
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 28 March 2022
Sec. Anxiety and Stress Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.843984
This article is part of the Research TopicUnderstanding Perinatal Mental Health Psychiatric ImpactView all 6 articles
 Dawit Tamiru1*
Dawit Tamiru1* Tadesse Misgana2
Tadesse Misgana2 Mandaras Tariku2
Mandaras Tariku2 Dejene Tesfaye2
Dejene Tesfaye2 Daniel Alemu2
Daniel Alemu2 Adisu Birhanu Weldesenbet3
Adisu Birhanu Weldesenbet3 Berhe Gebremichael3
Berhe Gebremichael3 Merga Dheresa4
Merga Dheresa4Background: Antenatal common mental disorder is a significant public health issue, especially in low- and middle-income countries with an extensive treatment gap. Common mental disorders have multifaceted implications on maternal and fetal health outcomes during pregnancy with long-running economic and social sequels. This study aimed to determine the prevalence of common mental disorder and associated factors among pregnant mothers in eastern Ethiopia, Kersa and Haramaya Health, and Demographic surveillance sites.
Methods: A community-based cross-sectional study was conducted in Kersa and Haramaya health and demographic surveillance sites from January 30 to April 30, 2021. World Health Organization Self-Reporting Questionnaire (SRQ-20) was used to measure common mental disorder among 1,015 randomly selected pregnant women. Data were collected face-to-face using open data kit software. Logistic regression was fitted to identify factors associated with common mental disorders.
Results: The overall prevalence of common mental disorders (SRQ > 6) among pregnant women was 37.5% (95% CI: 34.5, 40.5). Current substance use (AOR = 1.99, 95% CI 1.37, 2.88), intimate partner violence (AOR = 2.67, 95% CI 2.02, 3.53), null parity (AOR = 3.10, 95% CI 1.65, 5.84), gestational age [first trimester (AOR = 2.22, 95% CI 1.01, 4.93) and third trimester (AOR = 1.74, 95% CI 1.31, 2.31)], history of abortion (AOR = 2.03, 95% CI 1.27, 3.24), and absence of antenatal care follow-up (AOR = 1.43, 95% CI 1.08, 1.89) were significantly associated with common mental disorder during pregnancy.
Conclusion: Common mental disorders are prevalent among pregnant women in the study area with significant correlates. Administration of regular screening programs for maternal mental health conditions in rural, low-income communities, integrating into primary health care settings is imperative to reduce the risk.
Globally more than one billion people are affected by mental or addictive disorders, causing 19% of all years lived with disability (YLD) (1). Common mental disorders (CMDs) refer to a range of non-psychotic mental health conditions such as anxiety, depressive and somatoform disorders (1–3). The conditions are rampant in the population hence why they are deemed common and impact the mood or feelings of affected person. It is also common people experiencing more of these conditions simultaneously (3, 4).
The number of individuals with a CMD is increasing globally, mainly in lower-income countries, because of the increment in population and more people living to the age when depression and anxiety are common (2, 5). Globally, it is estimated that 3.6% (264 million) and 4.4% (322 million) and of the world’s population suffer from anxiety and depressive disorders, respectively. Estimates vary across regions, from a low of 2.6% in males in the western Pacific region to 7.7% among females in the Americas. In Ethiopia, 3.3% of the population suffers from anxiety disorders, while 4.7% face depression causing 3.5 and 10.1% of total YLD, respectively (2). The disorders are more common among females than males, particularly in pregnant women (2, 5, 6).
Mental health in pregnant women is a significant public health matter, especially in low- and middle-income countries (LMICs) (7, 8). Although pregnancy is generally considered a period of contentment, the state increases vulnerability to psychiatric conditions like common mental disorders (9). Even though symptom scores for depression in studies are elevated in antepartum compared to after childbirth, postnatal depression has been a focus of concern, while depression during pregnancy has been relatively neglected (10). The prevalence of CMDs among pregnant women ranges from 1 to 37%, with an increasing threshold, mainly in low and middle-income countries (11–13). However, common mental disorders during pregnancy are often left under diagnosed and untreated because conditions are usually ascribed to typical experiences of pregnancy (14).
Untreated CMD during pregnancy can lead to the negative child, mother, and family conditions, including poor antenatal clinic follow-up, poor nutrition and self-care, higher substance abuse, suicidal ideation, and thoughts of hurting the fetus, development of depression after childbirth, neglect of the child, and family breakdown (15, 16). CMDs during the antenatal period have also been associated with adverse pregnancy and child well-being effects, including lower birth weight, prematurity, neonatal mortality, and deficient child nutrition status, behavioral, emotional, and cognitive development (17, 18).
Multiple constituents and psychosocial determinants have been distinguished as contributing to common mental disorders during pregnancy. The most common ascertained circumstances include lack of social support, history of violence, pressure to have a child, history of mental illness, unplanned pregnancy, and adverse life events, complications in past or index pregnancy, and pregnancy loss (13, 19, 20).
In LMICs, the treatment gap for mental health conditions is estimated to be over 80% (21). The high mental health burden among pregnant women accentuates the need for mental health services within the maternal health care system in low-income settings (22). The World Health Organization (23) endorsed maternal mental health care be integrated into primary health care for improved access (24, 25). Integration of CMD screening with antenatal care has also been mentioned as an effective strategy to realize WHO’s Mental Health Gap Action Program (MhGAP), which will lead to better maternal and child health outcomes (23, 26). Although Ethiopia has recently integrated mental health services into the primary healthcare system, the implementation faces many barriers (27, 28).
Ethiopia is galvanizing efforts to achieve continuum Growth and Transformation Plan II (GTP II) and Sustainable Development Goals (SDG). The need for interdisciplinary and inter-sectorial solutions to reach maternal and child health, as well as mental health goals, is highlighted (29).
Attitudes and professional treatment-seeking behavior for mental health problems in Ethiopia are generally low; doubt of discrimination for having a mental disorder, depending in non-formal aid source, and negative beliefs toward mental health services were the most commonly cited barriers (30, 31). Despite effective treatments are available, studies reported that many affected people do not seek professional help. It was indicated that less than 35% of adults with identifiable mental problems looked for professional help, in which more than 80% visited informal help sources (31, 32). Modern mental health services centers are concentrated in urban settings, which are not accessible to the majority of the population.
