
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 25 July 2022
Sec. Addictive Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.918465
 Kilian Lommer1*
Kilian Lommer1* Timo Schurr1
Timo Schurr1 Beatrice Frajo-Apor1
Beatrice Frajo-Apor1 Barbara Plattner2
Barbara Plattner2 Anna Chernova1
Anna Chernova1 Andreas Conca2
Andreas Conca2 Martin Fronthaler3
Martin Fronthaler3 Christian Haring4
Christian Haring4 Bernhard Holzner1
Bernhard Holzner1 Christian Macina5
Christian Macina5 Josef Marksteiner6
Josef Marksteiner6 Carl Miller7
Carl Miller7 Silvia Pardeller1
Silvia Pardeller1 Verena Perwanger8
Verena Perwanger8 Roger Pycha9
Roger Pycha9 Martin Schmidt10
Martin Schmidt10 Barbara Sperner-Unterweger11
Barbara Sperner-Unterweger11 Franziska Tutzer1
Franziska Tutzer1 Alex Hofer1
Alex Hofer1Introduction: Next to an increased use of alcohol, the current pandemic has been associated with increased psychological distress among the general population. Research on its effects on individuals suffering from substance use disorders (SUD) is scarce. This study aimed at expanding the existing literature on this topic with a focus on the impact of loneliness and perceived social support.
Methods: Sixty-eight people diagnosed with SUD according to ICD-10 from the Austrian state of Tyrol and from the Italian Province of South Tyrol who had been treated in a psychiatric hospital in 2019 and one hundred and thirty-six matched reference subjects of the same regional background participated in an online survey. Sociodemographic variables and scores on the Brief Symptom Checklist, the Three-Item Loneliness Scale, and the Multidimensional Scale of Perceived Social Support were collected at baseline and 5 months thereafter. Baseline took place after the first wave, while follow-up largely coincided with the second wave of the pandemic.
Results: Among both patients and the matched reference group, substance use as a means to feel better facing the pandemic rose and predicted higher levels of psychological distress. Patients were less likely to receive specific care at follow-up than at baseline and presented with a significantly higher prevalence of clinically relevant psychological distress and loneliness than the matched reference group at both assessment times. Among both groups, psychological burden remained unchanged over time. Perceived social support was generally significantly higher in the matched reference group than in patients. Loneliness and, to a lesser degree, low perceived social support predicted psychological distress.
Conclusion: These findings emphasize the need of preventive and educational measures regarding substance use behavior for both individuals suffering from SUD and those without mental health disorders.
The COVID-19 pandemic has affected societies and individuals throughout the world as it spread globally in early 2020, leading to substantial numbers of infection and death. The first cases in Italy and Austria were confirmed on January 31st and February 8th, 2020, respectively. Several weeks later, first fatalities occurred and case numbers rose substantially, prompting the responsible authorities to implement public health measures, including the disruption of various aspects of public and social life. The ensuing psychosocial stress has had severe repercussions on the general population's wellbeing (1, 2). Notably, among the general population, various measures of mental health and psychological distress have deteriorated in the course of the pandemic (3–6), which held true for healthcare professionals involved in the pandemic response as well (7, 8). Individuals suffering from psychiatric diseases have been considered particularly vulnerable in that regard (9–11).
The individual response and the capability to cope with a stressor can differ substantially between individuals. Substance consumption as a strategy to alter one's emotional state when facing stressors (12–14) has been linked to a problematic substance use at later points (14, 15) and to disadvantageous consequences for mental health (16–18). While some research has provided a more ambiguous picture (8, 19, 20), a number of investigations have shown that in the course of the pandemic, the use of alcohol (21–25) and other addictive substances (24, 26) has increased among the general population across different countries. This has in turn been associated with poor mental health (22–25). Being subjected to lockdown measures has been linked to an increased risk of hazardous drinking patterns and of alcohol use disorder (27). Furthermore, substance use appeared connected to an increased risk and severity of COVID-19 infections (28, 29) and an increase in alcohol-related emergencies has been reported (29).
Social support has generally been identified as a protective variable in the face of different kinds of stressful events (30–33) such as the recent global health crisis (34, 35). Conversely, loneliness has been shown to be a relevant predictor of distress and psychopathology (36–40). In the context of the current pandemic, the available literature suggests an association of loneliness and increased distress (41–45) as well as an association of loneliness and increased alcohol consumption (25, 46). For example, one of our recent studies in a Tyrolean sample of the general population (1) found female sex, low income, and being single as well as the use of alcohol or other substances to be associated with high psychological distress and loneliness.
Based on third variables (e.g., neuroticism, traumatic live events) (47), alcohol use disorder appears connected to a higher propensity for psychological distress (47–51). At the same time, it has been associated with low resilience (52, 53) and reduced stress tolerance (54), suggesting a particular vulnerability of affected individuals facing the pandemic. However, research on the repercussions of the current crisis on individuals suffering from substance use disorder (SUD) is relatively scarce. Communications by professionals as well as qualitative research has pointed to challenges in the treatment of SUD, particularly in regard to increased psychosocial stress and reduced access to treatment services (55–59). While some research has found an ambiguous development of consumption patterns in individuals with alcohol use disorder (AUD) (60–62) and SUD (63), a number of publications related an increased risk of relapse in patients with AUD (64–67) and an increase of addictive behavior in other SUD (68, 69). This has been linked to increased psychosocial strain due to COVID-related stressors (62, 64, 67–69) with loneliness in particular having been identified as a factor associated with higher craving (68). To expand these findings, we undertook a longitudinal study on psychological distress and its relationship with loneliness and social support in individuals suffering from SUD in comparison to a community reference group without self-reported mental health disorders. We hypothesized that substance use would increase across participant groups and that increased substance use would be associated with increased psychological distress. Furthermore, we hypothesized that patients would be more severely affected in terms of psychological distress than matched references, that the attendance of mental health infrastructure would decrease over time, and that measures of social integration would be valid predictors of wellbeing during the pandemic.
We undertook a longitudinal online survey in people with and without a history of mental health disorders in the regions of Tyrol (Austria) and South Tyrol (Italy). South Tyrol has been annexed by Italy after World War I; however, the population has similar characteristics and is comparable with Tyrol in many ways (socioeconomic context, healthcare system, etc.) (70).
Individuals with a mental health disorder aged 18 and above who had been treated in one of a number of psychiatric wards in Tyrol and South Tyrol in 2019 were invited by letter to complete the online survey. Altogether, 1,285 patients diagnosed with SUD were invited to participate, of which 87 enrolled. 68 individuals completed both baseline and follow-up surveys and were included in the analyses of the current report. 46 (67.6%) had a primary diagnosis of SUD according to ICD-10, and 22 (32.4%) had a secondary diagnosis of SUD. A majority (n = 53, 77.9%) of the patient sample had been diagnosed with alcohol use disorder, with smaller numbers of participants diagnosed with (in descending frequency) disorders due to the use of sedatives and hypnotics, multiple substances, opioids, cannabinoids and tobacco. The primary diagnosis of the majority of those with a secondary diagnosis of SUD was a mood disorder. Diagnoses were confirmed using chart information.
