
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 29 August 2022
Sec. Mood Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.900277
Introduction: Emotional dysregulation (ED) is characterized by inappropriate emotional reactions related to environmental or cognitive stimuli. In most recent years, increasing interest has been devoted to its definition and detection across mental disorders for its detrimental role progressively highlighted in both neurodevelopment and adult mental disorders, with implications on the severity of clinical manifestations. The aim of this systematic review was to evaluate and gather the scientific evidence about ED in adult psychiatric population to elucidate the concept of ED as trans-nosographic entity.
Methods: The electronics databases PubMed, Scopus and Web of Science was reviewed to identify studies in accordance with the PRISMA guidelines; at the end of the selection process a total of 29 studies (N = 709; N = 658; N = 1,425) was included. All studies included assessed the presence of ED symptoms, by means of a validate scale in adult (>18 years of age), in clinically diagnosed patients as well as healthy control participants.
Results: Our results suggest ED as a trans-diagnostic factor across multiple mental disorders, such as bipolar disorder, attention deficit hyperactivity disorder, autism spectrum disorder, personality disorders; a better definition of this concept could be helpful to interpret and clarify many clinical cases and improve their diagnostic and therapeutic management.
Over most recent years, the concept of Emotional Dysregulation (ED) has received increasing interest in psychiatry being generally used to describe altered regulation of emotional states both in children, adolescents, and adults. Today, despite scientific research has been increasingly focused on the study of ED its description is still debated.
Emotions are temporary qualitative states associated with sub-cortical (1), limbic (2), and cortico-frontal (3) processing in response to internal or external stimuli, that are defined as salient for each individual, capable of influencing physiological, somatic and behavioral responses by a cyclic mechanism of continuous feedback and progressive structural remodeling (4, 5). Despite the importance of “emotional problems” in clinical conditions has conducted to an intense search for causes, in which ED occupied a prominent place (6, 7), a shared definition of ED is still not yet available. In 1991, Thompson provided a definition of the Emotion Regulation (ER) as “a set of processes by which any individual assesses, inhibits, maintains, or modifies the intensity, frequency or duration of emotional reactions in order to have the appropriate social behavior or to achieve goals” (8). The concept of ED was introduced only years later, and as of today, one of the most welcomed definitions comes from Bunford et al. (9) as “an individual's inability to exercise any or all aspects of the modulatory processes involved in emotion regulation, to such a degree that the inability results in the individual functioning meaningfully below his or her baseline.” According to Shaw et al. (10), ED is composed of three main alterations: the first, is an inappropriate and excessive emotional reaction compared to social norms, secondly uncontrolled and rapid shifts in emotions and lastly an abnormal allocation of attention to emotional stimuli. As the concept of ED, in the general scientific overview, tends to focus mainly on negative emotions, ED is frequently defined by low frustration tolerance, irritability, susceptibility to negative emotional experience and emotional lability (11); that is in line with the new clinical category of “disruptive mood dysregulation disorder” introduced in the DSM-5 (12), created to describe severe and persistent irritability in children, manifested by intense and prolonged outbursts of anger and angry mood. Further, ED includes the inability to recognize and accept emotions alongside lacks in the ability to adaptively choose effective strategies to manage arising emotions (13, 14) also associated with an increased risk for various forms of psychopathology (15).
The alteration of the processes of emotion regulation belongs to a dimension that is increasingly depicted as trans-nosographic and which entails the need for new studies (16). The large spreading of ED symptoms in different kind of disorders, strictly supports the dimension concept of mental disorders as the result of multiple element interactions, which do not always lead to the overt diagnosis as described by textbooks, but rather define a spectrum of behaviors from normal to pathologic conditions.
The emotional dimension was initially the focus of the research into understanding the cytoarchitectural and functional properties of subcortical structures (17, 18), and for the evaluation of the effects induced by pharmacologically active substances (19, 20). Only later the emotional dimension was reconsidered as a consequence and as an index of a psychopathological outfit, which can be used for diagnosis and clinical classification. Therefore, the dysregulated emotional dimension turns out to be a clinical element, the result of a behavioral manifestation in response to a psychopathological condition of various kinds (genetics and environmental), that may occur across different mental disorders.
ED has been recently highlighted to share features in various childhood mental disorders including Bipolar Spectrum Disorders, Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (21). Following the purpose of this paper, we will focus mainly on adulthood Bipolar Disorder (BD), ADHD, ASD and other mental disorders as psychopathological conditions presenting with an ED. Given these premises, our aim is to propose an objective examination of the studies based on scientific evidence that support the concept of ED as a trans-nosographic dimension in adults (22).
A systematic search was conducted from 1 May to 3 October 2021 in accordance with the PRISMA 2020 guidelines (23) and using the electronic databases PubMed, Scopus and Web of Science. The following search terms, without filters, restriction or limits, were used to identify all potentially eligible records: (“emotional dysregulation” OR “affective dysregulation” OR “emotion dysregulation”) AND (“neurodevelopmental disorders” OR “autism” OR “ASD” OR “autism spectrum disorder” OR “attention deficit hyperactivity disorder” OR “ADHD” OR “schizophrenia spectrum disorders” OR “schizophrenia” OR “bipolar disorder” OR “post-traumatic stress” OR “post-traumatic stress disorder” OR “PTSD” OR “borderline personality disorder” OR “personality disorders”). All studies from 1st January 1976 to 3rd October 2021 were included in the databases search.
The criteria used to include studies in this review were as follows:
• Human studies.
• Studies that included only individuals of ages > 18.
• Study that used a validated scale to evaluate the ED.
• Articles available in English.
Because we aimed at investigating the ED in human subject, studies investigating ED in animal models, were excluded. Furthermore, studies in the form of review, case reports and editorials were also excluded.
Three independent reviewers (L.C., D.G., B.N.) screened papers for inclusion and disagreements were resolved by discussion. The primary databases search produced a total of 2,792 records. After that, 2,119 articles were removed after titles because they were duplicates (N = 1,173) or not relevant (N = 946), and 638 were removed after abstract because not pertinent (N = 355), full text are not available or not in English (N = 53) or because they were other publication types (N = 230). After a full text reading other 6 articles were excluded because they didn't fit the eligibility criteria. Finally, a total of 29 articles were included in the present review. All three reviewers completed the process independently. We assessed the reference lists of selected papers for other eligible studies and any disagreement on included papers was resolved via discussion. The grade of agreement between the three authors was good. Decisions for inclusion or exclusion are summarized in a flowchart according to PRISMA 2020 recommendations (23). The study selection process is outlined in a flowchart (Figure 1).
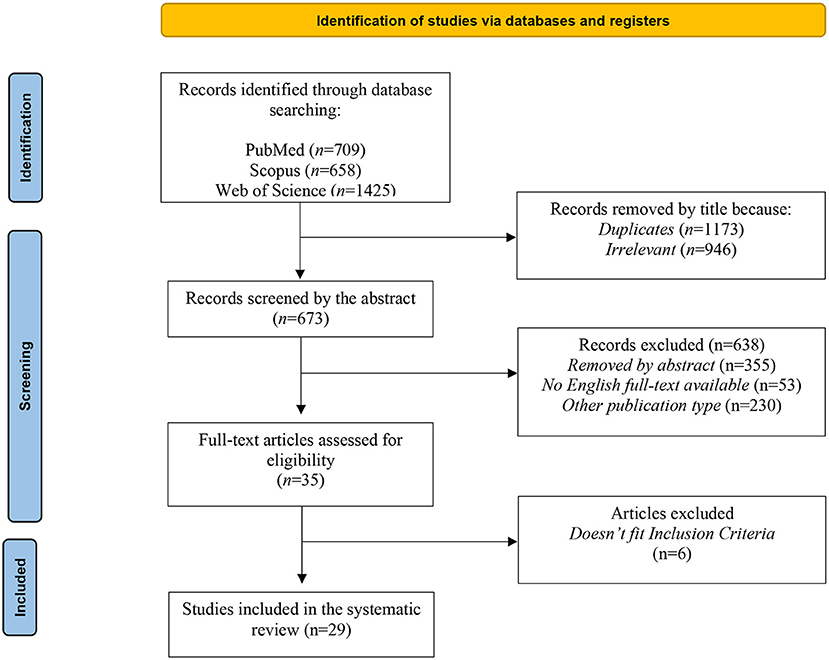
Figure 1. PRISMA flowchart of the study selection process. PRISMA, Preferred reporting items for systematic reviews and meta-analyses.
The quality of articles included was assessed by a standardized tool adapted from Murad et al. (24). Furthermore, we used the Quality Assessment Tool for Observational Cohort and CrossSectional Studies (QATOCCSS) to asses the quality of the other type of study. Each study was scored as either “good,” “fair,” or “poor” (see Table 1). The quality assessment was performed by two independent reviewers (D.G. and L.C.) and a third reviewer (C.C.) cross-checked quality assessment results. Disagreements were discussed and resolved with the research team. The degree of agreement between the independent authors was good.
A total of 29 publications were provided by the search, any of them are studies ranging from 2004 to 2021. Details of each study included in the review are reported in Table 1.
