- Department of Pediatric Health Care, The Children's Hospital, Zhejiang University School of Medicine, National Clinical Research Center for Child Health, Hangzhou, China
Background: High prevalence of sleep problems have been founded in children with Autism Spectrum Disorder (ASD), with rates ranging from 50 to 80%. We aimed to study the sleep status and the occurrence of sleep problems in children with autism spectrum disorder (ASD) aged 1–3 years, and to provide reference for guiding early comprehensive intervention for ASD children from the perspective of sleep.
Methods: From January 1 to December 31, 2021, 74 ASD children who met the diagnostic criteria of “Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-V)” served as case group while 84 typically-developing children of the same sex and age served as control group. An original Children's Sleep Habit Questionnaire was adopted to compare the sleep status of children in the two groups and to conduct statistical analysis on related factors.
Results: The incidence of sleep problems in the case group (78.4%) was significantly higher than that in the control group (34.5%) (P < 0.001). Compared with the children in the control group, children in the case group had later bedtime (P < 0.05) and less sleep duration (P < 0.05), and required longer time to fall asleep (P < 0.001) The incidence of sleep problems in children who could fall asleep autonomously in the case group was significantly lower than that in children who needed parental help (P < 0.05). In the case group, the longer the screen exposure time, the higher the incidence of sleep problems (P < 0.05).
Conclusions: The incidence of sleep problems in ASD children aged 1–3 years is also high, mainly manifested in late bedtime, difficulty falling asleep, frequent night awakenings and less sleep duration. Both sleep patterns and screen exposure can impact their sleep. In the early comprehensive intervention of ASD children, it is necessary to pay full heed to their sleep status and take timely intervention measures in order to improve the quality of life for the ASD children and their families.
Introduction
Autism spectrum disorder (ASD) is a chronic, lifelong neurodevelopmental disability characterized by impairments in social communication, restricted interests or activities, and repetitive behaviors (1). In the last decade, the prevalence rate of ASD has showed a sharp rise (2). The prevalence rate announced in the United States in 2006 was 0.9%, and the reported prevalence rate in 2020 has reached 1.8% (3). In China, the prevalence rate has rose from 0.35% in 2018 (4) to 0.7% in 2020 (5). This may be due to the advances in our understanding of the etiology of autism and the improved diagnostic techniques. ASD is a life-long disorder that has major implications for the quality of life of the individual with ASD as well as the families, resulting in a tremendous responsibility on the part of the public health and education systems. The comorbidity of ASD, such as sleep problems, gastrointestinal problems, and attention deficit hyperactivity disorder, has attracted more and more attention (6, 7). Studies have reported that the incidence of sleep problems in ASD children is 50–80% (8–10), much higher than the 29–50% reported in typically-developing children with normal development (11, 12). Sleep as an important physiological function impacts many aspects of early childhood development (13). For ASD children, sleep problems not only exacerbate certain core symptoms, such as restricted and repetitive behaviors and problematic behaviors, but may also affect the effectiveness of rehabilitation training (14–16). Previous studies have found that the sleep problems in ASD children are age-specific (12). But these research reports both at home and abroad aim at all preschool children and school-age children (17, 18). At present, the sleep status of ASD children aged 1–3 years has not been reported at home and abroad, and the impact of sleep problems on infants is far greater than that of children or adults. During the infant period, sleep occupies most of the time in their life. Good sleep not only contributes to the maturation of the central nervous system and the formation of the overall function of the infant, but also has an important influence on the formation of physical, cognitive, neuromotor and temperament development (19). Therefore, this study finds out the sleep characteristics of ASD children aged 1–3 years by analyzing the occurrence of sleep problems and sleep status, and provides a reference for early comprehensive intervention and improvement of their quality of life.
Materials and methods
Participants
Case group: 77 children with a diagnosis of ASD by the Children's Hospital, Zhejiang University School of Medicine from January 1 to December 31, 2021. Inclusion criteria: (1) Aged 1–3 years; (2) The diagnosis of ASD was performed independently by a developmental pediatrician and a psychiatrist using the DSM- 5 (20) in combination with the ADOS-2 (21, 22); (3) Excluding other organic diseases, hearing disorders, neurodevelopmental disorders, genetic metabolism diseases as well as mental and psychological disorders; (4) Stable medical conditions, and not taking psychiatric or sleep related medications in the past 3 months. A total of 77 questionnaires were collected, of which 74 (62 males and 12 females) were valid. The dropout rate was 3.9%.
