- 1Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy
- 2Child Neurology and Psychiatry Unit, Institute of Hospitalization and Care With Scientific Character (IRCCS) Mondino Foundation, Pavia, Italy
- 3Early Psychosis: Interventions and Clinical-Detection (EPIC) Lab, Department of Psychosis Studies, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 4OASIS Service, South London and Maudsley NHS Foundation Trust, London, United Kingdom
The presence of a positive family relationship has been suggested as a protective factor from parental stress and from the development of full-blown psychosis. However, to date, there is limited research on family functioning in adolescents with psychosis and at clinical high risk for psychosis (CHR-P). This study is aimed at comparing family functioning and perceived stress in parents of adolescents with either CHR-P, early onset psychosis (EOP), or other psychiatric disorders (no CHR-P). As a secondary aim, it will correlate family functioning with parental perceived stress in order to find critical targets of intervention. We conducted a Reporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD)—compliant, real-world, cross-sectional study. One-hundred and eleven adolescents aged 12–17 who access the institute of hospitalization and care with scientific character (IRCCS) Mondino Foundation Neuropsychiatric services (Pavia, Italy) between 2017 and 2020 and their parents (n = 222) were included. Sociodemographic characteristics of adolescents and their parents were collected. Family functioning was evaluated through the Family Adaptability and Cohesion Evaluation Scale-IV (FACES-IV) and the level of stress through the Perceived Stress Scale (PSS). Twenty adolescents had EOP, 38 had CHR-P, and 59 had no CHR-P. In total, 2.6% of CHR-P adolescents were adopted, 76.3% had separated-divorced parents, and 34.2% of parents had a depressive disorder. Among the FACES-IV sub-scale, maternal rigidity was progressively increased from no-CHR-P to CHR-P to EOP group, with statistical differences between EOP and the other two groups (p = 0.01). CHR-P mothers and fathers showed a high level of PSS values, without group difference. Lastly, PSS values correlated positively with the Rigidity, Disengagement, and Chaos scale of FACES-IV and negatively with the Communication scale (p < 0.05). Our results suggest that family functioning has a central role and could represent a worthwhile target of intervention for adolescents at CHR-P, leading the way to new preventive approaches.
Introduction
Psychotic disorders typically onset in adolescence and early adulthood (1), with a mean peak age at onset of 20.5 years (2). Once the disorder onsets, the opportunities to improve their course are limited (3). Therefore, early intervention and preventive approaches [termed “primary indicated prevention” (4–6)] in young people with clinical high risk for psychosis (CHR-P) have the potential to benefit their lives.
Recent studies and umbrella reviews indicate that CHR-P shows more comorbid mental disorders (7, 8), poorer functioning (1, 8–12), worse family relationships (13), higher level of perceived stress (14), and worse long-term outcomes (15) than healthy controls. CHR-P has about a 20% risk of developing psychosis at 2 years (16) but only one-third of them will eventually recover from their initial at-risk symptoms (15). On the contrary, less empirical evidence is available for what concerns effective preventive treatments (7), and it is currently insufficient to favor Cognitive Behavioral Therapy (5, 17). For what concerns family interventions, out of only three psychotherapeutic trials on family dynamics, two showed that an intervention on CHR-P adolescents and their parents improved the attenuated psychotic symptoms over time (7). Specifically, the parental role was identified as a determining factor that shows a negative correlation between mother’s criticism and improvement in the severity of symptoms at 12 months (18). However, these potential preventive effects are not consolidated.
In this regard, interventions that involve parents already represent a focal point for adolescent treatment in other psychiatric disorders (8). In fact, parental couples may incorrectly perceive the family dynamics when their child is affected by severe psychiatric disorders, leading to high levels of perceived stress. Therefore, in this point of view, dysfunctional family functioning and perceived stress could be both a consequence of psychiatric disorder and one of the risk factors that could persevere and increase the severity of symptoms (19). For these reasons, family functioning may represent a worthwhile target of intervention for adolescents at CHR-P (20). However, no comprehensive information about parental pair in CHR-P is available from the present literature, which is instead focused on adolescent perceptions and experiences (21, 22).
From currently knowledge is that both family relationships and social stress could impact the course and outcome of the illness (14). In detail, CHR-P adolescents report high levels of family conflict, childhood maltreatment, and general feelings of social stress when compared to healthy controls (22–24). Moreover, CHR-P adolescents living in less cohesive and supportive family environments show more severe symptoms, more functional impairment, and increased risk of symptom relapse (13, 25). While parents warmth, positive remarks, and involvement predict improvements in symptoms and social functioning (26), perceived stress is often associated with greater baseline symptom severity, progression, and increased likelihood of conversion to psychosis (13, 26, 27).
Overall, if on the one hand, the role of positive family relationships as a protective factor is clear (14), on the other, there is a lack of knowledge, especially about parents’ dynamics and functioning. The present study proposes to address this issue. Our hypothesis is that there may be specific characteristics in family functioning that could be identified as prognostic factors and, consequently, as possible targets for intervention. At the same time, it may also be important to identify the main sources of perceived stress in the parental couple in order to help in targeting future interventions. Specifically, we would like to investigate our hypotheses that compare family functioning and the stress perceived by parents of adolescents with either CHR-P, early onset psychosis (EOP), or other psychiatric disorders. As a secondary aim, it will correlate family functioning with parental perceived stress in order to find critical targets of intervention.
Materials and Methods
Design
This cross-sectional study was conducted according to the Reporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) Statement (see Supplementary Table 1) and has received ethical approval from the local ethics committee (P-20170028892). It is a part of the largest research protocol, which is explained in Molteni et al. (28).
Study Population
All help-seeking adolescents aged 12–17 years and their parents, consecutively admitted to the Child and Adolescent Neuropsychiatric Inpatient and Outpatient Units of institute of hospitalization and care with scientific character (IRCCS) Mondino Foundation (Pavia, Lombardy, Italy) between January 2017 and October 2020, were eligible to be recruited in this study.
Then, we applied the following exclusion criteria for parents: (i) absence of two caregivers for each family; (ii) cognitive and/or psychiatric problems of adolescent’s parents that could compromise the completion of study tests. The parental couples were included even if they were divorced/separated.
Indeed, exclusion criteria for adolescents were: (i) the previous history of any psychotic disorder according to Diagnostic and Statistically Manual of Mental Disorders 5 (DSM-5) (29), (ii) head injuries or any other underlying medical/neurological conditions, (iii) current DSM-5 illicit substance dependence or illicit substance-induced mental disorders, (iv) presence of Brief and Intermittent Psychotic Symptoms (BLIPS), according to Comprehensive Assessment of At Risk Mental State (CAARMS) criteria (30–32), and (v) established Wechsler Intelligence Scale for Children-IV (WISC-IV) (33) or Wechsler Adult Intelligence Scale-IV (WAIS-IV) (34) cognitive impairment (IQ < 70).
Once participants and their parents provided written consents, study enrollment was confirmed.
Participants were then divided into three groups as follows: (i) adolescents with established EOP (EOP hereby), (ii) adolescents meeting CAARMS CHR-P criteria (30) (CHR-P hereby), (iii) adolescents with other DSM-5 psychiatric disorders who did not meet Attenuated Psychotic Syndrome (APS)/EOP criteria (no CHR-P hereby).
