- 1School of Rehabilitation, Gannan Medical University, Ganzhou, China
- 2Department of Rehabilitation Medicine, YueBei People's Hospital, Shaoguan, China
Background: Sleep efficiency of <80% based on actigraphy was defined as insomnia as self-reported difficulty falling asleep or waking up at night three to four times per week. It is known that adequate sleep is very important for human wellbeing, affecting people's work and life, insomnia will seriously damage our daily life. There is no recognized non-drug treatment. Studies have found that Taijiquan has a positive effect on insomnia patients. This systematic review and meta-analysis will evaluate the effect of Taijiquan on insomnia.
Methods: To find all randomized controlled trials exploring the effects of Taijiquan on insomnia patients in Chinese and English, eight databases (Pubmed, Embase, Cochrane library, Web of Science, CNKI, CBM, VIP, and Wanfang Data) were searched. The retrieval time is from database construction to October 2021. Searches were conducted in both English and Chinese language. A meta-analysis by mean difference (MD) and 95% confidence interval (CI) was performed with RevMan 5.3. The risk of bias for each study was accounted for according to the Cochrane Handbook. Our primary outcome was Pittsburg Sleep Quality Index. We explored sources of heterogeneity by comparing effect sizes across different types of etiology, country, control group, and intervention type. The protocol was pre-registered with PROSPERO, CRD42021284511.
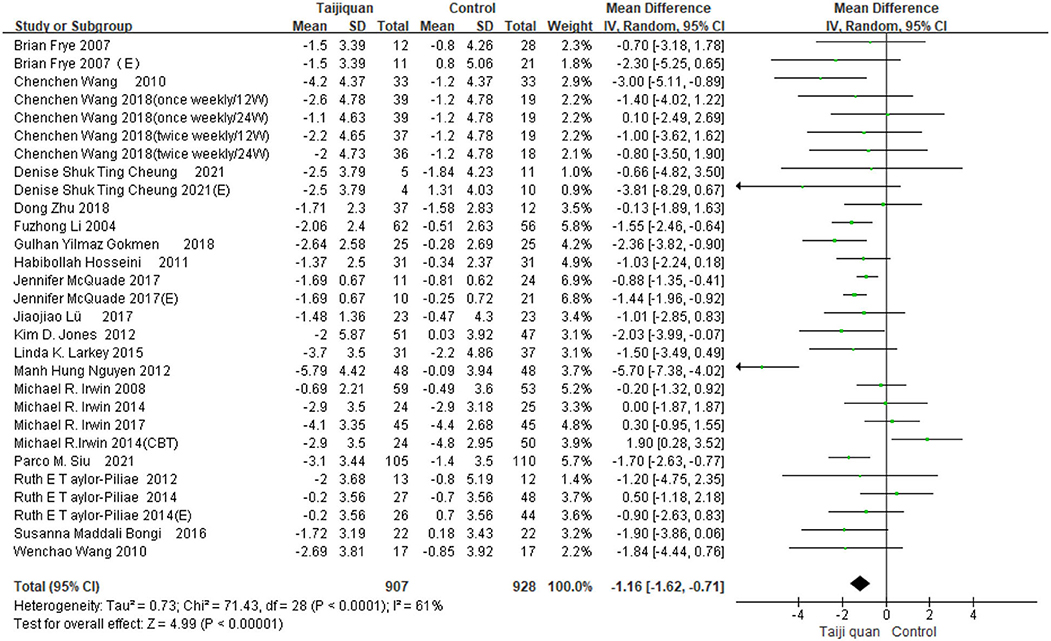
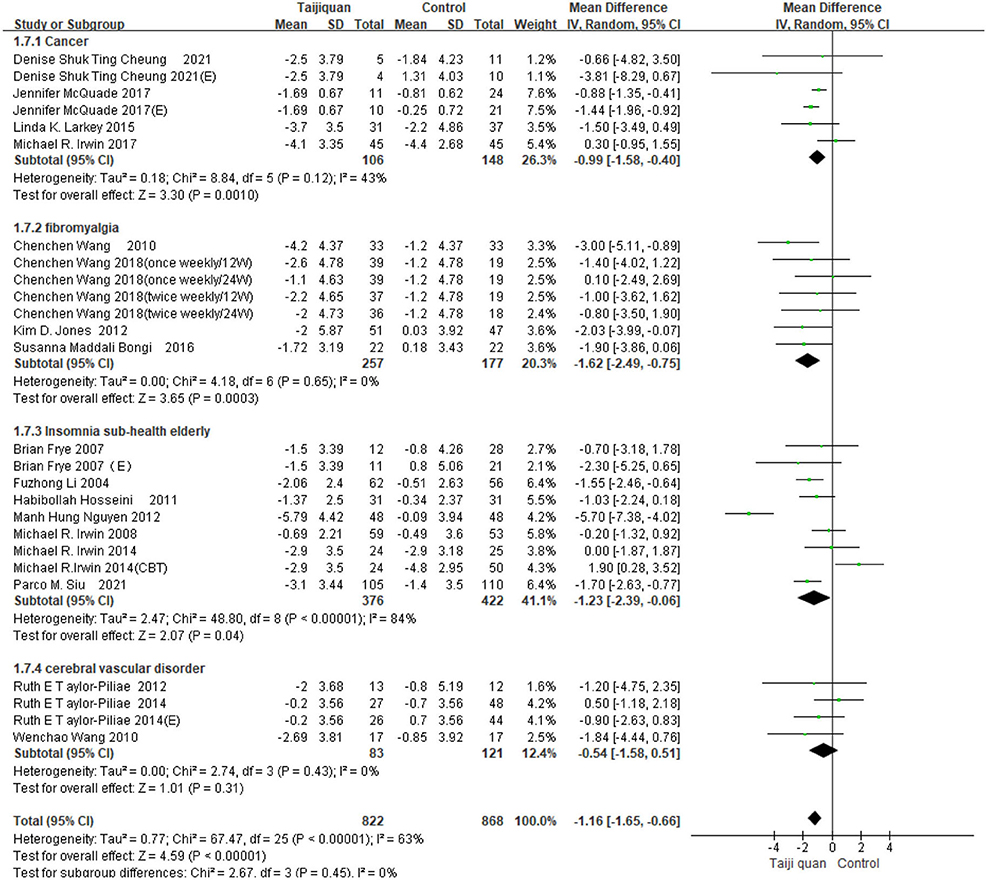
Results: Twenty-one RCTs published between 2004 and 2021 with 2,022 participants were included in this study. Twenty-one randomized controlled studies showed that Tai Chi significantly improved PSQI scores in patients with cancer, muscle fibrosis, and sub-health insomnia [MD = −1.16, 95% CI (−1.62, −0.71), P < 0.01]; There is insufficient evidence of improvement in patients with cerebrovascular disease [MD = −0.54, 95% CI (−1.58, 0.51), P = 0.31]; 8-form, 10-form or 24-form Yang's Taijiquan had the same effect in improving PSQI [MD = −1.33, 95% CI (−1.85, −0.81), P < 0.01]. When there is no treatment, exercise, exercise and health education as the control, taijiquan has a significant effect on insomnia treatment, and there is no difference in efficacy compared with cognitive behavioral therapy and health education (usual care) alone.
Conclusions: The results of the study showed that Taijiquan significantly improved sleep quality in healthy adults and patients with chronic diseases, which suggests that Taijiquan may be considered as an alternative behavioral therapy in the treatment of insomnia. In the future, more high-quality, well-controlled randomized trials are needed to better inform clinical decisions.
Introduction
Insomnia is very common in the population, which is characterized by difficulty starting or maintaining sleep, along with symptoms such as irritability or fatigue when awake (1). Adequate sleep is very important for human health, affecting people's work and life, while insomnia will seriously affect our daily life. Insomnia is defined in the fifth edition of the Diagnostic and statistical manual of mental disorders (DSM-5) as difficulty getting to sleep, staying asleep, or having non-restorative sleep despite having the adequate opportunity for sleep, together with associated impairment of daytime functioning, with symptoms being present for at least 4 weeks (2). Around the world, 15–30% of adults and 10% of adolescents suffer from some form of insomnia (3, 4). Insomnia has a great impact on the human body (1, 5, 6), first of all, insomnia will make the human immune decline, weakened resistance to various diseases. Long-term insomnia can cause high blood pressure, heart disease, high blood fat, senile dementia, and so on. Secondly, patients with long-term insomnia are easy to cause negative effects in mental aspects, such as inattention, decreased thinking ability, anxiety, depression, mental tension and other emotions, cerebral cortex dysfunction, causing plant neurological dysfunction, serious forms of psychosis, neurosis, and so on.
