
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 06 June 2022
Sec. Anxiety and Stress Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.899084
This article is part of the Research TopicCommunity Series in Interplay of Stress, Pain and Psychiatric Diseases - Volume IIView all 6 articles
 Joseph A. Boscarino1*
Joseph A. Boscarino1* Richard E. Adams2
Richard E. Adams2 Tiah J. Wingate2
Tiah J. Wingate2 Joseph J. Boscarino3
Joseph J. Boscarino3 Thomas G. Urosevich4
Thomas G. Urosevich4 Stuart N. Hoffman5
Stuart N. Hoffman5 H. Lester Kirchner1
H. Lester Kirchner1 Charles R. Figley6
Charles R. Figley6 William P. Nash7
William P. Nash7The impact of “moral injury” (MI) among deployed veterans, defined as actions in combat that violate a veteran's moral beliefs and result in psychological distress, has increasingly become a significant clinical concern separate from other trauma- and stressor-related disorders. MI involves severe distress over violations of core beliefs often followed by feelings of guilt and conflict and is common among veterans with PTSD. While the psychological impact of PTSD is well-documented among veterans, this has been done less so with respect to MI. We studied MI among 1,032 deployed veterans who were outpatients in a large non-profit multi-hospital system in central Pennsylvania. The study included active duty and Guard/Reserve members, as well as veterans who were not Department of Veterans Affairs (VA) service users. Our hypothesis was that, controlling for other risk factors, veterans with high MI would have current mental disorders. Our secondary hypothesis was that MI would be associated with other psychopathologies, including chronic pain, sleep disorders, fear of death, anomie, and use of alcohol/drugs to cope post deployment. Most veterans studied were deployed to Vietnam (64.1%), while others were deployed to post-Vietnam conflicts in Iraq and Afghanistan and elsewhere. Altogether, 95.1% of the veterans were male and their mean age was 61.6 years (SD = 11.8). Among the veterans, 24.4% had high combat exposure, 10.9% had PTSD, 19.8% had major depressive disorder, and 11.7% had a history of suicidal thoughts. Based on the Moral Injury Events Scale (MIES), 25.8% had high MI post deployment, defined as a score above the 75th percentile. Results show that high MI among veterans was associated with current global mental health severity and recent mental health service use, but not suicidal thoughts. In addition, as hypothesized, MI was also associated with pain, sleep disorders, fear of death, anomie, use of alcohol/drugs to cope post-deployment, and poor unit support/morale during deployment. Deployed veterans with MI are more likely to have current mental health disorders and other psychological problems years after deployment. Further research is advised related to the screening, assessment, treatment, and prevention of MI among veterans and others after trauma exposures.
In the current study, we examine the impact of “moral injury” (MI) among veterans, defined as the consequences of warzone exposures that violate the veteran's moral beliefs and result in severe psychological distress (1, 2). Consistent with earlier research (3), the objective of this study is to assess the post-deployment impact of moral injury among veterans, controlling for pre-deployment, deployment, and post-deployment risk factors. Given previous work (4, 5), our hypothesis was that moral injury would be associated with warzone exposures and the onset of mental health disorders and other psychopathology post-deployment. To assess this, we used a prediction models employed in past research (6–8). Our primary hypothesis is that MI would be associated with current mental health disorders, suicidal thoughts, mental health treatment, low self-esteem, among other risk factors, such as low unit deployment support (3, 7–10).
Our sample includes veterans from different conflicts recruited from non-VA community hospitals and include active-duty, Guard/Reserve, as well as former service members (3, 6, 8–10). We expected that veterans would have both risk and protective factors related to moral injury, including level of support, service history, among other factors (11, 12). This study is needed, since policy changes in the US have expanded access to care for veterans outside of the VA system (13). Understanding deployment-related risk factors among veterans is imperative for effective prevention and treatment of mental health disorders among veterans (6).
We note that while the concept of moral injury is still evolving, the traditional military model, the “combat stress” model, is that combat stress reactions occur following significant combat exposures, being taken prisoner of war, and/or following battlefield abandonment of service members (4). These experiences are often followed by feelings of guilt, despair, and in some cases character deterioration (1). Following the Vietnam War, however, the focus was on a trauma psychology model, which emphasized the impact of traumatic exposures, the onset and treatment of fear reactions, and emergence of a traumatic stress model (6, 9, 10). The traditional military model has been mostly focused management of psychological casualties in combat and the return of service members to active duty (4). The trauma model is grounded in psychoanalytic approach and is based on fear extinction and has focused on post deployment interventions, however, both models have merit. In addition, the earlier MI research focused on active-duty military personnel and VA patients using limited research measures (7). In the current study we used a valid and reliable MI scale (5), together with contemporary psychiatric instruments to assess MI among a large, diverse sample of veterans seen in community hospitals, where most veterans receive care (14, 15). Furthermore, research suggests moral injury may complicate PTSD treatment when present comorbidly, which is a clinical challenge (16, 17). Addressing MI among veterans is important because failing to treat this condition may cause greater harm post-deployment (1). Since the service branches typically support chaplaincy services, as do VA and Non-VA hospitals, this might be a practical yet effective intervention avenue if faith orientation is entangled in the moral conflict. While there is discussion on how best to assess MI (5), it clear that MI is a complex, multifactorial phenomenon associated with warzone exposures and clinicians should consider multiple resources to address this issue, including spiritual interventions, if needed. In addition, while our primary hypothesis is that MI is associated with current stress-related mental health disorders, we note that, based on past research (3, 6, 8, 9, 14), our secondary hypothesis is that MI will also be associated with a broad range of other psychopathologies, including sleep, substance misuse, pain, and neurotic disorders (9).
The population for the current study included a random sample of US military veterans (6, 8, 18). All veterans in the study were outpatients in the Geisinger Clinic, the largest private multi-hospital system in central Pennsylvania (3). In 2007, Geisinger initiated a registry for veterans receiving care at outpatient sites in Pennsylvania. Over 35,000 patients provided this information, and these data were used to select a random sample of veterans for the current study. Geisinger is an integrated health services organization that serves more than 3 million residents throughout 45 counties in central, south-central, and northeast Pennsylvania. This area encompasses a 40,000 square kilometer (25,000 square mile) service area (see: www.geisinger.org). The Geisinger system includes approximately 30,000 employees, 1,600 employed physicians, 10 hospital campuses, a 551,000-member managed care plan, a medical school, and is an open healthcare system that accepts all payor types, including private payors, public insurance (Medicare, Medicaid), Tricare, as well as payments for VA care.