Additionally, a matched reference group from the general population was recruited through advertising in social and print media, flyers, and e-mail lists. Due to the public nature of parts of the recruitment scheme, it was not possible to determine the number of eligible individuals that were reached but decided not to take part in the investigation. A total of 1,646 people participated in the baseline survey [results obtained in the Tyrolean subsample are reported in Tutzer et al. (1) and Chernova et al. (71)] and were asked to provide an email address to be reminded for follow-up assessment. Participants, who met the following inclusion criteria were selected for further processing: 18 years or older, no self-reported previous diagnosis of a mental health disorder (including SUD) as well as currently no psychopharmacological and/or psychotherapeutic treatment. The obtained sample (N = 1,197), included 481 individuals which completed all relevant questionnaires (i.e., sociodemographics, BSCL, TILS, and MSPSS) at baseline and follow-up.
Since SUD prevalences are strongly associated with age and sex (72, 73), we selected a matched reference sample based on the patients' age and sex distribution. Therefore, consistently five age groups (≤34 years; 35–43 years; 44–50 years; 51–58 years; ≥59 years) among female and male participants from the previously obtained reference sample were generated. The selection procedure was realized by randomly picking (fair coin toss) individuals, falling into the corresponding age and sex group, until the intended ratio was reached.
Due to the age and sex distribution within both samples as well as an intended increase in power regarding further statistical analyses, the ratio of the patient group and matched reference group was chosen to be 1:2 (74–76). Consequently, this resulted in a total sample of 68 patients diagnosed with SUD and 136 individuals meeting the aforementioned inclusion criteria.
The study was approved by the Ethics Committee of the Medical University Innsbruck, Austria (Approval Number 1147/2020) and by the Ethics Committee of the Sanitary Agency of South Tyrol, Italy (Approval Number 83-2020). All participants provided informed consent online. At the end of the survey, they received a downloadable information sheet on professional support numbers and addresses.
Data was gathered at two time points. In Tyrol, the baseline survey (T1) was conducted between June 26th, 2020 and September 13th, 2020, in South Tyrol between September 07th, 2020 and November 22nd, 2020. The 5-month follow-up (T2) took place between November 30th, 2020 and January 24th, 2021 (Tyrol) and between February 8th, 2021 and April 4th, 2021 (South Tyrol), respectively. The different time periods for the two regions were owed to organizational reasons, however, the time interval between surveys was equal in both countries.
Data acquisition was conducted via the Computer-based Health Evaluation System (CHES) (77). In the following, only data relevant to the present report will be presented. Further data provided by study participants (including individuals suffering from other mental health disorders) have been (1, 11, 71) or will be presented in other reports.
Firstly, sociodemographic data was recorded, including age, sex, educational level, relationship and employment status, and household income. In addition, participants were asked whether they had used alcohol or other substances since the outbreak of the pandemic in order to feel better. Clinical data was recorded for patients, including psychiatric diagnoses, time passed since initial diagnosis and first inpatient treatment, and currently attended modalities of psychiatric care.
Psychological distress was assessed using the Brief Symptom Checklist (BSCL) (78), a 53-item questionnaire with a Likert scale design and items to be scored from 0 (not at all/no distress) to 4 (extremely/very strong distress). Nine dimensions of psychological distress are measured, including anger-hostility, anxiety, depression, paranoid ideation, phobic anxiety, psychoticism, somatization, interpersonal sensitivity, and obsessive-compulsiveness. From the single items, an aggregate score referred to as Global Severity Index (GSI) is derived. In accordance with the authors' recommendations, an age- and sex-based normative T-Score of ≥63 was used as cut-off to consider values indicative of clinically relevant psychological distress.
Loneliness was measured via the Three-Item Loneliness Scale (TILS), a brief scale with favorable psychometric properties (79). It consists of the questions “How often do you feel that you lack companionship?,” “How often do you feel left out?,” and “How often do you feel isolated from others?” to which the answers “Often,” “Some of the time,” and “Hardly ever or never” are suggested. Thus, scores between 3 and 9 can be attained. In accordance with previous research, scores of 5 or 6 were considered indicative of moderate loneliness, whereas scores ≥7 were defined as indicating severe loneliness (38).
Lastly, we assessed perceived social support using the Multidimensional Scale of Perceived Social Support (MSPSS) (80). It is a 12-item scale evaluating social support on the three sub-dimensions of family, friends, and significant others. Items were scored on a Likert scale with scores ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). Scores >50% indicate high perceived support.
IBM SPSS 27 (81) was used for statistical analyses. Sociodemographic data, patient and COVID-19-related aspects, critical BSCL t-values, and means of outcome variables within the patient and the matched reference group at baseline were compared by non-parametric test procedures for dichotomous and categorical/non-normally distributed metric variables (Fisher's exact test; Mann-Whitney-U test). Parametric tests were used for metric variables (t-test), when normally distributed. McNemar tests were conducted for baseline and follow-up comparison within the respective group. Initially, a pre-analysis was conducted aiming to find possible associations between the GSI of the BSCL measured at baseline and at follow-up and perceived social support (MSPSS) as well as loneliness (TILS) at baseline by means of Spearman correlations. Furthermore, these variables were analyzed regarding substance use during the COVID-19 pandemic by means of non-parametric Mann-Whitney-U test. Correlation coefficients can be interpreted as follows: r < 0.10 no correlation; r = 0.10–0.29 low correlation; r = 0.30–0.49 moderate correlation, and r ≥ 0.50 high correlation (82). For the primary analyses complete-case repeated measures ANCOVA were employed in order to account for interactions and main effects of covariates and multiple assessments on psychological distress. The patient and matched reference group were used as factor, time as variable of multiple assessments (baseline and follow-up), and substance use, perceived social support (MSPSS), and loneliness (TILS) as covariates. Reported GSI score mean values were adjusted for included covariates within the repeated measures ANCOVA model. Furthermore, a second model controlling for the matching variables (age and sex) was analyzed, in order to account for possibly introduced associations between the matching factor and the outcome. Effect sizes expressed by η2 can be interpreted as: η2 ≥ 0.01 small effect; η2 ≥ 0.06 medium effect, and η2 ≥ 0.14 large effect. Since a complete-case analysis might produce increased standard errors and significance levels compared to the larger sample, first-order autoregressive (AR1) linear mixed models were employed to validate the results obtained by variance analyses. This method uses maximum-likelihood estimation to handle missing data. Additionally, due to distinct measurement periods in Tyrol and South Tyrol at baseline and follow-up, these analyses were used to account for both the COVID-19 seven-day incidence rate and the time of measurement. Therefore, in addition to the variables described in the repeated measures ANCOVA, these two variables were included. After transforming the date of participation into the respective month, it was used as a factor. The COVID-19 7-day incidence rate at the respective day of participation in the corresponding region was included as a covariate.
Power analysis was conducted with G*Power (version 3.1.9.2) (83). It is based on the assumption of type 1 error (alpha = 0.05) and power of 1 – beta = 0.8. Calculated f effect sizes were transformed into η2. The sample of 68 patients diagnosed with SUD and 136 individuals from the matched reference group is sufficiently large to detect in a correlation analysis effect sizes of r ≥ 0.33 and r ≥ 0.23, respectively. Concerning repeated measures ANCOVA between factors analysis, with a total sample of 188 participants, an effect size of η2 ≥ 0.021 can be detected. For within factors analyses, effect sizes of η2 ≥ 0.038 (patients), and η2 ≥ 0.014 (reference group) are detectable. Regarding within and between interaction analyses, the sample is sufficiently large to detect an effect size of η2 ≥ 0.010.