In the present search, 24.13% of the studies included ADHD patients (n = 7), 17.24% of the samples included patients with BD (n = 5) and another 17.24% included Borderline Personality Disorder patients (n = 5), with all the studies including both genders. Of the remaining studies, 6.89% included patients with Gambling Disorder (n = 2), 3.44% ASD (n = 1), 3.44% Problematic Internet Use (n = 1); 27.58% of the remaining included non-clinical (n = 4).
To assess ED, 17 studies (58.62%) used one scale only. The most utilized scale was the Difficulties in Emotion Regulation Scale (DERS) (n = 17; 58.62%), 9 studies utilized this scale in combination with another one, six alongside of the Emotion Regulation Questionnaire (ERQ), two with the Cognitive Emotion Regulation Questionnaire (CERQ), one with the Emotional Experiencing and Regulation Interview (EERI), the Adult Temperament Questionnaire (ATQ) and the ERQ, and one with the Barratt Impulsiveness Scale (BIS-11). Four studies used the CERQ (13.79%) of which one alone, two alongside the DERS and one with the Emotion Reactivity Scale (ERS) and the Base Empathy Scale in Adults (BES-A). Six studies used the ERQ, (20.68%), all in combination with the DERS. Two studies utilized the Affective Liability Scale (ALS) (6.89%), one in combination with AIM and one using both the extended and the shortened version; one study used the ED scale only (3.44%); one used the EMO CHECK Battery (3.44%); one the Current Behavior Scale Self Report (CBS-SF) (3.44%); one the Emotional Processing Scale (EPS-25) (3.44%); one the Emotion Regulation Checklist (ERC) (3.44%); one the Differential Emotion Scale (DES) (3.44%); one the General Emotional Dysregulation Measure (GEDM) (3.44%), and one the Emotional Dysregulation Measure (EDM) (3.44%).
The emotional dimension may play a relevant role in various life phases of patients suffering from Bipolar Disorder (BD). Patients with BD exhibit ED when compared to healthy controls, and display a greater overall difficulty regulating emotions (25), even during remission from mood episodes (26, 27); they clearly show a tendency to use negative strategies to regulate mood, such as rumination and catastrophizing (27). The depressive phase also involves a picture of dysregulation but is characterized by a marked inhibition of positive emotions and a predilection for negative attitudes and emotions, among which anhedonia and affective flattening dominate. In bipolar disorder type II, the dysregulated dimension of emotions in the manic component is less pronounced and tends to be hidden in the euthymic phases of the rest of the population (28). A small number of studies have focused on the comparison of the specific BD subtypes: for instance, Van Rheenen et al. (27) reported the lack of differences in ER between bipolar I and II groups, while Fletcher et al. (29) reported that BP II (but not BP I) patients were more likely to engage in emotion-focused and self-focused rumination about positive affect, compared to unipolar depression participants (29). A particularly important element is the assessment of the sleep pattern in patients with BD. In a sample of patients with BD type II diagnosis, the sleep pattern alteration determines an emotional alteration that leads to an increase in impulsiveness levels, resulting in a substantial and statistically relevant increase in suicidal behavior. Therefore, a careful assessment and an early intervention on sleep and emotional dimension could have a significant positive impact on the prognosis of the disorder (30). Various empirical studies thus establish and acknowledge that BD is a disorder of emotion and motivation. In particular, the orbitofrontal cortex and the amygdala are involved and the connection between these two regions is a marker of biological vulnerability in mood disorders (31). Therefore, ED was proposed to be associated not only with negative functional outcomes in BD patients (27) but has also been proposed as a central component in the development and maintenance of mood disorders and reinforcement of mood instability as well as being correlated to impulsive behaviors, and increased risk of suicidality in individuals (32–34).
In this contest, it is interesting to notice how different studies have identified ED as a nuclear factor of the Cyclothymic Disorder, is characterized by a chronic manifestation of low-grade depressive and hypomanic symptoms (12). Recent studies have highlighted how the Cyclothymic Disorder and the Cyclothymic Temperament are characterized by an elevated level of emotional and behavioral instability and over-reactivity (62, 63). Furthermore, the cyclothymic temperament was shown to be associated with an increased mood and emotional reactivity, with intense reactions to external stimuli, great irritability, anxiety and scarce impulse control (62).
ASD is a neurodevelopmental disorder, characterized by social-communication difficulties, the presence of repetitive behaviors and/or restricted interests with alterations in the sensory profile (12). Children with ASD are at risk of developing internalizing and externalizing problems, moreover both of them are recognized as important predictors of the development of the child's social competence. Dysregulated “externalizing” behaviors are represented by aggressiveness, impulsivity, and control problems, while dysregulated “internalizing” behaviors are depicted by withdrawal, anxiety, and depression (64–66).
ED has been confirmed as a trans-diagnostic risk factor for multiple disorders or symptoms, especially the ones concerning internalizing problems (15, 67). Given that those kinds of problems are a major pillar of ASD, and that multiple studies suggested that emotional regulation is impaired in ASD (67, 68), deficits in emotional regulation may help explaining increased rates of comorbid disorders in ASD patients (68, 69). A study carried by Sàez-Suanes et al. (40) reported that adults with ASD with greater anxiety symptoms also showed greater use of maladaptive emotional regulation strategies, therefore people with ASD are more vulnerable to manifest anxiety for their difficulties in managing negative emotions. In a more global view, some models suggest that anxiety in the general population could be based on emotional regulation and intolerance to uncertainty (70–72). Furthermore, affected individuals are particularly exposed to altered inhibition of emotional response (73), given the recognized difficulties they have in reading situations, identifying with others, assessing perspectives (74), leading to angry and excessive behavioral outcomes such as breaking down, hitting others, screaming with real fits of rage, the previously called “externalizing” behaviors.
Following the lead, many authors have suggested that ED may be an effective explanation to define the typical manifestations of externalizing behaviors (such as anger and aggression) and internalizing behaviors (like anxiety and depression) (15, 75, 76), specifically in adult patients with ASD, defining an extremely typical trajectory of the disorder (68, 74, 77–79).
Gender differences are also reported for ED in ASD patients. In an analytic sample, females have significantly higher emotional dysregulation than males when appropriately investigated (80). Given the gender disparity in ASD diagnosis and given potential differences in the manifestation of autistic traits in females compared to males (81–84) investigating emotional elements in advance could play an index factor in the correct diagnosis of ASD in females, given the male trend in diagnosis, proposing a trajectory and diagnosis perspective that in the most decisive cases of ED leads to complex and organized cluster B personality disorders as hypothesized in an adult trajectory of subthreshold autistic conditions.
ADHD is a neurodevelopmental disorder that persists into adulthood in ~50–60% of cases (85, 86) with a prevalence of 2.5–4.4% (87–89). It's characterized by inattention, impulsivity, and hyperactivity but also problems with mood instability, such as irritability, swift mood changes, hot temper, and low frustration tolerance, frequently appear to accompany the disorder (90). ADHD is a disorder in close relationship with ED (10, 91), in children, adolescents and adults (92–94) and it is estimated that 37–40% of individuals with ADHD have ED (95). Individuals with ADHD and ED are more impaired in daily life functioning than those with ADHD in the absence of ED (9, 47, 96–100).
A growing number of evidence are showing that ED symptoms are expressed in a large percentage of adult ADHD patients (99, 101–103), in particular in one adult study, 55% of ADHD patients showed ED that was of greater severity than >95% of control subjects (98, 104) emphasizing the importance of screening the emotional domain of ADHD. A first step was made by Wender (105), who described symptoms of ED in the Utah Criteria for the diagnosis of ADHD in adults and, later on, many other authors took into account the emotional experience of ADHD patients and proposed the consideration of emotional symptoms as an additional core component of ADHD psychopathology (106–108). However, in the last revision of the DSM-5-TR and ICD, ED is still not included as a third central dimension in the psychopathological core of the ADHD picture, although it's recognized its importance and its use is recommended for optimal framing (109). The dimension of ED is highly non-specific due to its trans-nosographic nature, the lack of standardization and, above all, the extreme subjectivity of behavioral manifestation that varies from individual to individual.
Various studies have shown that individuals with mental disorders have a tendency to use fewer effective strategies for emotion regulation, and particularly in ADHD it seems that the difficulty is related to the temporal dimension and the predilection for short-term rewards (16).
The severity of ADHD symptoms, as argued in the meta-analysis study conducted by Beheshti et al. (110), is significantly correlated with ED dimensions such as emotional lability and emotion recognition.
Although being correlated with all the core domains of ADHD (102, 111, 112), ED appears to be part of the same dimension of the hyperactivity/impulsivity symptoms, with which it shares a much stronger relationship compared to the attention deficit core (74, 101, 113, 114). Therefore, the classic domains of inattention, hyperactivity and impulsivity are not sufficient to explain the entire spectrum of symptoms in adults, especially when the disorder is found with other comorbid pathologies, so the assessment of the emotional dimension is fundamental for a better diagnostic framing and to avoid evaluating ED as a secondary effect due, for example, to an anxiety-type framework (52, 115).
Schizophrenia Spectrum Disorders are severe psychiatric conditions characterized by a varying severity of positive and negative symptoms. Patients with symptoms of severe ED have structural alterations in the limbic system, in particular a lower density of gray matter in the right ventral striatum has been shown (116).
