive symptoms? Do need satisfaction and positive youth development (PYD) attributes, including beliefs about adversity, psychosocial competence (resilience and emotional competence) and family functioning predict depression? Do PYD attributes moderate the predictive effect of need satisfaction on depression? We examined the above research questions using the Centre for Epidemiologic Studies Depression Scale Revised (CESD-R) in 1,648 university students in Hong Kong. For PYD attributes, we utilized validated measures of Chinese beliefs about adversity, psychosocial competence (resilience and emotional competence), and family functioning. For need satisfaction, we used a measure derived from two focus group interviews involving university students. Results showed that 48.4% of the respondents (95% confidence interval = [45.9%, 51.1%]) scored 16 or above (i.e., “at-risk” for clinical depression). As predicted, age, gender, student status (local vs. international), and family financial hardship were significant socio-demographic correlates of depressive symptoms. Besides, need satisfaction and PYD attributes negatively predicted depression scores. Finally, multiple regression analyses controlling for gender, age, and student status as covariates showed that all PYD attributes moderated the impact of need satisfaction on depression. The findings reinforce the theoretical proposition that PYD attributes serve as important factors in protecting the mental health of university students during the pandemic.
Introduction
The mental health of university students is a growing concern in the global context (1). In particular, researchers have reported that depression is a common problem in university students. For example, Vázquez and Blanco (2) revealed that 33% of Spanish university students were at-risk of moderate and severe depression. In Ghana, Oppong Asante and Andoh-Arthur (3) found that 31.1% of university students showed mild to moderate depression and 8.1% showed severe depression. Similarly, Tao et al. (4) found that 6.1% of Chinese university students reported at least moderate depressive symptoms. In a prospective longitudinal study conducted in China, Song et al. (5) found that 42% of non-depressed Chinese first-year students developed depressive symptoms within 2 years of college study.
COVID-19 has adversely affected the mental health of students because the learning mode has substantially changed under the pandemic (6). Interestingly, while many researchers have conducted studies in different parts of the world to understand the mental health of university students under the pandemic, related studies are almost non-existent in the Hong Kong context. As the mental health of university students might be adversely affected during the “Social Event” taking place in 2019–2020 (7), there is an urgent need to understand the mental health of Hong Kong university students under the pandemic. In this study, we examined several issues based on a large sample of university students in Hong Kong. These issues included the prevalence and socio-demographic correlates of depressive symptoms in university students, predictive effects of need satisfaction, positive youth development (PYD) attributes and family functioning on depression in college students, and the moderating effect of PYD attributes on the influence of need satisfaction on depression.
Literature Review
Prevalence of Depression and Socio-Demographic Correlates of Depression Under COVID-19
According to Shek et al. (8), the COVID-19 pandemic has brought many challenges to university students, such as intrapersonal, interpersonal, academic, and financial adjustments that may lead to increased stress. Obviously, these adjustments within a short time would eventually impair the mental health of university students under the pandemic. There are studies suggesting mental health problems of university students under the pandemic are alarming. Yu et al. (9) showed that 56.8% of Chinese students had moderate or severe levels of depression; Luo et al. (10) showed that 26.0% of Chinese students were at-risk of depression; Truchot et al. (11) showed that 52% of the French female students and 49% of French male students displayed depressive symptoms.
Regarding socio-demographic correlates of depression in university students under COVID-19, researchers have identified several significant correlates. The first correlate is age. Theoretically, with more life experience and better coping abilities (12) as well as resilience (13), older students’ mental health might be better than that of younger students. While many studies supported this hypothesis (14, 15), some studies showed the reverse pattern (16). The second significant demographic correlate is gender. While female college students showed poorer mental health than did male college students under the pandemic (17–19), male students showed more psychological symptoms than did female students (20). A recent meta-analysis also showed mixed findings (1).
The third factor is whether the student comes from abroad. Research generally showed that international students experienced many mental health problems during the pandemic (21) and their mental health was poorer than domestic students (22). Nevertheless, the picture may be different in Hong Kong. Cheung et al. (23) showed that some local students displayed high levels of depression while international students had the lowest level of depression. Furthermore, as the experience of social unrest preceding the pandemic may have already resulted in a deterioration in university students’ mental health (7, 20), the COVID-19 pandemic might further impair the mental health of university students (20, 24).
Finally, college students’ financial distress was significantly associated with anxiety, stress, depression, or post-traumatic stress symptoms [e.g., (25)]. As the pandemic creates a visible financial hardship for people, findings from different places (26, 27) showed that university students experiencing economic hardship had poorer mental health as compared to those without economic disadvantage.
Need Satisfaction and Positive Youth Development Attributes as Predictors of Depression
Self-determination theory maintains that satisfaction of one’s needs in different aspects (e.g., personal development and social interactions) leads to better adjustment such that need satisfaction results in better mental health while need frustration leads to more mental health problems such as depression (28). There are studies showing need satisfaction was positively related to student mental health (29–31). During the pandemic, university students’ need satisfaction may be threatened due to the interruption of a “normal life” resulting from social distancing measures and other sudden changes in life mode, which may in turn negatively affect their mental health. Hence, besides satisfaction with “basic psychological needs,” we should examine how satisfaction of needs in different life domains would be related to the mental health of university students under the pandemic.
Besides need satisfaction, there are other psychosocial predictors of student mental health under the pandemic. According to the positive youth development (PYD) framework (32), developmental assets such as good family support (33) and attributes including resilience, emotional competence, and optimism (34) are commonly regarded as protective factors of mental health (32). In the present study, we focused on three PYD attributes, including beliefs about adversity, psychosocial competence (resilience and emotional competence), and family functioning. These attributes represent students’ internal as well as external assets that may help them to cope with stressful situations such as the pandemic.
The first PYD attribute is “belief about adversity” that reflects one’s spiritual and positive beliefs about the future when experiencing hardship. Theoretically, holding positive meaning about adversity and positive life orientation can help one cope with stress arising from adversity, including the COVID-19 pandemic (9, 35). The second PYD attribute is “psychosocial competence,” which is operationally defined by resilience and emotional competence in the present study. For resilience, it has been found to be negatively associated with university students’ depression and anxiety during the COVID-19 pandemic (36). Emotional competence also showed a protective role in the context of the COVID-19 pandemic (37, 38). Besides “internal assets” indexed by resilience and psychosocial competence, “external asset” defined by family functioning also protects individual family members (39). There are research findings showing that family functioning was positively related to the mental health of young people under the pandemic (40–42).
Moderating Effect of Positive Youth Development Attributes
Besides the main effects of the above-mentioned PYD attributes on students’ mental health, PYD attributes may also buffer the negative influence of risk factors (43), including the lack of need satisfaction considered in the present study. There are studies showing significant moderating effect of PYD attributes on the association between risk factors (e.g., stress) and depression (40, 44). Some studies also showed that positive beliefs, such as optimism and meaning-centered coping (e.g., maintenance of hope), mitigated the impacts of COVID-related stress on individuals’ depressive symptoms (45, 46). Nevertheless, there are also studies showing insignificant findings (47, 48) or mixed findings on the moderating effect of PYD attributes on adolescent mental health (49). The inconclusive findings thus call for further exploration of this important issue.
The Present Study
We asked the following research questions in this study:
Research Question 1: What is the prevalence of depression amongst university students in Hong Kong?
Research Question 2: What are the socio-demographic correlates of depressive symptoms in university students?
• Based on the previous studies that older students showed better coping and resilience than did younger students, we proposed that there would be a negative relationship between age and the level of depressive symptoms (Hypothesis 1a).
• Regarding gender as a correlate, as the findings are inconclusive, we put forward two competing hypotheses: female university students would show a higher level of depression than male university students (Hypothesis 1b-x); male university students would show a higher level of depression than female university students (Hypothesis 1b-y).
• Regarding student status, because there are conflicting findings, we proposed two alternative hypotheses: international students would show a higher level of depression than local students (Hypothesis 1c-x); local students would show more depressive symptoms than international students (Hypothesis 1c-y).
• Based on the existing theoretical frameworks and previous studies, we hypothesized that students experiencing financial difficulty would have a higher level of depression compared to those without such experience (Hypothesis 1d).
Research Question 3: What is the relationship between need satisfaction and depressive symptoms among university students in Hong Kong? With reference to Shek et al. (8) we expected that there would be a negative relationship between these two domains (Hypothesis 2).
Research Question 4: Are PYD attributes related to depressive symptoms? Based on the general thesis that PYD attributes promote youth development, we expected that there would be negative relationships between PYD attributes (positive beliefs about adversity, psychosocial competence, and family functioning) and depressive symptoms (Hypotheses 3a, 3b, and 3c, respectively).
Research Question 5: Do the three PYD attributes moderate the impact of need satisfaction on depression? As PYD attributes are protective factors, we hypothesized that these three PYD attributes would moderate the negative relationship between need satisfaction and depressive symptoms (Hypotheses 4a, 4b, and 4c, respectively).
Methods
To understand the mental health of university students under the pandemic, we conducted an online survey in the 2020/21 academic year using different measures of mental health (e.g., depression, anxiety, and post-traumatic stress disorder) to examine prevalence rates as well as related socio-demographic correlates. We also examined the risk factors (e.g., stressors in different domains) and protective factors (e.g., positive beliefs about adversity, resilience, emotional management, and family functioning) of student mental health. In this paper, we cover the prevalence of depressive symptoms as well as related socio-demographic correlates in university students in Hong Kong. Besides, we examined the main effect of need satisfaction and PYD attributes and the moderating effect of PYD attributes on the influence of need satisfaction on depressive symptoms.