Control group: 86 typically-developing children who underwent physical examinations in the same period. Inclusion criteria: (1) Aged 1–3 years; (2) Conforming to the developmental process of children of the same age through routine examination by the Children's Hospital, Zhejiang University School of Medicine; (3) Excluding other organic diseases, hearing disorders, neurodevelopmental disorders, genetic metabolic diseases as well as mental and psychological disorders; (4) Stable medical conditions, and not taking psychiatric or sleep related medications in the past 3 months. A total of 86 questionnaires were collected, of which 84 (65 males and 19 females) were valid. The dropout rate was 2.3%.
This research was approved by The Children's Hospital, Zhejiang University School of Medicine and Affiliation of Ethics Committee, and informed consent was obtained from the guardians of the research subjects.
Sample size
The sample size calculation used the formula of two independent sample rates:
It was reported that the highest prevalence of sleep problems in the ASD was 80% (10), while that in typically-developing children with normal development was 50%. Alpha was set to 0.05, beta was 0.1, and missing rate was 10%. The sample size required for each group was 57 in each centers through calculation.
Original children's sleep habit questionnaire
As Children's Sleep Habit Questionnaire (CSHQ) is mainly used to assess the sleep status of children aged 4–10 (23, 24), its factor structure is not applicable for young children. Therefore, an original Children's Sleep Habit Questionnaire was used in this research based on to the sleep characteristics of children aged 1–3 years, which mainly included: children's basic information, general family information, children's bedtime, sleep latency, sleep duration at night, sleep duration in the day time, sleep patterns, difficulty falling asleep, night awakening, parasomnia (such as sleepwalking, teeth grinding), sleep-disordered breathing (such as snoring, dyspnea during sleep) and sleep behavior, etc. This original Children's Sleep Habit Questionnaire was reviewed and validated by several rounds of focus group interviews of experts in the relevant field of child health care. It was done in Mandarin Chinese. The language validation was checked, reviewed and revised by the experts during the focus group interviews in terms of its readability and understandability. This questionnaire should be filled in by parents based on their children's sleep status in the last month. The sleep problems is defined as children with difficulties in falling asleep, frequent night awakening (more than once a night), sleep-disordered breathing, parasomnia at least 3 times a week for at least one month according to the common sleep problems of ASD children and the sleep characteristics of healthy children aged 1–3 years.
Quality control
The questionnaire and informed consent are issued by professionals who have undergone unified training, and the content and precautions of the scales are explained by use of unified guidelines. The questionnaire should be filled out by the primary caregiver of the child. After the completion of the filling, it is reviewed by professionals for on-site supplement or correction of any omission, unclear information, and incorrect filling.
Statistical analysis
The SPSS26.0 statistical software was used to analyze the data. The experimental data of this study were qualitative, expressed as percentages (%). Comparison between groups was performed by sample Chi-square test. Trend comparison of bedtime was performed by The Mann—Whitney test. The difference was statistically significant with P < 0.05.
Results
Overview of the research subjects
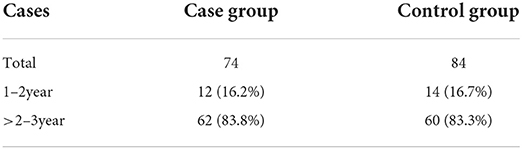
A total of 74 children (62 males, 12 females; mean age 30.62 ± 4.43 months) with a diagnosis of ASD and 84 healthy controls (65 males, 18 females; mean age of 30.90 ± 4.49 months) of the same age and sex were enrolled. No statistical significance in age and sex ratio existed between the two groups of children (P > 0.05), indicating comparability (Table 1).
Comparison of the incidence of sleep problems between the case group and the control group
The incidence of sleep problems in the case group was 78.4%, significantly higher than that in the control group (34.5%) (P < 0.001). The incidence of difficulty falling asleep (48.6%) was significantly higher than that of the control group (22.6%) (P = 0.001), and the incidence of frequent night awakenings (24.2%) was also obviously higher than that of the control group (9.5%) (P < 0.05). No statistical significance in the incidence of sleep-disordered breathing and parasomnia existed between the two groups (P > 0.05) (Table 2).
