
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 24 August 2022
Sec. Computational Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.907620
This article is part of the Research Topic New Advancement in Network and Path-analysis Approaches for the Study of Disorders within the Impulse-Compulsive Spectrum Disorders View all 7 articles
 Giammarco Cascino1*
Giammarco Cascino1* Francesca Marciello1
Francesca Marciello1 Giulia D’Agostino1
Giulia D’Agostino1 Rita Toricco2
Rita Toricco2 Eugenia Barone2
Eugenia Barone2 Alessio Maria Monteleone2
Alessio Maria Monteleone2Aggressive behaviors have been reported to be more frequent in people with eating disorders (ED), especially bulimia nervosa (BN). Network Analysis (NA) is particularly useful or examining the interactions among symptoms of comorbid conditions through the identification of “bridge symptoms,” defined as those symptoms playing a key role in the connection between two syndromic clusters. The aim of the present study was to investigate the association of ED core symptoms and ED-related psychopathology with aggressiveness in a clinical sample of women with BN through NA. Two hundred and seventy-nine women with BN completed the Eating Disorder Inventory-2 and the Buss-Durkee Hostility Inventory. A NA was conducted, including ED symptoms and aggressiveness measures. The bridge function was implied to identify symptoms bridging ED symptoms and aggressiveness. The most connected nodes among communities were asceticism and impulsivity from ED-related psychopathology, drive for thinness from ED-core psychopathology and guilt and suspicion from aggressiveness domain. In particular, drive for thinness connected ED-core community to verbal hostility, while impulsivity connected ED-related symptoms to guilt and suspicion of aggressiveness community. In conclusion the present study showed that in people with BN guilt is the specific negative emotion of the hostile dimensions that may be bidirectionally associated with ED symptoms.
Aggressiveness is defined as the intention to harm someone (1, 2). However, a distinction should be made between instances where harming others is secondary to the main goal of obtaining an advantage for themselves and other forms of aggressive behaviors in which the intention to harm someone is primary and is raised by emotionally driven lack of impulses control (3). The affective-driven form of aggressive behaviors is conceived as maladaptive and source of conflict between the subject and his family and/or peers (4). Aggressive behaviors have been reported to be more frequent in people with eating disorders (EDs), especially bulimia nervosa (BN), than in non-clinical populations (5–7). They were associated with the severity of bulimic symptoms (5, 8), self-harming behaviors (8, 9), comorbidity (10), and poorer treatment outcome (5, 11).
The association between aggressiveness and ED symptoms has been investigated considering the mediation role of several factors. First, people with ED and comorbid major depression disorder were characterized by irritable mood and showed anger attacks and angry outbursts with a prevalence approximately double than depressed patients without ED (10). A few studies have assessed anger and personality concomitantly in people with BN and, even if they did not reveal replicable patterns of association between anger and personality characteristics, a full mediation of anger between cooperativeness and binge-eating and impulsiveness has been found, supporting a relationship between anger feelings and interpersonal difficulties (12, 13). Finally, impulsive behaviors, such as self-injurious behavior and drug or alcohol abuse, have consistently been found associated with anger and eating disorder symptoms (14, 15). Because of wide differences across studies in methods and sample composition, the relationships between aggressiveness and ED psychopathology are not conclusive and need to be further investigated.
The application of network analysis (NA) in the study of psychopathology has become more common in the recent years. Indeed, the NA approach is believed to be a particularly useful tool for examining the interactions among symptoms of comorbid conditions (16). Networks are composed of nodes, representing the assessed symptoms of a psychiatric syndrome, and edges, which are the connections among nodes. A further use of NA is the identification of “bridge symptoms,” defined as those symptoms playing a key role in the connection between two syndromic clusters, namely, groups of symptoms that are very closely related (17). Therefore, it is thought that the nodes with the highest bridge centrality are spreading the activation of symptoms from one disorder to another and promote psychiatric comorbidity (18). A recent systematic review (19) showed that, in addition to ED-specific symptoms (i.e., overvaluation of shape and weight), anxious and depressive symptoms are central network nodes across ages and diagnoses in EDs. This review also included studies that examined bridge centrality in ED networks (19) and identified low self-esteem and interoceptive awareness as connecting ED-related symptoms to anxious and depressive symptoms (20–23). However, this review highlighted the need for future studies to include in the network nodes related to general psychopathology in addition to those specifically related to ED symptoms. To our knowledge, no study so far has applied the NA and the bridge function to examine the relationships between aggressive behaviors and ED symptoms.
