
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry, 29 July 2022
Sec. Sleep Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.919176
This article is part of the Research TopicThe Complex Relationship between Sleep, Rhythms, and Mood DisordersView all 7 articles
Objectives: Sleep disturbance and mental health are challenges for healthcare workers (HCWs). Especially during the COVID-19 pandemic, they experienced more severe sleep and mental health problems. However, the association between sleep disturbance and the mental health of HCWs is still controversial. This study aimed to systematically review the relationship by conducting a systematic review and meta-analysis.
Method: Two researchers retrieved the literature from Web of Science, PubMed, EMBASE, CINAHL, Psyclnfo, and Cochrane Library from the establishment of the databases until November 20, 2021. We used the New Castle-Ottawa Scale (NOS) and Agency for Healthcare Research and Quality (AHRQ) to evaluate the risk of bias in prospective research and cross-sectional research, respectively. The major exposure was HCWs’ sleep disturbance, and the major outcome was mental health. The correlation coefficients (r), regression coefficients (β) and odds ratios (OR) of the included studies were integrated.
Result: Fifty-nine studies were included for qualitative analysis, of which 30 studies could be combined and entered into quantitative analysis. There were 23 studies during the COVID-19 pandemic among the 59 included studies. The results of the meta-analysis showed that the correlation coefficient between sleep disturbance and mental health was 0.43 (95% CI: 0.39–0.47). HCWs with sleep disturbance had a 3.74 (95% CI: 2.76–5.07) times higher risk of mental health problems than those without sleep disturbance. The correlation coefficient during the COVID-19 epidemic was 0.45 (95% CI: 0.37–0.53), while it was 0.40 (95% CI: 0.36–0.44) during the non-epidemic period. Subgroup analysis compared the OR results in epidemic and non-epidemic periods of COVID-19, which were 4.48 (95% CI: 2.75–5.07) and 3.74 (95% CI: 2.74–7.32), respectively.
Conclusion: Sleep disturbance and mental health problems were positively correlated among HCWs. Particularly in the COVID-19 pandemic, more attention should be given to this issue.
Healthcare workers (HCWs) who encourage and improve most of the population’s lives are the backbone of each health system (1). Approximately 43,500,000 registered HCWs worldwide were reported from World Health Organization (WHO) publication data (2). Meanwhile, they play a key role in the control of every infectious and fatal disease. The screening, identification and treatment of clients are the responsibilities of HCWs, who are providing services for disease control 24 h a day (3). Therefore, sleep disturbances are health challenges in HCWs resulting from rotating or extended-duration shifts and other complicated work situations (4). The prevalence of these symptoms among clinical nurses was 63.9% in a cross-sectional study in China (5), while in Iran it was found that 53.1% of HCWs had sleep disturbances (6). COVID-19, which is an aggressive event in the global health system, causes more serious sleep problems in HCWs. A survey of 987 people stated that 58.8% of physicians and nurses suffered from sleep disturbance (7). In addition, 26.67% of front-line HCWs experienced severe insomnia (8).
However, HCWs, who are exposed to disease, face the transmission of infection to family members, a shortage of personal protective equipment (PPE), extended working hours and decisions about allocating limited resources to patients, have a risk of adverse mental health (9–11). It appealed that depression and anxiety prevalence among HCWs were 22.8 and 23.2%, respectively, derived from a meta-analysis including 33062 subjects (12). Meanwhile, existing literature has shown that HCWs represent the highest risk groups of depressive symptoms, suicide, and post-traumatic stress disorder (PTSD) among the general population (13–15). It leads to a high incidence of low job satisfaction, absenteeism and turnover directly (13). Hence, we should pay attention to HCWs’ mental health problems. There are numerous factors affecting mental health. Some research has shown that mental health situations can be attributed to individual, demographic, environmental, shift work, chemical and biological hazards, deficiencies in resiliency, coping strategies and sleep (16–18).
The correlation between sleep and mental health has been discovered in recent years (19, 20). It was reported that pregnant women with sleep disturbance in the 3rd trimester have a 5.27 times higher risk of depression (20). Nurses with sleep disorders had a 1.2 (95% confidence interval, CI: 1.13–1.27) times higher risk of anxiety than those without sleep problems (21). Furthermore, Yost et al. found that sleep disturbance level was positively correlated with burnout level among HCWs (r = 0.42) (22). Meanwhile, researchers have also explored the mechanism of how sleep impacts individual mental health (19). Nevertheless, there is doubt about the association between sleep disturbance and the mental health of HCWs. There is also a lack of systematic review. Therefore, we performed this research to provide evidence of enhancing HCWs’ mental health.
This systematic review was conducted and reported in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations (23). The study was registered with the International Prospective Register of Systematic Reviews (PROSPERO registration number CRD42021286163).
First, two researchers retrieved the literature from Web of Science, PubMed, EMBASE, CINAHL, Psyclnfo, and Cochrane Library from the establishment of the database until August 31, 2021. We updated the database search to November 15, 2021. The search strategy combined Medical Subject Headings (MeSH) and free text terms to identify the relevant articles. Keywords for the search were “sleep” OR “sleep wake disorder” OR “insomnia” OR “nightmare” OR “parasomnia” OR “circadian” OR “dyssomnia*” OR “chronotype” AND “healthcare workers” OR “Health Personnel” OR “Medical staff” OR “Health Care Provide” OR “Nurse” OR “Physician” AND (“Mental health” OR “mental disorders” OR “anxiety” OR “depression” OR “Stress, Psychological”). The detailed process of each database is supported in Supplementary material.
Studies were included by applying the following population-exposure-control-outcome-study design (PECOS):
(a) Population—studies of HCWs, including doctors, physicians, residents, nurses, nursing assistants, pharmacists, laboratory technologists, physical therapists, technicians, assistant healthcare staff, and other HCWs, which were not specific occupations but were classified as HCWs in the included studies.
(b) Exposure and control—data on HCWs with and without sleep disturbance during the study period. Sleep disturbance was defined as low sleep quality or short sleep duration. Sleep qualities were evaluated by subjective self-rating scales, such as the Pittsburgh Sleep Quality Index (PSQI), the Insomnia Severity Index (ISI), The PROMIS Sleep Disturbance Short Form, The Bergen Insomnia Scale (BIS), Symptom Checklist 90 (SCL-90) sleep part, Sleep Quality Scale (0–10 score), Sleep Habits Questionnaire (CHAS), Sleep Disorder Screening Questionnaire, Sleep Condition Indicator (SCI), “How many nightmares did you have that woke you up?,” “Health status (grade): “Do you have difficulty in sleeping (no/slight/serious),” Hamilton Depression Rating Scale (SIGH-D) sleep part, and some items designed by researchers. For example, what do you think of the quality of sleep? The answer was from good to very bad.