Describing the correlates of common mental disorders in pregnancy and childbirth is a crucial step in preventing and treating of the associated complications in lower-income countries. With a largely rural population, low mental health care service, and high maternal, infant, and neonatal mortality rates, Ethiopia lacks reliable data on the burden and effects of mental disorders (33, 34). Demographic and health surveys in the country generally have not included maternal mental health status as expected health outcomes and national data are rarely available; thus, the exact extent of the broader impact remains unclear and likely under-estimated (34, 35).
When resources are available, data are predominantly from health facility surveys, whereas a high proportion of pregnant women remain at home without seeking maternal health care service (34, 36). Therefore, this study aimed to determine the magnitude and determinants of common mental disorders during pregnancy in the eastern region of Ethiopia.
A community-based cross-sectional study was conducted in Kersa and Haramaya Health and Demographic Surveillance Sites (HDSS) from January 30 to April 30, 2021.
Kersa and Haramaya Health and Demographic Surveillance Site is one of the seven HDSS sites in the Ethiopian universities intended to reflect the countries’ health and demography. Kersa and Haramaya Demographic Surveillance and Health Research Center (KDS-HRC) was established in 2007. Kersa HDSS is located in Kersa District, Oromia Regional State, eastern Ethiopia. There are 35 rural sub-districts (Kebeles) and three small-town kebeles. The Kersa HDSS covers 24 of the 38 kebeles. Most inhabitants are farmers, with a small numbers working in trade, public service, or casual laborers.
Haramaya Woreda (district) is located in the East Hararghe Zone of Oromia Regional State. Haramaya Woreda has thirty-three rural and two urban kebeles (sub-districts). Haramaya HDSS covers 12 rural kebeles.
Rural eastern Ethiopia is where the majority of Khat (Catha edulis), psychoactive substances, in the country produced and exported abroad (37).
All pregnant women living in Kersa and Haramaya Health and Demographic Surveillance Sites (HDSS) were the source population. All registered pregnant women were enrolled in the study irrespective of their age and pregnancy trimester. Pregnant women were located from Health and Demographic surveillance sites registration server and interviewed in their homes. Pregnant women who could not communicate due to serious medical and psychiatric illnesses were excluded from the study.
The minimum sample size required for this study was determined using a single population proportion formula with assumptions of confidence level at 95% = 1.96, a margin of error (d) = 0.04, and a reasonable proportion of common mental disorder (P = 0.267) (38). After incorporating a design effect of 2 and a 10% non-response rate, the maximum sample size calculated for this study was 1,034. The calculated sample size was proportionally allocated based on the confirmed number of pregnant women in selected Kebeles (clusters); the study participants were then determined using simple random sampling.
Data was collected using Open Data Kit (ODK) tools. Observations were uploaded to the ODK aggregate server. The data collection instrument included socio-demographic and economic characteristics, reproductive, obstetric and gynecologic conditions, pre-existing medical and psychiatric conditions, substance use, intimate partner violence, and common mental disorder.
Self-Reporting Questionnaire (SRQ-20) was used to measure common antenatal mental disorders. The SRQ-20 is composed of twenty yes/no items asking about depressive, anxiety, panic, and somatic symptoms during the preceding 30 days. For this study, the total score was dichotomized (SRQ-20 < 6 versus SRQ ≥ 6), with high scores indicating a high level of CMD (39). Data on household economic status were collected using a tool adapted and modified from the Ethiopian Demographic and Health Survey (EDHS) of 2016 (40). Alcohol, Smoking, and Substance Involvement Screening Test (41) comprising eight questions or items covering ten substances, was used assessing substance use behavior of pregnant women. Khat was included under the stimulant category, and shisha was incorporated under tobacco. The experience of intimate partner violence (IPV) was assessed using the WHO multi-country study questionnaire constituting psychological, physical, and sexually violent acts, often accompanied by controlling behavior where a single positive answer indicated the presence of violence (42).
Twenty data collectors who have at least a B.Sc. degree in health sciences and working in Kersa and Haramaya Demographic Surveillance and Health Research Center (KDS-HRC) collected the data for this study. Besides, they were supervised by six M.Sc. holders. In addition, an intensive 3 days training was provided to data collectors and supervisors.
The data were collected by face-to-face interview using structured and semi-structured questionnaires prepared in ODK collect form, completed data were sent directly to the server. Pregnant women were interviewed in separate rooms in their home environment or inside their compounds during working hours 7 days of the week.
To maintain the consistency of the data collection tool, the questionnaire was prepared in English language and translated to local languages, Afaan Oromo and Amharic languages, and vice versa. To evaluate the acceptability and applicability of the procedures and tools, pre-testing was done on 5% of the sample size 1 week before the actual data collection in the kebeles that are not included in the samples from each site. To keep the completeness and consistency of the questionnaire, data collectors were closely supervised during the data collection process by the supervisors and investigators.
After data files were downloaded from the server, the data set were exported to Stata version 14.0 for cleaning, coding, and analysis. Categorical variables were described using simple frequencies and percentages. Continuous variables were defined using mean or median and inter-quartile ranges depending on their distribution and standard deviation. Bivariate analysis was done using binary logistic regression to see the association between each independent variable and common mental disorder. The final multivariate analysis model included all variables from the bivariate analysis with p ≤ 0.2 to control all possible confounders. The direction and strength of statistical association were measured by odds ratio with 95% CI. Finally, a P-value less than 0.05 were considered to declare the presence of a statistically significant association. The Hosmer–Lemeshow statistic and Omnibus test tested the model goodness of fit. The multi co-linearity test was also carried out to see the correlation between independent variables using VIF, standard error (SE), and tolerance tests.
Ethical approval was obtained from Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC) and submitted to the respective health bureau of each study site. The study was conducted under the Declaration of Helsinki and, participants were informed that participation in the study is voluntary; had the right to withdraw or refuse to participate in the study at any time. Throughout the study period, the confidentiality of the data was strictly followed; participants were interviewed in separate rooms in their home environment. Before starting data collection, information sheets are read, and written and signed consent was obtained from each participant. Pregnant women who screened positive for the common mental disorder were linked to health facilities for assessment and interventions.
