- 1Hunan Cancer Hospital/The Affiliated Cancer Hospital of Xiangya School of Medicine, Central South University, Changsha, China
- 2Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Changsha, China
- 3Department of Mathematics and Statistics, Mzuzu University, Mzuzu, Malawi
- 4Department of Epidemiology and Health Statistics, Xiangya School of Public Health, Central South University, Changsha, China
Background: Activities of daily living (ADL) disability is a concern in the aging population and can lead to increased health service demands and lower quality of life. The aim of this longitudinal study was to assess the associations of chronic conditions and depressive symptoms with ADL disability.
Methods: This prospective cohort study used two waves of data (2011 and 2015) from the China Health and Retirement Longitudinal Study (CHARLS). A total of 10,864 participants aged 45 and older were included for analysis. Chronic diseases were assessed by self-report and depressive symptoms were assessed using the validated 10-item of Center for Epidemiologic Studies Depression Scale at baseline. Incidents of ADL disability during follow-up were assessed using the Katz ADL scales.
Results: After 4 years of follow-up, there were 704 participants incidents of ADL disability. The incident rate was 17.22 per 1,000 person-years. Having at least one chronic disease was independently associated with a 39% increased risk of incident ADL disability (adjusted HR, 1.39; 95%CI: 1.16, 1.67). The presence of depression symptoms was independently associated with a 54% increased risk of incident ADL disability (adjusted HR, 1.54; 95%CI: 1.30, 1.82). However, there was no significant additive interaction effect between chronic diseases and depressive symptoms on ADL disability.
Conclusion: Chronic diseases and depressive symptoms are associated with an increased risk of ADL disability in middle-aged and older Chinese adults. Improving chronic diseases and depressive symptoms can prevent ADL disability.
Introduction
The increasing trend of the aging population is predictable all over the world, and China's aging population is estimated to increase at the rate of 6.2 million per year from 2021 to 2050, and is expected to exceed 400 million by 2050 (1). An aging population raises many concerns in the domain of health. For example, the impact of functional disability on individuals, especially in middle-aged and older adults, is manifested by increased demand for health services, reduced subjective wellbeing, and increased risk of death (2–4). Not only China, other East Asian countries, facing huge challenges. For example, the prevalence of functional disability in an elderly general population of Japanese was 20.1 and 4.9% of elderly in Korea reported functional decline of at least one of the seven activities of daily living (ADL) components after 2 years (5, 6). Moreover, the prevalence of depression was 33.5% in elderly Japanese and subjects with depression revealed significantly lower scores for ADL than those without depression (7).
Life expectancy is increasing worldwide, at the same time people are living longer with disabilities as well as functional health loss (8). ADL disability is the main source of functional disability, which are activities that individuals hard to perform to manage their basic physical needs in order to live independently and need help from others (9). The physical frailty indicators, such as body weight, gait speed, physical activity, and balance are predictors of future ADL disability (10, 11). ADL disability does not directly lead to death, but affects the quality of life, the burden of care and the prognosis of other diseases. Participants with ADL disability tended to have a lower quality of life based on the evidence that functional disability was significantly associated with all dimension scores of the 36-item short form survey (SF-36) in a cross-sectional study (12). According to a prospective study of 1,521 elderly individuals, ADL disability was a significant factor in increased use of care as reflected in the fact that medical expenditures were 2–3 times higher for patients with moderate to severe functional disabilities in the outpatient, emergency, and inpatient services (13).
Several studies from various regions have reported associations of chronic diseases or depressive symptoms with ADL disability but the magnitude of association remains to be assessed (14–17). According to the Canadian Study of Health and Aging (CSHA), among 9,008 community residents aged 65 and older, the occurrence of chronic diseases accounted for about 66% of the ADL disability (15). These findings suggest that chronic diseases are potential risk factors for functional disability, but evidence from cohort studies and the magnitude of association is lacking. Meanwhile, the effect of depressive symptoms on ADL disability is worthy of attention. People with depressive symptoms had a 130% greater risk of ADL disability than those without depressive symptoms among the African Americans of the Jackson Heart Study (16). In the Community Early Psychiatric Intervention Strategies (CEPIS) program in Singapore, higher levels of depressive symptoms were associated with a higher risk of ADL disability (17). However, the lack of evidence from large samples in China makes it impossible to assess the heterogeneity among current studies.
We aimed to explore the associations of chronic diseases and depressive symptoms with ADL disability according to the data from the China Health and Retirement Longitudinal Study (CHARLS). This has the potential benefit of providing a basis for targeted prevention policies to improve the efficiency of health services and reduce the burden of care.
Materials and methods
Study population
Participants in this cohort study were from the China Health and Retirement Longitudinal Study (CHARLS), which is an ongoing nationally representative longitudinal study. Details of the study design have been described elsewhere (18). In brief, a total of 17,708 participants were recruited by a multistage probability sampling procedure involving 150 counties or districts and 450 communities within 28 provinces of China at baseline in 2011 with a response rate of 80.5%. Data on socio-demographic and lifestyle factors and health-related information were collected by about 500 professional interviewers who worked in this field. Quality of these data was checked using a computer-assisted personal interviewing system. All participants were followed up biennially after the baseline survey. Therefore, this study used participants from two waves of the CHARLS (2011 and 2015), who were aged 45 and above at baseline. The CHARLS was approved by the Biomedical Ethics Review Committee (IRB00001052-11015), and written informed consent was obtained from all participants. At baseline, 17,708 CHARLS participants were enrolled. Of these, 423 individuals were excluded for being younger than 45 years, and 2,379 were excluded for having any disabilities at baseline. Further, respondents who had missing values on depressive symptoms, chronic diseases or covariates were excluded (n = 4,042). Finally, 10,864 participants were included for analysis in this study.
