
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 23 June 2022
Sec. Psychological Therapy and Psychosomatics
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.862289
This article is part of the Research Topic Women in Psychiatry 2022: Psychological Therapies View all 6 articles
Background: Imagery Rescripting (ImR) has proved to be effective in the treatment of different mental disorders as an integral part of broader clinical protocols or as a standalone technique. ImR has also been successfully incorporated as part of group Schema Therapy treatment; however, to the best of our knowledge, it has never been assessed as a standalone technique in a group setting.
Aim: In this study, we focused on ImR delivered via telehealth in groups and we aimed to assess whether group ImR is effective in responding to basic emotional needs, in changing participants’ affective state, and in reducing dysfunctional beliefs. We also wanted to assess whether memory realism is associated with a greater effectiveness of the technique.
Methods: A total of 52 participants were presented with 3 ImR sessions on childhood memories related to the current dysfunctional belief that elicited more suffering.
Results: The technique was effective in facilitating the retrieval of a memory in almost the entire sample (in the range of 92.3–100%). Overall, memory realism values (level of vividness, ability to immerse, and participants’ distance from the images) were high in all three sessions. Almost all participants were reported having their needs met during ImR (89.7%). Importantly, need satisfaction was associated with the ability to immerse in the image. In addition, the intensity of the dysfunctional belief decreased significantly from pre-test to Session 3. The technique also changed the affective state, reducing arousal. Importantly, we also observed a general reduction in shame levels from the first to the third session.
Conclusion: A telehealth delivered ImR group intervention on childhood memories provides cognitive and emotional improvement. Along with the ability to satisfy the patient’s basic emotional needs, the technique seems to be effective in modifying maladaptive beliefs encapsulated in memory.
Imaginative techniques have been used in therapeutic contexts, for several centuries and have now been extensively integrated into the Schema Therapy (ST) approach (1, 2). Imagery Rescripting (ImR) is a therapeutic technique that aims to reduce the distress associated with negative memories of early aversive experiences. It consists of prompting patients to rescript the autobiographical memory in order to satisfy their unmet needs. Although these basic needs are considered to be important in the genesis of maladaptive beliefs in Schema Therapy, studies specifically monitoring in which specific emotional needs are frustrated are scarce.
One of the salient features of ImR is its effectiveness in the treatment of different mental disorders. Over the past 10 years, abundant evidence proving efficacy has been collected, using ImR as both an integral part of broader clinical protocols and as a standalone technique (3, 4).
When considered as part of broader clinical protocols, ImR has proved to be effective in reducing the symptoms of posttraumatic stress disorder (PTSD) (5–7), social phobia (8, 9), and personality disorders (10). However, in these studies, ImR has not been experimentally isolated from cognitive restructuring.
The technique has proved to be effective also as a standalone technique in the treatment of PTSD (11–15), social phobia (16, 17), body dysmorphic disorder (18, 19), bulimia (20), depression (21, 22), and obsessive-compulsive disorder (OCD) (23–26). Recently, ImR has also been found to be effective at treating trauma-affected voice hearers (27).
The aforementioned studies delivered ImR individually, but ImR has also been successfully incorporated into Group Schema Therapy treatment of borderline personality disorder and eating disorder (28–32). The application of Group Schema Therapy has been described in the work by Farrel et al. (32).
However, to the best of our knowledge, the efficacy of group ImR on early childhood memories as a standalone technique has not yet been studied. Thus, in this study, we focused on ImR delivered in groups.
Initially, this research was conceived with the idea of delivering group ImR in person, but the spread of the COVID-19 pandemic forced the authors to perform the procedure via telehealth. A recent study supports the delivery of ImR via telehealth showing that, as long as privacy is granted, it is not less effective than face-to-face delivery (33). Group telehealth imagery setting might have the clear advantage of containing therapy costs. Moreover, it enables geographical distances to be reduced and thus allows access to population groups from more rural areas, which are often prevented from accessing clinical and research centers.
Notably, a growing body of literature has shown that the ability to become immersed in the autobiographical memory affects ImR outcome (34–37). Therefore, in this study, we assessed whether memory realism (level of vividness, ability to immerse, and participants’ distance from the images) was associated with a greater effectiveness of the group technique in meeting the subject’s core needs and in changing the dysfunctional belief attached to the memory.
Thus, the main purposes of this research were to verify the effectiveness of a group ImR intervention via telehealth. Specifically, we aimed to assess whether group ImR is effective in (i) responding to the basic emotional needs of participants as defined by ST, (ii) reducing dysfunctional beliefs and, and (iii) changing participants’ affective state.