Following patient consent, trained interviewers administered structured health interviews by telephone from February 2016 through February 2017, using a computer-assisted telephone interviewing (CATI) system by Sawtooth Technology (Northbrook Illinois, USA). During the survey, trained mental health counselors were available for the veterans, if required. All veterans for the current study had one or more warzone deployments. Veteran status and deployment history were confirmed based on military records. Among the veterans identified for the surveys, all were under 76 years old and served in Vietnam or a post-Vietnam conflict (i.e., Iraq, Afghanistan, Persian Gulf, or other recent conflict). After a total 10 telephone call attempts for each identified study veteran, we were able to complete interviews with 55% of eligible veterans in the study (3). Using demographic data in the electronic medical record, the only significant differences found between survey responders and non-responders were that responders tended to be younger and more often married (3).
To assess MI, we used the Moral Injury Events Scale (MIES) (5). The MIES is a validated scale with high reported internal validity (Cronbach's alpha = 0.90), concurrent validity, and discriminant validity (5). The MIES has nine items scored on a 6-point Likert scale (coded from “strongly agree” to “strongly disagree”), and included items such as, “I saw things that were morally wrong,” “I am troubled by having witnessed others' immoral acts.” Factor analyses revealed that the scale included two factors, explaining 64% of the common variance: perceived transgressions and perceived betrayals. In the current study, we combined this 9-item scale by summing each participant's responses to the item, with higher scores reflecting higher MI levels. The MI measure had an inter-quartile range of 3–19 (median = 10). Given the scale's skewed distribution, linear models, such as analysis of variance, are limited (19). Thus, we coded the MI scale both as a dichotomous variable classified as high vs, low MI, based on the 75th percentile and as an ordinal-level variable, coded in quintiles, representing low, moderate, high, very high and highest categories (19). For the dichotomous MI measure, we used logistic regression and for the ordinal-level variable we used ordinal logistic regression. These logistic regression models also included other independent variables as covariates, together with the stress exposures and personality measures noted (19). Goodness of fit statistics are also provided for all logistic regression models, including the area under the ROC curve, the Hosmer-Lemeshow χ2 statistic, and the McFadden Test (19).
Our study also included several mental health measures as dependent variables in estimating the association between MI and mental health status: These included the BSI-Anxiety and BSI-Global Severity scales, current depression, recent use of mental health services, and a single-item suicide ideation measure from the BSI (“Had thoughts of ending your life?”). The BSI-18 scales are based on self-report in the past 30 days and has been widely used in psychiatric research (20). The BSI scales are normalized and use a standardized score of 65 to define a case (21). The reliability and validity of these BSI scales are good (20–22). To assess PTSD, we used an instrument based on the Diagnostic and Statistical Manual of Mental Disorder, Fifth Edition (DSM-5), the PTSD Checklist for DSM-5 (23, 24). To receive a diagnosis of current PTSD, veterans had to meet the DSM-5 diagnostic criteria A through G. This PTSD scale has been used in several recent studies (25, 26) and is reported to be a valid and reliable PTSD scale (8) (Cronbach's alpha = 0.92).
Depression was assessed using a major depressive disorder scale based on the DSM-IV diagnostic criteria (27), which has been used in previous survey studies, including the National Woman's Study (NWS) among others (10, 28, 29) Data related to the validity of this depression scale were previously reported and suggest that this scale can be used to diagnose depression in community-based population studies (30) (Cronbach's alpha = 0.90). To meet criteria in the study, subjects had to meet the full criteria for major depressive disorder.
Use of mental health services was based on survey questions that asked about mental health treatments received in the past 12 months from mental health professionals, such as a psychiatrist, psychologist, social worker, mental health counselor, minister, etc., for problems with emotions or nerves or the use of alcohol or drugs. These mental health service questions were used and validated in past mental health research among both veterans and adult non-veterans (10, 20, 30).
Combat exposure was based on the Combat Experience Scale and versions of this measure have been used in studies since the Vietnam War (31–33). (Cronbach's alpha = 0.81). Based on previous research, scale measures for combat exposure were divided into standard cut-points (e.g., high vs. not high) that were used in previous research described elsewhere (3). Our study also assessed the occurrence of lifetime traumatic events using a traumatic event scale (e.g., ever experienced forced sexual contact, domestic abuse, a serious accident, major a disaster, etc.) used in previous research (20, 34). As we had no measure to judge the severity of these events, we collapsed these into three categories: <3 traumatic events, 3–5 events, and six or more events, as noted elsewhere (29). A total of 21% of respondents experienced six or more lifetime traumatic events in the current study and we used this to define “high” traumatic exposure as described in previous research (29, 30). Nearly 80% of the veterans in the current study reported that the most significant lifetime stressor they experienced was warzone exposure (3). This traumatic event scale was developed from other trauma studies, was also used in previous research, and had good reliability and validity (20, 29, 34). The study also included a measure of Adverse Childhood Events (ACE), a scale widely used in health research (35, 36). As done in previous research, we used a percentile cut-point to define a case (10).
We also assessed unit support, social support, homecoming support, self-esteem, and current life stressors, as these could have an impact on current health status (i.e., confounded with our independent and dependent variables) (3, 8, 37, 38). Social support, homecoming support, and current life stressors scales were based on previous research and had excellent reported reliability and validity (8, 37, 39). Additionally, in the survey we assessed current reported pain, reported health status in the past 12 months. In the survey, we also assessed “fear of death” (“afraid of news of death,” afraid you may die soon,” etc.) and “anomie” (i.e., social alienation, normlessness) (“a person does not know who to trust,” “the situation of the average person is getting worse,” etc.) both scales were coded “high” vs. “low” based on quartiles used in past research (Cronbach's alpha = 0.87 and 0.70, respectively) (40, 41). Additionally, we assessed the use of alcohol or drugs to cope since deployment based on the Brief Coping Scale, a widely used and validated instrument (10).
Furthermore, we included a measure of alcohol misuse using the CAGE scale, which assess alcohol dependence in the past 12 months. The CAGE scale is a widely used and validated measure of alcohol dependence symptoms (18, 42). Those who reported two or more symptoms in the past 12 months (e.g., “thought should cut down on drinking,” “criticized about drinking,” etc.) were classified as having probable alcohol dependence. Similarly, among those taking prescription opioids for pain in the past year, we assessed these patients for opioid use disorder using the Severity of Dependence Scale (SDS), a valid and reliable instatement used past research (43). We also assessed lifetime marijuana use (never used, some use, moderate use, heavy use), based previous research (43–45). Furthermore, our study included a valid measure of neurotic personality traits used in previous research (46), as well as a measure of antisocial personality (e.g., as a teenager, ever ran away from home, stole things, fought with parents, teachers, etc.) (47). Finally, our study included a survey measure of unit support/morale (categorized as high vs, low) that inquired about unit camaraderie, trust of others, leadership, and support during deployment based on the Deployment Risk and Resilience Inventory (Cronbach's alpha = 0.78) (48).