Therefore, the aim of the present study was to investigate the association of ED core symptoms and ED-related psychopathology with aggressiveness in a clinical sample of women with BN. First, to identify the most central symptoms of each psychopathological domain, two separate networks were estimated: one for ED psychopathology and one for the aggressiveness dimension. Second, a network including both ED psychopathology and aggressiveness related features was estimated to identify bridge nodes between the ED symptoms and aggressiveness clusters.
Consecutive patients attending the Eating Disorder Centre of the Department of Psychiatry at the University of Campania “Luigi Vanvitelli” were included in the study if they met the following criteria: (a) female sex; (b) age ≥ 18; (c) current diagnosis of BN according to the fifth edition of Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria and (d) willingness to sign a written informed consent. Trained psychiatrists made diagnostic assessment by means of the Structured Clinical Interview or DSM-5 Disorders-Research Version (24) and collected sociodemographic and clinical data. The Italian version of Eating Disorder Inventory-2 (EDI-2) (25) and Buss-Durkee Hostility Inventory (BDHI) (26) were completed at admission before starting specific treatment programs. The study was approved by the Institutional Board of the “Department of Mental Health, Physical Health, and Preventive Medicine” of the University of Campania “Luigi Vanvitelli,” Naples, Italy.
The EDI-2 is a 92 items self-report questionnaire, which provides 3 subscales measuring the ED core psychopathology (i.e., drive for thinness, body dissatisfaction, and bulimia) and 8 subscales measuring ED-related psychopathology: ineffectiveness, maturity fear, social insecurity, perfectionism, interpersonal distrust, impulsivity, interoceptive awareness, and asceticism. Cronbach’s α ranged from 0.90 (drive for thinness) to 0.71 (maturity fear).
The BDHI consists of 75 dichotomous items specifically developed to explore different subtypes of hostility and guilt (27). Heightened scores on the BDHI reflect greater hostility. This questionnaire includes the following subscales: assault, indirect hostility, irritability, negativism, resentment, suspicion, verbal hostility, guilt. Cronbach’s α for the BDHI total score was 0.84.
In the present study, partial correlation networks were estimated in which nodes represent observed variables and edges represent partial correlation coefficients between two variables after conditioning on all other variables in the dataset (28). Network associations do not imply any directionality, which means the lack of any causal inference or direction in the association. The thickness of an edge graphically represents the magnitude of the association. NA was performed through R, version 3.4.4, using qgraph package (29) that utilizes the package glasso in combination with Extended Bayesian Information Criterion (EBIC) model selection (30). The “least absolute shrinkage and selection operator” (LASSO) is a form of regularization, which applies a penalty by limiting the total sum of absolute parameter values leading many edges to zero and dropping them out of the model, returning a sparse and more interpretable network (31). The LASSO utilizes a tuning parameter to control the degree to which regularization is applied, i.e., EBIC, which was set to 0.5 in the analyses. Individuals with missing data (n = 21) were excluded from the analysis.
A typical way of assessing the importance of nodes in the network is to compute centrality indices of the network structure (32). The most informative is the node strength, that is the sum of the absolute edge-weights between a node and all other nodes to which it is connected in the network.
Following the Epskamp et al. recommendations (33) to assess the accuracy of the edge-weights and strength centrality index, we performed non-parametric bootstrap (nboots = 2,500) and obtained bootstrapped confidence intervals (CI) showing the accuracy of edge-weight estimates. Then we proceeded to the calculation of the correlation stability coefficient, which is the maximum proportion of population that can be dropped so that the correlation between the recalculated indices of the obtained networks and those of the original network is at least 0.7. Analyses of network accuracy were performed using the bootnet package (34).