In line with previous observations, we hypothesize that group ImR is effective in producing a cognitive and emotional improvement. In addition, we expect memory realism features to affect ImR effectiveness in meeting participants’ needs.
The sample was composed of 52 participants (48 F). Participants were recruited among the students and alumni of the School of Cognitive Psychotherapy (SPC) of Rome (Italy). Specifically, the study was advertised through the School newsletter. Those who were interested in taking part in the study could volunteer by contacting the authors. Importantly, participants were only included if they did not have previous experience with ImR (e.g., during therapy) or if they have not been theoretically introduced to this technique (e.g., during classes). Along with age, sex, and education level, participants were asked if they have ever been diagnosed with a psychiatric disorder, if they were currently (or had in the past) undertaking psychotherapy, and if they were taking psychiatric medication. Participants were from 10 different Italian regions, and mean age was 31.5 (SD = 5.06, range = 26–60). Notably, 51% had a university degree, 47.1% were specialized or held a PhD, and 2% had a high school diploma. Moreover, 13.46% of the entire sample was reported to have received a psychiatric diagnosis (i.e., three panic disorder; one anorexia nervosa; one cyclothymia; two major depressive disorder). Notably, 22% of the sample was currently undertaking psychotherapy and 2% was taking psychiatric medication.
All participants were given a digital informed consent form and gave their informed consent prior to inclusion in the study by choosing to proceed with the surveys. Procedures were carried out in accordance with the principles of the Declaration of Helsinki and were approved by the Guglielmo Marconi University Ethical Committee (Protocol Date: 24 March 2020).
All participants responded to the questionnaire online through the survey platform Question Pro.1 They were recruited by means of an advertisement, circulated by SPC. Participants did not receive any form of payment for their participation in the study. After signing the informed consent, they completed the Young Schema Questionnaire- Short Form (YSQ-SF) (38) and the Personality Belief Questionnaire- Short Form (PBQ-SF) (39). In addition, they were asked to choose the statement that evoked in them the greatest suffering among the 140 YSQ-SF and PBQ-SF items. Participants were then presented with 3 ImR sessions, as in previous studies (16, 26), starting from memories related to these statements (i.e., the dysfunctional belief) which currently elicits more suffering.
A week after completing the questionnaires, participants received the first ImR session. The three ImR sessions were delivered weekly.
Different ways of conducting the study of ImR have been proposed, but, in this study, we employed the three-stage one proposed by Arntz and Weertman (40), adapting it to the group setting which is in line with the work by Farrell et al. (32).
Participants were asked to close their eyes and imagine themselves in a previously identified safe place. Then, they were asked to think about the last time they experienced the negative self-belief they selected among the 140 YSQ and PBQ items and to focus on the emotional and somatic experience connected to this belief. This method of emotional activation is designed to bring about a connection to the memory of a childhood event. It is called a “bridge” (41), because it enables the emotions and/or somatic experience of a present event to connect with a memory of a past event in which the same feelings were experienced.
The memory retrieved was then revisited by the participant in detail, from the perspective of the participant as a child. After reliving the scene from the child’s perspective, the therapist asked the participant to change the point of view and to relive the past experience again, this time observing it through the eyes of the participant’s adult-self. In this study, the participant enters the image as an adult and performs all the actions that lead to the resolution of suffering and to the satisfaction of the child-self’s frustrated needs (e.g., protecting, taking care, being empathic, and setting limits).
Importantly, to increase the replicability, in each session, participants heard the same script (read by the first author of this study), which was adapted from the work of Farrell et al. (28). The script consisted of the following steps: (1) Instructions; (2) group safe place; (3) focusing on the recent situation that activates the belief; (4) floating back; (5) rescripting the memory emerged via the bridge emotion; and (6) back to the safe place (see Supplementary Appendix).
Subsequently, they were presented with an ad hoc questionnaire investigating memory features (see below). Before and after each ImR session, they assessed their affective state on the positive affect and negative affect scale (PANAS) (42).
The Young Schema Questionnaire short form (YSQ-SF) (38) is a 75-item self-report inventory that assesses 15 Early Maladaptive Schemas (EMS) proposed by Young et al. (1). Each item in the questionnaire is a statement based on a maladaptive belief as defined by schema theory. Respondents are asked to rate the degree to which they agree with the statements on a 6-point Likert scale (1–6). A mean score is calculated for each EMS, a higher score representing a higher endorsement of the EMS in question. Since no Italian validation of this reduced version of the YSQ is available, we selected 75 items on the basis of the English validation study (43), which reported the Cronbach’s alpha coefficient ranging from 0.80 to 0.93.