Assessment of chronic diseases
Chronic diseases were self-reported based on a physician's diagnosis using the following standardized question: “Have you been diagnosed with such conditions as listed below by a doctor?.” In this regard, CHARLS provided 14 chronic diseases in the inventory as follows: hypertension, dyslipidemia, diabetes, cancer or malignant tumor, chronic lung diseases (such as chronic bronchitis and emphysema), liver disease, heart problems (such as heart attack, coronary heart disease, angina, and congestive heart failure), stroke, kidney disease, stomach or other digestive diseases, emotional, nervous, or psychiatric problems, memory-related disease (such as dementia, brain atrophy, and Parkinson's disease), arthritis or rheumatism and asthma. Each of the conditions was ascertained one by one by the interviewers.
Assessment of depressive symptoms
Depressive symptoms in the past week were assessed at baseline using the 10-items Center for Epidemiologic Studies Depression (CESD-10) scale short form (19, 20). Each item was rated on a 4-point Likert scale with answers varying from 0 [rarely or none of the time (<1 day)] to 3[most or all of the time (5–7 days)]. The items 5 and 8 were reverse scored before summing all the item scores. The total score of CESD-10 ranged from 0 to 30, and higher scores indicated more depressive symptoms. The CESD-10 has been widely used in epidemiological studies and has high reliability and validity among Chinese adults (21). According to previous studies, participants with a total score of 12 or higher were defined as having elevated depressive symptoms (21).
Outcome ascertainment
The study outcome was incident ADL functional limitations. Functional limitations at follow-up were assessed using the Katz ADL scales (22). The Katz ADL scale assessed daily self-care tasks including taking bathing, dressing, eating, getting into and out of bed, toileting and controlling urination and defecation. The Katz ADL scale was extensively used in previous studies among Chinese older adults, and the Chinese version provided reliable and valid responses (23, 24). Each of the following answers, as provided in CHARLS, was used to assess each of the preceding items in the Katz ADL scale: (1) No, I do not have any difficulty, (2) I have difficulty but still can do it, (3) Yes, I have difficulty and need help, and (4) I cannot do it. Participants who reported needing any help in any item were classified as having ADL disability (25). Participants who reported one or more limitations during the follow-up period were defined as having incident ADL disability.
The measures of covariates
The socio-demographic information included age, gender, marital status and education level. Marital status was divided into married and non-married. That is, non-married status included the separated, divorced, widowed, and never married. Education level was classified as no formal education, primary school, middle or high school, and college or above.
Health-related information included self-rated childhood health, history of fall (yes/no), history of hip fracture (yes/no), history of traffic accident (yes/no), smoking (current/ex-smoker and no), alcohol drinking (often/seldom/never), sleep duration at night (<7, 7–8, and >8 h), nap duration after lunch (<30, 30–60, and >60 min), and body pain (yes/no). All these covariates were associated with ADL disability in the elderly in previous studies (26, 27). Self-rated childhood health status was assessed by asking participants the following question: “how would you evaluate your health during childhood, up to and including the age of 15?.” In this regard, the participants were asked to rate their health on a five points scale with the following response categories: (5) excellent, (4) very good, (3) good, (2) fair, and (1) poor. Further, (5), (4), and (3) were combined to indicate “good health.”
Participants who drank alcohol (such as beer, wine, or liquor) more than once a month in the past year were defined as often drinkers. Sleep duration at night was self-reported according to the question: “during the past month, how many hours of actual sleep did you get at night?” Sleep duration was divided into three groups: <7, 7–8, and >8 h. Nap duration was measured using a single question as follows: “during the past month, how long did you take a nap after lunch?”. Nap duration was classified into three groups: <30, 30–60, and >60 min. History of fall was assessed using a single item: “have you fallen down in the last two years?.” Body pain was assessed by the question: “are you often troubled with any body pains?.”
Social participation was measured by asking respondents to indicate whether they have participated in various social activities including playing mah-jong, and chess or cards; attending a community, sports, and social or other clubs; participating in a community-related organization; participating in voluntary or charity work; and attending any educational or training courses in the past 12 months. Participants who have not engaged in any activities stated above were defined as low social participation.
Statistical analysis
Data were summarized as mean and standard deviation (SD) for each normally distributed continuous variable, and as median and interquartile range for each non-normally distributed continuous variable. Frequencies and percentages were used to describe categorical variables. Baseline characteristics were summarized and stratified according to the depression symptoms. We used the Chi-square test, Student's t test or Mann-Whitney U test to examine the differences in sample characteristics between those with and without depression symptoms.