To identify the bridge symptoms, which play a primary role in connecting two or more symptom clusters (17), we estimate the bridge strength centrality index, which is the absolute sum of all edges that connect a node to all nodes that are not part of the same community (35). Thus, a high bridge expected value indicates that the node is strongly connected to other nodes included in other communities. The bridge function from networktools package was used (36). We applied a priori definition of communities that can be defined as clusters of symptoms. Three communities were defined: the first referred to ED core psychopathology and included EDI-2 drive for thinness, body dissatisfaction and bulimia sub-scores; the second was related to ED-related psychopathology and was composed by the other sub-scores of the EDI-2; the third was related to aggressiveness and included all sub-scores from the BDHI. First, all communities were considered for the estimate of bridge strength centrality, then communities to be included in the analysis were specified to disentangle the bridge symptoms connecting each community to the other two.
Three hundred women met the inclusions criteria. Two hundred-seventy-nine completed the self-report questionnaires. Demographic and clinical characteristics of the study population are reported in Table 1. Sixty-nine patients were taking antidepressant medications, namely SSRI.
In the network including ED-core and related psychopathology the node with the highest strength centrality was interoceptive awareness (M = 1.27), followed by ineffectiveness (M = 1.07), while in the network composed by BDHI measures the node with the highest strength centrality was resentment (M = 1.05), followed by verbal hostility (M = 0.99) (Figure 1).
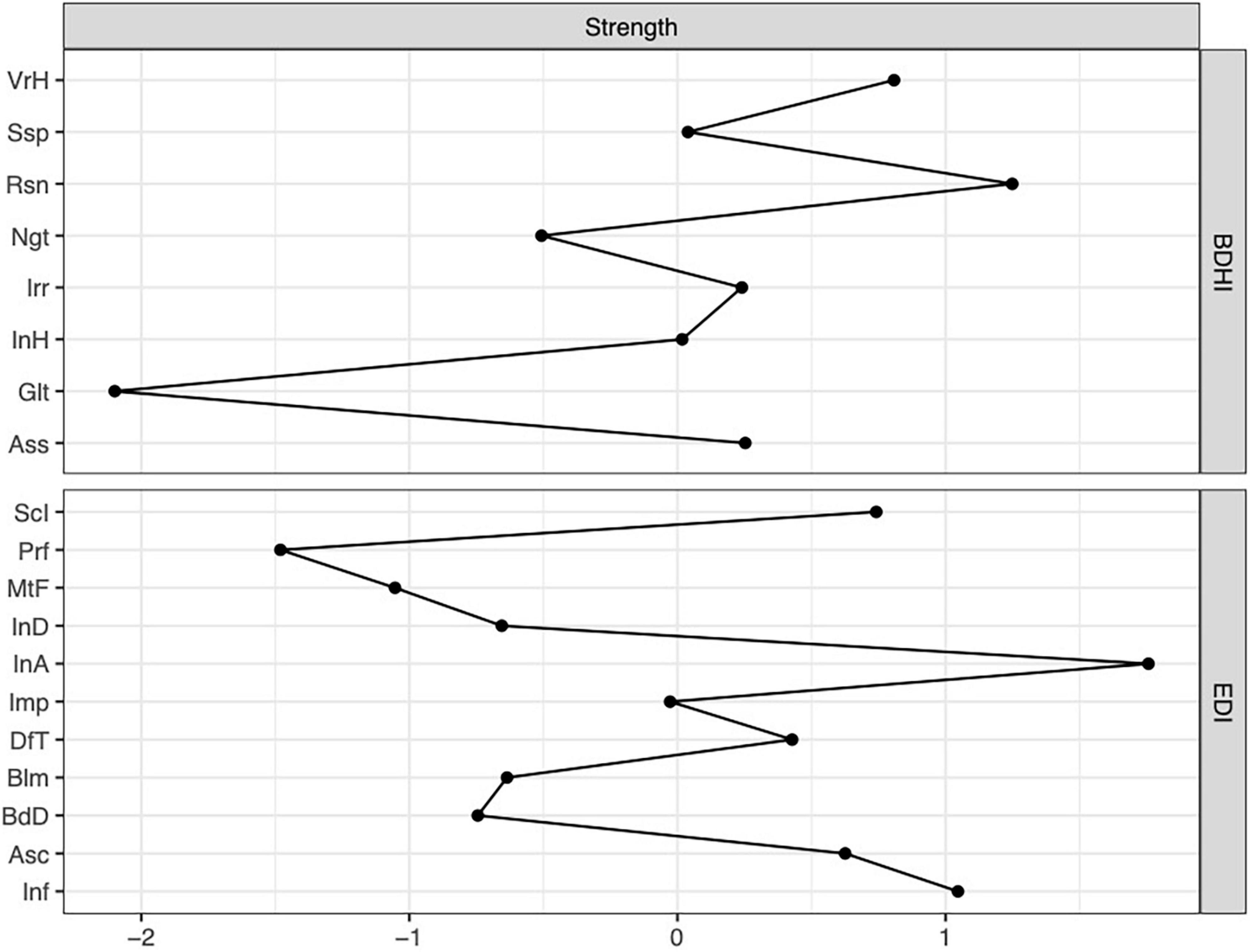
Figure 1. Plot of strength centrality index of the separate network for Eating Disorder Inventory-2 (EDI) and Buss-Durkee Hostility Inventory (BDHI). VrH, Verbal hostility; Ssp, Suspicion; Rsn, Resentments; Ngt, Negativism; Irr, Irritability; InH, Indirect hostility; Glt, Guilt; Ass, Assault; ScI, Social Insecurity; Prf, Perfectionism; MtF, Maturity Fear; InD, Interpersonal distrust; InA, Interoceptive awareness; Imp, Impulsivity; DfT, Drive for Thinness; Blm, Bulimia; BdD, Body Dissatisfaction; Asc, Asceticism; Inf, Ineffectiveness.
The partial correlation network including both aggressiveness variables and ED-core and related psychopathology is reported in Figure 2. When considering all the communities in the estimate of bridge strength centrality, the most connected nodes among communities were asceticism and impulsivity from ED-related psychopathology, drive for thinness from ED-core psychopathology and guilt and suspicion from the hostility domain (Figure 3). When considering the ED-core and the ED-related communities, the nodes with the highest bridge strength