
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 25 April 2022
Sec. Anxiety and Stress Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.868191
 Justyna Kosydar-Bochenek1
Justyna Kosydar-Bochenek1 Sabina Krupa1
Sabina Krupa1 Francesca Favieri2
Francesca Favieri2 Giuseppe Forte2,3
Giuseppe Forte2,3 Wioletta Medrzycka-Dabrowska4*
Wioletta Medrzycka-Dabrowska4*Objective: Translate and investigate psychometric properties of the Polish version of COVID-19-PTSD in a sample of healthcare workers.
Methods: The PTSD symptoms were investigated among 184 participants (physicians, nurses, and paramedics). The respondents completed Post-Traumatic Stress Disorder Related to COVID-19 Questionnaire (COVID-19-PTSD) via online survey. The psychometric properties (i.e., internal consistency, validity, and reliability) of the Polish version of COVID-19-PTSD were analyzed.
Results: The findings showed that the Polish version of COVID-19-PTSD is a reliable instrument. The total and subscale scores demonstrated good internal consistency. We also found that the prevalence of PTSD was reported at around 32% of healthcare workers.
Discussion: The Post-Traumatic Stress Disorder Related to COVID-19 Questionnaire (COVID-19-PTSD) is a first tool designed to assess the severity of PTSD symptoms related to the pandemic. The findings of our study confirmed good validity and reliability of the Polish version of COVID-19-PTSD which can be recommended to be used as a reliable screening tool to conduct psychological screening among Polish healthcare workers.
Post-traumatic stress disorder (PTSD) refers to a mental health condition occurring in an individual who experienced/witnessed a terrifying or traumatic event that is beyond the limit of personal psychological endurance. PTSD may result in significant psychological distress, cognitive dysfunction, and impairment in social and occupational areas of functioning (1). The four core symptoms of PTSD include (i) recurrent thoughts and feelings concerning the traumatic experience, (ii) constant avoidance of stimuli related to the traumatic event, (iii) negative changes in cognition and mood, and (iv) sustained increased alertness (2).
The outbreak of a pandemic, with no vaccines or any effective medical therapy, such as COVID-19, could be described as a traumatic experience due to its acute and chronic implications at both individual and community levels (3, 4). Being a major viral outbreak in the 21st century, the COVID-19 pandemic has resulted in an extraordinary burden on mental health worldwide (5, 6). Proportionately elevated rates of symptoms of anxiety (6.33–50.9%), depression (14.6–48.3%), post-traumatic stress disorder (7–53.8%), psychological distress (34.43–38%), and stress (8.1–81.9%) are observed in the general population at the times of the first outbreak of COVID-19 pandemic in China, Spain, Italy, Iran, the US, Turkey, Nepal, and Denmark (5, 7–11).
Moreover, the pandemic experience has called attention to its consequences on mental health among healthcare workers involved in the first-line response. Frontline health workers are experiencing severe stress and anxiety, facing increased workloads, and are being confronted with great suffering and high mortality rates (12). They are often forced to make difficult decisions that can cause ethical dilemmas with traumatic consequences. Their stress is aggravated by the risk of infection and transmission to the family. Unfortunately, there have been reports of social stigmatization of people working with people with COVID-19, while what they need is everyone's support. These experiences can have long-term emotional and functional consequences (13). Numerous studies demonstrated that a great share of healthcare workers is at significant risk for developing PTSD and Posttraumatic Stress Symptoms (PTSS) (14). Therefore, adequate mental health counseling for medical staff and other healthcare workers involved is a crucial task for public health (15, 16).
Escalation of PTSD during the pandemic requires a reliable assessment tool allowing to evaluate this condition. The present study investigates the Post-Traumatic Stress Disorder Related to COVID-19 Questionnaire (COVID-19-PTSD) - a 19-item self-report measure assessing the presence and severity of PTSD symptoms. From a clinical perspective the COVID-19 pandemic may be considered as a traumatic event. Therefore, psychological support to mitigate short- and long-term psychopathological consequences of the COVID-19 pandemic seem to be necessary (4). This study aimed to translate and investigate psychometric properties of the Polish version of COVID-19-PTSD in a sample of healthcare workers.