Person-time of follow-up for each subject from the date of 2011 to the dates of ADL disability ascertainment (every 2 years), death, loss to follow-up, or the end of follow-up (June 31, 2015), whichever came first. The incidence rate of ADL disability per 1,000 person-years was calculated based on cases of ADL disability and total person-time of follow-up according to different status of chronic disease (yes/no) and depression symptoms (yes/no), respectively. The association between chronic diseases, depressive symptoms and ADL disability was examined using Cox proportional hazards models, from which hazard ratios (HRs) with their corresponding 95% confidence intervals (CI) were obtained. Three models were estimated: in model 1, age and gender were adjusted; in model 2, age, gender, education, marital status, smoking, alcohol drinking, sleep duration, and nap duration were adjusted; and in model 3, variables in model 2 plus childhood health status, history of fall, history of hip fracture, history of traffic accident, body pain, and social participation were adjusted.
To further examine the association between the severity of depression symptoms and risk of ADL disability, the scores of depressive symptoms were split into quintiles and then were included in Cox proportional hazards models with quintile 1 as the reference group. Additionally, we explored the potential non-linear associations using 5-knotted restricted cubic spline regression.
To further examine the potential additive interaction between chronic diseases and depressive symptoms on the risk of incident ADL disability, four subgroups were created as follows: (1) people with no chronic disease and depressive symptoms, (2) people with no chronic disease but have depressive symptoms, (3) people with at least one chronic disease but no depressive symptoms, and (4) people with at least one chronic disease and depressive symptoms. Group (1) was the reference group. Synergy Index (SI) was used to provide more insight on the additive interaction between them (28). The synergy index is the ratio of the risk of the joint effect to the sum of the individual risks. If the confidence interval of SI contains 1, it indicates that the two factors have no interaction (29). All analyses were performed using STATA statistical software version 16.0 (STATA Corp, College Station, Texas, USA). Two-sided P < 0.05 was considered statistically significant.
Results
Baseline information
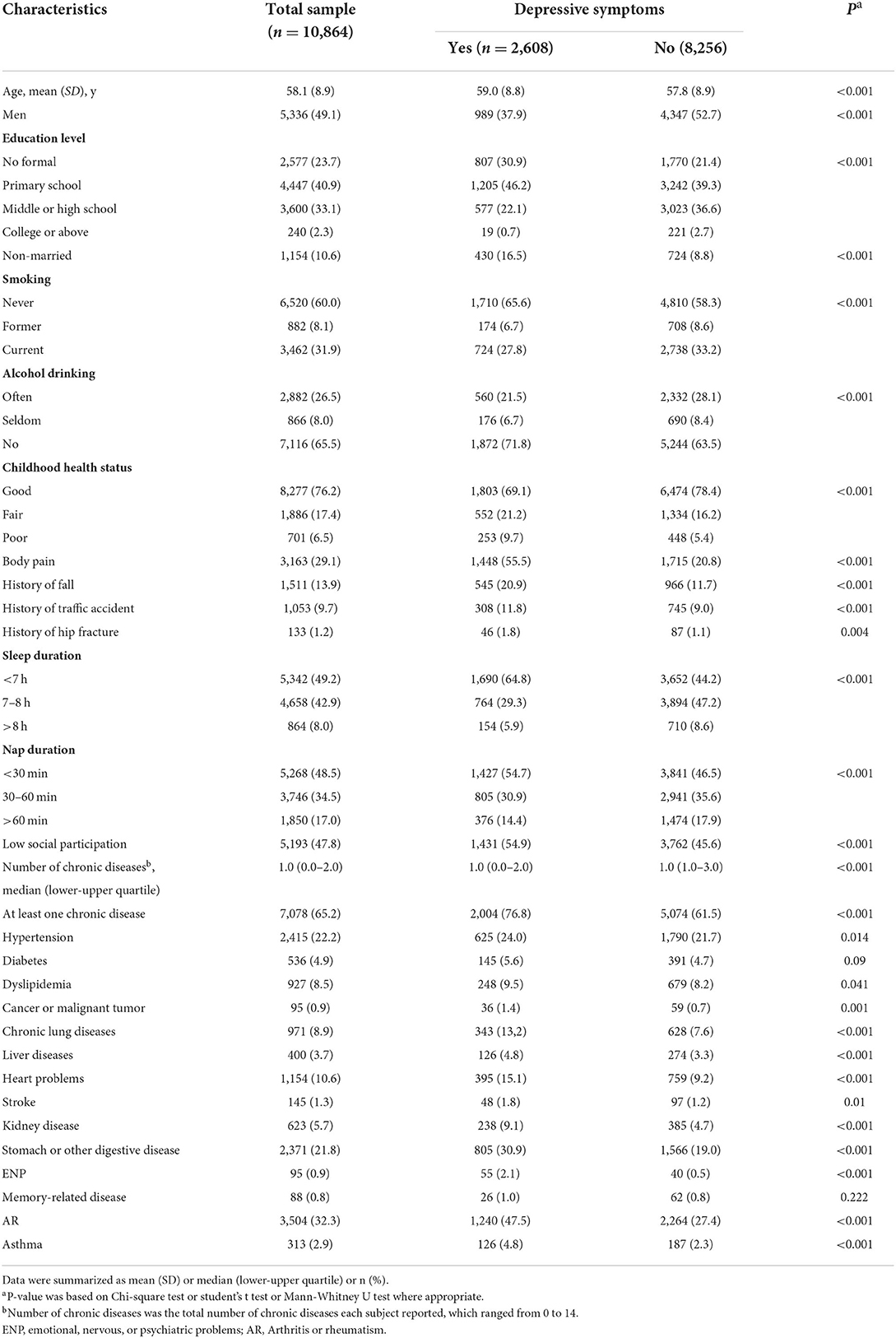
Baseline characteristics of participants according to depressive symptoms status are presented in Table 1. Thus, the mean (SD) age at baseline was 58.1 (8.9) years. In addition, 5,336 (49.1%) of the participants were men, 2,577 (23.7%) had no formal education and 1,154 (10.6%) of them had unstable marital status. A total of 2,608 (24.0%) of the participants reported having depressive symptoms. Furthermore, 6,520 (60.0%) of the participants never smoked, 2,882 (26.5%) often drank alcohol, 1,511 (13.9%) had a history of fall down, 1,053 (9.7%) had a history of traffic accidents and 133 (1.2%) had a history of hip fracture. Regarding chronic diseases, 7,078 (65.2%) individuals reported having at least one chronic disease.