were the ED-core psychopathological dimensions drive for thinness and bulimia (M = 0.34 and 0.33, respectively) and the ED-related psychopathological dimensions asceticism and interoceptive awareness (M = 0.36 and 0.26, respectively). When considering the ED-core and the hostility communities, the nodes with the highest bridge strength were drive for thinness and verbal hostility (M = 0.03, both) connected to each other by a negative edge. Finally, when considering the ED-related psychopathology and the hostility communities, the nodes with the highest bridge strength were impulsivity (M = 0.45) from ED-related psychopathology and guilt and suspicion (M = 0.46 and 0.38, respectively) from hostility community. Plots of bridge strength centrality are reported in the supplementary materials. Centrality stability coefficient for strength of the network of ED-psychopathology was 0.52, while that of the network of hostility symptoms was 0.44. Centrality stability coefficient of the network including both ED and hostility symptoms was 0.43 for bridge strength.
The current study investigated the psychopathology related to ED-specific symptoms and to the aggressiveness dimension in individuals with BN through NA. Also, the association between hostility and ED psychopathological features was evaluated through the bridge function analysis. The first finding of our study was that interoceptive awareness and ineffectiveness were the most central nodes in the network composed by measures of ED psychopathology, while resentment and verbal hostility were the most central nodes in the network composed by the BDHI sub-scores.
The high centrality of ineffectiveness and interoceptive awareness is consistent with previous studies exploring ED psychopathology through self-report questionnaires assessing not only ED-specific psychopathological features but also general psychopathology (19). Previous studies which included EDI-2 sub-scores in the networks merged individuals with different ED diagnoses in a unique ED group (37, 38) or were conducted in people with AN (39, 40). Only one study (41) has conducted an assessment of ED psychopathology through the EDI-2 in people with BN and found that ineffectiveness, anxiety, and depression scores and interpersonal sensitivity were the most central nodes in a network composed also by measures of general psychopathology and personality dimensions. Our findings are partially consistent and support the hypothesis that not only ED specific symptoms (e.g., bulimic symptoms measured through the corresponding EDI-2 subscale) but also more general features of psychopathology are essential in BN. The importance of ineffectiveness in individuals with BN has also been shown in a previous network study (42) which showed that this node was included in the shortest pathway between early traumatic experiences and ED-related core symptoms.