Participants and Procedures
We collected data via an online student survey from January 2021 to the end of March 2021, during which the fourth pandemic of COVID-19 in Hong Kong took place. Undergraduate students from one university participated in the study. Although it is desirable to recruit students via random sampling strategies, we were not able to do so in this study for two reasons. First, because of the “work from home” arrangement, it was not easy to get the complete student population list. Second, it was difficult to invite students to join this study via email because their email accounts were flooded with emails during the pandemic. Hence, we recruited participants via quota sampling using faculty and study year to form different categories. Actually, many studies used quota sampling in COVID-19 studies (50–52).
Because of the social distancing requirement, we conducted the online survey via Qualtrics XM. Online surveys have the advantage of flexibility, and they can also motivate participants to disclose information that would not be disclosed under other forms of survey (53, 54). In the online questionnaire, participants first read the information about the study as well as the confidentiality, anonymity, and participants’ rights of the study. If a participant agreed to join after understanding the above information, he/she checked “Yes, I consent to participate in the captioned research.” As an appreciation of their participation, students received a supermarket voucher for successful completion of the survey (HK$100 = roughly US$12.82).
A total of 2,050 students indicated their interest to join the study and 2,017 students met the inclusion criteria (e.g., being an undergraduate student) and gave their consent to join the study. As a measure of quality assurance, we inserted two “attention checking” questions in the questionnaire [e.g., (55, 56)]. In these two questions, we invited the respondents to choose a response option (e.g., “This is an attention check, please choose ‘exactly true”’). Eventually, we excluded 369 cases showing careless responses, with 1,648 students in the final sample.
Instruments
Centre for Epidemiologic Studies Depression Scale Revised
The Centre for Epidemiologic Studies Depression Scale Revised (CESD-R) is a 20-item assessment tool measuring depressive symptoms based on Major Depressive Disorder listed in the DSM-V criteria (57). The original version was developed by Radloff (58). These symptoms include sadness (e.g., “I felt depressed”), anhedonia (e.g., “Nothing made me happy”), appetite problem (e.g., “My appetite was poor”), sleep problem (e.g., “I slept much more than usual”), concentration (e.g., “I could not focus on the important things”), and worthlessness (e.g., “I do not like myself”). There are also items assessing fatigue (e.g., “I was tired all the time”), agitation (e.g., I felt like I was moving too slowly”), and suicidal ideation (e.g., “I wished I were dead”). For each item, respondents were asked to rate their experience in the past week on a five-point scale (“0 = Not at all or less than 1 day in the last week; 1 = 1–2 days in the last week, 2 = 3–4 days in the last week, 3 = 5–7 days in the last week; 4 = nearly every day for the last 2 weeks”). We calculated and interpreted the scale scores according to the instructions on the official website.1 There is support for the psychometric properties of the CES-D in the Chinese context (59, 60). The CESD-R was also validated in Chinese samples (61, 62). In the present study, the CESD-R was internally consistent (alpha = 0.96).
Need Satisfaction During the Pandemic Scale
To understand the specific needs of university students in Hong Kong, we conducted two focus groups for 22 undergraduate students to facilitate the development of the online questionnaire. Based on the findings, needs in several areas emerged from the findings, including physical needs (e.g., keep physical fitness), psychological needs (e.g., keep good emotional health), social needs (e.g., go out with friends), familial needs (e.g., maintain harmony in family) and academic needs (e.g., have effective online learning strategy). Based on the qualitative data, we developed 15 items. In each item, we asked the respondents how well their needs were met in the past year on a six-point scale (“1 = Not met at all; 6 = Fully met”). Reliability analysis showed that the scale is internally consistent (alpha = 0.89).
Chinese Cultural Beliefs About Adversity Scale
We used the Chinese Cultural Beliefs about Adversity Scale designed by Shek et al. (63). There are nine items based on traditional Chinese cultural beliefs (e.g., “hardship increases stature”; “when there is a will, there is a way”). To avoid misunderstanding of the items, in addition to the English version, the original Chinese version was also given for reference. Respondents were required to indicate the degree of agreement on each item by using a 6-point Likert scale (“1 = Strongly disagree, 6 = Strongly agree”). Shek et al. (63) showed that the scale scores were related to measures of psychological well-being. In this study, we found that this scale was reliable (alpha = 0.73).
The Chinese Positive Youth Development Scale
We used two subscales in Chinese Positive Youth Development Scale (CPYDS) to assess psychosocial competence, including resilience and emotional competence (64). There are three items in the resilience subscale (e.g., “I would not give up easily even in face of difficulties”) and three items in the emotional competence subscale (e.g., “I know how to ventilate my emotions appropriately in times of distress”). Respondents were required to indicate their level of agreement on the six items on a 6-point Likert scale ranging from “1” (Strongly disagree) to “6” (Strongly agree). The resilience and emotional competence subscales showed acceptable internal consistency (alpha = 0.78 and 0.81, respectively). We computed the mean score of these two subscales to indicate the construct of “psychosocial competence” (alpha = 0.86).
The Chinese Family Assessment Instrument
We used the 9-item Chinese Family Assessment Instrument (C-FAI) to assess family functioning in this study (65), including three items on family communication (e.g., “Parents often talk to their children”), three items on mutuality (e.g., “Family members love each other”) and three items on conflict (e.g., “There is no mutual concern among family members”). We asked the respondents to indicate their level of agreement with each statement on a 5-point Likert scale ranging from “1” (Very unlike my family) to “5” (Very like my family). This 9-item measure shows good reliability in this study (alpha = 0.77).
Results
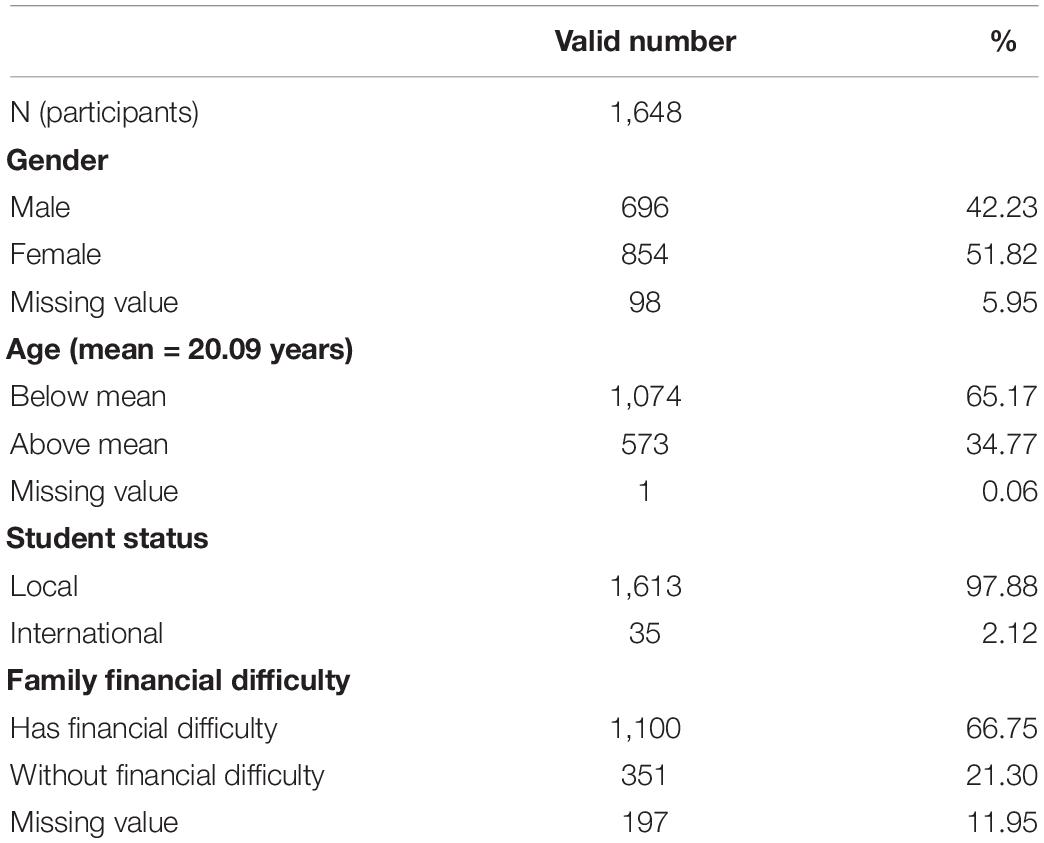
The mean age of the final sample (N = 1,648) was 20.09 years, with 696 (42.23%) male students and 854 (51.82%) female students. The remaining 98 (5.95%) participants did not indicate their gender in the questionnaire. Most of the students (N = 1,613; 97.88%) were local students and 35 (2.12%) were international students, mainly from mainland China and Malaysia. Some students (N = 351; 21.3%) indicated that their families experienced financial hardship at the time they completed the survey. Tables 1, 2 show the demographic characteristics of the sample and the descriptive statistics of the variables of the study, respectively.