(c) Outcome—studies on mental health measurement of HCWs. Types of mental health included anxiety, burnout, depression, distress, mental health complaints, post traumatic symptom disorder (PTSD) and stress. Research tools included the Depression, Anxiety, and Stress Scale (DASS-21), Self-Rating Anxiety Scale (SAS), Short Health Anxiety Inventory (SHAI), General Anxiety Disorder-7 (GAD-7), Hospital Anxiety and Depression Scale (HADS), Goldberg Anxiety and Depression Scale (GADS), Goldberg’s General Health Questionnaire (GHQ-28), and Beck Anxiety Inventory (BAI) were used to measure anxiety levels. Burnout was estimated by the Maslach Burnout Inventory-Human Services Survey (MBI-HSS), Professional Quality of Life Scale (ProQOL-CN), Maslach Burnout Inventory-Short Form (MBI-SF), Link Burnout Questionnaire (LBQ), Index Chronic Fatigue Scale (SSICFS), 11-item Chalder Fatigue Scale (CFS), Maslach Burnout Inventory-General Survey (MBI-GS), Copenhagen Burnout Inventory (CBI), and Swedish Occupational Fatigue Inventory (SOFI). The Center for Epidemiologic Studies Depression Scale (CES-D), DASS-21, Patient Health Questionnaire-9 (PHQ-9), Core Symptoms of Depression, HADS, Goldberg’s General Health Questionnaire (GHQ-28), GADS, and Self-Rating Depression Scale (SDS) were used to assess depression levels. General Health Questionnaire-12 (GHQ-12) was used to measure distress. The MHI-5 screening test was applied to evaluate mental health complaints. The Impact of Event Scale (IES-R) and Post-traumatic Stress Disorder Checklist for DSM-5 (PCL-5) assessed PTSD. Stress level was measured by DASS-21, IES-R, Perceived Stress Scale (PSS), Diary of Ambulatory Behavioral States, and other items designed by researchers. That was “‘I felt stressed’, rated on a scale of 0 (not at all) to 4 (extremely)” and “instrument containing 10 Likert scale questions by investigator.”
(d) Study design—observational research including cohort study, case-control study and cross-sectional studies.
The exclusion criteria were as follows: (a) Studies were not reported in English; (b) Reviews, letters, case reports, protocols, conference abstracts and any article without full text; (c) Studies’ results without data; (d) Only univariate analysis for statistics; and (e) Demonstration of the effects of mental health on sleep disturbance.
First, two researchers independently read the titles and abstracts when screening relevant studies. Subsequently, they read the full texts of the literature proved potentially eligible after title and abstract screening. In the process of reading, research on the inability to analyse the correlation between sleep and mental health was excluded. To collect data from each included study, the main examiner created a unified information extraction table based on the research questions. The following data were extracted from each study: (a) Study characteristics: publication year, research time, first author name, country, study design, multi-center study or single-center study, total population included, included population sample, mean age, sex ratio, and occupation; (b) Other data: COVID-19 pandemic or not, sleep disturbance type, diagnostic sleep scale, the cut-off of the scale (if it had), the number of sleep measurements, the case number, mental health problem type, the number of mental health measurements, the case number (for mental health measurements), diagnostic mental health scale and the cut-off of the scale (if it had); and (c) Statistical data: r, 95% CI of r, OR, 95% CI of OR, β, and 95% CI of β. The data were extracted directly into the table and cut or paste functions were used as much as possible to reduce the possibility of transcription errors. To ensure completeness, each study was reviewed at least twice by the principal reviewer.
Two researchers independently evaluated the quality of the included studies according to the 8 items of the Newcastle-Ottawa Scale (NOS) for cohort studies and case-control studies. The NOS scale is composed of three dimensions and eight items with a full score of 9 points. A score less than 4 was defined as a low-quality study. A score of 4–6 was defined as a medium-quality study, and a score of ≥ 7 was defined as a high-quality study. The higher the score, the lower the risk of bias (22, 23). Quality evaluation of the cross-sectional study adopted the scale recommended by the Agency for Healthcare Research and Quality (AHRQ) (24). The scale covers 11 items. The answers include yes, no, and unclear. If the answer was “yes,” the item was judged as a 1 point. A higher score means a higher quality level. Different scores correspond to different quality levels: low quality = 0–3; medium quality = 4–7; and high quality = 8–11. If the two researchers disagreed with the literature inclusion and quality evaluation, the third researcher arbitrated. The details about the risk of bias evaluation are shown in Supplementary material.
Statistical analysis was performed by using Stata 15.0. The correlation coefficient (r), regression coefficient (β) and odds ratio (OR) were calculated. Since r does not obey the normal distribution (25), we converted it to Fisher’s Z (Zr) for the integration of statistics. To facilitate the combination of statistics, the regression coefficient (β), which came from the logistic regression model, was converted into OR. The rule for conversion was that performed according to the β power of e equal to OR. Then, the ORs were combined. If the evaluation result adopted reverse scoring, the result score was converted (26), and the data were merged. Only descriptive analysis was performed for studies in which effect sizes could not be combined.
Heterogeneity among the trials was assessed using the Chi-square test (P < 0.10, defined as indicating significant heterogeneity) or I2 (> 50% heterogeneity was indicated). If substantial heterogeneity existed, we analysed the sources of heterogeneity and decided if a random effect model was applied. Otherwise, a fixed effect model was applied. Subgroup analysis was performed to determine whether different kinds of sleep disturbance and mental health were affected during COVID-19. The studies whose research time was the pandemic period were included in the COVID-19 pandemic subgroup. Sensitivity analysis was conducted to evaluate the robustness of the results by excluding individual studies for forest plots. Publication bias was evaluated by asymmetry of the funnel plot.
The literature retrieval process based on the PRISMA flow diagram is shown in Figure 1. A total of 8,882 records were retrieved initially. After removing duplication, 74,443 records remained. A total of 7368 records were excluded after reading the abstract, and 75 studies were selected to be included in the full text screening. Finally, 59 studies were included for analysis, of which 30 studies could be combined and entered into quantitative analysis. The reasons why 29 studies could not be qualitatively analysed were as follows: (a) The statistical model of the studies using β as the research result did not use logistic regression, so β could not be transformed and merged (n = 19). Research on correlation analysis using structural equation models was also excluded (n = 4); (b) Sleep included in logistic regression was defined as a continuous variable (n = 4); and (c) There was no 95% confidence interval for β or OR (n = 2).
