
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Psychiatry, 26 May 2022
Sec. Mood Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.925983
This article is part of the Research TopicComorbidity in Bipolar Disorder, volume IIView all 10 articles
Dissociative disorders are an important group of trauma-related disorders associated with significant disability. The co-occurrence of dissociative disorders (DD) and symptoms (DS) in bipolar disorder has been relatively understudied, but there is some evidence that this comorbidity may have significant mechanistic and clinical implications. This paper presents the results of a scoping review of the frequency and correlates of DS and DD in bipolar disorder. Based on the available evidence, DS/DD are more common in bipolar disorder than in healthy controls or in unipolar depression, are related to childhood trauma, and are associated with psychotic symptoms, suicide attempts, and a poorer response to treatment in patients with bipolar disorder. The implications of these findings, and possible mechanistic pathways underlying them, are discussed based on the current literature. Clinicians should be aware of the frequent occurrence of significant DS or DD when treating patients with bipolar disorder. A tentative future research agenda for this field, based on clinical, risk factor-related and neurobiological considerations, is outlined.
Bipolar disorders are a group of mental illnesses characterized by recurrent episodes of elevated and depressed mood, associated with significant levels of morbidity and an elevated mortality risk (1). Comorbidity with other psychiatric disorders is seen in over 50% of patients with BD, particularly with anxiety, attention-deficit/hyperactivity and substance use disorders (2). The presence of comorbid diagnoses in BD is associated with poorer treatment response and a more severe illness course; patients with these diagnoses often require more intensive or complex treatment regimens (3–6).
Dissociative disorders (DD), which are characterized by disruption or discontinuity in the integration of one's consciousness, memory, identity and behavior, are associated with risks of hospitalization, self-injury and suicide comparable to BD (7). Though the comorbidity of DD and BD has been relatively under-studied (8), there is evidence from the literature of several potential clinical and mechanistic links between them. BD and DD appear to share a genetic substrate to some extent (9, 10) and the onset of symptoms of DD may be a herald of subsequent BD in adolescents (11, 12). DD may be underdiagnosed in patients with BD because of diagnostic criteria that do not allow DD to be diagnosed in the presence of depression (13), confusion arising from similar symptoms (14), or a reluctance to diagnose DD among mental health professionals (15). A further problem is posed by patients with BD who have features of dissociation that are clinically significant, but do not fulfill criteria for DD; these are referred to as “pathological dissociation” or “dissociative symptoms” (DS).
The present of DD or DS in BD raises several important questions. How frequent and severe is this comorbidity? What is the impact of DD/DS on the clinical features and prognosis of BD? Are there any specific environmental risk factors, such as childhood adversity, that are associated with the presence of DD/DS? Are DD/DS in BD associated with specific genetic factors or other biomarkers? The current scoping review aims to address these questions in a preliminary manner.
Given the lack of a single specific question and the paucity of literature in this area, a scoping review was carried out instead of a systematic review (16). This review was carried out in accordance with the PRISMA guideline for scoping reviews (PRISMA-ScR) (17). The PubMed, Scopus and ScienceDirect databases were searched using combinations of the key words “bipolar disorder”, “bipolar disorders”, “bipolar spectrum”, “bipolar I disorder”, “bipolar II disorder” in association with “dissociative disorders”, “dissociative amnesia”, “dissociative identity disorder”, “depersonalization”, “derealization”, “dissociative symptoms”, “pathological dissociation”. All studies published up to April 15, 2022 were included in this review. Studies were included if they measured the frequency and/or correlates of the presence of DD/DS in BD, with or without the inclusion of comparator groups. Any study that provided information on the frequency, severity, clinical impact, association with environmental risk factors, or neurobiological correlates of DS/DD in patients with bipolar disorder was included in this review. Case reports/series, editorials, commentaries and general review articles were excluded.
A total of 471 citations were retrieved; after removal of duplicates, 333 citations were screened; after exclusion of 226 unrelated abstracts, 107 citations were tabulated and their full text was examined for relevance. Of these, 27 were included in the final review (18–44). This process is illustrated through a PRISMA-ScR flow diagram in Figure 1.
Following tabulation, study results were sorted thematically according to the objectives of this review, as follows:
• Frequency of comorbid DD in BD or vice versa
• Frequency of significant DS in BD
• Comparison of DD/DS in BD compared to other groups (major depression, other psychiatric diagnoses, healthy controls)
• Associations with BD subtype (e.g. type I vs type II)
• Associations with BD course (e.g., age at onset, number of episodes)
• Associations with BD symptomatology (e.g., mixed features, psychotic symptoms, suicide attempts)
• Associations with BD outcome (e.g., treatment response, disability, quality of life)
• Associations with other comorbidities in BD (e.g., anxiety disorders, substance use disorders)
• Associations with environmental factors in BD (e.g., childhood trauma, current stressors)
• Associations with other psychological variables (e.g., temperament, personality traits)
• Associations with neuropsychological deficits in BD (e.g., attention or memory deficits)
• Associations with genetic or other biological markers (e.g., specific genetic polymorphisms, levels of hormones or inflammatory markers)
The same schema was followed when reporting the results.