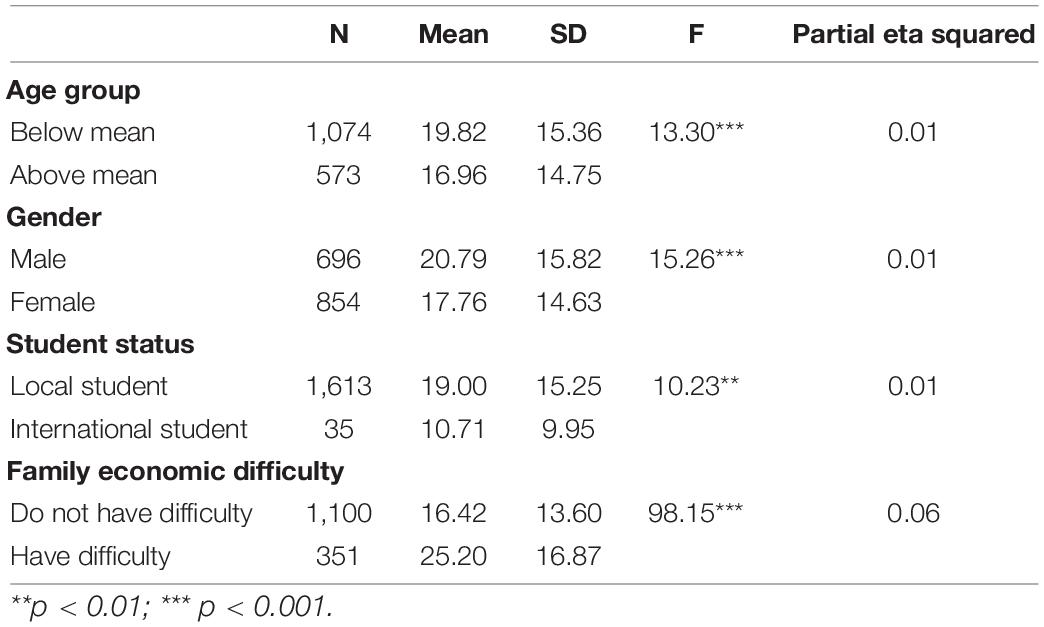
Among the 1,648 participants, 48.4% (95% CI = [45.9%, 51.1%]) scored 16 or higher in CESD-R (i.e., at-risk for clinical depression). Regarding the socio-demographic correlates of depressive symptoms (Table 3), younger participants (M = 19.82, SD = 15.36) scored higher depression scores than did older participants (M = 16.96, SD = 14.75; F = 13.30, p < 0.001, η2p = 0.01), providing support for Hypothesis 1a. For gender differences in depressive symptoms, male students (M = 20.79, SD = 15.82) displayed a higher level of depressive symptoms than did female students (M = 17.76, SD = 14.63; F = 15.26, p < 0.001, η2p = 0.01), lending support to Hypothesis 1b-y. For differences between international and local students, local Hong Kong students (M = 19.00, SD = 15.25) showed more depressive symptoms than did international students (M = 10.71, SD = 9.95; F = 10.23, p < 0.01, η2p = 0.01), giving support to Hypothesis 1c-y. Finally, supporting Hypothesis 1d, students experiencing financial hardship (M = 25.20, SD = 16.87) showed more depressive symptoms than did students without such an experience (M = 16.42, SD = 13.60; F = 98.15, p < 0.001, η2p = 0.06).
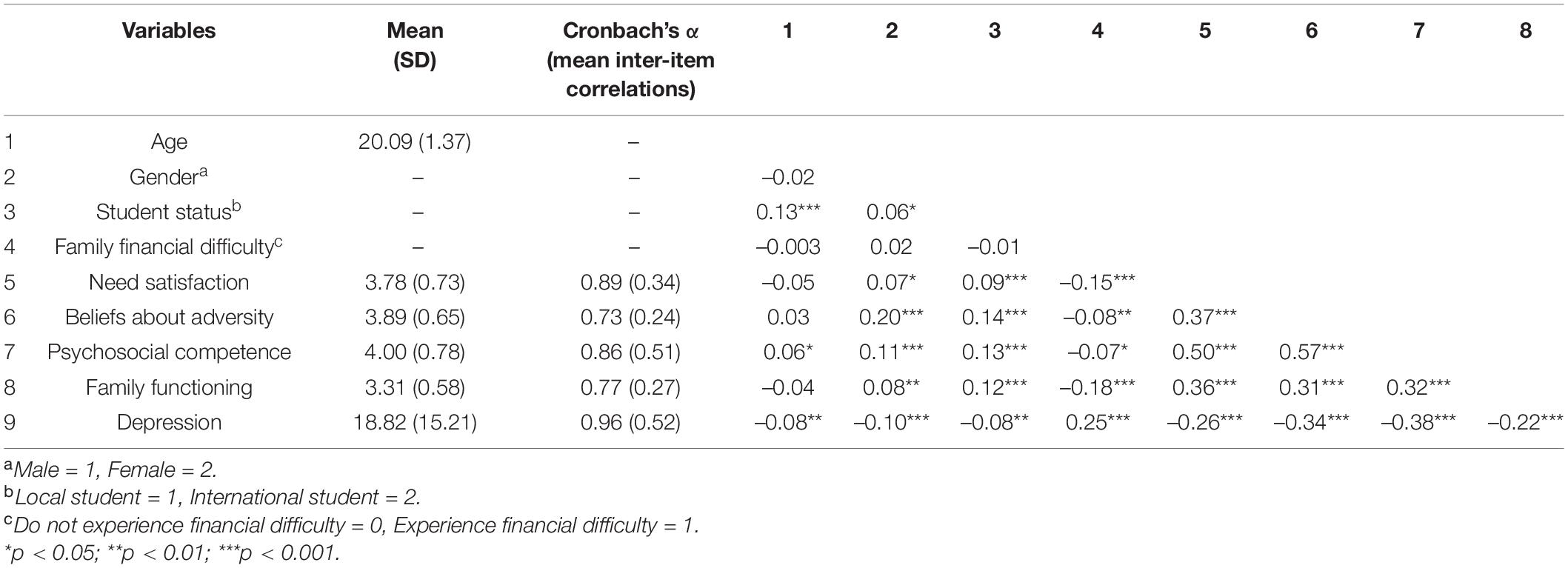
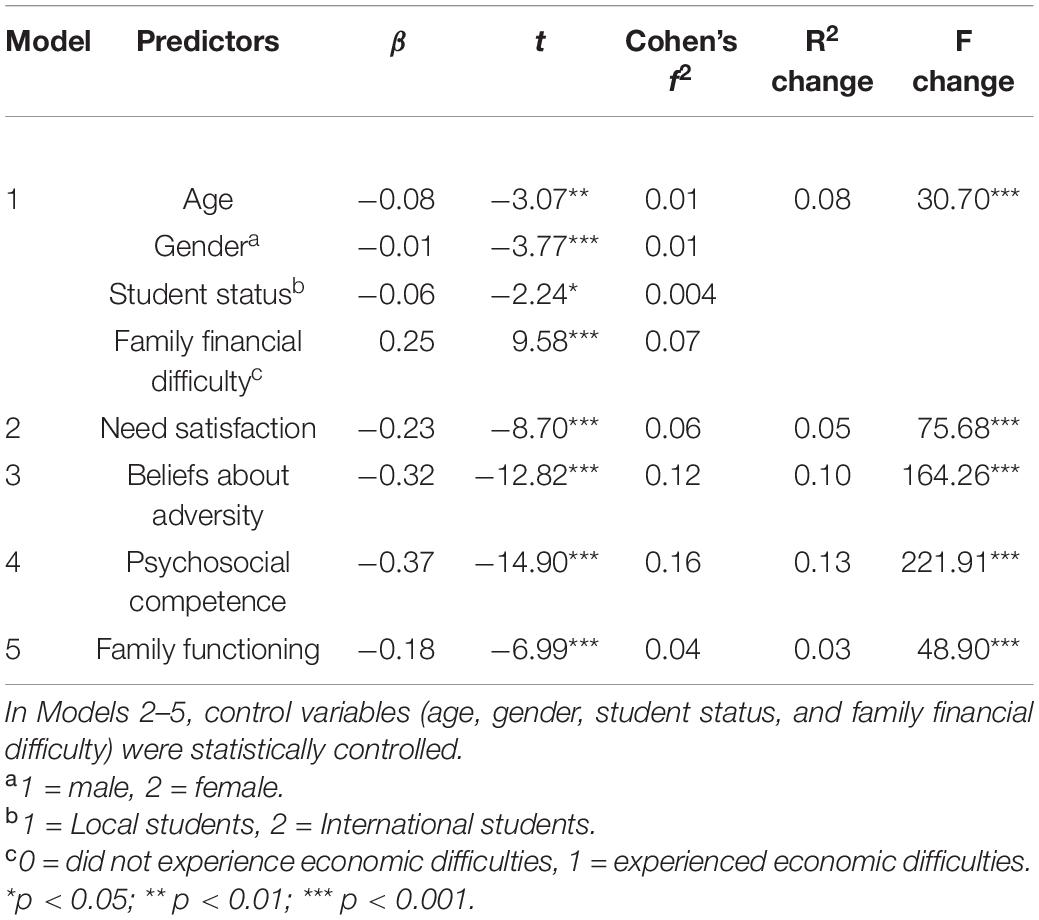
As predicted, need satisfaction, beliefs about adversity, psychosocial competence, and family functioning were negatively related to depression (see Table 2). To understand the predictive effect of these factors on depression, hierarchical multiple regression analyses were conducted with age, gender, student status, and financial difficulty as covariates. In Step 1, all covariates were entered as a block. Then we added each predictor separately in Model 2 to Model 5 (see Table 4). Results showed that these factors predicted depression in the expected direction (Hypothesis 2 and Hypotheses 3a to 3c).
To examine the main and moderating effects of PYD attributes, we conducted three multiple regression analyses (see Table 5). In each model, we examined the effects of need satisfaction and PYD attributes. Findings provided support for the significant main effects of need satisfaction (β = –0.23, p < 0.001, Cohen’s f2 = 0.06) and PYD attributes (β ranged between –0.34 and –0.23, p < 0.001, Cohen’s f2 ranged between 0.01 and 0.11). Results also showed significant interaction effects of need satisfaction and PYD attributes (β ranged between –0.91 and –0.70, p < 0.001, Cohen’s f2 = 0.01). The findings support Hypotheses 4a to 4c.