The basic characteristics of the studies are shown in Table 1. We found that research came from 20 countries: America (10), Brazil (1), Canada (1), China (20), Egypt (4), Ethiopia (1), Iran (2), Italy (2), Japan (2), Norway (1), Peru (1), Philippines (1), Poland (1), Romania (1), Saudi Arabia (2), Singapore (1), Spain (2), Sweden (1) andTurkey (5). The research sites were concentrated in general hospitals, and the research subjects were mainly physicians and nurses. A total of 41,566 samples were included, of which 71.35% were females (n = 29,659). There were 23 studies conducted during the COVID-19 pandemic.
The overall quality evaluation results of the study are shown in the last column of Table 1. A total of 59 observational studies were included in this systematic review, of which 55 were cross-sectional studies and 4 were cohort studies. In the cohort study, there were 3 studies (75.00%) with a quality evaluation score > 7, suggesting that most studies were of high quality. Among the 55 cross-sectional studies, 2 (3.65%) were low-quality studies, 31 (56.35%) were moderate-quality studies, and only 22 (40.00%) were high-quality studies.
Measures of sleep disturbance and mental health in the included studies are shown in Table 2. The most commonly used tools for measuring sleep disorders were the PSQI and ISI. The main tools for measuring mental health were the MBI, PHQ-9 and HAD. The statistical methods used focused on Pearson correlation, multiple linear regression and logistic regression.
For studies that reported the correlation coefficient, we combined r as the effect indicator. A total of 12 studies were included in the meta-analysis estimates of r (Figure 2). Because of the large heterogeneity of the included studies (I2 = 87.4% > 50%), RE was used to integrate the effect size. The integrated statistic r was 0.43, and the 95% CI was 0.39–0.47. The contrast of r between the epidemic and non-epidemic periods of COVID-19 is shown in Table 3. The r during the epidemic of new coronary pneumonia was 0.45 (95% CI: 0.37–0.53), while the r during the non-epidemic period was 0.40 (95% CI: 0.36–0.44). The comparison of the correlation between sleep disorders and different types of mental health is shown in Table 3. The r values of burnout, anxiety, depression, distress and mental health complaints were 0.35 (95% CI: 0.31–0.39), 0.46 (95% CI: 0.42–0.49), 0.44 (95% CI: 0.32–0.54), 0.20 (95% CI: 0.09–0.31) and 0.59 (95% CI: 0.49–0.67), respectively.
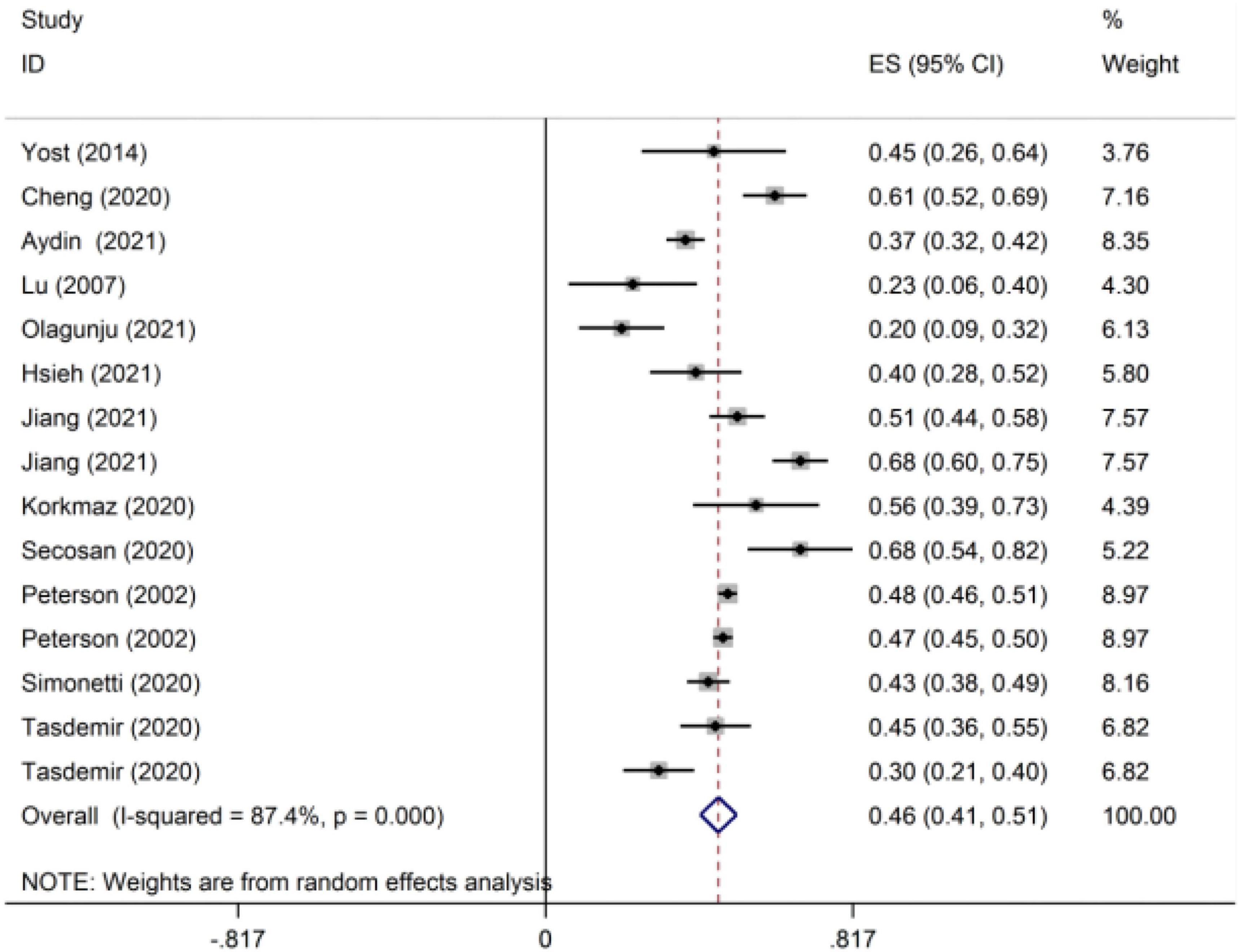
Figure 2. The meta-analytic estimates of the correlation coefficient (r)*. *The data were integrated as Fisher’s Z (Zr).
We used OR as the effect indicator for studies that reported β and OR. The meta-analysis estimate of the OR is shown in Figure 3. We chose the random effect model to combine the effect sizes resulting from I2 > 50%. The overall OR was 3.74 (95% CI: 2.76–5.07). Subgroup analysis compared the OR results in epidemic and non-epidemic periods of COVID-19, which were 4.48 (95% CI: 2.75–5.07) and 3.74 (95% CI: 2.74–7.32), respectively (Table 3). In the different subgroups of mental health types, the OR was also different (Table 3). The OR of stress was the highest (8.91, 95% CI: 2.54–31.28). Subgroup analysis compared the OR results in epidemic and non-epidemic periods of COVID-19, which were 4.48 (95% CI: 2.75–5.07) and 3.74 (95% CI: 2.74–7.32), respectively.
