- 1Department of Psychology, Stony Brook University, Stony Brook, NY, United States
- 2School of Graduate Psychology, Pacific University, Hillsboro, OR, United States
- 3Department of Psychology, Michigan State University, Lansing, MI, United States
- 4Department of Social Work, Northern Michigan University, Marquette, MI, United States
- 5Department of Psychology, The University of British Columbia, Vancouver, BC, Canada
- 6Department of Psychology, St. John’s University, Queens, NY, United States
- 7Department of Psychiatry, Rush University Medical Center, Chicago, IL, United States
- 8Hunter-Bellevue School of Nursing, City University of New York, New York, NY, United States
Objective: To examine patterns and predictors of familiarity with transdisciplinary psychosocial (e.g., non-pharmacologic) practices for practitioners treating youths with autism spectrum disorder (ASD) in the United States.
Method: Practitioners (n = 701) from behavioral, education, medical, and mental health backgrounds who worked with youth (ages 7–22) with ASD completed the Usual Care for Autism Survey, which assessed provider demographics and self-reported familiarity with transdisciplinary treatment practices for the most common referral problems of ASD. We examined relations between provider-, setting-, and client-level characteristics with familiarity of key groups of the treatment practices (practice sets). Practice sets were identified using exploratory factor analysis (EFA), and demographic predictors of practice subsets were examined using generalized estimating equations (GEE).
Results: The EFA yielded a three-factor solution: (1) environmental modifications/antecedent strategies; (2) behavior analytic strategies; and (3) cognitive strategies, with overall familiarity ranked in this order. Medical providers indicated the least familiarity across disciplines. More experience with ASD and treating those with intellectual disabilities predicted greater familiarity with only environmental modifications/antecedent strategies and behavior analytic, but not cognitive strategies. Experience treating low SES clients predicted familiarity with environmental modification and behavior analytic strategies while experience treating high SES clients predicted familiarity with behavior analytic and cognitive strategies.
Conclusion: This is the first study to identify transdisciplinary, interpretable sets of practices for treating youth with ASD based on community providers’ reported familiarity. Results highlight factors associated with familiarity with practice sets, which is essential for mapping practice availability, and optimizing training and dissemination efforts for youth with ASD.
Introduction
The prevalence of autism spectrum disorder (ASD) continues to rise in the United States, with current estimates indicating that ASD affects 1 in 44 children (1). Due to the chronicity and severity of ASD core deficits and co-occurring challenges, youth with ASD present for mental health services at higher rates than neurotypical youth (2, 3), particularly for treatment of social skills deficits, externalizing symptoms, and anxiety, which are the most common referring problems for school-age youth with ASD (4–6). There exist many effective behavioral and medical interventions for addressing core and associated symptoms of ASD (7, 8); however, there is still a well-known gap between treatment access and need (the treatment-access gap) for youth with ASD and their families (4, 8–10). This gap is often seen in usual care settings (e.g., community mental and behavioral health clinics, schools, private outpatient therapy clinics) that provide services to school-age youth and adolescents with ASD (11–15).
Although there are many barriers to reducing the treatment-access gap, one centrally important barrier is limited provider familiarity with treatment practices (16). Familiarity with treatments permits providers to perform two core professional roles: (1) to select and deliver appropriate direct services, and/or (2) to determine appropriate referrals. Indeed, such familiarity is related to self-reported use, referral, and recommendation of interventions for youth with ASD (4, 17). When providers are unfamiliar with treatment practices important to the care of a condition, they limit their ability to perform either role—that is, familiarity is a necessary (if not sufficient) condition for increasing service access.
Providers’ training and practice backgrounds are likely one factor that facilitates familiarity with ASD-specific treatment practices (17–19). For example, service providers with educational versus medical training backgrounds may reasonably differ in exposure to common practices used in clinical settings (20, 21). However, clinical care guidelines for ASD necessitate a multi-disciplinary model integrating educational, behavioral, medical, and allied health models (18, 22, 23). Similarly, ASD providers treat individuals across a wide range of cognitive functioning, with familiarity with specific practices potentially varying as a function of client intellectual disability; for example, cognitive strategies versus some behavioral strategies may be used differentially as a function of cognitive ability. Understanding the factors that predict familiarity with treatments used in the care of individuals with ASD has potential to identify gaps in knowledge and ultimately provider training, education and collaboration, with potential to improve quality and access to care (22). Indeed, familiarity may also mediate other access-related factors, such as availability of services. That is, while services may exist and be available in a given region, if a family’s clinician or provider is not aware of or familiar with them, they will in turn not refer to them.
This study offers the first comprehensive picture of the current landscape of provider familiarity with treatments for youth with ASD in usual care settings in the United States, across all disciplines that regularly treat this population. Specifically, this study sought to: (a) identify treatment practice sets with which providers across disciplines report familiarity (using common language that can be understood by practitioners regardless of discipline, rather than discipline-specific jargon) in treating youth with ASD; (b) determine which provider-level (discipline, educational attainment, years providing services, practice settings) and client-level [presence of client intellectual disability (ID) and client SES] characteristics predict familiarity with treatment practice sets for youth with ASD.