The second finding of the present study was that in the network composed by BDHI sub-scores, resentment, and verbal hostility were the nodes most connected to others. While resentment refers to jealousy and hatred of others, verbal hostility refers to expression of negative affect in both the style and content of speech (43). These variables both showed strong connection with irritability, while resentment showed also a strong connection with suspicion (i.e., the projection of hostility into others) and verbal hostility was strongly and positively associated with negativism, that is an oppositional behavior usually directed against authority. The lack of directionality of the current network edges and the cross-sectional nature of these findings do not allow to distinguish the direction of these connections: thus, a bidirectional relationship between these dimensions should be interpreted. Future studies will have to clarify if this aggressiveness profile characterizes individuals with BN and differs between the main ED diagnoses.
The partial correlation network including both aggressiveness variables and ED-core and related psychopathology with the application of the bridge strength estimates showed the importance of impulsivity, interoceptive awareness, suspicion, and guilt in the association between ED-core symptoms and aspects of hostility. Even if it is not possible to draw causal inference from the connections among variables, since network edges are undirected, the associations between these nodes may be interpreted in two ways. First, both suspicion and guilt could arise from the feeling of being unable to control body shape and weight or from conflicts due to disordered eating behaviors with feelings of being bad and having done wrong. Indeed, patients may project hostility onto others when they are not able to accomplish disordered eating behaviors because they feel to be inhibited by others. Second, suspicion and guilt may represent the negative affects that lead to eating psychopathology in individuals with BN. Indeed, people with a lifetime diagnosis of EDs showed an attentional bias to rejecting faces and a difficulty disengaging attention from these stimuli (44). This attentional bias to rejection was found to be positively correlated with adverse childhood experiences, which have been associated both with higher rates of aggressive behaviors and EDs symptoms (45, 46). Moreover, the negative interpretation bias toward social stimuli correlated with clinical symptoms (47). The tendency to act impulsively in response to negative emotions may trigger loss-of-control eating episodes (48). Indeed, negative mood has been found to precede often binge eating episodes and compensatory behaviors in patients with BN (49). Furthermore, interoceptive awareness is highly associated with the hostile dimensions. Impaired interoceptive awareness play a central role in the pointing to reduced trusting and listening of visceral signals related to body states for emotional information and behavioral guidance (50). Also, individuals with EDs show low ability to cope with distress by attending to their body signals (50). The current findings outline a possible connection between this psychopathological feature and hostile dimensions suggesting that unhealthy eating behaviors may serve to manage uncomfortable body sensations when perceiving guilt or hostile feelings.
The present study presents some limitations that need to be acknowledged. First, the use of cross-sectional data does not allow to draw causality effects. Second, it must be considered that the use of self-report questionnaires, although consistent with previous literature, may have led to the underestimation of aggressive behaviors. Then, assessments of personality traits and measures of general psychopathology, such as depression or anxiety, which are frequent in EDs (51), are lacking. Indeed, psychiatric comorbid depressive or anxiety syndromes could have affected anger expression, since people with ED and comorbid major depressive disorder exhibited outbursts of anger twice than depressed patients without ED (10). From a clinical point of view, if confirmed by future studies, the observed connections of hostility dimensions with impulsivity and interoceptive awareness may be worth of therapeutic attention.
This supports the importance to assess impulsivity to offer proper treatment for individuals with BN. Indeed, treatments that aim to manage impulsive behaviors can be particularly helpful as they act on what connects the ED psychopathology to hostility, which is known to worsen the outcome of treatments (11). For example, the dialectical behavior therapy aiming to manage impulsive behaviors (52) is a skills-based approach for teaching individuals general problem-solving skills, emotional regulation strategies, interpersonal skills, and distress tolerance (53). It could help to improve hostility behaviors, and it has been adapted and applied to the treatment of individuals with BN (54).
In conclusion the present results show for the first time that in people with BN guilt is the specific negative emotion of the hostile dimensions that may be bidirectionally associated with ED symptoms, although the verbal hostility and resentment are highly central in the hostility profile of these individuals. This may point to an ambivalent profile of people with BN which needs to be further explored in future studies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Board of the “Department of Mental Health, Physical Health, and Preventive Medicine” of the University of Campania “Luigi Vanvitelli,” Naples, Italy. The patients/participants provided their written informed consent to participate in this study.