In this meta-analysis, each study was randomly removed to verify the sensitivity. Sensitivity analysis showed that the results of this study were stable (Figure 4).
The funnel plot of the correlation coefficient between sleep disturbance and mental health demonstrated a symmetrical distribution, indicating that there was no obvious publication bias (Figure 5A). However, the funnel plot demonstrated an asymmetrical distribution of the studies that reported ORs, indicating that there may be publication bias (Figure 5B).
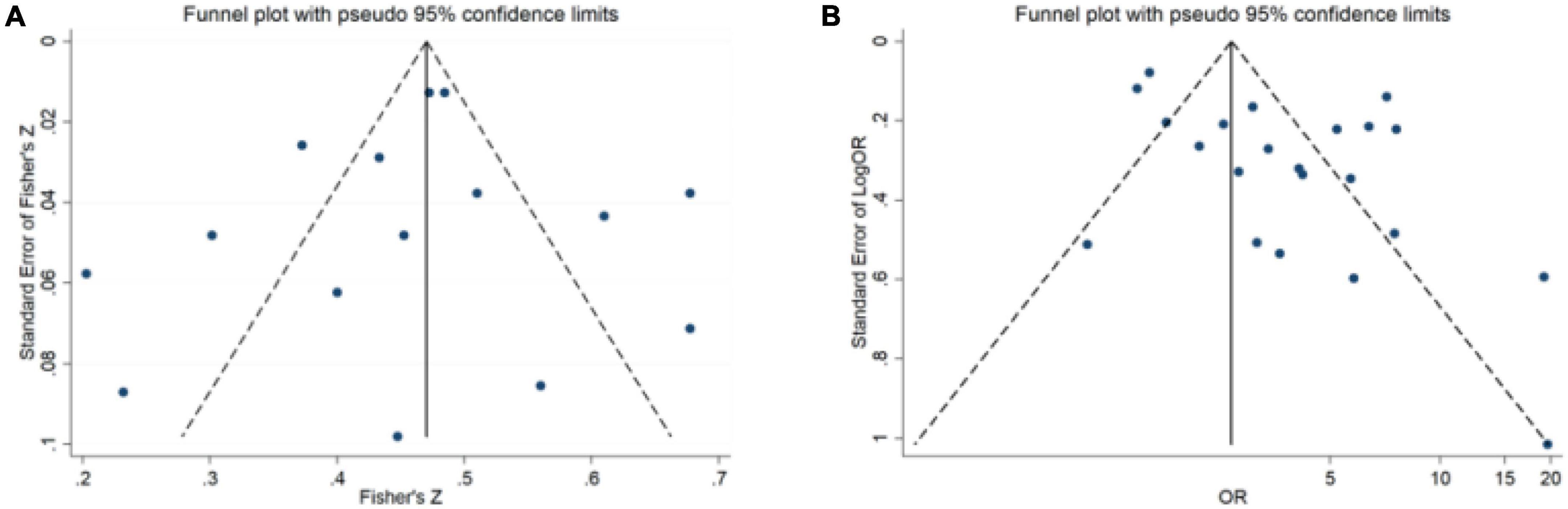
Figure 5. Publication bias analysis. (A) The studies were extracted. (B) The studies were extracted OR.
To the best of our knowledge, this meta-analysis was the first to examine the association between sleep disturbance and the mental health of HCWs. At the same time, the subgroup analysis discussed the relationship between different types of sleep disturbance and mental health, as well as sleep disturbance and different types of mental health problems. Moreover, it contrasted sleep disturbance and mental health during the COVID-19 pandemic with the non-COVID-19 pandemic. We found that the sleep disturbance level was positively correlated with mental health among HCWs. In other words, the more serious the sleep disorder, the more serious the mental health problems would be. HCWs with sleep problems have a 3.74 higher risk of mental health problems. The r during the COVID-19 epidemic was 0.46 (95% CI: 0.41–0.51), while it was 0.43 (95% CI 0.38–0.48) during the non-epidemic period. The ORs for the epidemic and non-epidemic periods of COVID-19 were 4.48 (95% CI: 2.75–5.07) and 3.74 (95% CI: 2.74–7.32), respectively. This reminded us of the importance of sleep problems among HCWs.
In the quality evaluation of these studies, 58.18% of the studies were of medium or low quality. Only 41.82% of the literature was high quality. In addition, the quantitative analysis of this study found that the heterogeneity of the study was large. This may be caused by the different questionnaires used in the included studies. The questionnaires for evaluating sleep disturbance were the PSQI and ISI, which have good reliability and validity. However, it seems necessary to choose an exact cut-off value for sleep disturbance in the face of the same population, for example, HCWs. On the one hand, it is conducive to the consistency of our judgment of the overall sleep status of HCWs. On the other hand, it further increases the uniformity of different research results. Many types of questionnaires on mental health appeared in the included studies. Some questionnaires have been used for patients (78). Whether it can be applied to HCWs remains to be determined. The evaluation items designed by the researchers themselves should also be used after testing their reliability and validity in the research. However, this part of the explanation was missing in the research we included (18, 31, 32, 42, 43, 50, 61, 75).
Regrettably, there were only four prospective studies in this meta-analysis, including one cohort study and three longitudinal studies. Due to the small number of prospective studies, the interpretation of the study results on the relationship between sleep and mental health was limited. Therefore, more high-quality prospective studies are still needed in the future.
This study found that sleep disturbance level was positively correlated with mental health problems among HCWs, of whom sleep disturbance was associated with a higher risk of mental health problems. This was like the results of (81, 82). Children with sleep disorders were 1.5 times more likely to have depression symptoms than children without sleep disorders (95% CI: 1.13–2.00). O’Callaghan’s meta-analysis result between subjective sleep and depressive symptoms among adolescents showed that r was 0.41, which was like the results of our study (82).
Recently, studies on the association between sleep disturbance and mental health have proliferated. Most studies were based on certain types of patients or healthy people (83, 84), but studies focusing on HCWs are rare. Some previous studies believe that the relationship between the two is mutual; that is, sleep disorders and mental health affect each other (85). However, there is still a lack of a unified theory and mechanism to explain the relationship. A review of studies pointed out that the underlying mechanisms include the theory of monoamine disorders, the theory of stress response change, the theory of immune system response, and the theory of neurotrophy (86). For example, the dysregulation of monoamine production and delivery is still considered to be an important factor in regulating mood, emotion, cognition, motivational behavior and stress response (87). In experimental studies of chronic sleep deprivation in animals, a reduction in monoamine production has been shown, including norepinephrine and dopamine (88). Due to the decrease in the production of monoamines in the serum, the individual’s vulnerability to mood changes leads to mental health problems (89). This provides a theoretical basis for the positive correlation between sleep disturbance and mental health. However, these mechanisms are still controversial. Therefore, future research should deeply explore the in-depth mechanism of the association between sleep disturbance and mental health.
