- 1Department of Medical Psychology, Army Medical University, Chongqing, China
- 2Teaching Examination Centre, Army Medical University, Chongqing, China
Objective: This study aims to investigate the indirect effect of impulsiveness on suicidal ideation through depression and the moderating effect of impulsiveness on the indirect effect in an integrated path model.
Methods: Self-rating depression scale (SDS), Barratt impulsiveness scale-11th version (BIS-11), and self-rating idea of suicide scale (SIOSS) were applied. A moderated mediation path model was established including impulsiveness, depression, and suicidal ideation as observed variables.
Results: The main results revealed that the moderated mediation path model fit well in describing the relationships among impulsiveness, depression, and suicidal ideation. The indirect effect of impulsiveness mediated by depression and the moderating effect of impulsiveness on suicidal ideation was significant. Multiple comparisons showed that the indirect effects under different conditions of impulsiveness had statistical differences. The higher the impulsiveness was, the stronger the predictive effect of depression on suicidal ideation was.
Conclusions: The present study confirms that people who have impulsive traits are riskier to generate suicidal thoughts because they are more likely to suffer from depression and that people who are depressive have even higher risk to develop suicidal thoughts when they simultaneously have impulsive traits. In clinical and health care work, when considering depression to prevent suicidal ideation, impulsiveness needs to be monitored throughout the process of premorbid and onset stages of depression.
Introduction
According to the newest worldwide statistics (1), about 9.2 persons per 100,000 died from suicide in 2019. Suicide is divided into three phases: suicidal ideation, suicide attempts and lethal suicide behavior (2). The prevalence rate of suicidal ideation, which ranges from 2.6 to 25.4% (3), is much higher than suicide attempts and lethal suicide behavior. It is thought to be an indispensable cognitive process before suicide actions take place (4, 5). Solano et al. found that the Internet searching behaviors of suicide-related information were positively correlated with the growth of suicide rates in the following three months (6). The Internet searching behaviors represent the existence of suicidal ideation (6). Therefore, Solano's study indicates that suicidal ideation is a preexisting factor of lethal suicide behavior. A large sample survey revealed that individuals with suicidal ideation were over four times more likely to commit suicide than whom without suicidal ideation (7). Accordingly, for suicide prevention, it is critical to detect, manage, and intervene in suicidal ideation.
As described in the diathesis-stress-model (8), vulnerable trait factors (diathesis) and unexpected life events [including subsequent negative/positive emotion and psychopaths, et al., namely, stress (9)] cause the onset of suicide behavior, specifically, suicidal ideation. Among the diathesis and stress, impulsiveness and depression have been widely studied, which are the two vital factors that confer high risk. However, it is inconsistent about how the two factors work together in suicidal cognitive process.
In some studies, impulsiveness and depression are two independent variables related to suicidal ideation (10–12). Another study constructed a linear regression model (13), finding that depression independently predicted suicidal ideation and that impulsiveness affected suicidal ideation through interacting with traumatic experience. It is inconsistent about whether impulsiveness can independently lead to suicidal ideation and not clear whether impulsiveness can interact with depression in predicting suicidal ideation.
The integrated motivational-volitional model holds that impulsiveness is an interacting variable with suicidal ideation in predicting suicide behavior, while does not mention the effect of impulsiveness on suicidal ideation nor its interaction with any psychopaths (5). One study showed that, when depression existed, impulsiveness could raise the risk of suicide behavior rather than suicidal ideation (14). It indicates that impulsiveness interacts with depression in the onset of suicide behavior but not suicidal ideation. However, according to Beck's cognitive model of suicide (4), vulnerability and psychiatric disturbance jointly contribute to suicide related thoughts at first, and then lead to suicide behavior. This is possibly because not every “impulsiveness” in previous studies is a kind of diathesis. Some of them may refer to a kind of state (15). It may confuse the medical or public health personnel in considering whether to deal with impulsiveness as a diathesis to monitor or as a state to intervene.
State impulsiveness is a process of fast decision or behavior without thinking (16). However, trait impulsiveness is a stable style of behavior as a personality (17). It is subjectively measured by questionnaires, usually based on Barratt's impulsiveness model (18) or UPPS (urgency-premeditation-perseverance-sensation-seeking) impulsiveness model (19). State impulsiveness is less likely to take effect together with depression among the cognitive process of suicide (5). Therefore, in the present study, we mainly paid attention to trait impulsiveness (called “impulsiveness” in the following text). According to the integrated motivational-volitional model, we hypothesize that (trait) impulsiveness interacts with depression in predicting suicidal ideation, which can be described by a simple moderation model with the moderating effect of impulsiveness on the path from depression to suicidal ideation. However, the simple moderation model does not consider the correlation between impulsiveness and depression which have been proved closely correlated in previous studies (20–25). Therefore, according to Beck's cognitive model (4), in which vulnerability influences suicidal cognitive process through psychiatric disturbance, we hypothesize that impulsiveness indirectly affects suicidal ideation through depression.
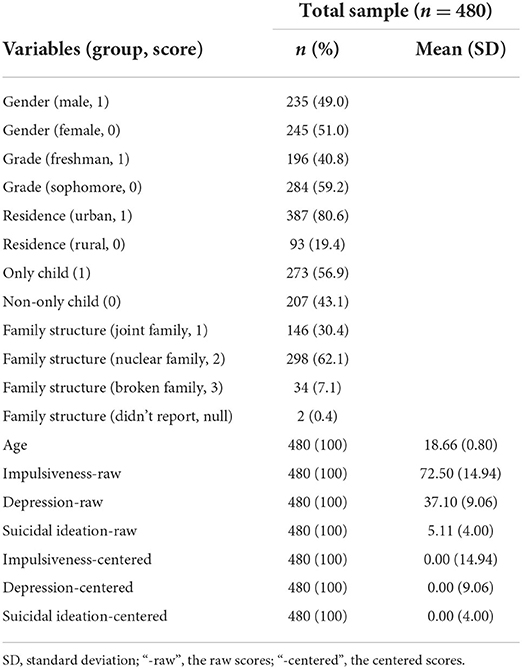
Combining these two hypotheses, we construct a moderated mediation path model (MODMEDPM). The whole hypothesis of this study is that impulsiveness indirectly affects suicidal ideation through depression and simultaneously moderates the indirect effect. To be more reliable, we take the simple moderation path model (SMODPM) as the alternative model for comparison. The conceptual diagrams of MODMEDPM and SMODPM are shown in Figure 1.