A complete description of the included studies is provided, in chronological order, in Table 1.
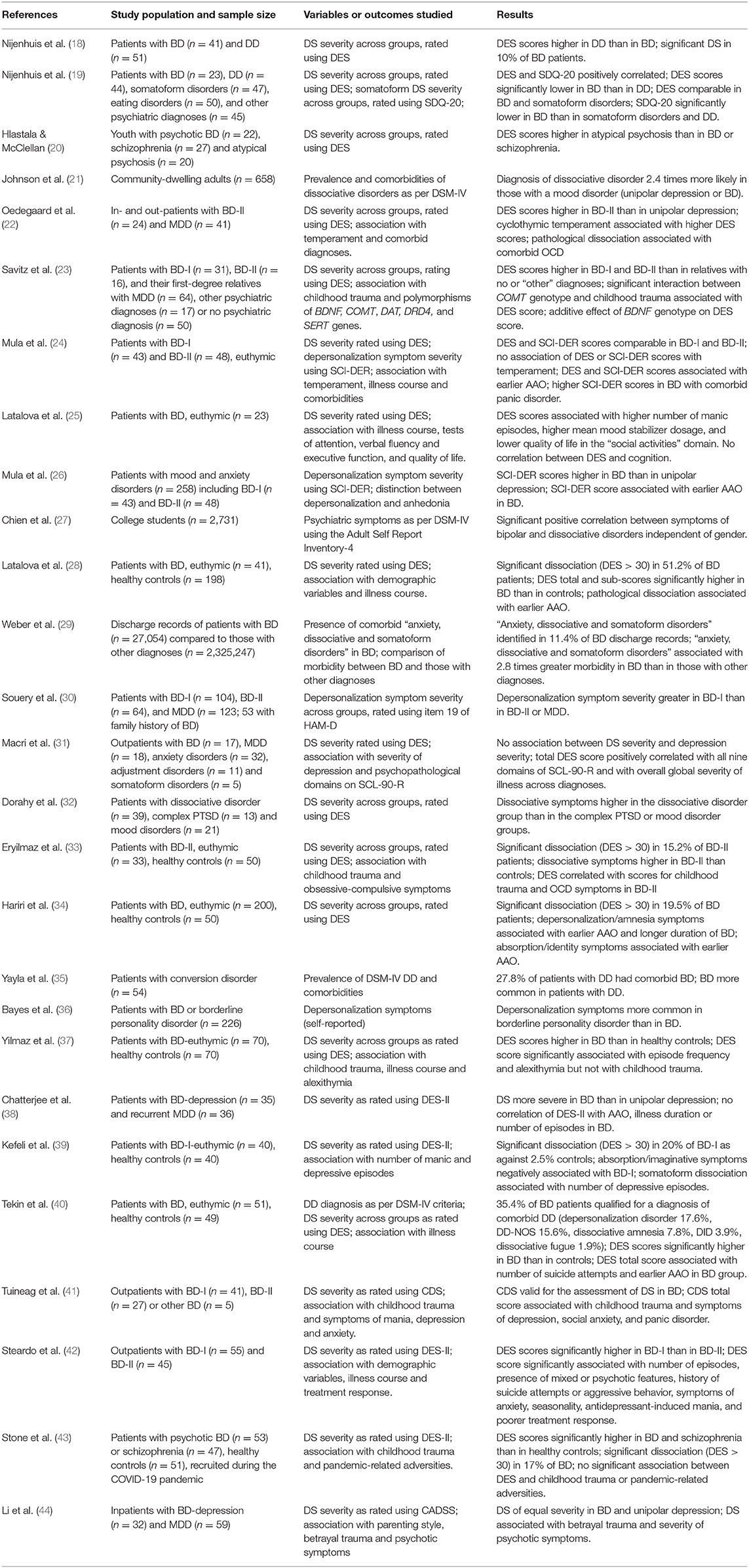
Table 1. Studies examining the association between dissociative symptoms or disorders and bipolar disorder, with a summary of their key findings.
The majority of the studies included in this review (n = 21) were cross-sectional clinical studies measuring the severity or correlates of DS in patients with BD. Three studies examined the association between syndromal DD and BD (21, 29, 40), while one study each examined associations with cognitive test performance (25) and polymorphisms of specific genes considered to be related to dissociation (23).
Only one study directly measured the frequency of DSM-IV categorical diagnoses of DD in patients with BD. In this study, 35.4% of BD patients fulfilled criteria for one or more DD, with depersonalization disorder (17.6%) being the most frequent (40). A community-based study found that DD were 2.4 times more likely to be diagnosed in patients with mood disorders, but did not distinguish between BD and unipolar depression (21). A study of patients with conversion disorder found a significant association between comorbid diagnoses of DD and BD (35). Finally, a study of discharge records found that 11.4% of patients discharged with BD received a comorbid diagnosis of “anxiety, somatoform or dissociative disorder” as per ICD-9 criteria, but details of individual diagnoses within this group were not reported by the authors (29).