Sleep disturbance was more closely related to mental health during the COVID-19 epidemic. HCWs with sleep disturbance had a 4.48 (95% CI: 2.74–7.32) times higher risk of mental health problems than those without sleep disorders. This result was like the result of Naglaa et al. (48). The reason may be that during the COVID-19 pandemic, HCWs had to be under long-term work-time (48). The working environment was more complex, the daily workload was greater, and the need for sleep was also higher (61). To date, with the continual state of the COVID-19 pandemic, HCWs around the world are still facing huge challenges, including a higher risk of infection, fears and worries about the epidemic, excessive work patterns, long-term isolation, coping with the patient’s negative emotions and lack of family contact (49). These factors will affect their sleep status. In addition, they were in a state of high arousal more potentially, which will seriously affect sleep (49). Kandemir et al. investigated 192 frontline HCWs in the fight against the epidemic and found that approximately 80.41% of them had sleep disturbance (69). Therefore, psychological problems were more likely to occur when sleep disturbance occurred.
In the subgroup analysis, we found that both low sleep quality and short sleep duration increased the risk of mental health problems for medical staff. Research by Furihata et al. also found that short sleep duration and poor sleep quality increase the risk of depression (51). The reason may be that poor sleep quality will increase the worry of medical staff and lead to adverse mental health events (35). Due to the short sleep duration, on the one hand, the integrity of the sleep cycle cannot be guaranteed. On the other hand, the rapid eye movement cycle in the sleep cycle may be shortened. The period of monoamine secretion is concentrated in the rapid eye movement cycle according to the theory of monoamine disorders (90). Subsequently, the reduction in serum monoamines affects the individual’s mental health.
Based on the above findings, we suggest that HCWs should put emphasis on sleep disturbance, including short duration and low quality. Actions should be taken as early as possible when the impact of sleep disturbance on individuals and lives is detected. For example, HCWs can take sleep-promoting drugs early or find ways to help them get better sleep. Of course, these methods may vary from person to person. So there is demanding for more RCT studies to verify effective measures to help HCWs to promote sleep in the future. Furthermore, administrators should allocate human resources rationally to balance individual workloads of HCWs. At the same time, it will helpful to alleviate sleep disturbance through flexible scheduling mechanism to ensure that HCWs have sufficient sleep time and rest time.
Our study has several advantages. First, the number of studies included in this review was large. The subjects of the study were HCWs, which is an important part of the health system. In the results section, the patients were divided into multiple subgroups for analysis. The results of this study laid the foundation for the subsequent formulation of interventions. For related departments, it is possible to improve the mental health of medical workers by intervening in their sleep quality or increasing their sleep time.
Nevertheless, there were still some limitations. First, we can see that this meta-analysis has highly heterogeneous. Additionally, there were few prospective studies. Therefore, there was a lack of cohort studies that can directly verify the causal relationship between sleep disturbance and mental health. In the future, more cohort studies still need to be included to further demonstrate the causal relationship between sleep disturbance and the mental health of HCWs. Third, due to the limited data defining sleep disturbance as short sleep duration, a subgroup analysis of the correlation between different sleep disturbance types and mental health was not carried out. Fourth, only literature published in English was included. Finally, only the Web of Science, PubMed, EMBASE, CINAHL, Psyclnfo, and Cochrane Library databases were searched for analyses. Hence, there may be literature that was not retrieved, which may have a potential influence on the results.
In summary, this meta-analysis mainly explored the association between sleep disturbance and the mental health of HCWs. It included 59 original studies for qualitative analysis and 30 of them for quantitative analysis. Meanwhile, sleep disturbance and mental health problems were positively correlated among HCWs. Sleep disturbance increased the risk of mental health problems. Moreover, subgroup analysis showed that sleep disturbance and mental health problems were higher during the COVID-19 pandemic. The risk of mental health problems was also elevated during this period. Therefore, the public should keep a watchful eye on HCWs’ sleep problems. Particularly in the COVID-19 epidemic today, more attention should be given to this issue.
YL designed and conducted information retrieval, risk of bias assessment, and wrote the manuscript. YL, HZ, and FJ assisted in searching the database and extracted and reviewed the data. LH and QZ finished the statistical analysis. HC and YZ supervised the design, reviewed the results, and revised the manuscript. All authors listed meet the author eligibility criteria according to the latest guidelines of the International Committee of Medical Journal Editors (ICMJE). All authors agreed with the manuscript.
We thank Prof. Roger Watson from Southwest Medical University for his excellent assistance in English language review.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.919176/full#supplementary-material
1. Anyangwe SC, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health. (2007) 4:93–100. doi: 10.3390/ijerph2007040002
2. World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. Geneva: World Health Organization (2016).
3. Aghalari Z, Dahms HU, Jafarian S, Gholinia H. Evaluation of organizational and social commitments and related factors during the coronavirus pandemic of healthcare workers in northern Iran. Glob Health. (2021) 17:12. doi: 10.1186/s12992-020-00658-0
4. Weaver MD, Robbins R, Quan SF, O’Brien CS, Viyaran NC, Czeisler CA, et al. Association of sleep disorders with physician burnout. JAMA Netw Open. (2020) 3:e2023256. doi: 10.1001/jamanetworkopen.2020.23256
5. Dong H, Zhang Q, Sun Z, Sang F, Xu Y. Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry. (2017) 17:241. doi: 10.1186/s12888-017-1402-3
6. Ghalichi L, Pournik O, Ghaffari M, Vingard E. Sleep quality among health care workers. Arch Iran Med. (2013) 16:100–3.