A previous review and meta-analyses of the available literature has reported that patients with schizophrenia are likely to use more maladaptive and less adaptive cognitive emotion regulation strategies compared to healthy controls (117) and that they are usually related to the maintenance and exacerbation of positive symptoms (118, 119). Maladaptive cognitive emotion regulation strategies were also found to increase the tendency for cognitive biases and misinterpretations of negative affective states, and return increase the risk of hallucinations and delusions (120). Patients with schizophrenia spectrum disorders are known to experience greater emotional distress (121). Some patients may engage in expressive suppression to cope with painful emotions. However, habitual use of expressive suppression is likely to increase arousal, amplify distress and worsen the course of positive symptoms (119).
In 1997 Gross and Levenson suggested that there may be important differences between the ability to regulate positive and negative emotions and later many other studies focused on the importance of ED in the psychopathology of schizophrenia. A study from Owens et al. (122) highlighted a positive correlation between global ED and both positive and negative symptoms; another from Lincoln et al. (123) observed that global ED and its components (e.g., emotional awareness, tolerance, acceptance, and modification) were negatively correlated with paranoia symptoms; contrasting results came instead in a study carried by Bonfils et al. (124) were they did not observe any significant correlations between global ED and positive or negative symptoms.
It is therefore important for future research to extend the current findings by examining the ability of schizophrenic patients to regulate these two entities, especially the processes of worry and anxiety may be causal elements of delusional symptoms, so a thorough investigation and assessment of the emotional dimension and application of treatment could result in an improved prognosis of schizophrenic disorder (125).
ED has been recently considered a fundamental component of the Post-traumatic Stress Disorder (PTSD) as the global literature on emotional regulation and intensity of PTSD symptoms suggests there is a general lack of emotional regulation in people exposed to various traumatic events (35). A recent meta-analysis reported that PTSD, regardless of the kind of traumatic event that generates it, is characterized by a general dysregulation of emotions that is more relevant in explaining the symptoms than any of the specific regulatory strategies used individually (126). In addition, ED gives rise to the hyper-vigilance and distortions of attention, hyper-excitement, emotional numbness and irritability (127). In support to the hypothesis, from a neuroanatomical perspective, the amygdala and insula are particularly hyperactive in response to stimuli that convey social threats (e.g., faces), aversive images, and signals that evoke personal trauma, in patients with PTSD.
The latest literature is greatly supporting the association between PTSD and constructs of emotional value, like: suppression (intended as the inhibition of expression of emotional responses (128), experiential avoidance (the attempt to suppress unwanted internal experiences such as emotions, thoughts, or memories (129), alexithymia (difficulty identifying what they feel (130), or dissociation (the mental process of disconnection from thoughts, and feelings (14). Litz et al. (131) defined the concept of “Emotional numbness” with the disaffection for emotion-provoking circumstances and the a lack of emotional reactivity, and furthermore proved it to be a relevant predictor of the endurance of post-traumatic symptoms. Besides, the 2014 study conducted by Abigail further defines the centrality of ED within PTSD and argues how it's the framework of ED that determines the presence of dissociative symptoms in PTSD. As PTSD can have a devastating impact on health and functioning, increasing the risk of comorbidity with other mental disorders (132) and adverse medical conditions [e.g., (133, 134)], therefore it is crucial to identify factors that can increase its risk early and preventively. These include ED, reflecting deficits in an individual's ability to recognize and accept their emotions, as well as deficits in the ability to adaptively choose effective strategies to manage emotions when they arise (13, 14). In fact, a great number of studies, suggest that the use of maladaptive strategies (i.e., self-blame, rumination, catastrophizing) may increase the vulnerability toward psychopathology, whereas adaptive cognitive styles (i.e., acceptance or positive refocusing and putting into perspective) can lead to more resilience to symptoms of psychological distress (135, 136). Researches showed that trauma, especially enduring or repeated traumatic experiences such as early life stress, seems to compromise the acquisition of appropriate emotion regulation skills (38). On that way, data indicate that the assessment of ED in standard medical care would allow the identification of those who are at risk of developing severe forms of PTSD (as they already possess a dysregulated emotional framework) providing a practical treatment target (132, 133, 137), given the association of ED with a variety of mental disorders.
Borderline Personality Disorder (BPD), is characterized by a pervasive pattern of instability of interpersonal relationships, self-image and affects, marked impulsivity, emotional instability, including impaired emotional awareness and “clarity” (138), problems employing emotion regulation strategies (139, 140), interpersonal difficulties and dysfunctional cognitive processes (141), with all of the above influencing the patients general functioning (142), treatment compliance (143, 144), physical health status (145) and relationship dimension (146).
Since the regulation of emotions is difficult in these patients, BPD perfectly fits in our examination, and ED should be central in clinical observation. Impulsivity and ED are pivotal and significant features in BPD over time (147). As argued in Sebastian et al. (148), the impulsivity seen in BPD (if not caused by ADHD) may be just another dependent and secondary element of ED; inter alia impulsivity is strongly associated with suicide attempts in both adults and adolescents (149–151) and non-suicidal self–injury (152, 153), whether it is planned or unplanned (154) meanwhile ED has been found to be the strongest predictor of self-harm over time (155–158) and serves as a maladaptive strategy to reduce negative affect and to regulate the mood (159, 160). Older patients diagnosed with BPD show alterations in emotion social functioning and regulation strategies, using maladaptive cognitive strategies such as rumination (161, 162) and thought suppression (163, 164); in contrast, younger people diagnosed with BPD are more likely to express anger and self-injurious behavior.
Other studies have instead focused on the role of ED in determining aggressive behavior (165–167) and behavioral dyscontrol (51, 168) in BPD.
Despite being the most extensively studied personality disorder (169, 170), its diagnosis is still quite problematic. BPD can be conceptualized as a severe mental disorder that continues over time with changing manifestations. Age-related symptoms should be considered in the diagnosis of BPD with the need for appropriate treatment focusing on ED and impulsive behavior (171). Focusing on the regulation of individual emotions in couple interaction, it seems to be a promising target to reduce relationship dysfunctions in BPD. This element contributes to enrich the mosaic of information that tends to centralize and consider as a dimension of necessary importance ED (50, 172, 173). As argued in the study conducted by Peter et al. (174), the application of practices of teaching or managing and understanding emotions by the therapist to the BPD patient, contributes to a substantial improvement in the psychopathological picture. In this setting, the use and implementation of a specific treatment practice such as dialectical behavior therapy (DBT) has been described. DBT mainly intervenes in the emotional dimension (175).
Regarding disruptive behavior disorders—impulse control and conduct disorders, nutrition and eating disorders, substance-related and addiction disorders, paraphilic disorders—the ED dimension is particularly evident. Many studies have highlighted the presence of ED in many mental disorders: oppositional defiant disorders (111, 115), borderline personality disorders (176, 177), mood disorders, (178, 179), anxiety disorders (33), eating disorders (180), and substance abuse/dependency (181).
By analyzing each psychopathological nucleus, the perspective of ED assessment is intended to challenge the current clinical-diagnostic dimension. In fact, emotional phenomena are rarely evaluated as primary dimensions of alterative processes, and more often as a derived and derivable dimension due to environmental effects, maladaptive and secondary to other psychiatric pathologies.
The aim of this review is to bring an essential vision of the concept of ED and its role in the frame of the adult psychopathology and its relevance in the clinical practice. Where the importance of ED is prominent in the study of children and adolescents' mental disorders, not many studies have yet focused on its role in the development and maintenance of adult mental disorders.
In the recent years, ED has been a new focus of interest in the adult psychiatric research, although to this day it still lacks of a univocal definition. One of the most commonly accepted, and the one we choose to relate to, pictures ED as the “inability to exercise any or all aspects of the modulatory processes involved in emotion regulation, to such a degree that the inability results in the individual functioning meaningfully below his or her baseline” (9). To this day, the most widely used method of assessment of ED, is the DERS scale, both developed and evaluated in an adult sample (182). It's a self-report questionnaire, structured in six domains exploring Awareness (acceptance of emotions), Clarity (knowledge about one's emotions), Goals (evaluating difficulty with goal-directed behavior when upset), Impulse (indicative of difficulty with behavioral control when experiencing negative emotions), Non-acceptance (indicative of negative secondary emotions) and Strategies (the belief that no strategy can decrease negative emotion) (97).
Researches in literature proves that in many mental disorders, such as ADHD, psychosis, or affective mood disorders, ED is an essential but often neglected part of psychopathology. We aimed at assessing ED as a trans-nosographic entity across the main mental disorders, highlighting its role in the development, manifestation and maintenance of such pathologies.