At present, the treatment methods for insomnia mainly include drug therapy (7), cognitive behavioral therapy (8), exercise therapy (9), mindfulness meditation (10), and traditional Chinese acupuncture therapy (11), etc. But these treatments have some limitations, no matter western medicine or Traditional Chinese medicine, the current treatment of insomnia is mainly drugs, but drugs have addictions, adverse reactions, or unstable compatibility, there are individual differences in curative effect (12) and the use of drugs like doxepin, ramelteon, and secobarbital is increasingly being discouraged due to their potential toxicity. According to the European insomnia guidelines, cognitive-behavioral therapy, which usually consists of sleep hygiene, relaxation training, sleep restriction therapy, and cognitive therapy, is the most studied non-pharmacologic treatment (13). However, it requires frequent monitoring and high maintenance costs (9). Acupuncture may be beneficial for insomnia, but it is invasive (14). Therefore, we need to find more effective, simple, and safe non-invasive treatments.
Studies have shown that Taijiquan, as a new intervention, has a good effect on insomnia. Irwin et al. (15) observed 112 healthy elderly people aged 59–86 who were randomly assigned to the Taijiquan group and the health education group, among adults with moderate sleep complaints, Taijiquan can be considered a useful non-pharmaco-logic approach to improve sleep quality in them. Siu et al. (16) studied the effect of Taijiquan or exercise on sleep of the elderly with insomnia and found that compared with the control group, the sleep efficiency of the taijiquan group was improved. However, evidence-based research remains insufficient in this area, and analysis of the efficacy of insomnia caused by different diseases is lacking. There has been no systematic review of the efficacy of various forms of Tai chi compared with different exercise interventions.
Therefore, we sought to summarize existing high-quality studies on Taijiquan intervention for insomnia, and overcome the limitations of the previous Meta-analysis, to seek a higher level of evidence-based medical evidence.
Materials and methods
Search strategy and selection criteria
Search strategy
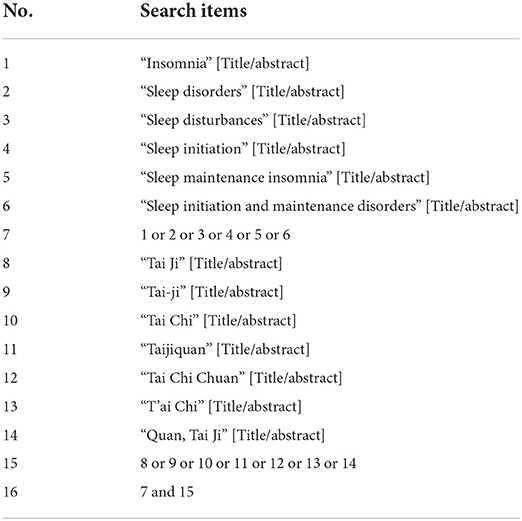
We conducted a comprehensive search for all published and unpublished RCTs of Taijiquan for patients with insomnia or other diseases with sleep complaints, in both Chinese and English language. We searched four English databases—Pubmed, Embase, Cochrane library, Web of Science, and four Chinese databases—CNKI, CBM, VIP, and Wanfang Data, from their inception to October 20, 2021. The search strategy is outlined in Appendix 1. Using the Pubmed database as an example, the search strategy was as follows (Table 1). In addition, efforts were made to find other literature sources, such as references from all included studies and clinical trial registries, which were also searched for additional relevant studies. If the original text or relevant data is not available, we will contact the original author for more information.
The inclusion criteria are presented as follows
1) Randomized and controlled design
2) Sample size ≥30
3) Duration of intervention ≥1 week
4) Use a suitable control intervention (non-active placebo or established positive control, e.g., benzodiazepine)
5) Have measurable results for sleep, any form of scale, or objective electrophysiological indicators
6) Any form of Taijiquan
7) Full text available and can get enough data.
Exclusion criteria
We excluded duplicate reports, reviews, conference abstracts and letters, trials enrolling patients with non-related subject research, and data that were incomplete or not obtainable. In addition, after the researchers reviewed the full text and discussed for many times, the articles identified as having serious quality defects, such as data confusion, and the articles with obvious flaws in the study design were also excluded.
Data extraction and outcome measures
The two authors (DMH and ZCL) independently searched and screened the retrieved literature. Unqualified trials were excluded, and the differences were resolved through discussion between the two authors. For problems that cannot be solved through discussion, consult the third author (YH) jointly to assess whether the trials met the inclusion criteria.
Some baseline information is extracted from the original studies, and they include the first author and published year, sample of patients, age, sex, outcome, intervention, frequency in two groups, and follow-up period. Data are extracted independently by two investigators (DMH and ZCL), and discrepancies are resolved by consensus. We have contacted the corresponding author to obtain the data when necessary. The primary outcome is Pittsburgh Sleep Quality Index (PSQI), PSQI is the most widely used sleep assessment tool with good reliability and validity (17, 18). It has been translated and used in many countries and can accurately reflect the sleep status of patients (19).
Assessment of risk of bias in included studies
Two review authors (DMH and ZCL) independently evaluated the risk of bias for each study according to the Cochrane Handbook for Systematic Reviews of Interventions. Disagreements were resolved by discussion or by consultation with a third reviewer (YH), when necessary. The following domains were assessed: sequence generation, allocation concealment, blinding of participants, providers and outcome assessors, completeness of outcome data, selective outcome reporting, and other sources of bias. Each potential source of bias was classified as either high, low, or unclear.
Statistical analysis
Review Manager (RevMan) version 5.3 software was used for the meta-analysis. Since this meta-analysis included only continuous data, we used the mean difference (MD) and 95% confidence interval (CI) for analysis. If the data was not available in the article, and the authors could not be contacted, estimates were made using the known data and the formula in the Cochrane Handbook for Systematic Reviews of Interventions. The I2 statistic was used to evaluate the heterogeneity revealed by data analysis. The interpretation of the I2 statistic is as follow (Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1.2008):
• 10–40%: might not be important
• 30–60%: may represent moderate heterogeneity
• 50–90%: may represent substantial heterogeneity
• 75–100%: considerable heterogeneity.
If substantial heterogeneity (above 50%) was detected, a random-effects model was used in the meta-analysis, where appropriate, subgroup or sensitivity analyses were performed to explore the source of heterogeneity.
