- 1Coping Skills and Learning to Manage Emotions Readily (CALMER) Lab, Department of Psychology, Virginia Polytechnic Institute and State University, Blacksburg, VA, United States
- 2Attention and Behavior Clinic, Department of Psychiatry and Behavioral Health, Penn State Milton S. Hershey Medical Center, Hershey, PA, United States
A Corrigendum on
A Mini-Review of Pharmacological and Psychosocial Interventions for Reducing Irritability Among Youth With ADHD
by Breaux, R., Dunn, N. C., Swanson, C. S., Larkin, E., Waxmonsky, J., and Baweja, R. (2022). Front. Psychiatry 13:794044. doi: 10.3389/fpsyt.2022.794044
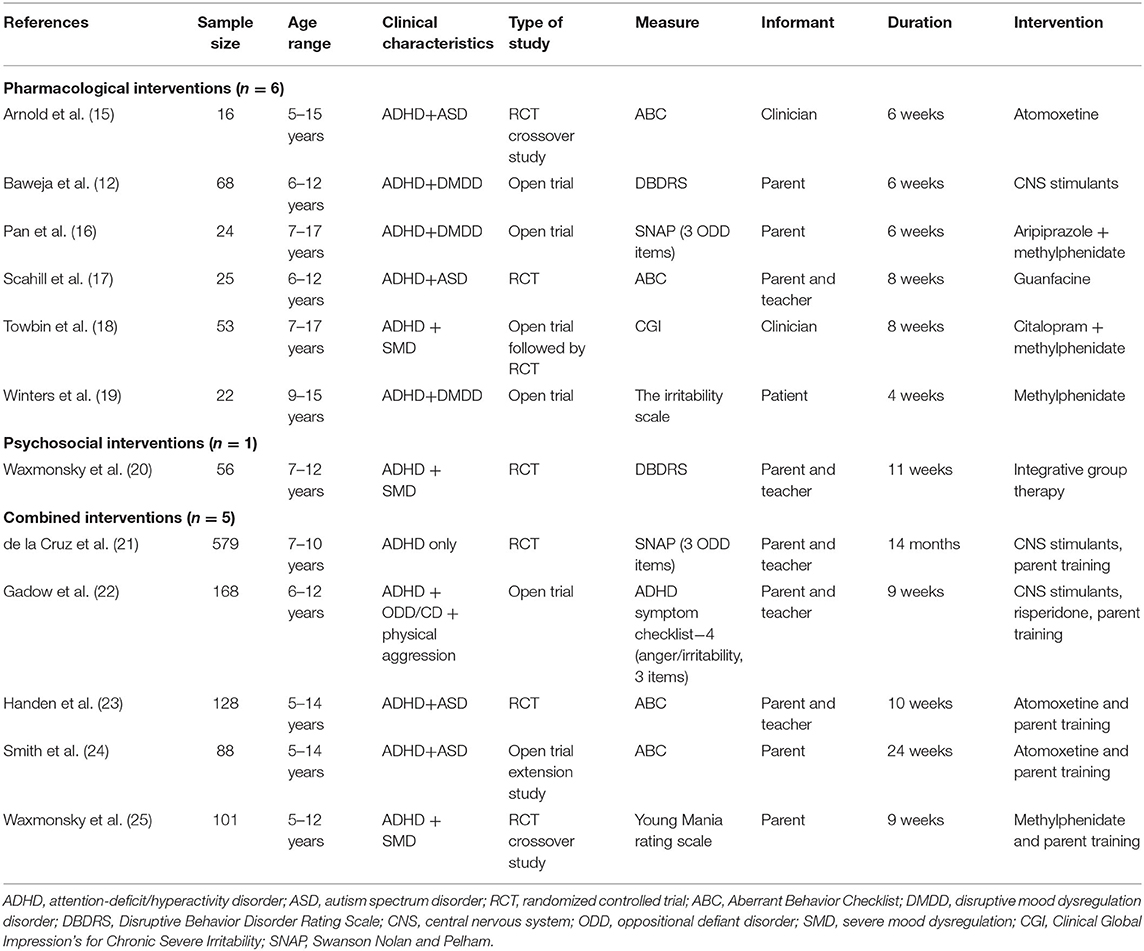
In the original article, we mistakenly reported on a secondary outcome for the Towbin et al. (2020) study, specifically the Children's Depression Rating Scale—Irritability item rather than the primary outcome, the Clinical Global Impression's for Chronic Severe Irritability. We have updated this information to Table 1; the corrected Table 1 appears below.
An update has been made to the “Pharmacological Interventions” section, at the end of paragraph 2:
The original text “A significant decrease in irritability was observed from baseline to the end of the 5-week open trial on MPH (d = 0.69, p < 0.001); however, a non-significant difference was observed between the citalopram and placebo groups for change in irritability during the subsequent blinded randomized trial phase (18)” has been replaced by “For their primary outcome of the Clinical Global Impression's for Chronic Severe Irritability, a significant decrease in irritability was found (d = 0.60), with the estimated response differing between the citalopram (35%) and placebo (6%) groups (OR = 1.70, p = 0.006) (18).”
This has resulted in updates to several places in the Discussion section.