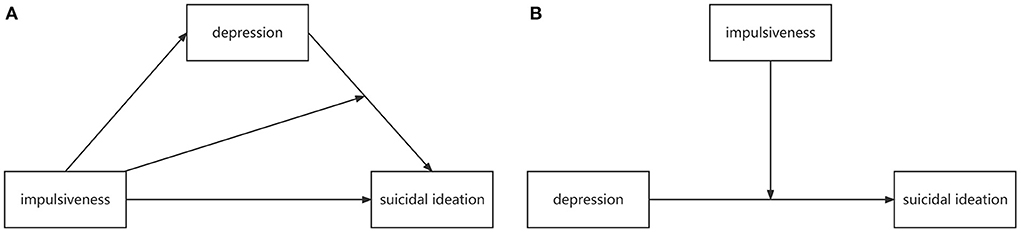
Figure 1. Conceptual diagrams of MODMEDPM (A) and SMODPM (B). MODMEDPM—moderated mediation path model; SMODPM—simple moderation path model.
Materials and methods
Participants
We applied cluster sampling method to select a cohort who was healthy in mentality. To control the confounding effects, we only recruited two grades of students, including 196 freshman (40.8%) and 284 sophomore (59.2%). Because the junior, senior and interns studied in different hospitals, who were faced with mixed stressors which could be confounding variables. The psychological tests were conducted within one month. All the 480 participants were examined. The cohort included 245 females (51.0%) and 235 males (49.0%) aged 16–21 (18.66 ± 0.80). Other demographic characteristics, including grade, residence, only child status, and family structure, as well as descriptive statistics of variables were shown in Table 1. There were two participants who did not report family structure. They were rejected only when the family structure was included as a factor in the analysis.
Measures
Suicidal ideation
Suicidal ideation was assessed by the twenty-six-item Self-rating idea of suicide scale (SIOSS). This scale was developed in Chinese by Xia (26). The participants choose yes or no concerning whether they have symptoms or ideas described in the items. Higher sum scores imply stronger suicidal ideation. The SIOSS has good reliability and validity in the Chinese population (27–29). In the present study, this scale had acceptable reliability of internal consistency (Cronbach's alpha = 0.822).
Impulsiveness
The Barratt impulsiveness scale (SIOSS) consists of 30 items. It was originally developed by Ernest S. Barratt in 1959 (18). The 11th Chinese version of the BIS was revised under the context of Chinese culture and retained good reliability and validity (30). The BIS had fine internal consistency reliability (Cronbach's alpha = 0.909) in this study.
Depression
The Self-rating depression scale (SDS) was initially developed by William W. K. Zung in 1965 for evaluating depression in patients with depressive disorder (31). The scale consists of 20 items. It can also be used for preliminary screening in outpatient clinics (32), early detection of depression (33) or depressive state evaluation in the general population (34, 35). The Chinese version of the SDS has demonstrated good reliability and validity across various groups of people (36). Its internal consistency reliability was good (Cronbach's alpha = 0.879) in this study.
Statistical analyses
The internal consistency reliability coefficients and the correlation coefficients of the variables were calculated in SPSS 20.0 (37). We also made the descriptive statistics for demographic variables in SPSS 20.0. Model fits and path analyses were conducted in Mplus 8.3 (38). The Mplus code for mediation and moderation models was developed by Stride et al. (39), according to Hayes' PROCESS macro program documentation (40). We modified the Mplus code for adjusting the purpose of the present study.
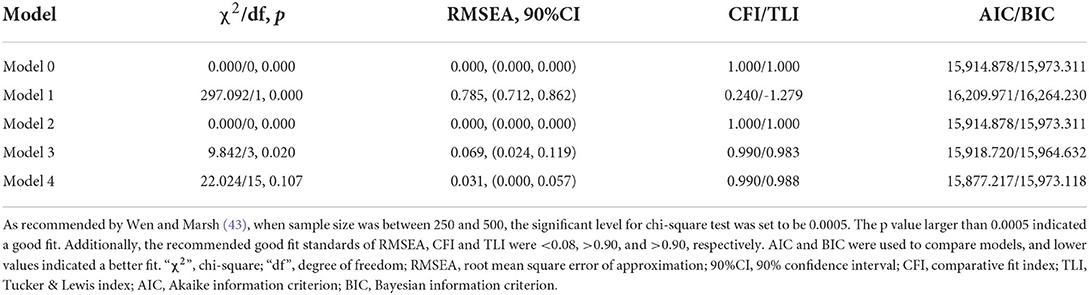
Firstly, we constructed a baseline model, which was a saturated model with all variables (impulsiveness, depression, interaction term of impulsiveness and depression, and suicidal ideation) linked by paths (statistical diagram shown in Figure 2A). Secondly, we chose MODMEDPM, which was defined Model 74 (statistical diagram shown in Figure 2B) in PROCESS macro (40), as the target model. Model 1 (statistical diagram shown in Figure 2C) in PROCESS (40), which was SMODPM, was chosen as the alternative model.