Results
Search results
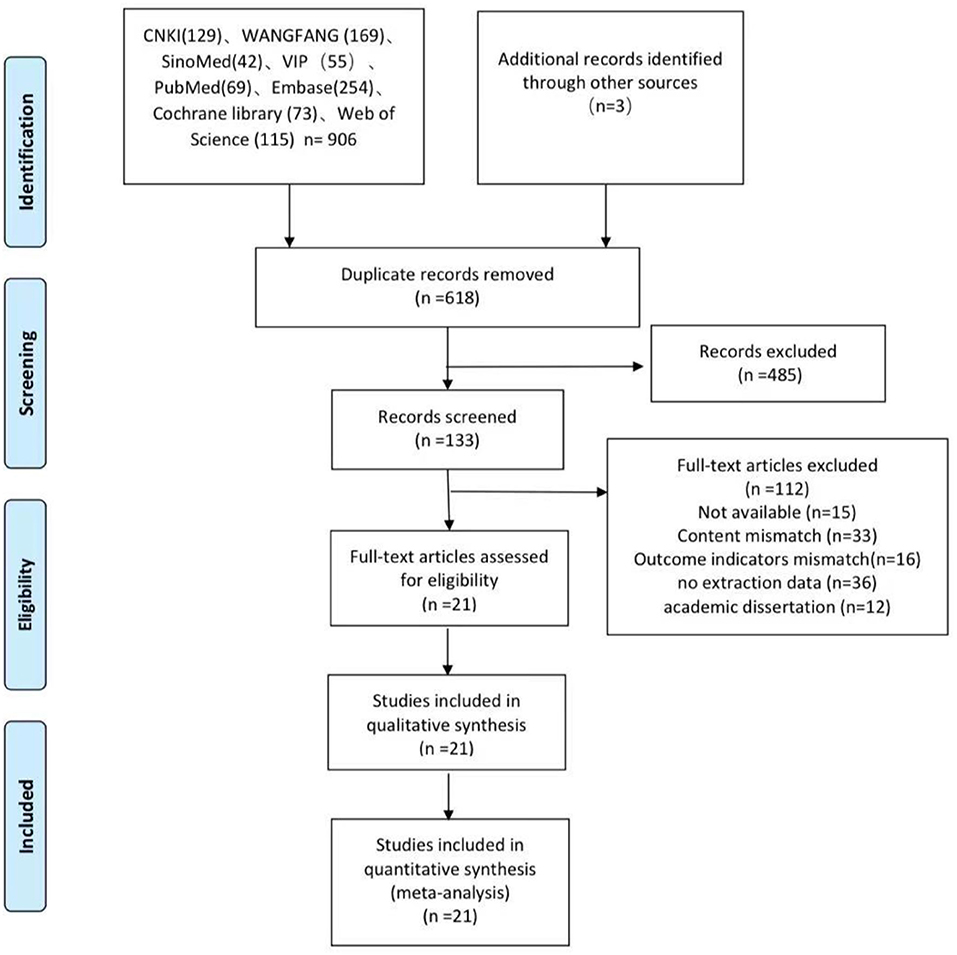
The review searched literature from eight databases. Figure 1 shows the search and selection process. A total of 909 potentially relevant articles were searched for strategies. After removing the duplicates, 618 articles need to be abstracted. 485 were excluded from titles and summaries, leaving 133 requiring full text. After reading the full text of these articles, were excluded, mainly because of inadequate study design, inadequate interventions, or incomplete data. The qualitative analysis included 21 studies (15, 16, 20–38).
Characteristics of included studies
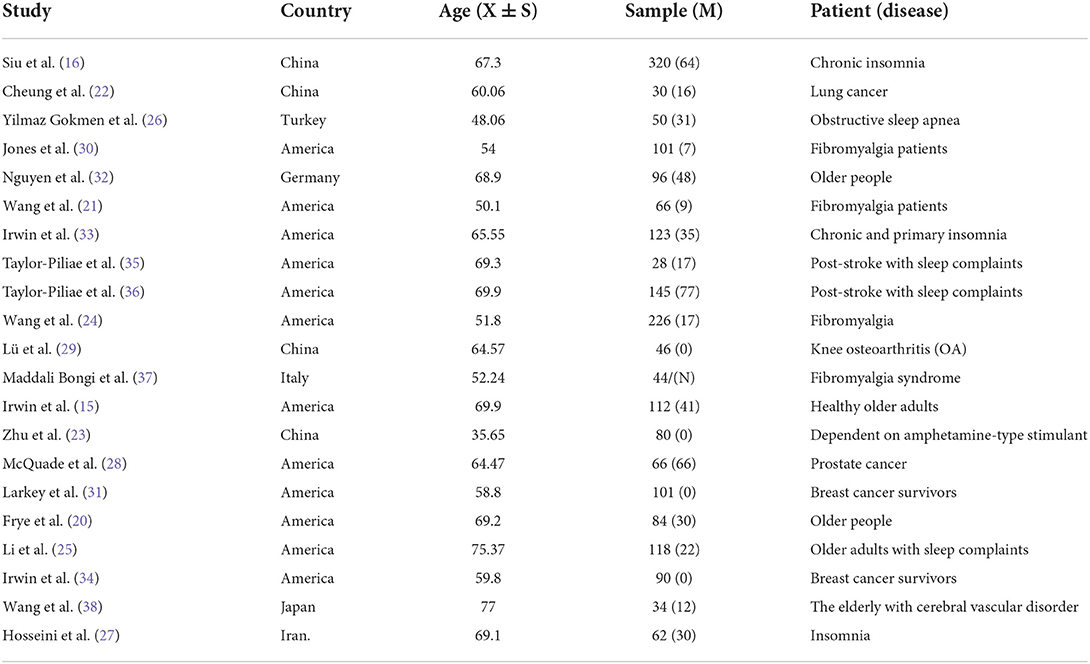
The study included 21 articles from seven countries—four from China, 12 from the United States, one from Iran, one from Italy, one from Turkey, one from Japan, and one from Germany. Their characteristics are presented in Table 2. In all of the studies, the mean total PSQI score at baseline was ≥5. This is consistent with insomnia diagnosis. In addition to insomnia, some patients also had other diseases such as depression, prostate cancer, knee osteoarthritis, fibromyalgia, post-stroke, or breast cancer. A total of 2,022 patients were included in this meta-analysis, of which 907 were allocated to the Taijiquan group and 1,115 were allocated to the control group. The average age of patients is over 35. One article (37) did not describe gender, and there were 522 male patients and 1,456 female patients in the retained literature (Table 2).
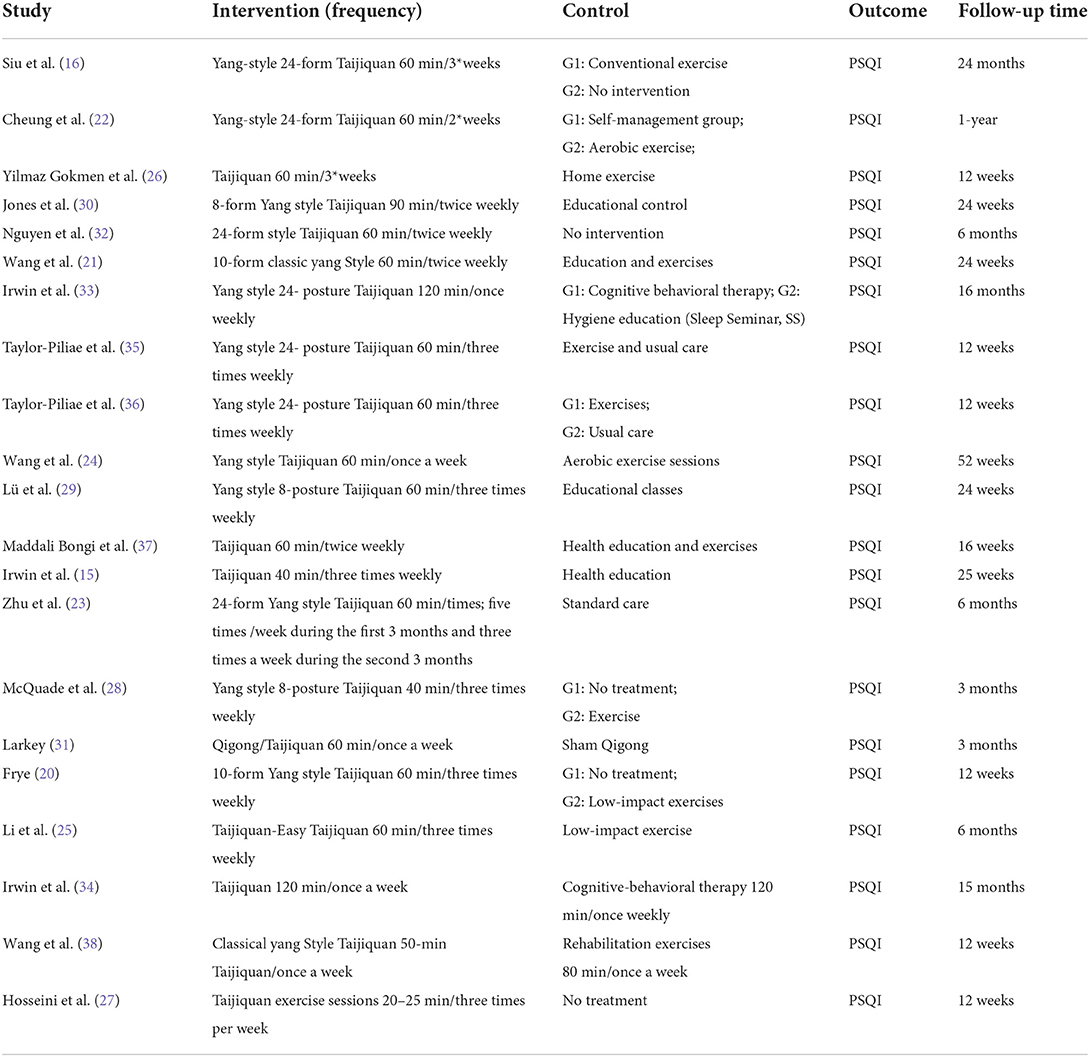
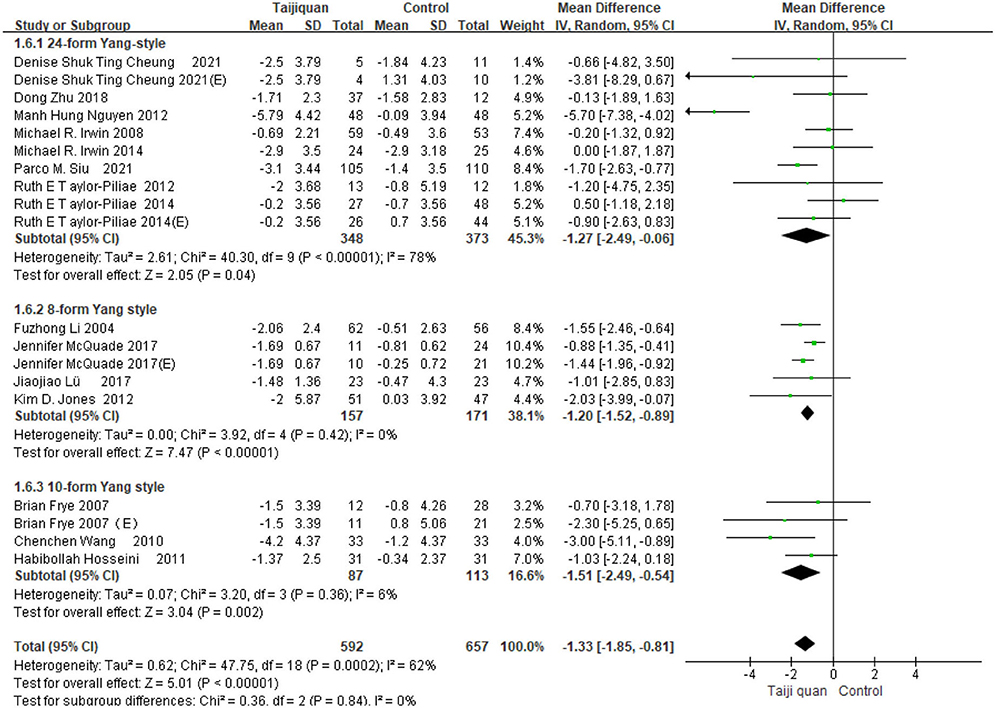
For the interventions, 15 articles trace back or describe in detail the types of taijiquan. eight studies used 24 forms of Yang's Taijiquan, and four studies used 8-form Yang style Taijiquan. Three studies used 10-form Yang style Taijiquan. Taijiquan lasts for a minimum of 12 weeks and a maximum of 24 months. Most are 3–6 months. The frequency of Taijiquan varies from 1 to 5 times per week (Table 3).