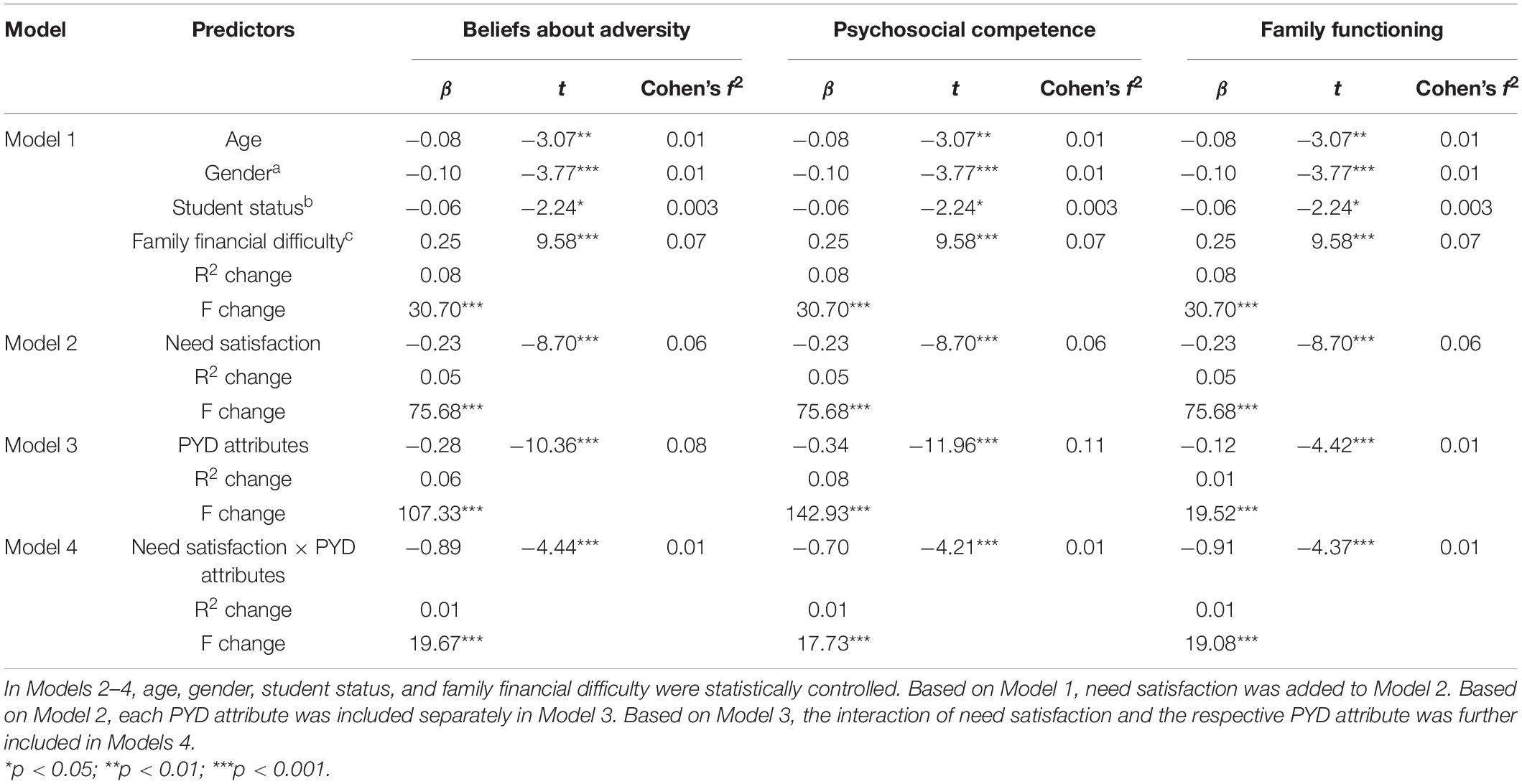
Table 5. The predictive effects of need satisfaction on depression and the moderating effect of three PYD attributes.
To understand the moderating effect of PYD attributes, we conducted simple slope analyses to check the predictive effect of need satisfaction on depression based on participants with high (scored one standard deviation above the mean score) or low (scored one standard deviation below the mean score) level on each PYD attribute. First, need satisfaction showed a significant negative predictive effect on depression among students with more positive beliefs about adversity (B = –4.46, SE = 0.69, p < 0.001, 95% confidence interval (CI) = [–5.82, –3.11]) but not among students with less positive beliefs about adversity (B = –0.76, SE = 0.68, p = 0.26, 95% CI = [–2.09, 0.56]). Second, need satisfaction only served as a negative predictor of depression among students with high psychosocial competence (B = –2.79, SE = 0.69, p < 0.001, 95% CI = [–4.15, –1.44]) but not among students with low psychological competence (B = 0.62, SE = 0.71, p = 0.38, 95% CI = [–0.78, 2.02]). Finally, need satisfaction demonstrated a stronger negative prediction on depression among students with better family functioning (B = –5.95, SE = 0.75, p < 0.001, 95% CI = [–7.42, –4.49]) than among those with poor family functioning (B = –2.03, SE = 0.68, p < 0.01, 95% CI = [–3.36, –0.69]). Figures 1–3 depict the moderating effect of these three PYD attributes.
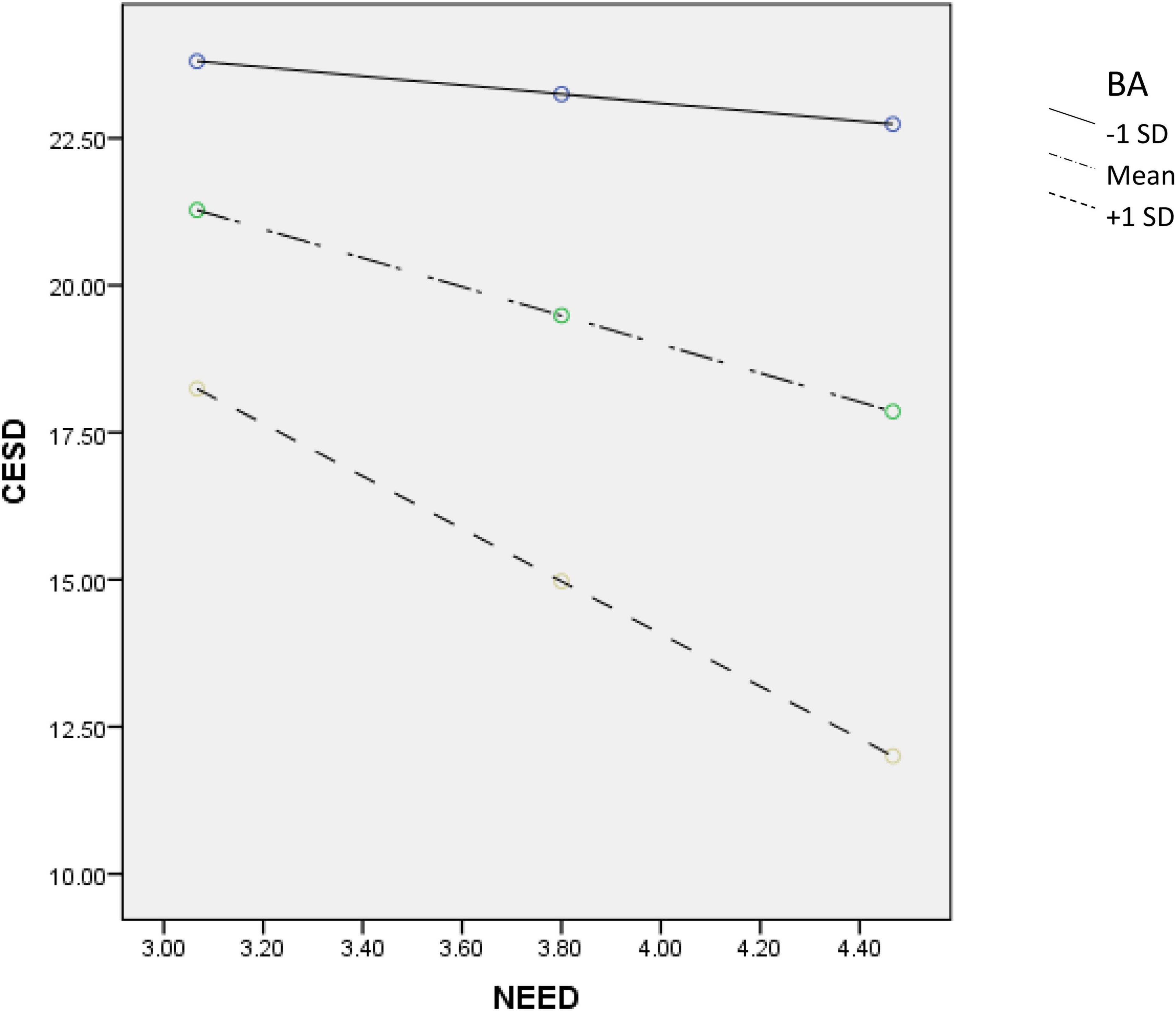
Figure 1. Moderating effect of BA (beliefs about adversity) on the relationship between need satisfaction and depression.