Arthritis or rheumatism (32.3%) was the most reported chronic disease in the middle-aged and older population. This was followed by hypertension (22.2%), then stomach or other digestive diseases (21.8%). Diabetes was reported in 536 (4.9%) of the participants, and 927 (8.5%) reported having dyslipidemia. Participants with the following attributes were more likely to have depressive symptoms: older, women, not married, lower education level, never smoking and drinking, less sleep and nap duration, poor self-rated childhood health, a history of fall, traffic accident or hip fracture, low social participation, a higher prevalence of hypertension, dyslipidemia, cancer, chronic lung disease, liver disease, digestive disease, heart problems, stroke, kidney disease, ENP, AR, and asthma.
The associations between chronic disease, depressive symptoms and ADL disability
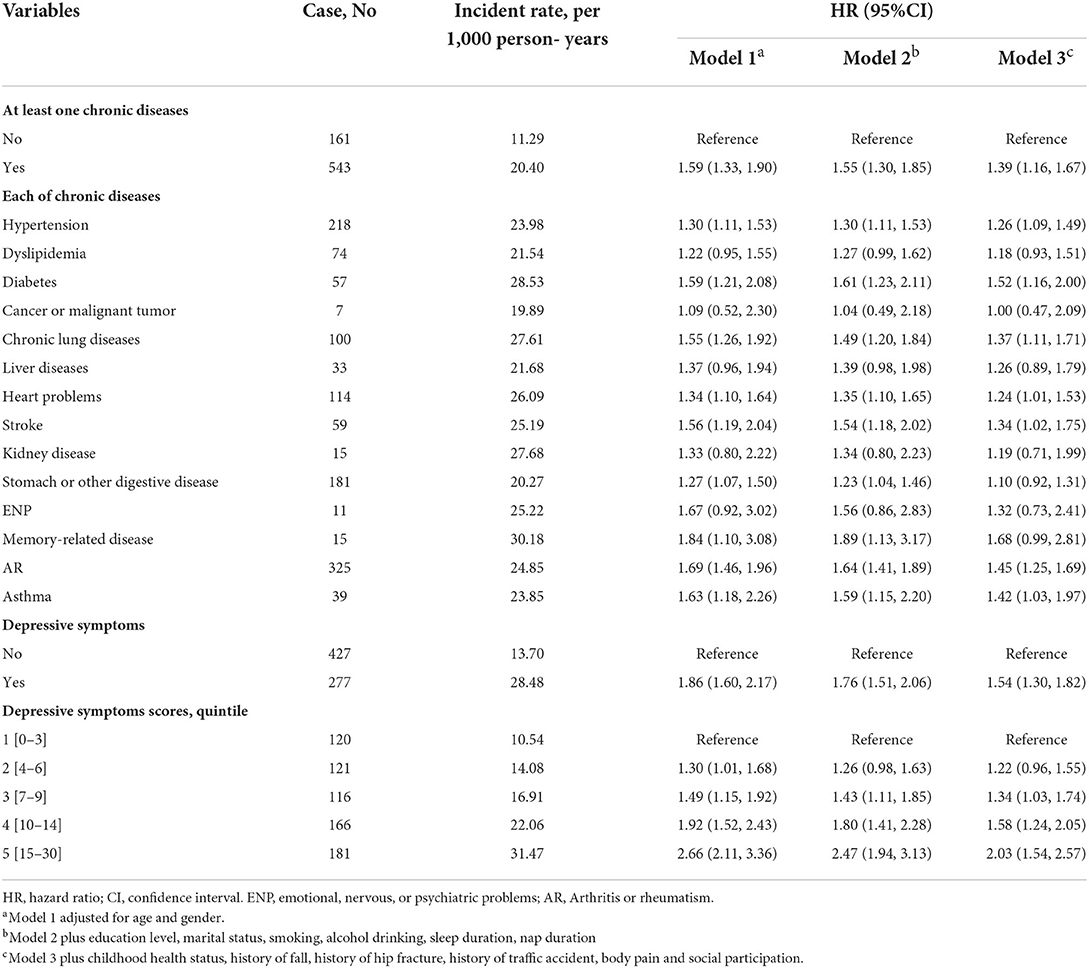
During the follow-up period from 2011 to 2015, a total of 704 participants reported having incident ADL disability. The incident rate of ADL disability was 17.22 per 1,000 person-years. The incident rate was 11.29 per 1,000 person-years among participants without chronic disease and 20.40 per 1,000 person-years among participants with chronic disease. The incident rate was 13.70 per 1,000 person-years among participants without depression symptoms and 28.48 per 1,000 person-years among participants with depression symptoms.