Risk of bias in the included studies
According to the Cochrane Handbook for Systematic Reviews of Interventions, we assessed the risk of bias in the included literature. The results are shown in Figures 2, 3. 12 RCTs described the appropriate random sequence generation method in detail. The other eight studies did not report the random sequence generation. Thus, the risk for these domains was determined to be unclear. Only nine of the studies reported using allocation concealment. Only 13 reported blinding the assessors. Due to the nature of Taijiquan, strict blinding of participants was difficult. All of the included studies reported the complete outcome data, and we considered them to be low-risk for this item. Most studies reported all of the outcomes. No other significant bias was found in any of the studies.
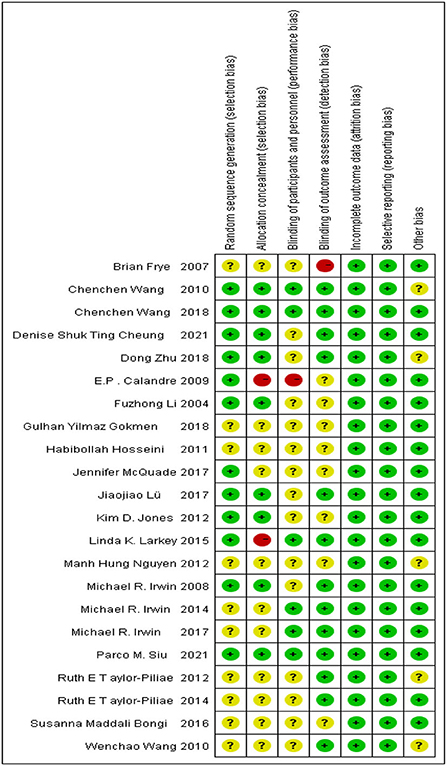
Figure 2. Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
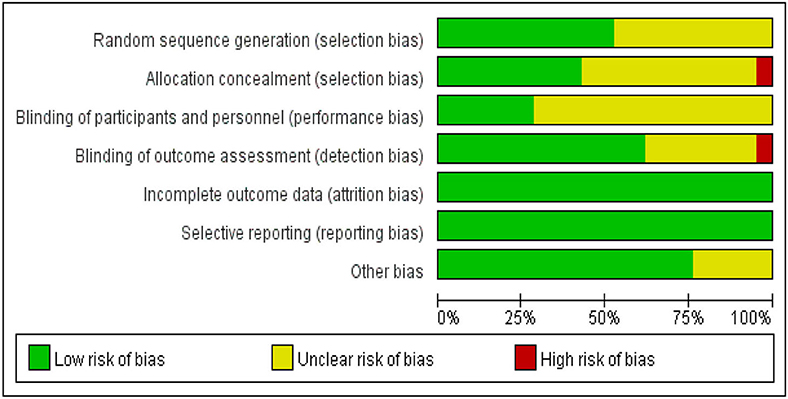
Figure 3. Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
Meta-analysis results
According to our retrieval results and the characteristics of the included studies, most of the studies used PSQI as the outcome indicator, while other outcome indicators could not be meta-analyzed due to the lack of a sufficient number of studies.
Our meta results suggest that Taijiquan is beneficial to insomnia patients and can significantly improve PSQI [MD = −1.16, 95% CI (−1.62, −0.71), P < 0.00001] (Figure 4). However, we found high heterogeneity of meta [I2 = 61%, P < 0.0001] (Figure 4), Further subgroup analysis is required to identify the source of heterogeneity.