Given the predictors assessed, we based our analyses on previous conceptual models and empirical results and selected variables that reflected key demographics, military, stressful events, and personality factors (8, 49). We note that the main health outcomes assessed were based on the past 12 months (PTSD, depression, mental health service use, pain, sleep problems, etc.). However, the BSI scales used for anxiety, global severity, and suicidal thoughts were based on the past 30 days. We also note that the time fame used for the MI scale was based “since joining the military” and the timeframe for using alcohol/drugs to cope was based on “since deployment.”
Independent and study control variables in this research included age, gender, race, warzone deployments, being drafted, concussion history, Guard/Reserve status, and combat exposure, which were derived from the study survey measures (10, 14). Warzone exposures included the Vietnam War, Persian Gulf War, Afghanistan/Iraq War, and “other” recent warzone deployments, as defined by the VA. Global War on Terrorism (GWOT) veterans were combined with Iraq/Afghanistan veterans, since these deployments were during the same timeframe and were in supporting theaters of operations.
Moral Injury likely involves survivor guilt and other concerns, including spiritual and conceivably existential issues (50–54). Consequently, we would expect the psychosocial impact of MI to be long-lasting resulting in enduing personality, relationship, and self-concept changes (9, 54, 55).
Our statistical analyses included descriptive statistics depicting the study population and we present the characteristics of the total population for the current survey (N = 1,032) and we show these results in Table 1. Due to the questionnaire length and study timing, we split the interviews into two surveys, the original baseline survey and a second survey about 7–8 months later (N = 1,032) that included additional scales, based on veteran feedback and exploratory analyses related to potential MI psychopathology. We begin by presenting descriptive statistics and cross-tabulation results showing the association between high vs. low MI and both our independent and study control variables (Table 1). However, to assess the overall contribution of these measures in predicting post-deployment MI, we conducted logistic multivariate analyses (MVA) regressions using the stress, trauma, and symptom measures described to predict high vs. low MI (Table 2). In Table 3, we present the multivariate results for the health main health outcomes of interest, with MI score used as an ordinal quintile-level variable (scored 0–4; n = 202, n = 210, n = 205, n = 202, n = 213, respectively) in a stepwise logistic regression predicting current mental health status (56). To select these predictor variables, we used stepwise backwards logistic regression (57, 58), and compare these results to the stress process conceptual model in selecting candidate variables (3).
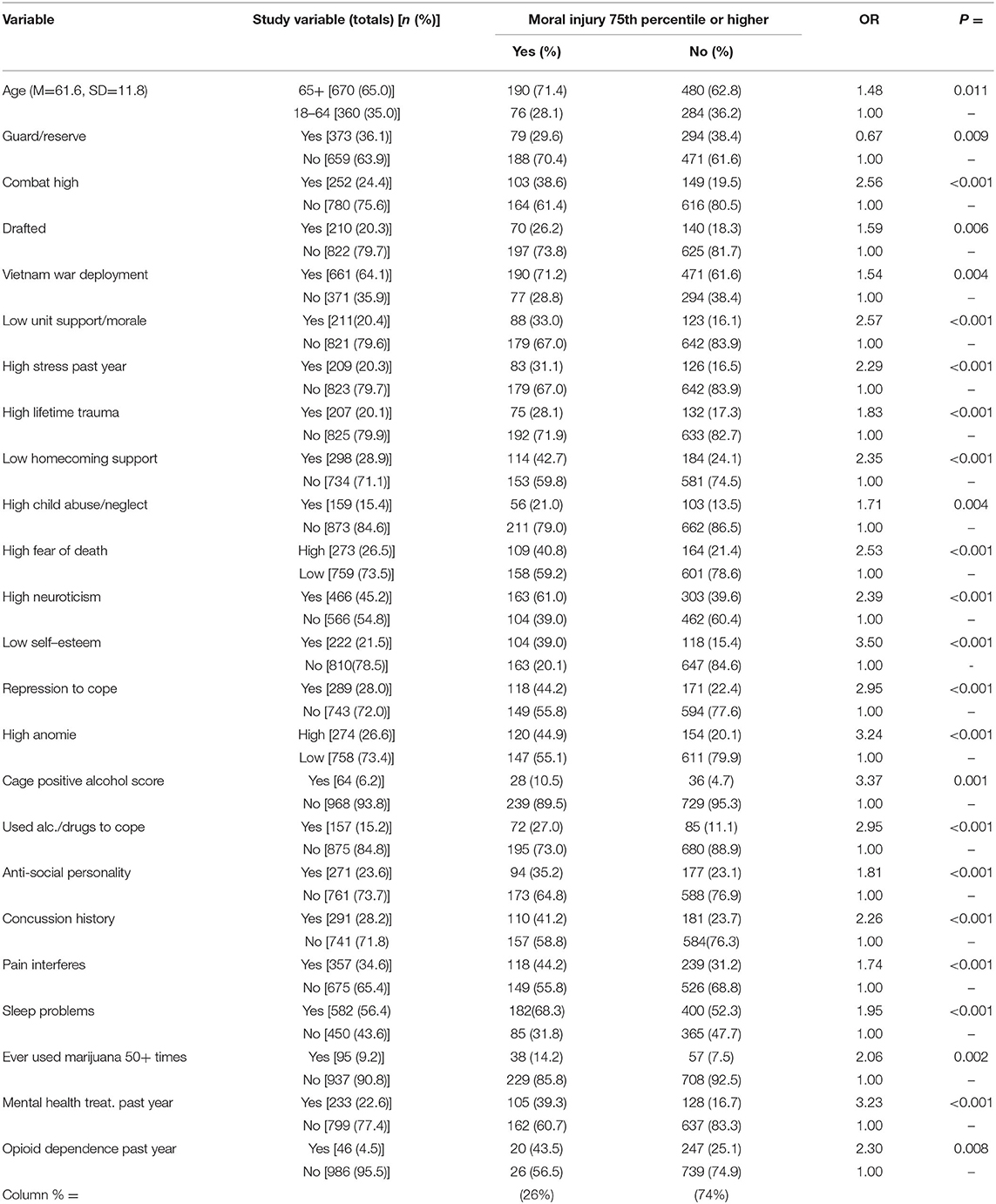
Table 1. High moral injury score vs. low score by study independent/control variables, based on Col. % (N = 1,032).