Table 1 depicts baseline characteristics of both groups. In comparison to the reference group, patients reported less educational years and annual household income, being single or retired more often, being less likely to work full-time, and having a smaller flat size. The number of study participants resorting to substance use as a means to feel better in the face of the pandemic increased among both groups (significant increase in the reference group only). However, at both time points of data acquisition, a significantly higher percentage of patients indicated an increased substance use.
Within the patient group, a significant decrease in the number of subjects receiving treatment due to their psychiatric disorder was observed over time.
Table 2 depicts the findings on psychological distress, loneliness, and perceived social support. At both assessment times, significantly more patients than individuals from the reference group achieved T-scores ≥63 in six out of nine BSCL subscales (anxiety, depression, psychoticism, somatization, interpersonal sensitivity, obsessive-compulsiveness), thus suffering from clinically relevant psychological symptoms. At baseline, significantly more patients than reference participants indicated moderate loneliness, whereas at follow-up, the percentage of individuals indicating moderate loneliness had significantly decreased within the patient group and significantly increased within the matched reference group, thus leading to a significant between-group-difference. On the other hand, the percentage of individuals indicating severe loneliness was comparable between groups at baseline and significantly higher among patients at follow-up. Regarding perceived social support from family, friends, and other significant close relationships, MSPSS mean scores were generally significantly higher in individuals from the reference group than in patients. However, the percentage of individuals highly perceiving social support was comparable between groups.
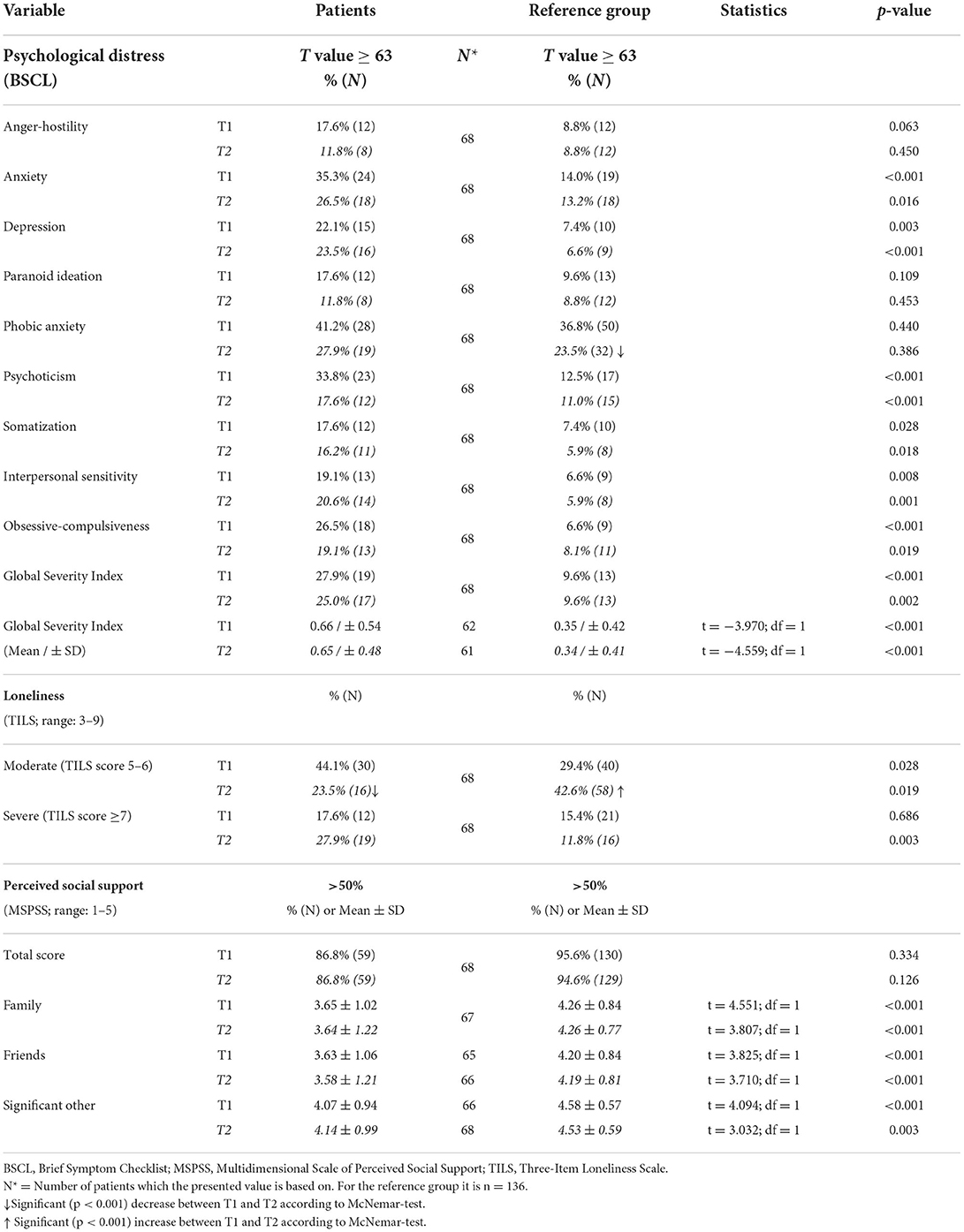
Table 2. Psychological distress, loneliness, and perceived social support at baseline (T1) and follow-up (T2).
Table 3 depicts Spearman correlations between GSI scores and covariates for patients and the reference group. The perception of social support was negatively associated with psychological distress and loneliness in patients as well as the reference group, whereas a positive association was detected between psychological distress and loneliness. According to Fisher's z transformed comparison, correlation coefficients did not differ significantly between groups.
In the matched reference group, substance use as a means to feel better in the face of the pandemic was associated with higher GSI scores at T1 (Mediannoconsume = 0.19 vs. Medianconsume = 0.47; |z| = 3.046; p = 0.002) and T2 (Mediannoconsume = 0.19 vs. Medianconsume = 0.42; |z| = 2.570; p = 0.010), whereas in the patient group, this was only the case at follow-up (Mediannoconsume = 0.49 vs. Medianconsume = 0.72; |z| = 2.160; p = 0.031). In addition, higher loneliness scores were observed in individuals from the reference group using alcohol or other substances (Mediannoconsume = 3.99 vs. Medianconsume = 6.00; |z| = 2.054; p = 0.040).
Findings of repeated measures analyses of covariance are shown in Table 4. This analysis revealed significant GSI score differences between patients and the reference group (higher scores in patients) when corrected for covariates (Meanpatients = 0.52, S.E. = 0.049; Meanreferences = 0.39, S.E. = 0.029). Substance use as well as loneliness were significant predictors (p = 0.023 and p < 0.001, respectively) of psychological distress. Testing for interactions between the individual predictor variables and time and/or group did not attain statistical significance.