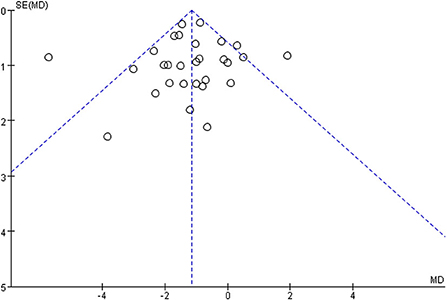
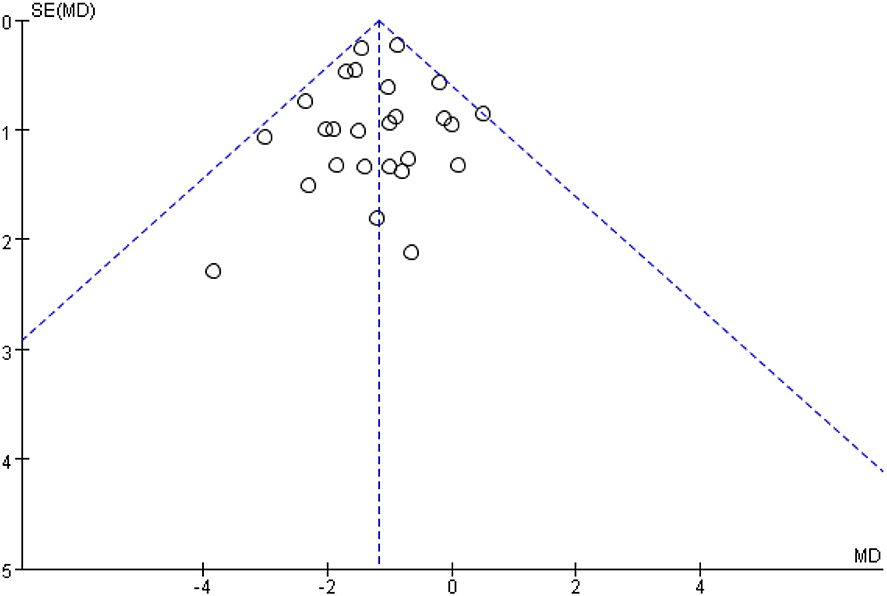
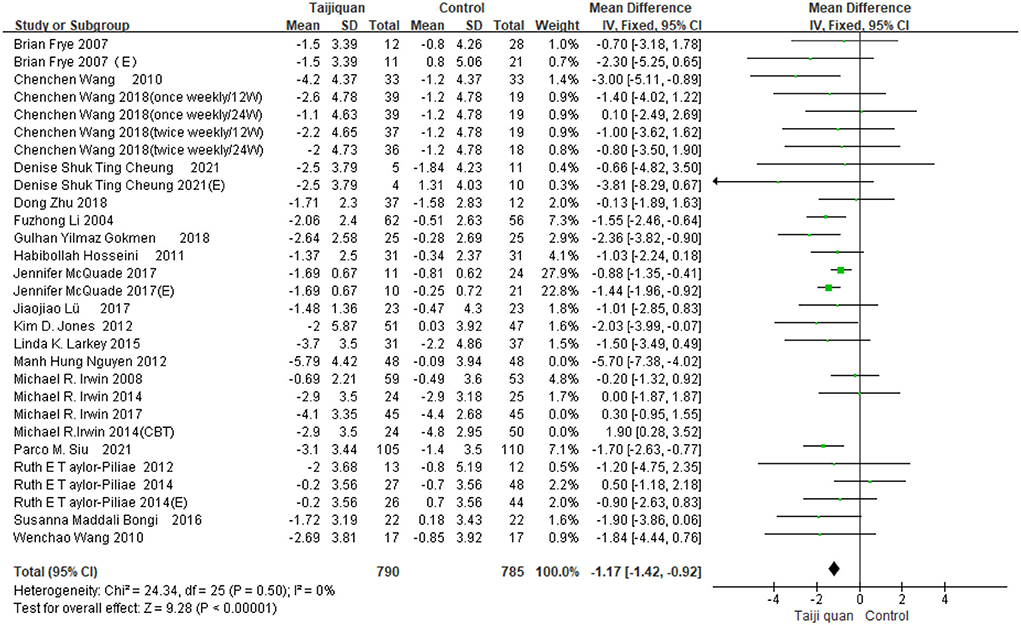
Figure 5 shows that the funnel diagram is symmetric, But there are three studies in the funnel outside, We use sensitivity analysis to determine that three studies with both large heterogeneity and publication bias from Irwin et al. (33, 34) studies and Nguyen et al. (32) study. After removing the three articles with publication bias, the Funnel plot is symmetric (Figure 6) and the combined results of the meta-analysis were stable [MD = −1.17, 95% CI (−1.42, −0.92), P < 0.00001] and the heterogeneity is small [I2 = 0, P = 0.05] (Figure 7).
Subgroup analysis
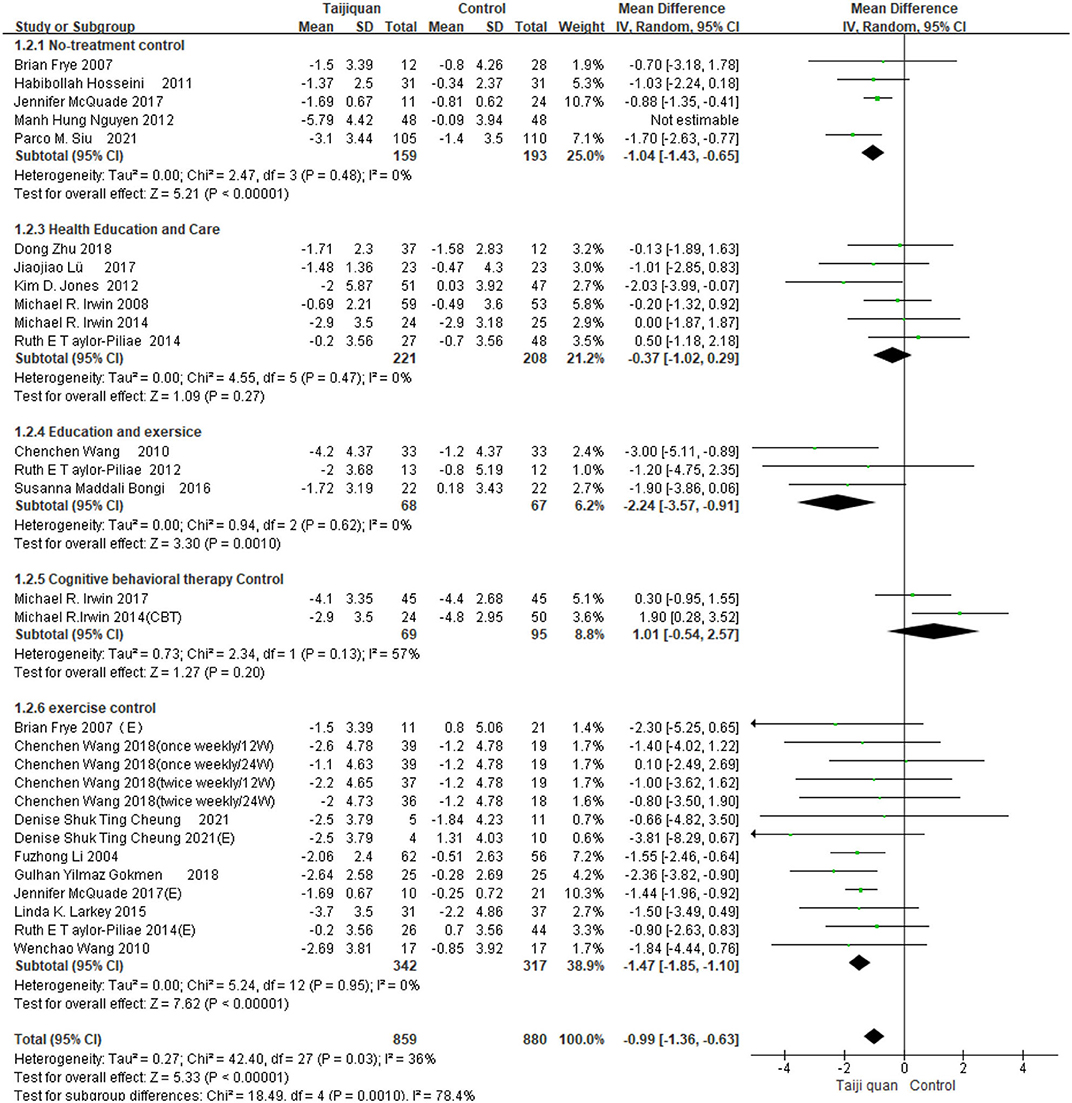
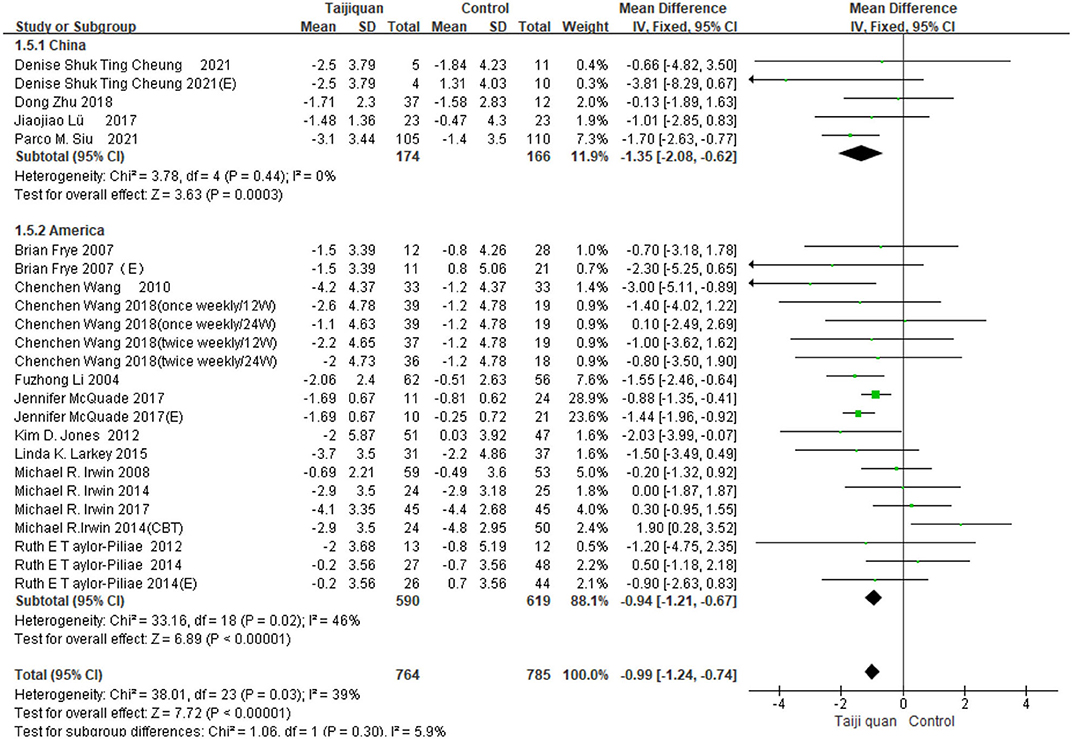
Five studies showed the effect of Taijiquan on global PSQI scores compared with non-treatment groups. Results of our meta-analysis showed that Taijiquan significantly reduced PSQI scores [MD = −1.95, 95% CI (−3.31, −0.59), P = 0.005], and a significant heterogeneity (I2 = 87%, P < 0.00001). When the Nguyen et al. (32) study was excluded, the heterogeneity of the overall PSQI score decreased to 0 (I2 = 0%, P = 0.48), and the meta-analysis still showed a stable, significant effect [MD = −1.04, 95% CI (−1.43, −0.65), P < 0.00001] (Figure 8, 1.2.1). Compared with simple exercise control group, Taijiquan has significant difference [MD = −1.47, 95% CI (−1.85, −1.10), P < 0.00001] (Figure 8, 1.2.6); When health education was combined with exercise as a control group, Taijiquan continued to significantly improve sleep [MD = −2.24, 95% CI (−3.57, −0.91), P = 0.0010] (Figure 8, 1.2.4). In addition, our subgroup analysis also found that compared with simple health education, both Taijiquan and health education or usual care could significantly reduce PSQI scores, but there was no significant difference between them [MD = −0.37, 95% CI (−1.02, 0.29), P = 0.27] (Figure 8, 1.2.3). Both cognitive behavioral therapy and Taijiquan can significantly reduce PSQI scores, but there is no significant difference between the two in improving insomnia [MD = 1.01, 95% CI (−0.54, 2.57), P = 0.20] (Figure 8, 1.2.5). There was no significant difference between studies in China and the United States, and Taijiquan was equally effective for Americans and Chinese (P = 0.30, Figure 9). Current studies mainly focus on Yang's Taijiquan, and different forms of Taijiquan have no significant difference in improving PSQI (P = 0.76, Figure 10); Through subgroup analysis of different patients, we found that Taijiquan significantly improved cancer, fibromyalgia, and insomnia of normal elderly people, while there seemed to be no significant difference in patients with cerebrovascular diseases (P = 0.31, Figure 11).
Discussion
In this systematic review and meta-analysis, we identified 21 RCTs of 2022 individuals from seven countries. Overall, taijiquan has a better effect on insomnia improvement compared with exercise and health education alone, and subgroup analyses found that tai chi was as effective as cognitive behavioral therapy in improving insomnia. In terms of different diseases, we found that Taijiquan significantly improved cancer, fibromyalgia, and insomnia in normal elderly people, while there seemed to be no significant difference in patients with cerebrovascular disease. Compared with other studies, Taijiquan was equally effective for Americans and Chinese. There are no influences that have a significant effect on Asians. This systematic evaluation includes all the studies on Taijiquan intervention for insomnia in both Chinese and English, and the research objects include both healthy people and various patients, the old and the young, which is a relatively complete systematic evaluation of Taijiquan intervention for insomnia. Additionally, since no adverse events were reported, Taijiquan could be promoted as a safe intervention for improving sleep quality.