The Personality Belief Questionnaire Short form [PBQ-SF; (39)] is a 65-item self-report inventory developed as a clinical and research instrument to assess dysfunctional beliefs associated with personality disorders, as described by the Diagnostic and Statistical Manual for Mental Disorders (44). The measure was developed starting from the original PBQ 126-items’ form (45). A total of 65 items were selected among the corresponding items contained in the 126 items’ PBQ Italian validation (46). The inventory assesses the specific beliefs related to 9 personality disorders, including Avoidant, Dependent, Passive-aggressive, Obsessive-compulsive, Antisocial, Narcissism, Histrionic, Schizoid, and Paranoid. PBQ-SF is a self-report Likert-type questionnaire that is scored from 0 (“I don’t believe it at all.”) to 4 (“I believe it totally.”). The Cronbach’s alpha coefficient for the total PBQ-SF score was α = 0.97 (39). The Cronbach’s alpha values for the single scales were as follows: Avoidant (0.84), Dependent (0.89), Passive-Aggressive (0.86), Obsessive-Compulsive (0.90), Antisocial (0.80), Narcissistic (0.83), Histrionic (0.89), Schizoid (0.79), and Paranoid (0.91).
The PANAS consists of 10 negative and 10 positive mood terms and a 5-point Likert-type response scale from 1, very slightly or not at all, to 5, extremely, with scale scores ranging between 10 and 50 (42). In this study, the scale scores were calculated to range between 0 and 40 (i.e., scale score −10), and respondents were asked to indicate how often they felt that way in general. Evidence of the validity of the Italian version is obtained from the pattern of the relationship with personality and depression measures. As reported by Terracciano (47), the relationship between PA and Extraversion and NA and Neuroticism found with this Italian sample replicated the American findings and the Cronbach’s alpha coefficient score ranged from 0.83 to 0.87 (48). The positive affect subscale reflects the extent to which a person feels interested, excited, strong, enthusiastic, proud, alert, inspired, determined, attentive, and active. On the other hand, the negative affect subscale includes descriptors such as stressed, upset, guilty, scared, hostile, irritable, ashamed, nervous, jittery, and afraid.
Memory features were investigated by means of an ad hoc questionnaire. Specifically, participants were asked if the technique was able to facilitate the retrieval of a memory (binary yes/no response). Furthermore, they were asked to report on a five-point scale how vivid the memory retrieved was, how much they were able to emotionally immerse into the memory, and how much far the images were. Subsequently, they were asked to report their age at the time of the memory and indicate which needs were frustrated in this memory, among the five core emotional needs described by Young et al. (1). Specifically, in the questionnaire, core emotional needs were described as follows (translated from the Italian): (i) “Secure attachment (protection, safety, stability, care, and acceptance)”; (ii) “Autonomy, Sense of competence, and Sense of identity”; (iii) “Realistic limits”; (iv) “Freedom to express emotions”; and (v) “Spontaneity and play.” Participants could indicate whether the need was frustrated providing a yes/no answer. After each ImR session, participants further assessed on a three-point scale to what extent they felt their needs were met during the rescripting (“0” = not at all; “1” = in part; “2”completely). Finally, before Session 1 and after Session 3, participants were assessed on a six-point scale to determine how much they believed in the dysfunctional belief they identified in the pre-test phase.
Descriptive statistics were employed to determine the percentage of participants who were able to retrieve a childhood memory; participants’ mean age (and standard deviations) in the memories and memory realism measures (mean and standard deviations across session). In addition, we assessed with which frequency participants reported unmet needs in each of the five domains and the percentage of participants who reported that their needs were met through rescripting. Furthermore, with the aim to test the association between realism measures and needs’ satisfaction, we performed Spearman correlations between average realism measures and average needs’ satisfaction scores.
Putative differences in the strength of the dysfunctional belief between the pre-test and the third ImR session were assessed by means of a paired sample t-test. Finally, differences in participants’ affective state (i.e., PANAS values) before and after each session were assessed by means of a series of paired sample t-tests.