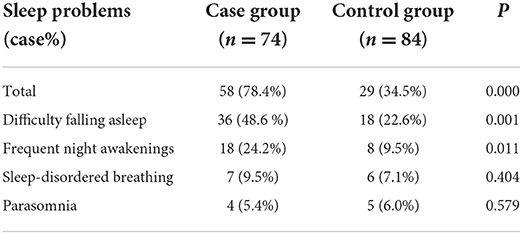
Table 2. Comparison of the incidence of sleep problems between the case group and the control group.
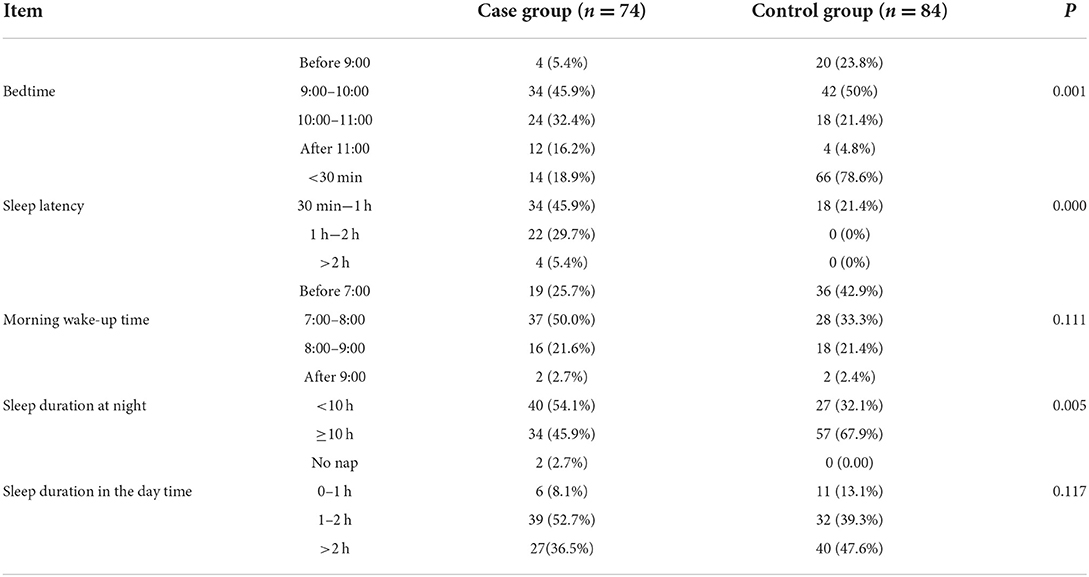
Comparison of sleep status between case group and control group
Statistical significance in the distribution of bedtime existed between the two groups, and the trend of bedtime was also statistically different (P < 0.001), indicating that the time for children to go to bed at night in the case group was obviously later than that in the control group. Compared with the control group, the children in the case group took significantly longer time to fall asleep (P < 0.001), and the sleep duration at night was less than that in the control group (P < 0.05). No statistically significant difference in awakening time in the morning and sleep duration in the daytime existed between the two groups (P > 0.05) (Table 3).
Comparison of the incidence of sleep problems between the two groups of children under different sleep behaviors and screen exposure
For the sleep pattern, the proportion of children who could fall asleep autonomously in the case group was significantly lower than that of the children in the control group, and the difference between the two groups had statistical significance (P = 0.001). In the control group, the incidence of sleep problems in children who could fall asleep autonomously was significantly lower than that in children who needed parental help (such as breastfeeding, hugging) (P < 0.05). The influence of whether the patient could fall asleep autonomously on the sleep problem was more significant in the case group than in the control group, and the difference had statistical significance (P < 0.001) (Tables 4, 5).

Table 4. Comparison of different sleep behaviors and screen exposure between case group and control group.
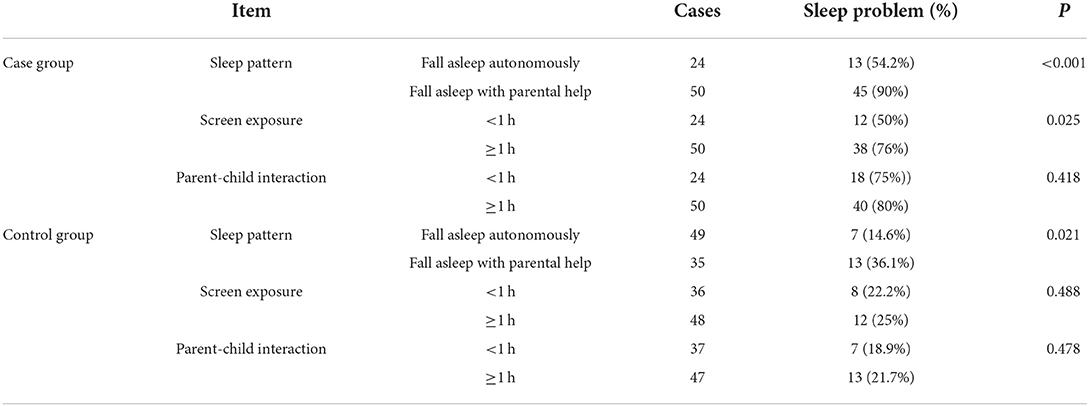
Table 5. Comparison of the incidence of sleep problems between the two groups of children under different sleep behaviors and screen exposure.