Insomnia is a common problem, with about a quarter of adults suffering from insomnia. Body and mind exercise is a hot topic in the intervention treatment of insomnia. Taijiquan was gradually formed in the late Ming and early Qing Dynasties. It is a centuries-old martial art that combines physical movement and relaxation and is a traditional Chinese sport that has spread worldwide in recent years, more than five million people practice Tai Chi in the US alone (39). At present, Tai Chi has been widely used in the intervention of various diseases, including the rehabilitation of motor function after stroke (40), Parkinson's disease (41), atherosclerosis (42), diabetic foot (43), and so on. The first research on the intervention of taijiquan in insomnia occurred in 2002 when Lu et al. (44) found that taijiquan could improve the sleep of cancer patients. So why does taijiquan affect people's sleep?
The exact biological mechanism of Taijiquan in treating insomnia is not clear, Compared to simple exercise training, current hypotheses suggest that Taijiquan may improve sleep outcomes by reducing sympathetic activity and stimulating the parasympathetic nervous system, restoring the homeostasis balance of sympathetic/parasympathetic function (45). As a low-intensity aerobic exercise, Taijiquan may also encourage the brain to induce normal sleep by inhibiting the non-5-HT spinal system or improving the plasma concentration of pro-inflammatory cytokines to prevent insomnia (46, 47). In addition, studies have shown that Tai Chi can enhance functional connections in the brain (48). It can cause a change in the central nervous medium, thus improving people's sleep conditions and treating insomnia symptoms (46). Studies have shown that chronic insomniacs have reduced hippocampal volume and orbitofrontal gray matter concentration and increased anterior cingulate rostral cortex volume compared to non-insomniacs (15, 49, 50). Taijiquan may improve insomnia by inducing changes in hippocampal volume and orbitofrontal gray matter concentration (51, 52). Changes in brain regions associated with insomnia have been observed in Taijiquan trained individuals. Decreased anterior cingulate cortex homogeneity was observed in patients with long-term Taijiquan use (53). Long-term Taijiquan exercise can slow down gray matter atrophy and this can decrease sympathetic activity (54, 55). In addition, Taijiquan significantly increased functional connectivity between the medial prefrontal cortex and the medial temporal lobe in insomniacs (56). Taijiquan can improve emotional stability and, to some extent, improve sleep quality. The Chinese believe that taijiquan exercises emphasize the leading role of consciousness of “mind first behind body” and pay attention to the two characteristics of “peace of mind” and “relaxation of the body.” “Peace of mind” is to eliminate all the adverse effects of sub-stimuli on the cerebral cortex. The combination of consciousness and exercise can stimulate the cerebral cortex, causing excitement in one area of the cerebral cortex, while other areas enter a state of inhibition and get sufficient rest. Taijiquan can improve the function of the central nervous system, improve the coordination between organs in the body, and play a role in regulating and training brain function (57). Compared with simple exercise training, Taijiquan exercise is to improve people's psychology, life and behavior, adjust the physical and mental conditions of insomnia patients, fundamentally cure insomnia.
This systematic review has some advantages and limitations. We conducted a relatively comprehensive systematic review, and the patient types included cancer, fibromyalgia and normal elderly people, etc. There were many diseases, so we could objectively evaluate the efficacy of Taijiquan on insomnia. Compared with previous systematic reviews (58), we included more RCTs with a larger sample size and strictly limited inclusion and exclusion criteria, with higher credibility. In terms of limitations, we only selected PSQI as the only evaluation index. However, most of the other evaluation results were insufficient or original data could not be obtained. In addition, subgroup analysis is lacking randomized controlled studies for some diseases, which may be biased.