Study Measures
Baseline Variables
Upon study entry, CAARMS (35) was carried out for all adolescents, allowing to divide them into the three abovementioned groups. For adolescents in no CHR-P group, other DSM-5 diagnosis than APS/EOP was identified (see Supplementary Methods 1). In addition, we evaluated:
(i) sociodemographic characteristics for both adolescents and parents. The presence of adoptive family or separated parents and Socio-Economic Status (SES) were also included as variables (36);
(ii) family history of any DSM-5 psychiatric disorders evaluated by two independent clinicians, in detail, we assessed by clinical interview the familiarity for psychiatric disorders presented in both parents and grandparents (first and second degrees) of the adolescents enrolled in the study.
(iii) perceived familial functioning and level of stress through self-administered questionnaires given to both parents (see below).
Perceived Familial Functioning Variables
We had investigated these aspects through a self-rated questionnaire, Family Adaptability and Cohesion Evaluation Scale-IV (FACES-IV) (37), administered to both parents independently.
In detail, this questionnaire was formulated to provide a qualitative and quantitative evaluation of family functioning. It is composed of different items to evaluate:
(i) Balanced scales: these are termed “balanced” because they are directly proportional to the family’s wellness, with they have a positive correlation. Balanced scales are represented by “cohesion” and “flexibility”;
(ii) Unbalanced scales: on the contrary, “unbalanced” scales represent features of family functioning that are considered extreme (in detail, as extreme areas of flexibility and cohesion). As extreme features, they are considered negative and, consequently, inversely related to family wellness. These are represented by “Disengagement,” “Enmeshment,” “rigidity,” and “Chaos.”
(iii) “Communication” and “satisfaction” scale: they represent the ability of family members to recognize the levels of communication and satisfaction in their own family.
(iv) Ratio measures between balanced and unbalanced scale, representing a global familial functioning and represented by:
- “cohesion ratio” = (cohesion)/[(disengagement + embeshment)/2
- “flexibility ratio” = (flexibility)/[(rigidity + cahos)/2
- “global ratio” = (cohesionratio + flexibilityratio)/ 2
All measures have a level of functioning according to FACES-IV score—both balanced and unbalanced scales are divided into three levels of functioning (dysfunctional, intermediate, and functional), communication and satisfaction scale in four levels of functioning (low, intermediate, good, and very good), and ratio measures in two (dysfunctional and functional).
Perceived Stress Variables
Perception of stress takes place when a subject realizes that situational demands exceed their resources. In this regard, in our study, we have investigated the level of stress through the self-administered questionnaire Perceived Stress Scale (PSS-10), administered by both parents independently. It was a stress scale composed of 10 items, previously validated (38) and used in other studies (39). Answers are given on a 5-point Likert scale ranging from 1 (never) to 5 (very often), with higher scores reflecting greater perceived stress. A score above 14 is considered to reflect significant perceived stress (40).
Outcome Measures
The primary outcome was to compare family functioning (using FACES-IV) and level of stress (as measured by PPS-10 scores) in parents of adolescents with CHR-P, EOP, and no CHR-P. The secondary outcome was to correlate family functioning variables (using FACES-IV sub-scale) to the level of stress (PSS-10 scores), considering the whole sample in order to test whether specific familial characteristics could be associated with greater stress.
Statistical Analysis
Descriptive analyses included median, first, and third quartiles, mean values, and standard deviation (SD), as appropriate for continuous variables, absolute and relative frequencies for categorical variables. Descriptive analyses were complemented by statistical comparisons between the three groups. Bivariate correlation analyses and Kruskal-Wallis were used for numerical variables and chi-square test for categorical variables, complemented by post-hoc analyses (Dunn test and Fisher test, respectively, appended supplementary). To reduce the chance of type I error due to multiple testing, Bonferroni correction was applied to all post-hoc analyses. More specifically, to test our main hypothesis, 24 (12 FACES-IV scales × 2 parents) comparisons between the three groups were performed using a series of Kruskal-Wallis tests with Bonferroni correction. We expected a 4.8% chance1 of observing at least one significant result.
Data were analyzed using R (48); all tests were two-sided, with alpha set at 0.05. All authors have complete access to our database, in which data were collected only after pseudonymization.
Results
Study Population
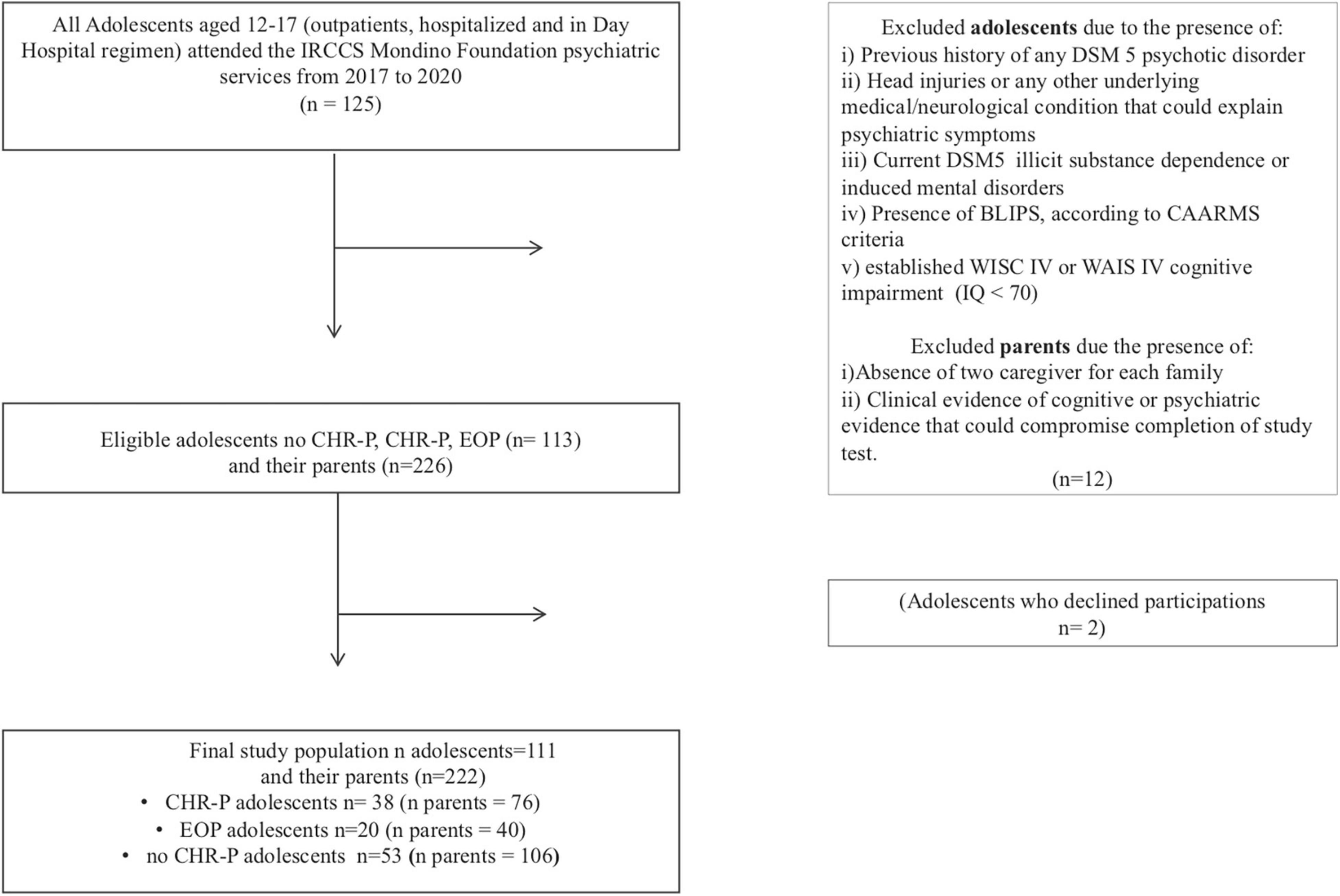
The flow chart of the study population is shown in Figure 1. In total, 111 adolescents and their parents (n = 222) were included. Among adolescents, 38 were in the CHR-P group, 20 in EOP, and 53 in no CHR-P groups (see Supplementary Table 3 for the specific psychiatric disorders of this subgroup). Across the CHR-P group, all adolescents met APS criteria and none met additionally Genetic Risk and Deterioration Syndrome (GRD) criteria.