As shown in Table 1, the technique was effective in facilitating the retrieval of a memory in almost the entire sample in all the three sessions. The earliest memory retrieved was of being 3 years old, the oldest was of being 16 years old. In addition, mean memory realism values were good in all three sessions. No differences in these measures were found across sessions other than participants, which revealed that they were able to immerse themselves in the memory more effectively in session 1 [F(1.98, 98.86) = 13, p < 0.001, ηp2 = 0.206, Post hoc tests: all Adj.ps < 0.001]. When asked about the type of unmet need in the memory, the majority of participants reported unmet needs in the Secure Attachment domain, followed by the Freedom to express emotions and needs’ domain and the Autonomy/sense of identity domain. Fewer unmet needs were reported in the Spontaneity and Play domain and in the Realistic Limit domain. Almost the entire sample was reported to be able to meet their emotional needs through rescripting (89% on average).
Spearman correlation coefficients and p-values are reported in Table 2. We found an association between the ability to immerse in the memory and needs’ satisfaction levels (ρ = 0.458, p = 0.000). No other significant association was found.
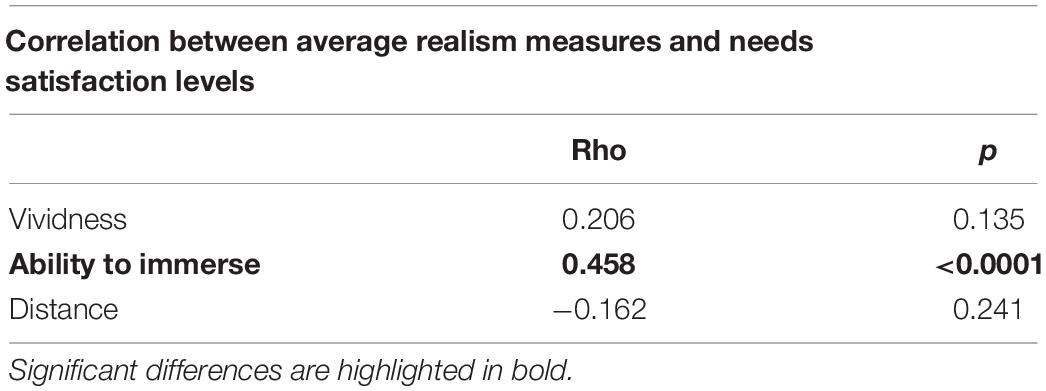
Table 2. Results of the Spearman correlation between memories average realism measures and needs satisfaction levels.
The paired-sample t-test performed on dysfunctional belief measures determined a significant difference between Session 1 (M = 4.24, SD = 1.11) and Session 3 (M = 3.02, SD = 1.22), indicating a significant decrease of the dysfunctional belief after 3 ImR weekly sessions (t = 5.20, p < 0.001, and Cohens’d = 0.74).
The repeated measures t-tests performed on PANAS measures determined some changes in the affective state after each ImR session. After Session 1, participants felt significantly more distressed, strong, inspired, proud, less ashamed, scared, active, attentive, and enthusiastic. After Session, 2 participants felt significantly less attentive, active, and ashamed. After Session 3, participants felt significantly stronger and prouder and less alerted, active, attentive, distressed, irritable, nervous, and ashamed. Overall, Table 3 shows the complete results of the t-tests.
To observe putative (increasing or decreasing) trends in PANAS scores between sessions, we compared mean PANAS values after S1, S2, and S3, by means of a repeated measure ANOVA. Only the emotions that resulted in significant changes after the ImR in each session (according to the t-test results, see Table 3) were included in the latter analysis.
The 10 repeated measure ANOVAs, with a Greenhouse-Geisser correction, performed separately on each PANAS emotion which significantly changed after ImR, determined a significant difference between sessions in Distress scores [F(2, 102) = 8.36, p < 0.001, η2p = 0.05]. Post hoc tests using the Bonferroni correction revealed that distress decreased from S1 (M = 1.92; SD = 0.86) to S3 (M = 1.40; SD = 0.82) (Adj.p < 0.001). No significant difference was observed between S1 and S2 (M = 1.69; SD = 0.91) and between sessions 2 and 3 (all ps < 0.05, NS). Moreover, a significant change in Active scores was observed [F(2, 102) = 7.07, p = 0.001, η2p = 0.05]. Bonferroni correction revealed that participants were reported to be more active in S1 (M = 3.17; SD = 0.87) as compared to S2 (M = 2.71; SD = 1.02) (Adj.p = 0.008) and S3 (M = 1.40; SD = 0.82) (Adj.p = 0.008). No significant difference was observed between sessions 2 and 3 (all ps < 0.05, NS). Finally, a significant change was revealed in Shame scores [F(2, 102) = 7.21, p = 0.001, η2p = 0.206]. Specifically, participants were reported to feel less ashamed after S3 (M = 1.19; SD = 0.52) as compared to post scores in S1 (M = 1.58; SD = 0.87) (Adj.p = 0.005). No significant difference was observed between S1 and S2 (M = 1.33; SD = 0.55) and between Sessions 2 and 3 (all ps < 0.05, NS). No other significant effect was found (all ps < 0.05, NS). Significant results are reported in Figure 1.