From a total of 1,034 participants selected for the study, 1,015 consented to participate in the study yielding a response rate of 98.2%. Among the participants, 676 (66.6%) were between the age of 20–35 years with a mean of 30.1 years (SD = 8.5). The majority of the study participants, 982 (96.75%) were married in their current relationship, 1,012 (99.7%) were Muslim followers, and 1,010 (99.51%) were Oromo in ethnicity. About 772 (76.06%) of the participants neither read nor write and 900 (88.67) were housewives. About 388 (38.2%) of the participants were on a lesser quintile of wealth index (Table 1).
Among the study participants, 26 (2.56%) had a previous history of mental illness with a mean duration of 2.7 years (SD = 1.37). Of them, 10 (38.46%) were on the treatment. Twenty-three (2.27%) had a chronic medical illness, the majority (43.5%) being hypertension.
The majority of the study participants were grand multipara, woman who has had ≥5 births (live or stillborn) ≥28 weeks of gestation, (46.50%). Over half, 52.12% of the participants were in the third trimester and the mean gestational age of pregnant mothers was 28.91 (SD = 6.63) weeks. About 98 (9.66%) of the participants had a previous history of abortion while 48.08% have Antenatal Care (ANC) follow-up. About 70 (6.9%) of the participants had a history of a gynecological problem, of this tumor (41.43%) was the most prevalent one. The median age of pregnancy interval and marriage was 1.7 years (IQR = 0.56) and 17.7 years (IQR = 2.12), respectively (Table 2).
Based on the assessment made on substance abuse using ASSIST, about 207 (20.39%) and 158 (15.57%) of the participants reported as they were used any type of substance at least once in their lifetime and the last 3 months, respectively (Figure 1). Concerning psycho-social factors, 493 (48.57%) of women reported that they experienced any act of physical, sexual, or emotional (psychological) violence or any combination of the three by an intimate partner during their current pregnancy.
The overall prevalence of common mental disorder (SRQ > 6) among pregnant mother was found to be 37.5% (95% CI: 34.5, 40.5). About 180 (17.73%) of the women had no CMD symptoms and 454 (44.73%) had low CMD symptoms. Regarding the distribution of the symptoms, poor appetite (n = 350) was the most complained symptom followed by sleep disturbance (n = 285). The median SRQ-20 score was 2 (25th centile 1, 75th centile 8).
On bivariate analysis, age, wealth index, history of mental illness, history of chronic medical illness, current substance use, intimate partner violence, parity, gestational age, history of abortion, ANC follow up, history of the gynecological problem and gynecological operation had p-value score of less than 0.2 and entered into the multivariable analysis. In the multivariable logistic regression analysis model, however, only current substance use, intimate partner violence, parity, gestational age, history of abortion, and ANC follow-up were significantly associated with common mental disorders among pregnant women at a p-value of <0.05.
Pregnant women who use any type of substance in the past 3 months were two times (AOR = 1.99, 95% CI 1.37, 2.88) more likely to have CMD as compared to those women who didn’t use any types of substance. Those pregnant women who reported that they experienced intimate partner violence were 2.67 times (AOR = 2.67, 95% CI 2.02, 3.53) more likely to have CMD as compared to those women who didn’t report any act of physical, sexual, or psychological violence or any combination of the three by an intimate partner during the current pregnancy.
The odds of developing CMD were three times (AOR = 3.10, 95% CI 1.65, 5.84) higher among nulliparous women as compared with a multiparous woman. Pregnant women who had been in the first trimester (AOR = 2.22, 95% CI 1.01, 4.93) and third trimester (AOR = 1.74, 95% CI 1.31, 2.31) were 2.2 times and 1.74 times more likely to have CMD as compared to those pregnant on the second trimester, respectively. Women with a history of abortion are two times (AOR = 2.03, 95% CI 1.27, 3.24) more likely to experience antenatal CMD. Pregnant women who didn’t have an ANC follow-up for their current pregnancy were 1.43 times (AOR = 1.43, 95% CI 1.08, 1.89) more likely to develop CMD as compared to those who had an ANC visit (Table 3).
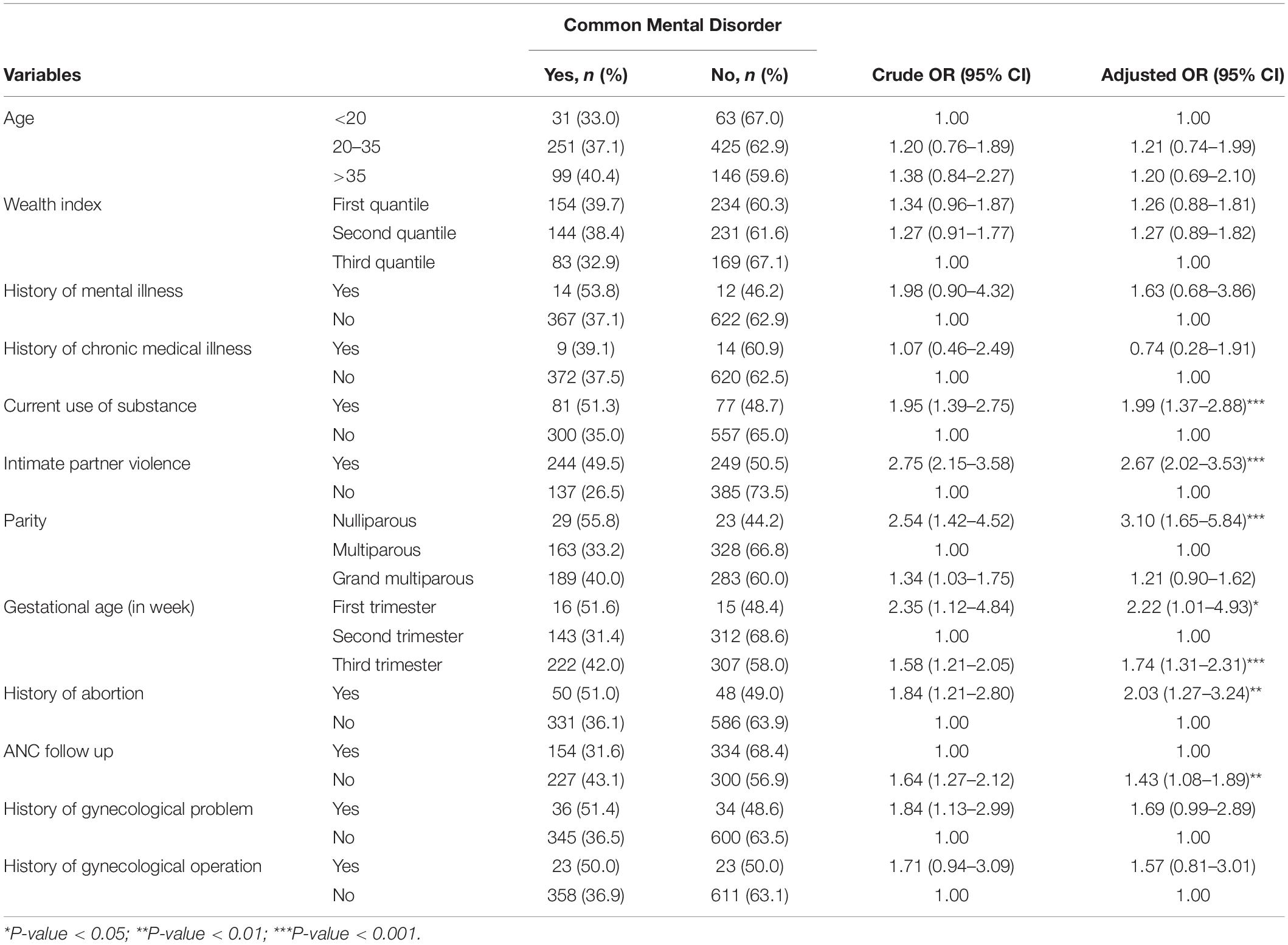
Table 3. Results of bivariate and multivariate analysis for factors associated with antenatal common mental disorders.
Almost two in five (37.5%) pregnant women had a common mental disorder in this study. In addition, current substance use, intimate partner violence, parity, gestational age, history of abortion, and lack of ANC attendance increased the odds of CMD.