Sociodemographics
The average age of adolescents was 15.1, 65.8% of them were women, and 92.1% were Italians.
Concerning parental information, 2.6% of adolescents were adopted, 76.3% from separated-divorced families. In our sample, there were not same-sex parental couples. The median SES, evaluated through Hollingshead Four Factor Index of SES scale, was 31.5 [interquartile range (IQR) 20.7–40.1]. Both for adolescents’ and families’ sociodemographic characteristics, there were no between-group differences (see Table 1).
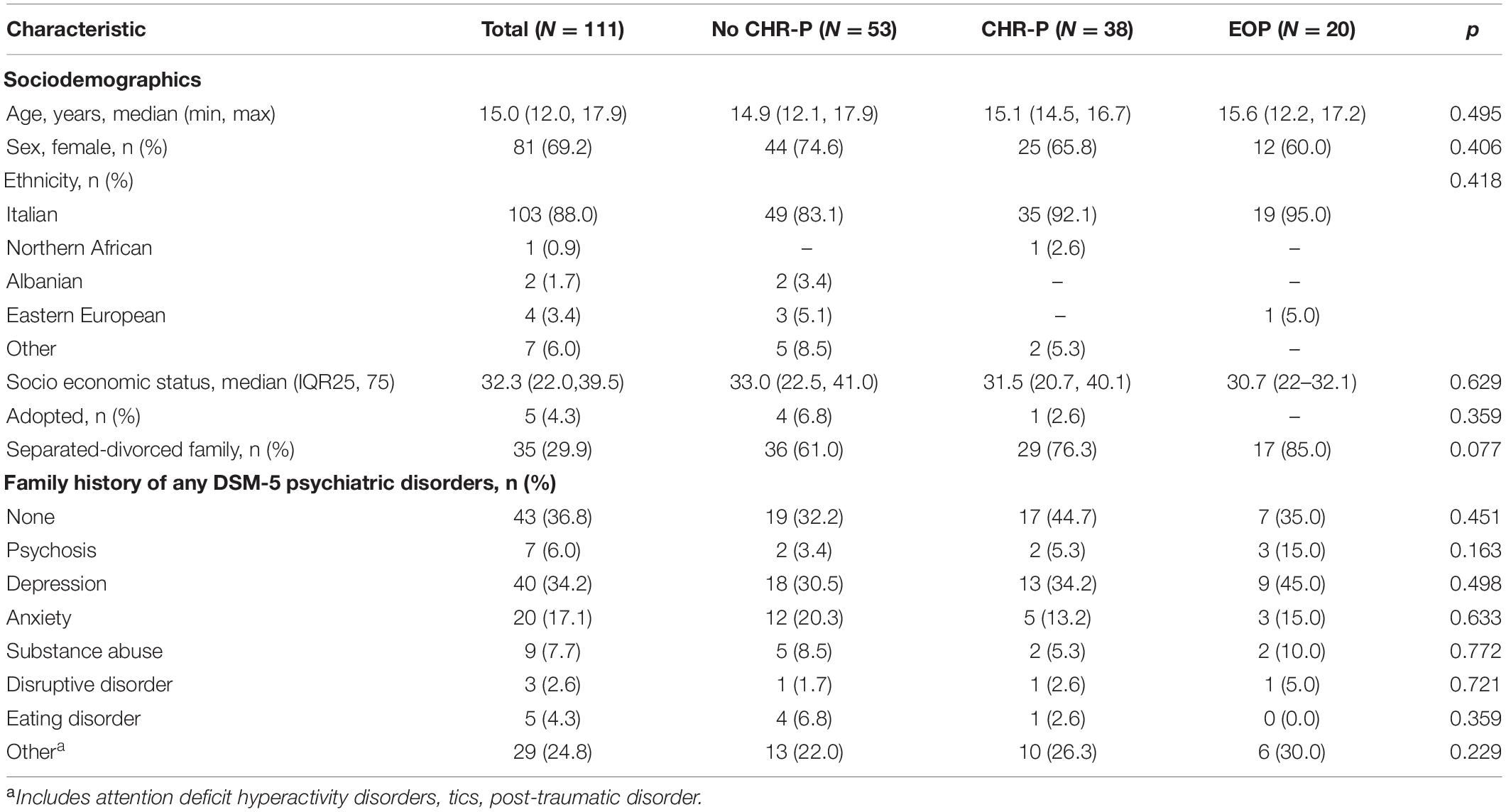
Table 1. Sociodemographics and family history of psychiatric disorders in the total adolescent sample and the clinical high risk state for psychosis (CHR-P), no CHR-P, and early onset psychosis (EOP) subgroups.
Family History of Psychiatric Disorders
Lack of positive family history of any mental disorder was present in 44.7% of CHR-P families; family history of psychosis was traceable in 5.3% of participants and the most frequent DSM-5 diagnosis was of depression disorders (34.2%); there were no between-groups differences (Table 1).
Perceived Mothers’ Family Functioning
Clinical high risk state for psychosis adolescent’s mothers showed on average intermediate values for both balanced and unbalanced scales and respectively: 45.45 cohesion, 46.89 flexibility, 60.66 Disengagement, 45.68 Enmeshment, 46.68 Rigidity, and 57.63 Chaos. Communication and satisfaction scales were, respectively, mean 33.13 and 31.29. The mean ratio values were 1.11 for the Cohesion Ratio, 1.27 for the Flexibility Ratio, and 1.04 for the Global Ratio (see Table 2).