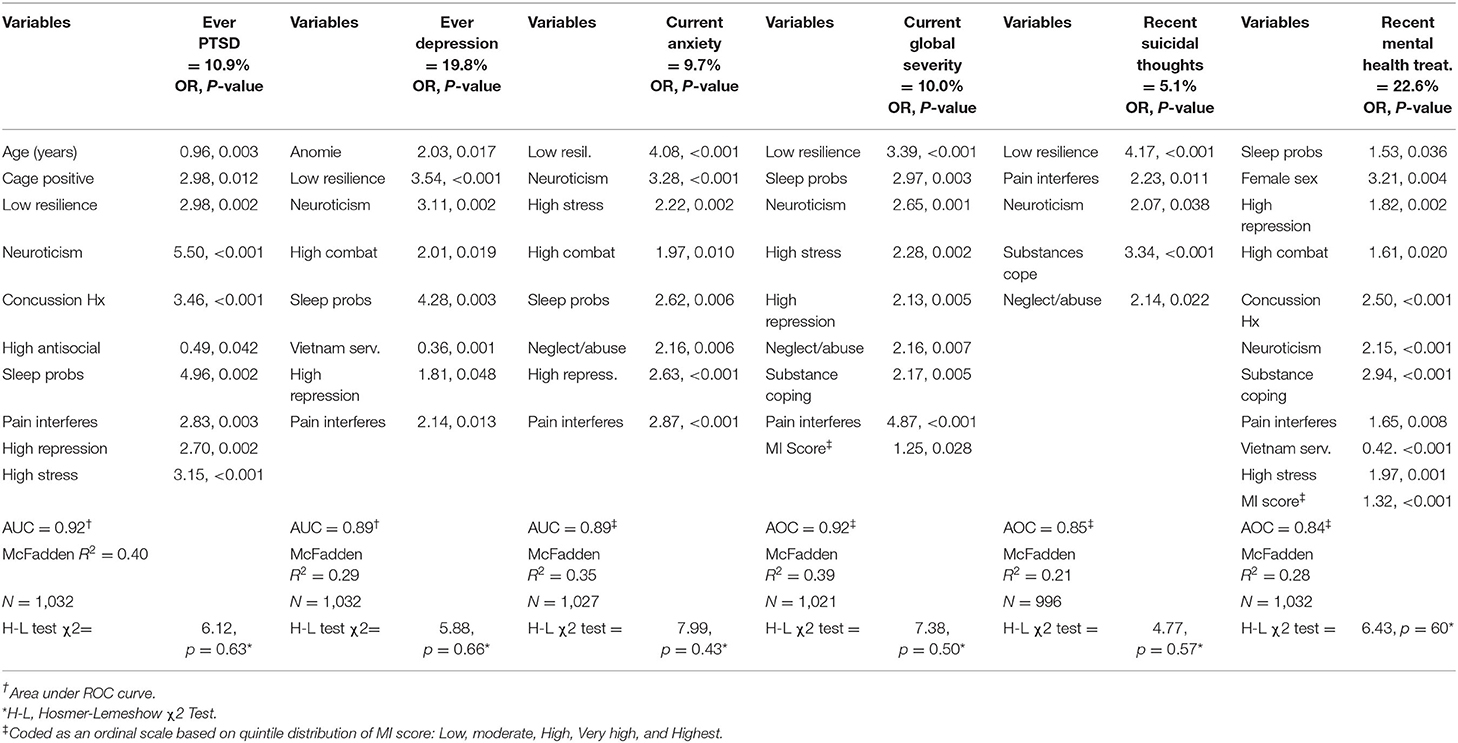
Table 3. Multivariable logistic regression odds ratios and p-values predicting PTSD, depression, anxiety, global severity, suicidal thoughts, and mental Health treatment among veterans from selected neuro-psychosocial predictor variables.
In the final regression models key risk/protective factors (e.g., lifetime trauma exposure, number of deployments, other stressors, and demographics) were entered, followed MI by including these variables in the regression model (Table 3). All variables in the final multivariable logistic models are included in the analyses shown in the table if they were <0.05 probability. However, due to the number of variables assessed in our study (see Table 1), we used a p-value <0.01 to define clinical significance in our study. Also, for brevity, we summarize the non-diagnostic symptom measures (e.g., anomie, pain, fear of death, sleep problems, anomie, etc.) in the results section showing the indicator variable with the more detailed (i.e., reference category) results are available from the study PI upon request (JAB). As a final check of our regression model, we also conducted an ordinal logistic MVA regression predicting MI as an original scale (coded none, low, moderate, very high, and highest) and describe these findings, with the detailed results provided upon request from the study PI (JAB). For predicting current PTSD, depression, and anxiety, we also assessed interaction effects for MI by recent mental health treatment and report these results (these results are available from the study PI, upon request). Finally, we used Cluster Analyses to confirm the symptoms identified in the regression models (59). We present these cluster results in Table 4. In the discussion section, we review these results as they relate to screening and care for veterans with possible MI. Statistical analyses were conducted using Stata, version 15.1 and SPSS, version 20 software (58, 60).
This study was approved by the Institutional Review Boards of the Geisinger Clinic (IRB # 2015-0441) and the US Department of Defense (IRB # A-18989). All patients provided their informed consent to participate in the study and were offered small monetary incentives for participation. The study data were also protected by a Certificate of Confidentiality (CoC) issued by the National Institutes of Health (NIH). This study was conducted in accordance with the principals stated in the Helsinki Declaration.
Most veterans surveyed were over 65 years old (65%) and male (95.5%). In addition, 64.1% served in Vietnam, with the remaining veterans having served in Iraq, Afghanistan, or the Global War on Terror (Table 1, column 2). In terms of potential mental health risk factors 37% served on multiple tour, 24.4% had high combat exposure, 20.1% had high lifetime trauma exposure, 20.3% had high life stress exposure in the past year, and 15.4% had a history childhood abuse/neglect (Table 1, column 2). An examination of the bivariate cross-tabulation results (Table 1, columns 5–6), suggest that high MI was associated with: being older (OR = 1.48, p = 0.011), having high combat exposure (OR = 2.56, p < 0.001), being drafted (OR = 1.59, p = 0.006), serving in Vietnam (OR = 1.54, p = 0.004), reporting low unit support during deployment (OR = 2.57, p < 0.001), having high life stress in past year (OR = 2.29, p < 0.001), having high lifetime trauma exposure (OR = 1.83, p < 0.001), reporting low homecoming support (OR = 2.35, p < 0.001), having a high fear of death (OR = 2.53, p < 0.001), having high neuroticism (OR = 2.39, p < 0.001), having low self-esteem (OR = 3.50, p < 0.001), using repression to cope post deployment (OR = 2.95, p < 0.001), having high anomie (OR = 3.24, p < 0.001), having alcohol dependence on the CAGE scale (OR = 3.37, p < 0.001), using alcohol/drugs to cope post deployment (OR = 2.95, p < 0.001), having opioid dependence on the SDS scale (OR = 2.30, p = 0.008), and having antisocial personality traits (OR = 1.81, p < 0.001). Conversely, serving in the National Guard/Reserve (OR = 0.67, p = 0.009) was related to lower MI scores. In addition, having an in-service concussion, current pain, sleep problems, and a history of heavy marijuana use were positively associated with having a high MI score (all p-values p <0.01) (Table 1, columns 5–6). Finally, having mental health treatment in the past year was also associated with high MI (OR = 3.23, p < 0.001).