GC and AM designed the study, wrote the protocol, and wrote the manuscript. FM, GD’A, and RT collected the data. GC and EB performed the statistical analyses. All authors contributed to the article and approved the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Gothelf D, Apter A, van Praag HM. Measurement of aggression in psychiatric patients. Psychiatry Res. (1997) 71:83–95.
2. Ramírez JM, Andreu JM. Aggression, and some related psychological constructs (anger, hostility, and impulsivity). Some comments from a research project. Neurosci Biobehav Rev. (2006) 30:276–91. doi: 10.1016/j.neubiorev.2005.04.015
4. Shugar G, Krueger S. Aggressive family communication, weight gain, and improved eating attitudes during systemic family therapy for anorexia nervosa. Int J Eat Disord. (1995) 17:23–31. doi: 10.1002/1098-108x(199501)17:1<23::aid-eat2260170103>3.0.co;2-8
5. Fava M, Rappe SM, West J, Herzog DB. Anger attacks in eating disorders. Psychiatry Res. (1995) 56:205–12. doi: 10.1016/0165-1781(95)02577-j
6. Zaitsoff SL, Geller J, Srikameswaran S. Silencing the self and suppressed anger: Relationship to eating disorder symptoms in adolescent females. Eur Eat Disord Rev. (2002) 10:51–60.
7. Miotto P, Pollini B, Restaneo A, Favaretto G, Preti A. Aggressiveness, anger, and hostility in eating disorders. Compr Psychiatry. (2008) 49:364–73. doi: 10.1016/j.comppsych.2008.01.004
8. Krug I, Bulik CM, Vall-Llovera ON, Granero R, Agüera Z, Villarejo C, et al. Anger expression in eating disorders: Clinical, psychopathological and personality correlates. Psychiatry Res. (2008) 161:195–205. doi: 10.1016/j.psychres.2007.10.003
9. Truglia E, Mannucci E, Lassi S, Maria Rotella C, Faravelli C, Ricca V. Aggressiveness, anger and eating disorders: A review. Psychopathology. (2006) 39:55–68. doi: 10.1159/000090594
10. Giovanni AD, Carla G, Enrica M, Federico A, Maria Z, Secondo F. Eating disorders and major depression: Role of anger and personality. Depress Res Treat. (2011) 2011:194732. doi: 10.1155/2011/194732
11. Fassino S, Abbate-Daga G, Piero A, Leombruni P, Rovera GG. Dropout from brief psychotherapy within a combination treatment in bulimia nervosa: Role of personality and anger. Psychother Psychosom. (2003) 72:203–10. doi: 10.1159/000070784
12. Fassino S, Daga GA, Piero A, Leombruni P, Rovera GG. Anger and personality in eating disorders. J Psychosom Res. (2001) 51:757–64. doi: 10.1016/s0022-3999(01)00280-x
13. Amianto F, Siccardi S, Abbate-Daga G, Marech L, Barosio M, Fassino S. Does anger mediate between personality and eating symptoms in bulimia nervosa?. Psychiatry Res. (2012) 200:502–12. doi: 10.1016/j.psychres.2012.07.036
14. Favaro A, Santonastaso P. Self-injurious behavior in anorexia nervosa. J Nerv Ment Dis. (2000) 188:537–42. doi: 10.1097/00005053-200008000-00010
15. Miotto P, Preti A. Eating disorders and suicide ideation: The mediating role of depression and aggressiveness. Compr Psychiatry. (2007) 48:218–24. doi: 10.1016/j.comppsych.2007.01.006
16. Borsboom D, Cramer AO. Network analysis: An integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608
17. Jones PJ, Ma R, McNally RJ. Bridge centrality: A network approach to understanding comorbidity. Multivariate Behav Res. (2021) 56:353–67. doi: 10.1080/00273171.2019.1614898
18. Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: A review of recent insights. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:1–10.