Figure 1. The differences in mean post ImR scores of distress, activation, and shame levels between sessions. **p < 0.01; ***p < 0.001.
The aim of this study was to assess the effectiveness of a telehealth delivered ImR group intervention on childhood memories, in producing cognitive and emotional improvement. One of the first questions, we attempted to reply, was if ImR group intervention would be able to make participants retrieve memories. From the data, it is found that group ImR was effective in facilitating the retrieval of childhood memories. Monitoring the types of frustrated needs was not the main aim of this study but it is nevertheless interesting given their central role in the genesis of maladaptive beliefs in Schema Therapy. Specifically, memories were associated mostly with the frustration of secure attachment needs, than with the need for autonomy, competence, and sense of identity, and subsequently with the need to express one’s own needs and emotions, the need for spontaneity and play, and finally with the need for realistic limits. Group ImR was effective in facilitating needs’ satisfaction in almost the totality of our sample. This result is very important because in ImR individual delivery, patients’ need satisfaction is the ultimate goal of the intervention, which is concluded by the therapist only when participants report that they are emotionally satisfied (36). Along with the ability to satisfy the patient’s basic emotional needs, the technique seems to be effective in modifying maladaptive beliefs encapsulated into memory as already reported by Lee and Kwon (16), Wild et al. (8, 9), Cooper (20), in clinical samples, and by Otera et al. (49) in a non-clinical sample. The change in the maladaptive belief is observable particularly between the pre-test and the second and third sessions. This result is consistent with previous studies that show that the efficacy of the ImR interventions is notable a week after the first intervention (4, 50). As several studies have already proposed, three ImR sessions seem to be effective in modifying dysfunctional intakes or symptomatic conditions (16, 26).
Memories evoked through the group script were generally described as vivid and close, and participants stated to have been able to immerse themselves in the image. Importantly, this latter measure was strongly associated with the perception of having one’s own needs satisfied. This result is in line with a recent study by Looney et al. (37), who compared ImR features between high and low responders, in a sample of PTSD participants. The authors found that the new elements incorporated into the imagery are perceived as more vivid in high responders than in low responders. Therefore, considering the growing interest in the delivery of therapeutic techniques outside the classical therapeutic setting (51), helping the client to immerse themselves in memory seems to be important in the memory rehearsal and in satisfying the unmet emotional needs. This is in line with the study showing larger effects when app-based interventions are combined with therapist support (52).
Finally, our data show that the intervention brought about a change in the affective state. In the three sessions, there was a reduction in attention and activation levels. It would seem that ImR sessions reduced arousal bringing participants to a state of greater calm. This effect could be associated with progressively reduced fatigue in processing the emotional content related to target memories. This result is in line with previous studies indicating that ImRs reduce state stress symptoms (53).
Importantly, we also observed a general reduction in shame levels from the first to the third sessions. To the best of our knowledge, studies directly investigating the effect of group ImR on the affective state are very limited. However, previous studies reported a pre- and post-therapy reduction in shame and anxiety levels in participants with eating disorders and mixed personality disorders (29, 30). Our results suggest that increased positive emotionality might constitute a mechanism for the effectiveness of ImR, which is in line with the study by Dibbets et al. (54).
In conclusion, this study suggests that group ImR is a promising technique. However, it underlines the importance of monitoring the degree of immersion in the memory, which not only facilitates the memory rehearsal, but also makes the memory more vivid and affectively characterized. This provides evidence for which clinical experience has been suggested with respect to the technique in changing dysfunctional beliefs. When the client is not emotionally immersed in the memory, the technique is ineffective in meeting clients’ needs.
The sample is unbalanced with regard to gender and refers to a specific population. In this sample, participants were highly educated and almost half of the sample was constituted by psychologists. This limits the generalization of our results since psychologists are more familiar with the concept of “basic emotional need” and are probably more aware than the general population of their frustrated needs. However, none of the participants had previous experience with ImR, nor with group ImR. Future studies should include a more heterogeneous sample.