Materials and methods
Participants
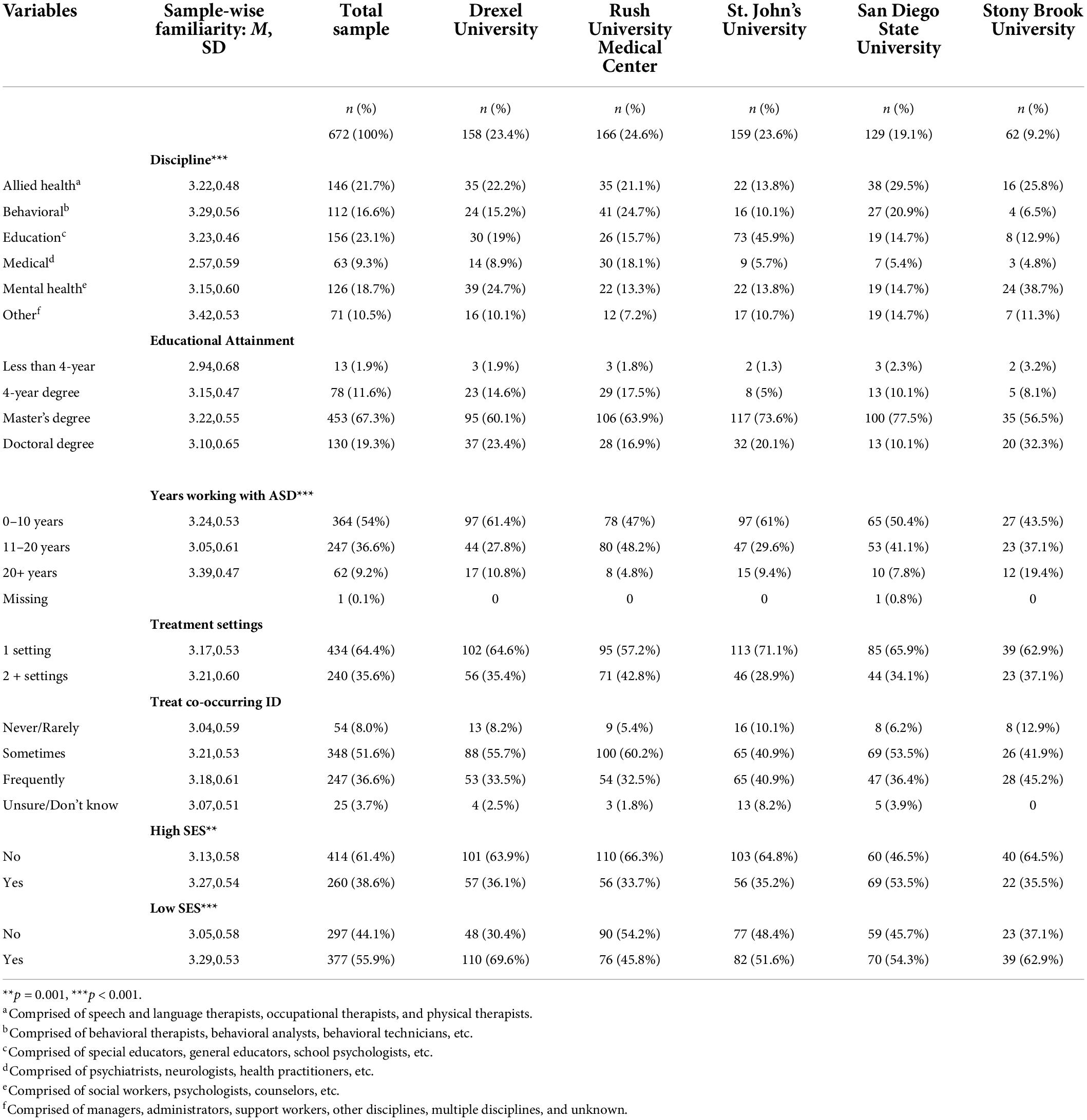
Participants targeted for recruitment included United States community-based behavioral, educational, medical, mental health, allied health, and other providers treating anxiety, externalizing behaviors, or social skills deficits in youth ages 7–22 years old with ASD during the year prior to recruitment. As outlined in the original protocol paper (8), this age range was selected because it represents the broadest possible window for treating school-age and teenage youth with ASD who may still be seen in the school system. Prior to age 7, some youth with ASD may still be transitioning to formal school-age classrooms, may not have developed some of the challenges that would indicate they may be referred for treatment (e.g., anxiety; school refusal), and so may not yet be accessing services designed to address the core challenge domains that are the focus of this project. After age 22, youth with autism will have transitioned out of school-based services. Participants were eligible if they completed the screening questionnaire identifying themselves as providing services to youth with ASD (see Table 1), provided an email address, and were located within 150 miles of one of the five academic sites (Drexel University, Rush University Medical Center, St. John’s University, Stony Brook University, and San Diego State University). This radius was identified because this project aimed to maximize the likelihood of including authentic participants who worked in discrete regions with youth with ASD. This design approach was selected to maximize interpretability and clarity of results. The identified geographic radius for each site allowed each site to leverage contact networks and distribute through established community channels, in hopes of achieving this maximization goal. As such, participants were recruited through existing regional networks and affiliate agencies, followed by snowball sampling. In total, 1,827 screening surveys were completed. Of these, 1,231 provider email addresses were supplied to Princeton Survey Research Associates International (PSRAI), an independent survey firm contracted to collect the online survey data. Of the 1,231 providers recruited to participate, 701 providers (56.9%) completed the study survey (see Data Screening below for final sample used in the present analyses). Data were collected from July 10 to October 6, 2017.
Procedure
Each academic site obtained institutional IRB approval for the study procedures and conducted recruitment activities. Each eligible respondent (determined by screening questionnaire) was emailed invitations and email reminders containing a unique URL link to access the study survey by PSRAI. Respondents who completed the survey were paid a $40 honorarium for their participation. Data were de-identified by PSRAI and provided to the academic site investigators in Fall 2017.