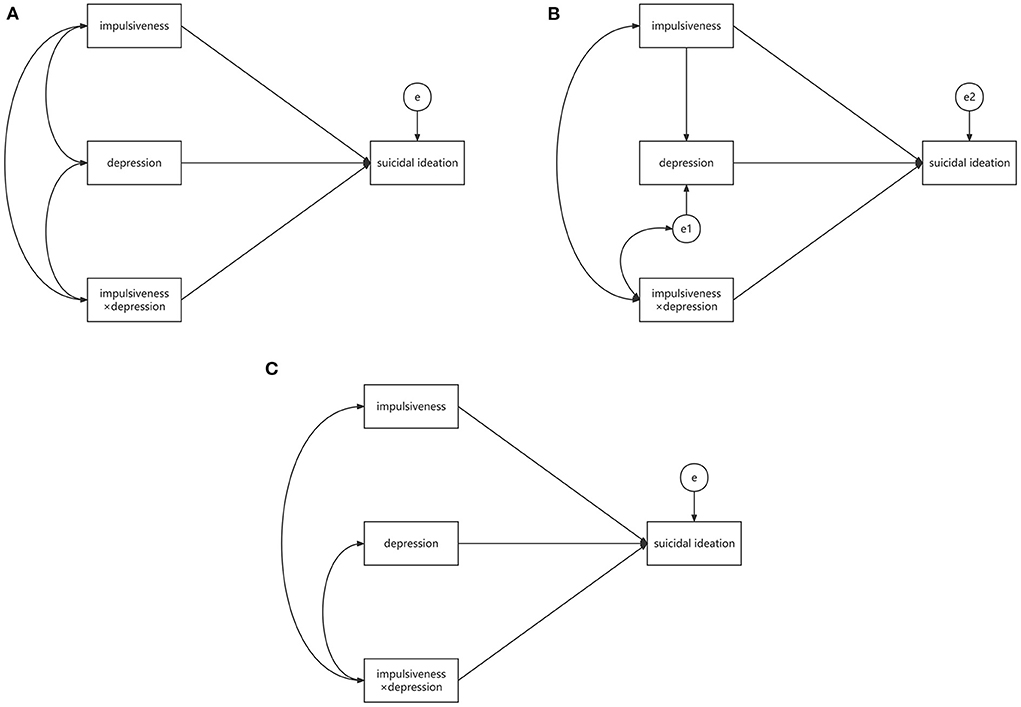
Figure 2. Statistical diagrams of baseline model (A), MODMEDPM (B), and SMODPM (C). MODMEDPM—moderated mediation path model; SMODPM—simple moderation path model; “impulsiveness × depression”—the interaction term; “e”, “e1” and “e2”—the residual variances of dependent variables.
The indexes of chi-square value, Akaike information criterion (AIC), Bayesian information criterion (BIC), comparative fit index (CFI), Tucker & Lewis index (TLI) and root mean square error of approximation (RMSEA) were used to compare the model fits. The level of significant tests for the paths was set to 0.05. The mediating effect was examined with the bootstrap method with a sampling size of 5,000. The scores of the three variables, including impulsiveness, depression, and suicidal ideation, were mean centered before modeling.
Results
Correlation matrix of impulsiveness, depression, and suicidal ideation
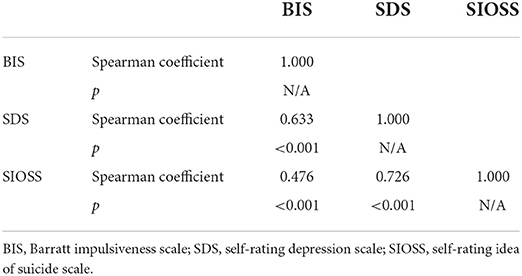
Mean centered scores were used when doing correlation analyses. Given that the scores of SIOSS did not fit a normal distribution (Kolmogorov-Smirnov Z = 2.770, p < 0.001), we performed correlation matrix with spearman coefficients. The results showed that all the three variables were correlated with each other significantly, as shown in Table 2. The correlation matrix showed large correlation coefficients between depression and suicidal ideation (r = 0.726, p < 0.001), as well as between impulsiveness and depression (r = 0.633, p < 0.001). From the perspective of psychometrics, there are several items as observed indicators of the three variables presenting similar meanings, which may result in strong correlations of depression with impulsiveness and suicidal ideation. Considering the possible serious common method biases, we conducted a test and got the first common factor's explained variation as 24.31% [50%, as an empirical value in previous studies (41), was recommended the upper cut-off value of serious common method biases]. It meant that the common method biases in this study was tolerable. Therefore, the study results could illustrate the real relationships among variables.
Model optimization
Although suicidal ideation scores did not fit normal distribution, its coefficients of skewness (=1.027) and kurtosis (=0.943) were lower than 2 and 7, respectively. According to Finney and DiStefano's estimating strategy for model parameters (42), maximum likelihood (ML) estimation could still be used as a robust method. In addition, the bootstrap method might help solve the non-normal distribution problem.
The baseline model (Model 0) fit indexes showed that it was a saturated model with chi-square value and degrees of freedom equal to zero. Because moderation model hypothesized that the independent and moderating variable were not correlated with each other, we deleted the linkage between depression and impulsiveness and got the SMODPM (Model 1). However, the fit indexes of SMODPM were not good, as shown in Table 3. Then, we examined the target model MODMEDPM (Model 2). Model 2 was an algebraically equivalence model of Model 0 but was theoretically different. In Model 2, the path between impulsiveness and depression was unidirectional, while in Model 0, the path was bidirectional. Obviously, only Model 2 represented the mediation hypothesis. However, the fit indexes of Model 2 were the same with Model 0, which referred to a saturated model (see Table 3). The diagram and path coefficients were displayed in Figure 3. To optimize the model fit, we deleted the non-significant paths, namely, bidirectional path between impulsiveness × depression and impulsiveness (β = 0.117, SE = 0.116, p = 0.312), bidirectional path between impulsiveness × depression and e1 (β = 0.080, SE = 0.065, p = 0.219), and unidirectional path from impulsiveness to suicidal ideation (β = −0.010, SE = 0.046, p = 0.829). The Resulted Model 3 fitted well and could be accepted (indexes shown in Table 3). Finally, we included the demographic factors as covariates to control the confounding effects and resulted in Model 4, which fit better than Model 3 (see Table 3). None of the covariates had significant effect on dependent variables.