In reviewing almost all about Taijiquan to improve insomnia, the high quality of research, we believe that Taijiquan to improve insomnia is convincing, however, the effects of different groups for different styles of Taijiquan treatment is not clear, Taijiquan differences between different age also needs to continue to study, different intervention dose and frequency of the need to continue to study. In addition, further research is needed on the physiological mechanism of Taijiquan in improving insomnia. Future research directions require more large-sample, multi-center, high-quality randomized controlled trials. It is necessary to further optimize the application of different types of Taijiquan in insomnia.
Conclusion
In conclusion, our meta-analysis showed that Taijiquan can improve sleep quality and improve insomnia. It provides evidence for taijiquan to treat different insomnia people and improve sleep quality. Subgroup analysis showed that Taijiquan can also improve insomnia caused by different diseases (except cerebrovascular diseases), which can be used as a supplement and alternative treatment for insomnia. There was no difference in the efficacy of different forms of Taijiquan, and there was no significant difference in the effect of Taijiquan on improving sleep between Chinese and Americans.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
DH and ZL conceptualized the study design, search and filter the title and abstract of the article, and confirmed the data and statistical analysis. YW and XW drafted and supplemented the methodology. HL and YH solved the difference. YH provided the funds. YC and XL modified their English and provided help in data analysis. JQ and JC are responsible for supervision and quality control. All authors provided information about the direction of research and the contents of the manuscript. All authors approved the final version of the manuscript.
Acknowledgments
We would like to thank all the authors for their hard work and thank the teachers of Gannan Medical University and Yuebei People's Hospital for their help, and thanks to XP for her English help with this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.892453/full#supplementary-material
References
1. Patel D, Steinberg J, Patel P. Insomnia in the elderly: a review. J Clin Sleep Med. (2018) 14:1017–24. doi: 10.5664/jcsm.7172
2. Battle DE. Diagnostic and statistical manual of mental disorders (DSM). Codas. (2013) 25:191–2. doi: 10.1590/s2317-17822013000200017
3. Mellor A, Hamill K, Jenkins MM, Baucom DH, Norton PJ, Drummond SPA, et al. Partner-assisted cognitive behavioural therapy for insomnia versus cognitive behavioural therapy for insomnia: a randomised controlled trial. Trials. (2019) 20:262. doi: 10.1186/s13063-019-3334-3
4. Hillman D, Mitchell S, Streatfeild J, Burns C, Bruck D, Pezzullo L, et al. The economic cost of inadequate sleep. Sleep. (2018) 41. doi: 10.1093/sleep/zsy083
5. Lin YF, Liu ZD, Ma W, Shen WD. Hazards of insomnia and the effects of acupuncture treatment on insomnia. J Integr Med. (2016) 14:174–86. doi: 10.1016/S2095-4964(16)60248-0
6. Cunnington D, Junge MF, Fernando AT. Insomnia: prevalence, consequences and effective treatment. Med J Aust. (2013) 199:S36–40. doi: 10.5694/mja13.10718
7. Shi ML, Zhao M, Wang YH, Sun TY, Li XL, Ren F, et al. [Network meta-analysis of efficacy and safety of Chinese patent medicines in treatment of insomnia]. Zhongguo Zhong Yao Za Zhi. (2021) 46:5403–17. doi: 10.19540/j.cnki.cjcmm.20210407.503
8. Haynes J, Talbert M, Fox S, Close E. Cognitive behavioral therapy in the treatment of insomnia. South Med J. (2018) 111:75–80. doi: 10.14423/SMJ.0000000000000769
9. Passos GS, Poyares DL, Santana MG, Tufik S, Mello MT. Is exercise an alternative treatment for chronic insomnia? Clinics. (2012) 67:653–60. doi: 10.6061/clinics/2012(06)17
10. Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK, et al. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. (2014) 37:1553–63. doi: 10.5665/sleep.4010
11. Yin X, Gou M, Xu J, Dong B, Yin P, Masquelin F, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med. (2017) 37:193–200. doi: 10.1016/j.sleep.2017.02.012
12. Lou BX, Oks M. Insomnia: pharmacologic treatment. Clin Geriatr Med. (2021) 37:401–15. doi: 10.1016/j.cger.2021.04.003
13. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. (2017) 26:675–700. doi: 10.1111/jsr.12594
14. Kim SB, Kim JY, Park SW, Lee NR, Lee SW, Kim YH, et al. Comparison of 2 methods of non-invasive treatment between transcutaneous electrical stimulation and pulsed electromagnetic field stimulation as replacement of invasive manual acupuncture. Acupunct Electrother Res. (2012) 37:247–61. doi: 10.3727/036012912X13831831256294
15. Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: a randomized controlled trial of Tai Chi Chih. Sleep. (2008) 31:1001–8.
16. Siu PM, Yu AP, Tam BT, Chin EC, Yu DS, Chung KF, et al. Effects of Tai Chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw Open. (2021) 4:e2037199. doi: 10.1001/jamanetworkopen.2020.37199
17. Xiong P, Spira AP, Hall BJ. Psychometric and structural validity of the pittsburgh sleep quality index among filipino domestic workers. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17145219
18. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
19. Farah NM, Saw Yee T, Mohd Rasdi HF. Self-reported sleep quality using the Malay version of the pittsburgh sleep quality index (PSQI-M) in Malaysian adults. Int J Environ Res Public Health. (2019) 16. doi: 10.3390/ijerph16234750
20. Frye B, Scheinthal S, Kemarskaya T, Pruchno R. Tai Chi and low impact exercise: effects on the physical functioning and psychological wellbeing of older people. J Appl Gerontol. (2007) 26:433–53. doi: 10.1177/0733464807306915
21. Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, et al. A randomized trial of tai chi for fibromyalgia. N Engl J Med. (2010) 363:743–54. doi: 10.1056/NEJMoa0912611
22. Cheung DST, Takemura N, Lam TC, Ho JCM, Deng W, Smith R, et al. Feasibility of aerobic exercise and Tai-Chi interventions in advanced lung cancer patients: a randomized controlled trial. Integr Cancer Ther. (2021) 20:15347354211033352. doi: 10.1177/15347354211033352
23. Zhu D, Dai G, Xu D, Xu X, Geng J, Zhu W, et al. Long-term effects of Tai Chi intervention on sleep and mental health of female individuals with dependence on amphetamine-type stimulants. Front Psychol. (2018) 9:1476. doi: 10.3389/fpsyg.2018.01476
24. Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ. (2018) 360:k851. doi: 10.1136/bmj.k851
25. Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C, et al. Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc. (2004) 52:892–900. doi: 10.1111/j.1532-5415.2004.52255.x
26. Yilmaz Gokmen G, Akkoyunlu ME, Kilic L, Algun C. The effect of T'ai Chi and Qigong training on patients with obstructive sleep apnea: a randomized controlled study. J Altern Complement Med. (2019) 25:317–25. doi: 10.1089/acm.2018.0197
27. Hosseini H, Esfirizi MF, Marandi SM, Rezaei A. The effect of Ti Chi exercise on the sleep quality of the elderly residents in Isfahan, Sadeghieh elderly home. Iran J Nurs Midwifery Res. (2011) 16:55–60.