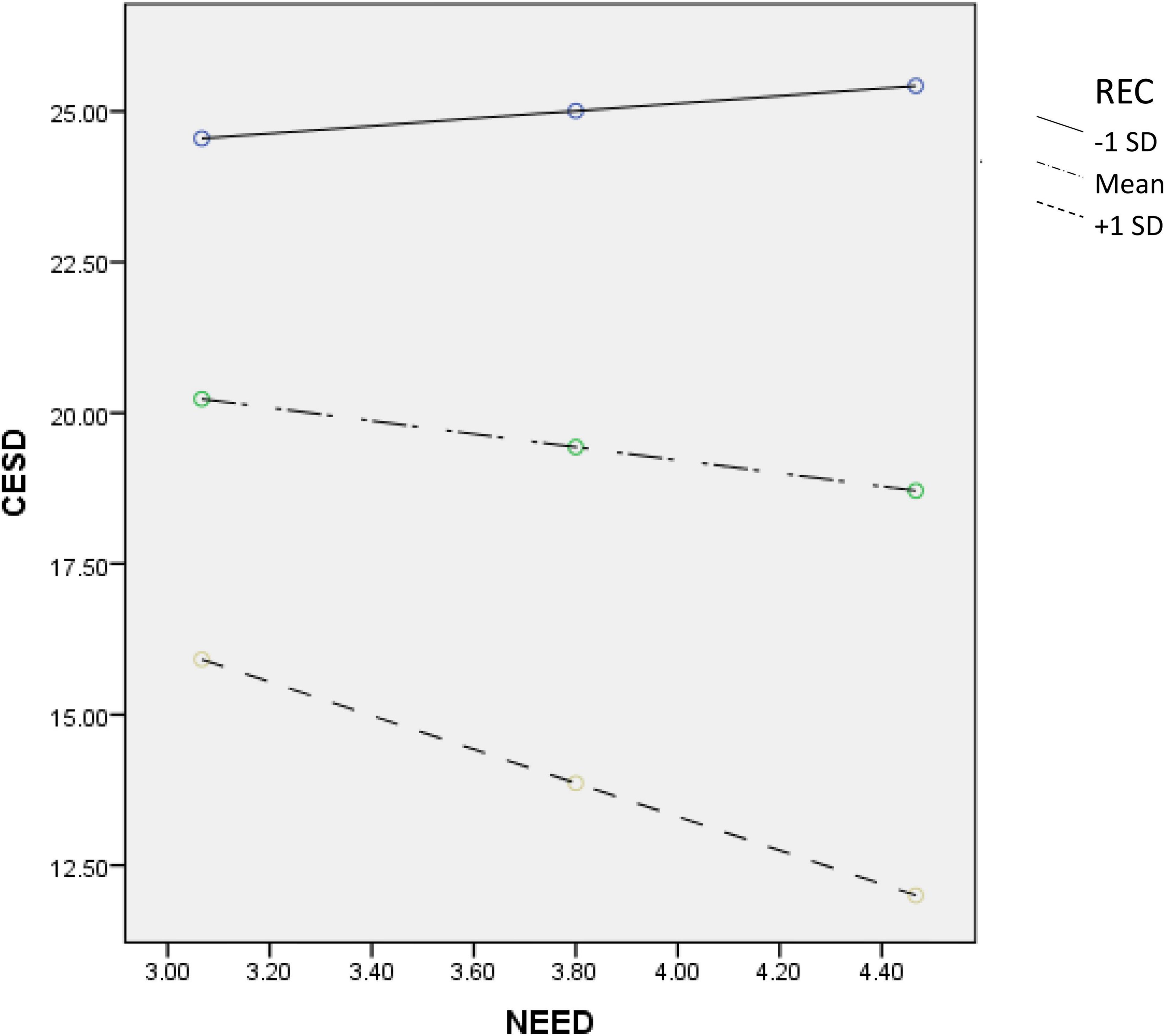
Figure 2. Moderating effect of REC (psychosocial competence) on the relationship between need satisfaction and depression.
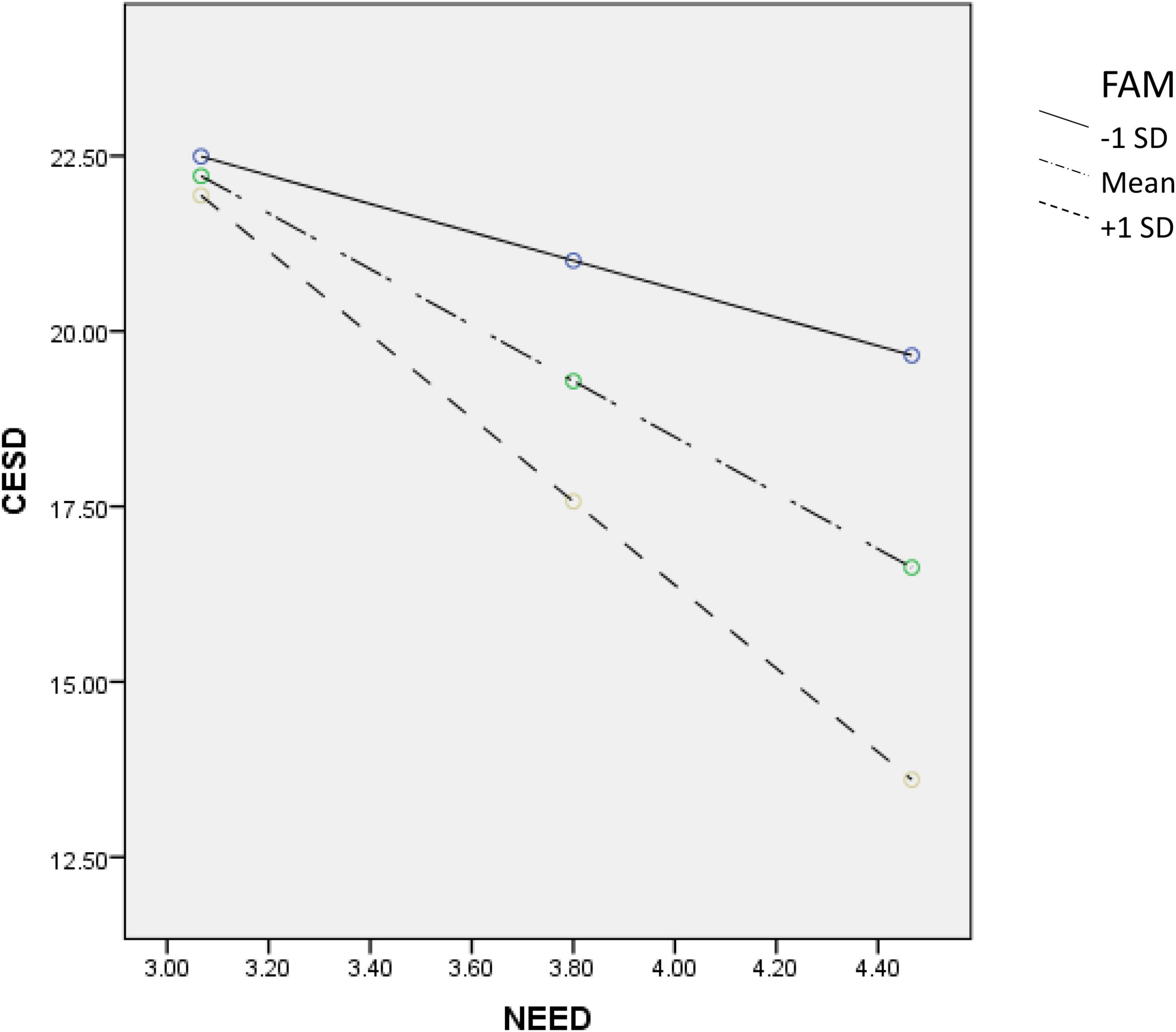
Figure 3. Moderating effect of FAM (family functioning) on the relationship between need satisfaction and depression.
Discussion
With reference to the limitations of the literature, this study has several advances. First, while studies on university students’ mental health have been conducted in mainland China, there are relatively fewer studies in Hong Kong. Second, using the CESD-R, we obtained a picture of depression among university students during the COVID-19 pandemic, which has practical service implications. Third, we identified socio-demographic correlates of depressive symptoms in university students in Hong Kong. Fourth, instead of examining basic psychological need satisfaction, we examined need satisfaction in different life domains during the pandemic. Fifth, we recruited a large sample of students for this study. Sixth, we examined the relationships between PYD attributes and depression in university students, which are not systematically examined in the literature. Finally, the present findings highlighted the moderating role of PYD attributes on the impact of need satisfaction on depressive symptoms.
Regarding Research Question 1, the finding that 48.4% of the respondents were at-risk for clinical depression deserves attention. While the prevalence rate in the present study was similar to those reported in some Western studies during the pandemic [e.g., (66)], it is also lower or higher than the prevalence rates reported previously based on Chinese university students (9, 10). Of course, we should be cautious in interpreting the prevalence rates using the CES-D across different studies because different versions of CES-D, samples, languages, and timing during the pandemic were involved. Nevertheless, the present findings suggest that depression is a common risk amongst university students in Hong Kong during the pandemic that calls for intervention.
For Research Question 2, there are several interesting observations. Consistent with previous findings (67), younger students showed a higher level of depression than old students. This observation can possibly be explained in terms of higher coping abilities amongst the older students (12). Furthermore, young students may not be familiar with the university environment and related facilities, which would contribute to their relatively higher depression level. For gender differences in depression, in contrast to the common finding that female college students showed poorer mental health, we found that male students displayed more depressive symptoms than did female students. Several factors may contribute to this finding (68, 69). First, as Hong Kong is an achievement-oriented society, males experience greater stress than females because males are expected to be successful in the Chinese culture. Second, Chinese men used to suppress their negative emotions. Third, Chinese men also tended not to seek help when encountering problems. Actually, previous studies also showed that males showed poorer mental health as compared to female students (20). Concerning student status, in contrast to the common belief that international students would experience more stress than local students, we found that Hong Kong students showed more depressive symptoms than did international students. There are three possible factors contributing to this observation. First, the mental health problems of university students in Hong Kong have been alarming historically (20). Second, because of social unrest and COVID-19, Hong Kong university students actually experience “cumulative stresses.” Third, Hong Kong people are facing many stressors under COVID-19, such as having stressful online classes because of the tight living space in Hong Kong (8).