Table 2 shows the associations between chronic disease, depressive symptoms and ADL disability. After adjusting for potential confounders in model 3, the results indicated that having at least one chronic disease among participants was independently associated with an increased risk of ADL disability (adjusted HR, 1.39; 95%CI: 1.16–1.67). Specifically, hypertension, diabetes, chronic lung diseases, heart problems, stroke, arthritis or rheumatism, and asthma were associated with the increased risk of ADL disability after adjusting for potential confounders. Moreover, participants with depressive symptoms were more likely to report ADL disability after adjusting for potential confounders (adjusted HR, 1.54; 95%CI: 1.30–1.82). Similar results were obtained when modeling the total CESD-10 scores as quintiles (Table 2). After adjusting for confounders, by comparing quintile 5 score with quintile 1, the adjusted HR was 2.03(95%CI: 1.54–2.57) for incident ADL disability. A linear and positive association between the CESD-10 total score and risk of incident ADL events using restricted cubic spline regression was also found (for non-linearity, P = 0.383) (Figure 1).
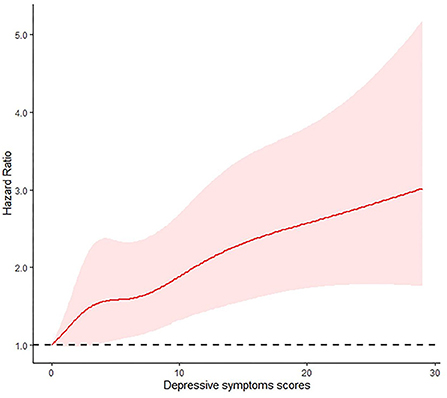
Figure 1. Adjusted Hazard Ratios (HRs) of depressive symptoms scores on ADL disability. Results from the restricted cubic spline Cox proportional hazards regression model.
The incidence rate was 10.00 per 1,000 person-years among participants without chronic disease and depression symptoms. The incidence rate was 31.62 per 1,000 person-years among participants with both chronic disease and depression symptoms. However, there is no statistically significant additive interaction between chronic disease and depression symptoms for incident ADL disability. The Synergy Index was 1.34 (95%CI: 0.65–2.75). The result was presented in Table 3.
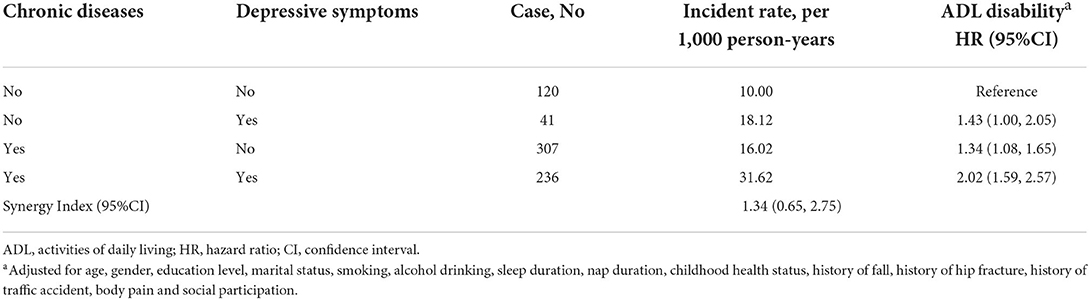
Table 3. The interaction between chronic diseases and depressive symptoms on incident ADL disability.
Discussion
This study has shown that chronic diseases and depressive symptoms were significantly associated with ADL disability. That is, people with at least one chronic disease had a 39% higher risk of developing functional disability than those without chronic disease. Also, depressive symptoms were positively associated with the risk of ADL disability.
The data from the longitudinal study were analyzed to elucidate the role of chronic diseases and depressive symptoms in the pathway from normal to ADL disability. Our study increased the evidence for the associations of chronic diseases and depressive symptoms with risk of ADL disability. In total, we considered 14 types of chronic diseases and estimated the magnitude of association between chronic diseases and ADL disability. According to a previous population-based cross-sectional study, ADL disability after a recent stroke was associated with a 45% higher risk of recurrent stroke (30). Stroke was the most common cause of ADL disability in subjects aged 65–74 years (6). Physical disability was highest for stroke, followed by cancer and diabetes at the time of the initial disease diagnosis (31). Diabetic polyneuropathy (DPN) is a common complication of diabetes, and the symptom of decreased muscle strength occurs in the lower limbs and progresses upward, eventually emerging in the upper extremities (32). Muscle strength is an important factor in maintaining ADL (33).