Measure
Usual care for youth with autism survey (7, 8)
The web-based survey was comprised of demographic questions as well as an inventory of 55 treatment practices derived through a literature review and two-round Delphi poll of expert ASD providers from multiple disciplines (7, 8). This process involved identifying practices referenced in the ASD intervention literature, providing them to the expert providers across disciplines, then, crucially, taking their feedback to both add and revise wording of items to ensure comprehensibility to their specific discipline and incorporating this into the next round of the poll to ensure transdisciplinarity. For example, expert providers across disciplines differentiated between shaping (reinforcing behaviors that are closer and closer “approximations” of a desired behavior until each approximation is mastered) and reinforcement schedules (controlling the timing and frequency of rewards in order to increase a desired behavior or decrease an undesired behavior), and identified practices that may be otherwise seen as less conventional, such as non-contingent reinforcement or built in breaks. Demographic items included provider- (i.e., race, ethnicity, discipline, years of experience working with individuals with ASD), setting- (i.e., region, practice setting, single vs. multiple practice settings), and client-level characteristics [i.e., SES, intellectual disability (ID)]. Notably, several of these characteristics (e.g., provider discipline, client SES) were non-mutually exclusive [e.g., a provider could be a Board Certified Behavioral Analyst (BCBA) and a Clinical Psychologist]. This study focused on the 32 practices that were implicated, based on expert consensus (7), in the treatment of the 3 identified key treatment areas: social skills, anxiety, and externalizing behavior. The remaining 23 practices were excluded from these analyses, as they were identified by experts as specific (e.g., implicated in social skills only), rather than transdiagnostic (implicated for all 3 presenting concerns). This process was undertaken because the present manuscript aimed to focus on familiarity with—and coherent sets of—practices for ASD regardless of treatment domains indicated by the participant. If a practice was identified to be specific only to the treatment of anxiety, for instance, this would likely skew its relation to other identified practices (i.e., participants would be more familiar with it if they treated anxiety or used other anxiety-related practices, and vice versa); thus, including only transdiagnostic practices allowed for identification of practices sets likely to be most generalized to all types of practitioners who work with youth with ASD. Participants rated their familiarity with each of these practices using a 4-point Likert rating scale ranging from 1 (never heard of/not at all familiar) to 4 (very familiar with).
Data analysis plan
Data screening
We first examined the data structure to ensure that variables included in the data analysis plan met assumptions for factor analyses. Further, 27 participants were flagged by PSRAI due to concerns about participant fraud (24), and subsequently excluded due to identified differences in response patterns. The project team applied the Reflect, Expect, Analyze, Label Framework (REAL) framework (24) to identify fraudulent participants. Thus, the final sample included in the data analyses was 674 providers.
Descriptive statistics
A familiarity score for each respondent was calculated by averaging across responses on the 32 treatment practices. Analysis of variance (ANOVA) tests were performed to examine differences between provider-, client-, and setting-level demographic contrasts on familiarity. Because demographic variables were non-mutually exclusive, such contrasts represent conditional variables rather than person-level effects. When an ANOVA yielded a significant F statistic, multiple pairwise comparisons were conducted to determine the nature of between-groups differences with Bonferroni corrections to reduce the risk of Type 1 error in multiple comparisons.
Factor analysis and factor-level comparisons
Exploratory factor analyses using WLSMV estimation and goemin rotation were run in M+ to identify converging practice sets (i.e., factors) for familiarity ratings. Once the practice sets were identified, overall average familiarity scores for each of the practice sets were calculated and compared using a series of paired-samples t-tests.
Generalized estimating equations
Generalized estimating equations—able to account for possible non-independence of participant responses—were used to identify the provider- and client-level characteristics associated with familiarity with practice sets. Accounting for site differences, we predicted average familiarity with practice sets (DVs) by the independent variables: provider discipline, educational attainment, number of years worked with youth with ASD, treatment settings, and child characteristics, including co-occurring ID, high SES background, and low SES background. We ran each GEE utilizing unstructured and independent model structures and then selected the model with the lowest QIC model criterion coefficient.
Results
Descriptive statistics
Participants indicated they were broadly “somewhat familiar” (M = 3.18, SD = 0.57) with the overall treatment practices. At the provider level (Table 1), differences emerged based on provider discipline, with MDs endorsing less familiarity than all other groups (p < 0.001). Differences in familiarity were also observed for provider experience, with mid-experience providers (i.e., 11–20 years worked) reporting less familiarity than low-experience providers (i.e., 0-10 years worked) and high-experience providers (i.e., 21+ years worked; both p < 0.001). Regarding client SES, providers who worked with high SES clients and low SES clients reported higher average familiarity than those who reported not working with each of these SES groups (p = 0.001, p < 0.001, respectively).