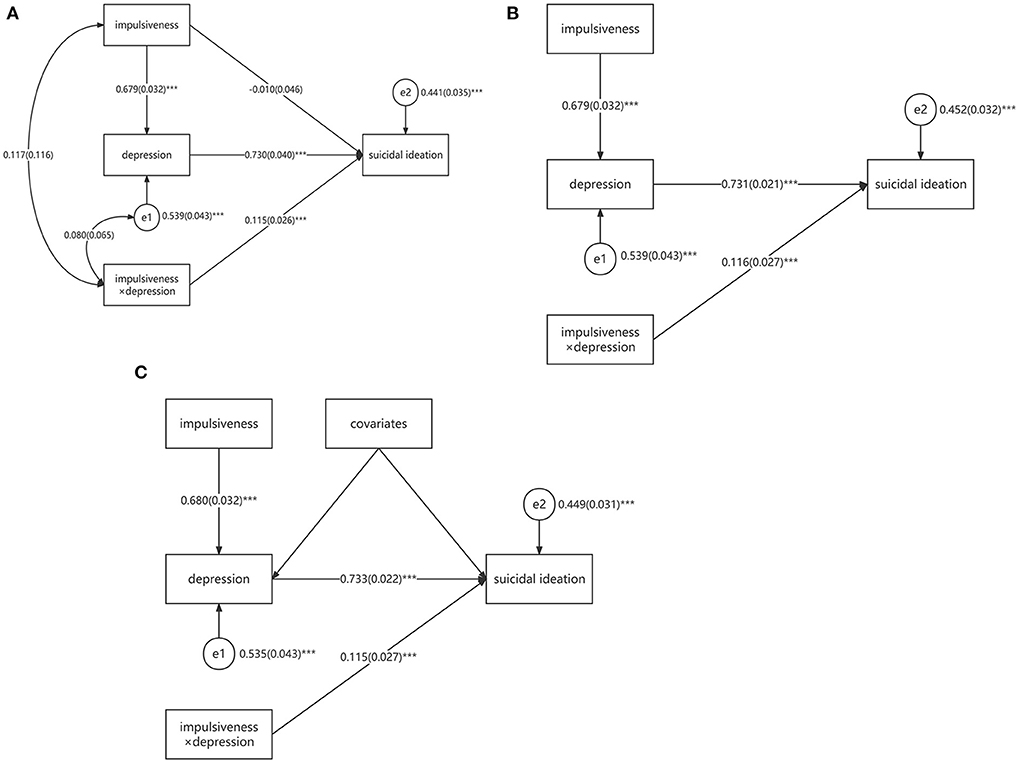
Figure 3. Statistical diagrams of saturated MODMEDPM [(A), Model 2], relatively acceptable MODMEDPM [(B), Model 3], and final MODMEDPM [(C), Model 4]. ***p < 0.001; MODMEDPM—moderated mediation path model; “impulsiveness × depression”—the interaction term; “e,” “e1,” and “e2”—the residual variances of dependent variables; Covariates included gender, grade, residence, only child, family structure and age. The path coefficients were standardized.
Moderated mediating effect analyses
Total effect
In the model, there were two nested models. Depression and suicidal ideation were the dependent variables in the two nested models, respectively. Depression was predicted by impulsiveness (R2 = 0.465, SE = 0.043, p < 0.001). Suicidal ideation was directly predicted by depression and indirectly predicted by impulsiveness. Meanwhile, the indirect effect was moderated by impulsiveness (R2 = 0.551, SE = 0.031, p < 0.001). This meant that the model could account for 55.1% of the total variances of suicidal ideation. The model summary was listed in Supplementary Table S1.
Mediating effect
As shown in Supplementary Table S2, the direct effect of impulsiveness on suicidal ideation was non-significant. The effects of impulsiveness on depression and of depression on suicidal ideation were significant [βondepression =0.680, SE=0.032, 95%CI = (0.609, 0.737), βonsuicidalideation =0.733 SE = 0.022, 95%CI = (0.688, 0.773)], and the indirect effect of impulsiveness on suicidal ideation was significant [βindirect = 0.499, SE = 0.031, 95%CI = (0.436, 0.558)]. The indirect effect here could be explained as mediating effect because all the significant coefficients were positive.
Moderating effect
We regarded the coefficient of path from the interaction term to suicidal ideation as the effect parameter of moderation [βmoderation =0.115, SE = 0.027, 95%CI = (0.059, 0.167)]. However, this coefficient really represented the moderating effect on the path from depression to suicidal ideation. To test the moderating effect of impulsiveness on the indirect effect from impulsiveness to suicidal ideation, the conditional indirect effect analysis (simple slope analysis) was conducted. Firstly, impulsiveness was divided into three conditions: low impulsiveness (mean-1SD), medium impulsiveness (mean), and high impulsiveness (mean + 1SD). Secondly, we calculated the simple slopes, which represented the moderated mediating effects, under the three conditions, respectively. Thirdly, we compared the three slopes to define whether they were statistically different. As these were multiple comparisons, the significant level was set to be 0.05/3 = 0.017. The results showed that the slope under the condition of high impulsiveness was higher than that under the condition of medium and low impulsiveness (ΔSlopeHigh−Low = 0.028, SE = 0.008, p < 0.001; ΔSlopeHigh−Medium = 0.014, SE = 0.004, p < 0.001), and the slope under the condition of medium impulsiveness was higher than that under the condition of low impulsiveness (ΔSlopeMedium−Low = 0.014, SE = 0.004, p < 0.001, see Supplementary Table S3). The simple slope diagram was shown in Figure 4. It indicated that impulsiveness positively moderated the indirect effect of impulsiveness on suicidal ideation. In other words, the mediating effect of depression between impulsiveness and suicidal ideation was reinforced by impulsiveness.