“Gaps of Existing Intervention Research,” paragraph one:
The original text “failed to find evidence of added benefits” has been replaced by “found evidence of added benefits when combining a SSRI with a CNS stimulant.”
“Gaps of Existing Intervention Research,” paragraph four:
The original text “Specifically, only five of the included studies utilized an established scale for irritability, with four using the ABC-I subscale (15, 17, 23, 24) and one utilizing youth self-report on The Irritability Scale (19). In contrast, five of the studies created irritability composites based on ODD items from rating scales for disruptive behavior, including the Swanson Nolan and Pelham version IV scale, the Disruptive Behavior Disorder Rating Scale, and the ADHD Symptom Checklist (12, 16, 20–22). Further, two utilized measures of depression or mania to assess irritability including the Children's Depression Rating Scale and Young Mania Rating Scale (18, 25). Surprisingly, none employed the Affective Reactivity Index (ARI) (36), which has well established psychometrics in pediatric populations. As such, we recommend that future research assessing interventions for irritability among youth with ADHD utilize well-validated measures, such as the ABC-I and ARI, as well as consider integrating multiple informants vs. sole reliance on parent report. Relatedly, several studies were excluded from the review due to only examining irritability as a side effect/adverse event (37, 38).” has been replaced by “Specifically, only six of the included studies utilized an established scale for irritability, with four using the ABC-I subscale (15, 17, 23, 24), one utilizing the Clinical Global Impression focused on irritability which was generated based on a semi-structured diagnostic interview (18), and one utilizing youth self-report on The Irritability Scale (19). In contrast, five of the studies created irritability composites based on ODD items from rating scales for disruptive behavior, including the Swanson Nolan and Pelham version IV scale, the Disruptive Behavior Disorder Rating Scale, and the ADHD Symptom Checklist (12, 16, 20–22). Further, one utilized a measure of mania to assess irritability, specifically the Young Mania Rating Scale (25). Surprisingly, none employed the Affective Reactivity Index (ARI) (36), which has well-established psychometrics in pediatric populations. As such, we recommend that future research assessing interventions for irritability among youth with ADHD utilize well-validated measures, such as the ABC-I and ARI, as well as consider integrating multiple informants vs. sole reliance on parent report. Such an approach was only used in one of the included studies in this review (18). Relatedly, several studies were excluded from the review due to only examining irritability as a side effect/adverse event (37, 38).”
Conclusion
The original text “This mini review addresses an important gap in the literature by discussing the existing pharmacological and psychosocial interventions targeting irritability among youth with ADHD. Findings suggest that CNS stimulants used alone or in combination with behavioral therapy (e.g., parent training) are effective at reducing irritability in youth with ADHD only or comorbid ADHD and DMDD/SMD. Less evidence was found for the efficacy of alpha agonists and atomoxetine, with existing studies focusing on youth with comorbid ASD. Parent training alone or in combination with atomoxetine was found to be effective at reducing irritability in youth with comorbid ADHD and ASD. Future research assessing the efficacy of other psychosocial interventions, particularly CBT is necessary, as are randomized trials with large samples using well validated scales designed to measure irritability that assess intervention sequencing and intensity among youth with ADHD.” has been replaced by “This mini review addresses an important gap in the literature by discussing the existing pharmacological and psychosocial interventions targeting irritability among youth with ADHD. Findings suggest that CNS stimulants used alone or in combination with behavioral therapy (e.g., parent training) are effective at reducing irritability in youth with ADHD only or comorbid ADHD and DMDD/SMD. Less evidence was found for the efficacy of alpha agonists and atomoxetine, with existing studies focusing on youth with comorbid ASD. One study found evidence for benefits of adding a selective serotonin reuptake inhibitor (citalopram) to MPH for reducing irritability in youth with ADHD and DMDD/SMD. Parent training alone or in combination with atomoxetine was found to be effective at reducing irritability in youth with comorbid ADHD and ASD. Future research assessing the efficacy of other psychosocial interventions, particularly CBT is necessary, as are randomized trials with large samples using well-validated scales designed to measure irritability that assess intervention sequencing and intensity among youth with ADHD.”
The authors apologize for this error; beyond these minor changes, this does not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: attention-deficit/hyperactivity disorder, irritability, intervention, mini review, medication, behavior therapy
Citation: Breaux R, Dunn NC, Swanson CS, Larkin E, Waxmonsky J and Baweja R (2022) Corrigendum: A Mini-Review of Pharmacological and Psychosocial Interventions for Reducing Irritability Among Youth With ADHD. Front. Psychiatry 13:879223. doi: 10.3389/fpsyt.2022.879223
Received: 19 February 2022; Accepted: 07 March 2022;
Published: 05 April 2022.
Edited and reviewed by:
Jean Marc Guile, University of Picardie Jules Verne, FranceCopyright © 2022 Breaux, Dunn, Swanson, Larkin, Waxmonsky and Baweja. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rosanna Breaux, cmJyZWF1eEB2dC5lZHU=
 Rosanna Breaux
Rosanna Breaux Nicholas C. Dunn
Nicholas C. Dunn Courtney S. Swanson
Courtney S. Swanson Emma Larkin
Emma Larkin James Waxmonsky
James Waxmonsky Raman Baweja
Raman Baweja