A prospective descriptive study was conducted.
A new self-report questionnaire (COVID-19-PTSD) was developed based on the PTSD Checklist for DSM-5 (PCL-5) questionnaire and administered to investigate its psychometric properties. The respondents are instructed as follows: “Referring to the current situation, characterized by the COVID-19 outbreak and the social distancing measures implemented to contain it, indicate how you feel for each of the following dimensions” (4).
The COVID-19-PTSD questionnaire includes 19 items, requiring a response on a 5-point Likert scale, from 0 (not at all) to 4 (extremely). To calculate the scale scores, add the items. A COVID-19-PTSD score of 26 was deemed to correctly categorize a participant as having or not having significant PTSD symptoms (4).
The psychometric properties of COVID-19-PTSD have been thoroughly investigated among the Italian population. The studies proved satisfactory psychometric properties of the COVID-19-PTSD questionnaire. Moreover, excellent internal consistency of all items was observed (Cronbach's α = 0.94). Cronbach's alpha for every item of the subscales was good in terms of the DSM-5 four-factors model (Cronbach's α = 0.70–0.86), as well as the seven-factors model (Cronbach's α = 0.52–0.85) (2). Confirmatory factor analyses results for Monofactorial Model, DSM-5 4-factors model and 7-factors model is shown in Table 1. COVID-19-PTSD questionnaire showed a significant correlation with the Impact of Event Scale—Revised (IES—R) (r = 0.70, p < 0.0001) which indicates good convergent validity. Moreover, significant positive correlations were found for all the IES—R subscales (ranging from 0.39 to 0.66) (4).
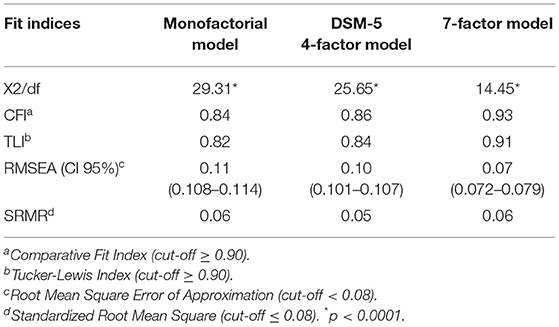
Table 1. Confirmatory factor analyses results for Monofactorial Model, DSM-5 4-factors model and 7-factors model.
According to the authors of the original questionnaire, COVID-19-PTSD is the first tool assessing PTSD in a situation of prolonged stress resulting from a pandemic (4). Therefore, it might be suitable to investigate its properties in other populations and professional groups.
The present study was conducted in two phases. The first phase was translation and cultural adaptation of the Italian version of COVID-19-PTSD into Polish. The second phase was the validation (face validity, content of COVID-19-PTSD). Consent was obtained from authors of original scale, who agreed and they also watch over the development of the Polish version. This study was conducted between May 1st and July 31th, 2021 that is 14 months from recording the first case of COVID-19 in Poland.
Before implementing the study in Poland, it was necessary to translate the scale and culturally adapt to Polish conditions. The authors of the original version of the scale were informed about the translation and expressed consent for the translation into Polish.
Two native translators fluent in Italian and Polish individually translated the Italian version of the instrument into Polish.
Two versions of the translation were reviewed and discussed item by item to achieve consensus regarding the best possible translation. The authors compared the two translations, and the final version was prepared after applying a few changes.
The preliminary version was then translated back into Italian by an experienced and certified language teacher without knowledge of the original version.
The back translation of the preliminary Polish version was then thoroughly compared with the original text regarding the necessity of performing adjustments. This back translation showed no substantial deviations from the original after close comparison and assessment performed by the translating authors. The translation was done by an independent translator specializing in medical translation, who accepted the version sent by the research team.