Given these results, we also conducted a multivariable logistic regression predicting high vs. low MI score to discover the relative contributions of key variables and risk factors on MI symptom status. These results are shown in Table 2. As can be seen, several variables standout. These include low unit support/morale, high combat exposure, low self-esteem, high anomie, and fear of death (all p-values = or < than 0.01). The statistical fit for this regression appears is good, with an area under ROC = 0.78 and a Hosmer-Lemeshow χ2 test = 7.93, df = 8, p = 0.440 (Table 2). We note we also ran a logit prediction model with MI as a dependent ordinal variable (with MI coded as an ordinal variable: none, low, high, and very high) and the results were like Table 2, with a McFadden R2 = 0.094 [results available from study PI (JAB) upon request].
In multivariable analyses predicting mental health status [including, lifetime PTSD (10.9%), lifetime depression (19.8%), anxiety in the past month (9.7%), global mental health severity in the past month (10.0%), suicidal thoughts in the past month (5.1%), and mental health treatment in the past year (22.6%), are shown in (Table 3). Significant variables in these prediction models were low resilience, high neuroticism, sleep problems, pain, and high repression. We note that MI score in the MVA models was significant in predicting global severity and mental health treatment seeking with the other variables also in the model (Table 3). In addition, our cluster analyses results confirm these MVA model results (Table 4). As can be seen, in Table 4, Cluster One (n = 745) is associated with older veterans, Vietnam service, low homecoming support, but higher anomie. Conversely, Cluster Two (n = 287) is associated with younger veterans and having history of depression but is otherwise like Cluster One in terms of high neuroticism, low self-esteem, high repression, and current pain (Table 4).
Consistent with previous research (61), our hypothesis was that moral injuries among veterans would be associated with stress exposures, negative life events, and warzone exposure factors (8). As suggested, MI is a psychosocial construct, often involving fear, guilt, and for some spiritual issues (50–52). Consequently, we would expect the impact of this injury would be clinically significant, prompting the need for surveillance and ongoing research. This conclusion is supported by our results. MI is not only related to service experiences but also to interpersonal (e.g., low unit morale/support), and psychological factors (e.g., low self-esteem, high anomie, and higher fear of death). These associations are confirmed in the multivariate analysis predicting MI (Table 2), as well as in the Cluster Analysis (Table 4). The logistic regression models also suggest that high MI may be implicated in a variety of health outcomes. For example, higher MI was associated with global mental health severity, recent mental health service use, and substance misuse (Tables 2, 3). In summary, we found risk for MI among a community-based sample of veterans, including not only current mental health disorders, but the presence of a spectrum of psychopathology years after warzone deployments, including substance misuse. These variables may be important in identifying and screening veterans at risk for MI in different settings in the future. However, as suggested, no interaction effects were detected for recent treatments outcomes by MI, which is a good thing (7).
The current study has several strengths. First, we recruited a large random sample of community-based veterans. Second, we used validated scales and survey measures from previous research (3). Third, we included veterans from Vietnam through to current conflicts in Iraq and Afghanistan, something not typically done in veteran studies, but may be more representative of veterans overall (10). Fourth, we examined key post-deployment mental health outcomes and multiple risk factors using a valid and reliable scale furthering the utility of our MI scale.
Our study has several limitations, including that it was based on a cross-sectional survey. Because of this limitation, it is possible that some associations found in could be reversed (62), such that those with post-deployment mental health problems may have a more negative recall of different symptoms and other health-related outcomes. In addition, although our study was based on a large survey, the study was conducted among mostly Caucasian patients in a multi-hospital system located in central and northeastern Pennsylvania. Furthermore, we found some survey participation differences, whereby survey respondents tended to be younger and more often married (both p-values < 0.05), compared to non-respondents (10). This limitation may also apply to the second survey as well, since only 60% of veterans complete the latter. Thus, it may not be possible to generalize these findings to other study populations (62). As noted elsewhere, however, there are few robust samples of veterans available for research, since this population tends to be dynamic, given multiple deployments, ongoing conflicts, VA policy changes, fluctuations in service use, and the aging of the veteran population (3, 63, 64). In addition, most veterans do not consistently use the VA system for health care (65), which complicates using representative samples of veterans for population health research. Furthermore, given the number of variables, assessed, multiple comparisons may be an issue in our study, although we raised the “clinical significance” level to p < 0.01 to avoid this problem. Finally, another limitation is that the main study measure in the current study, combined a 9-item scale that had an inter-quartile range of 3–19 (median = 10), suggesting the distribution of scores derived from this measure was skewed. Because of this limitation, we used this scale as a dichotomous variable and as an ordinal scale (coded as quintile-level variable from “low” to “highest” score, respectively) in stepwise logistic regressions predicting current mental health status (56). To select these predictor variables, we used stepwise backwards logistic regression (57, 58), and compared these results to the stress process conceptual model in selecting candidate variables (3), and then compared these results to our Cluster Analysis results, which were both similar.
Despite these limitations, our findings are consistent with recent studies (6, 8). We suggest that services for returning veterans that target MI-specific risk factors post-deployment may result in better outcomes (7). The reasons why some veterans are at greater risk for MI is still unclear and may involve personality and moral value issues (18, 52), as well as factors related to sensory processing of stimuli (9, 66). As noted, MI is complicated and likely involves survivor's guilt and other issues related to perceived transgressions and perceived betrayals in combat (50, 51). Practical interventions could include mindfulness training, brief interventions, and other minimally invasive treatments, but further research is required (66–69). Adaptive disclosure (AD) is relatively recent intervention for active-duty service members (70). Noteworthy is that AD considers unique aspects of military service in war to address difficulties such as moral injury and traumatic loss that may not receive adequate attention by conventional treatments that primarily address fear-inducing experiences and their sequelae.