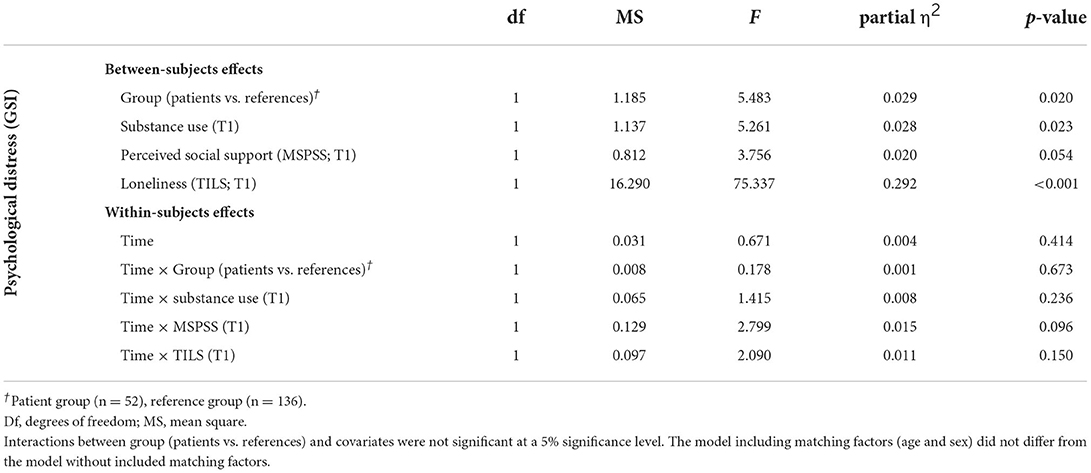
Table 4. Effect of substance use, perceived social support, and loneliness on psychological distress in patient and reference group—findings of repeated measures ANCOVA (z-standardized).
Findings for psychological distress at baseline and follow-up with adjustments for substance use, perceived social support, and loneliness are depicted in Supplementary Table 1. Here, significant differences were found between patients and individuals from the reference group (GSI T1: Meanpatients = 0.54, S.E. = 0.055; Meanreferences = 0.39, S.E. = 0.033; GSI T2: Meanpatients = 0.51, S.E. = 0.053; Meanreferencess = 0.38, S.E. = 0.031). A feeling of loneliness at baseline was the strongest predictor of psychological distress both at baseline (β = 0.246; = 0.274; p < 0.001) and at follow-up (β = 0.211; = 0.232; p < 0.001), whereas substance use arose as significant predictor of psychological distress only at baseline, but not at follow-up. In contrast, perceived social support at baseline was a significant predictor of the GSI score at follow-up only, but not at baseline.
Regarding the results of the linear mixed model analyses accounting for COVID-19 incidence rate and time of measurement, neither of the two variables were significant explanatory factors. This held true for both Tyrol and South Tyrol. Moreover, the results of the repeated measures ANCOVA described above remained unchanged, validating the complete-case analysis (see Supplementary Table 2).
With the current report, we intended to provide an account of the repercussions the pandemic has on individuals suffering from SUD. It should be noted that baseline and follow-up assessments took place during different phases of the pandemic. The baseline survey was performed in summer and fall 2020 after the first wave of infections, at which time public health measures were relatively lax compared to the regulations in the following winter, during which follow-up took place. Thus, we consider our findings to be associated with increasing psychosocial stress surrounding the pandemic situation. However, we lack pre-COVID-19 baseline measures and accordingly, causal relationships between the pandemic and people's mental health cannot be deduced from our data.
As expected, substance use was generally significantly more prevalent among patients compared to individuals from the matched reference group. However, it rose between time points among both groups. While the increase in substance use from baseline to follow-up was significant among the reference group only, this finding supports our first hypothesis and is in line with previous research from other countries (21, 23, 26, 43). Notably, our data show that across groups, substance use significantly predicted psychological distress. This is consistent with the findings of Taylor et al. (26) who reported on an association between substance use and COVID-19-related traumatic stress symptoms. While it cannot be ruled out that both substance use and psychological distress may be associated with further factors like personality traits, resilience etc., our data suggest that an increase in substance use may constitute a maladaptive coping strategy to exceptional psychosocial stress.
Our finding of reduced attendance of psychiatric and psychological/psychotherapeutic treatment facilities among SUD patients in the course of the pandemic is in line with previous findings from different countries and in varying diagnostic groups (84–88). This constitutes one of the detrimental effects of the pandemic on psychiatric care and underscores the necessity of maintaining low-threshold treatment offers.
As expected and in line with previous findings (47–51), the prevalence of clinically relevant psychological distress was significantly higher among SUD patients compared to the reference group (T1: 27.9 vs. 9.6%, T2: 25.0 vs. 9.6%). Individuals suffering from SUD generally tend to dispose of a comparatively limited amount of material and social resources (89, 90). This is reflected in the presently reported group differences in relationship status or annual household income and the more disadvantageous scores in the measures of loneliness and perceived social support. Evidence points toward a negative correlation of substance use and measures of resilience (52, 53). Thus, we expected the patient group to fare worse during the pandemic, i.e., to exhibit a comparatively larger increase in the GSI by T2. Our data did not support this hypothesis, as there was no significant effect of the time by group interaction on the GSI. As reflected in the scores of the TILS and the MSPSS, this observation might be due to the patient group enjoying less of a social network initially. Consequently, the reduction of social contacts resulting from lockdown measures could potentially not have had as profound an effect on their level of distress as among the reference group. Previous studies provide a similar picture among patients suffering from other psychiatric disorders. Pan et al. (91), for example, found that compared to healthy subjects, people with depressive, anxiety, or obsessive-compulsive disorders exhibited more pronounced psychopathology in a number of dimensions both before the pandemic and after the national lockdown in the Netherlands. Notably, symptom severity in patients increased by a lesser degree. The authors suggested greater stability encountered in everyday routines or a diminished sense of being an outsider as possible explanations, as all of society had to reduce social contacts during lockdowns (91). Similar effects could have taken place in our sample.
The prevalence of psychological distress did increase neither in SUD patients nor in individuals from the reference group over time. Previous research has shown an increase of psychological distress in the general population during the first wave of COVID-19 in spring 2020, which subsided by summer to early fall 2020 as restrictions and infection numbers were decreasing (5, 6, 44, 92). Data on psychological wellbeing during subsequent lockdowns point toward a similar mental health burden (93). Our baseline survey took place during a phase of relatively eased restrictions in 2020, while the follow-up was conducted during the second wave. Thus, a deterioration of psychological wellbeing appeared likely but could not be confirmed. This might be attributed to people having learned to adapt and cope during the first lockdown. Conversely, this observation could be connected to an ongoing sense of uncertainty and insecurity regarding people's economical and health-related outlook affecting them beyond immediate, short-term developments. Eventually, this issue cannot be sufficiently explored by the available data.
The results of the ANCOVA provided further support for the importance of a social network for psychological wellbeing. Loneliness was a highly significant factor determining the degree of psychological distress, which is consistent with previous publications showing that increased loneliness during the pandemic was associated with an increase in psychological distress or with the intensity of psychopathology (41–45). Regarding perceived social support, our findings were less conclusive. Only in an ANCOVA considering the GSI at both time points separately, perceived social support was significantly determining the GSI at follow-up. In line with previous research (34, 35), this can be interpreted as social support being a protective factor for mental health during the pandemic.