The prevalence of 37.5% (95% CI: 34.5, 40.5) for common mental disorder among pregnant women in this study is consistent with other findings found in Bale, Ethiopia (35.8%) (19), Tanzania (39.5%) (43), South Africa (39%) (44), and Vietnam (37.4%) (45).
On the other hand, this result was higher than studies conducted in various regions of Ethiopia and other countries; Butajira (12%) (46), Gondar (23%) (47), and Addis Ababa (24.94%) (48), Brazil (20.2%) (49), and Nigeria (24.5%) (49). Likewise, in one community-based cross-sectional survey done in 20 sites across four countries, the prevalence of CMD was 21% in Vietnam, 33% in Ethiopia, 30% in India, and 30% in Peru (50). This difference might be due to the high magnitude of substance use, particularly Khat, in the current study setting, which significantly contributed to the development of mental illness (51). Additionally, poor utilization of ANC follow-up in the study setting might contribute to high maternal CMD.
The result is, however, lower than studies done in Jamaica (56%) (52), Turkish women (47.6%) (53), Nicaragua (57%) (54), Pakistan (49%) (55), and India (65%) (56). These variations might be due to disparities in measurement tools, and cut-off points used, Jamaican study used Zung self-rating depression scale (SDS > 50), Edinburgh postnatal depression scale (EDS) and the state and trait anxiety scale (STAI) were used in Turkey, India, and Nicaragua studies while Anxiety and Depression Scale (HADS, 11–21) were used in Pakistan. Conjointly, socio-cultural and economic variations, and geographical settings might also explain the observed difference.
In congruent with population-based cohort studies conducted in Ethiopia (57), India (58), Jordan (59), and Netherlands (60), pregnant women who use any type of substance were more likely to have CMD compared to those women who did not use any substance in the past 3 months. Mental health and substance use issues have a bidirectional cause-and-effect relationship. A pregnant woman using a substance often has complex social and mental health problems (51, 61). On the other hand, antenatal anxiety and depression could have a significant role in the causal mechanisms of substance use and prenatal stress, leading individuals to poor stress management and behavioral problems, both of which increase the risk of substance use disorder (62, 63). Similarly, a recent cross-sectional study found pregnant women with antenatal distress were more likely to chew Khat, as the women benefited from stimulant effects of Khat, including elation and alleviation of their symptoms (64).
Pregnant women, who reported intimate partner violence, were more likely to have CMD than those who did not report any acts of physical, sexual, or psychological violence or any combination of the three by an intimate partner during the current pregnancy. A similar finding was reported from the studies conducted in other areas of Ethiopia, Bale (19) and Butajira (65), Tanzania (66), and Vietnam (67). This might be because IPV can directly affect antenatal mental illnesses (68). First, having experienced partner violence, pregnant women may develop a stress response profile which heightens the neuroendocrine responses (69, 70). The collective effect of these responses can lead to mental illnesses. Secondly, women who had perinatal mental illness are more likely to be exposed to IPV during pregnancy than those who do not (71, 72). Finally, psychiatric disorders and IPV can happen along with structural stressors, such as low socioeconomic status or poor social support (73).
Nulliparous women were more likely to have CMD as compared to multiparous women. This finding was in agreement with studies done in Ethiopia (74), Pakistan (75), Vietnam (76), and Finland (77). This might be because primigravida women do not have any previous delivery experience, may have uncertainty and fear of childbirth, and they don’t have the knowledge and skills to take care of a child, which may heighten the incidence of depression and increase vulnerability to other psychological morbidities. There have been contradictory findings in studies as some have found multiparous women are at increased risk of developing antenatal common mental illnesses (59, 78, 79), while others did not find a strong association between parity and perinatal mental disorder (80, 81).
Another factor associated with antenatal CMD is gestational age. Pregnant women were more likely to experience CMD during the first and third trimester compared to those in their second trimester. Previous longitudinal studies conducted in England (82), China (83), and Lithuania (84) found a similar trend. Thus, the increased prevalence of CMD in the third trimester might be linked with the proximity of giving birth. Additionally, these results might be induced by hormonal changes in the first trimester (85).