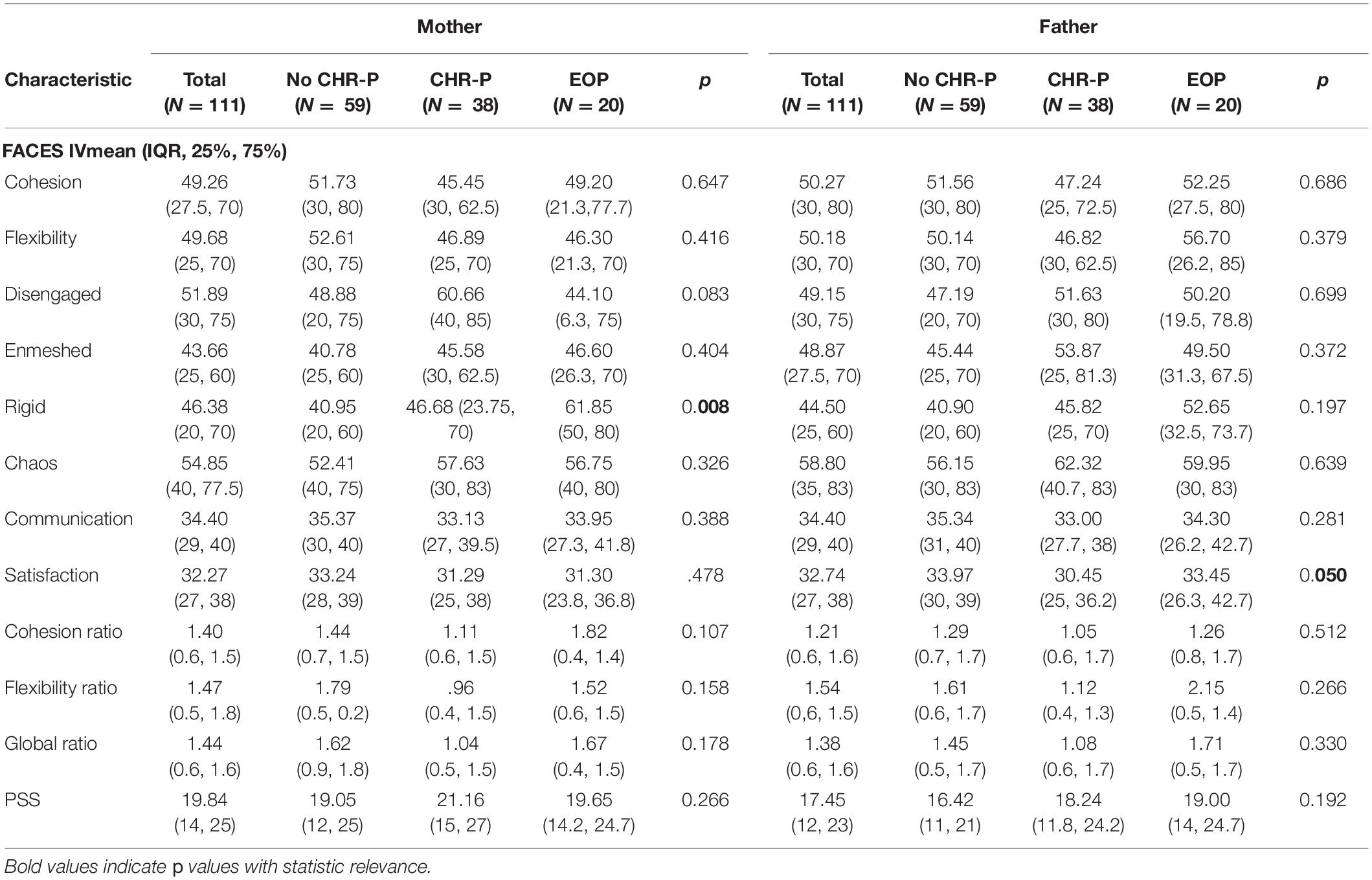
Table 2. Results of perceived family functioning and stress in both mothers and fathers independently in the whole sample and in the clinical high risk state for psychosis (CHR-P), no CHR-P, and early onset psychosis (EOP) subgroups.
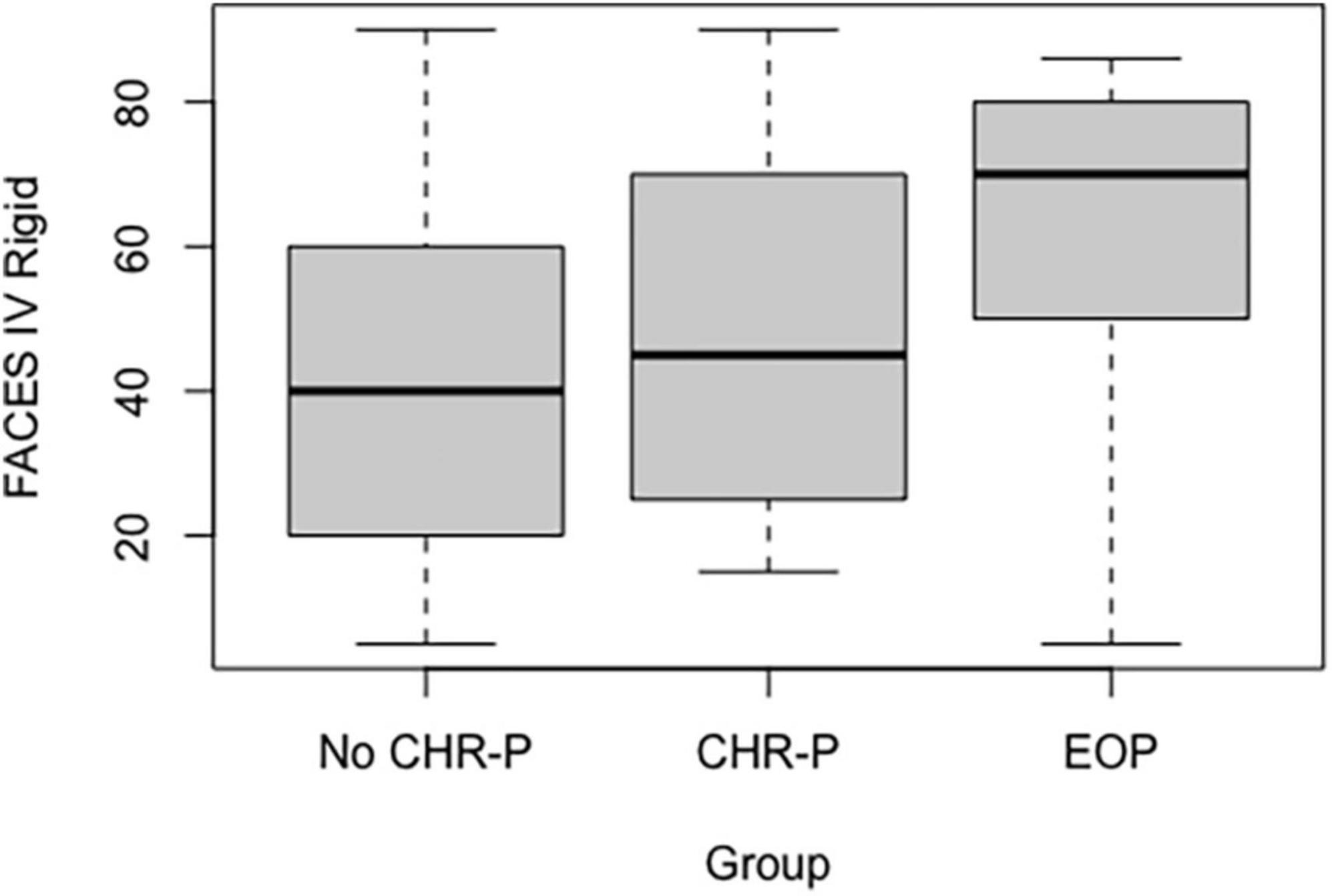
Regarding group comparison, we found only a significant difference with respect to the rigidity subscale (p = 0.008). In detail, mothers of the EOP group were shown to perceive more rigidity than both no CHR-P (p = 0.002) and CHR-P groups (p = 0.028; see Figure 2). On the contrary, there was not a significant difference between mothers of CHR-P and no CHR-P adolescents (see Supplementary Table 2).