28. McQuade JL, Prinsloo S, Chang DZ, Spelman A, Wei Q, Basen-Engquist K, et al. Qigong/tai chi for sleep and fatigue in prostate cancer patients undergoing radiotherapy: a randomized controlled trial. Psychooncology. (2017) 26:1936–43. doi: 10.1002/pon.4256
29. Lü J, Huang L, Wu X, Fu W, Liu Y. Effect of Tai Ji Quan training on self-reported sleep quality in elderly Chinese women with knee osteoarthritis: a randomized controlled trail. Sleep Med. (2017) 33:70–5. doi: 10.1016/j.sleep.2016.12.024
30. Jones KD, Sherman CA, Mist SD, Carson JW, Bennett RM, Li F, et al. A randomized controlled trial of 8-form Tai chi improves symptoms and functional mobility in fibromyalgia patients. Clin Rheumatol. (2012) 31:1205–14. doi: 10.1007/s10067-012-1996-2
31. Larkey LK, Roe DJ, Weihs KL, Jahnke R, Lopez AM, Rogers CE, et al. Randomized controlled trial of Qigong/Tai Chi Easy on cancer-related fatigue in breast cancer survivors. Ann Behav Med. (2015) 49:165–76. doi: 10.1007/s12160-014-9645-4
32. Nguyen MH, Kruse A. A randomized controlled trial of Tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin Interv Aging. (2012) 7:185–90. doi: 10.2147/CIA.S32600
33. Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Breen EC, Witarama T, et al. Cognitive behavioral therapy vs. Tai Chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial. Sleep. (2014) 37:1543–52. doi: 10.5665/sleep.4008
34. Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Nicassio P, Ganz PA, et al. Tai Chi Chih compared with cognitive behavioral therapy for the treatment of insomnia in survivors of breast cancer: a randomized, partially blinded, non-inferiority trial. J Clin Oncol. (2017) 35:2656–65. doi: 10.1200/JCO.2016.71.0285
35. Taylor-Piliae RE, Coull BM. Community-based Yang-style Tai Chi is safe and feasible in chronic stroke: a pilot study. Clin Rehabil. (2012) 26:121–31. doi: 10.1177/0269215511419381
36. Taylor-Piliae RE, Hoke TM, Hepworth JT, Latt LD, Najafi B, Coull BM, et al. Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch Phys Med Rehabil. (2014) 95:816–24. doi: 10.1016/j.apmr.2014.01.001
37. Maddali Bongi S, Paoletti G, Calà M, Del Rosso A, El Aoufy K, Mikhaylova S, et al. Efficacy of rehabilitation with Tai Ji Quan in an Italian cohort of patients with fibromyalgia syndrome. Complement Ther Clin Pract. (2016) 24:109–15. doi: 10.1016/j.ctcp.2016.05.010
38. Wang W, Sawada M, Noriyama Y, Arita K, Ota T, Sadamatsu M, et al. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single-blinded randomized controlled trial. Psychogeriatrics. (2010) 10:160–6. doi: 10.1111/j.1479-8301.2010.00334.x
39. Budhrani-Shani P, Berry DL, Arcari P, Langevin H, Wayne PM. Mind-body exercises for nurses with chronic low back pain: an evidence-based review. Nurs Res Pract. (2016) 2016:9018036. doi: 10.1155/2016/9018036
40. Wu S, Chen J, Wang S, Jiang M, Wang X, Wen Y, et al. Effect of Tai Chi exercise on balance function of stroke patients: a meta-analysis. Med Sci Monit Basic Res. (2018) 24:210–15. doi: 10.12659/MSMBR.911951
41. Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, et al. Tai chi and postural stability in patients with Parkinson's disease. N Engl J Med. (2012) 366:511–9. doi: 10.1056/NEJMoa1107911
42. Zhou S, Zhang Y, Kong Z, Loprinzi PD, Hu Y, Ye J, et al. The effects of Tai Chi on markers of atherosclerosis, lower-limb physical function, and cognitive ability in adults aged over 60: a randomized controlled trial. Int J Environ Res Public Health. (2019) 16. doi: 10.3390/ijerph16050753
43. Chao M, Wang C, Dong X, Ding M. The effects of Tai Chi on type 2 diabetes mellitus: a meta-analysis. J Diabetes Res. (2018) 2018:7350567. doi: 10.1155/2018/7350567
44. Lu H, Yu J, Qiaoping Y, Zhu H. Taijiquan can improve the sleep of cancer patients with insomnia. Chin Nurs Res. (2002) 79:799.
45. Raman G, Zhang Y, Minichiello VJ, D'Ambrosio CM, Wang C. Tai Chi improves sleep quality in healthy adults and patients with chronic conditions: a systematic review and meta-analysis. J Sleep Disord Ther. (2013) 2. doi: 10.4172/2167-0277.1000141
46. Melancon MO, Lorrain D, Dionne IJ. Exercise and sleep in aging: emphasis on serotonin. Pathol Biol. (2014) 62:276–83. doi: 10.1016/j.patbio.2014.07.004
47. Krueger JM, Fang J, Hansen MK, Zhang J, Obál F Jr. Humoral regulation of sleep. News Physiol Sci. (1998) 13:189–94. doi: 10.1152/physiologyonline.1998.13.4.189
48. Xie H, Zhang M, Huo C, Xu G, Li Z, Fan Y, et al. Tai Chi Chuan exercise related change in brain function as assessed by functional near-infrared spectroscopy. Sci Rep. (2019) 9:13198. doi: 10.1038/s41598-019-49401-9
49. Joo EY, Noh HJ, Kim JS, Koo DL, Kim D, Hwang KJ, et al. Brain gray matter deficits in patients with chronic primary insomnia. Sleep. (2013) 36:999–1007. doi: 10.5665/sleep.2796
50. Winkelman JW, Plante DT, Schoerning L, Benson K, Buxton OM, O'Connor SP, et al. Increased rostral anterior cingulate cortex volume in chronic primary insomnia. Sleep. (2013) 36:991–8. doi: 10.5665/sleep.2794
51. Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T, et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. (2011) 191:36–43. doi: 10.1016/j.pscychresns.2010.08.006
52. Luders E, Toga AW, Lepore N, Gaser C. The underlying anatomical correlates of long-term meditation: larger hippocampal and frontal volumes of gray matter. NeuroImage. (2009) 45:672–8. doi: 10.1016/j.neuroimage.2008.12.061
53. Wei GX, Dong HM, Yang Z, Luo J, Zuo XN. Tai Chi Chuan optimizes the functional organization of the intrinsic human brain architecture in older adults. Front Aging Neurosci. (2014) 6:74. doi: 10.3389/fnagi.2014.00074
54. Liu S, Li L, Liu Z, Guo X. Long-term Tai Chi experience promotes emotional stability and slows gray matter atrophy for elders. Front Psychol. (2019) 10:91. doi: 10.3389/fpsyg.2019.00091
55. Motivala SJ, Sollers J, Thayer J, Irwin MR. Tai Chi Chih acutely decreases sympathetic nervous system activity in older adults. J Gerontol A Biol Sci Med Sci. (2006) 61:1177–80. doi: 10.1093/gerona/61.11.1177
56. Li R, Zhu X, Yin S, Niu Y, Zheng Z, Huang X, et al. Multimodal intervention in older adults improves resting-state functional connectivity between the medial prefrontal cortex and medial temporal lobe. Front Aging Neurosci. (2014) 6:39. doi: 10.3389/fnagi.2014.00039
57. Fuqin J. Discussion on the principle of curing undergraduates of insomnia by Taijiquan. Liaoning Sport Science Technol. (2003) 25:61–7. doi: 10.13940/j.cnki.lntykj.2003.05.046
Keywords: Taijiquan, Tai chi, insomnia, meta-analysis, Hyposomnia
Citation: Han D, Cheng J, Qu J, Wen X, Liu X, Chen Y, Wen Y, Liu Z, Liu H and Huang Y (2022) Effectiveness of Taijiquan in treating insomnia: A systematic review and meta-analysis of randomized controlled studies. Front. Psychiatry 13:892453. doi: 10.3389/fpsyt.2022.892453
Received: 17 May 2022; Accepted: 31 August 2022;
Published: 27 September 2022.
Edited by:
Tao-Hsin Tung, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, ChinaReviewed by:
Zhang Jianglin, Jinan University, ChinaYijun Song, Tianjin Medical University General Hospital, China
Copyright © 2022 Han, Cheng, Qu, Wen, Liu, Chen, Wen, Liu, Liu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zicai Liu, MTQ1NDI2MjA2NUBxcS5jb20=; Huiyu Liu, bGl1aHVpeXVkb2N0b3JAc29odS5jb20=; Ying Huang, NTI3MjY3Mjg4QHFxLmNvbQ==
 Dongmiao Han
Dongmiao Han Jinling Cheng1
Jinling Cheng1 Xin Wen
Xin Wen Zicai Liu
Zicai Liu Huiyu Liu
Huiyu Liu