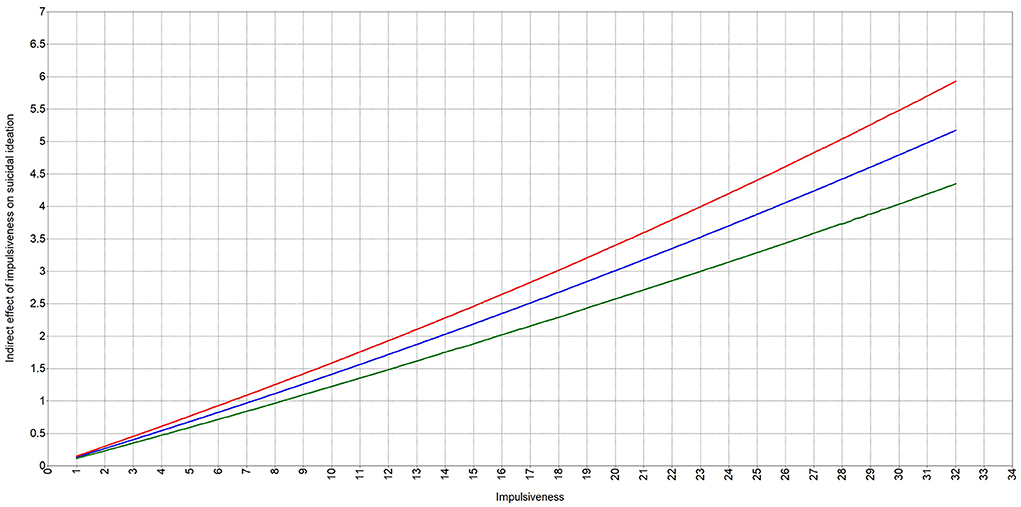
Figure 4. Simple slope diagram. Red line—the indirect effect curve under condition of high impulsiveness; Blue line—the indirect effect curve under condition of medium impulsiveness; Green line—the indirect effect curve under condition of low impulsiveness.
Discussion
In the present study, we found that the moderated mediation path model could finely describe the complex relationships among impulsiveness, depression, and suicidal ideation. Impulsiveness could indirectly lead to suicidal ideation through depression and enhance the indirect effect. These findings confirmed the hypothesis. Additionally, we found that impulsiveness did not affect suicidal ideation directly nor independently, and the presence of depression was necessary as both mediating and interacting variable.
Although impulsiveness was correlated with suicidal ideation in correlation matrix, the direct path from impulsiveness to suicidal ideation was not significant in the model. In a word, it can be explained as the complete mediating effect. This indicates that impulsiveness probably predicts depression and depression sequentially predicts suicidal ideation. It partly illustrates the mechanism of impulsiveness' effect on suicidal ideation. Impulsiveness in motivational-volitional model is not among the risk factors for suicidal ideation (5). This theoretical hypothesis was verified in model-based studies in which depression was included (13, 14), which might be due to the strong mediating effect. Therefore, conclusion can be drawn that impulsiveness is an indirect risk factor for suicidal ideation. We had noticed that the coefficient of the direct path was negative. In some studies (44–46), this kind of indirect effect is named suppressing effect. Nevertheless, it is based on the condition that the coefficient is significant. In the present study, the coefficient of direct effect from impulsiveness to suicidal ideation was far away from significance (there was 82.9% of probability for us to accept the null hypothesis). We tend to regard it as random error rather than a real effect.
The mediating effect indicates that depression is an important bridge between impulsiveness and suicidal ideation. On one hand, depression is a vital cause for suicidal ideation, which has been proved in previous studies, but with different interpretations [e.g., hopelessness (47), psychological pain (48), impaired executive function (49), and lack of pleasure (50, 51)]. On the other hand, depression is proved related to impulsiveness (20, 52, 53). In the present study, impulsiveness was scaled as a trait, thus logically pre-existed compared to depression. There was also a study confirming that depression was an outcome of impulsiveness, in which longitudinal designed observation was applied (54). Therefore, impulsiveness predicts depression. The bridge role of depression does not agree with the clinical diathesis-stress model (9), in which depression interacts with impulsiveness. It may not be reasonable to regard depression as stress itself, but a consequence when stress occurred, as is hypothesized in Beck's cognitive model (4).
Simultaneously, impulsiveness is the moderator for the mediating effect of impulsiveness on suicidal ideation through depression. Previous studies (55, 56) has discussed the moderating effect of impulsiveness between depression and suicidal ideation, finding that high level of impulsiveness can increase the depression's effect on suicidal ideation, which agrees with the present study. However, they do not consider the correlation between impulsiveness and depression, which exists and can lead to biases in the moderating effect analyses. Combining these two kinds of effects, we construct the well-fitted moderated mediating model, and illustrate the importance of both impulsiveness and depression in the generating of suicidal ideation. Depression is the necessary mediator between impulsiveness and suicidal ideation. Without depression, impulsiveness may not generate suicidal ideation directly. The precondition of impulsiveness leading to depression may be the existence of stress, in accordance with Beck's cognitive model of suicide (4). Impulsiveness is the reinforcer of its indirect effect on suicidal ideation. Therefore, impulsiveness is vital in generating of suicidal ideation, although it does not contribute to this process independently nor directly.
