
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Psychiatry , 07 April 2022
Sec. Child and Adolescent Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.876727
This article is part of the Research Topic Catatonia across the Lifespan View all 8 articles
Catatonia and delirium were originally different diagnostic concepts, but in recent years, their similarities have been highlighted. Catatonia was first described by Kahlbaum in 1874 as a psychosis with specific physical tension (1) and regarded as an important disease type, mainly within the framework of schizophrenia (2). However, catatonia is seen in not only schizophrenia but also neurodevelopmental, bipolar, and depressive disorders, as well as other medical conditions, and it has come to be regarded as a catatonic syndrome (3, 4). The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) has developed common diagnostic criteria for catatonia due to several disorders, differentiating between catatonia due to a mental disorder and another medical condition (5). Recently, catatonia due to a general medical condition has been more frequent than due to a mental disorder (6).
Delirium was described by Lipowski in 1987 as acute global brain dysfunction occurring in the setting of physical illness (7). Delirium is defined in the DSM-5 as a disturbance in attention and awareness (reduced orientation to the environment) (5) and is thought to be caused by physical factors or drugs (8).
The origins of the two diagnostic concepts of catatonia and delirium are different, and the DSM-5 description of catatonia due to a general medical condition specifies that “the disturbance does not occur exclusively during the course of a delirium” (5). However, as the diagnostic concept of catatonia has shifted, the similarities between the symptoms of catatonia and delirium have been noted. Jaimes-Albornoz and Serra-Mestres (9) studied catatonic phenomena in 112 patients aged over 65 years who were referred to a psychiatry service in a general hospital. Seven patients (6.3%) met the DSM-IV criteria for catatonia, and three of these patients presented concomitant delirium. Grover et al. (10) studied the prevalence of catatonic symptoms in 205 delirium patients. Symptoms common to catatonia were found, including excitement (72.7%), immobility or stupor (21.4%), mutism (15.6%), and negativism (10%). Of the delirium patients, 12.7% met the DSM-5 criteria for catatonia. Connell et al. (11) studied the occurrence of catatonia and delirium in 378 critically ill patients. Of these patients, 88 (23%) met the diagnostic criteria for catatonia, and 250 (66%) met the criteria for delirium, using the DSM-5. Of the 88 2 patients who experienced catatonia, 82 (93.2%) simultaneously experienced delirium. In clinical practice, many cases are difficult to differentiate (12, 13), and the current clinical issue is how to consider the overlap of symptoms between catatonia and delirium. The specificity of the diagnostic criteria of the DSM-5 has been criticized (6, 14). The International Classification of Diseases, 10th Revision (ICD-10) describes organic catatonic disorder: “It has not been conclusively determined whether an organic catatonic state may occur in clear consciousness or whether it is always a manifestation of delirium, with subsequent partial or total amnesia” (15). The concept of a catatonia–delirium spectrum has even been suggested (4).
Differentiating between catatonia and delirium is necessary because they have different treatment strategies. Catatonia is responsive to certain treatments such as benzodiazepines and modified electroconvulsive therapy (16), which are effective yet unspecific in their modes of action (17). However, both may also produce or exacerbate delirium, and conversely, antipsychotics used to treat symptoms of delirium may produce or exacerbate catatonia (13). Catatonia due to a mental disorder is not accompanied by disturbance of consciousness; memory is thought to be maintained even when symptoms appear in many instances. However, delirium is a type of disturbance of consciousness, and memory is thought to be impaired. Some patients recall their experiences after recovering from delirium (18, 19), and in catatonia due to a medical condition, consciousness is often impaired due to the influence of the medical condition, and some catatonia due to mental disorder, such as malignant catatonia, can display altered consciousness with autonomic instability (20). Electroencephalography (EEG) remains the most widely available physiological measure of delirium and reveals diffuse background slowing, typically in the delta range (8). Most catatonia tends to present with a normal EEG, but in one study, over 80% of catatonia caused by drugs or physical illness exhibited abnormal EEG findings, the most common being diffuse slowing (4). Two thirds of medical catatonia involved central nervous system (CNS)-specific disease, including encephalitis, neural injury, developmental disorders, structural brain pathology, or seizures. Whenever medical catatonia is considered, a workup directed at CNS-specific pathology is necessary (21). In addition, the presence of delirium strongly predicts a medical cause of catatonic features (4, 21), and a comprehensive evaluation for potential medical causes should be performed in suspected cases of both delirium and catatonia (Figure 1). Even in catatonia patients with psychiatric disorders, recent neuroimaging findings indicate increased neuronal activity in premotor areas, reduced GABA-A receptor density, and poor connectivity within the motor circuit (17). Thus, acute brain dysfunction includes both delirium and non-functional catatonia, and they often overlap. Further research is needed to better elucidate the specific contributions of the various potential mechanisms associated with both. It should also prompt a reevaluation of the conceptual model of acute brain dysfunction.