In order to examine the final version, 10 healthcare workers and researchers employed simultaneously at a University and a clinical hospital were randomly selected as critical judges. The people sent us their opinions about the difficulty, irrelevancy, and ambiguity of each item (qualitative face validity).
After combining some minor revisions, the final Polish version of the instrument was developed.
Convenience sampling was used in this study. Participants were recruited from the clinical hospital and one of the temporary COVID-19 hospitals established by the Polish government. Physicians, nurses, and paramedics with a high risk of infection and psychological stress were invited to participate in the study. We chose an online questionnaire to survey because face-to-face survey was impractical given the requirement of quarantine and risk of viral transmission from close personal interaction. Besides, the online survey was fast, easy and convenient for data collection and analysis. Participants were selected from those hospital departments that involved either direct contact care to suspected or confirmed 2019-nCoV cases. This included the emergency department, outpatient clinic, infectious disease, and intensive care unit. One selection criterion was that the current working environment is at high risk of infection, i.e., reported close contact with COVID-19 patients or pathogens. A total of 250 subjects were successfully recruited in this study. The questionnaire was sent to employees via e-mail with the management consent. A brief presentation informed the participants about the aims of the study, and electronic informed consent was required from each participant before starting the investigation. At the beginning participants were required to fill in a short demographic questionnaire, and to respond to questions about personal experience related to the COVID-19 outbreak. Then, the questionnaire was administered. To guarantee anonymity, no personal data, which enabled the identification of the respondents, was required. Due to the aim of the current study, the only inclusion criterion was to be at least 18 years of age and work as a doctor, a nurse, or a paramedic in the healthcare system. The completion of all questionnaires took about 10–15 min.
Descriptive analysis was used to characterize the study sample in terms of demographic information. For reliability, the internal consistency of COVID-19-PTSD was accessed using Cronbach's alpha coefficient, where 0.70 was considered satisfactory. In order to examine the influence of sociodemographic variables on the occurrence of PTSD, the chi-square test (χ2) was used to analyze the distribution of PTSD incidence in sociodemographic groups. The level of significance was at p < 0.05. Student's t-test was used to compare the mean levels of stress/anxiety/risk associated with the possibility of COVID-19 infection in the groups with and without PTSD. The level of significance was at p < 0.05. Analyses were performed using Statistica 13.3.
The link to the survey has been sent to 250 healthcare workers. A total of 189 respondents participated in the study. Of the total respondents that started the questionnaires, 97% (184 out of 189 people) completed the whole survey and were considered for the statistical analyses. There were 131 women (71% of the sample) and 53 men. The mean age of the participants was 34.32 (SD = 14.43), and the age ranged between 24 and 49 years. Most of the participants completed higher education at BSc level (56%), and 38% graduated from MSc studies (Table 2).
PTSD symptoms were evaluated according to the DSM-5-criteria. In the current study, we applied the 4-factors model which classifies PTSD symptoms into four specific criteria: Re-experiencing, Avoidance, Negative alterations in cognition and mood, and Increased arousal and reactivity. We also examined a seven-factors structure (Intrusion, Avoidance, Negative Affect, Anhedonia, Dysphoric arousal, Anxious arousal, and Externalizing behavior), and a A monofactorial structure of PTSD, according to the first version of COVID-19-PTSD.
Participants reported an average sum score of 17.47 (SD = 15.99) on the COVID-19-PTSD. A COVID-19-PTSD score of 26 was deemed to correctly categorize a participant as having or not having significant PTSD symptoms. The prevalence of PTSD, considering this cut-off score, was reported at around 32%. Means, standard deviations, minimum and maximum values for total score of COVID-19-PTSD and its subscales are presented in Table 3.