There was no statistical difference in the duration of screen exposure time existed between the case and the control groups (P > 0.05). In the case group, the longer the screen exposure time, the higher the incidence of sleep problems (P < 0.05), while the children in the control group had no statistical difference in the duration of screen exposure and the occurrence of sleep problems (P > 0.05) (Tables 4, 5).
There was no statistical difference in the duration of parent-child interaction between the case group and the control group, also no statistical in the duration of parent-child interaction and the occurrence of sleep problems in each group (P > 0.05) (Tables 4, 5).
Discussion
Children with ASD are extremely vulnerable to sleep problems due to underlying biological and behavioral rhythms that predispose them to extrinsic and intrinsic stressors that affect sleep (25). Sleep disorders may adversely affect children's daily function, thus affecting behavior, learning, memory regulation and cognition (26), and may also cause emotional problems such as aggression, irritability, over-reactivity and depression (27). Other studies have found that core symptoms also affect sleep, such as communication difficulties may exacerbate sleep disorders (28). All these problems not only reduce the quality of life, but also influence the effect of intervention. These connections all illustrate the severity of sleep problems in ASD. There is growing evidence that ASD is associated with arousal dysregulation and sensory hyper-reactivity, and calming strategies may be helpful in improving sleep (29).
Occurrence of sleep problems in ASD children aged 1–3 years
Researches have shown that children with neurodevelopmental disorders are more susceptible to sleep problems (30, 31), and ASD children have the highest incidence of 50–80% (8, 9). In this research, the incidence of sleep problems in the ASD children was 78.4%, significantly higher than that in the control group (34.5%), which was consistent with the conclusion given by Inthikoot N, et al. who found that the incidence of sleep problems in school-aged children with ASD was higher than that in typically-developing children (32). It was also higher than the incidence (67.4%) of sleep problems in ASD children aged 2–7 who underwent a large-scale multi-center study from 2018 to 2019 (33), showing that ASD children before the age of 3 also had sleep problems, and the incidence may be higher.
ASD children often suffer from comorbid sleep disorders mainly manifested as frequent night awakenings, difficulty falling asleep, late sleep habits, night terrors, excessive early awakening, short sleep duration, circadian rhythm disturbance, daytime sleepiness, sleep-disordered breathing, etc., (27). The etiology and pathogenesis are still unclear, but may be related to the influence of social environment, neurodevelopmental function, comorbidities, intestinal diseases, and respiratory diseases. It is generally believed that the interaction of biological and social or environmental factors lead to neurosecretory dysfunction and changes in sleep habits (34). A multi-center study by Hongyu Chen et al. found that the four dimensions with the highest prevalence of sleep problems in ASD children aged 2–7 were bedtime resistance (25.6%), sleep anxiety (22.7%), sleep delay (17.9%) and daytime somnolence (14.7%) (33). This study showed that difficulty falling asleep and frequent night awakenings were the most common sleep problems in ASD children aged 1–3 years with the incidence of 48.6 and 24.2%, respectively, which was obviously higher than that of the control group. Sleep-disordered breathing accounted for a small percentage of sleep problems, supporting previous findings of negligible relationship between breathing difficulties and ASD (35, 36). No statistical difference in sleep-disordered breathing and parasomnia existed between the case group and the control group. It can be seen that the manifestations of sleep problems vary in different age groups, which is determined by the sleep characteristics of different age groups. ASD children are usually excited before going to bed and cannot calm down quickly after going to bed, so they are difficult to fall asleep. These sleep problems make it even harder to foster an ASD child. For this reason, ASD children should be helped to establish good sleeping habits from an early age and create a quiet and comfortable sleeping environment. Before going to bed, they shall be provided with regular preparatory activities, and improved sleep procedures, and shall be prevented from strenuous exercise, overeating, watching cartoons so as to improve sleep.
