- 1Institute of Acupuncture and Moxibustion, China Academy of Chinese Medical Sciences, Beijing, China
- 2Psychiatry Department, The First Hospital of Hebei Medical University, Shijiazhuang, China
- 3Psychological Department, Guang'anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 4Data Centre of Traditional Chinese Medicine, China Academy of Chinese Medical Sciences, Beijing, China
- 5Psychiatry Department, Beijing Anding Hospital, Capital Medical University, Beijing, China
- 6The School of Chinese Medicine, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
Background: Depression accompanying chronic pain (CP) is one of the most common comorbid psychiatric disorders. This study aimed to investigate the effectiveness of transcutaneous auricular vagus nerve stimulation (taVNS) combined with electroacupuncture at Baihui (GV20) and Yintang (GV29) acupoints compared with citalopram.
Methods: Sixty patients with depression and pain comorbidity were enrolled in a prospective 8-week, single-blind, randomized controlled trial. Participants were randomly assigned to receive either taVNS combined with electroacupuncture treatment (taVNS: 8 weeks, 3 sessions per week; electroacupuncture: 8 weeks, twice per day, no drugs) or citalopram treatment (8 weeks, 40 mg/day). The primary outcome was Montgomery–Åsberg Depression Rating Scale (MADRS). The secondary endpoints were evaluated using the McGill Pain Questionnaire (SF-MPQ), self-reported 36-Item Short Form Survey (SF-36), Pittsburgh Sleep Quality Index (PSQI), Hamilton Depression Rating Scale (HAMD) and Hamilton Anxiety Scale (HAMA).
Results: Both the taVNS combined with electroacupuncture and citalopram groups had significant reductions in depressive and pain symptoms, as indicated by the decrease in MARDS and SF-MPQ scores. Regarding the analgesic effect, the pain intensity score of the SF-MPQ showed a larger reduction with citalopram than with taVNS combined with electroacupuncture at 6 weeks (P = 0.036). The reduction in the BP score of the SF-36 was higher at week 4 (P = 0.000), with no significant difference observed at week 8 (P = 0.1110). This result indicated that the pain intensity can be improved rapidly with citalopram compared with taVNS combined with electroacupuncture. Similarly, the comparison of PSQI scores at 4, 6, and 8 weeks indicates that there was no significant difference between groups, except in the use of sleeping medications. At week 6, higher medication use was found in the citalopram group than in the taVNS combined with electroacupuncture group (P = 0.049).
Conclusion: In summary, compared with citalopram, taVNS combined with electroacupuncture produces similar positive effects on depressive and pain symptoms in patients with depression and chronic pain, which last for at least 8 weeks.
Introduction
Chronic pain (CP) is a highly prevalent and disabling illness that is costly and poses a substantial burden on patients, their significant others, and society. The prevalence of CP in the United States was reported to be 30.7%, meaning that approximately 1 in 3 Americans lives with CP (1). CP has high comorbidity with depression, with a mean prevalence rate of comorbid major depressive disorder (MDD) in patients with CP ranging from 18% in population-based settings up to 85% in specialized pain clinics (2). In patients with depression, the prevalence of pain ranges from 15 to 100% (mean prevalence, 65%) (3). Although it is generally understood that pain and depression are common comorbidities and that their combination is costlier and more disabling than either condition alone, their interaction is not fully understood. Pain and depression share potential genetic factors (4). Genes and stress interact to alter neuronal size and function in depression. Neurotransmitters such as glutamate, substance P, serotonin, norepinephrine, dopamine, BDNF, and gamma-aminobutyric acid are activated in CP (5). These same neurotransmitters, especially serotonin and norepinephrine, have long been considered key to understanding depression (6).
CP and concomitant depression is common and can recur easily, but prolonged medication use carries risks of addiction, tolerance and obvious toxic side effects (7–10). Transcutaneous auricular vagus nerve stimulation (taVNS) is a non-invasive electrical stimulation method that overcomes potential barriers to the use of vagus nerve stimulation (VNS) by stimulating the afferent fibers of the vagus nerve in the ear to produce an effect similar to classical VNS in reducing depressive symptoms (11). Acupuncture has been recommended by the World Health Organization for the treatment of CP and has even been approved by the U.S. military and Veterans Administration (12). It has been proven that acupuncture and transcutaneous electric stimulation have a lasting analgesic effect (12–15). The underlying mechanism of its therapeutic effects is mainly through the periphery, spinal cord and spinal cord at the central level (16–18). Additionally, evidence-based medicine has verified that acupuncture has the advantages of being simple, safe and effective for anxiety and depressive mood disorders (19, 20), with the mechanism of relevance among neuroendocrine function, cell signal transduction, hippocampal neurogenesis and proinflammatory cytokines (17, 21). However, as a number of these studies lack methodological vigor, further appropriately designed clinical studies are recommended to verify their conclusions. Despite evidence suggesting that acupuncture has therapeutic benefits for patients with CP and comorbid depression, the relative benefits of acupuncture compared to commonly used antidepressants remain unknown. Citalopram, one of the first selective serotonin reuptake inhibitors (SSRIs) introduced to the market, is a widely used treatment for depression (16, 22, 23). The aim of this assessor-blinded, randomized clinical trial is to evaluate the effectiveness of taVNS combined with electroacupuncture treatment compared with citalopram for 8 weeks in patients with CP and mild to moderate comorbid depression. We hypothesize that taVNS combined with electroacupuncture will be superior to citalopram, as measured by the Montgomery–Åsberg Depression Rating Scale (MADRS), Simplify the McGill Pain Questionnaire (SF-MPQ), self-reported 36-Item Short Form Survey (SF-36), Pittsburgh Sleep Quality Index (PSQI), Hamilton Depression Rating Scale (HAMD) and Hamilton Anxiety Scale (HAMA).