Perceived Fathers’ Family Functioning
As mothers, also CHR-P adolescent’s fathers showed intermediate mean values for both balanced and unbalanced scales and respectively: 47.23 cohesion, 46.82 flexibility, 51.63 Disengagement, 53.87 Enmeshment, 45.81 Rigidity, and 62.31 Chaos. Communication and satisfaction scales were, respectively, mean 33.00 and 30.44. The mean ratio values were 1.05 for the Cohesion Ratio, 1.12 for the Flexibility Ratio, and 1.08 for the Global Ratio (see Table 2).
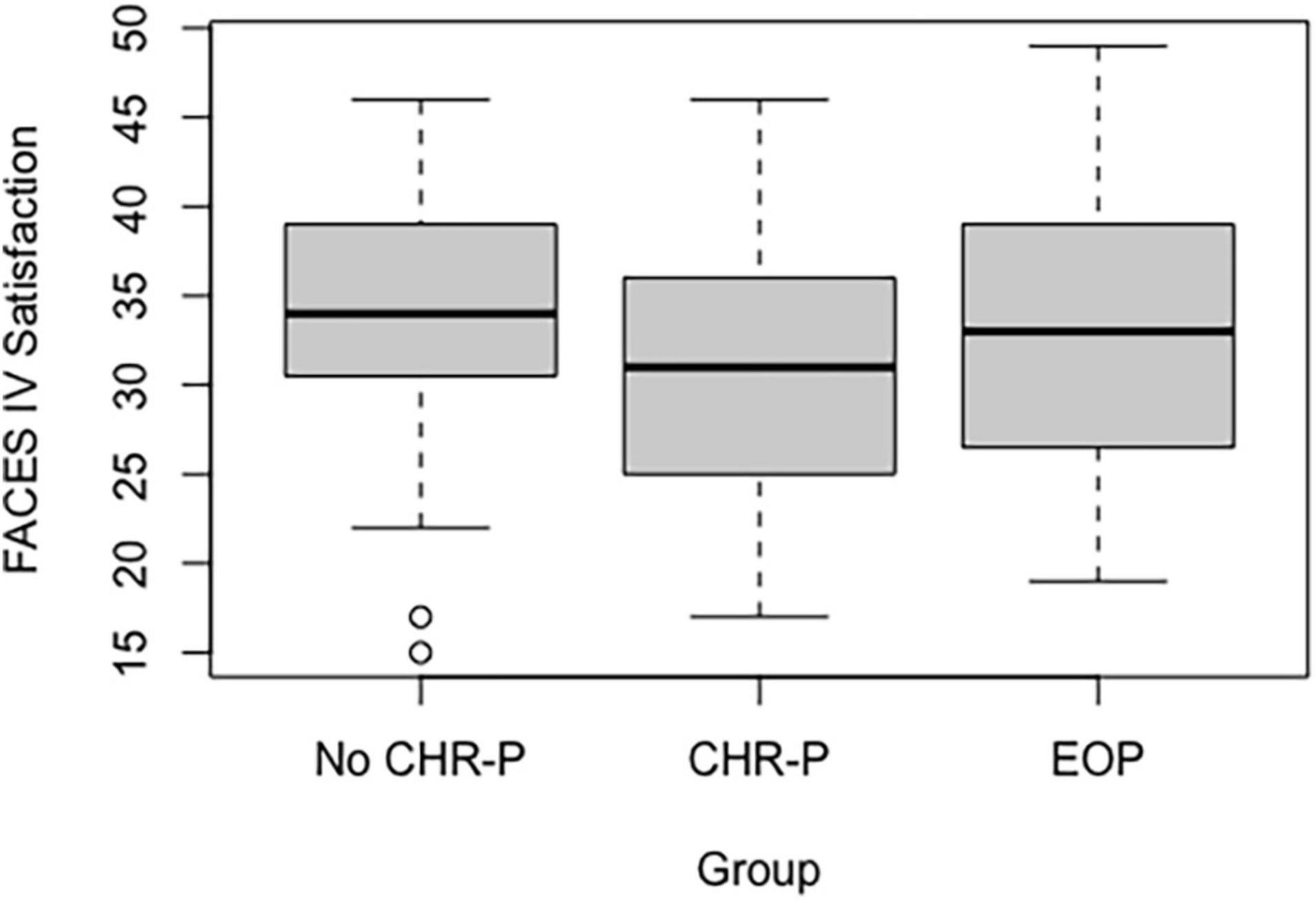
Regarding group comparison, we found only one significant difference in the satisfaction subscale (p = 0.05), with more perception of satisfaction in fathers of no CHR-P as compared to CHR-P group (p = 0.015) (see Figure 3 and Supplementary Table 2).
Perceived Mothers’ Stress
The mean value of perceived stress of CHR-P adolescents’ mothers was 21.16, showing a high and significant level of perceived stress (see Table 2). There were no between-group differences.
Perceived Fathers’ Stress
As mothers, also fathers show a high and significant level of perceived stress with a mean value of 18.23 (see Table 2). There were no between-group differences.
Pearson Correlation Between Family Functioning and Perceived Stress
Among Faces-IV scales and PSS-10 level of stress, we found weak/moderate positive correlations for both mothers and fathers between the level of perceived stress and values of Disengaged (p < 0.05 for both mothers and fathers), Rigid (p < 0.01 for mothers and p < 0.05 for fathers), and Chaos (p < 0.01 for both mothers and fathers). In addition, for only mothers, there was a negative correlation between the level of stress and the Communication scale (p < 0.05; see Table 3).
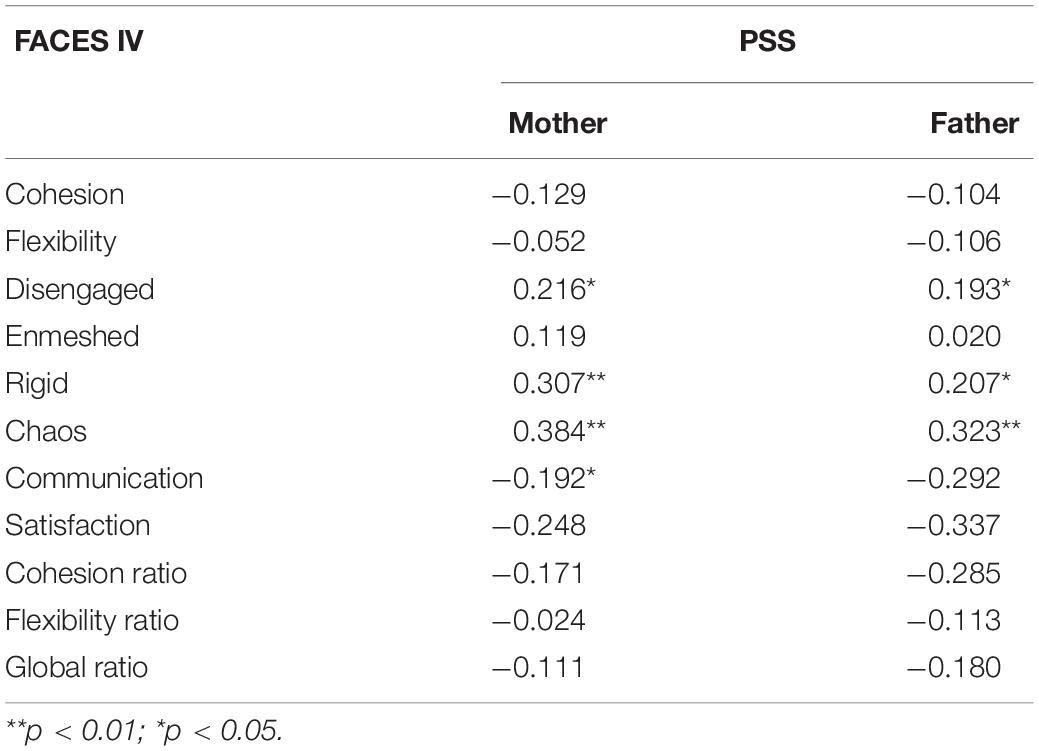
Table 3. Pearson correlation between family adaptability and cohesion evaluation scale-IV (FACES-IV) scales and perceived stress scale (PSS) in the whole sample.