Description of sleep status of ASD children aged 1–3 years
A growing number of researches have shown that sleep problems have a negative impact on the daily lives of ASD children (37), and will exacerbate social communication problems and repetitive behaviors (38). Sikora et al. found that sleep problems were negatively correlated with daytime behaviors in 1,193 ASD children, and ASD children had more internalized behavior problems and poorer adaptability. Children with moderate or severe sleep problems had more behavioral problems than children with mild sleep problems (39). The guidelines issued by the WHO in 2019 define sleep duration <10 h a day is insufficient sleep duration for preschoolers (40). This study showed that ASD children had later bedtime and less sleep duration, and longer time to fall asleep autonomously than that in the control group. No statistically significant difference in awakening time in the morning and sleep duration in the daytime existed between the two groups. This is consistent with the results of a study by Miano S et al. that 22.6% of children with ASDs slept for fewer than 8 h a night compared with only 9.6% of typically developing children (41). It is of great significance to timely master the sleep status of ASD children and provide targeted interventions.
Effects of different sleep patterns and parenting styles on sleep quality in ASD children aged 1–3 years
Previous studies have shown that the sleep pattern affects the occurrence of sleep problems (42, 43). This study has shown that a significant difference in sleep patterns exists between the case group and the control group, and children in the case group are more difficult to sleep autonomously. Nevertheless, the incidence of sleep problems in children who could fall asleep autonomously in both groups was lower than that in children who need parental help. Whether, ASD children could fall asleep autonomously in the case group had a more obvious impact on sleep problems than that in the control group. It can be seen that children who need help to fall asleep, such as family members' hugging, cuddling, nursing, rely on other people's support. They have a high incidence of sleep problems due to poor transition ability from mild awakening to sleep (44), and ASD children are more vulnerable. Therefore, we need to begin from the cultivation of autonomous sleep from childhood in order to improve the sleep quality of ASD children.
Screen exposure usually refers to the contact and use of electronic products such as mobile phones, computers, and TVs. With further development of scientific research, the adverse effects of screen exposure on children's sleep have also attracted the attention of scholars worldwide (45, 46). The guidelines issued by the American Academy of Pediatrics in 2016 pointed out that electronic products should not be used by children under the age of 1.5 years, and screen exposure time for children aged 2–5 years should not be exceed 1 h a day (47). This study found that screen exposure of both the case group and the control group was long, but no statistical difference existed between the two groups. More than half of children aged 1–3 years have more than an hour of screen time a day, which also reflected a bad current situation in China. Yet, with the same screen exposure, the longer the screen exposure time, the higher the incidence of sleep problems in the case group, while there is no significant difference between screen exposure time and sleep problems in the control group. It can be seen that ASD children aged 1–3 years with more screen exposure are more susceptible to sleep problems, while the exposure factor has little impact on sleep quality for typically-developing children. This will also provide a new guideline for sleep problems in ASD children aged 1–3 years. Reduced screen exposure needs to be incorporated into sleep guidelines for children with autism.
Conclusion
Our study described and discussed the sleep problems and related factors of ASD children aged 1–3 years in detail, so as to provide information for the comprehensive diagnosis and intervention of ASD children in the younger age group. The sleep status of ASD children is closely related to the pathography of autism. Moreover, ASD children aged 1–3 years have later bedtime, less sleep duration at night, difficulty falling asleep, and frequent night awakenings, which made it even harder to foster an ASD child for the guardians. We must pay sufficient attention to the sleep status of ASD children aged 1–3 years. At the same time, cultivating autonomous sleep and reducing screen exposure time can improve sleep quality of ASD children to some extent, and are also worthy of our attention when behavioral intervention improves sleep quality. In summary, sleep is an important guarantee for children's neurodevelopment and maturation. Parents and medical staff are called upon to detect sleep problems in ASD children early and conduct behavioral interventions timely in order to improve the quality of lives for ASD children and their families (48).