A number of limitations of the present study have to be addressed. Firstly, we repeatedly observed interesting trends in our data, which failed to reach statistical significance (e.g., increased substance use and an increase in severe loneliness over time in patients). Thus, the current investigation might have profited from a larger number of participants. Also, only a fraction of the contacted patients responded and completed both surveys, not all potential study participants may have had access to the internet and thus to the online surveys, and data was entirely self-reported, which made the current investigation prone to a number of biases. In particular, the absence of previous psychiatric conditions among individuals from the reference group could not be verified independently. Moreover, we only surveyed if participants used alcohol or other substances in response to the pandemic, while the amount and frequency as well as the type of substances used remained unclear. Further studies are needed to investigate this issue in more detail. We defined the patient group across diagnoses with a majority having been treated for alcohol use disorder. Thus, we considered a range of different conditions as a single entity, which might have led to biased conclusions or to missing effects.
Furthermore, the current data is derived from a transnational sample. As the authorities in Austria and Italy decided independently on what measures to implement and when to do so, the psychosocial stress on participants might not have been identical in both regions. Additionally, organizational reasons caused data acquisition in South Tyrol to be delayed by several weeks and accordingly, some of the baseline data was gathered when incidence rates were on the rise. In Tyrol, relatively low case numbers had been reported during the first data acquisition period (94) and substantial tightening of measures only took place after this period had ended (95). Conversely, in South Tyrol, there was a surge in infection numbers toward the end of the respective period (96), accompanied by an escalation of public health measures including tightening of curfews, business closures and domestic travel restrictions in early November toward the end of the acquisition period. However, neither the COVID-19 seven-day incidence rate nor the time of measurement were significant explanatory factors and we therefore consider it reasonable to assume that this time lag did not have relevant effects on our findings. Still, we assume that the observed changes between time points can be sensibly attributed to pandemic-related changes. Even though the incidence rates did not prove to be an explanatory factor, public health measures and the resulting effects on social embeddedness, economic uncertainties, and personal health-related worries have changed in the course of the pandemic. They clearly constitute a psychosocial burden of multifaceted nature going beyond single descriptive parameters like the incidence rate. In contrast to the described differences during the first period of data acquisition, the pandemic situation in both subpopulations were resembling each other more closely in the second. In both regions, infection rates had reached a peak before the onset of and were consistently high throughout data acquisition with a surge of numbers in Italy in early March (94, 96). In Tyrol, a strict lockdown was in place for most of the period, while in South Tyrol, wide-ranging travel restrictions, curfews and business closures were in place throughout the respective period as well as lockdown measures over the Easter holidays in early April.
Lastly and possibly most importantly, we lacked pre-pandemic baseline data, which might have allowed more comprehensive and meaningful inferences of the pandemic's differential effect on both individuals with SUD and those without self-reported mental health disorders.
Investigations of the exact ways in which substance use patterns change during crises are needed in order to gain a better understanding of how to address individuals suffering from SUD under such circumstances. The current study found both, patients and individuals from the reference group to resort to substance use as a means of coping, which underlines the need for preventive and educational measures on a societal scale. Adapting these measures to the current situation, as could be achieved by an implementation of digital strategies, is of major relevance (97, 98). Further, efforts to develop treatment schemes that allow maintaining patients under professional attendance in difficult circumstances appear crucial. As it has been indicated that online resources are an effective way to complement care in times of contact restriction (99, 100), implementing Digital Health Infrastructure appears to be a sensible approach (57, 101).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Commission of the Medical University Innsbruck and the Ethics Committee for Clinical Research of the Sanitary Agency of South Tyrol. The patients/participants provided their written informed consent to participate in this study.
AH, BF-A, SP, BH, and BP designed the study and wrote the protocol. Recruitment was performed by FT and ACh. TS undertook statistical analysis. KL wrote the first draft of the manuscript with contributions by TS. Revision of the manuscript was carried out by TS, KL, and AH. All authors contributed to and have approved the final manuscript.
This work was supported by the Federal State of Tyrol (Grant No. F.21427). The funder of this study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author BH owns part of the IPRs of the CHES software tool.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.918465/full#supplementary-material
1. Tutzer F, Frajo-Apor B, Pardeller S, Plattner B, Chernova A, Haring C, et al. Psychological distress, loneliness, and boredom among the general population of tyrol, Austria during the COVID-19 pandemic. Front Psychiatry (2021) 12:691896. doi: 10.3389/fpsyt.2021.691896
2. Quaglieri A, Lausi G, Fraschetti A, Burrai J, Barchielli B, Pizzo A, et al. “Stay at Home” in Italy during the COVID-19 outbreak: a longitudinal study on individual well-being among different age groups. Brain Sci. (2021) 11:993. doi: 10.3390/brainsci11080993
3. McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA (2020) 324:93–4. doi: 10.1001/jama.2020.9740
4. Richter D, Riedel-Heller S, Zürcher SJ. Mental health problems in the general population during and after the first lockdown phase due to the sars-cov-2 pandemic: rapid review of multi-wave studies. Epidemiol Psychiatric Sci. (2021) 30:e27. doi: 10.1017/S2045796021000160
5. Daly M, Robinson E. Longitudinal changes in psychological distress in the UK from 2019 to September 2020 during the COVID-19 pandemic: evidence from a large nationally representative study. Psychiatry Res. (2021) 300:113920. doi: 10.1016/j.psychres.2021.113920
6. Robinson E, Daly M. Explaining the rise and fall of psychological distress during the covid-19 crisis in the United States: longitudinal evidence from the understanding America study. Br J Health Psychol. (2021) 26:570–87. doi: 10.1111/bjhp.12493