Furthermore, in our study, women with past pregnancy complications or abortion had a higher odds of antenatal CMD. This is similar to the findings from various other studies (86–88). This might be because women who had a previous abortion or pregnancy complications may develop different psychosocial problems, worrying about possible complications in the index pregnancy. This may induce fear, uncertainty, worry, and anxiety, further enhancing the risk of depression during the subsequent pregnancies (89, 90).
Consistent with previous studies conducted in Gondar (47) and Debre Markos (74), Ethiopia, pregnant women who did not have ANC follow-up for their current pregnancy were more likely to have CMDs than those who had an ANC visit. The most likely explanation for this association is that antenatal clinic attendance may construct maternal self-esteem and resiliency, increase chance to obtain information about pregnancy preparedness and minimize risk factors, and increase knowledge about complications during pregnancy, including mental illnesses (91, 92).
This study has some limitations that should be kept in mind when interpreting the results. SRQ-20 is a screening but not diagnostic tool. Beside, this report did not evaluate biological determinants of common mental disorders, such as thyroid dysfunction and immunity. Additionally, the study did not differentiate women with new-onset mental disorders from those with a pre-existing conditions. Lastly, since we recruited multiple data collectors, there may be interviewer bias.
Pregnancy is a time of increased susceptibility for the occurrence of common mental disorder. Almost two in every five pregnant women suffered from antenatal CMD in the study area. Currently, using a substance in early and late pregnancy, experiencing intimate partner violence, null parity, having a history of abortion or pregnancy complications, and no ANC follow-up were significantly associated with antenatal CMD. Administration of regular screening programs for maternal mental health conditions in rural, low-income communities, integrating into primary health care settings is imperative to reduce the risk. This study also underscores the importance of routine maternal mental health assessment and intervention when pregnant women present to maternity services. Pregnant women in this setting should be informed that substance use in pregnancy should be avoided or reduced.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC). The patients/participants provided their written informed consent to participate in this study.
All authors contributed to the conception of the study, organized the data collection process, equally contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
This study was funded by the Haramaya University. The funding body has no role in the design of the study and collection, analysis, and interpretation of data, and writing the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Kersa and Haramaya HDSS for providing opportunity and technical support throughout the study. We are grateful to all mothers who participated in this research. We would also like to acknowledge the Haramaya University for funding and facilitating the research, and the data collectors.
ANC, antenatal care; AOR, adjusted odds ratio; ASSIST, Alcohol, Smoking and Substance Involvement Screening Test; CI, confidence interval; CMD, common mental disorder; COR, crude odds ratio; GTP, Growth and Transformation Plan; HDSS, health and demographic surveillance sites; IPV, intimate partner violence; MhGAP, Mental Health Gap Action Program; ODK, open data kit; SDG, sustainable development goals; SRQ-20, Self-Reporting Questionnaire; VIF, variance inflation factor; YLD, years lived with disability.
1. Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. (2019) 21:10. doi: 10.1007/s11920-019-0997-0
2. World Health Organization [WHO]. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization (2017).
3. Goldberg D. A bio-social model for common mental disorders. Acta Psychiatr Scand Suppl. (1994) 385:66–70. doi: 10.1111/j.1600-0447.1994.tb05916.x
4. Kalin NH. The critical relationship between anxiety and depression. Am J Psychiatry. (2020) 177:365–7. doi: 10.1176/appi.ajp.2020.20030305
5. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. (2014) 43:476–93. doi: 10.1093/ije/dyu038
6. Leight KL, Fitelson EM, Weston CA, Wisner KL. Childbirth and mental disorders. Int Rev Psychiatry. (2010) 22:453–71. doi: 10.3109/09540261.2010.514600
7. Shidhaye P, Giri P. Maternal depression: a hidden burden in developing countries. Ann Med Health sci Res. (2014) 4:463–5. doi: 10.4103/2141-9248.139268
8. Howard LM, Piot P, Stein A. No health without perinatal mental health. Lancet. (2014) 384:1723–4. doi: 10.1016/S0140-6736(14)62040-7
9. Marcus SM, Heringhausen JE. Depression in childbearing women: when depression complicates pregnancy. Prim Care. (2009) 36:151–65; ix. doi: 10.1016/j.pop.2008.10.011
10. Govender D, Naidoo S, Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depress Res Treat. (2020) 2020:5364521. doi: 10.1155/2020/5364521
11. Jha S, Salve HR, Goswami K, Sagar R, Kant S. Burden of common mental disorders among pregnant women: a systematic review. Asian J Psychiatr. (2018) 36:46–53. doi: 10.1016/j.ajp.2018.06.020
12. Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. (2016) 3:973–82. doi: 10.1016/S2215-0366(16)30284-X
13. Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Org. (2012) 90:139g–49g. doi: 10.2471/BLT.11.091850
14. Whitton A, Warner R, Appleby L. The pathway to care in post-natal depression: women’s attitudes to post-natal depression and its treatment. Br J Gen Pract. (1996) 46:427–8.
15. Sūdžiūtė K, Murauskienė G, Jarienė K, Jaras A, Minkauskienė M, Adomaitienė V, et al. Pre-existingmental health disorders affect pregnancy and neonatal outcomes: a retrospectivecohort study. BMC Pregnancy Childbirth. (2020) 20:419. doi: 10.1186/s12884-020-03094-5
16. Pagel MD, Smilkstein G, Regen H, Montano D. Psychosocial influences on new born outcomes: a controlled prospective study. Soc Sci Med. (1990) 30:597–604. doi: 10.1016/0277-9536(90)90158-o
17. Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. (2014) 384:1800–19. doi: 10.1016/S0140-6736(14)61277-0
18. Mongan D, Lynch J, Hanna D, Shannon C, Hamilton S, Potter C, et al. Prevalence of self-reported mental disorders in pregnancy and associations with adverse neonatal outcomes: a population-based cross-sectional study. BMC Pregnancy Childbirth. (2019) 19:412. doi: 10.1186/s12884-019-2572-4
19. Woldetsadik AM, Ayele AN, Roba AE, Haile GF, Mubashir K. Prevalence of common mental disorder and associated factors among pregnant women in South-East Ethiopia, 2017: a community based cross-sectional study. Reprod Health. (2019) 16:173. doi: 10.1186/s12978-019-0834-2
20. Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord. (2016) 191:62–77. doi: 10.1016/j.jad.2015.11.014
21. Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. (2004) 291:2581–90. doi: 10.1001/jama.291.21.2581
22. Nakku JE, Okello ES, Kizza D, Honikman S, Ssebunnya J, Ndyanabangi S, et al. Perinatal mental health care in a rural African district, Uganda: a qualitative study of barriers, facilitators and needs. BMC Health Serv Res. (2016) 16:295. doi: 10.1186/s12913-016-1547-7
23. WHO. WHO Guidelines Approved by the Guidelines Review Committee. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP): Version 20. Geneva: World Health Organization (2016).