See Supplementary Results 1 for Pearson correlation between mothers and fathers in both FACES-IV subscales and PSS values.
Discussion
Until now, there are no comprehensive studies in the literature that have investigated the role of the parental couple in CHR-P adolescents. In addition, to the authors’ knowledge, the studies with reliable sample sizes did not investigate family functioning (7, 8). This is thus the largest real-world study that investigated the role of the family in CHR-P adolescents.
Firstly, in our sample, about 75% of CHR-P adolescents come from separated-divorced families: it is known that parental couple’s separation could impact adolescents’ functioning and that may be associated with a higher level of emotional distress (41). However, in our study, this percentage does not differ from other psychiatric disorders (both psychotic and others), underlying how family relationships may have a central role in general psychopathology (19).
Secondly, most CHR-P adolescents had no family history of mental disorders (44.7%). In addition, among those who had psychiatric familiarity, depressive disorders were more frequent than psychotic disorders (34.2 and 5.3%, respectively). Our results were consistent with previous studies in the literature (8). In detail, a recent study showed that depressive symptoms were present in one-third of caregivers of CHR-P individuals, triggering criticism and distress (42). In the same way, a caregiver’s depressive symptoms negatively impact family functioning and promote the insurgence of psychiatric disorders (43). Therefore, previous researches (14, 19) suggested that screening for the presence of emotional distress in families of adolescents accessing mental healthcare could be relevant to orient psychoeducational approaches.
The core finding of the study was that both mothers and fathers of CHR adolescents did not show a specific profile on perceived familial functioning. In all FACES-IV subscales (balanced and unbalanced), we found intermediate values: this suggests that, at presentation, there were no clinically disturbed family relationships. At the same time, the presence of intermediate values showed that caregivers were only partially satisfied with their family functioning and communication, with aspects that were potentially improvable. In this view, a psychotherapeutic approach that aims to encourage an improvement in family dynamics has the potential to be a valid therapeutic intervention (13).
In this context, the most interesting finding concerns maternal rigidity, which was progressively increased from no CHR-P to CHR-P to EOP group. This domain was significantly higher in EOP than in the other groups. Rigidity represents the extreme upper end of flexibility in contrast with the lower end represented by disorganization: mothers with a higher expression of rigidity, therefore, responded positively to questions, such as “In our family when rules are broken, there are severe consequences” or “In our family, there is a rule for every possible situation,” indicating that there were rules and norms within the family that could not be violated (37). This finding is in line with previous literature, as family members of an individual with psychosis are more likely to report extreme family difficulties, such as Disengagement, Rigidity, and Chaos: these families are generally more rigid, less structured, less flexible, and more chaotic (44).
A high maternal rigidity could have a double role: on the one side, mothers could have a restraining function for EOP adolescents that are by definition disorganized in their thought and behavior (25). At the same time, an excessive rigidity may represent a trigger for psychotic symptoms or other types of crises. Therefore, this result also underscores its intrinsic ambivalence: the presence of maternal rigidity could be both a factor preceding the onset of symptoms and a consequence of the disease itself. Indeed, as written above, the disorganization typical of the psychotic adolescent could have favored a more restraining and rigid attitude of family members.
Overall, to date, these findings remain largely unexplored, and their influence on adolescents’ symptoms remains unclear. In the light of the present findings, developing an empirical understanding of factors that initiate and maintain adaptive family functioning in the presence of a psychiatric illness becomes an important research goal for the field of early psychosis intervention (44). For instance, one study reports negative correlations between CHR-P symptoms and maternal criticism (18). If a strict correlation between rigidity and criticism has not yet been studied in CHR-P adolescents, it is true that in other psychiatric conditions, such as eating disorders, rigidity, and criticism, sometimes coexist (45). Similarly, to criticism, rigidity could represent a target of family intervention with the aim to fit the flexibility of the parental couple to the psychopathological characteristics of their child (18). Rigidity could be addressed in psychotherapy focused both on parental-couple or in family-system level: here, could be important to understand and mentalize the deeper emotional states of ourselves and the other, such as the family dynamics. Indeed, a deeper understanding of what happens, especially when a clinical psychopathology occurs, with the sharing of the experience of each member of the family could promote the development of a more balanced family style (not excessively rigid or, on the contrary, not excessively disorganized).
Conversely, it is important to highlight that those familial features cannot be considered as pathogenetic factors themselves for psychosis. Indeed, psychosis remains a multifactorial disease whose pathogenesis is known to have different risk factors, such as, biological factors, stress sensitivity, and environment (3). In this point of view, maternal rigidity could be considered as a risk factor in the context of a predisposition: knowing, however, each individual risk and prognostic factor (i.e., family characteristics) could be a starting point for improving early intervention.
Fourthly, parents’ perceived stress was also investigated. Notably, we found high levels of perceived stress in the CHR-P group for both mothers and fathers, with no difference between EOP and no CHR-P group. The absence of differences between the three groups highlighted the importance of this factor in CHR-P families: it could be a negative factor, such as for adolescents suffering from other psychiatric conditions (both EOP or with other psychiatric disorders) (22, 46). However, as for maternal rigidity, there is a double role of this finding. Indeed, perceived stress may be one of the factors that promote the disease, but at the same time also a consequence of the disease itself (46).
Lastly, correlations between family functioning and perceived stress showed interesting associations: as the imbalance in FACES-IV scales increased, also did the value of perceived stress. Notably, perceived stress increased together with values of Disengagement, Rigidity, and Chaos, which are the three negative domains of the FACES-IV. Disengagement represents distance and lack of involvement within the family, while Rigidity and Chaos are the opposite extremes of good family flexibility (from the most rigid rules to a total lack) (37). The fact that these findings were replicated in mothers and fathers strengthens their validity. Conversely, good communication between family members seems to be important in decreasing perceived stress. In fact, mothers in our sample showed a decrease in perceived stress when family communication was more functional. Overall, these results support the main ones, underlining how a family intervention could be useful. In detail, good cohesion and flexibility may represent a target of family intervention as already shown in other psychiatric disorders, such as eating disorders (45). Although to date, there are no guidelines in the treatment of CHR-P, family therapy could be a good target of intervention. Fostering communication could be important both within the parental couple (with a parental-focused therapy) and with the patients (with a therapy focused on all family members). In this point of view, in the family and parental nucleus, it is of fundamental importance to work on the mentalization and understanding of one’s own and other’s emotions, on the ability to listen and share, even negative experiences, such as the disease itself (45).