Factor analysis
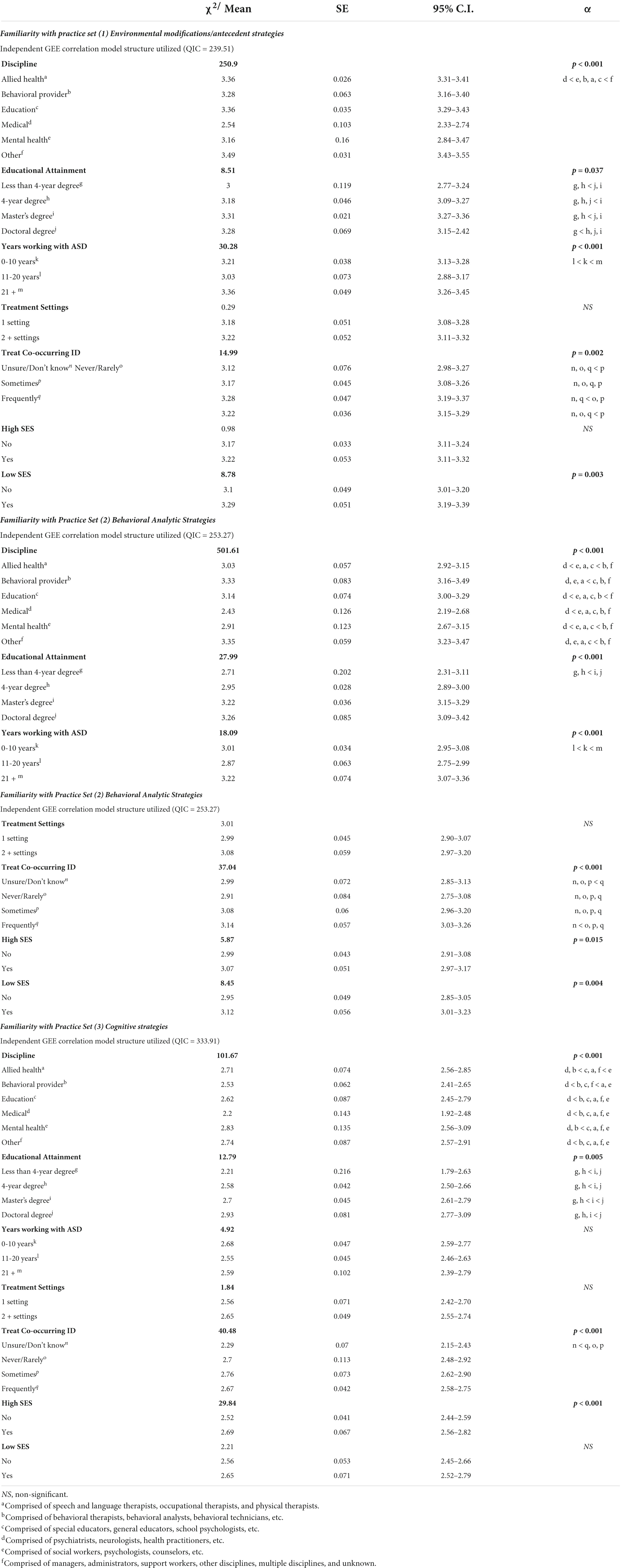
Exploratory factor analysis yielded a three-factor solution with loading patterns that accounted for 75% of the variance in item responses (Table 2). The first factor, environmental modifications/antecedent strategies, included nine items, with an overall familiarity rating of 3.34 (SD = 0.60), explaining 61% of the overall variance in familiarity. The second factor, behavior analytic strategies, included 18 items, with an overall familiarity rating of 3.20 (SD = 0.62), explaining 8% of the overall variance. The third factor, cognitive strategies, included five items, and had an overall familiarity rating of 2.84 (SD = 0.71), explaining 6% of the overall variance. Providers reported greater familiarity with the environmental modifications/antecedent strategies practice set than with the behavior analytic strategies practice set, which in turn had greater familiarity than the cognitive strategies practice set.
Comparative GEE analyses
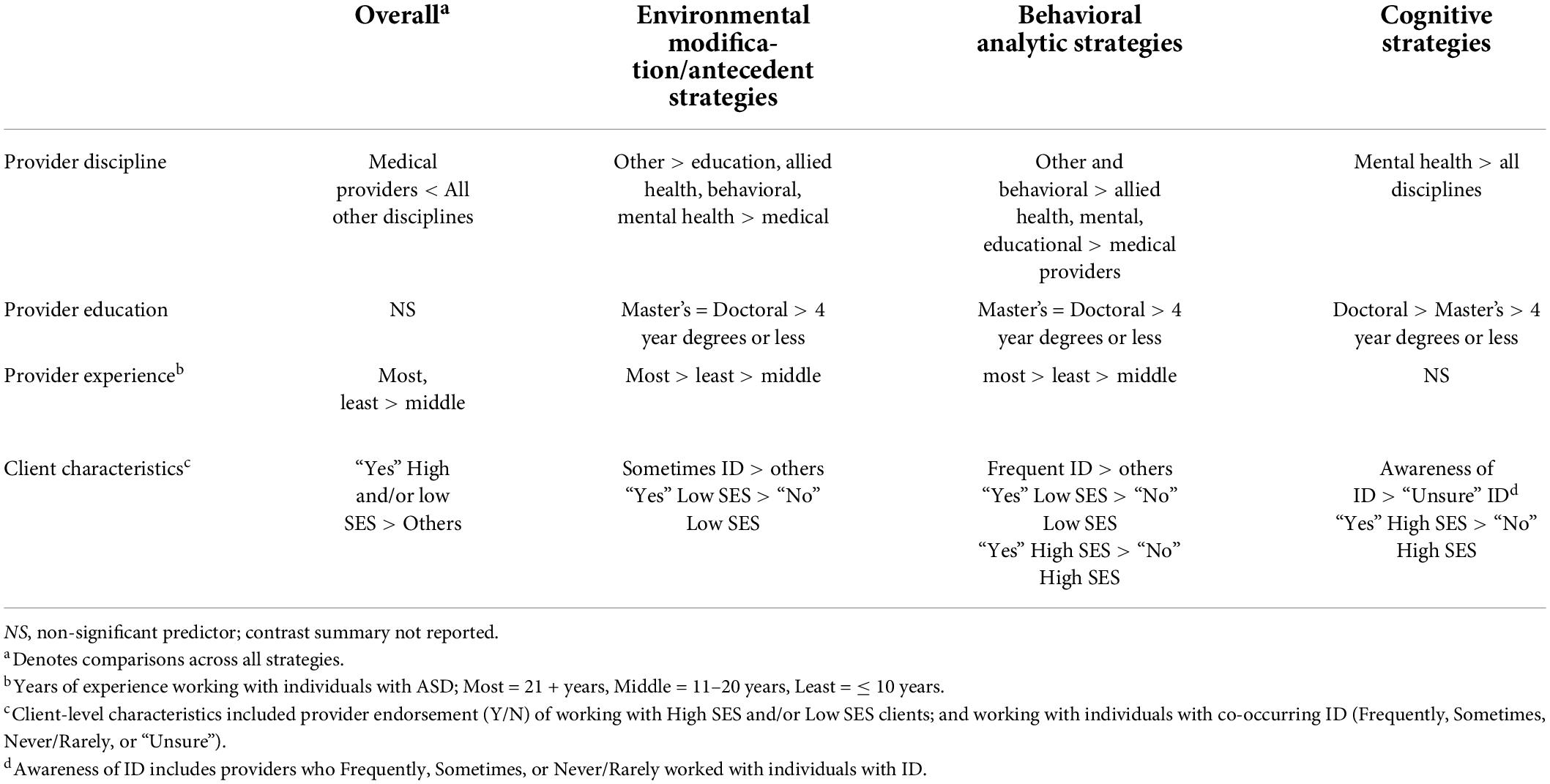
See Table 3 for selected model correlation structures and QIC coefficients. See Table 4 for a summary of the overall patterns of effects across contrast categories.