24. Keynejad RC, Dua T, Barbui C, Thornicroft G. WHO mental health gap action programme (mhGAP) intervention guide: a systematic review of evidence from low and middle-income countries. Evid Based Ment Health. (2018) 21:30–4. doi: 10.1136/eb-2017-102750
25. Funk M. Integrating Mental Health into Primary Care: A Global Perspective. Geneva: World Health Organization (2008).
26. ACOG. ACOG committee opinion No. 757: screening for perinatal depression. Obstet Gynecol. (2018) 132:e208–12. doi: 10.1097/AOG.0000000000002927
27. Yitbarek K, Birhanu Z, Tucho GT, Anand S, Agenagnew L, Ahmed G, et al. Barriers and facilitators for implementing mental health services into the Ethiopian health extension program: a qualitative study. Risk Manag Health Policy. (2021) 14:1199–210. doi: 10.2147/RMHP.S298190
28. Sudhakar M, Woldie M, Yitbarek K, Abamecha F, Tamirat A. Primary care systems profiles and performance (PRIMASYS): Ethiopian case study. Alliance Heal Policy Syst Res. (2017) 18–25.
29. Federal Ministry of Health Ethiopia [FMOH]. Ethiopia-Health-System-Transformation-Plan(HSTP) 2015/16–2019/20. (2015). Available online at: https://www.globalfinancingfacility.org/ethiopia-health-sector-transformation-plan-201516-201920 (accessed July 19, 2021).
30. Tesfaye Y, Agenagnew L, Terefe Tucho G, Anand S, Birhanu Z, Ahmed G, et al. Attitude and help-seeking behavior of the community towards mental health problems. PLoS One. (2020) 15:e0242160. doi: 10.1371/journal.pone.0242160
31. Kerebih H, Abera M, Soboka MJ. Pattern of help seeking behavior for common mental disorders among urban residents in Southwest Ethiopia. Qual Prim Care. (2017) 25:208–16.
32. Gebreegziabher Y, Girma E, Tesfaye M. Help-seeking behavior of Jimma university students with common mental disorders: a cross-sectional study. PLoS One. (2019) 14:e0212657. doi: 10.1371/journal.pone.0212657
33. Federal Democratic Republic of Ethiopia Ministry of Health, Federal Democratic Republic of Ethiopia. National Mental Health Strategy 2012/13–2015/16. (2012). Available online at: https://www.mhinnovation.net/resources/national-mental-health-strategy-ethiopia (accessed July 19, 2021).
34. Ethiopian Public Health Institute [EPHI]. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. (2019). Available online at: https://dhsprogram.com/publications/publication-FR363-DHS-Final-Reports.cfm (accessed July 27, 2021).
35. World Health Organization [WHO]. Maternal Mental Health and Child Health and Development in Low and Middle Income Countries: Report of the Meeting. Geneva: World Health Organization (2008).
36. Mossie TB, Sibhatu AK, Dargie A, Ayele AD. Prevalence of antenatal depressive symptoms and associated factors among pregnant women in Maichew, North Ethiopia: an institution based study. Ethiop J Health Sci. (2017) 27:59–66. doi: 10.4314/ejhs.v27i1.8
37. Reda AA, Moges A, Biadgilign S, Wondmagegn BY. Prevalence and determinants of khat (Catha edulis) chewing among high school students in eastern Ethiopia: a cross-sectional study. PLoS One. (2012) 7:e33946. doi: 10.1371/journal.pone.0033946
38. Gebremichael G, Yihune M, Ajema D, Haftu D, Gedamu G. Perinatal depression and associated factors among mothers in Southern Ethiopia: evidence from Arba Minch Zuria Health and demographic surveillance site. Psychiatry J. (2018) 2018:7930684. doi: 10.1155/2018/7930684
39. Beusenberg M, Orley JH, World Health Organization. A User’s guide to the Self Reporting Questionnaire (SRQ. World Health Organization. (1994). Available online at: https://apps.who.int/iris/handle/10665/61113 (accessed September 23, 2021).
40. Central Statstics Agency ECS, DHS. Ethiopian Demographic and Health Survey. (2017). Available online at: https://dhsprogram.com/publications/publication-fr328-dhs-final-reports.cfm (accessed September 23, 2021).