7. Al Maqbali M. Sleep disturbance among frontline nurses during the COVID-19 pandemic. Sleep Biol Rhythms. (2021) 19:467–73. doi: 10.1007/s41105-021-00337-6
8. Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. (2020) 26:e924085. doi: 10.12659/MSMBR.924085
9. Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 107:110247. doi: 10.1016/j.pnpbp.2021.110247
10. Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. (2020) 13:40. doi: 10.1186/s12245-020-00299-5
11. Mokhtari R, Moayedi S, Golitaleb M. COVID-19 pandemic and health anxiety among nurses of intensive care units. Int J Ment Health Nurs. (2020) 29:1275–7. doi: 10.1111/inm.12800
12. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 1591:901–7. doi: 10.1016/j.bbi.2020.05.026
13. Zhang Y, ElGhaziri M, Siddique S, Gore R, Kurowski A, Nobrega S, et al. Emotional labor and depressive symptoms among healthcare workers: the role of sleep. Work Health Saf. (2021) 69:383–93. doi: 10.1177/21650799211014768
14. Awan S, Diwan M, Aamir A, Allahuddin Z, Irfan M, Carano A, et al. Suicide in healthcare workers: determinants, challenges, and the impact of COVID-19. Front Psychiatry. (2021) 12:792925. doi: 10.3389/fpsyt.2021.792925
15. Berardis D, Fornaro M, Ventriglio A, Valchera A, Vellante F, Pettorruso M, et al. Trazodone add-on in covid-19-related selective serotonin reuptake inhibitor-resistant post-traumatic stress disorder in healthcare workers: two case reports. Clin Psychopharmacol Neurosci. (2021) 19:780–5. doi: 10.9758/cpn.2021.19.4.780
16. Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. (2018) 60:248–57. doi: 10.1097/JOM.0000000000001235
17. Centers for Disease Control and Prevention. Healthcare Workers. Atlanta, GA: Centers for Disease Control and Prevention (2017).
18. Pang Y, Fang H, Li L, Chen M, Chen Y, Chen M. Predictive factors of anxiety and depression among nurses fighting coronavirus disease 2019 in China. Int J Ment Health Nurs. (2021) 30:524–32. doi: 10.1111/inm.12817
19. Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
20. Tsai SY, Lee PL, Gordon C, Cayanan E, Lee CN. Objective sleep efficiency but not subjective sleep quality is associated with longitudinal risk of depression in pregnant women: a prospective observational cohort study. Int J Nurs Stud. (2021) 120:103966. doi: 10.1016/j.ijnurstu.2021.103966
21. Sørengaard TA, Karlsen HR, Langvik E, Pallesen S, Bjorvatn B, Waage S, et al. Insomnia as a partial mediator of the relationship between personality and future symptoms of anxiety and depression among nurses. Front Psychol. (2019) 10:901. doi: 10.3389/fpsyg.2019.00901
22. Yost MG, Johnson JC, Johns MM III, Burchett KD. Burnout among osteopathic otolaryngology residents: identification during formative training years. J Am Osteopath Assoc. (2014) 114:632–41. doi: 10.7556/jaoa.2014.128
23. Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:N71. doi: 10.1136/bmj.n71
24. Michalska da Rocha B, Rhodes S, Vasilopoulou E, Hutton P. Loneliness in psychosis: a meta-analytical review. Schizophr Bull. (2018) 44:114–25. doi: 10.1093/schbul/sbx036
25. Hedges L, Olkin I. Statistical Methods for Meta-Analysis. New York, NY: Academic Press (1985). 54 p.
26. Bland JM, Altman DG. Statistics notes. The odds ratio. BMJ. (2000) 320:1468. doi: 10.1136/bmj.320.7247.1468
27. Hillhouse J, Adler C, Walters D. A simple model of stress, burnout and symptomatology in medical residents: a longitudinal study. Psychol Health Med. (2000) 5:63–73. doi: 10.1080/135485000106016
28. Wang J, Zhang X, Yang B, Li J, Li Y, Chen Q, et al. Suicidal ideation among nurses: unique and cumulative effects of different subtypes of sleep problems. J Affect Disord. (2020) 276:600–7. doi: 10.1016/j.jad.2020.07.095
29. Fang Y, Forger DB, Frank E, Sen S, Goldstein C. Day-to-day variability in sleep parameters and depression risk: a prospective cohort study of training physicians. NPJ Digit Med. (2021) 4:28. doi: 10.1038/s41746-021-00400-z
30. Ruggiero JS. Correlates of fatigue in critical care nurses. Res Nurs Health. (2003) 26:434–44. doi: 10.1002/nur.10106
31. Lu JL. Multiple interactions of hazard exposures, role stressors and situational factors, and burnout among nurses. Int J Occup Saf Ergon. (2007) 13:73–82. doi: 10.1080/10803548.2007.11076710
32. Peterson U, Demerouti E, Bergström G, Samuelsson M, Asberg M, Nygren A. Burnout and physical and mental health among Swedish healthcare workers. J Adv Nurs. (2008) 62:84–95. doi: 10.1111/j.1365-2648.2007.04580.x
33. Rutledge T, Stucky E, Dollarhide A, Shively M, Jain S, Wolfson T, et al. A real-time assessment of work stress in physicians and nurses. Health Psychol. (2009) 28:194–200. doi: 10.1037/a0013145
34. Stucky ER, Dresselhaus TR, Dollarhide A, Shively M, Maynard G, Jain S, et al. Intern to attending: assessing stress among physicians. Acad Med. (2009) 84:251–7. doi: 10.1097/ACM.0b013e3181938aad
35. Sun W, Fu J, Chang Y, Wang L. Epidemiological study on risk factors for anxiety disorder among Chinese doctors. J Occup Health. (2012) 54:1–8. doi: 10.1539/joh.11-0169-oa
36. Aldrees TM, Aleissa S, Zamakhshary M, Badri M, Sadat-Ali M. Physician well-being: prevalence of burnout and associated risk factors in a tertiary hospital, Riyadh, Saudi Arabia. Ann Saudi Med. (2013) 33:451–6. doi: 10.5144/0256-4947.2013.451
37. Chin W, Guo YL, Hung YJ, Yang CY, Shiao JS. Short sleep duration is dose-dependently related to job strain and burnout in nurses: a cross sectional survey. Int J Nurs Stud. (2015) 52:297–306. doi: 10.1016/j.ijnurstu.2014.09.003
38. Qiao Z, Chen L, Chen M, Guan X, Wang L, Jiao Y, et al. Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: a cross-sectional study. BMC Public Health. (2016) 16:335. doi: 10.1186/s12889-016-2890-7
39. Koyama F, Yoda T, Hirao T. Insomnia and depression: Japanese hospital workers questionnaire survey. Open Med. (2017) 12:391–8. doi: 10.1515/med-2017-0056