Consistent with the literature, financial difficulty is a risk factor for depression among university students. Theoretically, family economic burdens would adversely affect family processes (e.g., family functioning and parenting) which would eventually impair the mental health of children (70). Under COVID-19, because of city lockdown and social distancing measures, the economy is adversely affected. In Hong Kong, financial difficulty is particularly intense for three reasons. First, there is no unemployment benefit in Hong Kong. Hence, unemployment under COVID-19 is a big problem for families in Hong Kong, particularly grass-root families. Although the Government has launched employment protection schemes, only those who are employed are protected. Second, as university students commonly take up part-time jobs and such job opportunities drop under COVID-19, reduced income is a problem for university students. Third, as the cost of living in Hong Kong is very high, financial strain under COVID-19 is particularly painful.
With regard to Research Question 3, we found that need satisfaction was negatively related to depressive symptoms as predicted. As we have pointed out, while there are some studies examining the relationships between “general” or “basic” psychological needs and mental health, we found that satisfaction of “specific” needs was related to mental health in the present study. As the inability to satisfy needs can be regarded as “daily hassles,” the present findings are consistent with the literature that daily hassles were positively related to mental health problems (71, 72). Theoretically, the present findings are in line with the theoretical proposition that satisfaction of basic psychological needs contributes to mental health (73). However, the present findings go beyond to show that need satisfaction with real-life challenges under COVID-19 is related to depression. Practically, university administrators and teachers have to figure out ways to meet the practical needs of the students.
Concerning Research Question 4, we found that PYD attributes indexed by the three measures were negatively related to depressive symptoms. Generally speaking, the findings are in line with the PYD literature demonstrating the protective effects of PYD attributes, including belief about adversity, emotional competence, and family functioning, on adolescents’ overall development (32) and mental health under the COVID-19 (41, 74). These findings are also consistent with the theoretical proposition that developmental assets such as PYD attributes promote holistic youth development such as positive mental health (75).
The first PYD attribute covered in this study is beliefs about adversity. The present finding provides support for the theoretical propositions that hope (76) or life meaning (77) are important factors helping people to adjust to life adversities. A special feature of this study is that we use indigenous Chinese beliefs about adversity that could strengthen the ecological validity of the measure. Obviously, how to remain hopeful and find out meaning in life under COVID-19 is important (78). In particular, the present findings echo the argument that cultural resources could help people to deal with adversity (79, 80).
We covered psychosocial competence as the second PYD attribute in this study. Theoretically, the importance of competence is highlighted in different PYD models (32). Empirically, there are studies showing that psychosocial competence contributes to positive development in young people. For example, in a meta-analysis, Durlak et al. (81) reported that compared to control participants, students joining social-emotional learning programs showed better developmental outcomes. With reference to Hong Kong, studies based on high school students showed that curricular-based PYD programs could promote the development of adolescents (82). In the university context, research findings also showed that credit-bearing subjects utilizing PYD principles were effective in promoting psychosocial competence in students (83, 84). Obviously, as there is much support for the effectiveness of social-emotional learning programs (85), there is a need to “inoculate” university students against the harmful effects of adversity by developing and implementing PYD programs.
Finally, in line with family functioning theories (86), family functioning was negatively associated with depressive symptoms. However, although family functioning is an important factor shaping adolescent development, systematic research work is not rich, particularly in the Chinese context. In fact, one can argue that although COIVD-19 may lead to a drop in “family financial capital,” healthy family functioning can promote “family social capital” that can lead to the healthy development of young people. With particular reference to the Chinese culture, families are strongly emphasized as the core socialization base for children in a family. Nevertheless, there are three common problems within Chinese families. First, family communication is not open as Chinese people believe that “taboo” topics (e.g., parental problems) should not be openly discussed. Second, as Chinese culture emphasizes interpersonal harmony, expression of negative emotions is not commonly encouraged. Third, there are inter-generational differences in viewing family responsibilities. Obviously, it is important to promote family functioning in university students. However, as university students are commonly regarded as “grown-up” individuals, there are very few related programs for them.
As for research question 5, the findings revealed significant moderating effects of PYD attributes in shaping the relationship between students’ need satisfaction and their depression. For students with higher levels of PYD attributes, the negative relationship between need satisfaction and depressive symptoms was stronger than that for those with lower levels of PYD attributes. These findings echo the general theoretical prediction of PYD models that both internal assets (such as emotional competence, resilience, and beliefs about adversity) and external developmental assets (such as family functioning) protect adolescent mental health (32). Overall speaking, the present finding provides support that the theoretical view that a higher level of developmental assets is a protective factor for adolescent development [(87), p. 894].
The finding based on Chinese cultural belief about adversity broadens our understanding of the theoretical mechanisms involved in moderation. Of course, how to promote Chinese beliefs about adversity in Chinese young people when they do not endorse the Chinese culture (7) is an important point for reflection. For psychosocial competence, the present findings reinforce the notion that PYD attributes can be regarded as the “royal road” to optimal development in young people. In addition to resilience and emotional competence covered in this study, it would be exciting to understand how other PYD attributes, such as positive identity and cognitive competence, would contribute to thriving. Finally, the present study enriches the family ecological approach that family functioning is a key in promoting the wellbeing of young people. Obviously, good family functioning constitutes life meaning (e.g., maintaining a happy family and loving each other) and provides hope for an individual. Hence, how to promote family functioning is important during the COVID-19 pandemic, particularly when family members have to spend more time at home because of social distancing measures.
Despite the pioneering nature and the theoretical as well as practical implications of the study, there are several limitations of the study. First, although self-report measures are widely used, it has been criticized for low validity (88). However, Chan (89) argued that these limitations may have been exaggerated, claiming that “these errors may also apply to non-self-report measures” (p. 330), implying the importance of critically assessing the weaknesses (or strengths) of self-report data. Second, the present study is a cross-sectional study. However, cross-sectional studies are useful because they are relatively inexpensive, less time-consuming, and easy to perform (90, 91). Employing a cross-sectional design in this study can provide a “snapshot” of outcomes and features associated with COVID-19 related depressive symptoms and other mental health risk factors among university students at a particular point in time (90). Third, quota sampling instead of stratified random sampling was used in this study. Again, many studies, particularly during the COVID-19 pandemic, use quota sampling approach, with some researchers believing that this sampling method can generate representative samples. As commented by Sharma (92), using quota sampling has certain limitations (e.g., lack of random selection), but it is particularly useful when researchers are not able to get a probability sample but still want to generate a sample that’s “mirrors” the population being researched. Despite these limitations, this study is a pioneering attempt to understand depression in university students and its related socio-demographic correlates, need satisfaction, and PYD attributes in university students in Hong Kong.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (or its Delegate) at the Hong Kong Polytechnic University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DS contributed to all steps of the work. DD and XZ contributed to the project implementation, data interpretation, and revising the work. TW and LT helped draft part of the work. All authors approved the final version of the manuscript.
Funding
This study was financially supported by the University Grants Committee of Hong Kong and Wofoo Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Chang J-J, Ji Y, Li Y-H, Pan H-F, Su P-Y. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J Affect Disord. (2021) 292:242–54.
2. Vázquez FL, Blanco V. Symptoms of depression and related factors among Spanish university students. Psychol Rep. (2006) 99:583–90.