Some previous studies have proved that age is an important factor of impulsiveness (57, 58). Compared to the adults, adolescents are more impulsive (57, 58). The underlie mechanism may be the “ongoing maturation of parietal brain areas in adolescents” (58). Therefore, age's influence on impulsiveness may be the result of brain development. In the present study, to control the possible confounding effects of age, we only recruited participants who are adolescents and young adults aged from 16 to 21. According to the previous studies (57, 58), they might be more susceptible to impulsiveness than older adults. It is not clear whether the present results can be generalized to individuals of other age groups, which needs more considerations in future studies.
There are still some limitations of this study. First, we do not consider stress in this model, which is probably the moderator of impulsiveness' effect on depression and suicidal ideation. Second, the cross-sectional design cannot interpret the real causal relationships among impulsiveness, depression, and suicidal ideation. We only construct the unidirectional path model based on theoretical analyses. In fact, there are studies (59, 60) show that depression as a trait (e.g., the depressive component of affective temperament) can also predict suicide behaviors. This indicates that depression is not always the outcome of impulsiveness but may overlap with it on the trait level. What roles impulsiveness and depression play in generating suicidal thoughts and behaviors needs more evidence from longitudinal studies. Third, the sample comes from college students. It is not clear whether the results could be generalized to a more widely range of populations. Future studies would include both stress and depressive trait as the predictors and conduct longitudinal design to optimize the model. Meanwhile, more participants of different age, social status, occupations, and ethnics can be included for unbiased results.
Conclusions
The present study finds that impulsiveness indirectly affects suicidal ideation through the mediator depression, and simultaneously moderates the mediating effect. This implies first that people who have impulsive traits are riskier to generate suicidal thoughts because they are more likely to suffer from depression. Second, people who are depressive have even higher risk to develop suicidal thoughts when they simultaneously have impulsive traits. Therefore, in clinical and health care work, when considering depression to prevent suicidal ideation, impulsiveness needs to be monitored throughout the process of premorbid and onset stages of depression.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Army Medical University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
JZ contributed to the design of the research, conducting statistical analyses, and drafting the manuscript. XZ contributed to the arranging of materials and data, conducting statistical analyses, and editing manuscript. GY contributed to the data processing and manuscript revising. ZF contributed to the design of the whole study and critical revising of the manuscript. All authors have read and revised the final manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research is supported by the National Natural Science Foundation of China (81971278).
Acknowledgments
We thank all the co-authors and participants who contributed to this research and the Psychological Training Center of Army Medical University for data arrangement.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.913680/full#supplementary-material
Abbreviations
UPPS, urgency-premeditation-perseverance-sensation-seeking; MODMEDPM, moderated mediation path model; SMODPM, simple moderation path model; SDS, self-rating depression scale; BIS, Barratt impulsiveness scale; SIOSS, self-rating idea of suicide scale; RMSEA, root mean square error of approximation; CFI, comparative fit index; TLI, Tucker & Lewis index; AIC, Akaike information criterion; BIC, Bayesian information criterion; SD, standard deviation; ML, maximum likelihood; SE, standard error; CI, confidence interval.
References
1. World Health Organization. World Health Statistics 2021: Monitoring Health for the SDGs, Sustainable Development Goals. Geneva: World Health Organization (2021).
2. Du R, Jiang G. Suicidal behaviors: risk factor, psychological theory and future research. Adv Psychol Sci. (2015) 23:1437–52. doi: 10.3724/SP.J.1042.2015.01437
3. Serafini G, Solano P, Amore M. Suicidal ideation: a comprehensive overview. In: Weaver B, editor. Suicidal Ideation: Predictors, Prevalence and Prevention. New York, NY: Nova Science Publishers (2015). p. 1–42.
4. Wenzel A, Beck AT. A cognitive model of suicidal behavior: theory and treatment. Appl Prevent Psychol. (2008) 12:189–201. doi: 10.1016/j.appsy.2008.05.001
5. O'Connor RC, Kirtley OJ. The integrated motivational-volitional model of suicidal behaviour. Philos Trans R Soc Lond B Biol Sci. (2018) 373:20170268. doi: 10.1098/rstb.2017.0268
6. Solano P, Ustulin M, Pizzorno E, Vichi M, Pompili M, Serafini G, et al. A Google-based approach for monitoring suicide risk. Psychiatry Res. (2016) 246:581–6. doi: 10.1016/j.psychres.2016.10.030
7. Maguire A, Ross E, O'Hagan D, O'Reilly D. RF12 Suicide ideation and mortality risk: population wide data linkage study. J Epidemiol Commun Health. (2019) 73:A60. doi: 10.1136/jech-2019-SSMabstracts.127
8. Schotte D, Clum G. Problem-solving skills in suicidal psychiatric patients. J Consult Clin Psychol. (1987) 55:49–54. doi: 10.1037/0022-006X.55.1.49
9. Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. (1999) 156:181–9.
10. Zhu H, Yao J, Fan H, Wang Q, Wang X, Gao Q. Prevalence and risk factors of suicidal ideation in adult inpatients with five different types of mental disorders. J Affect Disord. (2021) 291:344–51. doi: 10.1016/j.jad.2021.05.033
11. Kumar P, Kumar P, Mishra S. Socio-demographic variables and suicidal ideation, cognitive distortions, impulsivity and depression in young adults, Patna (Bihar) India. Int J Indian Psychology. (2021) 9:464–79.