Of the six studies providing estimates of clinically significant DS in BD, as indicated by symptom scores above a specified cut-off, five yielded very similar values in the range of 10–20% (18, 33, 34, 39, 43). A single study yielded a much higher estimate of 51%, but in this study, the control group also reported high levels of DS (24%), suggesting concerns related to methodology or sample selection (28).
Five studies have compared the severity of DS in patients with BD and major depressive disorder (MDD), have measured DS during depressive episodes. In four of these studies, DS were more prominent in BD than in MDD (22, 26, 30, 38), while in the other, they were comparable (44). Studies comparing the severity of DS between BD and other, non-affective psychiatric disorders found that DS were significantly less in BD than in somatoform disorders and DD (18, 19, 32), complex post-traumatic stress disorder (PTSD) (32), atypical psychosis in adolescents (20), and borderline personality disorder (36). DS were comparable in BD and schizophrenia in a single study (43). However, DS scores were significantly higher in patients with BD than in their asymptomatic first-degree relatives (23) and were consistently higher in BD than in healthy controls (28, 33, 34, 37, 39, 43).
Though some researchers have reported no difference in DS severity scores between BD-I and BD-II (23, 24), there is some evidence that DS and particularly depersonalization symptoms may be more severe in BD-I (30, 42). Only one study assessed DS in patients with other BD subtypes (BD-III and BD not otherwise specified) along with BD-I and BD-II, but the small number of cases in this subgroup precluded a meaningful comparison (41).
DS scores have been associated with the severity of psychotic symptoms (42, 44); both positive and null results have been reported for associations between DS and depressive symptom severity (31, 41). DS severity has also been associated with general symptom severity across psychopathological dimensions (31), with the severity of symptoms of social anxiety, panic disorder and obsessive-compulsive disorder (33, 41), with the presence of mixed symptoms (42), with suicide attempts (40, 42) and with aggression (42).
Five studies found a negative correlation between the severity of DS and the age at onset of BD (AAO), suggesting an association between dissociation and an early AAO (24, 26, 28, 34, 40). This association appeared to be more specific for depersonalization-related symptoms (24, 26, 34). Only one study reported no association between DS and AAO in BD (38). Associations between DS severity and episode frequency (37), total number of episodes (42) and frequency of manic (25) and depressive episodes (39) have been reported in individual studies. However, a lack of association with episode number has also been reported (38).
The severity of DS appears to be associated with treatment response; associations with a higher dose requirement for mood stabilizers (25), with a higher risk of antidepressant-induced mania (42) and with a poorer response to treatment (42) have all been observed. DS are also associated with a poorer quality of life in the “social activities” domain in euthymic BD patients (25).
Higher DS scores have been associated with elevated rates of comorbid obsessive-compulsive disorder (OCD) (22) and panic disorder (24) in BD; no other specific associations with any comorbid diagnosis have been reported.
Six studies have examined the association between childhood abuse or neglect and DS in BD; four of these found a positive association between childhood trauma and DS severity (23, 33, 41, 44), while two failed to do so (37, 43). A single study examined the relationship between DS and current stress related to the COVID-19 pandemic, but did not find any significant association between the two (43).
Cyclothymic temperament, considered to be a developmental precursor of BD, was associated with the presence of DS in BD patients in one study (22) but not in another (24). DS severity has also been associated with measures of alexithymia in BD (37).
A study examining the association between DS and performance on tests of cognition (attention, concentration, executive function and verbal fluency) found no significant association between DS severity and scores on these tests (25).
Only one study has examined the potential genetic correlates of DS in BD; in this study, an interaction between childhood trauma and a functional polymorphism of the COMT gene, as well as an additive effect of the BDNF gene, was found to predict the severity of DS (23). No other study of any specific biomarker associated with DS/DD in BD has been conducted to date.
Certain features emerge clearly from an overview of the current literature. A significant minority of patients (10–20%) with bipolar disorder experience significant DS, even during the euthymic phase. The overall severity of DS is higher in BD than in healthy controls and in major depression, but is lower in BD when compared with “trauma spectrum disorders” such as DD, complex PTSD and borderline personality disorder. When considering the clinical profile of BD, replicated results suggest that DS are associated with psychotic symptoms, suicide attempts, and a poorer response to treatment. DS also appear to be associated with the severity of childhood trauma in patients with BD. Results related to other symptom domains, episode number and frequency, and quality of life, though of interest, require replication.
The above findings are consistent with the existing literature on DS/DD. Both pathological dissociation and DD are considered part of the “trauma spectrum” of disorders, which are related to exposure to traumatic stress, particularly in childhood (45). This group also includes PTSD and borderline personality disorder; it is perhaps significant that these conditions are also often comorbid with BD (46, 47). Given that childhood adversity is itself a risk factor for BD (48) and was associated with DS in the reviewed studies, this factor may explain a significant proportion of the co-occurrence of DD/DS and BD. Moreover, dissociation is an important mediator of the links between childhood abuse and both psychotic symptoms (49) and suicide (50), which is consistent with the findings observed in patients with BD.