Methods
Patient selection
The multicentre study recruited patients from The First Hospital of Hebei Medical University, Guang'anmen Hospital of CACMS, and Beijing Anding Hospital of Capital Medical University via advertisements, posters, flyers or physician referrals. Patients were enrolled from the outpatient departments of the three hospitals above from May 12, 2018, to April 15, 2019.
The inclusion criteria were as follows: (1) patients with at least one psychogenic pain event and a visual analog scale (VAS) score of 3 or more; (2) patients meeting the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnostic standard [Depressive symptoms typically last at least 2 weeks; Changes in appetite and weight, sleep disorders, and psychomotor agitation or hysteresis; Lack of energy; Feelings of worthlessness or guilt; Difficulty thinking, concentrating, or making decisions (23, 24)]; (3) patients aged 18 to 50 years old; patients with first-onset depression; (4]) patients with mild-to-moderate depression who scored 12–30 points on the MADRS; (5)volunteer participants who were willing to cooperate and adhere to the treatment.
The exclusion criteria were as follows: (1) pregnant women. (2) patients with serious suicidal thoughts or suicidal behavior. (3) patients with other severe organic diseases, such as malignant tumors and liver failure. (4) patients with an ongoing addiction to drugs and alcohol. (5) patients with a history of schizophrenia or other mental disorders. (6) patients with cognitive impairment or personality disorders. After passing a pre-screening performed by study physicians in accordance with the inclusion and exclusion criteria, potentially eligible patients provided informed consent to participate in the presence of a study physician.
Study design
A randomized, 8-week, assessor-blind controlled clinical trial was developed, consisting of taVNS combined with electroacupuncture and citalopram groups. The protocol was approved by the Institutional Ethics Committee of the China Academy of Chinese Medical Sciences (CACMS) (2017-07-31-2). All participants were informed about the study and had to provide written informed consent. This study has been registered at Clinicaltrials.gov (NCT03282110).
Randomization
The population comprised 60 patients diagnosed with CP and comorbid depression. Eligible patients were randomly assigned in a 1:1 ratio to the taVNS combined with electroacupuncture or citalopram group via a central randomization system. The randomization sequence was generated in blocks of varying size and stratified by the center. The definition of the block size and the factor were 4 and center, respectively, used in stratification. Information on each participant's group allocation was sealed in opaque envelopes by an independent researcher who was not involved in outcome assessments at each clinical site.
Sample size calculation
According to the formula, (1-p)/ (p1-p2)2 (25), α = 0.05, β = 0.1, k = 1, p1 = 0.50, p2 = 0.10, p = 0.3. p = (p1+kp2)/ (1+k)=0.3. The sample size is Calculated as follows: n = (1.64+1.28)2× 2 × 0.3 × (1–0.3)/[(0.5–0.1)2], N is 22.38, or about 23 cases, that is, the sample size of a single group is 23 cases, so a total of 46 cases are required for this experiment. Take into account the rate of loss. The total of cases is 60.
Outcomes
The primary outcome was evaluated with the MADRS (26), which has been validated and used in clinical studies including people with and without pain. Lower scores of MADRS indicated the better mental state. The effective rate was defined as the number of participants with a 50% or greater reduction from baseline in the MADRS at weeks 4 and 8. The secondary outcomes were evaluated with SF-MPQ (27), which is widely used to assess the pain condition, the lower the scores of SF-MPQ, the better the mental state of the patients. Other secondary endpoints were evaluated with SF-36 (28) [including Physical Functioning (PF), Role-Physical (RP), Bodily Pain (BP), General Health (GH), Vitality (VT), Social Functioning (SF), Role-Emotional (RE), Mental Health (MH) and Health Transition (HT)], PSQI, HAMD and HAMA. The higher the SF-36 score, the better the health, the lower the scores of PSQI, HAMD and HAMA, the better the mental state of the patients. All endpoints were measured at weeks 0, 4, and 8 by trained interviewers who were blinded to treatment information.
Interventions
taVNS combined with electroacupuncture group
taVNS
Patients took a seated position or laid on their sides. After skin disinfection, electrodes were attached to the auricular concha to be stimulated (Hwato brand SDZ-IIB electronic stimulator, Suzhou Medical Application Factory, Suzhou, China), which is similar to our previous clinical studies. The stimulation parameters included the following: 1) a dilatational wave of 4/20 Hz was used (4 Hz for 5 s, 20 Hz for 10 s, the sparse and dense wave alternated). 2) the intensity of stimulation adjusted individually based on the tolerance of the patient. 3) each treatment lasted for 30 min, 2 times per day (once in the morning, the other in the evening), for 5 consecutive days from Monday to Friday per week for 8 weeks. After group randomization, taVNS group patients were trained on how to use the taVNS device so that it could be self-administered at home. The stimulated region is located at the auricular conch, where there is a rich vagus nerve branch distribution.
Electroacupuncture
The electroacupuncture acupoints were Baihui (GV20) and Yintang (GV29), which are located in the parietal and frontal skin that distributes the supraorbital nerve of the trigeminal nerve (Figure 1). Electroacupuncture was conducted for 3 sessions, Monday to Friday every other day, per week over 8 consecutive weeks. Disposable acupuncture needles (0.30 mm in diameter and 25–40 mm in length) were inserted obliquely at a depth of 10–30 mm into the two acupoints, through which electrical stimulation with continuous waves with 2 Hz at 9 volts was delivered with an electrical acupuncture simulation instrument (Hwarto, SMY-10A). The use of a low frequency rather than high frequency was adopted because it could induce biochemical changes in the brain in a more favorable manner for alleviating depressive symptoms. The intensities of stimulation were adjusted to a level at which subjects felt most comfortable. Each simulation lasted 30 min, with 3 sessions per week over 8 consecutive weeks.