Ultimately, the absence of long-term follow-up does not allow us to monitor whether changes in beliefs have remained stable over time.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Guglielmo Marconi University Ethical Committee. The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.862289/full#supplementary-material
1. Young Jeffrey E, Klosko Janet S, Weishaar Marjorie E. Schema Therapy: A Practitioner’s Guide. New York, NY: Guilford Press (2003).
2. Tenore K, Serrani FM. La Schema Therapy. Caratteristiche Distintive. Milano: Franco Angeli (2003).
3. Arntz A. Imagery rescripting as a therapeutic technique: review of clinical trials, basic studies, and research agenda. J Exp Psychopathol. (2012) 3:189–208.
4. Morina N, Lancee J, Arntz A. Imagery rescripting as a clinical intervention for aversive memories: a meta-analysis. J Behav Ther Exp Psychiatry. (2017) 55:6–15. doi: 10.1016/j.jbtep.2016.11.003
5. Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behav Res Ther. (2005) 43:413–31. doi: 10.1016/j.brat.2004.03.006
6. Arntz A, Tiesema M, Kindt M. Treatment of PTSD: a comparison of imaginal exposure with and without imagery rescripting. J Behav Ther Exp Psychiatry. (2007) 38:345–70. doi: 10.1016/j.jbtep.2007.10.006
7. Kindt M, Buck N, Arntz A, Soeter M. Perceptual and conceptual processing as predictors of treatment outcome in PTSD. J Behav Ther Exp Psychiatry. (2007) 38:491–506. doi: 10.1016/j.jbtep.2007.10.002
8. Wild J, Hackmann A, Clark DM. Rescripting early memories linked to negative images in social phobia: a pilot study. Behav Ther. (2008) 39:47–56. doi: 10.1016/j.beth.2007.04.003
9. Wild J, Hackmann A, Clark DM. When the present visits the past: updating traumatic memories in social phobia. J Behav Ther Exp Psychiatry. (2007) 38:386–401. doi: 10.1016/j.jbtep.2007.07.003
10. Bamelis LLM, Evers SMAA, Spinhoven P, Arntz A. Results of a multicenter randomized controlled trial of the clinical effectiveness of schema therapy for personality disorders. Am J Psychiatry. (2014) 171:305–22. doi: 10.1176/appi.ajp.2013.12040518
11. Boterhoven De Haan KL, Lee CW, Fassbinder E, van Es SM, Menninga S, Meewisse ML, et al. Imagery rescripting and eye movement desensitisation and reprocessing as treatment for adults with post-traumatic stress disorder from childhood trauma: randomised clinical trial. Br J Psychiatry. (2020) 217:609–15. doi: 10.1192/bjp.2020.158
12. Arntz A, Sofi D, van Breukelen G. Imagery rescripting as treatment for complicated PTSD in refugees: a multiple baseline case series study. Behav Res Ther. (2013) 51:274–83. doi: 10.1016/j.brat.2013.02.009
13. Alliger-Horn C, Zimmermann P, Mitte K. Vergleichende wirksamkeit von IRRT und EMDR bei kriegstraumatisierten deutschen soldaten. Trauma Gewalt. (2015) 9:204–15.
14. Øktedalen T, Hoffart A, Langkaas TF. Trauma-related shame and guilt as time-varying predictors of posttraumatic stress disorder symptoms during imagery exposure and imagery rescripting—a randomized controlled trial. Psychother Res. (2014) 25:518–32. doi: 10.1080/10503307.2014.917217
15. Raabe S, Ehring T, Marquenie L, Olff M, Kindt M. Imagery rescripting as stand-alone treatment for posttraumatic stress disorder related to childhood abuse. J Behav Ther Exp Psychiatry. (2015) 48:170–6. doi: 10.1016/j.jbtep.2015.03.013
16. Lee SW, Kwon JH. The efficacy of imagery rescripting (IR) for social phobia: a randomized controlled trial. J Behav Ther Exp Psychiatry. (2013) 44:351–60. doi: 10.1016/j.jbtep.2013.03.001
17. Reimer SG, Moscovitch DA. The impact of imagery rescripting on memory appraisals and core beliefs in social anxiety disorder. Behav Res Ther. (2015) 75:48–59. doi: 10.1016/j.brat.2015.10.007
18. Ritter V, Stangier U. Seeing in the mind’s eye: imagery rescripting for patients with body dysmorphic disorder. A single case series. J Behav Ther Exp Psychiatry. (2016) 50:187–95. doi: 10.1016/j.jbtep.2015.07.007
19. Willson R, Veale D, Freeston M. Imagery rescripting for body dysmorphic disorder: a multiple-baseline single-case experimental design. Behav Ther. (2016) 47:248–61. doi: 10.1016/j.beth.2015.08.006
20. Cooper MJ. Working with imagery to modify core beliefs in people with eating disorders: a clinical protocol. Cogn Behav Pract. (2011) 18:454–65.