In many disorders, such as BD, PTSD, and Schizophrenia, ED has a major role in the development and maintenance of the symptomatology; in BD acts as a reinforcement of mood instability and is associated to impulsive behaviors, and increased risk of suicidality (32–34). Also studies in BPD patients have confirmed ED as the strongest predictor of impulsivity and self-harm over time (148, 155–158). Both BD and Schizophrenia, patiens have also shown a greater difficulty regulating emotions during episodes as well add during remission (25–27, 117) and in Schizophrenia being related to both positive and negative symptoms (118, 119, 122). In neurodevelopement disorder such as ASD and ADHD, ED represent an explanation for most of the externalizing and internalizing behaviors (15, 75, 76), specifically in adults. Evermore, a growing number of studies are confirming the close relationship between ADHD and ED and how the latter is strongly correlated with all the core domains of ADHD (102, 111, 112). Even PTSD, regardless of the kind of traumatic event that generates it, is knowingly characterized by a general dysregulation of emotions (126), giving rise to hyper-vigilance, hyper-excitement, emotional numbness and irritability (127).
ED has thus confirmed it pivotal role as trans-diagnostic risk factor for multiple disorders and symptoms, especially the ones concerning internalizing problems (15, 67). In this view, it is strongly highlighted both the importance of conducting an attentive assessment of the strategies of emotional regulation during the diagnostical framing of clinical practice and the therapeutic central role that it occupy.
The inclusion of ED as a trans-nosographic entity could be stimulant or provocatory, but would perfectly fit the vision of mental disorders as a wide range of behavioral conditions that progressively move away from conventional, through the most intrinsic dimensions of each individual and how they tend to relate to the external environment. ED and related symptoms are well integrated in this kind of clinical features and could be a helpful concept to interpret and clarify many clinical cases.
The concept of ED will probably help in discovering basic approaches to the understanding, diagnosis, and treatment of mental disorders. ED may possibly be a new concept, allowing mental disorders to be defined by their essential nature instead being defined by their phenotype and objectively measured symptoms.
When discussing our results some limitations should be taken into account.
Firstly, the dimension of ED is highly non-specific due to its trans-nosographic nature, the lack of a univocal definition, especially when investigated in adulthood, the variety and heterogeneity of the scales available for its assessment and, above all, the extreme subjectivity of behavioral manifestation that varies from individual to individual. Second, studies on ED are mainly centered on the pediatric population, therefore data on its manifestation and its association with some mental disorders in adulthood, are still scant. However, one of the aims of the present review was to shed light on the need for further studies in adult population. Third, due to the heterogeneity of ED nomenclatures, the terms we chose to include in the literature search might not be comprehensive of all the terminology used to this day. Lastly, during the selection process we didn't use controlled vocabulary (e.g., MeSH) and we included only articles in English language.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
CC: conceptualization, methodology, investigation, writing—original draft, writing—review and editing, and supervision. LC and DG: methodology, investigation, writing—original draft, and writing—review and editing. BN: methodology, investigation, writing original draft, and writing—review. LD'O: supervision and final manuscript version revision. All authors contributed to the article and approved.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer MB declared a shared affiliation with the authors to the handling editor at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Damasio AR, Grabowski TJ, Bechara A, Damasio H, Ponto LL, Parvizi J, et al. Subcortical and cortical brain activity during the feeling of self-generated emotions. Nat Neurosci. (2000) 3:1049–56. doi: 10.1038/79871
2. Catani M, Dell'Acqua F, De Schotten MT. A revised limbic system model for memory, emotion and behavior. Neurosci Biobehav Rev. (2013) 37:1724–37. doi: 10.1016/j.neubiorev.2013.07.001
3. Kelley NJ, Hughes ML. Resting frontal EEG asymmetry and emotion regulation in older adults: the midlife in the United States (MIDUS) study. Psychol Aging. (2019) 34:341. doi: 10.1037/pag0000344
4. Pace-Schott EF, Amole MC, Aue T, Balconi M, Bylsma LM, Critchley H, et al. Physiological feelings. Neurosci Biobehav Rev. (2019) 103:267–304. doi: 10.1016/j.neubiorev.2019.05.002
6. Kring AM, Sloan DM. Emotion Regulation and Psychopathology: A Transdiagnostic Approach to Etiology and Treatment. New York, NY: Guilford Press (2009).
7. Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin Psychol Sci. (2014) 2:387–401. doi: 10.1177/2167702614536164
8. Thompson RA. Emotional regulation and emotional development. Educ Psychol Rev. (1991) 3:269–307. doi: 10.1007/BF01319934
9. Bunford N, Evans SW, Wymbs F. ADHD and emotion dysregulation among children and adolescents. Clin Child Fam Psychol Rev. (2015) 18:185–217. doi: 10.1007/s10567-015-0187-5
10. Shaw P, Stringaris A, Nigg J, Leibenluft E. Emotion dysregulation in attention deficit hy peractivity disorder. Am J Psychiatry. (2014) 171:276–93. doi: 10.1176/appi.ajp.2013.13070966
11. Gross JJ, Levenson RW. Hiding feelings: the acute effects of inhibiting negative and positive emotion. J Abnorm Psychol. (1997) 106:95. doi: 10.1037/0021-843X.106.1.95
12. American Psychiatric Association. DSM-V How does emotion regulation strategy use and psychological wellbeing predict mood in adults with and without autism spectrum disorder? a naturalistic assessment. J Autism Develop Disord. 50:1786–99. doi: 10.1007/s10803-019-03934-0
13. Gross JJ, Thompson RA. Emotion regulation. Conceptual foundations. In: J. Gross, editor. Handbook of Emtion Regulation. Guilford Press, New York, NY (2007). p. 3–24.
14. Powers A, Cross D, Fani N, Bradley B. PTSD, emotion dysregulation, and dissociative symptoms in a highly traumatized sample. J Psychiatr Res. (2015) 61:174–9. doi: 10.1016/j.jpsychires.2014.12.011
15. Aldao A, Gee DG, De Los Reyes A, Seager I. Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: current and future directions. Dev Psychopathol. (2016) 28:927–46. doi: 10.1017/S0954579416000638
16. Sheppes G, Suri G, Gross JJ. Emotion regulation and psychopathology. Annu Rev Clin Psychol. (2015) 11:379–405. doi: 10.1146/annurev-clinpsy-032814-112739
17. Jesberger JA, Richardson JS. Brain output dysregulation induced by olfactory bulbectomy: an approximation in the rat of major depressive disorder in humans? Int J Neurosci. (1988) 38:241–65. doi: 10.3109/00207458808990688
18. Stratakis CA, Chrousos GP. Neuroendocrinology and pathophysiology of the stress system. Ann N Y Acad Sci. (1995) 771:1–18. doi: 10.1111/j.1749-6632.1995.tb44666.x
19. Siever LJ, Uhde TW, Insel TR, Kaye WH, Jimerson DC, Lake CR, et al. Biological alterations in the primary affective disorders and other tricyclic-responsive disorders. Progr Neuro-Psychopharmacol Biologic Psychiatr. (1985) 9:15–24. doi: 10.1016/0278-5846(85)90175-7
20. von Bardeleben U, Holsboer F. Cortisol response to corticotropin releasing hormone in dexamethasone-pretreated patients with depression. In Neuropsychopharmacology, Berlin, Heidelberg: Springer, (1990). p. 221–233.