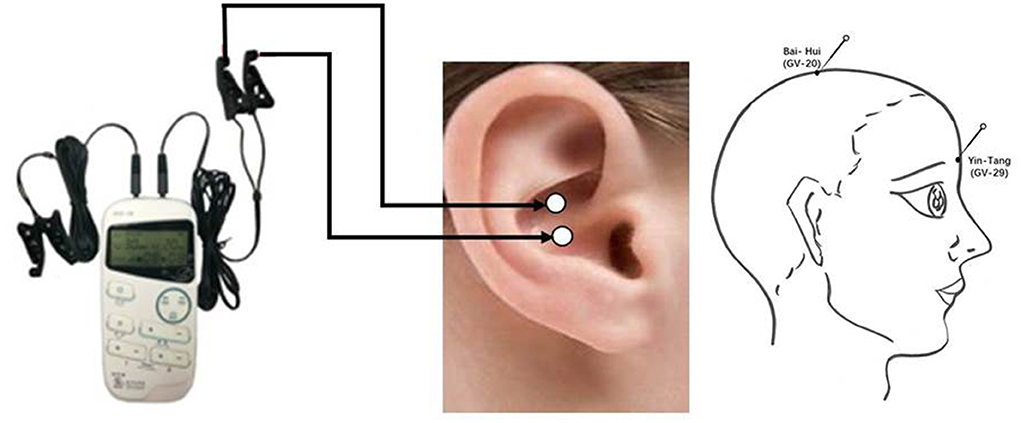
Figure 1. Location of acupuncture and taVNS. taVNS, transcutaneous auricular vagus nerve stimulation.
Citalopram group
Patients in the citalopram group received oral citalopram. Citalopram was provided at an initial dose of 10 mg daily for 3 days, followed by 20 mg daily for 4 days. A daily dose of 40 mg of citalopram, which was taken for 7 weeks, was provided after 1 week. At the end of the study (8 weeks), most of the patients in the citalopram group continued treatment under the guidance of the study physicians.
Statistical analysis
A descriptive analysis was used, with continuous variables expressed as the mean ± sd and categorical variables expressed as frequencies and percentages. We used t-test for continuous outcomes and Chi-square test or Fisher's exact test for binary outcomes to compare the differences between the groups. The changes from baseline of the primary outcome were analyzed by fitting linear mixed-effects models with repeated measures analysis using the baseline as a covariate, treatment, visit, and their interaction as fixed effects, the intercept as the random effect. The same analysis was used for other longitudinal continuous variables. Besides, effect size was showed by calculating the Cohen's d value, and >0.8 was considered large effect. All statistical analyses were performed using SAS version 9.4 (SAS Institute) or R version 4.1.2. P < 0.05 indicated a statistically significant difference.
Results
Participants and baseline characteristics
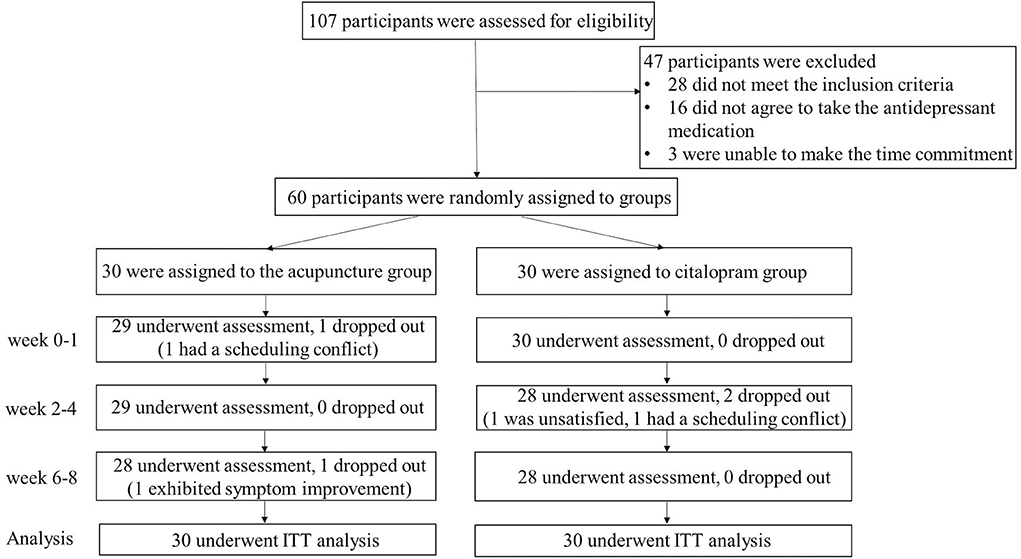
Initially, of the 107 patients screened, 60 participants were enrolled and randomly divided into two groups (30 in the taVNS combined with electroacupuncture group and 30 in the citalopram group). Some patients were excluded from the study for the following reasons: reluctance to be assigned randomly to a treatment group, refusal of antidepressant medication, and inability to be assessed every 2 weeks. At week eight (end of treatment), 28 subjects in the taVNS combined with electroacupuncture group and 28 subjects in the citalopram group had completed the study. Specifically, two patients dropped out of the taVNS combined with electroacupuncture group (one due to scheduling conflicts at week one and one due to significant improvement at week eight); two patients dropped out of the citalopram group (one due to the lack of a satisfactory effect and one due to scheduling conflicts) (Figure 2).