40. Vilchez-Cornejo J, Viera-Morón RD, Larico-Calla G, Alvarez-Cutipa DC, Sánchez-Vicente JC, Taminche-Canayo R, et al. Depression and abuse during medical internships in peruvian hospitals. Rev Colomb Psiquiatr. (2020) 49:76–83. doi: 10.1016/j.rcpeng.2020.04.003
41. Cai S, Lin H, Hu X, Cai YX, Chen K, Cai WZ. High fatigue and its associations with health and work related factors among female medical personnel at 54 hospitals in Zhuhai, China. Psychol Health Med. (2018) 23:304–16. doi: 10.1080/13548506.2017.1361038
42. Vidotti V, Ribeiro RP, Galdino M, Martins JT. Burnout syndrome and shift work among the nursing staff. Rev Lat Am Enfermage. (2018) 26:e3022. doi: 10.1590/1518-8345.2550.3022
43. Wang J, Okoli C, He H, Feng F, Li J, Zhuang L, et al. Factors associated with compassion satisfaction, burnout, and secondary traumatic stress among Chinese nurses in tertiary hospitals: a cross-sectional study. Int J Nurs Stud. (2020) 102:103472. doi: 10.1016/j.ijnurstu.2019.103472
44. Ibrahim AY, Chamsi Basha A, Saquib J, Zaghloul MS, Al-Mazrou A, Saquib N. Sleep duration is associated with depressive symptoms among expatriate nurses. J Affect Disord. (2019) 257:658–61. doi: 10.1016/j.jad.2019.07.073
45. Dai C, Qiu H, Huang Q, Hu P, Hong X, Tu J, et al. The effect of night shift on sleep quality and depressive symptoms among Chinese nurses. Neuropsychiatr Dis Treat. (2019) 15:435–40. doi: 10.2147/NDT.S190689
46. Ghasemi F, Samavat P, Soleimani F. The links among workload, sleep quality, and fatigue in nurses: a structural equation modeling approach. Fatigue. (2019) 7:141–52. doi: 10.1080/21641846.2019.1652422
47. Aydin Sayilan A, Kulakaç N, Uzun S. Burnout levels and sleep quality of COVID-19 heroes. Perspect Psychiatr Care. (2021) 57:1231–6. doi: 10.1111/ppc.12678
48. Youssef N, Mostafa A, Ezzat R, Yosef M, El Kassas M. Mental health status of health-care professionals working in quarantine and non-quarantine Egyptian hospitals during the COVID-19 pandemic. East Mediterr Health J. (2020) 26:1155–64. doi: 10.26719/emhj.20.116
49. Yin Q, Sun Z, Liu T, Ni X, Deng X, Jia Y, et al. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother. (2020) 27:384–95. doi: 10.1002/cpp.2477
50. Ji L, Xiaowei Z, Ling K, Yao F, Qingkun S, Jun Z. Burnout level and job satisfaction in Chinese pediatrics residents: a web-based cross-sectional study. Medicine. (2020) 99:e19249. doi: 10.1097/MD.0000000000019249
51. Furihata R, Saitoh K, Suzuki M, Jike M, Kaneita Y, Ohida T, et al. A composite measure of sleep health is associated with symptoms of depression among Japanese female hospital nurses. Compr Psychiatry. (2020) 97:152151. doi: 10.1016/j.comppsych.2019.152151
52. Cheng FF, Zhan SH, Xie AW, Cai SZ, Hui L, Kong XX, et al. Anxiety in Chinese pediatric medical staff during the outbreak of coronavirus disease 2019: a cross-sectional study. Transl Pediatr. (2020) 9:231–6. doi: 10.21037/tp.2020.04.02
53. Higgins JT, Okoli C, Otachi J, Lawrence J, Bryant ED, Lykins A, et al. Factors associated with burnout in trauma nurses. J Trauma Nurs. (2020) 27:319–26. doi: 10.1097/JTN.0000000000000538
54. Ng A, Chin WY, Wan E, Chen J, Lau CS. Prevalence and severity of burnout in Hong Kong doctors up to 20 years post-graduation: a cross-sectional study. BMJ Open. (2020) 10:e040178. doi: 10.1136/bmjopen-2020-040178
55. Ding J, Gehrman PR, Liu S, Yang F, Ma R, Jia Y, et al. Recovery experience as the mediating factor in the relationship between sleep disturbance and depressive symptoms among female nurses in Chinese public hospitals: a structural equation modeling analysis. Psychol Res Behav Manag. (2020) 13:303–11. doi: 10.2147/PRBM.S243864
56. Díaz-Ramiro EM, Rubio-Valdehita S, López-Núñez MI, Aparicio-García ME. Sleep habits as predictors of psychological health in healthcare professionals. An Psicol. (2020) 36:242. doi: 10.6018/analesps.350301
57. Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine. (2020) 99:e20769. doi: 10.1097/MD.0000000000020769
58. Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in health care workers during the COVID-19 Epidemic. A cross-sectional survey. Int J Environ Res Public Health. (2020) 17:5218. doi: 10.3390/ijerph17145218
59. Korkmaz S, Kazgan A, Çekiç S, Tartar AS, Balcı HN, Atmaca M. The anxiety levels, quality of sleep and life and problem-solving skills in healthcare workers employed in COVID-19 services. J Clin Neurosci. (2020) 80:131–6. doi: 10.1016/j.jocn.2020.07.073
60. Secosan I, Virga D, Crainiceanu ZP, Bratu T. The mediating role of insomnia and exhaustion in the relationship between secondary traumatic stress and mental health complaints among frontline medical staff during the COVID-19 pandemic. Behav Sci. (2020) 10:164. doi: 10.3390/bs10110164
61. Teo W, Yap ES, Yip C, Ong L, Lee CT. The psychological impact of COVID-19 on “hidden” frontline healthcare workers. Int J Soc Psychiatry. (2021) 67:284–9. doi: 10.1177/0020764020950772
62. Tasdemir Yigitoglu G, Yilmaz A, Yilmaz H. The effect of Covid-19 on sleep quality, anxiety and depression on healthcare staff at a tertiary hospital in Turkey. Arch Psychiatr Nurs. (2021) 35:504–10. doi: 10.1016/j.apnu.2021.07.001
63. Wang H, Dai X, Yao Z, Zhu X, Jiang Y, Li J, et al. The prevalence and risk factors for depressive symptoms in frontline nurses under COVID-19 pandemic based on a large cross-sectional study using the propensity score-matched method. BMC Psychiatry. (2021) 21:152. doi: 10.1186/s12888-021-03143-z
64. Mousavi M, Ahmadi N, Seyedhosseini Ghaheh H, Vaezi A, Javanmard SH. Psychological impact of COVID-19 on health-care workers: a multicenter cross-sectional study. J Res Med Sci. (2021) 26:77. doi: 10.4103/jrms.JRMS_1046_20
65. Simonetti V, Durante A, Ambrosca R, Arcadi P, Graziano G, Pucciarelli G, et al. Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: a large cross-sectional study. J Clin Nurs. (2021) 30:1360–71. doi: 10.1111/jocn.15685
66. Zhang R, Hou T, Kong X, Wang G, Wang H, Xu S, et al. PTSD Among healthcare workers during the COVID-19 outbreak: a study raises concern for non-medical staff in low-Risk Areas. Front Psychiatry. (2021) 12:696200. doi: 10.3389/fpsyt.2021.696200