21. Masi G, Sesso G, Pfanner C, Valente E, Molesti A, Placini F, et al. An exploratory study of emotional dysregulation dimensions in youth with attention deficit hyperactivity disorder and/or bipolar spectrum disorders. Front Psychiatr. (2021) 12:409. doi: 10.3389/fpsyt.2021.619037
22. Rucci P, Frank E, Fagiolini A, Kupfer DJ, Shear MK, Dell'Osso L, et al. Development and preliminary testing of the general 5-Spectrum measure (GSM-V). Depress Anxi. (2003) 18:109–17. doi: 10.1002/da.10123
23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
24. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. (2018) 23:60–3. doi: 10.1136/bmjebm-2017-110853
25. Becerra R, Cruise K, Murray G, Bassett D, Harms C, Allan A, et al. Emotion regulation in bipolar disorder: are emotion regulation abilities less compromised in euthymic bipolar disorder than unipolar depressive or anxiety disorders? Jama. (2013) 3:34. doi: 10.4236/ojpsych.2013.34A001
26. Hay AC, Sheppes G, Gross JJ, Gruber J. Choosing how to feel: emotion regulation choice in bipolar disorder. Emotion. (2015) 15:139. doi: 10.1037/emo0000024
27. Van Rheenen TE, Murray G, Rossell SL. Emotion regulation in bipolar disorder: profile and utility in predicting trait mania and depression propensity. Psychiatry Res. (2015) 225:425–32. doi: 10.1016/j.psychres.2014.12.001
28. Miklowitz DJ, Johnson SL. The psychopathology and treatment of bipolar disorder. Annu Rev Clin Psychol. (2006) 2:199–235. doi: 10.1146/annurev.clinpsy.2.022305.095332
29. Fletcher K, Parker GB, Manicavasagar V. Coping profiles in bipolar disorder. Compr Psychiatry. (2013) 54:1177–84. doi: 10.1016/j.comppsych.2013.05.011
30. Palagini L, Cipollone G, Masci I, Caruso D, Paolilli F, Perugi G, et al. Insomnia symptoms predict emotional dysregulation, impulsivity and suicidality in depressive bipolar II patients with mixed features. Compr Psychiatry. (2019) 89:46–51. doi: 10.1016/j.comppsych.2018.12.009
31. Wessa M, Kanske P, Linke J. Bipolar disorder: a neural network perspective on a disorder of emotion and motivation. Restor Neurol Neurosci. (2014) 32:51–62. doi: 10.3233/RNN-139007
32. Henry C, Phillips M, Leibenluft E, M'bailara K, Houenou J, Leboyer M. Emotional dysfunction as a marker of bipolar disorders. Front Biosci. (2012) 4:2722. doi: 10.2741/e578
33. Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depress Anxiety. (2012) 29:409–16. doi: 10.1002/da.21888
35. Muñoz-Rivas M, Bellot A, Montorio I, Ronzón-Tirado R, Redondo N. Profiles of emotion regulation and post-traumatic stress severity among female victims of intimate partner violence. Int J Environ Res Public Health. (2021) 18:6865. doi: 10.3390/ijerph18136865
36. Faustino B. Transdiagnostic perspective on psychological inflexibility and emotional dysregulation. Behav Cogn Psychother. (2020) 49:233–46. doi: 10.1017/S1352465820000600
37. Ciuluvica C, Amerio P, Grossu IV. Emotional dysregulation mechanisms in psychosomatic chronic diseases revealed by the instability coefficient. Brain Sci. (2020) 10:673. doi: 10.3390/brainsci10100673
38. Demir Z, Böge K, Fan Y, Hartling C, Harb MR, Hahn E, et al. The role of emotion regulation as a mediator between early life stress and posttraumatic stress disorder, depression and anxiety in Syrian refugees. Transl Psychiatry. (2020) 10:1–10. doi: 10.1038/s41398-020-01062-3
39. Anker E, Haavik J, Heir T. Alcohol and drug use disorders in adult attention-deficit/hyperactivity disorder: prevalence and associations with attention-deficit/hyperactivity disorder symptom severity and emotional dysregulation. World J Psychiatry. (2020) 10:202. doi: 10.5498/wjp.v10.i9.202
40. Sáez-Suanes GP, García-Villamisar D, del Pozo Armentia A, Dattilo J. Emotional dysregulation and uncertainty intolerance as transdiagnostic mediators of anxiety in adults with autism spectrum disorders and intellectual disability. Res Develop Disabil. (2020) 106:103784. doi: 10.1016/j.ridd.2020.103784
41. Pettorruso M, Valle S, Cavic E, Martinotti G, Di Giannantonio M, Grant JE. Problematic Internet use (PIU), personality profiles and emotion dysregulation in a cohort of young adults: trajectories from risky behaviors to addiction. Psychiatry Res. (2020) 289:113036. doi: 10.1016/j.psychres.2020.113036
42. Rogier G, Beomonte Zobel S, Velotti P. Pathological personality facets and emotion (dys) regulation in gambling disorder. Scand J Psychol. (2020) 61:262–70. doi: 10.1111/sjop.12579
43. Mestre-Bach G, Steward T, Potenza MN, Granero R, Fernandez-Aranda F, Mena-Moreno T, et al. The role of ADHD symptomatology and emotion dysregulation in gambling disorder. J Atten Disord. (2021) 25:1230–9. doi: 10.1177/1087054719894378
44. Rüfenacht E, Euler S, Prada P, Nicastro R, Dieben K, Hasler R, et al. Emotion dysregulation in adults suffering from attention deficit hyperactivity disorder (ADHD), a comparison with borderline personality disorder (BPD). Borderline Personal Disord Emot Dysregulat. (2019) 6:1–10. doi: 10.1186/s40479-019-0108-1
45. Raudales AM, Short NA, Schmidt NB. Emotion dysregulation mediates the relationship between trauma type and PTSD symptoms in a diverse trauma-exposed clinical sample. Personality and Individual Differences. (2019) 139:28–33.
46. Liu J, Chan TCT, Chong SA, Subramaniam M, Mahendran R. Impact of emotion dysregulation and cognitive insight on psychotic and depressive symptoms during the early course of schizophrenia spectrum disorders. Early Intervention in Psychiatry. (2019). eip.12895. doi: 10.1111/eip.12895
47. Bodalski EA, Knouse LE, Kovalev D. Adult ADHD, emotion dysregulation, and functional outcomes: examining the role of emotion regulation strategies. J Psychopathol Behav Assess. (2019) 41:81–92. doi: 10.1007/s10862-018-9695-1
48. Hirsch O, Chavanon M, Riechmann E, Christiansen H. Emotional dysregulation is a primary symptom in adult Attention-Deficit/Hyperactivity Disorder (ADHD). J Affect Disord. (2018) 232:41–7. doi: 10.1016/j.jad.2018.02.007
49. Garofalo C, Velotti P, Callea A, Popolo R, Salvatore G, Cavallo F, et al. Emotion dysregulation, impulsivity and personality disorder traits: a community sample study. Psychiatry Res. (2018) 266:186–92. doi: 10.1016/j.psychres.2018.05.067
50. Rufino KA, Ellis TE, Clapp J, Pearte C, Fowler JC. Variations of emotion dysregulation in borderline personality disorder: a latent profile analysis approach with adult psychiatric inpatients. Borderline Personal Disord Emot Dysregulat. (2017) 4:1–9. doi: 10.1186/s40479-017-0068-2
51. Terzi L, Martino F, Berardi D, Bortolotti B, Sasdelli A, Menchetti M. Aggressive behavior and self-harm in borderline personality disorder: the role of impulsivity and emotion dysregulation in a sample of outpatients. Psychiatry Res. (2017) 249:321–6. doi: 10.1016/j.psychres.2017.01.011
52. Corbisiero S, Mörstedt B, Bitto H, Stieglitz RD. Emotional dysregulation in adults with attention-deficit/hyperactivity disorder–validity, predictability, severity, and comorbidity. J Clin Psychol. (2017) 73:99–112. doi: 10.1002/jclp.22317
53. Lagerberg TV, Aminoff SR, Aas M, Bjella T, Henry C, Leboyer M, et al. Alcohol use disorders are associated with increased affective lability in bipolar disorder. Journal of Affective Disorders. (2017) 208:316–324.
54. Chamberlain SR, Ioannidis K, Leppink EW, Niaz F, Redden SA, et al. ADHD symptoms in non-treatment seeking young adults: relationship with other forms of impulsivity. CNS Spectrums. (2017) 22:22–30.
55. Richard-Lepouriel H, Etain B, Hasler R, Bellivier F, Gard S, Kahn JP, et al. Similarities between emotional dysregulation in adults suffering from ADHD and bipolar patients. J Affect Disord. (2016) 198:230–6. doi: 10.1016/j.jad.2016.03.047
56. Ruscitti C, Rufino K, Goodwin N, Wagner R. Difficulties in emotion regulation in patients with eating disorders. Borderline Personal Disord Emot Dysregulat. (2016) 3:1–7. doi: 10.1186/s40479-016-0037-1
57. Bayes A, Parker G, McClure G. Emotional dysregulation in those with bipolar disorder, borderline personality disorder and their comorbid expression. J Affect Disord. (2016) 204:103–11. doi: 10.1016/j.jad.2016.06.027
58. Yoon J, Knight RA. Emotional processing of individuals high in psychopathic traits. Aust J Psychol. (2015) 67:29–37. doi: 10.1111/ajpy.12063
59. Scott LN, Stepp SD, Pilkonis PA. Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Personal Disord Theory Res Treat. (2014) 5:278. doi: 10.1037/per0000070
60. Beblo T, Pastuszak A, Griepenstroh J, Fernando S, Driessen M, Schütz A, et al. Self-reported emotional dysregulation but no impairment of emotional intelligence in borderline personality disorder: an explorative study. The Journal of Nervous and Mental Disease. (2010) 198:385–8.