Recent research has shed some light on the neurobiological correlates of dissociative symptoms (51). Some of the replicated biomarkers of pathological dissociation, such as reduced hippocampal and thalamic volumes and elevated peripheral levels of oxytocin, have also been identified in bipolar disorder (52–54), suggesting common neuroanatomical and biochemical substrates for these conditions. It should however be noted that for other biomarkers of dissociation, such as levels of tumor necrosis factor alpha, findings in bipolar disorder are in the opposite direction (55). This suggests that there may be shared mechanistic pathways, but not a complete overlap, between BD and dissociative symptoms.
Besides exposure to childhood trauma or other environmental stressors, the link between DS/DD and BD may be partly mediated through genetic vulnerability. While earlier researchers suggested that this might result from variations in single genes, such as the serotonin transporter (56), more recent results suggest that the overlap between bipolar and dissociative disorders may be polygenic in origin (10).
These findings must be interpreted in the light of important limitations in study design and methodology in the existing literature. The majority of reviewed studies are cross-sectional and focus on clinical variables, with very few studies examining neuropsychological or neurobiological correlates of DD or DS in BD. Most studies have been conducted in remitted, euthymic or clinically stable BD patients, and have measured DS using standardized scales instead diagnosing comorbid DD using standard criteria. There is also substantial heterogeneity in the measurement of DS, with some studies focusing on a subset of DS such as depersonalization/derealization or somatoform dissociation. Sample sizes for BD were generally low (mean: 61.2 ± 47.8), suggesting that some studies may have been underpowered to detect significant differences. Further, in some studies, associations between DS and clinical or environmental variables of interest were not estimated even when the data was available. These factors limit both the value of the conclusions that can be drawn from individual studies and the likelihood of their replication, and suggest the need for better designs even if the research questions are purely clinical in nature.
A further limitation arises from the fact that the link between DS/DD and BD may be non-specific. Dissociative symptoms of severity comparable to or slightly greater than those reported in BD have been observed in a wide range of psychiatric disorders, including schizophrenia, anxiety disorders, eating disorders and substance use disorders (57). These findings suggest that dissociation may be better considered from a dimensional rather than a categorical perspective, or that it may be related to a common genetic substrate that cuts across traditional psychiatric diagnoses (58).
Despite these limitations, the above review suggests that the presence of DS/DD in patients with BD may have significant clinical and research implications. From a clinical perspective, practitioners should be aware of the co-occurrence of these conditions, and maintain a high index of clinical suspicion; in cases of doubt, a standardized rating scale such as the DES can aid decision-making. Given the replicated associations with psychotic symptoms, suicidality, and poor treatment response, these patients may require more intensive clinical management. Lithium therapy, which has been shown to reverse the hippocampal and thalamic volume reductions common to bipolar disorder and dissociation (51, 52), may be a useful therapeutic option. Bipolar patients with DS/DD should be screened for other comorbid anxiety disorders as well as post-traumatic stress disorder (22, 24, 33, 41). Given the link between childhood trauma and dissociation in BD, a sensitive inquiry into possible childhood abuse or neglect should be made when patients are clinically stable. Finally, when there are significant DS or a syndromal DD, appropriate psychological interventions should be provided (59).
From a research perspective, the following areas require particular attention in the study of the links between dissociation and bipolarity:
• Replications of findings related to clinical and psychological variables of interest, such as affective temperaments, alexithymia, cycle length and the presence of mixed features
• Accurate studies of the prevalence of comorbid DD in BD, and of comorbid BD in DD, using standard diagnostic criteria
• Longitudinal studies of the impact of DS or DD on the course and outcome of BD
• Studies of high-risk youth (e.g., with a family history of BD or with a history of childhood abuse) with DS or DD, to assess their subsequent risk of BD and the possibility of early intervention (12, 60)
• Studies of structural, functional and biochemical markers of the link between BD and DD; areas that could be immediately explored include associations with peripheral levels of cytokines (61) and functional brain imaging studies focusing on key frontal and subcortical regions implicated in both disorders (49, 62)
• Assessment of the utility of a dimensional rather than a categorical approach to the study of dissociation in patients with BD, and of the correlations between DS and other symptom dimensions in BD (63)
• Genome-wide association studies using either a narrower definition of DD (i.e., without lumping them with anxiety and somatoform disorders) or a continuous measure of DS, to identify specific and shared genetic loci associated with vulnerability to pathological dissociation in patients with BD
• Evaluation of the efficacy of specific pharmacological (mood stabilizer, antipsychotic), brain stimulation (rTMS) and psychotherapeutic (trauma-focused) approaches in patients with BD and DD/DS (64, 65).