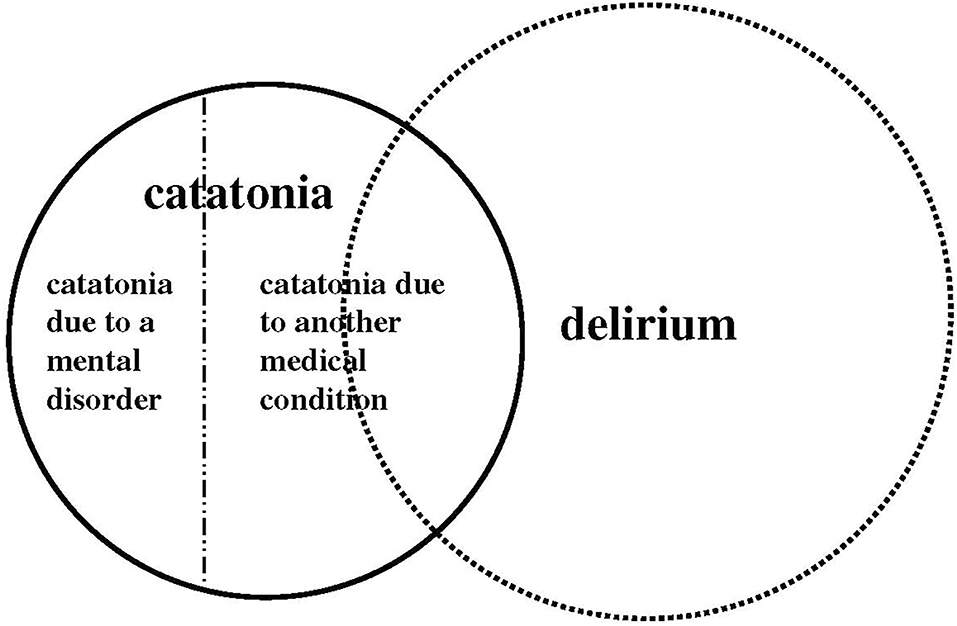
Figure 1. Schematic image of the overlap of symptoms between catatonia and delirium according to the DSM-5 diagnostic criteria.
MT, KI, and TI planned, organized, and selected the papers be included in the special issue. All authors contributed to the article and approved the submitted version.
This work was partly supported by JSPS KAKENHI Grant Number JP19K08071.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. Kendler KS. The development of Kraepelin's mature diagnostic concept of catatonic dementia praecox: a close reading of relevant texts. Schizophr Bull. (2020) 46:471–83. doi: 10.1093/schbul/sbz101
3. Fink M, Taylor MA. The many varieties of catatonia. Eur Arch Psychiatry Clin Neurosci. (2001) 251 (Suppl. 1):I8–13. doi: 10.1007/PL00014200
4. Oldham MA, Lee HB. Catatonia Vis-À-Vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. (2015) 37:554–9. doi: 10.1016/j.genhosppsych.2015.06.011
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder. 5th ed. Washington, DC: American Psychiatric Publishing (2013).
6. Llesuy JR, Coffey MJ, Jacobson KC, Cooper JJ. Suspected delirium predicts the thoroughness of catatonia evaluation. J Neuropsychiatry Clin Neurosci. (2017) 29:148–54. doi: 10.1176/appi.neuropsych.15090230
7. Lipowski ZJ. Delirium (acute confusional states). JAMA. (1987) 258:1789–92. doi: 10.1001/jama.1987.03400130103041
8. Neufeld KJ, Thomas C. Delirium: definition, epidemiology, and diagnosis. J Clin Neurophysiol. (2013) 30:438–42. doi: 10.1097/WNP.0b013e3182a73e31
9. Jaimes-Albornoz W, Serra-Mestres J. Prevalence and clinical correlations of catatonia in older adults referred to a liaison psychiatry service in a general hospital. Gen Hosp Psychiatry. (2013) 35:512–6. doi: 10.1016/j.genhosppsych.2013.04.009
10. Grover S, Ghosh A, Ghormode D. Do patients of delirium have catatonic features? An exploratory study. Psychiatry Clin Neurosci. (2014) 68:644–51. doi: 10.1111/pcn.12168
11. Connell J, Kim A, Brummel NE, Patel MB, Vandekar SN, Pandharipande P, et al. Advanced age is associated with catatonia in critical illness: results from the delirium and catatonia prospective cohort investigation. Front Psychiatry. (2021) 12:673166. doi: 10.3389/fpsyt.2021.673166
12. Nunes AL, Cheniaux E. Delirium and mania with catatonic features in a Brazilian patient: response to ect. J Neuropsychiatry Clin Neurosci. (2014) 26:E1–3. doi: 10.1176/appi.neuropsych.12110262
13. Penland HR, Weder N, Tampi RR. The catatonic dilemma expanded. Ann Gen Psychiatry. (2006) 5:14. doi: 10.1186/1744-859X-5-14
14. Regal P. Malignant catatonia versus delirium. Am J Med. (2017) 130:e33. doi: 10.1016/j.amjmed.2016.07.033
15. World Health Organization. The Icd-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization (1992).
16. Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. (2003) 160:1233–41. doi: 10.1176/appi.ajp.160.7.1233
17. Walther S, Stegmayer K, Wilson JE, Heckers S. Structure and neural mechanisms of catatonia. Lancet Psychiatry. (2019) 6:610–9. doi: 10.1016/S2215-0366(18)30474-7
19. Grover S, Ghosh A, Ghormode D. Experience in delirium: is it distressing? J Neuropsychiatry Clin Neurosci. (2015) 27:139–46. doi: 10.1176/appi.neuropsych.13110329
20. Perju-Dumbrava L, Kempster P. Movement disorders in psychiatric patients. BMJ Neurol Open. (2020) 2:e000057. doi: 10.1136/bmjno-2020-000057
Keywords: catatonia, delirium, acute brain dysfunction, diagnostic concepts, overlap
Citation: Tachibana M, Ishizuka K and Inada T (2022) Catatonia and Delirium: Similarity and Overlap of Acute Brain Dysfunction. Front. Psychiatry 13:876727. doi: 10.3389/fpsyt.2022.876727
Received: 15 February 2022; Accepted: 02 March 2022;
Published: 07 April 2022.
Edited by:
Jorge Cuevas Esteban, Hospital Germans Trias i Pujol, SpainReviewed by:
Max Fink, Stony Brook Medicine, United StatesCopyright © 2022 Tachibana, Ishizuka and Inada. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Toshiya Inada, dG9zaGl5YS5pbmFkYUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.