41. WHO Assist Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. (2002) 97:1183–94. doi: 10.1046/j.1360-0443.2002.00185.x
42. Coll CV, Ewerling F, García-Moreno C, Hellwig F, Barros AJD. Intimate partner violence in 46 low-income and middle-income countries: an appraisal of the most vulnerable groups of women using national health surveys. BMJ Glob Health. (2020) 5:e002208. doi: 10.1136/bmjgh-2019-002208
43. Kaaya S, Mbwambo J, Kilonzo G, Van Den Borne H, Leshabari M, Fawzi MS, et al. Socio-economic and partner relationship factors associated with antenatal depressive morbidity among pregnant women in Dar es Salaam, Tanzania. Tanzan J Health Res. (2010) 12:23–35. doi: 10.4314/thrb.v12i1.56276
44. Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, le Roux I, et al. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health. (2011) 8:9. doi: 10.1186/1742-4755-8-9
45. Niemi M, Falkenberg T, Petzold M, Chuc NT, Patel V. Symptoms of antenatal common mental disorders, preterm birth and low birthweight: a prospective cohort study in a semi-rural district of Vietnam. Trop Med Int Health. (2013) 18:687–95. doi: 10.1111/tmi.12101
46. Medhin G, Hanlon C, Dewey M, Alem A, Tesfaye F, Lakew Z, et al. The effect of maternal common mental disorders on infant undernutrition in Butajira. Ethiopia: the P-MaMiE study. BMC Psychiatry. (2010) 10: 32. doi: 10.1186/1471-244X-10-32
47. Ayele TA, Azale T, Alemu K, Abdissa Z, Mulat H, Fekadu AJ. Prevalence and associated factors of antenatal depression among women attending antenatal care service at Gondar University Hospital, Northwest Ethiopia. PLoS One. (2016) 11:e0155125. doi: 10.1371/journal.pone.0155125
48. Biratu A, Haile DJ. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reprod Health. (2015) 12:1–8. doi: 10.1186/s12978-015-0092-x
49. Faisal-Cury A, Menezes P, Araya R, Zugaib M. Common mental disorders during pregnancy: prevalence and associated factors among low-income women in São Paulo, Brazil: depression and anxiety during pregnancy. Arch Womens Ment Health. (2009) 12:335–43. doi: 10.1007/s00737-009-0081-6
50. Harpham T, Huttly S, De Silva MJ, Abramsky T. Maternal mental health and child nutritional status in four developing countries. J Epidemiol Community Health. (2005) 59:1060–4. doi: 10.1136/jech.2005.039180
51. Cook JL, Green CR, de la Ronde S, Dell CA, Graves L, Ordean A, et al. Epidemiology and effects of substance use in pregnancy. J Obstet Gynaecol Can. (2017) 39:906–15. doi: 10.1016/j.jogc.2017.07.005
52. Wissart J, Parshad O, Kulkarni S. Prevalence of pre- and postpartum depression in Jamaican women. BMC Pregnancy Childbirth. (2005) 5:15. doi: 10.1186/1471-2393-5-15
53. González-Mesa E, Kabukcuoglu K, Blasco M, Körükcü O, Ibrahim N, González-Cazorla A, et al. Comorbid anxiety and depression (CAD) at early stages of the pregnancy. A multicultural cross-sectional study. J Affect Disord. (2020) 270:85–9. doi: 10.1016/j.jad.2020.03.086
54. Verbeek T, Arjadi R, Vendrik JJ, Burger H, Berger MY. Anxiety and depression during pregnancy in Central America: a cross-sectional study among pregnant women in the developing country Nicaragua. BMC psychiatry. (2015) 15:292. doi: 10.1186/s12888-015-0671-y
55. Waqas A, Raza N, Lodhi HW, Muhammad Z, Jamal M, Rehman A. Psychosocial factors of antenatal anxiety and depression in Pakistan: is social support a mediator? PLoS One. (2015) 10:e0116510. doi: 10.1371/journal.pone.0116510
56. Srinivasan N, Murthy S, Singh AK, Upadhyay V, Mohan SK, Joshi A. Assessment of burden of depression during pregnancy among pregnant women residing in rural setting of Chennai. J Clin Diagn Res. (2015) 9:Lc08–12. doi: 10.7860/JCDR/2015/12380.5850
57. Damena T, Mossie A, Tesfaye M. Khat chewing and mental distress: a community based study, in Jimma city, Southwestern Ethiopia. Ethiop J Health Sci. (2011) 21:37–45. doi: 10.4314/ejhs.v21i1.69042
58. Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women: population-based longitudinal study. Br J Psychiatry. (2006) 189:547–55. doi: 10.1192/bjp.bp.106.022558
59. Abuidhail J, Abujilban S. Characteristics of Jordanian depressed pregnant women: a comparison study. J Psychiatr Ment Health Nurs. (2014) 21:573–9. doi: 10.1111/jpm.12125
60. Wagena EJ, van Amelsvoort LG, Kant I, Wouters EF. Chronic bronchitis, cigarette smoking, and the subsequent onset of depression and anxiety: results from a prospective population-based cohort study. Psychosom Med. (2005) 67:656–60. doi: 10.1097/01.psy.0000171197.29484.6b
61. Conway KP, Vullo GC, Nichter B, Wang J, Compton WM, Iannotti RJ, et al. Prevalence and patterns of polysubstance use in a nationally representative sample of 10th graders in the United States. J Adolesc Health. (2013) 52:716–23. doi: 10.1016/j.jadohealth.2012.12.006
62. Morley KI, Lynskey MT, Moran P, Borschmann R, Winstock AR. Review a. Polysubstance use, mental health and high−risk behaviours: results from the 2012 Global Drug Survey. Drug Alcohol Rev. (2015) 34:427–37. doi: 10.1111/dar.12263
63. Pastor V, Antonelli MC, Pallarés ME. Unravelling the link between prenatal stress, dopamine and substance use disorder. Neurotox Res. (2017) 31:169–86. doi: 10.1007/s12640-016-9674-9
64. Mekuriaw B, Belayneh Z, Yitayih Y. Magnitude of Khat use and associated factors among women attending antenatal care in Gedeo zone health centers, southern Ethiopia: a facility based cross sectional study. BMC Public Health. (2020) 20:110. doi: 10.1186/s12889-019-8026-0
65. Hanlon C, Medhin G, Alem A, Tesfaye F, Lakew Z, Worku B, et al. Impact of antenatal common mental disorders upon perinatal outcomes in Ethiopia: the P-MaMiE population-based cohort study. Trop Med Int Health. (2009) 14:156–66. doi: 10.1111/j.1365-3156.2008.02198.x
66. Mahenge B, Likindikoki S, Stöckl H, Mbwambo J. Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in T anzania: a cross-sectional study. BJOG. (2013) 120:940–7. doi: 10.1111/1471-0528.12185
67. Fisher J, Tran TD, Biggs B, Dang TH, Nguyen TT, Tran T. Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. Int Health. (2013) 5:29–37. doi: 10.1093/inthealth/ihs012
68. Martin SL, Li Y, Casanueva C, Harris-Britt A, Kupper LL, Cloutier S. Intimate partner violence and women’s depression before and during pregnancy. Violence against women. (2006) 12:221–39. doi: 10.1177/1077801205285106
69. Osório C, Probert T, Jones E, Young AH, Robbins I. Adapting to stress: understanding the neurobiology of resilience. Behav Med. (2017) 43:307–22. doi: 10.1080/08964289.2016.1170661