As a result of the analysis, more frequent occurrences of PTSD stress was found in women than in men (81 vr 19%; χ2 4.19; p = 0.04). The highest intensity of PTSD symptoms was observed in the group of emergency departments, while the lowest in staff of the outpatient clinic (29 vr 14%; χ2 23.47; p < 0.001). Higher percentage of PTSD was observed in people without COVID-19 risk factors (86 vr 14%; χ2 22.67; p < 0.001). The participants who were in quarantine had a higher total score of PTSD than healthcare workers who were not in quarantine (74 vr 26%; χ2 12.36; p = 0.002). Those infected with SARS-CoV-2 had a higher PTSD percentage than the ones who were not infected (38 vr 62%; χ2 9.54; p = 0.002). The subjects who knew someone who died of COVID-19 were significantly more likely to have a higher PTSD rate than those who did not know anyone who died of that disease (97 vr 3%; χ2 35.57; p < 0.001). A statistically significant relationship was found in the case of the level of education - people with higher education have a higher intensity of PTSD symptoms than people with post-secondary education (p < 0.1).
In participants without PTSD symptoms, the subjective assessment of the level of stress/anxiety/threat related to the possibility of COVID-19 infection was on average 4.46 ± 2.41 (median scores: 5 on a Likert scale from 1 to 10).
In people with PTSD, the assessment of the level of stress/anxiety/risk related to the possibility of COVID-19 infection was 6.67 ± 2.64 and was significantly higher than in the participants without PTSD and the average was 3.62 ± 1.76 (t = 8.02, p < 0.0001). The results are presented in Figure 1.
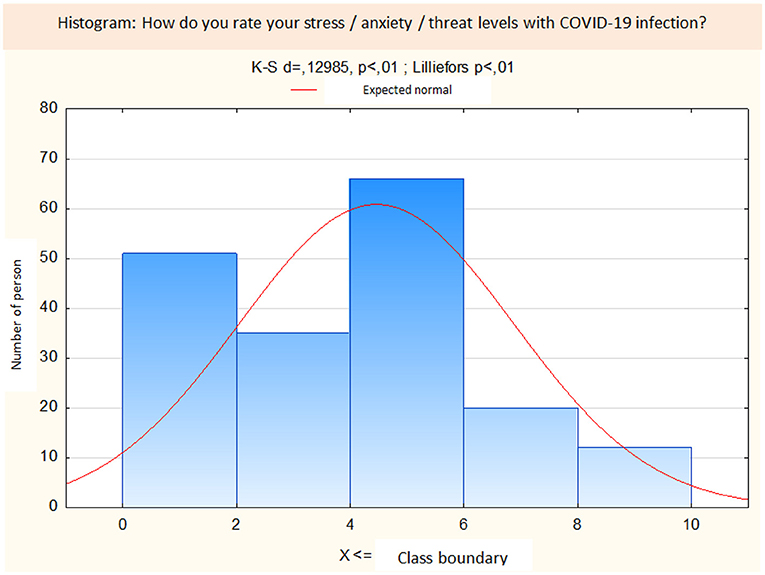
Figure 1. Distribution histogram of self-assessment of the level of stress/anxiety/risk related to the possibility of COVID-19 infection.
Cronbach's alphas were calculated for the internal consistency of COVID-19-PTSD. The Cronbach's coefficients of subscale scores in terms of the seven-factor model and DSM-5 four-factor model were summarized in Table 4. The Cronbach's alpha coefficient of the total score was 0.94, higher than the threshold of 0.70 and indicates high reliability of COVID-19-PTSD Polish version. Internal consistency reliability for each subscale is also satisfactory. The subscale results in the four-factor structure with good internal consistency (reliability ranging from 0.79 to 0.92). The mean correlation of the subscale scores with the total was ranging from 0.46 to 0.75. Also, the 7-factor structure evidenced good internal consistency (reliability from 0.72 to 0.92). The mean correlation of the subscale results with the whole was from 0.46 to 0.75. Based on the collected data, the Spearmann-Brown Coefficient was calculated, which is 0.85.
The present study aimed to test the reliability and validity of the Polish version of COVID-19-PTSD to investigate COVID-19 related trauma during COVID-19 pandemic among healthcare workers. We demonstrated that the Polish version of COVID-19-PTSD had good psychometric indices (i.e., internal consistency and validity). The internal consistency of the total (Cronbach's alpha = 0.94) and subscale scores in the context of seven-factor structures (alpha = 0.72–0.92) was comparable to original version of the scale (alpha for total score = 0.94, and for subscale score in terms of four-factor structure = 0.52–0.85) (4).