12. Loas G, Dalleau E, Lecointe H, Yon V. Relationships between anhedonia, alexithymia, impulsivity, suicidal ideation, recent suicide attempt, C-reactive protein and serum lipid levels among 122 inpatients with mood or anxious disorders. Psychiatry Res. (2016) 246:296–302. doi: 10.1016/j.psychres.2016.09.056
13. Koyama E, Zai CC, Bryushkova L, Kennedy JL, Beitchman JH. Predicting risk of suicidal ideation in youth using a multigene panel for impulsive aggression. Psychiatry Res. (2020) 285:112726. doi: 10.1016/j.psychres.2019.112726
14. Javdani S, Sadeh N. Suicidality as a function of impulsivity, callous-unemotional traits, and depressive symptoms in youth. J Abnorm Psychol. (2011) 120:400–13. doi: 10.1037/a0021805
15. Myung W, Han CE, Fava M, Mischoulon D, Papakostas GI, Heo JY, et al. Reduced frontal-subcortical white matter connectivity in association with suicidal ideation in major depressive disorder. Transl Psychiatry. (2016) 6:e835. doi: 10.1038/tp.2016.110
16. Wenzel A, Brown G, Beck A. A cognitive model of suicidal acts. In: Wenzel A, Brown G, Beck A, editors. Cognitive Therapy for Suicidal Patients: Scientific and Clinical Applications. Washington, DC: American Psychological Association (2009). p. 263–82.
17. Swann A, Dougherty D, Pazzaglia P, Pham M, Steinberg J, Moeller F. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. Am J Psychiatry. (2005) 162:1680–7. doi: 10.1176/appi.ajp.162.9.1680
18. Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, Patton JH. Fifty years of the Barratt impulsiveness scale: an update and review. Pers Individ Differe. (2009) 47:385–95. doi: 10.1016/j.paid.2009.04.008
19. Donati MA, Beccari C, Bacherini A, Capitanucci D, Primi C. Psychometric properties of the short UPPS-P scale in adolescents: gender, age invariance, and validity among italian youth. Addict Behav. (2021) 120:106987. doi: 10.1016/j.addbeh.2021.106987
20. d'Acremont M, Van der Linden M. How is impulsivity related to depression in adolescence? Evidence from a French validation of the cognitive emotion regulation questionnaire. J Adolesc. (2007) 30:271–82. doi: 10.1016/j.adolescence.2006.02.007
21. Jakubczyk A, Klimkiewicz A, Topolewska-Wochowska A, Serafin P, Sadowska-Mazuryk J, Pupek-Pyziol J, et al. Relationships of impulsiveness and depressive symptoms in alcohol dependence. J Affect Disord. (2012) 136:841–7. doi: 10.1016/j.jad.2011.09.028
22. Moustafa AA, Tindle R, Frydecka D, Misiak B. Impulsivity and its relationship with anxiety, depression and stress. Compr Psychiatry. (2017) 74:173–9. doi: 10.1016/j.comppsych.2017.01.013
23. Steiger H, Young SN, Kin NM, Koerner N, Israel M, Lageix P, et al. Implications of impulsive and affective symptoms for serotonin function in bulimia nervosa. Psychol Med. (2001) 31:85–95. doi: 10.1017/S003329179900313X
24. Takahashi T, Oono H, Inoue T, Boku S, Kako Y, Kitaichi Y, et al. Depressive patients are more impulsive and inconsistent in intertemporal choice behavior for monetary gain and loss than healthy subjects–an analysis based on Tsallis' statistics. Neuro Endocrinol Lett. (2008) 29:351–8.
25. Carver CS, Johnson SL, Joormann J. Major depressive disorder and impulsive reactivity to emotion: toward a dual-process view of depression. Br J Clin Psychol. (2013) 52:285–99. doi: 10.1111/bjc.12014
26. Xia C, Wang D, Wu S, Ye J. The development of self-rating idea of suicide scale. J Clin Psychiatry. (2002) 12:100–2. doi: 10.3969/j.issn.1005-3220.2002.02.030
27. Xia C, Wang D, He X, Ye H. Study of self-rating idea undergraduates in the mountain area of southern Zhejiang. Chin J School Health. (2012) 33:144–6. doi: 10.16835/j.cnki.1000-9817.2012.02.006
28. Xie P, Wu K, Zheng Y, Guo Y, Yang Y, He J, et al. Prevalence of childhood trauma and correlations between childhood trauma, suicidal ideation, and social support in patients with depression, bipolar disorder, and schizophrenia in southern China. J Affect Disord. (2018) 228:41–8. doi: 10.1016/j.jad.2017.11.011
29. Liu ST, Wu X, Wang N, Zhao QQ, Xiao L, Fang CK, et al. Serial multiple mediation of demoralization and depression in the relationship between hopelessness and suicidal ideation. Psychooncology. (2020) 29:1321–8. doi: 10.1002/pon.5439
30. Zhou L, Xiao S, He X, Li J, Liu H. Reliability and validity of Chinese version of Barratt Impulsiveness Scale-11. Chin J Clin Psychol. (2006) 14:343–4. doi: 10.16128/j.cnki.1005-3611.2006.04.005
31. Zung WW. A Self-Rating Depression Scale. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
32. Zung WW, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. (1965) 13:508–15. doi: 10.1001/archpsyc.1965.01730060026004
33. Colon de. Marti LN, Guzman Yunque FS, Guevara-Ramos LM. Early detection of depression using the Zung Self-Rating Depression Scale. P R Health Sci J. (1997) 16:375–9.
34. Kawada T, Suzuki S. Factor structure of self-rating depression scale by Zung and prevalence of depressive state of night shift workers. Sangyo Igaku. (1992) 34:131–6. doi: 10.1539/joh1959.34.131
35. Martinez KG, Guiot HM, Casas-Dolz I, Gonzalez-Tejera G, Colon de. Marti LN. Applicability of the Spanish translation of the zung self-rating depression scale in a general puerto rican population. P R Health Sci J. (2003) 22:179–85.
36. Wang C, Cai Z, Xu Q. Self-rating depression scale: an analysis for 1,340 general participants. Chin J Nerv Ment Dis. (1986) 12:267–8.
39. Stride C, Gardner S, Catley N, Thomas F. Mplus Code for Mediation, Moderation, Moderated Mediation Models. (2015). Available online at: http://www.offbeat.group.shef.ac.uk/FIO/mplusmedmod.htm
40. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press (2013).