70. Heim C, Nemeroff CB. Neurobiology of posttraumatic stress disorder. CNS Spectr. (2009) 14(1 Suppl. 1):13–24.
71. Kim J, Lee J. Prospective study on the reciprocal relationship between intimate partner violence and depression among women in Korea. Soc Sci Med. (1982) 2013:42–8. doi: 10.1016/j.socscimed.2013.10.014
72. Lehrer JA, Buka S, Gortmaker S, Shrier LA. Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Arch Pediatr Adolesc Med. (2006) 160:270–6. doi: 10.1001/archpedi.160.3.270
73. Dutton MA. Pathways linking intimate partner violence and posttraumatic disorder. Trauma Violence Abuse. (2009) 10:211–24. doi: 10.1177/1524838009334451
74. Belete AH, Assega MA, Abajobir AA, Belay YA, Tariku MK. Prevalence of antenatal depression and associated factors among pregnant women in Aneded woreda, North West Ethiopia: a community based cross-sectional study. BMC Res Notes. (2019) 12:713. doi: 10.1186/s13104-019-4717-y
75. Ali NS, Azam IS, Ali BS, Tabbusum G, Moin SS. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-based cross-sectional study. ScientificWorldJournal. (2012) 2012:653098. doi: 10.1100/2012/653098
76. Fisher J, Tran T, Duc Tran T, Dwyer T, Nguyen T, Casey GJ, et al. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in Vietnamese women: a prospective population-based study. J Affect Disord. (2013) 146:213–9. doi: 10.1016/j.jad.2012.09.007
77. Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Risk factors for and perinatal outcomes of major depression during pregnancy: a population-based analysis during 2002-2010 in Finland. BMJ Open. (2014) 4:e004883. doi: 10.1136/bmjopen-2014-004883
78. Redshaw M, Henderson J. From antenatal to postnatal depression: associated factors and mitigating influences. J Womens Health. (2013) 22:518–25. doi: 10.1089/jwh.2012.4152
79. Yanikkerem E, Ay S, Mutlu S, Goker A. Antenatal depression: prevalence and risk factors in a hospital based Turkish sample. J Pak Med Assoc. (2013) 63:472–7.
80. Abujilban SK, Abuidhail J, Al-Modallal H, Hamaideh S, Mosemli O. Predictors of antenatal depression among Jordanian pregnant women in their third trimester. Health Care Women Int. (2014) 35:200–15. doi: 10.1080/07399332.2013.817411
81. Dibaba Y, Fantahun M, Hindin MJ. The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregnancy Childbirth. (2013) 13:135. doi: 10.1186/1471-2393-13-135
82. Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. (2001) 323:257–60. doi: 10.1136/bmj.323.7307.257
83. Lee AM, Lam SK, Lau SMSM, Chong CSY, Chui HW, Fong DY, et al. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. (2007) 110:1102–12. doi: 10.1097/01.AOG.0000287065.59491.70
84. Bunevicius R, Kusminskas L, Bunevicius A, Nadisauskiene RJ, Jureniene K, Pop VJ. Psychosocial risk factors for depression during pregnancy. Acta Obstet Gynecol Scand. (2009) 88:599–605. doi: 10.1080/00016340902846049
85. Yan H, Ding Y, Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front Psychol. (2020) 11:617001. doi: 10.3389/fpsyg.2020.617001
86. Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. (2013) 22:37. doi: 10.4103/0972-6748.123615
87. Stewart RC, Umar E, Tomenson B, Creed F. A cross-sectional study of antenatal depression and associated factors in Malawi. Arch Womens Ment Health. (2014) 17:145–54. doi: 10.1007/s00737-013-0387-2
88. Weobong B, Soremekun S, Ten Asbroek AH, Amenga-Etego S, Danso S, Owusu-Agyei S, et al. Prevalence and determinants of antenatal depression among pregnant women in a predominantly rural population in Ghana: the DON population-based study. J Affect Disord. (2014) 165:1–7. doi: 10.1016/j.jad.2014.04.009
89. Duko B, Ayano G, Bedaso A. Depression among pregnant women and associated factors in Hawassa city, Ethiopia: an institution-based cross-sectional study. Reprod Health. (2019) 16:1–6. doi: 10.1186/s12978-019-0685-x
90. Tesfaye Y, Agenagnew L. Antenatal depression and associated factors among Pregnant women attending antenatal care service in Kochi Health Center, Jimma town, Ethiopia. J pregnancy. (2021) 2021:5047432. doi: 10.1155/2021/5047432
91. Dadras O, Nakayama T, Kihara M, Ono-Kihara M, Seyedalinaghi S, Dadras F. The prevalence and associated factors of adverse pregnancy outcomes among Afghan women in Iran; Findings from community-based survey. PLoS One. (2021) 16:e0245007. doi: 10.1371/journal.pone.0245007
92. Tendean AF, Dewi A, Wirasto A. The implementation of antenatal care with telehealth towards pregnant women’s mental health. (2021) 10:103–18. Availavble online at: https://journal.umy.ac.id/index.php/mrs/article/view/11399 (accessed October 16, 2021).
Keywords: common mental disorder, pregnancy, antenatal care, gestational age, rural Ethiopia
Citation: Tamiru D, Misgana T, Tariku M, Tesfaye D, Alemu D, Weldesenbet AB, Gebremichael B and Dheresa M (2022) Prevalence and Associated Factors of Common Mental Disorders Among Pregnant Mothers in Rural Eastern Ethiopia. Front. Psychiatry 13:843984. doi: 10.3389/fpsyt.2022.843984
Received: 27 December 2021; Accepted: 01 March 2022;
Published: 28 March 2022.
Edited by:
Suraj Bahadur Thapa, University of Oslo, NorwayReviewed by:
Eero Kajantie, National Institute for Health and Welfare, FinlandCopyright © 2022 Tamiru, Misgana, Tariku, Tesfaye, Alemu, Weldesenbet, Gebremichael and Dheresa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dawit Tamiru, ZGF3aXR0YW1ydTVAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.