Another finding of the present study was that a high percentage of healthcare professionals (32%) reported PTSD symptoms (average sum score of 17.47). These results are in line with previous studies reporting a high percentage of PTSD symptomatology (29.5%) and ower psychological wellbeing related to COVID-19 diffusion in the Italian population (4, 9).
Our results using the PCL-5 scale to investigate PTSD linked to COVID also highlight that healthcare workers at pandemic frontline are at higher-risk becoming infected and experiencing negative psychological outcomes including PTSD and burnout, anxiety, fear of transmitting infection, feeling of incompatibility, depression, increased substance-dependence (17, 18). Moreover, mental issues linked to the health emergency (i.e., PTSD, anxiety, depression, and sleep disorders) are more often observed in healthcare workers, mainly those at pandemic frontline (19). Accordingly, increase of PTSD symptoms from moderate to severe among the healthcare worker was showed in different worldwide hospital, such as China (20, 21), Saudi Arabian (22), Italian (23), Spanish (24–26). Generally, the percentage of PTSD symptoms ranging from 10 to 40% of healthcare workers. Elevated post-traumatic symptomatology correlated with age below 50 and <10 years of work seniority (24). Higher incidence was found among frontline workers than non-frontline ones (21).
Moreover, moderate to severe symptoms of psychological distress were observed in the healthcare professionals: depression (21%), anxiety (20%) and PTSD (29%), associated with burnout, prior psychiatric history, profession and resilience, in spite of low levels of COVID contact (25, 26).
A recent meta-analysis on psychological effect of outbreaks such as SARS, MERS, COVID-19, ebola, and influenza A on doctors, nurses, and auxiliary staff indicated that from 11 to 73.4% of them had PTSD symptoms during epidemic/pandemic, while in 10–40% they lasted up to 3 years after the traumatic event (27). These results are in line with other findings demonstrating that 37.8% healthcare staff during SARS/MERS/COVID-19 complained of psychological distress (95%CI = 28.4–48.2%, k = 15, n = 24,346) while 20.7% of PTSD (95%CI = 13.2–31%, k = 11, n = 3,826) (25). Accordingly, it could be interesting to develop longitudinal studies to follow the trend of PTSD symptoms among the healthcare population.
The prevalence of PTSD in the study group seems to be high compared to other studies, which may be due to various reasons. The data was collected during the peak period of infection and death from COVID-19 in Poland, characterized by a large overload of the national health care system and the restrictive measures adopted by the government, which could be perceived as a very acute stressor. In addition, the respondents were asked to focus only on COVID-19 issues, which could have influenced the perception of the pandemic as a highly traumatic event.
In sum, healthcare staff are particularly in danger of developing adverse mental health outcomes due to coronavirus. However, character and prevalence of these outcomes still need to be investigated (28). Therefore, monitoring mental wellbeing of healthcare workers as well as providing psychological support are warranted at times of COVID-19 pandemic (25, 29).
The limitations of this study are as follows: First, as this is the first study investigating psychometric properties of COVID-19-PTSD in the adapted version, no similar study about validation is available in any language to compare cross-cultural similarities and differences in reliability and validity of the scale. Since the original COVID-19-PTSD was developed in Italy, it has been validated only in the Italian population so far, therefore, discussion was a challenge. However, the specific sample adopted for the validation of the Polish COVID-19-PTSD generated interesting insight in the analysis of the phenomenon in a particularly vulnerable population. The results of our study in the discussion are partially related to studies conducted with the use of the PCL-5 scale, which is the prototype of the COVID-19-PTSD scale. Secondly, since the sample size was small, the statistical strength of the study may be diminished. To obtain better generalizability, future studies on a larger population and other samples are needed. Finally, the data collection in the more chronic period of the pandemic (following the first year of pandemic spread) could be influenced the results of the analysis, although according to the previous literature the evidence may show the maintenance of critical thresholds of PTSD symptoms even in the period following the first and sudden outbreak.