Moral injury is said to be a risk when there has been a betrayal of “what's right” either by a person in authority or by oneself, or in a high-stake situation (1). This can occur when a military unit is overrun forcing difficult choices to me made (1, 4). Clinical challenges in working with moral injury include coping with being made witness to atrocities and depravity through repeated exposure to trauma narratives, characteristic assignment of survivor's transference roles to clinicians, and the clinicians' countertransference emotions and judgments of self and others. A trustworthy clinical community and, particularly, a well-functioning clinical team provide protection for clinicians and are a major factor in successful outcomes with morally injured combat veterans (1).
However, following deployments, most veterans return to local communities and are typically seen in non-government facilities (71), complicating their psychological and emotional care. Therefore, providers in non-VA settings need to be aware of the potential impact moral injury and PTSD among veterans (15, 72), as well as the potential significance of “veteran identity” in the recovery process (61) The concept of moral injury may help clinicians gauge exposure to traumatic events that contradict the veterans' deeply held moral beliefs, which, may result in disordered thinking and mental illness among veterans' years afterwards. As we have shown, high combat exposure, history of other trauma exposures, high current life stressor, low self-esteem, and poor unit support/morale are also associated with moral injury. Furthermore, having a high fear of death, anomie, and neurotic personality traits are also associated with MI, as well as increased pain, sleep problems, and growing evidence of substance abuse involving misuse of both alcohol and drugs. Further research is warranted building from the current study and others. With the ending of the post-9/11 combat era and with state-sponsored terrorism diminishing, concurrent with a renewed focus on conventional warfighting, battlefield stress management, unit morale, and return of service members to their original units (4), may be the future emphasis in military combat medicine. Time will tell.
The datasets presented in this article are not readily available because these data are still being analyzed by the study team. Requests to access the datasets should be directed to JAB, amFib3NjYXJpbm9AZ2Vpc2luZ2VyLmVkdQ==; am9zZXBoLmJvc2Nhcmlub0BnbWFpbC5jb20=.
This study was approved by the Institutional Review Boards of the Geisinger Clinic (IRB # 2015-0441) and the US Department of Defense (IRB # A-18989). This study was conducted in accordance with the principals stated in the Helsinki Declaration. The patients/participants provided their written informed consent to participate in this study.
JAB was responsible for study funding, research design, and drafting the first version of the manuscript. JJB, RA, and TW assisted with analysis and manuscript writing. HK provided statistical consulting. WN and CF provided clinical consultations related to mortal injury. All the authors reviewed and approved the manuscript.
Funding was provided by: Geisinger Auxiliary Fund, the Kline & Ditty Health Fund (#752109 & #762170), National Institute of Mental Health (Grant No. R21-MH-086317), Wounded Warrior Project, and the Department of Defense (Contract No. W81XWH-15-1-0506) to JAB. The sponsors had no role in the analysis, writing, or submission of the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The study PI also acknowledges the impact his brother, a US Army Vietnam combat veteran, had on his thinking on moral injury, which compelled him to conduct this research. The study PI also acknowledges the valuable input of Dr. William P. Nash in this research. A version of this paper was presented at the Health Care Systems Research Network Conference, Pasadena, CA, April 13, 2022.
2. Currier JM, Holland JM, Drescher K, Foy D. Initial psychometric evaluation of the Moral Injury Questionnaire–Military version. Clin Psychol Psychother. (2015) 22:54–63. doi: 10.1002/cpp.1866
3. Boscarino JA, Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Boscarino JJ, et al. Mental health impact of homecoming experience among 1730 formerly deployed veterans from the Vietnam war to current conflicts: results from the veterans' health study. J Nerv Ment Dis. (2018) 206:757–64. doi: 10.1097/NMD.0000000000000879
4. Jones FD, Sparacino LR, Wilcox VL, Rothberg JM, Stokes JM. Textbook of Miliary Medicine: War Psychiatry. Falls Church, VA: Office of the Surgeon General, United States Army.
5. Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz BT. Psychometric evaluation of the Moral Injury Events Scale. Mil Med. (2013) 178:646–52. doi: 10.7205/MILMED-D-13-00017
6. Boscarino JA, Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Dugan RJ, et al. Guard/Reserve service members and mental health outcomes following deployment: results from the Veterans' Health Study. Gen Hosp Psychiatry. (2020) 62:102–3. doi: 10.1016/j.genhosppsych.2019.03.002
7. Koenig HG, Youssef NA, Pearce M. Assessment of moral injury in veterans and active duty military personnel with PTSD: a review. Front Psychiatry. (2019) 10:443. doi: 10.3389/fpsyt.2019.00443
8. Hu Y, Chu X, Urosevich TG, Hoffman SN, Kirchner HL, Adams RE, et al. Predictors of current DSM-5 PTSD diagnosis and symptom severity among deployed veterans: significance of predisposition, stress exposure, and genetics. Neuropsychiatr Dis Treat. (2020) 16:43–54. doi: 10.2147/NDT.S228802
9. Hoffman SN, Urosevich TG, Kirchner HL, Boscarino JJ, Dugan RJ, Withey CA, et al. Grapheme-color synesthesia is associated with PTSD among deployed veterans: confirmation of previous findings and need for additional research. Int J Emerg Ment Health. (2019) 21:1–6.
10. Boscarino JA, Hoffman SN, Pitcavage JM, Urosevich TG. Mental health disorders and treatment seeking among veterans in non-VA facilities: results and implications from the veterans' health study. Mil Behav Health. (2015) 3:244–54. doi: 10.1080/21635781.2015.1077179
11. Bryan CJ, Hernandez AM. The functions of social support as protective factors for suicidal ideation in a sample of air force personnel. Suicide Life Threat Behav. (2013) 43:562–73. doi: 10.1111/sltb.12039
12. MacDermott D. Psychological hardiness and meaning making as protection against sequelae in veterans of the wars in Iraq and Afghanistan. Int J Emerg Ment Health. (2010) 12:199–206.
13. Stroupe KT, Martinez R, Hogan TP, Gordon EJ, Gonzalez B, Kale I, et al. Experiences with the veterans' choice program. J Gen Intern Med. (2019) 34:2141–9. doi: 10.1007/s11606-019-05224-y
14. Boscarino JJ, Figley CR, Adams RE, Urosevich TG, Kirchner HL, Boscarino JA. Mental health status in veterans residing in rural versus non-rural areas: results from the veterans' health study. Mil Med Res. (2020) 13:861–8. doi: 10.1186/s40779-020-00272-6
15. Boscarino JA, Larson S, Ladd I, Hill E, Paolucci SJ. Mental health experiences and needs among primary care providers treating OEF/OIF veterans: preliminary findings from the Geisinger Veterans Initiative. Int J Emerg Ment Health. (2010) 12:161.