Consistent with the findings of this study, depression symptoms was strongly associated with ADL disability, even after adjustment for demographic factors, socioeconomic conditions, and chronic diseases (34, 35). The finding of the Chicago Neighborhood and Disability Study showed that depressive symptoms were associated with ADL disability in both older blacks and whites. Meanwhile, depressive symptoms increased the odds of onset of disability over time in whites more than blacks (36). Our study suggests that the improvement of depressive symptoms has a positive preventive effect on ADL disability in Chinese. However, several studies demonstrated that people with ADL dependency would be more likely to develop depressive symptoms (37, 38). The relationships between each other need more studies to explore in the future.
Inflammation and albuminuria are involved in the effects of chronic diseases on ADL disability, and the detection of these biomarkers has clinical significance. Elevated levels of C-reactive protein (CRP) and urinary albumin-to-creatinine ratio were independently associated with ADL disability among older adults with cardiovascular disease, and subjects with higher levels of both markers had a more unfavorable metabolic profile than those with lower levels (39). In addition, macroalbuminuria was associated with disability in ADL (OR = 1.94, 95%CI: 1.24–3.03) and there was an interaction effect between elevated CRP and albuminuria on ADL disability among older adults with diabetes (40). Meanwhile, high-sensitivity CRP has sufficient value as a predictor of the prognosis of ADL disability after the first-ever stroke (41).
There are several potential mechanisms on the association between depressive symptoms and risk of ADL disability. First, this increased risk is partly due to the fact that people with depression decrease physical activity (42, 43). Physical activity is a beneficial protective factor of ADL disability that deserves attention. Second, depression is a risk factor for non-adherence to treatment that can affect prognosis and lead to poor outcomes, including ADL disability (44). Patients with comorbid depression and other diseases, such as diabetes and heart problems, have more symptoms of the disease, making it difficult to recover and leading to disability development (45). Considering this, policymakers should adopt strategies to improve chronic disease management in the community while screening older adults for mental health issues to prevent ADL disability.
Several limitations of this study need to be acknowledged. First, there are problems with the accuracy of self-reported depression symptoms and medical status in large-scale follow-up surveys, thus recall bias cannot avoidable. Second, it would be cautious to infer the causal relationship due to the observational study design. Third, only participants from China were involved in this study, thus the findings may not fully generalize to other countries and populations. Fourth, we did not adjust the analysis for the covariate such as financial situation and cognition, and they affected ADL and also affected depressive symptoms (46, 47), thus confounding bias could not be ruled out. Fifth, we did not find a statistically significant interaction between chronic diseases and depressive symptoms on incident ADL disability. However, people with chronic diseases and depressive symptoms have a higher risk of ADL disability based on the point estimate. Finally, our study provided evidence for previous studies and verified these results, however, an inherent limitation is lack of substantial novelty.
Conclusions
Chronic diseases and depressive symptoms are associated with an increased risk of ADL disability in middle-aged and older Chinese adults. Potential strategies need to focus on improving chronic diseases and depressive symptoms to prevent functional disability in the future.
Data availability statement
CHARLS data are available at http://charls.pku.edu.cn/pages/data/111/zh-cn.html.
Ethics statement
The studies involving human participants were reviewed and approved by the Biomedical Ethics Review Committee of Peking University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
ZH designed the study. YH and FZ drafted the manuscript. ZH, ACK, and SY edited the manuscript. All authors approved the final version of the manuscript.
Funding
This study was supported by the Natural Science Foundation of Hunan Province (No. 2022JJ40248), Hunan Cancer Hospital Climb Plan (No. QH2021003), and Scientific Research Project of Hunan Provincial Health Commission (No. 202212054721).