Environmental modifications/antecedent strategies
Provider familiarity with environmental modifications/antecedent strategies was predicted by: provider discipline, educational attainment, years working with individuals with ASD, and client characteristics including co-occurring ID and low SES. Post hoc analyses found that providers from the “other” discipline (i.e., managers, administrators, support workers, other disciplines, multiple disciplines, and unknown) category were more familiar with environmental modifications/antecedent strategies than all discretely-defined disciplines; medical providers were least familiar with this practice set as compared to all other disciplines. No statistically significant differences were found between non-medical providers on familiarity with environmental modifications/antecedent strategies.
Providers with master’s degrees reported greater familiarity with this practice set relative to providers with 4-year and less than 4-year degrees, whereas providers with doctoral degrees were only more familiar with environmental modifications/antecedent strategies than providers with less than 4-year degrees. In terms of years of experience, providers with ≥21 years of experience were the most familiar with this practice set, followed by providers with the least number of years (0–10 years) and then providers in the middle range of experience (11–20 years). Providers who sometimes work with those with co-occurring ID were generally the most likely to be familiar with this practice set, as were those who work with low SES populations.
Behavior analytic strategies
Provider familiarity with behavior analytic strategies was predicted by: provider discipline, educational attainment, years working with individuals with ASD, and client characteristics (i.e. co-occurring ID, low SES background). Post hoc analyses found that providers from the “other” discipline category were more familiar with behavior analytic strategies than the rest of the provider disciplines except for behavioral provider discipline. Providers from the behavioral discipline were more familiar with behavior analytic strategies than providers from the allied health, mental health, and medical disciplines. Providers from medical disciplines were the least familiar with behavior analytic strategies.
Providers with doctoral and master’s degrees were more familiar with this practice set than providers with 4-year degrees or less than a 4-year degree. Providers with the most experience working with individuals with ASD (≥21 years) were the most familiar with behavior analytic strategies, followed by the least experienced providers (0–10 years), and then middle range of experience (11–20 years or experience). Providers who worked frequently with individuals with co-occurring ID generally had more familiarity with this practice set, as did providers working with both low and high SES populations.
Cognitive strategies
Provider discipline, educational attainment, youth characteristics (co-occurring ID and high SES background), but not years of ASD experience significantly predicted familiarity with cognitive strategies. Post hoc analyses found that providers from mental health disciplines were the most familiar with cognitive strategies and were significantly more familiar with cognitive strategies than behavioral or medical providers.
Providers with doctoral degrees endorsed the greatest familiarity with cognitive strategies, followed by providers with master’s degrees, and then providers with less than a master’s degree. Finally, providers who were unsure if they provided services to youth with co-occurring ID were least likely to be familiar with cognitive strategies compared with providers who were sure, regardless of the frequency of such service delivery, and providers who provide services to youth with ASD from high SES backgrounds were more familiar with cognitive strategies compared to providers who did not.
Discussion
This study provides the first large-scale, multidisciplinary, comprehensive evaluation of the landscape of treatment practice familiarity for youth with ASD and co-occurring anxiety, externalizing behaviors, and social skills deficits in usual care settings in the United States. Findings suggest that common treatment practices are largely familiar to practitioners, though those with medical degrees, in middle career stages, and those who did not report treating high- or low-SES clients indicated less familiarity overall. They also suggest that such practices fall into three practice sets: environmental modification/antecedent strategies, behavior analytic strategies, and cognitive strategies. This suggests that treatment practices—rather than being discrete atomistic entities—are known to the providers (and likely available to ASD communities) in contiguous groups or packages, and such groupings are intelligible to practitioners across disciplines. That is, providers who are familiar with one practice are rarely familiar with only that practice, and the groups of practices with which practitioners are familiar tend to “hang together” in consistent and meaningful ways.