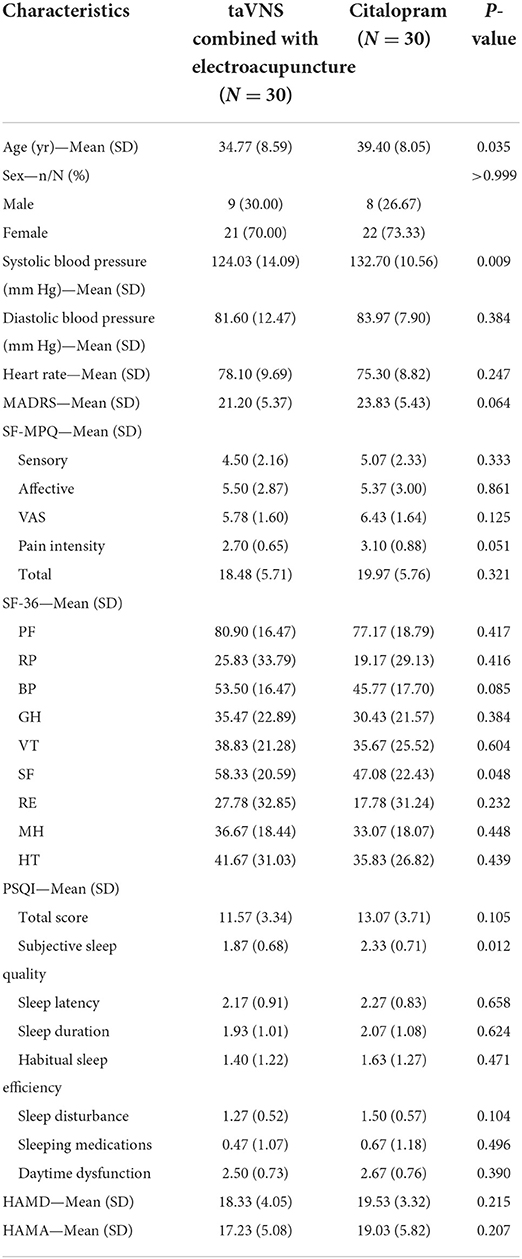
The baseline characteristics were comparable between the two groups (Table 1), except for systolic blood pressure, which was lower in the taVNS combined with electroacupuncture group. The study population suffered from a wide variety of pain conditions, including chronic back pain, migraines, neuropathic pain, osteoarthritis and fibromyalgia.
Comparison between taVNS combined with electroacupuncture and citalopram on primary and secondary outcome measurements
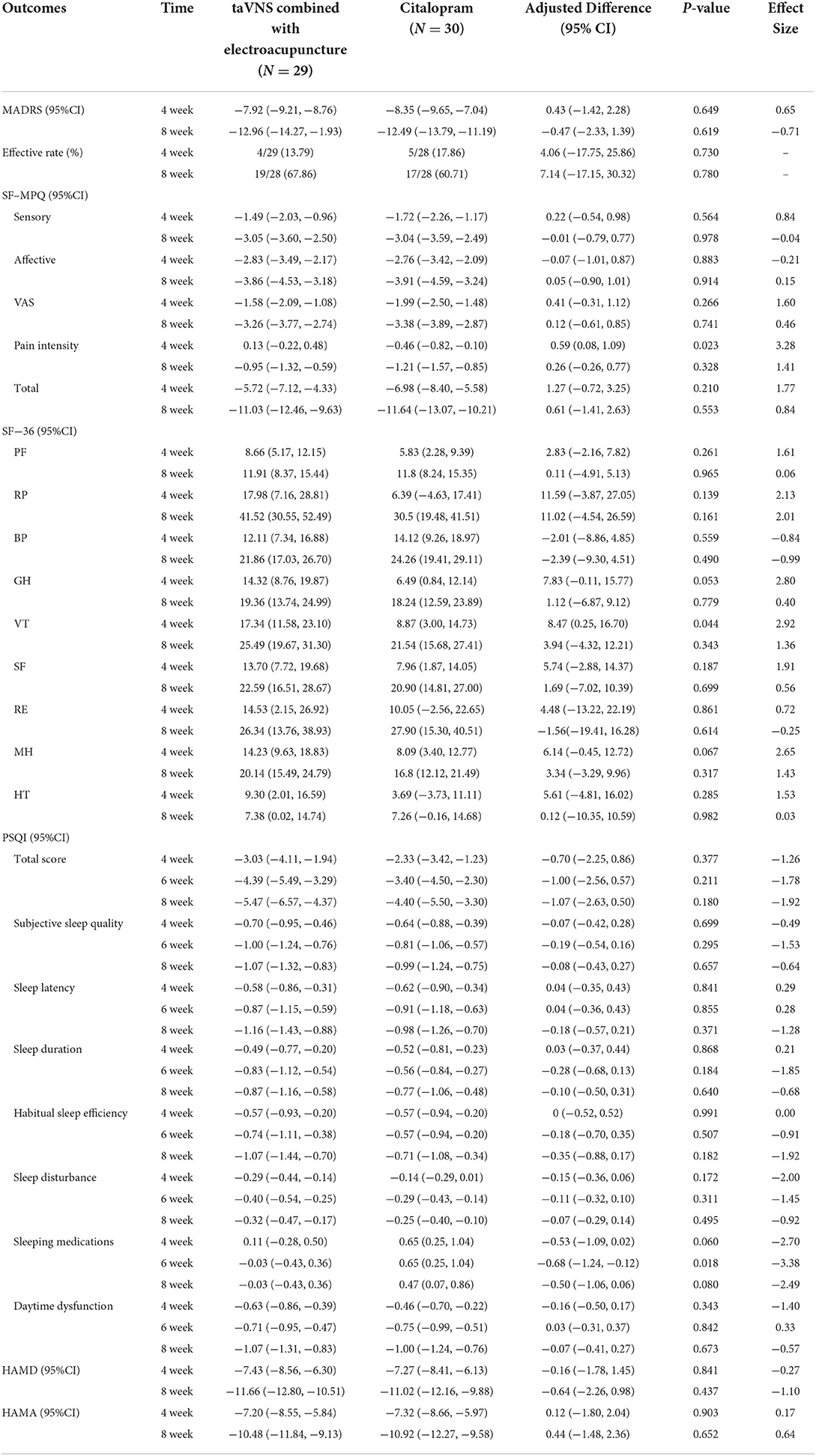
The adjusted scores for the MARDS, SF-MPQ, SF-36, PSQI, HAMD and HAMA at different time points are illustrated in Table 2. Between group differences in the effective rate were −4.06% (95%CI: −17.75%, 25.86%) and 7.14% (95%CI: −17.15%, 30.30%, each P > 0.05) at weeks 4 and 8. Both the taVNS combined with electroacupuncture and citalopram groups showed reductions in depressive and pain symptoms, as indicated by the decrease in MARDS and SF-MPQ scores at week 8. We found that during the 8-week treatment, the antidepressant effect of taVNS combined with electroacupuncture remained similar to that of citalopram in terms of the MADRS, HAMD and HAMA scores, with differences between groups of −0.47 (95%CI: −2.33, 1.39), −0.64 (95%CI: −2.26, 0.98) and 0.44 (95%CI: −1.48, 2.36), respectively (P > 0.05).
To explore the effects of the two different treatments on the quality of life, we measured the SF-36 score with 9 items, including PF, RP, BP, GH, VT, SF, RE, MH and HT, at weeks 4 and 8. No significant difference (P > 0.05) was found in terms of changes to the SF-36 score at any assessment time point (Table 2).
Similarly, the comparison of PSQI scores at 4, 6, and 8 weeks indicates that there was no significant difference between the two groups, except in the use of sleeping medications. At week 6, higher medication use was found in the citalopram group [adjusted score and 95% CI: 0.65 (0.25, 1.04)] than in the taVNS combined with electroacupuncture group [adjusted score and 95% CI: −0.03 (−0.43, 0.36), P = 0.018].
Safety and compliance
Based on the patients' treatment journals and verbal reports, the main side effect of acupuncture was sharp pain during stimulation (one subject). For citalopram, side effects included digestive problems such as nausea, sour regurgitation (two subjects), early wake-up, drowsiness (one subject) and dry eyes (one subject).
Discussion
For nearly a century, the relevant theory and application research of the ear has greatly promoted the development of auricular acupoint therapy in traditional Chinese medicine, and finally proposed the concept of taVNS. taVNS can transmit signals to the solitary tract nucleus by activating the vagal afferent fiber, and then regulate the body function, and taVNS has been widely used in the clinical treatment of epilepsy, depression, consciousness disorders and other neurological diseases (29). Our randomized controlled trial with 107 depression patients failed to show a significant advantage of taVNS over citalopram (30). Therefore, we expect to involve additional invasive intervention to enhance the effectiveness of taVNS in the treatment of depression combined with CP.