Acknowledgments
The data used in this paper are from China Health and Retirement Longitudinal Study (CHARLS). We thank all participants and staff from CHARLS.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kanasi E, Ayilavarapu S, Jones J. The aging population: demographics and the biology of aging. Periodontol 2000. (2016) 72:13–8. doi: 10.1111/prd.12126
2. Spannella F, Giulietti F, Cocci G, Landi L, Lombardi FE, Borioni E, et al. Acute exacerbation of chronic obstructive pulmonary disease in oldest adults: predictors of in-hospital mortality and need for post-acute care. J Am Med Dir Assoc. (2019) 20:893–8. doi: 10.1016/j.jamda.2019.01.125
3. Chen CM, Su YY, Lan TY, Mullan J, Shi HY, Chiu HC. Health-related services use and the onset of functional disability: 10 year follow-up study. Arch Gerontol Geriatr. (2014) 58:356–63. doi: 10.1016/j.archger.2013.11.011
4. Tsai AC, Lee LC, Wang JY. Complementarity of the mini-nutritional assessment and activities of daily living for predicting follow-up mortality risk in elderly Taiwanese. Br J Nutr. (2013) 109:658–66. doi: 10.1017/S0007114512001730
5. Kim SH, Cho B, Won CW, Hong YH, Son KY. Self-reported health status as a predictor of functional decline in a community-dwelling elderly population: nationwide longitudinal survey in Korea. Geriatr Gerontol Int. (2017) 17:885–92. doi: 10.1111/ggi.12797
6. Yoshida D, Ninomiya T, Doi Y, Hata J, Fukuhara M, Ikeda F, et al. Prevalence and causes of functional disability in an elderly general population of Japanese: the Hisayama study. J Epidemiol. (2012) 22:222–9. doi: 10.2188/jea.JE20110083
7. Wada T, Ishine M, Sakagami T, Okumiya K, Fujisawa M, Murakami S, et al. Depression in Japanese community-dwelling elderly–prevalence and association with ADL and QOL. Arch Gerontol Geriatr. (2004) 39:15–23. doi: 10.1016/j.archger.2003.12.003
8. GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1260–1344. doi: 10.1016/S0140-6736(17)32130-X
9. Mlinac ME, Feng MC. Assessment of activities of daily living, self-care, and independence. Arch Clin Neuropsychol. (2016) 31:506–16. doi: 10.1093/arclin/acw049
10. Vermeulen J, Neyens JCL, van Rossum E, Spreeuwenberg MD, de Witte LP. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review. BMC Geriatr. (2011) 11:33. doi: 10.1186/1471-2318-11-33
11. Okabe T, Abe Y, Tomita Y, Mizukami S, Kanagae M, Arima K, et al. Age-specific risk factors for incident disability in activities of daily living among middle-aged and elderly community-dwelling Japanese women during an 8-9-year follow up: the Hizen-Oshima study. Geriatr Gerontol Int. (2017) 17:1096–101. doi: 10.1111/ggi.12834
12. Ji J, Zhang L, Zhang Q, Yin R, Fu T, Li L, et al. Functional disability associated with disease and quality-of-life parameters in Chinese patients with rheumatoid arthritis. Health Qual Life Outcomes. (2017) 15:89. doi: 10.1186/s12955-017-0659-z
13. Wu CY, Hu HY, Li CP, Fang YT, Huang N, Chou YJ. The association between functional disability and acute care utilization among the elderly in Taiwan. Arch Gerontol Geriatr. (2013) 57:177–83. doi: 10.1016/j.archger.2013.04.011
14. Li ZY, Wu JL, Li JJ, Pei LJ. A cohort study on the influence of the chronic diseases on activities of daily living of the elderly aged 65 years and over in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2019) 40:33–40. doi: 10.3760/cma.j.issn.0254-6450.2019.01.008
15. Griffith L, Raina P, Wu H, Zhu B, Stathokostas L. Population attributable risk for functional disability associated with chronic conditions in Canadian older adults. Age Ageing. (2010) 39:738–45. doi: 10.1093/ageing/afq105
16. Kalyani RR, Ji N, Carnethon M, Bertoni AG, Selvin E, Gregg EW, et al. Diabetes, depressive symptoms, and functional disability in African Americans: the Jackson Heart Study. J Diabetes Complications. (2017) 31:1259–65. doi: 10.1016/j.jdiacomp.2017.03.003
17. Nyunt MSZ, Lim ML, Yap KB, Ng TP. Changes in depressive symptoms and functional disability among community-dwelling depressive older adults. Int Psychogeriatr. (2012) 24:1633–41. doi: 10.1017/S1041610212000890
18. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
19. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
20. Fu H, Si L, Guo R. What is the optimal cut-off point of the 10-item center for epidemiologic studies depression scale for screening depression among chinese individuals aged 45 and over? An exploration using latent profile analysis. Front Psychiatry. (2022) 13:820777. doi: 10.3389/fpsyt.2022.820777
21. Chen H, Mui AC. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int Psychogeriatr. (2014) 26:49–57. doi: 10.1017/S1041610213001701
22. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. (1963) 185:914–9. doi: 10.1001/jama.1963.03060120024016
23. Han Y, Xue J, Pei W, Fang Y. Hierarchical structure in the activities of daily living and trajectories of disability prior to death in elderly Chinese individuals. BMC Geriatr. (2021) 21:522. doi: 10.1186/s12877-021-02460-y
24. Yang Y, Du Z, Liu Y, Lao J, Sun X, Tang F. Disability and the risk of subsequent mortality in elderly: a 12-year longitudinal population-based study. BMC Geriatr. (2021) 21:662. doi: 10.1186/s12877-021-02611-1
25. Connolly D, Garvey J, McKee G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil Rehabil. (2017) 39:809–16. doi: 10.3109/09638288.2016.1161848