When considering the practice sets, the environmental modification/antecedent strategies (e.g., providing choices, environmental structuring, visual supports) was the one with which providers, on average, indicated themselves to be most familiar, and also the one that explained the most variance in familiarity in general. Indeed, while the three factors explain 75% of the variance in familiarity ratings (a notably high proportion in large scale surveys such as the present one), the vast majority of that variance was explained by the 9-item environmental modification/antecedent strategies factor. This suggests that, when providers report being familiar with practices to treat youth with ASD, it is likely the case that they are either primarily or also familiar with environmental modification/antecedent strategies. In fact, familiarity with environmental modification/antecedent strategies could be considered a potential proxy for overall familiarity with treatment practices for this population. Future research may capitalize on this finding by utilizing familiarity with the nine environmental modification/antecedent strategies items to gauge general familiarity with ASD treatment in novel practitioner communities. Likewise, in training settings, introducing these strategies (particularly when there is evidence to support their effectiveness) may provide valuable inroads for training ASD treatment-naïve practitioners on potential domain-general “core elements” of treating ASD (rather than, for instance, focusing on practice elements specific only to treating specific cognitive or behavioral sequelae of ASD). Such strategy introduction represents one of numerous ways of increasing familiarity, and others are worthy of exploration based on consonance with discipline-specific learning strategies. For instance, some disciplines may respond best to case studies, while others may respond to video vignettes, provision of contact information (e.g., of local providers who utilize a given strategy), or testimonials from families and individuals describing their own experience of a given strategy.
The practice sets were largely familiar to providers who serve youth with ASD and present with varied levels of educational attainment and years of experience. The relationship between provider background and familiarity with the array of treatment practices used for this population was variable depending on the practice set. For example, medical providers reported the least familiarity with all practice sets, while mental health providers were most familiar with cognitive strategies only. The relative lack of familiarity with all presented strategies among medical providers is important to highlight given that they report a lack of confidence and training in strategies to work effectively with youth with ASD, particularly when it comes to the challenging behaviors that are often exhibited by children with ASD, including during medical visits (25). Moreover, even if medical providers themselves are not directly providing these interventions, knowledge of existing practices for the population is critical for discussing treatment recommendations with families and facilitating timely referrals to appropriate services. To be sure, pediatricians and primary care providers represent the “front line” of providers who are among the first to raise concerns about ASD and facilitate referrals to additional services (26). As such, efforts to increase medical providers’ awareness and familiarity with behavioral approaches may result in improved care within the medical visits, as well as more efficient and effective care coordination and treatment access.
It is notable that having a doctoral degree did not appear to confer consistent advantages in terms of familiarity with environmental modification/antecedent strategies and behavior analytic strategies beyond a 4-year degree or less. Indeed, master’s level and doctoral level clinicians reported similar familiarity with environmental modification/antecedent strategies and behavior analytic strategies, whereas cognitive strategies were more familiar to doctoral-level providers than masters-level providers and all other groups, suggesting greater exposure to these strategies in doctoral-level training and/or continuing education. The adaptation of cognitive behavioral therapy (CBT) to individuals with ASD represents a relatively new treatment approach (27, 28); increased awareness of how cognitive strategies can be delivered to individuals with ASD might be more salient among those highly connected to research settings (e.g., doctoral level clinicians) (29, 30). In addition, while mid-career practitioners indicated the least familiarity overall, the most experienced providers (>21 years’ experience), followed by the least experienced providers (<11 years’ experience) endorsed greatest familiarity with environmental modification/antecedent and behavior analytic strategies, but not cognitive strategies, highlighting both the longer history of these strategies in the field, and their more frequent inclusion in introductory training settings.
Client-level characteristics, such as co-occurring ID and client SES, were also associated with providers’ endorsement of familiarity, although this too varied by specific practice set. Indeed, those providers who frequently or sometimes treated youth with co-occurring ID endorsed greater familiarity with the environmental modification/antecedent strategies and behavior analytic strategies practice sets relative to providers who never or rarely treated these youths. Notably, for the cognitive strategies practice set, the only familiarity differences were that providers who were unsure of whether they treated youths with ID reported less familiarity than the other providers, perhaps because these providers work in roles (e.g., supervisory) that keep them at a greater distance from individual participants and strategies used for them. That is, if a provider does not know whether they are serving ay children with ID, it may be because they are not directly interacting with those children (and may be in a supervisory role). Similarly, some practices may not require the practitioner to ascertain formal cognitive ability in the children they serve; for instance, if someone uses the “choice making” practice, they may do so regardless of whether the child they are serving can speak or not. Thus, future work should better ascertain this unusual response type and what it may denote.
For SES, those who reported treating high and/or low SES clients reported the greatest overall familiarity, though this pattern was more nuanced at the level of the practice sets. Specifically, providers who endorsed treating high SES clients reported greater familiarity with behavior analytic and cognitive strategies, perhaps because they can be provided in more individualized formats; conversely, providers who endorsed treating low SES clients reported greater familiarity with environmental modification/antecedent and behavior analytic strategies, perhaps because they are more amenable to setting-level implementation when resources are low.
Limitations
Several limitations warrant comment. First, although data were collected across five geographically distinct sites, the participant sample may not be representative of providers delivering services to youth with ASD across the entire United States. Next, this study examined only practices relevant to all three indicated referral problems, and therefore does not represent familiarity with practices specific only to a given one (e.g., video modeling for social skills). Another limitation is that our data reflect providers’ self-reported familiarity with intervention strategies as described in the UCAS—they may recognize them if exposed to them directly (e.g., via video). Further, it cannot be known whether providers correctly identified themselves as being familiar—that is, they may have stated awareness of a given practice, but perhaps might have misunderstood what was intended. Relatedly, the cell size for the group who indicated they are “unsure/don’t know” if they treat intellectual disability was small, and while this study did employ an analytic approach that mitigates site-specific effects, many in this cell happened to be from a single site. In addition, our study did not delineate between which practices or practice sets are evidence-based practices, as determined by various criteria (31, 32). Given the vast scope of practices used by practitioners from a range of professional backgrounds, the current study sought to broadly capture the landscape of familiarity of practices in general, regardless of whether the practice may be evidence-based. It will be imperative that future studies delineate between evidence-based practices and those practices with less empirical support, as the delivery of evidence-based practices to youths—especially those with ASD—represents a critical need-to-practice gap (33).