21. Wheatley J, Brewin CR, Patel T, Hackmann A, Wells A, Fisher P, et al. “I’ll believe it when I can see it”: imagery rescripting of intrusive sensory memories in depression. J Behav Ther Exp Psychiatry. (2007) 38:371–85. doi: 10.1016/j.jbtep.2007.08.005
22. Brewin CR, Wheatley J, Patel T, Fearon P, Hackmann A, Wells A, et al. Imagery rescripting as a brief stand-alone treatment for depressed patients with intrusive memories. Behav Res Ther. (2009) 47:569–76. doi: 10.1016/j.brat.2009.03.008
23. Page N, Veale D, Salkovskis P. Imagery – Google Scholar. (2010). Available online at: https://scholar.google.com/scholar?hl=it&as_sdt=0%2C5&q=Page%2C+N.%2C+Veale%2C+D.%2C+%26+Salkovskis%2C+P.+%282010%29.+Imagery+rescripting+for+obsessive-compulsive+disorder.+Paper+presented+at+the+38th+annual+conference+of+British+Association+of+Behavioral+and+Cognitive+Psychotherapy%2C+21st-23rd+July+2010%2C+Manchester+UK&btnG=#d=gs_cit&u=%2Fscholar%3Fq%3Dinfo%3AJuhsSjXG4HYJ%3Ascholar.google.com%2F%26output%3Dcite%26scirp%3D0%26hl%3Dit (accessed Dec 12, 2021).
24. Veale D, Page N, Woodward E, Salkovskis P. Imagery rescripting for obsessive compulsive disorder: a single case experimental design in 12 cases. J Behav Ther Exp Psychiatry. (2015) 49:230–6. doi: 10.1016/j.jbtep.2015.03.003
25. Maloney G, Koh G, Roberts S, Pittenger C. Imagery rescripting as an adjunct clinical intervention for obsessive compulsive disorder. J Anxiety Disord. (2019) 66:102110. doi: 10.1016/j.janxdis.2019.102110
26. Tenore K, Basile B, Cosentino T, de Sanctis B, Fadda S, Femia G, et al. Imagery rescripting on guilt-inducing memories in OCD: a single case series study. Front Psychiatry. (2020) 11:1018. doi: 10.3389/fpsyt.2020.543806
27. Paulik G, Steel C, Arntz A. Imagery rescripting for the treatment of trauma in voice hearers: a case series. Behav Cogn Psychother. (2019) 47:709–25.
28. Farrell JM, Reiss N, Shaw IA. The Schema Therapy Clinician’s Guide: A Complete Resource for Building and Delivering Individual, Group and Integrated Schema Mode Treatment Programs. Chichester: John Wiley & Sons (2014).
29. Simpson SG, Morrow E, van Vreeswijk M, Reid C. Group schema therapy for eating disorders: a pilot study. Front Psychol. (2010) 1:182. doi: 10.3389/fpsyg.2010.00182
30. Simpson SG, Skewes SA, van Vreeswijk M, Samson R. Commentary: short-term group schema therapy for mixed personality disorders: an introduction to the treatment protocol. Front Psychol. (2015) 6:609. doi: 10.3389/fpsyg.2015.00609
31. Arntz A, Jacob GA, Lee CW, Brand-de Wilde OM, Fassbinder E, Harper RP, et al. Effectiveness of predominantly group schema therapy and combined individual and group schema therapy for borderline personality disorder: a randomized clinical trial. JAMA Psychiatry. (2022) 79:287–99.
32. Farrell JM, Shaw IA, Webber MA. A schema-focused approach to group psychotherapy for outpatients with borderline personality disorder: a randomized controlled trial. J Behav Ther Exp Psychiatry. (2009) 40:317–28.
33. Paulik G, Maloney G, Arntz A, Bachrach N, Koppeschaar A, McEvoy P. Delivering imagery rescripting via telehealth: clinical concerns, benefits, and recommendations. Curr Psychiatry Rep. (2021) 23:24. doi: 10.1007/s11920-021-01238-8
34. Çili S, Pettit S, Stopa L. Impact of imagery rescripting on adverse self-defining memories and post-recall working selves in a non-clinical sample: a pilot study. Cogn Behav Ther. (2017) 46:75–89. doi: 10.1080/16506073.2016.1212396
35. Watson H, Rapee R, Todorov N. Imagery rescripting of revenge, avoidance, and forgiveness for past bullying experiences in young adults. Cogn Behav Ther. (2016) 45:73–89. doi: 10.1080/16506073.2015.1108360
36. Kunze AE, Arntz A, Kindt M. Investigating the effects of imagery rescripting on emotional memory: a series of analogue studies. J Exp Psychopathol. (2019) 10:2043808719850733.