7. Awan S, Diwan MN, Aamir A, Allahuddin Z, Irfan M, Carano A, et al. Suicide in healthcare workers: determinants, challenges, and the impact of COVID-19. Front Psychiatry (2021) 12:792925. doi: 10.3389/fpsyt.2021.792925
8. Grandinetti P, Gooney M, Scheibein F, Testa R, Ruggieri G, Tondo P, et al. Stress and maladaptive coping of italians health care professionals during the first wave of the pandemic. Brain Sci. (2021) 11:20211130. doi: 10.3390/brainsci11121586
9. Chiappini S, Guirguis A, John A, Corkery JM, Schifano F. COVID-19: the hidden impact on mental health and drug addiction. Front Psychiatry. (2020) 11:767. doi: 10.3389/fpsyt.2020.00767
10. Neelam K, Duddu V, Anyim N, Neelam J, Lewis S. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain Behav Immun Health (2021) 10:100177. doi: 10.1016/j.bbih.2020.100177
11. Hofer A, Kachel T, Plattner B, Chernova A, Conca A, Fronthaler M, et al. Mental health in individuals with severe mental disorders during the COVID-19 pandemic: a longitudinal investigation. NPJ Schizophrenia (2022) 8:1–10. doi: 10.1038/s41537-022-00225-z
12. Kuntsche E, Knibbe R, Gmel G, Engels R. Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addict Behav. (2006) 31:1844–57. doi: 10.1016/j.addbeh.2005.12.028
13. Park CL, Levenson MR. Drinking to cope among college students: prevalence, problems and coping processes. J Stud Alcohol. (2002) 63:486–97. doi: 10.15288/jsa.2002.63.486
14. George FK, Patricia P, Aaron W. Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19. Am J Psychiatry (2020) 177:1031–7. doi: 10.1176/appi.ajp.2020.20091375
15. Fisher S, Hsu WW, Adams Z, Arsenault C, Milich R. The effect of impulsivity and drinking motives on alcohol outcomes in college students: a 3-year longitudinal analysis. J Am Coll Health. (2020) 1–10:20201013. doi: 10.1080/07448481.2020.1817033
16. Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope, emotional distress and alcohol use and abuse: a ten-year model. J Stud Alcohol. (2001) 62:190–8. doi: 10.15288/jsa.2001.62.190
17. McDevitt-Murphy ME, Zakarian RJ, Luciano MT, Olin CC, Mazzulo NN, Neimeyer RA. Alcohol use and coping in a cross-sectional study of African American homicide survivors. J Ethn Subst Abuse. (2021) 20:135–50. doi: 10.1080/15332640.2019.1598905
18. Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, Frohlich JR, et al. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res. (2020) 44:2073–83. doi: 10.1111/acer.14425
19. Sohi I, Chrystoja BR, Rehm J, Wells S, Monteiro M, Ali S, et al. Changes in alcohol use during the COVID-19 pandemic and previous pandemics: a systematic review. Alcohol Clin Exp Res. (2022) 46:498–513. doi: 10.1111/acer.14792
20. Kilian C, O'Donnell A, Potapova N, Lopez-Pelayo H, Schulte B, Miquel L, et al. Changes in alcohol use during the covid-19 pandemic in Europe: a meta-analysis of observational studies. Drug Alcohol Rev. (2022) 41:918–31. doi: 10.1111/dar.13446
21. Barbosa C, Cowell AJ, Dowd WN. Alcohol consumption in response to the COVID-19 pandemic in the United States. J Addict Med. (2020) 15:341. doi: 10.1097/ADM.0000000000000767
22. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open (2020) 3:e2022942. doi: 10.1001/jamanetworkopen.2020.22942
23. Jacob L, Smith L, Armstrong NC, Yakkundi A, Barnett Y, Butler L, et al. Alcohol use and mental health during covid-19 lockdown: a cross-sectional study in a sample of UK adults. Drug Alcohol Depend. (2021) 219:108488. doi: 10.1016/j.drugalcdep.2020.108488
24. Roberts A, Rogers J, Mason R, Siriwardena AN, Hogue T, Whitley GA, et al. Alcohol and other substance use during the COVID-19 pandemic: a systematic review. Drug Alcohol Depend. (2021) 229:109150. doi: 10.1016/j.drugalcdep.2021.109150
25. Thompson K, Dutton DJ, MacNabb K, Liu T, Blades S, Asbridge M. Changes in alcohol consumption during the COVID-19 pandemic: exploring gender differences and the role of emotional distress. Health Promot Chronic Dis Prev Can. (2021) 41:254–63. doi: 10.24095/hpcdp.41.9.02
26. Taylor S, Paluszek MM, Rachor GS, McKay D, Asmundson GJG. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: a network analysis. Addict Behav. (2021) 114:106754. doi: 10.1016/j.addbeh.2020.106754
27. Killgore WDS, Cloonan SA, Taylor EC, Lucas DA, Dailey NS. Alcohol dependence during COVID-19 lockdowns. Psychiatry Res. (2021) 296:113676. doi: 10.1016/j.psychres.2020.113676
28. Kumar N, Janmohamed K, Nyhan K, Martins SS, Cerda M, Hasin D, et al. Substance, use in relation to COVID-19: a scoping review. Addict Behav. (2022) 127:107213. doi: 10.1016/j.addbeh.2021.107213
29. Murthy P, Narasimha VL. Effects of the COVID-19 pandemic and lockdown on alcohol use disorders and complications. Curr Opin Psychiatry. (2021) 34:376–85. doi: 10.1097/YCO.0000000000000720
30. Bal S, Crombez G, Van Oost P, Debourdeaudhuij I. The role of social support in well-being and coping with self-reported stressful events in adolescents. Child Abuse Negl. (2003) 27:1377–95. doi: 10.1016/j.chiabu.2003.06.002
31. Arnberg FK, Hultman CM, Michel PO, Lundin T. Social support moderates posttraumatic stress and general distress after disaster. J Trauma Stress (2012) 25:721–7. doi: 10.1002/jts.21758
32. Ouyang M, Gui D, Cai X, Yin Y, Mao X, Huang S, et al. Stressful life events and subjective well-being in vocational school female adolescents: the mediating role of depression and the moderating role of perceived social support. Front Psychol. (2020) 11:603511. doi: 10.3389/fpsyg.2020.603511
33. Xiong T, Milios A, McGrath PJ, Kaltenbach E. The influence of social support on posttraumatic stress symptoms among children and adolescents: a scoping review and meta-analysis. Eur J Psychotraumatol. (2022) 13:2011601. doi: 10.1080/20008198.2021.2011601
34. Szkody E, Stearns M, Stanhope L, McKinney C. Stress-buffering role of social support during COVID-19. Fam Process. (2020) 60:1002–1015. doi: 10.1111/famp.12618
35. Ye Z, Yang X, Zeng C, Wang Y, Shen Z, Li X, et al. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl Psychol Health Well Being (2020) 12:1074–94. doi: 10.1111/aphw.12211
36. Lasgaard M, Goossens L, Bramsen RH, Trillingsgaard T, Elklit A. Different sources of loneliness are associated with different forms of psychopathology in adolescence. J Res Pers. (2011) 45:233–7. doi: 10.1016/j.jrp.2010.12.005
37. Shevlin M, McElroy E, Murphy J. Loneliness mediates the relationship between childhood trauma and adult psychopathology: evidence from the adult psychiatric morbidity survey. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:591–601. doi: 10.1007/s00127-014-0951-8
38. Lasgaard M, Friis K, Shevlin M. “Where are all the lonely people?” A population-based study of high-risk groups across the life span. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:1373–84. doi: 10.1007/s00127-016-1279-3
39. Richardson T, Elliott P, Roberts R. Relationship between loneliness and mental health in students. J Public Ment Health (2017) 16:48–54. doi: 10.1108/JPMH-03-2016-0013