67. Yitayih Y, Mekonen S, Zeynudin A, Mengistie E, Ambelu A. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open. (2020) 7:e1. doi: 10.1192/bjo.2020.130
68. Chen L, Lin D, Feng H. An Investigation of mental health status among medical staff following COVID-19 outbreaks: a cross-sectional study. Med Sci Monit. (2021) 27:E929454. doi: 10.12659/MSM.929454
69. Kandemir D, Temiz Z, Ozhanli Y, Erdogan H, Kanbay Y. Analysis of mental health symptoms and insomnia levels of intensive care nurses during the COVID-19 pandemic with a structural equation model. J Clin Nurs. (2022) 31:601–11. doi: 10.1111/jocn.15918
70. Aydin Guclu O, Karadag M, Akkoyunlu M, Acican T, Sertogullarindan B, Kirbas G, et al. Association between burnout, anxiety and insomnia in healthcare workers: a cross-sectional study. Psychol Health Med. (2021) 27:1117–30. doi: 10.1080/13548506.2021.1874434
71. Chang Q, Xia Y, Bai S, Zhang X, Liu Y, Yao D, et al. Association between Pittsburgh sleep quality index and depressive symptoms in chinese resident physicians. Front Psychiatry. (2021) 12:564815. doi: 10.3389/fpsyt.2021.564815
72. Mokros KJ, Leszczyński P, Nowakowska-Domagała K, Witusik A, Pietras T. Can chronotype and social jet lag predict burnout among physical therapists? Biol Rhythm Res. (2021) 52:1604–17. doi: 10.1080/09291016.2019.1678243
73. Abdelghani M, Mahdy Rehab S, El-Gohari Hayam M. Health anxiety to COVID-19 virus infection and its relationship to quality of life in a sample of health care workers in Egypt: a cross-sectional study. Arch Psychiatry Psychother. (2021) 1:19–28. doi: 10.12740/APP/130304
74. Abu-Elenin MM. Immediate psychological outcomes associated with COVID-19 pandemic in frontline physicians: a cross-sectional study in Egypt. BMC Psychiatry. (2021) 21:215. doi: 10.1186/s12888-021-03225-y
75. Abbas A, Ali A, Bahgat S, Shouman W. Prevalence, associated factors, and consequences of burnout among ICU healthcare workers: an Egyptian experience. Egypt J Chest Dis Tuberc. (2019) 68:514–25. doi: 10.4103/ejcdt.ejcdt_188_18
76. Olagunju AT, Bioku AA, Olagunju TO, Sarimiye FO, Onwuameze OE, Halbreich U. Psychological distress and sleep problems in healthcare workers in a developing context during COVID-19 pandemic: implications for workplace wellbeing. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 110:110292. doi: 10.1016/j.pnpbp.2021.110292
77. Hsieh HF, Liu Y, Hsu HT, Ma SC, Wang HH, Ko CH. Relations between stress and depressive symptoms in psychiatric nurses: the mediating effects of sleep quality and occupational burnout. Int J Environ Res Public Health. (2021) 18:7327. doi: 10.3390/ijerph18147327
78. Jiang Y, Chen J, Wang Y, Zhang X, Hong W. Sleep quality and mental health status of healthcare professionals during the outbreak of coronavirus disease 2019 (COVID-19). Psychol Health Med. (2022) 27:488–95. doi: 10.1080/13548506.2021.1954669
79. Geng S, Zhou Y, Zhang W, Lou A, Cai Y, Xie J, et al. The influence of risk perception for COVID-19 pandemic on posttraumatic stress disorder in healthcare workers: a survey from four designated hospitals. Clin Psychol Psychother. (2021) 28:1146–59. doi: 10.1002/cpp.2564
80. Garcia O, Slavish DC, Dietch JR, Messman BA, Contractor AA, Haynes PL, et al. What goes around comes around: nightmares and daily stress are bidirectionally associated in nurses. Stress Health. (2021) 37:1035–42. doi: 10.1002/smi.3048
81. Marino C, Andrade B, Campisi SC, Wong M, Zhao H, Jing X, et al. Association between disturbed sleep and depression in children and youths: a systematic review and meta-analysis of cohort studies. JAMA Netw Open. (2021) 4:e212373. doi: 10.1001/jamanetworkopen.2021.2373
82. O’Callaghan VS, Couvy-Duchesne B, Strike LT, McMahon KL, Byrne EM, Wright MJ. A meta-analysis of the relationship between subjective sleep and depressive symptoms in adolescence. Sleep Med. (2021) 79:134–44. doi: 10.1016/j.sleep.2021.01.011
83. Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. (2012) 73:e1160–7. doi: 10.4088/JCP.11r07586
84. Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. (2014) 18:521–9. doi: 10.1016/j.smrv.2014.03.006
85. Scott AJ, Webb TL, Rowse G. Does improving sleep lead to better mental health? A protocol for a meta-analytic review of randomised controlled trials. BMJ Open. (2017) 7:e016873. doi: 10.1136/bmjopen-2017-016873
86. Palagini L, Bastien CH, Marazziti D, Ellis JG, Riemann D. The key role of insomnia and sleep loss in the dysregulation of multiple systems involved in mood disorders: a proposed model. J Sleep Res. (2019) 28:e12841. doi: 10.1111/jsr.12841
87. Chaudhury D, Liu H, Han MH. Neuronal correlates of depression. Cell Mol Life Sci. (2015) 72:4825–48. doi: 10.1007/s00018-015-2044-6
88. Monti JM. The structure of the dorsal raphe nucleus and its relevance to the regulation of sleep and wakefulness. Sleep Med Rev. (2010) 14:307–17. doi: 10.1016/j.smrv.2009.11.004
89. Meerlo P, Havekes R, Steiger A. Chronically restricted or disrupted sleep as a causal factor in the development of depression. Curr Top Behav Neurosci. (2015) 25:459–81. doi: 10.1007/7854_2015_367
Keywords: healthcare workers, mental health, sleep, COVID-19, systematic review
Citation: Liu Y, Zhang Q, Jiang F, Zhong H, Huang L, Zhang Y and Chen H (2022) Association between sleep disturbance and mental health of healthcare workers: A systematic review and meta-analysis. Front. Psychiatry 13:919176. doi: 10.3389/fpsyt.2022.919176
Received: 13 April 2022; Accepted: 05 July 2022;
Published: 29 July 2022.
Edited by:
Agata Gabryelska, Medical University of Lodz, PolandReviewed by:
Domenico De Berardis, Mental Health Center (CSM) and Psychiatric Service of Diagnosis and Treatment (SPDC), ItalyCopyright © 2022 Liu, Zhang, Jiang, Zhong, Huang, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Zhang, eWFuZ3poYW5nMDcyOUBob3RtYWlsLmNvbQ==; Hong Chen, MTM2NjEwOTg3OEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.