61. Newhill CE, Mulvey EP, Pilkonis PA. Initial development of a measure of emotional dysregulation for individuals with cluster B personality disorders. Res Soc Work Pract. (2004) 14:443–9. doi: 10.1177/1049731504267332
62. Pisano S, Senese VP, Bravaccio C, Santangelo P, Milone A, Masi G, et al. Cyclothymic-hypersensitive temperament in youths: Refining the structure, the way of assessment and the clinical significance in the youth population. J Affect Disord. (2020) 271:272–8. doi: 10.1016/j.jad.2020.03.155
63. Brancati GE, Barbuti M, Schiavi E, Colombini P, Moriconi M, Pallucchini A, et al. Comparison of emotional dysregulation features in cyclothymia and adult ADHD. Medicina. (2021) 57:489. doi: 10.3390/medicina57050489
64. Burt KB, Obradović J, Long JD, Masten AS. The interplay of social competence and psychopathology over 20 years: testing transactional and cascade models. Child Dev. (2008) 79:359–74. doi: 10.1111/j.1467-8624.2007.01130.x
65. Hay DF, Payne A, Chadwick A. Peer relations in childhood. J Child Psychol Psychiatr. (2004) 45:84–108. doi: 10.1046/j.0021-9630.2003.00308.x
66. Dell'Osso L, Cremone IM, Carpita B, Fagiolini A, Massimetti G, Bossini L, et al. Correlates of autistic traits among patients with borderline personality disorder. Compr Psychiatry. (2018) 83:7–11. doi: 10.1016/j.comppsych.2018.01.002
67. Cai RY, Richdale AL, Dissanayake C, Uljarević M. Brief report: Inter-relationship between emotion regulation, intolerance of uncertainty, anxiety, and depression in youth with autism spectrum disorder. J Autism Dev Disord. (2018) 48:316–25. doi: 10.1007/s10803-017-3318-7
68. Bruggink A, Huisman S, Vuijk R, Kraaij V, Garnefski N. Cognitive emotion regulation, anxiety and depression in adults with autism spectrum disorder. Res Autism Spectr Disord. (2016) 22:34–44. doi: 10.1016/j.rasd.2015.11.003
69. Charlton AS, Smith IC, Mazefsky CA, White SW. The role of emotion regulation on co-occurring psychopathology in emerging adults with ASD. J Autism Dev Disord. (2020) 50:2585–92. doi: 10.1007/s10803-019-03983-5
70. Dugas MJ, Koerner N. Cognitive-behavioral treatment for generalized anxiety disorder: current status and future directions. J Cogn Psychother. (2005) 19:61. doi: 10.1891/jcop.19.1.61.66326
71. Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behav Res Ther. (2005) 43:1281–310. doi: 10.1016/j.brat.2004.08.008
72. Ouellet C, Langlois F, Provencher MD, Gosselin P. Intolerance of uncertainty and difficulties in emotion regulation: proposal for an integrative model of generalized anxiety disorder. Euro Rev Appl Psychol. (2019) 69:9–18. doi: 10.1016/j.erap.2019.01.001
73. Antezana L, Mosner MG, Troiani V, Yerys BE. Social-emotional inhibition of return in children with autism spectrum disorder vs. typical development. J Autism Dev Disord. (2016) 46:1236–46. doi: 10.1007/s10803-015-2661-9
74. Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, et al. The role of emotion regulation in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. (2013) 52:679–88. doi: 10.1016/j.jaac.2013.05.006
75. Carleton RN. Fear of the unknown: one fear to rule them all? J Anxiety Disord. (2016) 41:5–21. doi: 10.1016/j.janxdis.2016.03.011
76. McEvoy PM, Mahoney AE. To be sure, to be sure: Intolerance of uncertainty mediates symptoms of various anxiety disorders and depression. Behav Ther. (2012) 43:533–45. doi: 10.1016/j.beth.2011.02.007
77. Hodgson AR, Freeston MH, Honey E, Rodgers J. Facing the unknown: Intolerance of uncertainty in children with autism spectrum disorder. J Appl Res Intellect Disabil. (2017) 30:336–44. doi: 10.1111/jar.12245
78. Neil L, Olsson NC, Pellicano E. The relationship between intolerance of uncertainty, sensory sensitivities, and anxiety in autistic and typically developing children. J Autism Dev Disord. (2016) 46:1962–73. doi: 10.1007/s10803-016-2721-9
79. Samson AC, Hardan AY, Lee IA, Phillips JM, Gross JJ. Maladaptive behavior in autism spectrum disorder: the role of emotion experience and emotion regulation. J Autism Dev Disord. (2015) 45:3424–32. doi: 10.1007/s10803-015-2388-7
80. Wieckowski AT, Luallin S, Pan Z, Righi G, Gabriels RL, Mazefsky C. Gender differences in emotion dysregulation in an autism inpatient psychiatric sample. Autism Research. (2020) 13:1343–8. doi: 10.1002/aur.2295
81. Westwood H, Eisler I, Mandy W, Leppanen J, Treasure J, Tchanturia K. Using the autism-spectrum quotient to measure autistic traits in anorexia nervosa: a systematic review and meta-analysis. J Autism Dev Disord. (2016) 46:964–77. doi: 10.1007/s10803-015-2641-0
82. Westwood H, Tchanturia K. Autism spectrum disorder in anorexia nervosa: an updated literature review. Curr Psychiatry Rep. (2017) 19:41. doi: 10.1007/s11920-017-0791-9
83. Dell'Osso L, Carpita B, Gesi C, Cremone IM, Corsi M, Massimetti E, et al. Subthreshold autism spectrum disorder in patients with eating disorders. Comprehen Psychiatr. (2018) 81:66–72. doi: 10.1016/j.comppsych.2017.11.007
84. Dell'Osso L, Carpita B, Muti D, Morelli V, Salarpi G, Salerni A, et al. Mood symptoms and suicidality across the autism spectrum. Comprehen Psychiatr. (2019) 91:34–8. doi: 10.1016/j.comppsych.2019.03.004
85. Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. (2006) 36:159–65. doi: 10.1017/S003329170500471X
86. Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi EVA, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. (2005) 35:245–56. doi: 10.1017/S0033291704002892
87. Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatr. (2007) 190:402–9. doi: 10.1192/bjp.bp.106.034389
88. Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. (2006) 163:716–23. doi: 10.1176/ajp.2006.163.4.716
89. Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatr. (2009) 194:204–11. doi: 10.1192/bjp.bp.107.048827
90. Skirrow C, McLoughlin G, Kuntsi J, Asherson P. Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Rev Neurother. (2009) 9:489–503. doi: 10.1586/ern.09.2
91. Martel MM. Research Review: A new perspective on attention-deficit/hyperactivity disorder: emotion dysregulation and trait models. J Child Psychol Psychiatr. (2009) 50:1042–51. doi: 10.1111/j.1469-7610.2009.02105.x
92. Corbisiero S, Stieglitz RD, Retz W, Rösler M. Is emotional dysregulation part of the psychopathology of ADHD in adults?. ADHD Atten Deficit Hyperactiv Disord. (2013) 5:83–92. doi: 10.1007/s12402-012-0097-z
93. Biederman J, Spencer T, Lomedico A, Day H, Petty CR, Faraone SV. Deficient emotional self-regulation and pediatric attention deficit hyperactivity disorder: a family risk analysis. Psychol Med. (2012) 42:639–46. doi: 10.1017/S0033291711001644
94. Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, et al. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J Child Psychol Psychiatr. (2010) 51:915–23. doi: 10.1111/j.1469-7610.2010.02217.x
95. Hirsch O, Chavanon ML, Christiansen H. Emotional dysregulation subgroups in patients with adult attention-deficit/hyperactivity disorder (ADHD): a cluster analytic approach. Sci Rep. (2019) 9:1–11. doi: 10.1038/s41598-019-42018-y
96. Barkley RA, Fischer M. Predicting impairment in major life activities and occupational functioning in hyperactive children as adults: self-reported executive function (EF) deficits vs. EF tests. Dev Neuropsychol. (2011) 36:137–61. doi: 10.1080/87565641.2010.549877
97. Bunford N, Dawson AE, Evans SW, Ray AR, Langberg JM, Owens JS, et al. The difficulties in emotion regulation scale–parent report: a psychometric investigation examining adolescents with and without ADHD. Assessment. (2020) 27:921–40. doi: 10.1177/1073191118792307
98. Surman CB, Biederman J, Spencer T, Miller CA, McDermott KM, Faraone SV. Understanding deficient emotional self-regulation in adults with attention deficit hyperactivity disorder: a controlled study. ADHD Attent Deficit Hyperactiv Disord. (2013) 5:273–81. doi: 10.1007/s12402-012-0100-8
99. Barkley RA, Murphy KR. Attention-deficit Hyperactivity Disorder: A Clinical workbook. New York, NY: Guilford Press (2006).
100. Skirrow C, Asherson P. Emotional lability, comorbidity and impairment in adults with attention-deficit hyperactivity disorder. J Affect Disord. (2013) 147:80–6. doi: 10.1016/j.jad.2012.10.011
101. Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J Am Acad Child Adolesc Psychiatry. (2010) 49:503–13. doi: 10.1016/j.jaac.2010.01.019
102. Reimherr FW, Marchant BK, Olsen JL, Halls C, Kondo DG, Williams ED, et al. Emotional dysregulation as a core feature of adult ADHD: its relationship with clinical variables and treatment response in two methylphenidate trials. J ADHD Relat Disord. (2010) 1:53–64.
103. Robison RJ, Reimherr FW, Marchant BK, Kondo D, Lyon GJ, Olsen J, et al. The use of emotional dysregulation as an endophenotype for genetic studies in adults with attention-deficit hyperactivity disorder. J ADHD Relat Disord. (2010) 1:29–38.
104. Surman CB, Biederman J, Spencer T, Miller CA, Petty CR, Faraone SV. Neuropsychological deficits are not predictive of deficient emotional self-regulation in adults with ADHD. J Atten Disord. (2015) 19:1046–53. doi: 10.1177/1087054713476548
105. Wender PH. Attention-deficit hyperactivity disorder in adults. Psychiatric Clinic North America. (1998) 21:761–74. doi: 10.1016/S0193-953X(05)70039-3
106. Barkley RA. Attention-Deficit Hyperactivity Disorder: A Handbook For Diagnosis and Treatment. New York, NY: Guilford. (2015).
107. Brown TE. Brown Attention Deficit Disorder Scales. San Antonio: The Psychological Corporation (1996).
108. Conners CK, Erhard D, Sparrow D. Conners' Adult ADHD Rating Scales (CAARS). New York, NY: Multi-Healt Systems (1999).