Acupuncture on GV20 and GV29, those forehead acupoints are found innervated by the trigeminal nerve, while the stimulation process activates the sensory pathways of the trigeminal nerve (24). This study found that taVNS combined with electroacupuncture treatment results in symptom improvement, reflected in the MADRS, SF-MPQ, SF-36, PSQI, HAMD and HAMA scores, and that this improvement is similar to that of citalopram, a commonly prescribed anti-depressant for patients with pain and comorbid mild to moderate depression. This result is consistent with the findings of several meta-analyses assessing the effectiveness of acupuncture monotherapy in comparison with antidepressants (31, 32). Although we found that participants in the taVNS combined with electroacupuncture group showed a lower analgesic benefit at week four compared with the citalopram group, no significant difference was found at week eight, indicating that citalopram may have a faster analgesic effect than acupuncture. taVNS combined with electroacupuncture has a certain protective effect on the maintenance of patients' energy, suggesting that this method is safer than citalopram group. No serious adverse events related to the interventions were reported. Our results demonstrated the potential of taVNS and electroacupuncture for the simultaneous treatment of mild and moderate MDD with CP comorbidity.
Regarding clinical research, effectiveness of taVNS and electroacupuncture on Baihui (GV20) and Yintang (GV29) in relieving depressive and pain symptoms has been implied by previous studies. Hein and colleagues (33) found that 2 weeks of taVNS treatment could significantly reduce Becker Depression Index scores when compared to the sham condition. Nevertheless, there was no significant difference in the HAMD scores. In a subsequent non-randomized clinical study (11), we found that after the fourth week, the taVNS group had greater decreases in the 24-item HAMD score. The clinical improvements continued until week 12. In another recent study (34), Trevizol and colleagues found that the 17-item HAMD scores were significantly reduced after 2 weeks of taVNS treatment in a single-arm study. Liu CY and colleagues (35) found that patients in the acupuncture (GV20 and GV29) group showed a lower HAMD score compared with the sham acupuncture group. Acupuncture has been increasingly used as an integrative or complementary therapy for chronic pain, which is well tolerated with little risk of serious adverse effects (36, 37). In an open randomized trial, transcutaneous electrical nerve stimulation, infrared laser therapy and acupuncture on GV20 combined with other acupoints were proven to be effective in reducing the frequency of headache attacks (38). Liu CZ and colleagues carried out a multicentre randomized sham-controlled trial of patients with knee osteoarthritis and found that compared to SA, intensive acupuncture resulted in less pain and better function at week 8, and these effects persisted until week 26 (39, 40). Acupuncture is well tolerated with little risk of serious adverse effects on pain syndromes (36).