Conclusion
Overall, this study found that common treatment practices used in intervention with youth with ASD fall into three coherent familiarity practice sets, with several provider- client- and setting-related characteristics predicting differences. It also suggests that environmental modification/antecedent strategies may represent the most common or “core” practice elements representing familiarity with ASD treatment practices. Given the importance of familiarity for both direct service provision and service referral, variability of provider familiarity reveals several needs. First, differences in familiarity highlight the need for knowledge of practices to be broadly and regularly disseminated to providers, especially for those providers who facilitate referral to services (e.g., medical providers). Second, provider familiarity of strategies could also be improved through coordinated multidisciplinary treatment approaches and integrated care settings. Finally, training programs and their curricula—regardless of discipline—play an essential role in increasing provider familiarity with and consequent access to interventions that are used with ASD youth. These findings provide guidance on each of these fronts, offering the first mapping of familiarity with treatment practices for youth with ASD in the United States across disciplines.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Office of Research Compliance at Stony Brook University, the Institutional Review Board (IRB) at St. John’s University, the IRB at Drexel University, the IRB at Rush University’s Office of Research Affairs, and the IRB at San Diego State University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ML contributed to study conceptualization, methodology, project multisite administration, recruitment, leading statistical analyses and interpretations of results, and writing the original text. CB, AS, JT, PF, and EL contributed to statistical analysis and writing – original draft. CK, LM, AW, and EC contributed to project administration, recruitment, and data collection and review/editing of the manuscript. AD contributed to project administration and data collection, statistical analyses and results interpretation, writing the original text, and edited manuscript content and format. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Adelphi University Center for Health Innovation, Pershing Charitable Trust, the Brian Wright Memorial Autism Fund and by funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD087472 [PI: Kerns]), National Institute of Mental Health (K01MH093477 [PI: Drahota], R01MH110585 [PI: Lerner]), and the Simons Foundation (SFARI# 381283; PI: Lerner).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years – autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill Summ. (2021) 70:1–20.
2. Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. (2006) 118:e1203–11. doi: 10.1542/peds.2006-0127
3. Gurney JG, McPheeters ML, Davis MM. Parental report of health conditions and health care use among children with and without autism. Arch Pediatr Adolesc Med. (2006) 160:825. doi: 10.1001/archpedi.160.8.825
4. Brookman-Frazee L, Drahota A, Stadnick N, Palinkas LA. Therapist perspectives on community mental health services for children with autism spectrum disorders. Adm Policy Ment Health. (2012) 39:365–73. doi: 10.1007/s10488-011-0355-y
5. Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. (2008) 47:921–9. doi: 10.1097/CHI.0b013e318179964f
6. Zablotsky B, Pringle BA, Colpe LJ, Kogan MD, Rice C, Blumberg SJ. Service and treatment use among children diagnosed with autism spectrum disorders. J Dev Behav Pediatr. (2015) 36:98–105. doi: 10.1097/DBP.0000000000000127
7. Kerns CM, Moskowitz LJ, Rosen T, Drahota A, Wainer A, Josephson AR, et al. A multisite, multidisciplinary Delphi consensus study describing “usual care” intervention strategies for school-age to transition-age youth with autism. J Clin Child Adolesc Psychol. (2019) 48:S247–68. doi: 10.1080/15374416.2017.1410826
8. Wainer A, Drahota A, Cohn E, Kerns C, Lerner M, Marro B, et al. Understanding the landscape of psychosocial intervention practices for social, emotional, and behavioral challenges in youth with ASD: a study protocol. J Ment Health Res Intellect Disabil. (2017) 10:178–97. doi: 10.1080/19315864.2017.1284289
9. Brookman-Frazee L, Baker-Ericzén M, Stadnick N, Taylor R. Parent perspectives on community mental health services for children with autism spectrum disorders. J Child Fam Stud. (2012) 21:533–44. doi: 10.1007/s10826-011-9506-8
10. McLennan JD, Huculak S, Sheehan D. Brief report: pilot investigation of service receipt by young children with autistic spectrum disorders. J Autism Dev Disord. (2008) 38:1192–6. doi: 10.1007/s10803-007-0535-5
11. Narendorf SC, Shattuck PT, Sterzing PR. Mental health service use among adolescents with an autism spectrum disorder. Psychiatr Serv. (2011) 62:975–8. doi: 10.1176/ps.62.8.pss6208_0975
12. Pickard K, Meza R, Drahota A, Brikho B. They’re doing what? A brief paper on service use and attitudes in ASD community-based agencies. J Ment Health Res Intellect Disabil. (2018) 11:111–23. doi: 10.1080/19315864.2017.1408725
13. Ryan S, Lai J, Weiss JA. Mental health service use among youth with autism spectrum disorder: a comparison of two age groups. J Dev Behav Pediatr. (2018) 39:20–7. doi: 10.1097/DBP.0000000000000500
14. Shattuck PT, Roux AM, Hudson LE, Taylor JL, Maenner MJ, Trani JF. Services for adults with an autism spectrum disorder. Can J Psychiatry. (2012) 57:284–91. doi: 10.1177/070674371205700503
15. Wood JJ, McLeod BD, Klebanoff S, Brookman-Frazee L. Toward the implementation of evidence-based interventions for youth with autism spectrum disorders in schools and community agencies. Behav Ther. (2015) 46:83–95. doi: 10.1016/j.beth.2014.07.003
16. Levesque JF, Harris MF, Russell G. Patient-centered access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. (2013) 12:18. doi: 10.1186/1475-9276-12-18
17. Christon LM, Arnold CC, Myers BJ. Professionals’ reported provision and recommendation of psychosocial interventions for youth with autism spectrum disorder. Behav Ther. (2015) 46:68–82. doi: 10.1016/j.beth.2014.02.002
18. Morris R, Greenblatt A, Saini M. Healthcare providers’ experiences with autism: a scoping review. J Autism Dev Disord. (2019) 49:2374–88. doi: 10.1007/s10803-019-03912-6
19. Volkmar FR, Reichow B, Doehring P. Evidence-based practices in autism: where we are now and where we need to go. In: B Reichow, P Doehring, DV Cicchetti, FR Volkmar editors. Evidence-Based Practices and Treatments for Children With Autism. Boston, MA: Springer (2011). p. 365–91.