Though research on dissociative symptoms and disorders in patients with bipolar disorders is still in its infancy, existing evidence suggests that these symptoms are significantly associated with both risk factors—particularly childhood abuse—and a specific illness profile in bipolar disorder. It is hoped that the findings reviewed and summarized above will be of use to clinicians working with patients with bipolar disorder. Moreover, the tentative research agenda outlined above could improve our understanding of this specific comorbidity, leading to improved strategies for early intervention as well as treatment in subsequent stages of bipolar disorder.
RR selected the review topic and method, conducted the literature search and article selection, analyzed and summarized the results, and wrote and edited the manuscript.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AAO, age at onset; BD, bipolar disorders; BD-I, bipolar I disorder; BD-II, bipolar II disorder; BDNF, brain-derived neurotrophic factor; CADSS, Clinician-Administered Dissociative States Scale; CDS, Cambridge Depersonalization Scale; COMT, catechol O-methyltransferase; DAT, dopamine transporter; DID, dissociative identity disorder; DRD4, dopamine type 4 receptor; DD, dissociative disorders; DD-NOS, dissociative disorder not otherwise specified; DES, Dissociative Experiences Scale; DSM-IV, Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition; HAM-D, Hamilton Rating Scale for Depression; MDD, major depressive disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; SCI-DER, Structured Clinical Interview for Depersonalization/Derealization Spectrum; SCL-90-R, Symptom Checkist-90 Revised; SDQ-20, Somatoform Dissociation Questionnaire-20; SERT, serotonin transporter.
1. GBD 2019 Mental Disorders Collaborators. Global, regional and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
2. Frías Á, Palma C, Farriols N. Comorbidity in pediatric bipolar disorder: prevalence, clinical impact, etiology and treatment. J Affect Disord. (2015) 174:378–89. doi: 10.1016/j.jad.2014.12.008
3. Preti A, Vrublevska J, Veroniki AA, Huedo-Medina TB, Fountoulakis KN. Prevalence, impact and treatment of generalised anxiety disorder in bipolar disorder: a systematic review and meta-analysis. Evid Based Ment Health. (2016) 19:73–81. doi: 10.1136/eb-2016-102412
4. Consoli A, Bouzamondo A, Guilé JM, Lechat P, Cohen D. Comorbidity with ADHD decreases response to pharmacotherapy in children and adolescents with acute mania: evidence from a metaanalysis. Can J Psychiatry. (2007) 52:323–8. doi: 10.1177/070674370705200507
5. Messer T, Lammers G, Müller-Siecheneder F, Schmidt RF, Latifi S. Substance abuse in patients with bipolar disorder: a systematic review and meta-analysis. Psychiatry Res. (2017) 253:338–50. doi: 10.1016/j.psychres.2017.02.067
6. Berk M, Ng F, Wang WV, et al. Going up in smoke: tobacco smoking is associated with worse treatment outcomes in mania. J Affect Disord. (2008) 110:126–34. doi: 10.1016/j.jad.2008.01.018
7. Gonzalez Vazquez AI, Seijo Ameneiros N, Díaz Del Valle JC, Lopez Fernandez E, Santed Germán MA. Revisiting the concept of severe mental illness: severity indicators and healthcare spending in psychotic, depressive and dissociative disorders. J Ment Health. (2020) 29:670–6. doi: 10.1080/09638237.2017.1340615
8. Mauritz MW, Goossens PJJ, Draijer N, van Achterberg T. Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illnesses. Eur J Psychotraumatol. (2013) 4:19985. doi: 10.3402/ejpt.v4i0.19985
9. Palomo T, Kostrzewa RM, Beninger RJ, Archer T. Genetic variation and shared biological susceptibility underlying comorbidity in neuropsychiatry. Neurotox Res. (2007) 12:29–42. doi: 10.1007/BF03033899
10. Kember RL, Merikangas AK, Verma SS, Verma A, Judy R, Damrauer SM, et al. Polygenic risk of psychiatric disorders exhibits cross-trait associations in electronic health record data from European ancestry individuals. Biol Psychiatry. (2021) 89:236–45. doi: 10.1016/j.biopsych.2020.06.026
11. Ghosal MK, Guha P, Sinha M, Majumdar D, Sengupta P. Conversion (dissociative) symptoms as a presenting feature in early onset bipolar disorder: a case series. BMJ Case Rep. (2009) 2009:bcr01.2009.1448. doi: 10.1136/bcr.01.2009.1448
12. Leopold K, Ritter P, Correll CU, Marx C, Ozgurdal S, Juckel G, et al. Risk constellations prior to the development of bipolar disorders: rationale of a new risk assessment tool. J Affect Disord. (2012) 136:1000–10. doi: 10.1016/j.jad.2011.06.043
13. Spiegel D, Loewenstein RJ, Lewis-Fernández R, Sar V, Simeon D, Vermetten E, et al. Dissociative disorders in DSM-5. Depress Anxiety. (2011) 28:824–52. doi: 10.1002/da.20874
14. Savitz J, Solms M, Pietersen E, Ramesar R, Flor-Henry P. Dissociative identity disorder associated with mania and change in handedness. Cog Behav Neurol. (2004) 17:233–7.