The results of the present study suggest that the Polish version of COVID-19-PTSD demonstrated acceptable reliability and validity in the sample of Polish healthcare workers. This tool is very important from a clinical and practical point of view. The COVID-19-PTSD could be considered a sensitive screening tool in a population faced with pandemic, and it can represent a first step toward the assessment of the risk of PTSD. This instrument can be used to identify and reduce the risk of PTSD related to the COVID-19 pandemic. It may facilitate establishing and improving the warning mechanism of the PTSD crisis for early intervention of potential PTSD patients during and after 2019-nCoV disaster. Furthermore, COVID-19-PTSD is a time sparing tool due to its simplicity and small number of items. This is the first and comprehensive tool that is DSM-5 compliant and refers to the COVID-19 pandemic as a traumatic event. The COVID-19-PTSD questionnaire may also be useful for measuring symptom severity of PTSD in other populations. For better generalizability, future studies on a larger population and other samples are needed. Focusing on the risk of PTSD during the COVID pandemic, may lead to the development of effective prevention programs and therapeutic interventions. The impact of COVID-19 on the physical and mental health of healthcare workers should become a priority of the global public health strategies. Comprehensive Understanding PTSD is possible if further research is conducted. It is important to undertake research on different groups. Thanks to the from pathogenesis to intervention approach, it is possible to create a program that reduces PTSD in healthcare workers.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Bioethics Committee of the University of Rzeszow (KBE No. 13/11/2020). The patients/participants provided their written informed consent to participate in this study.
JK-B: conceptualization and resources. FF: formal analysis. JK-B and SK: methodology. WM-D: supervision. SK, GF, and WM-D: writing—original draft. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cheng P, Xu L-Z, Zheng W-H, Ng RMK, Zhang L, Li L-J, et al. Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. J Affect Disord. (2020) 277:368–74. doi: 10.1016/j.jad.2020.08.038
2. Auxéméry Y. Post-traumatic psychiatric disorders: PTSD is not the only diagnosis. Presse Med. (2018) 47:423–30. doi: 10.1016/j.lpm.2017.12.006
3. Bridgland VME, Moeck EK, Green DM, Swain TL, Nayda DM, Matson LA, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE. (2021) 16:e0240146. doi: 10.1371/journal.pone.0240146
4. Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Environ Res Public Health. (2020) 17:4151. doi: 10.3390/ijerph17114151
5. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
6. Chidiebere Okechukwu E, Tibaldi L, La Torre G. The impact of COVID-19 pandemic on mental health of nurses. Clin Ter. (2020) 171:e399–400. doi: 10.7417/CT.2020.2247
7. Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. (2020) 75:12–20. doi: 10.1016/j.sleep.2020.05.011
8. Forte G, Favieri F, Tambelli R, Casagrande M. The enemy which sealed the world: effects of COVID-19 diffusion on the psychological state of the Italian population. J Clin Med. (2020) 9:1802. doi: 10.3390/jcm9061802
9. Favieri F, Forte G, Tambelli R, Casagrande M. The Italians in the time of coronavirus: psychosocial aspects of the unexpected COVID-19 pandemic. Front Psychiatry. (2021) 12:551924. doi: 10.3389/fpsyt.2021.551924
10. Casagrande M, Forte G, Tambelli R, Favieri F. The coronavirus pandemic: a possible model of the direct and indirect impact of the pandemic on sleep quality in Italians. Nat Sci Sleep. (2021) 13:191–9. doi: 10.2147/NSS.S285854
11. El-Hage W, Hingray C, Lemogne C, Yrondi A, Brunault P, Bienvenu T, et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks? Encephale. (2020) 46:S73–80. doi: 10.1016/j.encep.2020.04.008