109. Faraone SV, Rostain AL, Blader J, Busch B, Childress AC, Connor DF, et al. Practitioner Review: emotional dysregulation in attention-deficit/hyperactivity disorder–implications for clinical recognition and intervention. J Child Psychol Psychiatr. (2019) 60:133–50. doi: 10.1111/jcpp.12899
110. Beheshti A, Chavanon ML, Christiansen H. Emotion dysregulation in adults with attention deficit hyperactivity disorder: a meta-analysis. BMC Psychiatry. (2020) 20:1–11. doi: 10.1186/s12888-020-2442-7
111. Reimherr FW, Marchant BK, Strong RE, Hedges DW, Adler L, Spencer TJ, et al. Emotional dysregulation in adult ADHD and response to atomoxetine. Biol Psychiatry. (2005) 58:125–31. doi: 10.1016/j.biopsych.2005.04.040
112. Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry. (1991) 148:1647–58. doi: 10.1176/ajp.148.12.1647
113. Marchant BK, Reimherr FW, Robison D, Robison RJ, Wender PH. Psychometric properties of the wender-reimherr adult attention deficit disorder scale. Psychol Assess. (2013) 25:942. doi: 10.1037/a0032797
114. Chamberlain SR, Ioannidis K, Leppink EW, Niaz F, Redden SA, Grant JE. ADHD symptoms in non-treatment seeking young adults: relationship with other forms of impulsivity. CNS Spectr. (2017) 22:22–30. doi: 10.1017/S1092852915000875
115. Reimherr FW, Marchant BK, Gift TE, Steans TA. ADHD and anxiety: clinical significance and treatment implications. Curr Psychiatry Rep. (2017) 19:109. doi: 10.1007/s11920-017-0859-6
116. Stegmayer KDL, Horn HJ, Federspiel A, Razavi N, Bracht T, Wiest R, et al. Ventral striatum gray matter density reduction in schizophrenia patients with psychotic emotional dysregulation. Clinic EEG Neurosci. (2013) 44:E119. doi: 10.1016/j.nicl.2013.12.007
117. O'Driscoll C, Laing J, Mason O. Cognitive emotion regulation strategies, alexithymia and dissociation in schizophrenia, a review and meta-analysis. Clin Psychol Rev. (2014) 34:482–95. doi: 10.1016/j.cpr.2014.07.002
118. Liu J, Chua JJX, Chong SA, Subramaniam M, Mahendran R. The impact of emotion dysregulation on positive and negative symptoms in schizophrenia spectrum disorders: a systematic review. J Clin Psychol. (2020) 76:612–24. doi: 10.1002/jclp.22915
119. Nittel CM, Lincoln TM, Lamster F, Leube D, Rief W, Kircher T, et al. Expressive suppression is associated with state paranoia in psychosis: an experience sampling study on the association between adaptive and maladaptive emotion regulation strategies and paranoia. Br J Clinic Psychol. (2018) 57:291–312. doi: 10.1111/bjc.12174
120. Garety PA, Freeman D. The past and future of delusions research: from the inexplicable to the treatable. Br J Psychiatr. (2013) 203:327–33. doi: 10.1192/bjp.bp.113.126953
121. Morrison AP, Wells A. Relationships between worry, psychotic experiences and emotional distress in patients with schizophrenia spectrum diagnoses and comparisons with anxious and non-patient groups. Behav Res Ther. (2007) 45:1593–600. doi: 10.1016/j.brat.2006.11.010
122. Owens KA, Haddock G, Berry K. The role of the therapeutic alliance in the regulation of emotion in psychosis: an attachment perspective. Clinic Psychol Psychotherap. (2013) 20:523–30. doi: 10.1002/cpp.1793
123. Lincoln TM, Hartmann M, Köther U, Moritz S. Dealing with feeling: Specific emotion regulation skills predict responses to stress in psychosis. Psychiatry Res. (2015) 228:216–22. doi: 10.1016/j.psychres.2015.04.003
124. Bonfils KA, Minor KS, Leonhardt BL, Lysaker PH. Metacognitive self-reflectivity moderates the relationship between distress tolerance and empathy in schizophrenia. Psychiatry Res. (2018) 265:1–6. doi: 10.1016/j.psychres.2018.04.042
125. Henry JD, Green MJ, de Lucia A, Restuccia C, McDonald S, O'Donnell M. Emotion dysregulation in schizophrenia: reduced amplification of emotional expression is associated with emotional blunting. Schizophr Res. (2007) 95:197–204. doi: 10.1016/j.schres.2007.06.002
126. Seligowski AV, Lee DJ, Bardeen JR, Orcutt HK. Emotion regulation and posttraumatic stress symptoms: a meta-analysis. Cogn Behav Ther. (2015) 44:87–102. doi: 10.1080/16506073.2014.980753
127. Fitzgerald JM, DiGangi JA, Phan KL. Functional neuroanatomy of emotion and its regulation in PTSD. Harv Rev Psychiatry. (2018) 26:116. doi: 10.1097/HRP.0000000000000185
128. Clohessy S, Ehlers A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. Br J Clinic Psychol. (1999) 38:251–65. doi: 10.1348/014466599162836
129. Kumpula MJ, Orcutt HK, Bardeen JR, Varkovitzky RL. Peritraumatic dissociation and experiential avoidance as prospective predictors of posttraumatic stress symptoms. J Abnorm Psychol. (2011) 120:617. doi: 10.1037/a0023927
130. Frewen PA, Dozois DJ, Neufeld RW, Lane RD, Densmore M, Stevens TK, et al. Emotional numbing in posttraumatic stress disorder: a functional magnetic resonance imaging study. J Clin Psychiatry. (2011) 72:1. doi: 10.4088/JCP.10m06477
131. Litz BT, Litz BT, Gray MJ. Emotional numbing in posttraumatic stress disorder: Current and future research directions. Austral NZ J Psychiatr. (2002) 36:198–204. doi: 10.1046/j.1440-1614.2002.01002.x
132. Chopra MP, Zhang H, Kaiser AP, Moye JA, Llorente MD, Oslin DW, et al. PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. Am J Geriatric Psychiatr. (2014) 22:86–97. doi: 10.1016/j.jagp.2013.01.064
133. Kubzansky LD, Koenen KC, Spiro A, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. (2007) 64:109–16. doi: 10.1001/archpsyc.64.1.109
134. Powers A, Fani N, Cross D, Ressler KJ, Bradley B. Childhood trauma, PTSD, and psychosis: Findings from a highly traumatized, minority sample. Child Abuse & Neglect. (2016) 58:111–8.