15. Loewenstein RJ. Dissociation debates: everything you know is wrong. Dialogues Clin Neurosci. (2018) 20:229–42. doi: 10.31887/DCNS.2018.20.3/rloewenstein
16. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. (2018) 18:143. doi: 10.1186/s12874-018-0611-x
17. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
18. Nijenhuis ER, Spinhoven P, van Dyck R, van der Hart O, de Graaf A, Knoppert EAM. Dissociative pathology discriminates between bipolar mood disorder and dissociative disorder. Br J Psychiatry. (1997) 170:581. doi: 10.1192/S0007125000259187
19. Nijenhuis ER, van Dyck R, Spinhoven P, van der Hart O, Chatrou M, Vanderlinden J, et al. Somatoform dissociation discriminates among diagnostic categories over and above general psychopathology. Aust N Z J Psychiatry. (1999) 33:511–20. doi: 10.1080/j.1440-1614.1999.00601.x
20. Hlastala SA, McClellan J. Phenomenology and diagnostic stability of youths with atypical psychotic symptoms. J Child Adolesc Psychopharmacol. (2005) 15:497–509. doi: 10.1089/cap.2005.15.497
21. Johnson JG, Cohen P, Kasen S, Brook JS. Dissociative disorders among adults in the community, impaired functioning, and axis I and II comorbidity. J Psychiatr Res. (2006) 40:131–40. doi: 10.1016/j.jpsychires.2005.03.003
22. Oedegaard KJ, Neckelmann D, Benazzi F, Syrstad VE, Akiskal HS, Fasmer OB. Dissociative experiences differentiate bipolar-II from unipolar depressed patients: the mediating role of cyclothymia and the type A behaviour speed and impatience subscale. J Affect Disord. (2008) 108:207–16. doi: 10.1016/j.jad.2007.10.018
23. Savitz JB, van der Merwe L, Newman TK, Solms M, Stein DJ, Ramesar RS. The relationship between childhood abuse and dissociation. Is it influenced by catechol-O-methyltransferase (COMT) activity? Int J Neuropsychopharmacol. (2008) 11:149–61. doi: 10.1017/S1461145707007900
24. Mula M, Pini S, Preve M, Masini M, Giovannini I, Cassano GB. Clinical correlates of depersonalization symptoms in patients with bipolar disorder. J Affect Disord. (2009) 115:252–6. doi: 10.1016/j.jad.2008.08.001
25. Latalova K, Prasko J, Diveky T, Kamaradova D, Velartova H. Cognitive dysfunction, dissociation and quality of life in bipolar affective disorders in remission. Psychiatr Danub. (2010) 22:528–34.
26. Mula M, Pini S, Calugi S, Preve M, Masini M, Giovannini I, et al. Distinguishing affective depersonalization from anhedonia in major depression and bipolar disorder. Compr Psychiatry. (2010) 51:187–92. doi: 10.1016/j.comppsych.2009.03.009
27. Chien YL, Gau SS, Gadow KD. Sex difference in the rates and co-occurring conditions of psychiatric symptoms in incoming college students in Taiwan. Compr Psychiatry. (2011) 52:195–207. doi: 10.1016/j.comppsych.2010.03.009
28. Latalova K, Prasko J, Pastucha P, Grambal A, Kamaradova D, Diveky T, et al. Bipolar affective disorder and dissociation–comparison with healthy controls. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. (2011) 155:181–6. doi: 10.5507/bp.2011.007
29. Weber NS, Fisher JA, Cowan DN, Niebuhr DW. Psychiatric and general medical conditions comorbid with bipolar disorder in the national hospital discharge survey. Psychiatr Serv. (2011) 62:1152–8. doi: 10.1176/ps.62.10.pss6210_1152
30. Souery D, Zaninotto L, Calati R, Linotte S, Mendlewicz J, Sentissi O, et al. Depression across mood disorders: review and analysis in a clinical sample. Compr Psychiatry. (2012) 53:24–38. doi: 10.1016/j.comppsych.2011.01.010
31. Macri F, Salviati M, Provenzano A, Melcore C, Terlizzi S, Campi S, et al. Psychopathological severity index and dissociative symptomatology in a group of non-psychotic outpatients. J Psychopathol. (2013) 19:105–8.