40. Richard A, Rohrmann S, Vandeleur CL, Schmid M, Barth J, Eichholzer M. Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a swiss national survey. PLoS ONE (2017) 12:e0181442. doi: 10.1371/journal.pone.0181442
41. Hoffart A, Johnson SU, Ebrahimi OV. Loneliness and social distancing during the COVID-19 pandemic: risk factors and associations with psychopathology. Front Psychiatry (2020) 11:589127. doi: 10.3389/fpsyt.2020.589127
42. Horesh D, Kapel Lev-Ari R, Hasson-Ohayon I. Risk factors for psychological distress during the COVID-19 pandemic in israel: loneliness, age, gender, and health status play an important role. Br J Health Psychol. (2020) 25:925–33. doi: 10.1111/bjhp.12455
43. Horigian VE, Schmidt RD, Feaster DJ. Loneliness, mental health, and substance use among US young adults during COVID-19. J Psychoactive Drugs. (2021) 53:1–9. doi: 10.1080/02791072.2020.1836435
44. Liu S, Heinzel S, Haucke MN, Heinz A. Increased psychological distress, loneliness, and unemployment in the spread of COVID-19 over 6 months in Germany. Medicina (2021) 57:53. doi: 10.3390/medicina57010053
45. McQuaid RJ, Cox SML, Ogunlana A, Jaworska N. The burden of loneliness: implications of the social determinants of health during COVID-19. Psychiatry Res. (2021) 296:113648. doi: 10.1016/j.psychres.2020.113648
46. Bragard E, Giorgi S, Juneau P, Curtis BL. Loneliness and daily alcohol consumption during the COVID-19 pandemic. Alcohol. (2022) 57:198–202. doi: 10.1093/alcalc/agab056
47. Jackson KM, Sher KJ. Alcohol use disorders and psychological distress: a prospective state-trait analysis. J Abnorm Psychol. (2003) 112:599–613. doi: 10.1037/0021-843X.112.4.599
48. Tsai J, Floyd RL, O'Connor MJ, Velasquez MM. Alcohol use and serious psychological distress among women of childbearing age. Addict Behav. (2009) 34:146–53. doi: 10.1016/j.addbeh.2008.09.005
49. Balogun O, Koyanagi A, Stickley A, Gilmour S, Shibuya K. Alcohol consumption and psychological distress in adolescents: a multi-country study. J Adolesc Health (2014) 54:228–34. doi: 10.1016/j.jadohealth.2013.07.034
50. Bartlett BA, Smith LJ, Lebeaut A, Tran JK, Vujanovic AA. PTSD symptom severity and impulsivity among firefighters: associations with alcohol use. Psychiatry Res. (2019) 278:315–23. doi: 10.1016/j.psychres.2019.06.039
51. Ruiz P, Pilatti A, Pautassi RM. Consequences of alcohol use, and its association with psychological distress, sensitivity to emotional contagion and age of onset of alcohol use, in uruguayan youth with or without college degree. Alcohol (2020) 82:91–101. doi: 10.1016/j.alcohol.2019.09.001
52. Wingo AP, Ressler KJ, Bradley B. Resilience characteristics mitigate tendency for harmful alcohol and illicit drug use in adults with a history of childhood abuse: a cross-sectional study of 2024 inner-city men and women. J Psychiatr Res. (2014) 51:93–9. doi: 10.1016/j.jpsychires.2014.01.007
53. Long EC, Lonn SL Ji J, Lichtenstein P, Sundquist J, Sundquist K, et al. Resilience and risk for alcohol use disorders: a swedish twin study. Alcohol Clin Exp Res. (2017) 41:149–55. doi: 10.1111/acer.13274
54. Holzhauer CG, Wemm S, Wulfert E. Distress tolerance and physiological reactivity to stress predict women's problematic alcohol use. Exp Clin Psychopharmacol. (2017) 25:156–65. doi: 10.1037/pha0000116
55. Calvey T, Scheibein F, Saad NA, Shirasaka T, Dannatt L, Stowe MJ, et al. The changing landscape of alcohol use and alcohol use disorder during the COVID-19 pandemic—perspectives of early career professionals in 16 countries. J Addict Med. (2020) 14:e284–e6. doi: 10.1097/ADM.0000000000000735
56. Stowe MJ, Calvey T, Scheibein F, Arya S, Saad NA, Shirasaka T, et al. Access to healthcare and harm reduction services during the COVID-19 pandemic for people who use drugs. J Addict Med. (2020) 14:e287–e9. doi: 10.1097/ADM.0000000000000753
57. Bayers T, Strohmaier T, Shreffler J, Huecker M. Perceptions of individuals in treatment for substance use disorder during COVID-19: insight on mental health, sobriety, access to treatment, and telehealth. J Addict Dis. (2022) 40:111–3. doi: 10.1080/10550887.2021.1948292
58. Russell C, Ali F, Nafeh F, Rehm J, LeBlanc S, Elton-Marshall T. Identifying the impacts of the COVID-19 pandemic on service access for people who use drugs (PWUD): a national qualitative study. J Subst Abuse Treat. (2021) 129:108374. doi: 10.1016/j.jsat.2021.108374
59. Kesten JM, Holland A, Linton MJ, Family H, Scott J, Horwood J, et al. Living under coronavirus and injecting drugs in Bristol (LUCID-B): a qualitative study of experiences of COVID-19 among people who inject drugs. Int J Drug Policy. (2021) 98:103391. doi: 10.1016/j.drugpo.2021.103391
60. Hanson JD, Noonan C, Harris A, Oziel K, Sarche M, MacLehose RF, et al. Alcohol consumption during COVID among women with an existing alcohol-use disorder. Int J Environ Res Public Health (2021) 18:9460. doi: 10.3390/ijerph18189460
61. Gilbert PA, Soweid L, Kersten SK, Brown G, Zemore SE, Mulia N, et al. Maintaining recovery from alcohol use disorder during the COVID-19 pandemic: the importance of recovery capital. Drug Alcohol Depend. (2021) 229:109142. doi: 10.1016/j.drugalcdep.2021.109142
62. Na PJ, Norman SB, Nichter B, Hill ML, Rosen MI, Petrakis IL, et al. Prevalence, risk and protective factors of alcohol use disorder during the COVID-19 pandemic in US military veterans. Drug Alcohol Depend. (2021) 225:108818. doi: 10.1016/j.drugalcdep.2021.108818
63. Fuchs-Leitner I, Yazdi K, Gerstgrasser NW, Rosenleitner J. Developments in drug addiction during COVID-19-an Austrian perspective based on a clinical sample. Front Psychiatry (2020) 11:602033. doi: 10.3389/fpsyt.2020.602033
64. Yazdi K, Fuchs-Leitner I, Rosenleitner J, Gerstgrasser NW. Impact of the COVID-19 pandemic on patients with alcohol use disorder and associated risk factors for relapse. Front Psychiatry (2020) 11:620612. doi: 10.3389/fpsyt.2020.620612
65. Kim JU, Majid A, Judge R, Crook P, Nathwani R, Selvapatt N, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. (2020) 5:886–7. doi: 10.1016/S2468-1253(20)30251-X
66. Barrio P, Baldaqui N, Andreu M, Kilian C, Rehm J, Gual A, et al. Abstinence among alcohol use disorder patients during the COVID-19 pandemic: insights from Spain. Alcohol Clin Exp Res. (2021) 45:802–7. doi: 10.1111/acer.14555
67. Constant A, Sanz M, Moirand R. Predictors of short-term alcohol drinking in patients with alcohol use disorders during the third wave of the COVID-19 pandemic: prospective study in three addiction outpatient centers in France. Int J Environ Res Public Health (2022) 19:1948. doi: 10.3390/ijerph19041948
68. Bonny-Noach H, Gold D. Addictive behaviors and craving during the COVID-19 pandemic of people who have recovered from substance use disorder. J Addict Dis. (2021) 39:257–64. doi: 10.1080/10550887.2020.1856298
69. Hurley EA, Pina K, Cegielski V, Noel-MacDonnell JR, Miller MK. Recovering from substance use disorders during the early months of the COVID-19 pandemic: a mixed-methods longitudinal study of women in Kansas city. J Subst Abuse Treat (2021) 129:108378. doi: 10.1016/j.jsat.2021.108378
70. Eurostat. (2021). Available online at: https://ec.europa.eu/eurostat/web/national-accounts/data/database (accessed November 14, 2021).