26. Li ZH, Lv YB, Kraus VB, Yin ZX, Liu SM, Zhang XC, et al. Trends in the incidence of activities of daily living disability among Chinese older adults from 2002 to 2014. J Gerontol A Biol Sci Med Sci. (2020) 75:2113–8. doi: 10.1093/gerona/glz221
27. Cwirlej-Sozańska A, Wiśniowska-Szurlej A, Wilmowska-Pietruszyńska A, Sozański B. Determinants of ADL and IADL disability in older adults in southeastern Poland. BMC Geriatr. (2019) 19:297. doi: 10.1186/s12877-019-1319-4
28. Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. (2005) 20:575–9. doi: 10.1007/s10654-005-7835-x
29. de Mutsert R, Jager KJ, Zoccali C, Dekker FW. The effect of joint exposures: examining the presence of interaction. Kidney Int. (2009) 75:677–81. doi: 10.1038/ki.2008.645
30. Park JH, Ovbiagele B. Relationship of functional disability after a recent stroke with recurrent stroke risk. Eur J Neurol. (2016) 23:361–7. doi: 10.1111/ene.12837
31. Chou CY, Chiu CJ, Chang CM, Wu CH, Lu FH, Wu JS, et al. Disease-related disability burden: a comparison of seven chronic conditions in middle-aged and older adults. BMC Geriatr. (2021) 21:201. doi: 10.1186/s12877-021-02137-6
32. Nomura T, Kawae T, Kataoka H, Ikeda Y. Assessment of lower extremity muscle mass, muscle strength, and exercise therapy in elderly patients with diabetes mellitus. Environ Health Prev Med. (2018) 23:20. doi: 10.1186/s12199-018-0710-7
33. Wang DXM, Yao J, Zirek Y, Reijnierse EM, Maier AB. Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle. (2020) 11:3–25. doi: 10.1002/jcsm.12502
34. Dunlop DD, Manheim LM, Song J, Lyons JS, Chang RW. Incidence of disability among preretirement adults: the impact of depression. Am J Public Health. (2005) 95:2003–8. doi: 10.2105/AJPH.2004.050948
35. Peng S, Wang S, Feng XL. Multimorbidity, depressive symptoms and disability in activities of daily living amongst middle-aged and older Chinese: evidence from the China Health and Retirement Longitudinal Study. J Affect Disord. (2021) 295:703–10. doi: 10.1016/j.jad.2021.08.072
36. Rajan KB, Barnes LL, Wilson RS, Evans DA, Mendes de Leon CF. Racial differences on association of depressive symptoms with combined basic and instrumental activities of daily living. J Gerontol A Biol Sci Med Sci. (2014) 69:215–22. doi: 10.1093/gerona/glt074
37. He M, Ma J, Ren Z, Zhou G, Gong P, Liu M, et al. Association between activities of daily living disability and depression symptoms of middle-aged and older Chinese adults and their spouses: a community based study. J Affect Disord. (2019) 242:135–42. doi: 10.1016/j.jad.2018.08.060
38. Luna-Orozco K, Fernández-Niño JA, Astudillo-García CI. Association between physical disability and incidence of depressive symptoms in older Mexican adults. Biomedica. (2020) 40:641–55. doi: 10.7705/biomedica.5398
39. Kuo HK, Al Snih S, Kuo YF, Raji MA. Chronic inflammation, albuminuria, and functional disability in older adults with cardiovascular disease: the National Health and Nutrition Examination Survey, 1999-2008. Atherosclerosis. (2012) 222:502–8. doi: 10.1016/j.atherosclerosis.2012.03.004
40. Kuo HK, Al Snih S, Kuo YF, Raji MA. Cross-sectional associations of albuminuria and C-reactive protein with functional disability in older adults with diabetes. Diabetes Care. (2011) 34:710–7. doi: 10.2337/dc10-1977
41. Song IU, Kim YD, Kim JS, Lee KS, Chung SW. Can high-sensitivity C-reactive protein and plasma homocysteine levels independently predict the prognosis of patients with functional disability after first-ever ischemic stroke? Eur Neurol. (2010) 64:304–10. doi: 10.1159/000321415
42. Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health. (1999) 89:1346–52. doi: 10.2105/AJPH.89.9.1346
43. Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. (2013) 45:649–57. doi: 10.1016/j.amepre.2013.08.001
44. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. (2000) 160:2101–7. doi: 10.1001/archinte.160.14.2101
45. Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. (2011) 13:7–23. doi: 10.31887/DCNS.2011.13.1/wkaton
46. Gracia-García P, López-Antón R, Santabárbara J, Quintanilla MÁ, De la Cámara C, Marcos G, et al. Cognition and daily activities in a general population sample aged +55. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. (2021) 28:270–83. doi: 10.1080/13825585.2020.1745140
Keywords: chronic diseases, depressive symptoms, activities of daily living, cohort study, the elderly
Citation: Hu Y, Zhou F, Kaminga AC, Yan S and Hu Z (2022) Associations of depressive symptoms and chronic diseases with activities of daily living among middle-aged and older population in China: A population-based cohort study. Front. Psychiatry 13:848255. doi: 10.3389/fpsyt.2022.848255
Received: 04 January 2022; Accepted: 04 July 2022;
Published: 08 August 2022.
Edited by:
Ondrej Bezdicek, Charles University, CzechiaReviewed by:
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, IranJiun-Yi Wang, Asia University, Taiwan
Chi Shen, Xi'an Jiaotong University, China
Copyright © 2022 Hu, Zhou, Kaminga, Yan and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shipeng Yan, eWFuc2hpcGVuZ0BobmNhLm9yZy5jbg==; Zhao Hu, NjM1MDk0NDgxQHFxLmNvbQ==
†These authors have contributed equally to this work
 Yingyun Hu
Yingyun Hu Feixiang Zhou
Feixiang Zhou Atipatsa Chiwanda Kaminga
Atipatsa Chiwanda Kaminga Shipeng Yan
Shipeng Yan Zhao Hu
Zhao Hu