Limitations
The sample age of this study is limited to ASD children aged 1–3 years, so the results of this study cannot be extended to ASD patient over 3 years old. Meanwhile, this study did not analyze the intelligence level and comorbidities of the subjects. So further research is needed in this aspect. In addition, This study is essentialy based on subjective reports from parents. Objective assessment (i.e., with actigraphy or polisomnography) can be carried out in the future for in-depth research on the sleep problems of ASD children.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Children's Hospital, Zhejiang University School of Medicine. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
DY conceptualized and designed the study, enrolled patients, interpreted the data, drafted the initial manuscript, and revised the manuscript. SW enrolled patients, collated and inputted the data, conducted the analysis, and interpreted the data. FL and MG collected and reviewed the questionnaire. JS conceptualized and designed the study and reviewed and revised the manuscript for important intellectual content. All authors approved the final content of the manuscript.
Funding
This research was supported by grants from Natural Science Foundation of Zhejiang Province (LQ20H090017 to DY).
Acknowledgments
We are very grateful to all the researchers involved in the data collection as well as to the children and parents who volunteered to participate in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lord C, Brugha TS, Charman T, Cusack J, Dumas G, Frazier T, et al. Autism spectrum disorder. Nat Rev Dis Primers. (2020) 6:5. doi: 10.1038/s41572-019-0138-4
2. Centers for Disease Control and Prevention. Correction and republication: prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Morb Mortal Wkly Rep. (2018) 67:1279. Erratum for: MMWR Surveill Summ. (2016) 65:1–23. doi: 10.15585/mmwr.mm6745a7
3. Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill Summ. (2021) 70:1–16. doi: 10.15585/mmwr.ss7011a1
4. Zhu ZW, Jin Y, Wu LL, Liu XL. Current status and challenge in clinical work of autism spectrum disorders in China. World J Pediatr. (2018) 14:209–11. doi: 10.1007/s12519-018-0166-2
5. Zhou H, Xu X, Yan W, Zou X, Wu L, Luo X, et al. Prevalence of autism spectrum disorder in China: a nationwide multi-center population-based study among children aged 6 to 12 years. Neurosci Bull. (2020) 36:961–71. doi: 10.1007/s12264-020-00530-6
6. Antshel KM, Russo N. Autism spectrum disorders and ADHD: overlapping phenomenology, diagnostic issues, and treatment considerations. Curr Psychiatry Rep. (2019) 21:34. doi: 10.1007/s11920-019-1020-5
7. Galli J, Loi E, Visconti LM, Mattei P, Eusebi A, Calza S, et al. Sleep disturbances in children affected by autism spectrum disorder. Front Psychiatry. (2022) 13:736696. doi: 10.3389/fpsyt.2022.736696
8. Wang G, Liu Z, Xu G, Jiang F, Lu N, Baylor A, et al. Sleep disturbances and associated factors in Chinese children with autism spectrum disorder: a retrospective and cross-sectional study. Child Psychiatry Hum Dev. (2016) 47:248–58. doi: 10.1007/s10578-015-0561-z
9. Aathira R, Gulati S, Tripathi M, Shukla G, Chakrabarty B, Sapra S, et al. Prevalence of sleep abnormalities in Indian children with autism spectrum disorder: a cross-sectional study. Pediatr Neurol. (2017) 74:62–7. doi: 10.1016/j.pediatrneurol.2017.05.019
10. Petruzzelli MG, Matera E, Giambersio D, Marzulli L, Gabellone A, Legrottaglie AR, et al. Subjective and electroencephalographic sleep parameters in children and adolescents with autism spectrum disorder: a systematic review. J Clin Med. (2021) 10:3893. doi: 10.3390/jcm10173893
11. Blunden S, Fatima Y, Yiallourou S. Sleep health in Indigenous Australian children: a systematic review. Sleep Med. (2021) 80:305–14. doi: 10.1016/j.sleep.2021.01.065
12. Hodge D, Carollo TM, Lewin M, Hoffman CD, Sweeney DP. Sleep patterns in children with and without autism spectrum disorders: developmental comparisons. Res Dev Disabil. (2014) 35:1631–8. doi: 10.1016/j.ridd.2014.03.037