135. Garnefski N, Teerds J, Kraaij V, Legerstee J, van Den Kommer T. Cognitive emotion regulation strategies and depressive symptoms: differences between males and females. Pers Individ Dif. (2004) 36:267–76. doi: 10.1016/S0191-8869(03)00083-7
136. Kraaij V, Garnefski N, de Wilde EJ, Dijkstra A, Gebhardt W, Maes S, et al. Negative life events and depressive symptoms in late adolescence: Bonding and cognitive coping as vulnerability factors? J Youth Adolesc. (2003) 32:185–93. doi: 10.1023/A:1022543419747
137. Dell'Osso L, Stratta P, Conversano C, Massimetti E, Akiskal KK, Akiskal HS, et al. Lifetime mania is related to post-traumatic stress symptoms in high school students exposed to the 2009 L'Aquila earthquake. Comprehen Psychiatr. (2014) 55:357–62. doi: 10.1016/j.comppsych.2013.08.017
138. Leible TL, Snell Jr WE. Borderline personality disorder and multiple aspects of emotional intelligence. Pers Individ Dif. (2004) 37:393–404. doi: 10.1016/j.paid.2003.09.011
139. Bornovalova MA, Gratz KL, Daughters SB, Nick B, Delany-Brumsey A, Lynch TR, et al. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. J Psychiatr Res. (2008) 42:717–26. doi: 10.1016/j.jpsychires.2007.07.014
140. Chapman AL, Leung DW, Lynch TR. Impulsivity and emotion dysregulation in borderline personality disorder. J Pers Disord. (2008) 22:148–64. doi: 10.1521/pedi.2008.22.2.148
141. Gunderson JG. Borderline personality disorder: a clinical guide. Am Psychiatric Pub. (2009) 12:1825. doi: 10.1176/appi.ajp.2009.08121825
142. Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. (2002) 159:276–83. doi: 10.1176/appi.ajp.159.2.276
143. Chiesa M, Martino F, Pozzi E. Psychosocial treatment refusal in personality disorder: a comparative study. Personal Ment Health. (2010) 4:64–74. doi: 10.1002/pmh.121
144. Martino F, Menchetti M, Pozzi E, Berardi D. Predictors of dropout among personality disorders in a specialist out-patients psychosocial treatment: a preliminary study. Psychiatry Clin Neurosci. (2012) 66:180–6. doi: 10.1111/j.1440-1819.2012.02329.x
145. Douzenis A, Tsopelas C, Tzeferakos G. Medical comorbidity of cluster B personality disorders. Curr Opin Psychiatry. (2012) 25:398–404. doi: 10.1097/YCO.0b013e3283558491
146. Martino F, Lia L, Bortolotti B, Menchetti M, Monari M, Ridolfi ME, et al. La famiglia del paziente con disturbo borderline di personalità: carico della malattia e interventi destinati ai caregiver. Riv Psichiatr. (2014) 49:199–206. doi: 10.1708/1668.18258
147. Links PS, Heslegrave R, Reekum RV. Impulsivity: core aspect of borderline personality disorder. J Pers Disord. (1999) 13:1–9. doi: 10.1521/pedi.1999.13.1.1
148. Sebastian A, Jacob G, Lieb K, Tüscher O. Impulsivity in borderline personality disorder: a matter of disturbed impulse control or a facet of emotional dysregulation?. Curr Psychiatr Rep. (2013) 15:339. doi: 10.1007/s11920-012-0339-y
149. Soloff PH, Lis JA, Kelly T, Cornelius JR, Ulrich R. Risk factors for suicidal behavior in borderline personality disorder. Am J Psychiatr. (1994) 4:257. doi: 10.1521/pedi.1994.8.4.257
150. Brodsky BS, Malone KM, Ellis SP, Dulit RA, Mann JJ. Characteristics of borderline personality disorder associated with suicidal behavior. Am J Psychiatry. (1997) 154:1715–9. doi: 10.1176/ajp.154.12.1715
151. Dougherty DM, Mathias CW, Marsh-Richard DM, Prevette KN, Dawes MA, Hatzis ES, et al. Impulsivity and clinical symptoms among adolescents with non-suicidal self-injury with or without attempted suicide. Psychiatry Res. (2009) 169:22–7. doi: 10.1016/j.psychres.2008.06.011
152. Herpertz S, Sass H, Favazza A. Impulsivity in self-mutilative behavior: psychometric and biological findings. J Psychiatr Res. (1997) 31:451–65. doi: 10.1016/S0022-3956(97)00004-6
153. Carli V, Jovanović N, Podlešek A, Roy A, Rihmer Z, Maggi S, et al. The role of impulsivity in self-mutilators, suicide ideators and suicide attempters—a study of 1,265 male incarcerated individuals. J Affect Disord. (2010) 123:116–22. doi: 10.1016/j.jad.2010.02.119
154. Rawlings J, Shevlin M, Corcoran R, Morriss R, Taylor PJ. Out of the blue: Untangling the association between impulsivity and planning in self-harm. J Affect Disord. (2015) 184:29–35. doi: 10.1016/j.jad.2015.05.042
155. Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, et al. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. Am J Psychiatry. (2004) 161:1296–8. doi: 10.1176/appi.ajp.161.7.1296
156. Tragesser SL, Solhan M, Schwartz-Mette R, Trull TJ. The role of affective instability and impulsivity in predicting future BPD features. J Pers Disord. (2007) 21:603–14. doi: 10.1521/pedi.2007.21.6.603
157. Glenn CR, Klonsky ED. Emotion dysregulation as a core feature of borderline personality disorder. J Pers Disord. (2009) 23:20–8. doi: 10.1521/pedi.2009.23.1.20
158. Stepp SD, Scott LN, Morse JQ, Nolf KA, Hallquist MN, Pilkonis PA. Emotion dysregulation as a maintenance factor of borderline personality disorder features. Compr Psychiatry. (2014) 55:657–66. doi: 10.1016/j.comppsych.2013.11.006
159. Klonsky ED. The functions of deliberate self-injury: a review of the evidence. Clin Psychol Rev. (2007) 27:226–39. doi: 10.1016/j.cpr.2006.08.002
160. Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and non-suicidal self-injury in women with borderline personality disorder. J Abnorm Psychol. (2002) 111:198. doi: 10.1037/0021-843X.111.1.198
161. Baer RA, Sauer SE. Relationships between depressive rumination, anger rumination, and borderline personality features. Personal Disord Theory Res Treat. (2011) 2:142. doi: 10.1037/a0019478
162. Selby EA, Joiner Jr TE. Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Rev General Psychol. (2009) 13:219–29. doi: 10.1037/a0015687
163. Chapman AL, Specht MW, Cellucci T. Borderline personality disorder and deliberate self-harm: does experiential avoidance play a role? Suicide Life-Threaten Behav. (2005) 35:388–99. doi: 10.1521/suli.2005.35.4.388
164. Rosenthal MZ, Cheavens JS, Lejuez CW, Lynch TR. Thought suppression mediates the relationship between negative affect and borderline personality disorder symptoms. Behav Res Ther. (2005) 43:1173–85. doi: 10.1016/j.brat.2004.08.006
165. Allen A, Links PS. Aggression in borderline personality disorder: evidence for increased risk and clinical predictors. Curr Psychiatry Rep. (2012) 14:62–9. doi: 10.1007/s11920-011-0244-9
166. Gardner KJ, Archer J, Jackson S. Does maladaptive coping mediate the relationship between borderline personality traits and reactive and proactive aggression? Aggress Behav. (2012) 38:403–13. doi: 10.1002/ab.21437
167. Newhill CE, Eack SM, Mulvey EP. A growth curve analysis of emotion dysregulation as a mediator for violence in individuals with and without borderline personality disorder. J Pers Disord. (2012) 26:452–67. doi: 10.1521/pedi.2012.26.3.452
168. Tragesser SL, Robinson RJ. The role of affective instability and UPPS impulsivity in borderline personality disorder features. J Pers Disord. (2009) 23:370–83. doi: 10.1521/pedi.2009.23.4.370
169. Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet. (2011) 377:74–84. doi: 10.1016/S0140-6736(10)61422-5
170. McMain S, Pos AE. Advances in psychotherapy of personality disorders: a research update. Curr Psychiatry Rep. (2007) 9:46–52. doi: 10.1007/s11920-007-0009-7
171. Martino F, Gammino L, Sanza M, Berardi D, Pacetti M, Sanniti A, et al. Impulsiveness and emotional dysregulation as stable features in borderline personality disorder outpatients over time. J Nerv Ment Dis. (2020) 208:715–20. doi: 10.1097/NMD.0000000000001204
172. Miano A, Grosselli L, Roepke S, Dziobek I. Emotional dysregulation in borderline personality disorder and its influence on communication behavior and feelings in romantic relationships. Behav Res Ther. (2017) 95:148–57. doi: 10.1016/j.brat.2017.06.002
173. Clifton A, Pilkonis PA. Evidence for a single latent class of diagnostic and statistical manual of mental disorders borderline personality pathology. Compr Psychiatry. (2007) 48:70–8. doi: 10.1016/j.comppsych.2006.07.002
174. Peters JR, Geiger PJ. Borderline personality disorder and self-conscious affect: Too much shame but not enough guilt? Personality Disorders: Theory, Research, and Treatment. (2016) 7:303.
175. Linehan M, Bohus M, Lynch T. How dialectical behavior therapy changes emotion dysregulation in borderline personality disorder. Eur Psychother. (2010) 9:141−66.
176. Carpenter RW, Trull TJ. Components of emotion dysregulation in borderline personality disorder: a review. Curr Psychiatry Rep. (2013) 15:1–8. doi: 10.1007/s11920-012-0335-2
177. Kröger C, Vonau M, Kliem S, Kosfelder J. Emotion dysregulation as a core feature of borderline personality disorder: comparison of the discriminatory ability of two self-rating measures. Psychopathology. (2011) 44:253–60. doi: 10.1159/000322806
178. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. (2010) 30:217–37. doi: 10.1016/j.cpr.2009.11.004
179. Klassen LJ, Katzman MA, Chokka P. Adult ADHD and its comorbidities, with a focus on bipolar disorder. J Affect Disord. (2010) 124:1–8. doi: 10.1016/j.jad.2009.06.036
180. Merwin RM, Moskovich AA, Wagner HR, Ritschel LA, Craighead LW, Zucker NL. Emotion regulation difficulties in anorexia nervosa: relationship to self-perceived sensory sensitivity. Cogn Emot. (2013) 27:441–52. doi: 10.1080/02699931.2012.719003
181. Bradley B, DeFife JA, Guarnaccia C, Phifer J, Fani N, Ressler KJ, et al. Emotion dysregulation and negative affect: association with psychiatric symptoms. J Clin Psychiatry. (2011) 72:0–0. doi: 10.4088/JCP.10m06409blu
Keywords: emotional dysregulation, affective dysregulation, adults, ADHD, ASD, emotion dysregulation
Citation: Carmassi C, Conti L, Gravina D, Nardi B and Dell'Osso L (2022) Emotional dysregulation as trans-nosographic psychopathological dimension in adulthood: A systematic review. Front. Psychiatry 13:900277. doi: 10.3389/fpsyt.2022.900277
Received: 20 March 2022; Accepted: 08 August 2022;
Published: 29 August 2022.
Edited by:
Maj Vinberg, University Hospital of Copenhagen, DenmarkReviewed by:
Maria Faurholt-Jepsen, Region Hovedstad Psychiatry, DenmarkCopyright © 2022 Carmassi, Conti, Gravina, Nardi and Dell'Osso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lorenzo Conti, bG9yZW56by5jb250aS50ZXJwQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.