16. Held P, Klassen BJ, Steigerwald VL, Smith DL, Bravo K, Rozek DC, et al. Do morally injurious experiences and index events negatively impact intensive PTSD treatment outcomes among combat veterans? Eur J Psychotraumatol. (2021) 12:1877026. doi: 10.1080/20008198.2021.1877026
17. Griffin BJ, Purcell N, Burkman K, Litz BT, Bryan CJ, Schmitz M, et al. Moral injury: an integrative review. J Trauma Stress. (2019) 32:350–62. doi: 10.1002/jts.22362
18. Adams RE, Boscarino JA, Hoffman SN, Urosevich TG, Kirchner HL, Boscarino JJ, et al. Psychological well-being and alcohol misuse among community-based veterans: results from the Veterans' Health Study. J Addict Dis. (2022) 40:217–26. doi: 10.1080/10550887.2021.1972747
19. Long JS, Freese J. Regression Models for Categorical Dependent Variables Using Stata. 3rd ed. College Station, TX: Stata Press (2014).
20. Boscarino JA, Adams RE, Figley CR. Mental health service use 1-year after the World Trade Center disaster: implications for mental health care. Gen Hosp Psychiatry. (2004) 26:346–58. doi: 10.1016/j.genhosppsych.2004.05.001
21. Derogatis L. Brief Symptom Inventory 18 (BSI-18) Manual. Minnetonka, MN: NCS Assessments (2001).
22. Adams RE, Boscarino JA. Differences in mental health outcomes among Whites, African Americans, and Hispanics following a community disaster. Psychiatry. (2005) 68:250–65. doi: 10.1521/psyc.2005.68.3.250
23. Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol Assess. (2016) 28:1379. doi: 10.1037/pas0000254
24. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. (2015) 28:489–98. doi: 10.1002/jts.22059
25. Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. (2016) 28:1392. doi: 10.1037/pas0000260
26. Cox KS, Resnick HS, Kilpatrick DG. Prevalence and correlates of posttrauma distorted beliefs: evaluating DSM-5 PTSD expanded cognitive symptoms in a national sample. J Trauma Stress. (2014) 27:299–306. doi: 10.1002/jts.21925
27. Spitzer RL, Williams JB, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID): I: history, rationale, and description. Arch Gen Psychiatry. (1992) 49:624–9. doi: 10.1001/archpsyc.1992.01820080032005
28. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. (1993) 61:984. doi: 10.1037/0022-006X.61.6.984
29. Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, et al. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. (2002) 346:982–7. doi: 10.1056/NEJMsa013404
30. Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatr Serv. (2004) 55:274–83. doi: 10.1176/appi.ps.55.3.274
31. Centers for Disease Control. Health status of Vietnam veterans. I. Psychosocial characteristics. The Centers for Disease Control Vietnam Experience Study. JAMA. (1988) 259:2701–7. doi: 10.1001/jama.259.18.2701
32. Boscarino JA, Forsberg CW, Goldberg JA. twin study of the association between PTSD symptoms and rheumatoid arthritis. Psychosom Med. (2010) 72:481–6. doi: 10.1097/PSY.0b013e3181d9a80c
33. McLeod DS, Koenen KC, Meyer JM, Lyons MJ, Eisen S, True W, et al. Genetic and environmental influences on the relationship among combat exposure, posttraumatic stress disorder symptoms, and alcohol use. J Trauma Stress. (2001) 14:259–75. doi: 10.1023/A:1011157800050
34. Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consult Clin Psychol. (2003) 71:692. doi: 10.1037/0022-006X.71.4.692
35. Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. (2004) 82:217–25. doi: 10.1016/j.jad.2003.12.013
36. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
37. Adams RE, Hu Y, Figley CR, Urosevich TG, Hoffman SN, Kirchner HL, et al. Risk and protective factors associated with mental health among female military veterans: results from the veterans' health study. BMC Womens Health. (2021) 21:55. doi: 10.1186/s12905-021-01181-z
38. Sinclair SJ, Blais MA, Gansler DA, Sandberg E, Bistis K, LoCicero A. Psychometric properties of the Rosenberg Self-Esteem Scale: overall and across demographic groups living within the United States. Eval Health Prof. (2010) 33:56–80. doi: 10.1177/0163278709356187
39. Daida YG, Boscarino JA, Moorman AC, Lu M, Rupp LB, Gordon SC, et al. Mental and physical health status among chronic hepatitis B patients. Qual Life Res. (2020) 29:1567–77. doi: 10.1007/s11136-020-02416-6
40. Adams RE, Boscarino JA. Volunteerism and well-being in the context of the world trade center terrorist attacks. Int J Emerg Ment Health. (2015) 17:274–82. doi: 10.4172/1522-4821.1000158
41. Boscarino JA, Adams RE, Figley CR, Galea S, Foa EB. Fear of terrorism and preparedness in New York City 2 years after the attacks: implications for disaster planning and research. J Public Health Manag Pract. (2006) 12:505. doi: 10.1097/00124784-200611000-00002
42. O'Brien CP. The CAGE questionnaire for detection of alcoholism. JAMA. (2008) 300:2054–6. doi: 10.1001/jama.2008.570
43. Boscarino JA, Withey CA, Dugan RJ, Hu Y, Auciello J, Alfieri T. Opioid medication use among chronic non-cancer pain patients assessed with a modified drug effects questionnaire and the association with opioid use disorder. J Pain Res. (2020) 13:2697–705. doi: 10.2147/JPR.S275397
44. Vlahov D, Galea S, Ahern J, Resnick H, Boscarino JA, Gold J, et al. Consumption of cigarettes, alcohol, and marijuana among New York City residents six months after the September 11 terrorist attacks. Am J Drug Alcohol Abuse. (2004) 30:385–407. doi: 10.1081/ADA-120037384
45. Boscarino JA, Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Chu X, et al. Genetic and psychosocial risk factors associated with suicide among community veterans: implications for screening, treatment and precision medicine. Pharmgenomics Pers Med. (2022) 15:17–27. doi: 10.2147/PGPM.S338244
46. Gosling SD, Rentfrow PJ, Swann Jr WBA. very brief measure of the Big-Five personality domains. J Res Pers. (2003) 37:504–28. doi: 10.1016/S0092-6566(03)00046-1