71. Chernova A, Frajo-Apor B, Pardeller S, Tutzer F, Plattner B, Haring C, et al. The mediating role of resilience and extraversion on psychological distress and loneliness among the general population of Tyrol, Austria between the first and the second wave of the COVID-19 pandemic. Front Psychiatry (2021) 12:766261. doi: 10.3389/fpsyt.2021.766261
72. Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: gender and racial/ethnic differences. J Adolesc Health (2012) 50:154–63. doi: 10.1016/j.jadohealth.2011.05.013
73. Vasilenko SA, Evans-Polce RJ, Lanza ST. Age trends in rates of substance use disorders across ages 18–90: differences by gender and race/ethnicity. Drug Alcohol Depend (2017) 180:260–4. doi: 10.1016/j.drugalcdep.2017.08.027
74. Hennessy S, Bilker WB, Berlin JA, Strom BL. Factors influencing the optimal control-to-case ratio in matched case-control studies. Am J Epidemiol. (1999) 149:195–7. doi: 10.1093/oxfordjournals.aje.a009786
75. Grimes DA, Schulz KF. Compared to what? Finding controls for case-control studies. Lancet (2005) 365:1429–33. doi: 10.1016/S0140-6736(05)66379-9
77. Holzner B, Giesinger JM, Pinggera J, Zugal S, Schöpf F, Oberguggenberger AS, et al. The computer-based health evaluation software (CHES): a software for electronic patient-reported outcome monitoring. BMC Med Inform Decis Mak. (2012) 12:126. doi: 10.1186/1472-6947-12-126
79. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
80. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
82. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic. (1988).
83. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. (2009) 41:1149–60. doi: 10.3758/BRM.41.4.1149
84. Clerici M, Durbano F, Spinogatti F, Vita A, de Girolamo G, Micciolo R. Psychiatric hospitalization rates in italy before and during COVID-19: did they change? An analysis of register data. Ir J Psychol Med. (2020) 37:283–90. doi: 10.1017/ipm.2020.29
85. Boldrini T, Girardi P, Clerici M, Conca A, Creati C, Di Cicilia G, et al. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 110:110304. doi: 10.1016/j.pnpbp.2021.110304
86. Rodriguez-Jimenez R, Rentero D, Romero-Ferreiro V, Garcia-Fernandez L. Impact of outbreak COVID-19 pandemic on psychiatry emergencies in Spain. Psychiatry Res. (2021) 295:113581. doi: 10.1016/j.psychres.2020.113581
87. Simpson SA, Loh RM, Cabrera M, Cahn M, Gross A, Hadley A, et al. The impact of the COVID-19 pandemic on psychiatric emergency service volume and hospital admissions. J Acad Consult Liaison Psychiatry. (2021) 62:588–594. doi: 10.1016/j.jaclp.2021.05.005
88. Hoyer C, Ebert A, Szabo K, Platten M, Meyer-Lindenberg A, Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. (2021) 271:377–9. doi: 10.1007/s00406-020-01151-w
89. Groh DR, Jason LA, Davis MI, Olson BD, Ferrari JR. Friends, family, and alcohol abuse: an examination of general and alcohol-specific social support. Am J Addict. (2007) 16:49–55. doi: 10.1080/10550490601080084
90. Karriker-Jaffe KJ, Roberts SC, Bond J. Income inequality, alcohol use, and alcohol-related problems. Am J Public Health. (2013) 103:649–56. doi: 10.2105/AJPH.2012.300882
91. Pan K-Y, Kok AAL, Eikelenboom M, Horsfall M, Jörg F, Luteijn RA, et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three dutch case-control cohorts. Lancet Psychiatry. (2021) 8:121–9. doi: 10.1016/S2215-0366(20)30491-0
92. Riehm KE, Holingue C, Smail EJ, Kapteyn A, Bennett D, Thrul J. et al. Trajectories of mental distress among US adults during the COVID-19 pandemic. Ann Behav Med. (2021) 55:93–102. doi: 10.1093/abm/kaaa126
93. Hamama-Raz Y, Goodwin R, Leshem E, Ben-Ezra M. The toll of a second lockdown: a longitudinal study. J Affect Disord. (2021) 294:60–2. doi: 10.1016/j.jad.2021.06.080
94. Worldometer. Austria COVID—Coronavirus Statistics – Worldometer (2016). Available online at: https://www.worldometers.info/coronavirus/country/austria/ (accessed June 26, 2022).
95. Bundesministerium für Soziales G, Pflege Pflege und Konsumentenschutz (Federal Ministry of Social Affairs, Health Care and Consumer Protection). 398. Verordnung: Nderung Der COVID-19-Lockerungsverordnung - 10. COVID-19-Lv- Novelle (2020). Available online at: https://www.ris.bka.gv.at/Dokumente/BgblAuth/BGBLA_2020_II_398/BGBLA_2020_II_398.pdfsig (accessed June 26, 2022).
96. Worldometer. Italy COVID—Coronavirus Statistics—Worldometer. Available online at: https://www.worldometers.info/coronavirus/country/italy/ (accessed June 26, 2022).
97. Doring N, Holz C. Alcohol in social media: where is the space for prevention? Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2021) 64:697–706. doi: 10.1007/s00103-021-03335-8
98. Prediger C, Helmer SM, Hrynyschyn R, Stock C. Virtual reality-based alcohol prevention in adolescents: a systematic review. Adolescents (2021) 1:138–50. doi: 10.3390/adolescents1020011
99. Bergman BG, Kelly JF. Online digital recovery support services: an overview of the science and their potential to help individuals with substance use disorder during COVID-19 and beyond. J Subst Abuse Treat. (2021) 120:108152. doi: 10.1016/j.jsat.2020.108152
100. Kruse CS, Lee K, Watson JB, Lobo LG, Stoppelmoor AG, Oyibo SE. Measures of effectiveness, efficiency, and quality of telemedicine in the management of alcohol abuse, addiction, and rehabilitation: systematic review. J Med Internet Res. (2020) 22:e13252. doi: 10.2196/13252
Keywords: COVID-19, substance use disorders, psychological distress, loneliness, social support
Citation: Lommer K, Schurr T, Frajo-Apor B, Plattner B, Chernova A, Conca A, Fronthaler M, Haring C, Holzner B, Macina C, Marksteiner J, Miller C, Pardeller S, Perwanger V, Pycha R, Schmidt M, Sperner-Unterweger B, Tutzer F and Hofer A (2022) Addiction in the time of COVID-19: Longitudinal course of substance use, psychological distress, and loneliness among a transnational Tyrolean sample with substance use disorders. Front. Psychiatry 13:918465. doi: 10.3389/fpsyt.2022.918465
Received: 12 April 2022; Accepted: 01 July 2022;
Published: 25 July 2022.
Edited by:
Carlos Roncero, University of Salamanca, SpainReviewed by:
Pilar Andrés-Olivera, University Hospital of Salamanca, SpainCopyright © 2022 Lommer, Schurr, Frajo-Apor, Plattner, Chernova, Conca, Fronthaler, Haring, Holzner, Macina, Marksteiner, Miller, Pardeller, Perwanger, Pycha, Schmidt, Sperner-Unterweger, Tutzer and Hofer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kilian Lommer, a2lsaWFuLmxvbW1lckBpLW1lZC5hYy5hdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.