13. Sundell AL, Angelhoff C. Sleep and its relation to health-related quality of life in 3-10-year-old children. BMC Public Health. (2021) 21:1043. doi: 10.1186/s12889-021-11038-7
14. Mazurek MO, Sohl K. Sleep and behavioral problems in children with autism spectrum disorder. J Autism Dev Disord. (2016) 46:1906–15. doi: 10.1007/s10803-016-2723-7
15. Hundley RJ, Shui A, Malow BA. Relationship between subtypes of restricted and repetitive behaviors and sleep disturbance in autism spectrum disorder. J Autism Dev Disord. (2016) 46:3448–57. doi: 10.1007/s10803-016-2884-4
16. Wang Y, Lin J, Zeng Y, Liu Y, Li Y, Xia K, et al. Effects of sleep disturbances on behavioral problems in preschool children with autism spectrum disorder. Front Psychiatry. (2021) 11:559694. doi: 10.3389/fpsyt.2020.559694
17. Cortese S, Wang F, Angriman M, Masi G, Bruni O. Sleep disorders in children and adolescents with autism spectrum disorder: diagnosis, epidemiology, and management. CNS Drugs. (2020) 34:415–23. doi: 10.1007/s40263-020-00710-y
18. Romeo DM, Brogna C, Belli A, Lucibello S, Cutrona C, Apicella M, et al. Sleep disorders in autism spectrum disorder pre-school children: an evaluation using the sleep disturbance scale for children. Medicina. (2021) 57:95. doi: 10.3390/medicina57020095
19. MacLean JE, Fitzgerald DA, Waters KA. Developmental changes in sleep and breathing across infancy and childhood. Paediatr Respir Rev. (2015) 16:276–84. doi: 10.1016/j.prrv.2015.08.002
20. First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis. (2013) 201:727–9. doi: 10.1097/NMD.0b013e3182a2168a
21. Gotham K, Risi S, Pickles A, Lord C. The autism diagnostic observation schedule: revised algorithms for improved diagnostic validity. J Autism Dev Disord. (2007) 37:613–27. doi: 10.1007/s10803-006-0280-1
22. Colombi C, Fish A, Ghaziuddin M. Utility of the ADOS-2 in children with psychiatric disorders. Eur Child Adolesc Psychiatry. (2020) 29:989–92. doi: 10.1007/s00787-019-01411-8
23. Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. (2000) 23:1043–51. doi: 10.1093/sleep/23.8.1d
24. Katz T, Shui AM, Johnson CR, Richdale AL, Reynolds AM, Scahill L, et al. Modification of the children's sleep habits questionnaire for children with autism spectrum disorder. J Autism Dev Disord. (2018) 48:2629–41. doi: 10.1007/s10803-018-3520-2
25. Doldur-Balli F, Imamura T, Veatch OJ, Gong NN, Lim DC, Hart MP, et al. Synaptic dysfunction connects autism spectrum disorder and sleep disturbances: A perspective from studies in model organisms. Sleep Med Rev. (2022) 62:101595. doi: 10.1016/j.smrv.2022.101595
26. Mazzone L, Postorino V, Siracusano M, Riccioni A, Curatolo P. The relationship between sleep problems, neurobiological alterations, core symptoms of autism spectrum disorder, and psychiatric comorbidities. J Clin Med. (2018) 7:102. doi: 10.3390/jcm7050102
27. Souders MC, Zavodny S, Eriksen W, Sinko R, Connell J, Kerns C, et al. Sleep in children with autism spectrum disorder. Curr Psychiatry Rep. (2017) 19:34. doi: 10.1007/s11920-017-0782-x
28. Seo WS. An update on the cause and treatment of sleep disturbance in children and adolescents with autism spectrum disorder. Yeungnam Univ J Med. (2021) 38:275–81. doi: 10.12701/yujm.2021.01410
29. Pattison E, Papadopoulos N, Marks D, McGillivray J, Rinehart N. Behavioural treatments for sleep problems in children with autism spectrum disorder: a review of the recent literature. Curr Psychiatry Rep. (2020) 22:46. doi: 10.1007/s11920-020-01172-1
30. Robinson-Shelton A, Malow BA. Sleep disturbances in neurodevelopmental disorders. Curr Psychiatry Rep. (2016) 18:6. doi: 10.1007/s11920-015-0638-1
31. Shelton AR, Malow B. Neurodevelopmental disorders commonly presenting with sleep disturbances. Neurotherapeutics. (2021) 18:156–69. doi: 10.1007/s13311-020-00982-8
32. Inthikoot N, Chonchaiya W. Sleep problems in children with autism spectrum disorder and typical development. Pediatr Int. (2021) 63:649–57. doi: 10.1111/ped.14496