The main limitation of the current study is represented by the absence of adolescents’ perceived point of view on perceived familial functioning and stress. However, we will fill this gap in future research that will include all points of view in the family. Another limitation is that since we included adolescents recruited at a third-level center, the CHR-P patients may represent a more severe part of the high-risk spectrum (47).
Conclusion
Our findings support how family dynamics could be a source of perceived stress and highlight how specific features, such as rigidity, could represent potential directions for family intervention.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study received ethical approval from the local ethics committee (P-20170028892). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
RB, MM, and MI conceived and designed the study and participated in the acquisition of data. EC analyzed the data. MI drafted the manuscript. PF-P and SD revised the manuscript. All authors have read and approved the final manuscript.
Funding
This project was supported by the Italian Ministry of Education, University, and Research (MIUR) between 2012 and 2017. This research was supported by the Italian Ministry of Health (Current research 2017-2020).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank the Colleagues, Capone Luca, Carpani Adriana, Chiappedi Matteo Alessio, Silvia Molteni, Eleonora Filosi for the clinical management and evaluations of many of the patients reported in this study during these years.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.861201/full#supplementary-material
Abbreviations
CHR-P, Clinical High Risk state for Psychosis; DMS-5, Diagnostic and Statistically Manual of mental disorders 5; WISC IV, Wechsler Intelligence Scale for Children IV; WAIS, Wechsler Adult Intelligence Scale; BLIPS, Brief and Intermittent Psychotic Symptoms; CAARMS, Comprehensive Assessment of At Risk Mental State; EOP, Early Onset Psychosis; FACES-IV, Family Adaptability and Cohesion Evaluation Scale-IV; PSS-10, Perceived Stress Scale.
Footnotes
- ^ To calculate this percentage, we performed the following formula: p (at least one significant result) = 1 – p (no significant results) = 1 − (1 – α/n)24.
References
1. Radua J, Valentina R-C, John PAI, Abraham R, Nacharin P, Taha A, et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. (2018) 17:49–66. doi: 10.1002/wps.20490
2. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2021). doi: 10.1038/s41380-021-01161-7 [Epub ahead of print].
3. Fusar-Poli P, Millan MJ, Ricca V, Oliver D, Kingdon J, Valmaggia L, et al. Deconstructing vulnerability for psychosis: meta-analysis of environmental risk factors for psychosis in subjects at ultra high-risk. Eur Psychiatry. (2017) 40:65–75. doi: 10.1016/j.eurpsy.2016.09.003
4. Arango C, Díaz-Caneja CM, McGorry PD, Rapoport J, Sommer IE, Vorstman JA, et al. Preventive strategies for mental health. Lancet Psychiatry. (2018) 5:591–604. doi: 10.1016/S2215-0366(18)30057-9
5. Fusar-Poli P, Salazar De Pablo G, Correll CU, Meyer-Lindenberg A, Millan MJ, Borgwardt S, et al. Prevention of psychosis: advances in detection, prognosis, and intervention. JAMA Psychiatry. (2020) 77:755–65. doi: 10.1001/jamapsychiatry.2019.4779
6. Fusar-Poli P, Correll CU, Arango C, Berk M, Patel V, Ioannidis JPA. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry. (2021) 20:200–21. doi: 10.1002/wps.20869
7. Catalan A, Salazar de Pablo G, Vaquerizo Serrano J, Mosillo P, Baldwin H, Fernández-Rivas A, et al. Annual research review: prevention of psychosis in adolescents – systematic review and meta-analysis of advances in detection, prognosis and intervention. J Child Psychol Psychiatry Allied Discip. (2021) 62:657–73. doi: 10.1111/jcpp.13322
8. Mensi MM, Molteni S, Iorio M, Filosi E, Ballante E, Balottin U, et al. Prognostic accuracy of DSM-5 attenuated psychosis syndrome in adolescents: prospective real-world 5-year cohort study. Schizophr Bull. (2021) 7:1–11. doi: 10.1093/schbul/sbab041
9. Carrión RE, McLaughlin D, Goldberg TE, Auther AM, Olsen RH, Olvet DM, et al. Prediction of functional outcome in individuals at clinical high risk for psychosis. JAMA Psychiatry. (2013) 70:1133–42. doi: 10.1001/jamapsychiatry.2013.1909
10. Tor J, Dolz M, Sintes A, Muñoz D, Pardo M, de la Serna E, et al. Clinical high risk for psychosis in children and adolescents: a systematic review. Eur Child and Adolesc Psychiatry. (2018) 27:683–700. doi: 10.1007/s00787-017-1046-3
11. Velthorst E, Zinberg J, Addington J, Cadenhead KS, Cannon TD, Carrión RE, et al. Potentially important periods of change in the development of social and role functioning in youth at clinical high risk for psychosis. Dev Psychopathol. (2018) 30:39–47. doi: 10.1017/S0954579417000451
12. Fusar-Poli P, Rocchetti M, Sardella A, Avila A, Brandizzi M, Caverzasi E, et al. Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. Br J Psychiatry. (2015) 207:198–206. doi: 10.1192/bjp.bp.114.157115
13. Schlosser DA, Zinberg JL, Loewy RL, Casey-Cannon S, O’Brien MP, Bearden CE, et al. Predicting the longitudinal effects of the family environment on prodromal symptoms and functioning in patients at-risk for psychosis. Schizophr Res. (2010) 118:69–75. doi: 10.1016/j.schres.2010.01.017
14. Bentley E, Millman ZB, Thompson E, Demro C, Kline E, Pitts SC, et al. High-risk diagnosis, social stress, and parent-child relationships: a moderation model. Schizophr Res. (2016) 174:65–70. doi: 10.1016/j.schres.2016.04.014
15. Salazar de Pablo G, Besana F, Arienti V, Catalan A, Vaquerizo-Serrano J, Cabras A, et al. Longitudinal outcome of attenuated positive symptoms, negative symptoms, functioning and remission in people at clinical high risk for psychosis: a meta-analysis. EClinicalMedicine. (2021) 36:100909. doi: 10.1016/j.eclinm.2021.100909
16. Salazar de Pablo G, Radua J, Pereira J, Bonoldi I, Arienti V, Besana F, et al. Probability of transition to psychosis in individuals at clinical high risk: an updated meta-analysis. JAMA Psychiatry. (2021) 78:970. doi: 10.1001/jamapsychiatry.2021.0830
17. Davies C, Radua J, Cipriani A, Stahl D, Provenzani U, McGuire P, et al. Efficacy and acceptability of interventions for attenuated positive psychotic symptoms in individuals at clinical high risk of psychosis: a network meta-analysis. Front Psychiatry. (2018) 9:187. doi: 10.3389/fpsyt.2018.00187
18. Tsai KH, López S, Marvin S, Zinberg J, Cannon TD, O’Brien M, et al. Perceptions of family criticism and warmth and their link to symptom expression in racially/ethnically diverse adolescents and young adults at clinical high risk for psychosis. Early Interv Psychiatry. (2015) 9:476–86. doi: 10.1111/eip.12131