Peijing Rong and colleagues used CUMS rats and chronic constriction injury (CCI) of the sciatic nerve to generate a depression and chronic somatic pain comorbidity model. The results showed that electroacupuncture and taVNS have antidepressant and analgesic effects (20). The results of this trial are consistent with the findings reported in the abovementioned studies, demonstrating the benefit of taVNS and electroacupuncture in relieving symptoms of MDD and CP.
Citalopram is a second-generation antidepressant that has been approved by regulatory agencies and shows good acceptability (41). Studies have found that it is more efficacious than placebo in adults with MDD. It has been reported that citalopram is also used as an antidepressant for chronic non-cancer pain in children and adolescents. We found that the therapeutic effects from taVNS and electroacupuncture were similar to those from citalopram in patients with MDD and CP. In addition, participants in the taVNS combined with electroacupuncture group showed a lower analgesic benefit at week six than those in the citalopram group. This finding also suggests that citalopram may have a faster analgesic effect than taVNS and electroacupuncture. Future studies are needed to validate this finding.
We did not detect serious side effects for taVNS based on the patients' treatment journals and verbal reports. One subject reported sharp pain during stimulation, which may be due to hypersensitivity of the stimulation area. For citalopram, the side effects reported include digestive problems such as nausea, sour regurgitation, waking up early, drowsiness, and dry eyes. This result is consistent with the literature on the side effects of citalopram (41).
It is the first time to investigate the effectiveness of combination therapy on depression with CP. There are still several limitations of this small sample exploratory study that should be noted. First, this study was assessor-blinded; the participants could not be blinded due the nature of the treatment. Second, taVNS combined with electroacupuncture was administered for 8 weeks. Thus, our results only demonstrate the similarity between the effects of taVNS combined with electroacupuncture and those of citalopram over 2 months. Third, we included only patients with mild to moderate depression and comorbid CP. We are not sure if the effects of taVNS combined with electroacupuncture and citalopram are similar for patients with severe depression or other symptoms. We also did not exclude patients based on prior treatment; thus, patients included in this study may have some heterogeneity. In addition, some of the patients may have had residual symptoms of a more severe episode (refractory), and some could have had a persistent depressive disorder. We are not sure if the effects of taVNS combined with electroacupuncture and citalopram are similar for treatment-resistant depression, which is the target population of classic VNS. Finally, taVNS and citalopram were administered by the patients themselves, so we cannot be completely sure that all patients precisely followed the experimental protocol. Nevertheless, the self-administration of taVNS provides direct evidence of the feasibility of the widespread application of this method, which could significantly reduce treatment expenses.
Conclusion
In summary, we found that compared to citalopram, a commonly prescribed anti-depression agent, taVNS combined with electroacupuncture produces similar effects in relieving depressive and pain symptoms in patients with MDD and CP for at least 8 weeks. Therefore, this safe and low-cost peripheral neuromodulation approach may be considered a therapeutic option for the multidisciplinary management of patients with depression and comorbid CP.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Ethics Committee of the China Academy of Chinese Medical Sciences (CACMS) (2017-07-31-2). The patients/participants provided their written informed consent to participate in this study.
Author contributions
SL: conceptualization, project administration, formal analysis, writing—original draft, writing—review and editing, and funding acquisition. ZiZ: project administration, data section, writing—original draft, and writing—review and editing. YJ: data section and methodology. GJ, YW, HJ, and FX: data section. YZ: methodology and formal analysis. ZQ and ZhZ: methodology and writing—review and editing. PR: funding acquisition, conceptualization, project administration, supervision, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
The work was supported by Young Elite Scientists Sponsorship Program by CAST (2021-2023ZGZJXH-QNRC001), National Natural Science Foundation of China (82004181), Excellent Youth Fund of Chinese Academy of Chinese Medicine (ZZ15-YQ-048), and International Cooperation Project of Traditional Chinese Medicine in CACMS (GH2017-07).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer LH declared a shared affiliation with the authors ZQ and ZhZ to the handling editor at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BP, Bodily Pain; CACMS, China Academy of Chinese Medical Sciences; CP, Chronic pain; GH, General Health; HAMD, Hamilton Depression Rating Scale; HT, Health Transition; HAMA, Hamilton Anxiety Scale; MH, Mental Health; MADRS, Montgomery–Åsberg Depression Rating Scale; MDD, major depressive disorder; PF, Physical Functioning; PSQI, Pittsburgh Sleep Quality Index; RE, Role-Emotional; RP, Role-Physical; S, Social Functioning; SF-36, self-reported 36-Item Short Form Survey; SF-MPQ, self-reported McGill Pain Questionnaire; taVNS, transcutaneous auricular vagus nerve stimulation; VAS, visual analog scale; VT, Vitality.