3. Oppong Asante K, Andoh-Arthur J. Prevalence and determinants of depressive symptoms among university students in Ghana. J Affect Disord. (2015) 171:161–6. doi: 10.1016/j.jad.2014.09.025
4. Tao S, Wu X, Yang Y, Tao F. The moderating effect of physical activity in the relation between problematic mobile phone use and depression among university students. J Affect Disord. (2020) 273:167–72. doi: 10.1016/j.jad.2020.04.012
5. Song Y, Liu Z, Chen H, Guo Q, Huang Y. Incidence and risk factors of depressive symptoms in Chinese college students. Neuropsychiatric Dis Treat. (2020) 16:2449–57. doi: 10.2147/ndt.s264775
6. Shek DTL. COVID-19 and quality of life: twelve reflections. Appl Res Qual Life. (2021) 16:1–11. doi: 10.1007/s11482-020-09898-z
7. Shek DTL. Protests in Hong Kong (2019–2020): a perspective based on quality of life and well-being. Appl Res Qual Life. (2020) 15:619–35. doi: 10.1007/s11482-020-09825-2
8. Shek DTL, Dou D, Zhu X. Prevalence and correlates of mental health of university students in Hong Kong: what happened one year after the occurrence of COVID-19? Front Public Health. (in press). doi: 10.3389/fpubh.2022.857147
9. Yu M, Tian F, Cui Q, Wu H. Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatry. (2021) 21:66. doi: 10.1186/s12888-021-03066-9
10. Luo W, Zhong B-L, Chiu HF-K. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol Psychiatric Sci. (2021) 30:e31. doi: 10.1017/S2045796021000202
11. Truchot D, Andela M, Takhiart H. Stressors met by quarantined French students during the covid-19 pandemic. Their links with depression and sleep disorders. J Affect Disord. (2021) 294:54–9. doi: 10.1016/j.jad.2021.06.059
12. Babicka-Wirkus A, Wirkus L, Stasiak K, Kozłowski P. University students’ strategies of coping with stress during the coronavirus pandemic: data from Poland. PLoS One. (2021) 16:e0255041. doi: 10.1371/journal.pone.0255041
13. Sánchez-Teruel D, Robles-Bello MA, Valencia-Naranjo N. Do psychological strengths protect college students confined by COVID-19 to emotional distress? The role of gender. Pers Individ Differ. (2021) 171:110507. doi: 10.1016/j.paid.2020.110507
14. AlHadi AN, Alhuwaydi AM. The mental health impact of pandemic COVID-19 crisis on university students in Saudi Arabia and associated factors. J Am College Health. (2021):1–9. [Online ahead of print], doi: 10.1080/07448481.2021.1947839
15. Debowska A, Horeczy B, Boduszek D, Dolinski D. A repeated cross-sectional survey assessing university students’ stress, depression, anxiety, and suicidality in the early stages of the COVID-19 pandemic in Poland. Psychol Med. (2020):1–4. [Online ahead of print], doi: 10.1017/S003329172000392X
16. Lukács A. Mental well-being of university students in social isolation. Eur J Health Psychol. (2021) 28:22–9. doi: 10.1027/2512-8442/a000065
17. Cam HH, Ustuner Top F, Kuzlu Ayyildiz T. Impact of the COVID-19 pandemic on mental health and health-related quality of life among university students in Turkey. Curr Psychol. (2022) 41:1033–42. doi: 10.1007/s12144-021-01674-y
18. Fruehwirth JC, Biswas S, Perreira KM. The Covid-19 pandemic and mental health of first-year college students: examining the effect of Covid-19 stressors using longitudinal data. PLoS One. (2021) 16:e0247999. doi: 10.1371/journal.pone.0247999
19. Li Y, Wang A, Wu Y, Han N, Huang H. Impact of the COVID-19 pandemic on the mental health of college students: a systematic review and meta-analysis. Front Psychol. (2021) 12:669119. doi: 10.3389/fpsyg.2021.669119
20. Li X, Shek DTL, Shek EYW. Psychological morbidity among university students in Hong Kong (2014–2018): psychometric properties of the Depression Anxiety Stress Scales (DASS) and related correlates. Int J Environ Res Public Health. (2021) 18:8305. doi: 10.3390/ijerph18168305
21. Maleku A, Kim YK, Kirsch J, Um MY, Haran H, Yu M, et al. The hidden minority: discrimination and mental health among international students in the US during the COVID-19 pandemic. Health Soc Care Commun. (2021):1–14. [Online ahead of print], doi: 10.1111/hsc.13683
22. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. (2021) 301:113863. doi: 10.1016/j.psychres.2021.113863
23. Cheung DK, Tam DKY, Tsang MH, Zhang DLW, Lit DSW. Depression, anxiety and stress in different subgroups of first-year university students from 4-year cohort data. J Affect Disord. (2020) 274:305–14. doi: 10.1016/j.jad.2020.05.041
24. Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. (2020) 17:3740. doi: 10.3390/ijerph17103740
25. Oh H, Marinovich C, Rajkumar R, Besecker M, Zhou S, Jacob L, et al. COVID-19 dimensions are related to depression and anxiety among US college students: findings from the Healthy Minds Survey 2020. J Affect Disord. (2021) 292:270–5. doi: 10.1016/j.jad.2021.05.121
26. Galanza MAMC, Aruta JJBR, Mateo NJ, Resurreccion RR, Bernardo ABI. Mental health of Filipino university students during the COVID-19 pandemic: the distinct associations of fear of COVID-19 and financial difficulties. Educ Dev Psychol. (2021):1–6. doi: 10.1080/20590776.2021.1999168 [Epub ahead of print].
27. Solomou I, Constantinidou F, Karekla M, Psaltis C, Chatzittofis A. The COVID-19 international student well-being study (C-19 ISWS). Eur J Psychol Open. (2021) 80:99–110. doi: 10.1024/2673-8627/a000014
28. Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psychol. (2008) 49:182–5. doi: 10.1037/a0012801
29. Dasinger TM, Gibson DJ. Perceptions of mental health and need satisfaction/frustration among rural university students. J Am College Health. (2022):1–8. [Online ahead of print], doi: 10.1080/07448481.2022.2032089
30. Levine SL, Andrade G, Koestner R. A not so perfect plan: an examination of the differential influence of multidimensional perfectionism on missed and gained events during the COVID-19 pandemic. Pers Individ Differ. (2022) 184:111214. doi: 10.1016/j.paid.2021.111214
31. Teuber Z, Jia H, Niewöhner T. Satisfying students’ psychological needs during the COVID-19 outbreak in German higher education institutions [Original Research]. Front Educ. (2021) 6:679695. doi: 10.3389/feduc.2021.679695
32. Shek DTL, Dou D, Zhu X, Chai W. Positive youth development: current perspectives. Adolescent Health Med Ther. (2019) 10:131–41. doi: 10.2147/ahmt.s179946
33. Benson PL. All Kids Are Our Kids: What Communities Must Do to Raise Caring and Responsible Children and Adolescents. Hoboken, NJ: Jossey-Bass (1997).
34. Catalano RF, Berglund ML, Ryan JAM, Lonczak HS, Hawkins JD. Positive youth development in the United States: research findings on evaluations of positive youth development programs. Ann Am Acad Polit Soc Sci. (2004) 591:98–124. doi: 10.1177/0002716203260102
35. Wen F-F, Zhu J-L, Ye H-X, Li L-Y, Ma Z, Wen X-X, et al. Associations between insecurity and stress among Chinese university students: the mediating effects of hope and self-efficacy. J Affect Disord. (2021) 281:447–53. doi: 10.1016/j.jad.2020.12.047
36. Tam CC, Ye Z, Wang Y, Li X, Lin D. Self-care behaviors, drinking, and smoking to cope with psychological distress during COVID-19 among Chinese college students: the role of resilience. Psychol Health. (2021):1–20. [Online ahead of print], doi: 10.1080/08870446.2021.2007913
37. Panayiotou G, Panteli M, Leonidou C. Coping with the invisible enemy: the role of emotion regulation and awareness in quality of life during the COVID-19 pandemic. J Contextual Behav Sci. (2021) 19:17–27. doi: 10.1016/j.jcbs.2020.11.002
38. Zhang Y-T, Li R-T, Sun X-J, Peng M, Li X. Social media exposure, psychological distress, emotion regulation, and depression during the COVID-19 outbreak in community samples in China [Original Research]. Front Psychiatry. (2021) 12:644899. doi: 10.3389/fpsyt.2021.644899
39. Shek DTL, Ma CMS. The Chinese family assessment instrument (C-FAI): hierarchical confirmatory factor analyses and factorial invariance. Res Soc Work Pract. (2010) 20:112–23. doi: 10.1177/1049731509355145
40. Green ZA, Faizi F, Jalal R, Zadran Z. Emotional support received moderates academic stress and mental well-being in a sample of Afghan university students amid COVID-19. Int J Soc Psychiatry. (2021):207640211057729. [Online ahead of print], doi: 10.1177/00207640211057729
41. Wu Z, Zou Z, Wang F, Xiang Z, Zhu M, Long Y, et al. Family functioning as a moderator in the relation between perceived stress and psychotic-like experiences among adolescents during COVID-19. Comprehensive Psychiatry. (2021) 111:152274. doi: 10.1016/j.comppsych.2021.152274
42. Zhu X, Chu CKM, Lam YC. The predictive effects of family and individual Wellbeing on University students’ online learning during the COVID-19 pandemic. Front Psychol. (2022) 13:898171. doi: 10.3389/fpsyg.2022.898171
43. Shek DTL, Zhao L, Dou D, Zhu X, Xiao C. The impact of positive youth development attributes on posttraumatic stress disorder symptoms among Chinese adolescents under COVID-19 [Article]. J Adolescent Health. (2021) 68:676–82. doi: 10.1016/j.jadohealth.2021.01.011
44. Havnen A, Anyan F, Hjemdal O, Solem S, Gurigard Riksfjord M, Hagen K. Resilience moderates negative outcome from stress during the COVID-19 pandemic: a moderated-mediation approach. Int J Environ Res Public Health. (2020) 17:6461. doi: 10.3390/ijerph17186461
45. Eisenbeck N, Carreno DF, Pérez-Escobar JA. Meaning-centered coping in the era of COVID-19: direct and moderating effects on depression, anxiety, and stress [Original Research]. Front Psychol. (2021) 12:648383. doi: 10.3389/fpsyg.2021.648383
46. Hou L, Long F, Meng Y, Cheng X, Zhang W, Zhou R. The relationship between quarantine length and negative affect during the COVID-19 epidemic among the general population in China: the roles of negative cognition and protective factors. Front Psychol. (2021) 12:575684. doi: 10.3389/fpsyg.2021.575684
47. Kubo T, Sugawara D, Masuyama A. The effect of ego-resiliency and COVID-19-related stress on mental health among the Japanese population. Pers Individ Differ. (2021) 175:110702. doi: 10.1016/j.paid.2021.110702
48. Kuhlman KR, Straka K, Mousavi Z, Tran M-L, Rodgers E. Predictors of adolescent resilience during the COVID-19 pandemic: cognitive reappraisal and humor. J Adolescent Health. (2021) 69:729–36. doi: 10.1016/j.jadohealth.2021.07.006
49. Traunmüller C, Stefitz R, Schneider M, Schwerdtfeger A. Resilience moderates the relationship between the psychological impact of COVID-19 and anxiety. Psychol Health Med. (2021):1–12. [Online ahead of print], doi: 10.1080/13548506.2021.1955137
50. Helmina SN, Linawati H, Nisa H. Pengetahuan dan motivasi kepatuhan protokol kesehatan Covid-19: survei online pada Mahasiswa Jawa Timur. Buletin Penelitian Kesehatan. (2021) 49:71–80. doi: 10.22435/bpk.v49i2.4214
51. Krok D, Zarzycka B. Risk perception of COVID-19, meaning-based resources and psychological well-being amongst healthcare personnel: the mediating role of coping. J Clin Med. (2020) 9:3225. doi: 10.3390/jcm9103225
52. Nomura S, Eguchi A, Yoneoka D, Kawashima T, Tanoue Y, Murakami M, et al. Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: a large cross-sectional national survey. Lancet Regional Health Western Pacific. (2021) 14:100223. doi: 10.1016/j.lanwpc.2021.100223
53. Campos JADB, Zucoloto ML, Bonafé FSS, Jordani PC, Maroco J. Reliability and validity of self-reported burnout in college students: a cross randomized comparison of paper-and-pencil vs. online administration. Comput Hum Behav. (2011) 27:1875–83. doi: 10.1016/j.chb.2011.04.011
54. Kim HS, Hodgins DC. Reliability and validity of data obtained from alcohol, cannabis, and gambling populations on Amazon’s Mechanical Turk. Psychol Addict Behav. (2017) 31:85–94. doi: 10.1037/adb0000219
55. Al-Salom P, Miller CJ. The problem with online data collection: predicting invalid responding in undergraduate samples. Curr Psychol. (2019) 38:1258–64. doi: 10.1007/s12144-017-9674-9
56. Aust F, Diedenhofen B, Ullrich S, Musch J. Seriousness checks are useful to improve data validity in online research. Behav Res Methods. (2013) 45:527–35. doi: 10.3758/s13428-012-0265-2
57. Eaton WW, Ybarra M, Schwab J. The CESD-R is available on the web. Psychiatry Res. (2012) 196:161. doi: 10.1016/j.psychres.2011.08.018
58. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
59. Dou D, Shek DTL, Zhu X, Zhao L. Dimensionality of the Chinese CES-D: is it stable across gender, time, and samples? Int J Environ Res Public Health. (2021) 18:11818. doi: 10.3390/ijerph182211818
60. Zhu X, Shek DTL, Dou D. Factor structure of the Chinese CES-D and invariance analyses across gender and over time among Chinese adolescents. J Affect Disord. (2021) 295:639–46. doi: 10.1016/j.jad.2021.08.122
61. Ip P, Chim D, Chan KL, Li TMH, Ho FKW, Van Voorhees BW, et al. Effectiveness of a culturally attuned Internet-based depression prevention program for Chinese adolescents: a randomized controlled trial. Depression Anxiety. (2016) 33:1123–31. doi: 10.1002/da.22554
62. Li J, Zhao F, Bai H, Lin P, Shao D, Sun J, et al. Psychometric properties of the Chinese version of the center for epidemiologic studies depression scale-revised in patients with cancer: a cross-sectional study. Int J Nurs Stud. (2019) 97:14–20. doi: 10.1016/j.ijnurstu.2019.04.008
63. Shek DTL, Tang V, Lam CM, Lam MC, Tsoi KW, Tsang KM. The relationship between chinese cultural beliefs about adversity and psychological adjustment in Chinese families with economic disadvantage. Am J Fam Ther. (2003) 31:427–43. doi: 10.1080/01926180390228955
64. Shek DTL, Siu AMH, Lee TY. The Chinese positive youth development scale:a validation study. Res Soc Work Pract. (2007) 17:380–91. doi: 10.1177/1049731506296196
65. Shek DTL. Assessment of family functioning in chinese adolescents: the chinese family assessment instrument. In: NN Singh, TH Ollendick, AN Singh editors. International Perspectives on Child and Adolescent Mental Health. Vol. 2. Amsterdam: Elsevier (2002). p. 297–316.