20. Atun-Einy O, Ben-Sasson A. Pediatric allied healthcare professionals’ knowledge and self-efficacy regarding ASD. Res Autism Spectr Disord. (2018) 47:1–13. doi: 10.1016/j.rasd.2017.12.001
21. Ghaderi G, Watson SL. “In medical school, you get far more training on medical stuff than developmental stuff”: perspectives on ASD from Ontario physicians. J Autism Dev Disord. (2019) 49:683–91. doi: 10.1007/s10803-018-3742-3
22. Carbone PS, Behl DD, Azor V, Murphy NA. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. (2010) 40:317–24. doi: 10.1007/s10803-009-0874-5
23. Swiezy N, Stuart M, Korzekwa P. Bridging for success in autism: training and collaboration across medical, educational, and community systems. Child Adolesc Psychiatr Clin N Am. (2008) 17:907–22. doi: 10.1016/j.chc.2008.06.001
24. Lawlor J, Thomas C, Guhin AT, Kenyon K, Lerner M Ucas Consortium Suspicious and fraudulent online survey participation: introducing the REAL framework. Methodol Innov. (2021) 2021:1–10. doi: 10.1177/20597991211050467
25. Bultas MW, McMillin SE, Zand DH. Reducing barriers to care in the office-based health care setting for children with autism. J Pediatr Health Care. (2016) 30:5–14. doi: 10.1016/j.pedhc.2015.08.007
26. Mazurek MO, Curran A, Burnette C, Sohl K. ECHO autism STAT: accelerating early access to autism diagnosis. J Autism Dev Disord. (2019) 49:127–37. doi: 10.1007/s10803-018-3696-5
27. Attwood T, Scarpa A. Modifications of cognitive-behavioral therapy for children and adolescents with high-functioning ASD and their common difficulties. In: A Scarpa, SW White, T Attwood editors. CBT for Children and Adolescents with High-Functioning Autism Spectrum Disorders. New York, NY: Guilford Press (2016). p. 27–44. doi: 10.1002/14651858.CD013173.pub2
28. Kerns CM, Roux AM, Connell JE, Shattuck PT. Adapting cognitive behavioral techniques to address anxiety and depression in cognitively able emerging adults on the autism spectrum. Cogn Behav Pract. (2016) 23:329–40. doi: 10.1016/j.cbpra.2016.06.002
29. Vasa RA, Keefer A, Reaven J, South M, White SW. Priorities for advancing research on youth with autism spectrum disorder and co-occurring anxiety. J Autism Dev Disord. (2018) 48:925–34. doi: 10.1007/s10803-017-3320-0
30. Winter AS, Fountain C, Cheslack-Postava K, Bearman PS. The social patterning of autism diagnoses reversed in California between 1992 and 2018. Proc Natl Acad Sci U.S.A. (2020) 117:30295–302. doi: 10.1073/pnas.2015762117
31. Steinbrenner JR, Hume K, Odom SL, Morin KL, Nowell SW, Tomaszewski B, et al. Evidence-Based Practice for Children, Youth, and Young Adults With Autism. Chapel Hill, NC: The University of North Carolina at Chapel Hill (2020). p. 143.
32. Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, et al. Evidence-based practices for children, youth, and young adults with autism spectrum disorder: a comprehensive review. J Autism Dev Disord. (2015) 45:1951–66. doi: 10.1007/s10803-014-2351-z
Keywords: autism spectrum disorder, psychosocial treatment, community-based, usual care, familiarity, treatment practices, youth
Citation: Lerner MD, Brown CE, Sridhar A, Tschida JE, Felsman P, Libsack EJ, Kerns CM, Moskowitz LJ, Soorya L, Wainer A, Cohn E and Drahota A (2022) Usual care for youth with autism spectrum disorder: Community-based providers’ reported familiarity with treatment practices. Front. Psychiatry 13:923025. doi: 10.3389/fpsyt.2022.923025
Received: 18 April 2022; Accepted: 04 July 2022;
Published: 26 July 2022.
Edited by:
David Quentin Beversdorf, University of Missouri, United StatesReviewed by:
Jill Howard, Duke University, United StatesCarla Wall, Duke University, United States, in collaboration with reviewer JH
Benjamin Black, University of Missouri, United States
Copyright © 2022 Lerner, Brown, Sridhar, Tschida, Felsman, Libsack, Kerns, Moskowitz, Soorya, Wainer, Cohn and Drahota. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew D. Lerner, bWF0dGhldy5sZXJuZXJAc3Rvbnlicm9vay5lZHU=
 Matthew D. Lerner
Matthew D. Lerner Cynthia E. Brown
Cynthia E. Brown Aksheya Sridhar
Aksheya Sridhar Jessica E. Tschida
Jessica E. Tschida Peter Felsman
Peter Felsman Erin J. Libsack1
Erin J. Libsack1 Connor M. Kerns
Connor M. Kerns Lauren J. Moskowitz
Lauren J. Moskowitz Latha Soorya
Latha Soorya Allison Wainer
Allison Wainer Amy Drahota
Amy Drahota