33. Chen H, Yang T, Chen J, Chen L, Dai Y, Zhang J, et al. Sleep problems in children with autism spectrum disorder: a multicenter survey. BMC Psychiatry. (2021) 21:406. doi: 10.1186/s12888-021-03405-w
34. Ballester P, Martínez MJ, Javaloyes A, Inda MD, Fernández N, Gázquez P, et al. Sleep problems in adults with autism spectrum disorder and intellectual disability. Autism Res. (2019) 12:66–79. doi: 10.1002/aur.2000
35. Limoges E, Mottron L, Bolduc C, Berthiaume C, Godbout R. Atypical sleep architecture and the autism phenotype. Brain. (2005) 128:1049–61. doi: 10.1093/brain/awh425
36. Malow BA, Marzec ML, McGrew SG, Wang L, Henderson LM, Stone WL. Characterizing sleep in children with autism spectrum disorders: a multidimensional approach. Sleep. (2006) 29:1563–71. doi: 10.1093/sleep/29.12.1563
37. Mazurek MO, Petroski GF. Sleep problems in children with autism spectrum disorder: examining the contributions of sensory over-responsivity and anxiety. Sleep Med. (2015) 16:270–9. doi: 10.1016/j.sleep.2014.11.006
38. Veatch OJ, Sutcliffe JS, Warren ZE, Keenan BT, Potter MH, Malow BA. Shorter sleep duration is associated with social impairment and comorbidities in ASD. Autism Res. (2017) 10:1221–38. doi: 10.1002/aur.1765
39. Sikora DM, Johnson K, Clemons T, Katz T. The relationship between sleep problems and daytime behavior in children of different ages with autism spectrum disorders. Pediatrics. (2012) 130 Suppl 2:S83–90. doi: 10.1542/peds.2012-0900F
40. Willumsen J, Bull F. Development of WHO guidelines on physical activity, sedentary behavior, and sleep for children less than 5 years of age. J Phys Act Health. (2020) 17:96–100. doi: 10.1123/jpah.2019-0457
41. Miano S, Bruni O, Elia M, Trovato A, Smerieri A, Verrillo E, et al. Sleep in children with autistic spectrum disorder: a questionnaire and polysomnographic study. Sleep Med. (2007) 9:64–70. doi: 10.1016/j.sleep.2007.01.014
42. Philbrook LE, Teti DM. Bidirectional associations between bedtime parenting and infant sleep: Parenting quality, parenting practices, and their interaction. J Fam Psychol. (2016) 30:431–41. doi: 10.1037/fam0000198
43. Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Med Rev. (2018) 40:93–108. doi: 10.1016/j.smrv.2017.10.007
44. Covington LB, Rogers VE, Armstrong B, Storr CL, Black MM. Toddler bedtime routines and associations with nighttime sleep duration and maternal and household factors. J Clin Sleep Med. (2019) 15:865–71. doi: 10.5664/jcsm.7838
45. Marinelli M. Impact of television on the quality of sleep in preschool children. Sleep Med. (2016) 20:138–9. doi: 10.1016/j.sleep.2015.07.011
46. Carter B, Rees P, Hale L, Bhattacharjee D, Paradkar MS. Association between portable screen-based media device access or use and sleep outcomes: a systematic review and meta-analysis. JAMA Pediatr. (2016) 170:1202–8. doi: 10.1001/jamapediatrics.2016.2341
47. Gonzalez-Nahm S, Grossman ER, Frost N, Babcock C, Benjamin-Neelon SE. Media and young minds: comparing state screen media use regulations for children under 24 months of age in early care and education to a national standard. Matern Child Health J. (2018) 22:445–53. doi: 10.1007/s10995-018-2487-0
Keywords: autism spectrum disorder, children, sleep status, sleep problems, quality, China
Citation: Yao D, Wang S, Li F, Gao M and Shao J (2022) Analysis of sleep problem in children aged 1–3 years with autism spectrum disorder in Zhejiang province, China. Front. Psychiatry 13:923757. doi: 10.3389/fpsyt.2022.923757
Received: 19 April 2022; Accepted: 01 August 2022;
Published: 30 August 2022.
Edited by:
Ho Wai Koo, Sultan Abdul Halim Hospital, MalaysiaReviewed by:
Lucia Marzulli, University of Bari Aldo Moro, ItalyHaitham Jahrami, Arabian Gulf University, Bahrain
Copyright © 2022 Yao, Wang, Li, Gao and Shao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Yao, eWFveWFvZjExJiN4MDAwNDA7emp1LmVkdS5jbg==
 Dan Yao
Dan Yao Shasha Wang
Shasha Wang