12. Unützer J, Kimmel RJ, Snowden M. Psychiatry in the age of COVID-19. World Psychiatry. (2020) 19:130–1. doi: 10.1002/wps.20766
13. Adhanom Ghebreyesus T. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry. (2020) 19:129–30. doi: 10.1002/wps.20768
14. Carmassi C, Foghi C, Dell'Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. (2020) 292:113312. doi: 10.1016/j.psychres.2020.113312
15. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Hear J Acute Cardiovasc Care. (2020) 9:241–7. doi: 10.1177/2048872620922795
16. Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I. COVID-19 pandemia and public and global mental health from the perspective of global health securit. Psychiatr Danub. (2020) 32:6–14. doi: 10.24869/psyd.2020.6
17. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. (2020) 14:779–88. doi: 10.1016/j.dsx.2020.05.035
18. Restauri N, Sheridan AD. Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: intersection, impact, and interventions. J Am Coll Radiol. (2020) 17:921–6. doi: 10.1016/j.jacr.2020.05.021
19. Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, Lulli LG, et al. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. (2020) 17:7857. doi: 10.3390/ijerph17217857
20. Geng S, Zhou Y, Zhang W, Lou A, Cai Y, Xie J, et al. The influence of risk perception for COVID-19 pandemic on posttraumatic stress disorder in healthcare workers: a survey from four designated hospitals. Clin Psychol Psychother. (2021) 28:1146–59. doi: 10.1002/cpp.2564
21. Yang X, Chen D, Chen Y, Wang N, Lyv C, Li Y, et al. Geographical distribution and prevalence of mental disorders among healthcare workers in China: a cross-sectional country-wide survey: a cross-sectional study to assess mental disorders of healthcare workers in China. Int J Health Plann Manage. (2021) 36:1561–74. doi: 10.1002/hpm.3186
22. Alshehri AS, Alghamdi AH. Post-traumatic stress disorder among healthcare workers diagnosed with COVID-19 in Jeddah, Kingdom of Saudi Arabia, 2020 to 2021. Cureus. (2021) 13:e17371. doi: 10.7759/cureus.17371
23. Lamiani G, Borghi L, Poli S, Razzini K, Colosio C, Vegni E. Hospital employees' well-being six months after the COVID-19 outbreak: results from a psychological screening program in Italy. Int J Environ Res Public Health. (2021) 18:5649. doi: 10.3390/ijerph18115649
24. Marco CA, Larkin GL, Feeser VR, Monti JE, Vearrier L. Post-traumatic stress and stress disorders during the COVID-19 pandemic: survey of emergency physicians. J Am Coll Emerg Phys Open. (2020) 1:1594–601. doi: 10.1002/emp2.12305
25. Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Aust Psychiatry Bull R Aust New Zeal Coll Psychiatr. (2021) 29:26–30. doi: 10.1177/1039856220965045
26. Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and Burnout in Spanish Health Personnel during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:5514. doi: 10.3390/ijerph17155514
27. Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. (2020) 22:43. doi: 10.1007/s11920-020-01166-z
28. Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J Affect Disord. (2020) 275:48–57. doi: 10.1016/j.jad.2020.06.022
Keywords: COVID-19, pandemic, post-traumatic stress disorder, PTSD, healthcare workers, self-report questionnaire
Citation: Kosydar-Bochenek J, Krupa S, Favieri F, Forte G and Medrzycka-Dabrowska W (2022) Polish Version of the Post-traumatic Stress Disorder Related to COVID-19 Questionnaire COVID-19-PTSD. Front. Psychiatry 13:868191. doi: 10.3389/fpsyt.2022.868191
Received: 02 February 2022; Accepted: 16 March 2022;
Published: 25 April 2022.
Edited by:
Xiancang Ma, First Affiliated Hospital of Xi'an Jiaotong University, ChinaReviewed by:
Roberto Ariel Abeldaño Zuñiga, University of the South Sierra, MexicoCopyright © 2022 Kosydar-Bochenek, Krupa, Favieri, Forte and Medrzycka-Dabrowska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wioletta Medrzycka-Dabrowska, d2lvbGV0dGEubWVkcnp5Y2thLWRhYnJvd3NrYUBndW1lZC5lZHUucGw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.