32. Dorahy MJ, Middleton W, Seager L, McGurrin P, Williams M, Chambers R. Dissociation, shame, complex PTSD, child maltreatment and intimate relationship self-concept in dissociative disorder, chronic PTSD and mixed psychiatric groups. J Affect Disord. (2015) 172:195–203. doi: 10.1016/j.jad.2014.10.008
33. Eryilmaz G, Kesebir S, Gul IG, Ozten E, Karamustafalioglu KO. Dissociative experiences in bipolar disorder II: are they related to childhood trauma and obsessive-compulsive symptoms? Arch Clin Psychiatry. (2015) 42:38–40. doi: 10.1590/0101-60830000000045
34. Hariri AG, Gulec MY, Orengul FFC, Sumbul EA, Elbay RY, Gulec H. Dissociation in bipolar disorder: relationships between clinical variables and childhood trauma. J Affect Disord. (2015) 184:104–10. doi: 10.1016/j.jad.2015.05.023
35. Yayla S, Bakim B, Tankaya O, Ozer OA, Karamustafalioglu O, Ertekin H, et al. Psychiatric comorbidity in patients with conversion disorder and presence of dissociative symptoms. J Trauma Dissociation. (2015) 16:29–38. doi: 10.1080/15299732.2014.938214
36. Bayes AJ, McGlure G, Fletcher K, Del Moral YERR, Hadzi-Pavlovic D, Stevenson JL, et al. Differentiating the bipolar disorders from borderline personality disorder. Acta Psychiatr Scand. (2016) 133:187–95. doi: 10.1111/acps.12509
37. Yilmaz O, Ates MA, Semiz UB, Tutuncu R, Bez Y, Algul A. Childhood traumas in patients with bipolar disorder: association with alexithymia and dissociative experiences. Anatol J Psychiatry. (2016) 17:188–95. doi: 10.5455/apd.188358
38. Chatterjee SS, Pal A, Mallik N, Ghosal M, Saha G. Dissociative experience in unipolar and bipolar depression: exploring the great divide. Clin Psychopharmacol Neurosci. (2018) 16:262–6. doi: 10.9758/cpn.2018.16.3.262
39. Kefeli MC, Turow RG, Yildirim A, Boysan M. Childhood maltreatment is associated with attachment insecurities, dissociation and alexithymia in bipolar disorder. Psychiatry Res. (2018) 260:391–9. doi: 10.1016/j.psychres.2017.12.026
40. Tekin A, Demiryürek EÖ, Güleken MD, Bakim B, Özer ÖA, Karamustafalioglu O. Investigation of the comorbidity of dissociative disorders in patients with bipolar disorder. Eur Res J. (2019) 5:667–72. doi: 10.18621/eurj.412272
41. Tuineag M, Therman S, Lindgren M, Rouanet M, Nahon S, Bertrand L, et al. Dissociative symptoms as measured by the Cambridge depersonalization scale in patients with a bipolar disorder. J Affect Disord. (2020) 263:187–92. doi: 10.1016/j.jad.2019.11.137
42. Steardo L Jr, Carbone EA, Ventura E, de Filippis R, Luciano M, Segura-Garcia C. Dissociative symptoms in bipolar disorder: impact on clinical course and treatment response. Front Psychiatry. (2021) 12:732843. doi: 10.3389/fpsyt.2021.732843
43. Stone LMD, Millman ZB, Öngür D, Shinn AK. The intersection between childhood trauma, the COVID-19 pandemic, and trauma-related and psychotic symptoms in people with psychotic disorders. Schizophr Bull Open. (2021) 2:sgab050. doi: 10.1093/schizbullopen/sgab050
44. Li D-J, Hsieh Y-C, Chiu C-D, Lin C-H, Chou L-S. The moderation of maternal parenting on the association of trauma, dissociation, and psychosis in depressive inpatients. Eur J Psychotraumatol. (2022) 13:2024974. doi: 10.1080/20008198.2021.2024974
45. Bremner JD, Wittbrodt MT. Stress, the brain, and trauma spectrum disorders. Int Rev Neurobiol. (2020) 152:1–22. doi: 10.1016/bs.irn.2020.01.004
46. Fornaro M, Orsolini L, Marini S, De Berardis D, Perna G, Valchera A, et al. The prevalence and predictors of bipolar and borderline personality disorders comorbidity: systematic review and meta-analysis. J Affect Disord. (2016) 195:105–18. doi: 10.1016/j.jad.2016.01.040
47. Nabavi B, Mitchell AJ, Nutt D, A. Lifetime prevalence of comorbidity between bipolar affective disorder and anxiety disorders: a meta-analysis of 52 interview-based studies of psychiatric population. EBioMedicine. (2015) 2:1405–19. doi: 10.1016/j.ebiom.2015.09.006
48. Palmier-Claus JE, Berry K, Bucci S, Mansell W, Varese F. Relationship between childhood adversity and bipolar affective disorder: systematic review and meta-analysis. Br J Psychiatry. (2016) 209:454–9. doi: 10.1192/bjp.bp.115.179655
49. Williams J, Bucci S, Berry K, Varese F. Psychological mediators of the association between childhood adversities and psychosis: a systematic review. Clin Psychol Rev. (2018) 65:175–96. doi: 10.1016/j.cpr.2018.05.009