37. Looney K, El-Leithy S, Brown G. The role of simulation in imagery rescripting for post-traumatic stress disorder: a single case series. Behav Cogn Psychother. (2021) 49:257–71. doi: 10.1017/S1352465820000806
38. Young JE, Brown G. Young Schema Questionnaire Short Form. New York, NY: Cognitive Therapy Centre (1988).
39. Butler AC, Beck AT, Cohen LH. The personality belief questionnaire-short form: development and preliminary findings. Cogn Ther Res. (2006) 31:357–70.
40. Arntz A, Weertman A. Treatment of childhood memories: theory and practice. Behav Res Ther. (1999) 37:715–40. doi: 10.1016/s0005-7967(98)00173-9
41. Watkins JG. The affect bridge: a hypnoanalytic technique. Int J Clin Exp Hypnosis. (2008) 19:21–7. doi: 10.1080/00207147108407148
42. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. (1988) 54:1063–70.
43. Welburn K, Coristine M, Dagg P, Pontefract A, Jordan S. the schema questionnaire—short form: factor analysis and relationship between schemas and symptoms. Cogn Ther Res. (2002) 26:519–30.
44. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5–Text Revision (TR)). Washington, DC: American Psychiatric Association (2022).
45. Beck AT, Beck JS. The Personality Belief Questionnaire. Unpublished Assessment Instrument. Bala Cynwyd, PA: The Beck Institute for Cognitive Therapy and Research (1991).
46. Flebus GB, Montano A. Presentazionedellaversioneitaliana del personal beliefs questionnaire di beck e freeman. Psicoterapia Cognitiva Comportamentale. (2006) 12:181–95.
47. Terracciano A. The Italian version of the NEO PI-R: conceptual and empirical support for the use of targeted rotation. Pers Individ Differ. (2003) 35:1859–72. doi: 10.1016/S0191-8869(03)00035-7
48. Terracciano A, McCrae RR, Costa PT. Factorial and construct validity of the Italian positive and negative affect schedule (PANAS). Eur J Psychol Assess. (2003) 19:131. doi: 10.1027//1015-5759.19.2.131
49. Otera R, Aragona B, Figoli G, Montesano L, Pucci S, Mancini F, et al. Efficacia dell’Imagery Rescripting nel Ridurre le Convinzioni Disfunzionali: uno Studio Pilota. (2021). p. 5–19.
50. Schacter DL, Addis DR. On the constructive episodic simulation of past and future events. Behav Brain Sci. (2007) 30:331–2.
51. Oliveira C, Pereira A, Vagos P, Nóbrega C, Gonçalves J, Afonso B. Effectiveness of mobile app-based psychological interventions for college students: a systematic review of the literature. Front Psychol. (2021) 12:1440. doi: 10.3389/fpsyg.2021.647606
52. Linardon J, Cuijpers P, Carlbring P, Messer M, Fuller-Tyszkiewicz M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. (2019) 18:325–36. doi: 10.1002/wps.20673
53. Strohm M, Siegesleitner M, Kunze AE, Werner GG, Ehring T, Wittekind CE. Psychological and physiological effects of imagery rescripting for aversive autobiographical memories. Cogn Ther Res. (2021) 45:1093–104.
Keywords: imagery rescripting, maladaptive beliefs, autobiographical memories, memory realism, emotional needs, affective state, needs’ satisfaction
Citation: Tenore K, Mancini A, Luppino OI and Mancini F (2022) Group Imagery Rescripting on Childhood Memories Delivered via Telehealth: A Preliminary Study. Front. Psychiatry 13:862289. doi: 10.3389/fpsyt.2022.862289
Received: 25 January 2022; Accepted: 16 May 2022;
Published: 23 June 2022.
Edited by:
Andressa Radiske, Edmond and Lily Safra International Institute of Neuroscience (IIN-ELS/ISD), BrazilReviewed by:
David John Arthur Edwards, Rhodes University, South AfricaCopyright © 2022 Tenore, Mancini, Luppino and Mancini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katia Tenore, dGVub3JlQGFwYy5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.