References
1. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH, et al The prevalence of chronic pain in United States adults: resul.ts of an Internet-based survey. J Pain. (2010) 11:1230–39. doi: 10.1016/j.jpain.2010.07.002
2. Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. (2003) 163:2433–45. doi: 10.1001/archinte.163.20.2433
3. Gambassi G. Pain and depression: the egg and the chicken story revisited. Arch Gerontol Geriatr. (2009) 49 (Suppl. 1):103–12. doi: 10.1016/j.archger.2009.09.018
4. Diatchenko L, Slade GD, Nackley AG, Bhalang K, Sigurdsson A, Belfer I, et al Genetic basis for individual variations in pain perception and the development of a chronic pain condition. Hum Mol Genet. (2005) 14:135–43. doi: 10.1093/hmg/ddi013
5. Jones AK, Kulkarni B, Derbyshire SW. Pain mechanisms and their disorders. Br Med Bull. (2003) 65:83–93. doi: 10.1093/bmb/65.1.83
6. Price JB, Bronars C, Erhardt S, Cullen KR, Schwieler L, Berk M, et al Bioenergetics and synaptic plasticity as potential targets for individualizing treatment for depression. Neurosci Biobehav Rev. (2018) 90:212–20. doi: 10.1016/j.neubiorev.2018.04.002
7. Braden JB, Sullivan MD, Ray GT, Saunders K, Merrill J, Silverberg MJ, et al Trends in long-term opioid therapy for non-cancer pain among persons with a history of depression. Gen Hosp Psychiatry. (2009) 31:564–70. doi: 10.1016/j.genhosppsych.2009.07.003
8. Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Green CE, Perez AM, et al Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. (2013) 170:1134–42. doi: 10.1176/appi.ajp.2013.13030392
9. Ehrich E, Turncliff R, Du Y, Leigh-Pemberton R, Fernandez E, Jones R, et al Evaluation of opioid modulation in major depressive disorder. Neuropsychopharmacology. (2015) 40:1448–55. doi: 10.1038/npp.2014.330
10. Fan AY, Miller DW, Bolash B, Bauer M, McDonald J, Faggert S, et al Acupuncture's role in solving the opioid epidemic: evidence cost-effectiveness and care availability for acupuncture as a primary non-pharmacologic method for pain relief and management-white paper. J Integr Med. (2017) 15:411–25. doi: 10.1016/S2095-4964(17)60378-9
11. Rong PJ, Liu J, Wang L, Liu R, Fang J, Zhao J, et al Effect of transcutaneous auricular vagus nerve stimulation on major depressive disorder: a nonrandomized controlled pilot study. J Affect Disord. (2016) 195:172–9. doi: 10.1016/j.jad.2016.02.031
12. Platon B, Andréll P, Raner C, Rudolph M, Dvoretsky A, Mannheimer C, et al High-frequency high-intensity high-intensity transcutaneous electrical nerve stimulation as treatment of pain after surgical abortion. Pain. (2010) 148:114–9. doi: 10.1016/j.pain.2009.10.023
13. King T, Qu C, Okun A, Melemedjian OK, Mandell EK, Maskaykina IY, et al Contribution of PKMζ-dependent and independent amplification to components of experimental neuropathic pain. Pain. (2012) 153:1263–73. doi: 10.1016/j.pain.2012.03.006
14. Coutaux A. Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine. (2017) 84:657–61. doi: 10.1016/j.jbspin.2017.02.005
15. Zhang XY, Liu Y, Zhang WJ, Song XY, Yang YY. Analysis and reflection of characteristics of evidence review by CMS on acupuncture treatment for chronic low back pain. World J Acupuncture-Moxibustion. (2021) 31:59–64. doi: 10.1016/j.wjam.2020.11.011
16. Ulett GA, Han S, Han JS. Electroacupuncture: mechanisms and clinical application. Biol Psychiatry. (1998) 44:129–38. doi: 10.1016/S0006-3223(97)00394-6
17. Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. (2003) 26:17–22. doi: 10.1016/S0166-2236(02)00006-1
18. Armour M, Smith CA, Wang LQ, Naidoo D, Yang GY, MacPherson H, et al Acupuncture for depression: a systematic review and meta-analysis. J Clin Med. (2019) 8:1140. doi: 10.3390/jcm8081140
19. Smith CA, Armour M, Lee MS, Wang LQ, Hay PJ. Acupuncture for depression. Cochrane Database Syst Rev. (2018) 3:Cd004046. doi: 10.1002/14651858.CD004046.pub4
20. Guo X, Zhao Y, Huang F, Li S, Luo M, Wang Y, et al Effects of transcutaneous auricular vagus nerve stimulation on peripheral and central tumor necrosis factor alpha in rats with depression-chronic somatic pain comorbidity. Neural Plast. (2020) 2020:8885729. doi: 10.1155/2020/8885729
21. Chen XY, Zhang GB. Progress and prospects of acupuncture research on the mechanism of post-stroke depression. World J Acupuncture-Moxibustion. (2020) 30:285–87. doi: 10.1016/j.wjam.2020.09.003
22. Lavretsky H, Reinlieb M, St Cyr N, Siddarth P, Ercoli LM, Senturk D, et al Citalopram methylphenidate or their combination in geriatric depression: a randomized double-blind placebo-controlled trial. Am J Psychiatry. (2015) 172:561–9. doi: 10.1176/appi.ajp.2014.14070889
23. Kim JS, Lee EJ, Chang DI, Park JH, Ahn SH, Cha JK, et al Efficacy of early administration of escitalopram on depressive and emotional symptoms and neurological dysfunction after stroke: a multicentre double-blind randomised placebo-controlled study. Lancet Psychiatry. (2017) 4:33–41. doi: 10.1016/S2215-0366(16)30417-5
24. Zhang ZJ, Chen HY, Yip KC, Ng R, Wong VT. The effectiveness and safety of acupuncture therapy in depressive disorders: systematic review and meta-analysis. J Affect Disord. (2010) 124:9–21. doi: 10.1016/j.jad.2009.07.005