19. Santesteban-Echarri O, MacQueen G, Goldstein BI, Wang JL, Kennedy SH, Bray S, et al. Family functioning in youth at-risk for serious mental illness. Compr Psychiatry. (2018) 87:17–24. doi: 10.1016/j.comppsych.2018.08.010
20. Thompson E, Rakhshan P, Pitts SC, Demro C, Millman ZB, Bussell K, et al. Family functioning moderates the impact of psychosis-risk symptoms on social and role functioning. Schizophr Res. (2019) 204:337–42. doi: 10.1016/j.schres.2018.08.035
21. Miklowitz DJ, O’Brien MP, Schlosser DA, Addington J, Candan KA, Marshall C, et al. Family-focused treatment for adolescents and young adults at high risk for psychosis: results of a randomized trial. J Am Acad Child Adolesc Psychiatry. (2014) 53:848–58. doi: 10.1016/j.jaac.2014.04.020
22. Yee CI, Gupta T, Mittal VA, Haase CM. Coping with family stress in individuals at clinical high-risk for psychosis. Schizophr Res. (2020) 216:222–8. doi: 10.1016/j.schres.2019.11.057
23. Addington J, Farris M, Stowkowy J, Santesteban-Echarri O, Metzak P, Kalathil MS. Predictors of transition to psychosis in Individuals at clinical high risk. Curr Psychiatry Rep. (2019) 21:39. doi: 10.1007/s11920-019-1027-y
24. Thompson E, Kline E, Ellman LM, Mittal V, Reeves GM, Schiffman J. Emotional and behavioral symptomatology reported by help-seeking youth at clinical high-risk for psychosis. Schizophr Res. (2015) 162:79–85. doi: 10.1016/j.schres.2015.01.023
25. Koutra K, Triliva S, Roumeliotaki T, Basta M, Simos P, Lionis C, et al. Impaired family functioning in psychosis and its relevance to relapse: a two-year follow-up study. Compr Psychiatry. (2015) 62:1–12. doi: 10.1016/j.comppsych.2015.06.006
26. O’Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz A, Cannon TD. Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophr Res. (2006) 81:269–75. doi: 10.1016/j.schres.2005.10.005
27. Kraan T, Velthorst E, Smit F, de Haan L, van der Gaag M. Trauma and recent life events in individuals at ultra high risk for psychosis: review and meta-analysis. Schizophr Res. (2015) 161:143–9. doi: 10.1016/j.schres.2014.11.026
28. Molteni S, Filosi E, Mensi MM, Spada G, Zandrini C, Ferro F, et al. Predictors of outcomes in adolescents with clinical high risk for psychosis, other psychiatric symptoms, and psychosis: a longitudinal protocol study. Front Psychiatry. (2019) 10:787. doi: 10.3389/fpsyt.2019.00787
29. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013).
30. Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell’Olio M, et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry. (2005) 39:964–71. doi: 10.1080/j.1440-1614.2005.01714.x
31. Fusar-Poli P, Cappucciati M, Bonoldi I, Hui LMC, Rutigliano G, Stahl DR, et al. Prognosis of brief psychotic episodes a meta-analysis. JAMA Psychiatry. (2016) 73:211–20. doi: 10.1001/jamapsychiatry.2015.2313
32. Fusar-Poli P, Cappucciati M, De Micheli A, Rutigliano G, Bonoldi I, Tognin S, et al. Diagnostic and prognostic significance of brief limited intermittent psychotic symptoms (BLIPS) in individuals at ultra high risk. Schizophr Bull. (2017) 43:48–56. doi: 10.1093/schbul/sbw151
33. Renner G, Schroeder A, Irblich D. Discriminative validity of the wechsler intelligence scale for children – iv (Wis) in a social-pediatric sample. Prax Kinderpsychol Kinderpsychiatr. (2019) 68:183–97. doi: 10.13109/prkk.2019.68.3.183
34. Hartman DE. Test review wechsler adult intelligence scale IV (WAIS IV): return of the gold standard. Appl Neuropsychol. (2009) 16:85–7. doi: 10.1080/09084280802644466
35. Pelizza L, Paterlini F, Azzali S, Garlassi S, Scazza I, Pupo S, et al. The approved Italian version of the comprehensive assessment of at-risk mental states (CAARMS-ITA): field test and psychometric features. Early Interv Psychiatry. (2019) 13:810–7. doi: 10.1111/eip.12669
37. Olson D. FACES IV and the circumplex model: validation study. J Marital Fam Ther. (2011) 37:64–80. doi: 10.1111/j.1752-0606.2009.00175.x
38. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
39. Concerto C, Conti C, Muscatello MR, Signorelli MS, Zoccali R, Coira D, et al. Sleep quality, perceived stress, and caffeinated drinks intake in psychiatry residents: a cross-sectional study. J Caffeine Res. (2017) 7:18–22. doi: 10.1089/jcr.2016.0014
40. Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S editors. The Social Psychology of Health. (Newbury Park, CA: Sage) (1988).
42. Hamaie Y, Ohmuro N, Katsura M, Obara C, Kikuchi T, Ito F, et al. Correction: criticism and depression among the caregivers of at-risk mental state and first-episode psychosis patients. PLoS One. (2016) 11:e0156590. doi: 10.1371/journal.pone.0156590
43. Herba CM, Glover V, Ramchandani PG, Rondon MB. Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiatry. (2016) 3:983–92. doi: 10.1016/S2215-0366(16)30148-1
44. Gupta M, Bowie CR. Family cohesion and flexibility in early episode psychosis. Early Interv Psychiatry. (2018) 12:886–92. doi: 10.1111/eip.12384
45. Kluck AS. Family factors in the development of disordered eating: integrating dynamic and behavioral explanations. Eat Behav. (2008) 9:471–83. doi: 10.1016/j.eatbeh.2008.07.006
46. Fusar-Poli P, Rutigliano G, Stahl D, Schmidt A, Ramella-Cravaro V, Hitesh S, et al. Deconstructing pretest risk enrichment to optimize prediction of psychosis in individuals at clinical high risk. JAMA Psychiatry. (2016) 73:1260–7. doi: 10.1001/jamapsychiatry.2016.2707
47. Schultze-Lutter F, Michel C, Ruhrmann S, Schimmelmann BG. Prevalence and clinical significance of DSM-5-attenuated psychosis syndrome in adolescents and young adults in the general population: the bern epidemiological at-risk (BEAR) study. Schizophr Bull. (2014) 40:1499–508. doi: 10.1093/schbul/sbt171
Keywords: family functioning, psychosis, schizophrenia, risk, prevention, adolescence, CHR-P, perceived stress (PS)
Citation: Iorio M, Casini E, Damiani S, Fusar-Poli P, Borgatti R, Mensi MM and Clinical High Risk state for Psychosis Research Group (2022) Perceived Family Functioning Profile in Adolescents at Clinical High Risk for Psychosis: Rigidity as a Possible Preventive Target. Front. Psychiatry 13:861201. doi: 10.3389/fpsyt.2022.861201
Received: 24 January 2022; Accepted: 02 March 2022;
Published: 15 April 2022.
Edited by:
Veit Roessner, University Hospital Carl Gustav Carus, GermanyReviewed by:
Michelle Worthington, Yale University, United StatesKatherine Damme, Northwestern University, United States
Copyright © 2022 Iorio, Casini, Damiani, Fusar-Poli, Borgatti, Mensi and Clinical High Risk State for Psychosis Research Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renato Borgatti, UmVuYXRvLkJvcmdhdHRpQG1vbmRpbm8uaXQ=
†The Clinical High-Risk State for Psychosis Group includes the following colleagues: Chiara Rogantini, Marika Orlandi, Arianna Vecchio
 Melanie Iorio
Melanie Iorio Erica Casini2
Erica Casini2 Stefano Damiani
Stefano Damiani