47. Boscarino JA, Rukstalis M, Hoffman SN, Han JJ, Erlich PM, Gerhard GS, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction. (2010) 105:1776–82. doi: 10.1111/j.1360-0443.2010.03052.x
48. Vogt D, Smith BN, King LA, King DW, Knight J, Vasterling JJ. Deployment risk and resilience inventory-2 (DRRI-2): an updated tool for assessing psychosocial risk and resilience factors among service members and veterans. J Trauma Stress. (2013) 26:710–7. doi: 10.1002/jts.21868
49. Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Hyacinthe JC, Figley CR, et al. Social support, help-seeking, and mental health outcomes among veterans in non-VA facilities: results from the veterans' health study. Mil Behav Health. (2017) 5:393–405. doi: 10.1080/21635781.2017.1333067
50. Murray H, Pethania Y, Medin E. Survivor guilt: a cognitive approach. Cogn Behav Therap. (2021) 14:e28. doi: 10.1017/S1754470X21000246
51. Boska RL, Capron DW. Exploring the maladaptive cognitions of moral injury within a primarily combat-trauma military sample. Psychol Trauma. (2021) 13:861–8. doi: 10.1037/tra0001071
52. Nazarov A, Jetly R, McNeely H, Kiang M, Lanius R, McKinnon MC. Role of morality in the experience of guilt and shame within the armed forces. Acta Psychiatr Scand. (2015) 132:4–19. doi: 10.1111/acps.12406
53. Yeterian JD, Berke DS, Carney JR, McIntyre-Smith A, St Cyr K, King L, et al. Defining and measuring moral injury: rationale, design, and preliminary findings from the moral injury outcome scale consortium. J Trauma Stress. (2019) 32:363–72. doi: 10.1002/jts.22380
54. Letica-Crepulja M, Stevanovic A, Protuder M, Grahovac Juretic T, Rebic J, Franciskovic T. Complex PTSD among treatment-seeking veterans with PTSD. Eur J Psychotraumatol. (2020) 11:1716593. doi: 10.1080/20008198.2020.1716593
55. Maercker A. Development of the new CPTSD diagnosis for ICD-11. Borderline Personal Disord Emot Dysregul. (2021) 8:7. doi: 10.1186/s40479-021-00148-8
57. Hosmer DW, Lemeshow S, Cook E. Applied Logistic Regression. 2nd ed. New York, NY: John Wiley & Sons (2000).
58. IBM Corporation. IBM SPSS. Statistics 20 Command Syntax Reference. Armonk, NY: IBM Corporation (2011).
59. Fisher S, Stevens RF. Subgroups of frequent users of an inpatient mental health program at a community hospital in Canada. Psychiatr Serv. (1999) 50:244–7. doi: 10.1176/ps.50.2.244
61. Adams RE, Urosevich TG, Hoffman SN, Kirchner HL, Figley CR, Withey CA, et al. Social and psychological risk and protective factors for veteran well-being: the role of veteran identity and its implications for intervention. Mil Behav Health. (2019) 7:304–14. doi: 10.1080/21635781.2019.1580642
62. Hulley S, Cummings S, Browner W, Grady D, Newman T. Designing Clinical Research. Philadelphia, PA; Baltimore, NY; London, Buenos Aires; Hong Kong: Lippincott Williams (2013).
63. Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn M, et al. Veterans' access to and use of medicare and veterans affairs health care. Med Care. (2007) 45:214–23. doi: 10.1097/01.mlr.0000244657.90074.b7
64. Ritchie EC, Llorente MD. Veteran Psychiatry in the US: Optimizing Clinical Outcomes. Cham, Switzerland: Springer (2019).
65. Dursa EK, Barth SK, Bossarte RM, Schneiderman AI. Demographic, military, and health characteristics of VA health care users and nonusers who served in or during operation enduring freedom or operation Iraqi Freedom, 2009-2011. Public Health Rep. (2016) 131:839–43. doi: 10.1177/0033354916676279
66. Gennaro RJ. Synesthesia, hallucination, and autism. Front Biosci. (2021) 26:797–809. doi: 10.2741/4918
67. Interian A, Chesin MS, Stanley B, Latorre M, St Hill LM, Miller RB, et al. Mindfulness-based cognitive therapy for preventing suicide in military veterans: a randomized clinical trial. J Clin Psychiatry. (2021) 82:20m13791. doi: 10.4088/JCP.20m13791
68. Shapiro F. The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. Perm J. (2014) 18:71–7. doi: 10.7812/TPP/13-098
69. Bergen-Cico D, Possemato K, Pigeon W. Reductions in cortisol associated with primary care brief mindfulness program for veterans with PTSD. Med Care. (2014) 52 (12 Suppl. 5):S25–31. doi: 10.1097/MLR.0000000000000224
70. Gray MJ, Schorr Y, Nash W, Lebowitz L, Amidon A, Lansing A, et al. Adaptive disclosure: an open trial of a novel exposure-based intervention for service members with combat-related psychological stress injuries. Behav Ther. (2012) 43:407–15. doi: 10.1016/j.beth.2011.09.001
71. Urosevich TG, Boscarino JJ, Hoffman SN, Kirchner HL, Figley CR, Adams RE, et al. Visual dysfunction and associated co-morbidities as predictors of mild traumatic brain injury seen among veterans in non-VA facilities: implications for clinical practice. Mil Med. (2018) 183:e564–70. doi: 10.1093/milmed/usy102
Keywords: veterans, moral injury, PTSD, depression, pain, substance misuse, fear of death, unit support
Citation: Boscarino JA, Adams RE, Wingate TJ, Boscarino JJ, Urosevich TG, Hoffman SN, Kirchner HL, Figley CR and Nash WP (2022) Impact and Risk of Moral Injury Among Deployed Veterans: Implications for Veterans and Mental Health. Front. Psychiatry 13:899084. doi: 10.3389/fpsyt.2022.899084
Received: 18 March 2022; Accepted: 12 May 2022;
Published: 06 June 2022.
Edited by:
Emre Umucu, Michigan State University, United StatesReviewed by:
Laura E. Watkins, Emory University, United StatesCopyright © 2022 Boscarino, Adams, Wingate, Boscarino, Urosevich, Hoffman, Kirchner, Figley and Nash. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph A. Boscarino, amFib3NjYXJpbm9AZ2Vpc2luZ2VyLmVkdQ==; am9zZXBoLmJvc2Nhcmlub0BnbWFpbC5jb20=; orcid.org/0000-0002-9965-6805
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.