50. Bertule M, Sebre SB, Kolesovs A. Childhood abuse experiences, depression and dissociation symptoms in relation to suicide attempts and suicidal ideation. J Trauma Dissociation. (2021) 22:598–614. doi: 10.1080/15299732.2020.1869652
51. Roydeva MI, Reinders AATS. Biomarkers of Pathological Dissociation: A Systematic Review. Neurosci Biobehav Rev. (2021) 123:120–202. doi: 10.1016/j.neubiorev.2020.11.019
52. Lien YJ, Chang HH, Tsai HC, Kuang Yang Y, Lu RB, See Chen P. Plasma oxytocin levels in major depressive and bipolar II disorders. Psychiatry Res. (2017) 258:402–6. doi: 10.1016/j.psychres.2017.08.080
53. Otten M, Meeter M. Hippocampal structure and function in individuals with bipolar disorder: a systematic review. J Affect Disord. (2015) 174:113–25. doi: 10.1016/j.jad.2014.11.001
54. Radenbach K, Flaig V, Schneider-Axmann T, Usher J, Reith W, Falkai P, et al. Thalamic volumes in patients with bipolar disorder. Eur Arch Psychiatry Clin Neurosci. (2010) 260:601–7. doi: 10.1007/s00406-010-0100-7
55. Solmi M, Suresh Sharma M, Osimo EF, Fornaro M, Bortolato B, Croatto G, et al. Peripheral levels of C-reactive protein, tumor necrosis factor-α, interleukin-6, and interleukin-1β across the mood spectrum in bipolar disorder: a meta-analysis of mean differences and variability. Brain Behav Immun. (2021) 97:193–203. doi: 10.1016/j.bbi.2021.07.014
56. Kuzelova H, Ptacek R, Macek M Jr. The serotonin transporter gene (5-HTT) variant and psychiatric disorders. Neuro Endocrin Lett. (2010) 31:4–10.
57. Lyssenko L, Schmahl C, Bockhacker L, Vonderlin R, Bohus M, Kleindienst N. Dissociation in psychiatric disorders: a meta-analysis of studies using the dissociative experiences scale. Am J Psychiatry. (2018) 175:37–46. doi: 10.1176/appi.ajp.2017.17010025
58. Andlauer TFM, Mühleisen TW, Hoffstaedter F, Teumer A, Wiffeld K, Teuber A, et al. Genetic factors influencing a neurobiological substrate for psychiatric disorders. Transl Psychiatry. (2021) 11:192. doi: 10.1038/s41398-021-01317-7
59. Ganslev CA, Storebø OJ, Callesen HE, Ruddy R, Søgaard U. Psychosocial interventions for conversion and dissociative disorders in adults. Cochrane Database Syst Rev. (2020) 7:CD005331. doi: 10.1002/14651858.CD005331.pub3
60. Brandt JM, Hemager N, Gregersen M, Sondergaard A, Krantz MF, Ohland J, et al. Childhood trauma in children at familial high risk of schizophrenia or bipolar disorder: a longitudinal study. The Danish High Risk and Resilience Study - VIA 7 and VIA 11. Br J Clin Psychol. (2022). doi: 10.1111/bjc.12364
61. Bob P, Raboch J, Maes M, Susta M, Pavlat J, Jasova D, et al. Depression, traumatic stress and interleukin-6. J Affect Disord. (2010) 120:231–4. doi: 10.1016/j.jad.2009.03.017
62. Janiri D, Moser DA, Doucet GE, Luber MJ, Rasgon A, Lee WH et al. Shared neural phenotypes for mood and anxiety disorders: a meta-analysis of 226 task-related functional imaging studies. JAMA Psychiatry. (2020) 77:172–9. doi: 10.1001/jamapsychiatry.2019.3351
63. Henry C, Etain B. New ways to classify bipolar disorders: going from categorical groups to symptom clusters or dimensions. Curr Psychiatry Rep. (2010) 12:505–11. doi: 10.1007/s11920-010-0156-0
64. Dadomo H, Grecucci A, Giardini I, Ugolini E, Carmelita A, Panzeri M. schema therapy for emotional dysregulation: Theoretical implication and clinical applications. Front Psychol. (2016) 7:1987. doi: 10.3389/fpsyg.2016.01987
65. Orrú G, Bertelloni D, Cesari V, Conversano C, Gemignani A. Targeting temporal parietal junction for assessing and treating disembodiment phenomena: A systematic review of TMS effect on depersonalization and derealization disorders (DPD) and body illusions. AIMS Neurosci. (2021) 8:181–94. doi: 10.3934/Neuroscience.2021009
Keywords: bipolar disorders, dissociative disorders, depression, depersonalization, derealization, comorbidity
Citation: Rajkumar RP (2022) Dissociative Symptoms and Disorders in Patients With Bipolar Disorders: A Scoping Review. Front. Psychiatry 13:925983. doi: 10.3389/fpsyt.2022.925983
Received: 22 April 2022; Accepted: 03 May 2022;
Published: 26 May 2022.
Edited by:
Michele Fornaro, University of Naples Federico II, ItalyReviewed by:
Jacopo Lisoni, Asst Spedali Civili di Brescia, ItalyCopyright © 2022 Rajkumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ravi Philip Rajkumar, cmF2aS5wc3ljaEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.