66. Giuntella O, Hyde K, Saccardo S, Sadoff S. Lifestyle and mental health disruptions during COVID-19. Proc Natl Acad Sci U S A. (2021) 118:e2016632118. doi: 10.1073/pnas.2016632118
67. Horita R, Nishio A, Yamamoto M. The effect of remote learning on the mental health of first year university students in Japan. Psychiatry Res. (2021) 295:113561. doi: 10.1016/j.psychres.2020.113561
68. Lo SM, Wong HC, Lam CY, Shek DTL. Common mental health challenges in a university context in Hong Kong: a study based on a review of medical records. Appl Res Qual Life. (2020) 15:207–18. doi: 10.1007/s11482-018-9673-5
69. Lo SM, Wong HC, Lam CY, Shek DTL. An innovative multidisciplinary healthcare model in student mental health: experience in Hong Kong. Appl Res Qual Life. (2021) 16:301–13. doi: 10.1007/s11482-019-09770-9
70. McLoyd VC, Kaplan R, Purtell KM, Bagley E, Hardaway CR, Smalls C. Poverty and socioeconomic disadvantage in adolescence. In: RM Lerner, L Steinberg editors. Handbook of Adolescent Psychology: Contextual Influences on Adolescent Development. Vol. 2. 3rd ed. Hoboken, NJ: John Wiley & Sons, Inc (2009). p. 444–91.
71. Bouteyre E, Maurel M, Bernaud J-L. Daily hassles and depressive symptoms among first year psychology students in France: the role of coping and social support. Stress Health. (2007) 23:93–9. doi: 10.1002/smi.1125
72. Tajalli P, Sobhi A, Ganbaripanah A. The relationship between daily hassles and social support on mental health of university students. Proc Soc Behav Sci. (2010) 5:99–103. doi: 10.1016/j.sbspro.2010.07.058
73. Church AT, Katigbak MS, Locke KD, Zhang H, Shen J, de Jesús Vargas-Flores J, et al. Need satisfaction and well-being:testing self-determination theory in eight cultures. J Cross-Cultural Psychol. (2013) 44:507–34. doi: 10.1177/0022022112466590
74. Krifa I, van Zyl LE, Braham A, Ben Nasr S, Shankland R. Mental health during COVID-19 pandemic: the role of optimism and emotional regulation. Int J Environ Res Public Health. (2022) 19:1413. doi: 10.3390/ijerph19031413
75. Hamilton SF, Hamilton MA, Pittman K. Principles for youth development. In: SF Hamilton, MA Hamilton editors. The Youth Development Handbook: Coming of Age in American Communities. Thousand Oaks, CA: SAGE Publications (2004). p. 3–22.
76. Snyder CR. TARGET ARTICLE: hope theory: rainbows in the mind. Psychol Inquiry. (2002) 13:249–75. doi: 10.1207/S15327965PLI1304_01
78. Shek DTL. COVID-19 pandemic and developmental outcomes in adolescents and young adults: in search of the missing links. J Adolescent Health. (2021) 69:683–4. doi: 10.1016/j.jadohealth.2021.07.035
79. Almuhtaseb MIA, Alby F, Zucchermaglio C, Fatigante M. Social support for breast cancer patients in the occupied Palestinian territory. PLoS One. (2021) 16:e0252608. doi: 10.1371/journal.pone.0252608
80. Sue S. In defense of cultural competency in psychotherapy and treatment. Am Psychol. (2003) 58:964–70. doi: 10.1037/0003-066X.58.11.964
81. Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev. (2011) 82:405–32. doi: 10.1111/j.1467-8624.2010.01564.x
82. Shek DTL, Sun RCF. Development and Evaluation of Positive Adolescent Training Through Holistic Social Programs (P.A.T.H.S.). Berlin: Springer (2013).
83. Li X, Shek DTL. Objective outcome evaluation of a leadership course utilising the positive youth development approach in Hong Kong. Assess Eval Higher Educ. (2020) 45:741–57. doi: 10.1080/02602938.2019.1696944
84. Yu L, Lin L, Shek TLD, Chai W. Students’ perceived attributes and benefits of a leadership course: subjective outcome evaluation. Res Soc Work Pract. (2022) 32:199–214. doi: 10.1177/10497315211042823
85. Weissberg RP. Promoting the social and emotional learning of millions of school children. Perspect Psychol Sci. (2019) 14:65–9. doi: 10.1177/1745691618817756
86. Dai L, Wang L. Review of family functioning. Open J Soc Sci. (2015) 3:134–41. doi: 10.4236/jss.2015.312014
87. Benson PL, Scales PC, Hamilton SF, Sesma A Jr. Positive youth development: theory, research, and applications. In: RM Lerner, W Damon editors. Handbook of Child Psychology: Theoretical Models of Human Development. 6th ed. Vol. 1. Hoboken, NJ: John Wiley & Sons Inc (2006). p. 894–941.
88. Kormos C, Gifford R. The validity of self-report measures of proenvironmental behavior: a meta-analytic review. J Environ Psychol. (2014) 40:359–71. doi: 10.1016/j.jenvp.2014.09.003
89. Chan D. So why ask me? Are self-report data really that bad? In: C. E. Lance, R. J. Vandenberg editors. Statistical and Methodological Myths and Urban Legends: Doctrine, Verity and Fable in the Organizational and Social Sciences. Milton Park: Taylor & Francis (2009). p. 309–36.
90. Levin KA. Study design III: cross-sectional studies. Evidence-Based Dentistry. (2006) 7:24–5. doi: 10.1038/sj.ebd.6400375
91. Sedgwick P. Cross sectional studies: advantages and disadvantages. BMJ Br Med J. (2014) 348:g2276. doi: 10.1136/bmj.g2276
Keywords: depression, positive youth development, beliefs about adversity, psychosocial competence, family functioning
Citation: Shek DTL, Dou D, Zhu X, Wong T and Tan L (2022) Need Satisfaction and Depressive Symptoms Among University Students in Hong Kong During the COVID-19 Pandemic: Moderating Effects of Positive Youth Development Attributes. Front. Psychiatry 13:931404. doi: 10.3389/fpsyt.2022.931404
Received: 29 April 2022; Accepted: 20 June 2022;
Published: 07 July 2022.
Edited by:
Kai Yuan, Peking University Sixth Hospital, ChinaReviewed by:
Diego Gomez-Baya, University of Huelva, SpainBanglin Yang, East China Normal University, China
Shiyu Lu, City University of Hong Kong, Hong Kong SAR, China
Copyright © 2022 Shek, Dou, Zhu, Wong and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel T. L. Shek, ZGFuaWVsLnNoZWtAcG9seXUuZWR1Lmhr
 Daniel T. L. Shek
Daniel T. L. Shek Diya Dou
Diya Dou Xiaoqin Zhu
Xiaoqin Zhu Tingyin Wong
Tingyin Wong Lindan Tan
Lindan Tan