41. Podsakoff P, MacKenzie S, Lee J-Y, Podsakoff N. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
42. Finney SJ, DiStefano C. Nonnormal and categorical data in structural equation modeling. In: Hancock GR, Mueller RO, editors. Structural Equation Modeling: A Second Course. 2nd ed. Charlotte, NC: IAP Information Age Publishing (2013). p. 439–92.
43. Wen ZL, Hau KT, Marsh HW. Structural equation model testing. Cutoff criteria for goodness of fit indices and chi-square test. Acta Psychologica Sinica. (2004) 36:186–94.
44. MacKinnon D, Lockwood C, Hoffman J, West S, Sheets V. A comparison of methods to test the mediation and other intervening variable effects. Psychol Methods. (2002) 8:1–35. doi: 10.1037/1082-989X.7.1.83
45. MacKinnon D. Introduction to Statistical Mediation Analysis. New York, NY: Lawrence Erlbaum Associates (2008).
46. Shrout P, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. (2002) 7:422–45. doi: 10.1037/1082-989X.7.4.422
47. Lamis D, Ballard E, May A, Dvorak R. Depressive symptoms and suicidal ideation in college students: the mediating and moderating roles of hopelessness, alcohol problems, and social support. J clin psychol. (2016) 72:919–32. doi: 10.1002/jclp.22295
48. van Heeringen K, Van den Abbeele D, Vervaet M, Soenen L, Audenaert K. The functional neuroanatomy of mental pain in depression. Psychiatry Res. (2010) 181:141–4. doi: 10.1016/j.pscychresns.2009.07.011
49. Gujral S, Dombrovski AY, Butters M, Clark L, Reynolds CF, Szanto K. Impaired executive function in contemplated and attempted suicide in late life. Am J Geriatr Psychiatry. (2014) 22:811–9. doi: 10.1016/j.jagp.2013.01.025
50. Winer ES, Nadorff MR, Ellis TE, Allen JG, Herrera S, Salem T. Anhedonia predicts suicidal ideation in a large psychiatric inpatient sample. Psychiatry Res. (2014) 218:124–8. doi: 10.1016/j.psychres.2014.04.016
51. Yang X, Liu S, Wang D, Liu G, Harrison P. Differential effects of state and trait social anhedonia on suicidal ideation at 3-months follow up. J Affect Disord. (2019) 262:23–30. doi: 10.1016/j.jad.2019.10.056
52. Carver CS, Johnson SL, Joormann J. Serotonergic function, two-mode models of self-regulation, and vulnerability to depression: what depression has in common with impulsive aggression. Psychol Bull. (2008) 134:912–43. doi: 10.1037/a0013740
53. Johnson SL, Tharp JA, Peckham AD, Carver CS, Haase CM. A path model of different forms of impulsivity with externalizing and internalizing psychopathology: Towards greater specificity. Br J Clin Psychol. (2017) 56:235–52. doi: 10.1111/bjc.12135
54. Hasegawa A, Hattori Y, Nishimura H, Tanno Y. Prospective associations of depressive rumination and social problem solving with depression: a 6-month longitudinal study. Psychol Rep. (2015) 116:870–88. doi: 10.2466/02.20.PR0.116k28w7
55. Wang Y-y, Jiang N-z, Cheung E, Sun H-w, Chan R. Role of depression severity and impulsivity in the relationship between hopelessness and suicidal ideation in patients with major depressive disorder. J Affect Dis. (2015) 183:83–9. doi: 10.1016/j.jad.2015.05.001
56. Radzi M, Mohd Radzi Tarmizi AH, Abdul Kadir NBy, Kadir FA, Rahman A, Roseliza-Murni A, et al. Moderation effect of impulsivity in the relationship between depression and suicide ideation among late adolescent in Malaysia. Int J Res Bus Soc Sci. (2020) 10:110–9. doi: 10.6007/IJARBSS/v10-i10/7920
57. Vaidya JG, Grippo AJ, Johnson AK, Watson D. A comparative developmental study of impulsivity in rats and humans: the role of reward sensitivity. Ann N Y Acad Sci. (2004) 1021:395–8. doi: 10.1196/annals.1308.051
58. Ripke S, Hubner T, Mennigen E, Muller KU, Rodehacke S, Schmidt D, et al. Reward processing and intertemporal decision making in adults and adolescents: the role of impulsivity and decision consistency. Brain Res. (2012) 1478:36–47. doi: 10.1016/j.brainres.2012.08.034
59. Baldessarini RJ, Vazquez GH, Tondo L. Affective temperaments and suicidal ideation and behavior in mood and anxiety disorder patients. J Affect Disord. (2016) 198:78–82. doi: 10.1016/j.jad.2016.03.002
Keywords: impulsiveness, depression, suicidal ideation, moderated mediation path model, indirect effect
Citation: Zhang J, Zhang X, Yang G and Feng Z (2022) Impulsiveness indirectly affects suicidal ideation through depression and simultaneously moderates the indirect effect: A moderated mediation path model. Front. Psychiatry 13:913680. doi: 10.3389/fpsyt.2022.913680
Received: 06 April 2022; Accepted: 01 July 2022;
Published: 27 July 2022.
Edited by:
Johnette Magner, Louisiana Tech University, United StatesReviewed by:
Gianluca Serafini, San Martino Hospital (IRCCS), ItalyCaroline Elise Sagrera, Louisiana State University Health Shreveport, United States
Copyright © 2022 Zhang, Zhang, Yang and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhengzhi Feng, Znp6QHRtbXUuZWR1LmNu
 Jingxuan Zhang
Jingxuan Zhang Xiaolin Zhang
Xiaolin Zhang Guoyu Yang
Guoyu Yang Zhengzhi Feng
Zhengzhi Feng