19. Monteleone AM, Cascino G. A systematic review of network analysis studies in eating disorders: Is time to broaden the core psychopathology to non specific symptoms. Eur Eat Disord Rev. (2021) 29:531–47. doi: 10.1002/erv.2834
20. Elliott H, Jones PJ, Schmidt U. Central symptoms predict posttreatment outcomes and clinical impairment in anorexia nervosa: A network analysis. Clin Psychol Sci. (2020) 8:139–54. doi: 10.1177/2167702619865958
21. Forrest LN, Sarfan LD, Ortiz SN, Brown TA, Smith AR. Bridging eating disorder symptoms and trait anxiety in patients with eating disorders: A network approach. Int J Eat Disord. (2019) 52:701–11. doi: 10.1002/eat.23070
22. Kerr-Gaffney J, Halls D, Harrison A, Tchanturia K. Exploring relationships between autism spectrum disorder symptoms and eating disorder symptoms in adults with anorexia nervosa: A network approach. Front Psychiatry. (2020) 11:401. doi: 10.3389/fpsyt.2020.00401
23. Monteleone AM, Mereu A, Cascino G, Criscuolo M, Castiglioni MC, Pellegrino F, et al. Re-conceptualization of anorexia nervosa psychopathology: A network analysis study in adolescents with short duration of the illness. Int J Eat Disord. (2019) 52:1263–73. doi: 10.1002/eat.23137
24. First MB, Williams JBW, Karg RS, Spitzer RL. Structured clinical interview for DSM-5 research version. Arlington, VA: American Psychiatric Association (2015).
25. Rizzardi M, Trombini E, Trombini G. Manuale: EDI-2. Eating Disorder Inventory-2. Firenze: Giunti Organizzazioni Speciali (1995).
26. Castrogiovanni P, Maremmani I, Di Muro A, Nistico G, Akiskal HS. Aggressive behaviour and hostility in depression: Clinical aspects. In: Placidi GF, Dell’Osso L editors. Recurrent Mood Disorders. Berlin: Springer-Verlag (1993). p. 51–65.
27. Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. (1957) 21:343–9. doi: 10.1037/h0046900
28. Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. (2018) 23:617–34. doi: 10.1037/met0000167
29. Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. Qgraph: Network visualizations of relationships in psychometric data. J Stat Softw. (2012) 48:1–18. doi: 10.18637/jss.v048.i04
30. Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. (2008) 95:759–71. doi: 10.1093/biomet/asn034
31. Tibshirani R. Regression shrinkage and selection via the lasso: A retrospective. J R Statist Soc B. (2011) 73:273–82. doi: 10.1111/j.1467-9868.2011.00771.x
32. Costantini G, Epskamp S, Borsboom D, Perugini M, Mottus R, Waldorp LJ, et al. State of the aRt personality research: A tutorial on network analysis of personality data in R. J Res Pers. (2015) 54:13–29. doi: 10.1016/j.jrp.2014.07.003
33. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
34. Epskamp S, Maris G, Waldorp L, Borsboom D. Network psychometrics. In: Irwing P, Hughes D, Booth T editors. Handbook of Psychometrics. New York, NY: Wiley (2016).
35. Levinson CA, Brosof LC, Vanzhula I, Christian C, Jones P, Rodebaugh TL, et al. Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. Int J Eat Disord. (2018) 51:693–709. doi: 10.1002/eat.22890
36. Jones P. Networktools: Assorted Tools for Identifying Important Nodes in Networks. R package Version 1.1.0. (2017). Available online at: https://CRAN.Rproject.org/package=networktools (accessed February 2, 2022).