25. Wang JL, Wang BY. Clinical Epidemiology. 3d edition. Beijing: People's Medical Publishing house Co, LTD. (2008).
26. Paketci S. Interpretation of the Montgomery-Åsberg Depression Rating Scale (MADRS). BJPsych. (2021) 219:620–1. doi: 10.1192/bjp.2021.162
27. Melzack R. The short-form McGill pain questionnaire. Pain. (1987) 30:191–7. doi: 10.1016/0304-3959(87)91074-8
28. Page AC, Hooke GR, Rutherford EM. Measuring mental health outcomes in a private psychiatric clinic: health of the nation outcome scales and medical outcomes short Form SF-36. Aust N Z J Psychiatry. (2001) 35:377–81. doi: 10.1046/j.1440-1614.2001.00908.x
29. Wang Y, Li SY, Wang D, Wu MZ, He JK, Zhang JL, et al Transcutaneous auricular vagus nerve stimulation: from concept to application. Neurosci Bull Jun. (2021) 37:853–62. doi: 10.1007/s12264-020-00619-y
30. Li S, Rong P, Wang Y, Jin G, Hou X, Li S, et al Comparative effectiveness of transcutaneous auricular vagus nerve stimulation versus citalopram for major depressive disorder: a randomized trial. Neuromodulation. (2022) 25:450–60. doi: 10.1016/j.neurom.2021.10.021
31. Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, et al Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. (2018) 75:336–46. doi: 10.1001/jamapsychiatry.2017.4602
32. Usichenko TI, Hua K, Cummings M, Nowak A, Hahnenkamp K, Brinkhaus B, et al Auricular stimulation for preoperative anxiety - a systematic review and meta-analysis of randomized controlled clinical trials. J Clin Anesth. (2022) 76:110581. doi: 10.1016/j.jclinane.2021.110581
33. Hein E, Nowak M, Kiess O, Biermann T, Bayerlein K, Kornhuber J, etale Auricular transcutaneous electrical nerve stimulation in depressed patients: a randomized controlled pilot study. J Neural Transm (Vienna). (2013) 120:821–7. doi: 10.1007/s00702-012-0908-6
34. Trevizol AP, Shiozawa P, Taiar I, Soares A, Gomes JS, Barros MD, et al Transcutaneous vagus nerve stimulation (taVNS) for major depressive disorder: an open label proof-of-concept trial. Brain Stimul. (2016) 9:453–4. doi: 10.1016/j.brs.2016.02.001
35. Liu C, Zhao Y, Qin S, Wang X, Jiang Y, Wu W, et al Randomized controlled trial of acupuncture for anxiety and depression in patients with chronic insomnia. Ann Transl Med. (2021) 9:1426. doi: 10.21037/atm-21-3845
36. Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, et al Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
38. Allais G, De Lorenzo C, Quirico PE, Lupi G, Airola G, Mana O, et al Non-pharmacological approaches to chronic headaches: transcutaneous electrical nerve stimulation lasertherapy and acupuncture in transformed migraine treatment. Neurol Sci. (2003) 24 (Suppl. 2):S138–142. doi: 10.1007/s100720300062
39. Lin LL, Tu JF, Wang LQ, Yang JW, Shi GX, Li JL, et al Acupuncture of different treatment frequencies in knee osteoarthritis: a pilot randomised controlled trial. Pain. (2020) 161:2532–8. doi: 10.1097/j.pain.0000000000001940
40. Tu JF, Yang JW, Shi GX, Yu ZS, Li JL, Lin LL, et al Efficacy of intensive acupuncture versus sham acupuncture in knee osteoarthritis: a randomized controlled trial. Arthritis Rheumatol. (2021) 73:448–58. doi: 10.1002/art.41584
41. Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. (2018) 391:1357–66. doi: 10.1016/S0140-6736(17)32802-7
Keywords: taVNS, acupuncture, depression, chronic pain, randomized clinical trial
Citation: Li S, Zhang Z, Jiao Y, Jin G, Wu Y, Xu F, Zhao Y, Jia H, Qin Z, Zhang Z and Rong P (2022) An assessor-blinded, randomized comparative trial of transcutaneous auricular vagus nerve stimulation (taVNS) combined with cranial electroacupuncture vs. citalopram for depression with chronic pain. Front. Psychiatry 13:902450. doi: 10.3389/fpsyt.2022.902450
Received: 23 March 2022; Accepted: 14 July 2022;
Published: 04 August 2022.
Edited by:
Kele Ding, Kent State University, United StatesReviewed by:
LM Ho, The University of Hong Kong, Hong Kong SAR, ChinaXuerui Wang, Capital Medical University, China
Copyright © 2022 Li, Zhang, Jiao, Jin, Wu, Xu, Zhao, Jia, Qin, Zhang and Rong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peijing Rong, ZHJyb25ncGomI3gwMDA0MDsxNjMuY29t; cm9uZ3BqJiN4MDAwNDA7Y2FjbXMuY24=
 Shaoyuan Li
Shaoyuan Li Zixuan Zhang
Zixuan Zhang Yue Jiao1
Yue Jiao1 Fengquan Xu
Fengquan Xu Zongshi Qin
Zongshi Qin Zhangjin Zhang
Zhangjin Zhang Peijing Rong
Peijing Rong