37. Vervaet M, Puttevils L, Hoekstra RHA, Fried E, Vanderhasselt MA. Transdiagnostic vulnerability factors in eating disorders: A network analysis. Eur Eat Disord Rev. (2021) 29:86–100. doi: 10.1002/erv.2805
38. Schlegl S, Smith KE, Vierl L, Crosby RD, Moessner M, Neumayr C, et al. Using network analysis to compare diagnosis-specific and age-specific symptom networks in eating disorders. Int J Eat Disord. (2021) 54:1463–76. doi: 10.1002/eat.23523
39. Olatunji BO, Levinson C, Calebs B. A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry Res. (2018) 262:270–81. doi: 10.1016/j.psychres.2018.02.027
40. Cascino G, Castellini G, Stanghellini G, Ricca V, Cassioli E, Ruzzi V, et al. The role of the embodiment disturbance in the anorexia nervosa psychopathology: A network analysis study. Brain Sci. (2019) 9:276. doi: 10.3390/brainsci9100276
41. Solmi M, Collantoni E, Meneguzzo P, Degortes D, Tenconi E, Favaro A. Network analysis of specific psychopathology and psychiatric symptoms in patients with eating disorders. Int J Eat Disord. (2018) 51:680–92. doi: 10.1002/eat.22884
42. Monteleone AM, Tzischinsky O, Cascino G, Alon S, Pellegrino F, Ruzzi V, et al. The connection between childhood maltreatment and eating disorder psychopathology: A network analysis study in people with bulimia nervosa and with binge eating disorder. Eat Weight Disord. (2022) 27:253–61. doi: 10.1007/s40519-021-01169-6
43. Vassar M, Hale W. Reliability reporting across studies using the Buss Durkee Hostility Inventory. J Interpers Violence. (2009) 24:20–37. doi: 10.1177/0886260508314931
44. Cardi V, Di Matteo R, Corfield F, Treasure J. Social reward and rejection sensitivity in eating disorders: An investigation of attentional bias and early experiences. World J Biol Psychiatry. (2013) 14:622–33. doi: 10.3109/15622975.2012.665479
45. Driessen M, Schroeder T, Widmann B, von Schönfeld CE, Schneider F. Childhood trauma, psychiatric disorders, and criminal behavior in prisoners in Germany: A comparative study in incarcerated women and men. J Clin Psychiatry. (2006) 67:1486–92. doi: 10.4088/jcp.v67n1001
46. Monteleone AM, Cascino G, Ruzzi V, Pellegrino F, Patriciello G, Barone E, et al. Emotional traumatic experiences significantly contribute to identify a maltreated ecophenotype sub-group in eating disorders: Experimental evidence. Eur Eat Disord Rev. (2021) 29:269–80. doi: 10.1002/erv.2818
47. Cardi V, Turton R, Schifano S, Leppanen J, Hirsch CR, Treasure J. Biased interpretation of ambiguous social scenarios in anorexia nervosa. Eur Eat Disord Rev. (2017) 25:60–4. doi: 10.1002/erv.2493
48. Wolz I, Granero R, Fernández-Aranda F. A comprehensive model of food addiction in patients with binge-eating symptomatology: The essential role of negative urgency. Compr Psychiatry. (2017) 74:118–24. doi: 10.1016/j.comppsych.2017.01.012
49. Becker KR, Fischer S, Crosby RD, Engel SG, Wonderlich SA. Dimensional analysis of emotion trajectories before and after disordered eating behaviors in a sample of women with bulimia nervosa. Psychiatry Res. (2018) 268:490–500. doi: 10.1016/j.psychres.2018.08.008
50. Brown TA, Berner LA, Jones MD, Reilly EE, Cusack A, Anderson LK, et al. Psychometric evaluation and norms for the multidimensional assessment of interoceptive awareness (MAIA) in a clinical eating disorders sample. Eur Eat Disord Rev. (2017) 25:411–6. doi: 10.1002/erv.2532
51. Spindler A, Milos G. Links between eating disorder symptom severity and psychiatric comorbidity. Eat Behav. (2007) 8:364–73. doi: 10.1016/j.eatbeh.2006.11.012
52. Linehan MM. Skills Training Manual for Borderline Personality Disorder. New York: Guilford (1993).
53. Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. (2001) 158:1783–93. doi: 10.1176/appi.ajp.158.11.1783
Keywords: eating disorders, bulimia nervosa, aggressiveness, hostility, network analysis
Citation: Cascino G, Marciello F, D’Agostino G, Toricco R, Barone E and Monteleone AM (2022) Using network analysis to explore the association between eating disorders symptoms and aggressiveness in Bulimia nervosa. Front. Psychiatry 13:907620. doi: 10.3389/fpsyt.2022.907620
Received: 29 March 2022; Accepted: 22 July 2022;
Published: 24 August 2022.
Edited by:
Isabel Krug, The University of Melbourne, AustraliaReviewed by:
Giovanni Castellini, University of Florence, ItalyCopyright © 2022 Cascino, Marciello, D’Agostino, Toricco, Barone and Monteleone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giammarco Cascino, TWdjYXNjaW5vQHVuaXNhLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.