- 1Department of Medical Psychology and Medical Sociology, Ruhr University Bochum, Bochum, Germany
- 2Mental Health Research and Treatment Center, Department of Psychology, Ruhr-University Bochum, Bochum, Germany
- 3Department of Neurology and Center for Translational Neuro- and Behavioral Sciences, University Hospital Essen, Essen, Germany
Avoidance behaviors are shaped by associative learning processes in response to fear of impending threats, particularly physical harm. As part of a defensive repertoire, avoidance is highly adaptive in case of acute danger, serving a potent protective function. However, persistent or excessive fear and maladaptive avoidance are considered key factors in the etiology and pathophysiology of anxiety- and stress-related psychosomatic disorders. In these overlapping conditions, avoidance can increase the risk of mental comorbidities and interfere with the efficacy of cognitive behavioral treatment approaches built on fear extinction. Despite resurging interest in avoidance research also in the context of psychosomatic medicine, especially in conditions associated with pain, disturbed interoception, and disorders of the gut-brain axis, current study designs and their translation into the clinical context face significant challenges limiting both, the investigation of mechanisms involved in avoidance and the development of novel targeted treatment options. We herein selectively review the conceptual framework of learning and memory processes, emphasizing how classical and operant conditioning, fear extinction, and return of fear shape avoidance behaviors. We further discuss pathological avoidance and safety behaviors as hallmark features in psychosomatic diseases, with a focus on anxiety- and stress-related disorders. Aiming to emphasize chances of improved translational knowledge across clinical conditions, we further point out limitations in current experimental avoidance research. Based on these considerations, we propose means to improve existing avoidance paradigms to broaden our understanding of underlying mechanisms, moderators and mediators of avoidance, and to inspire tailored treatments for patients suffering from psychosomatic disorders.
Introduction
Learning to flexibly respond to dynamic environmental challenges constitutes a highly adaptive mechanism aimed at self-protection, particularly when faced with impending physical harm (1). One of the most defensive, yet in case of acute threat particularly protective responses is avoidance behavior (2). Based on the influential fear avoidance model (FAM) (3, 4), which has initially provided a theoretical framework for the pathology of fear, avoidance behavior involves a cascade of fear-related responses shaped by associative learning, particularly classical and operant conditioning. While beneficial during phases of acute danger, when threats cease but fear and its consequences persist, avoidance or safety behaviors lose their adaptive function and the formerly protective cascade becomes maladaptive. This can initiate a vicious circle of fear and distress, potentially culminating in the development and persistence of disease (5, 6).
More recently, the FAM has been extended to conceptualize the key role of fear in chronic pain (7–10) and disturbances of the gut-brain axis (11) as highly common psychosomatic disorders (12–14) presenting with eminent comorbidity rates with anxiety disorders (15). Evidence from experimental research in these fields supports the assumptions of the FAM, showing that pain-related fear and avoidance are associated with dysfunctional cognitive, behavioral, and affective responses, including negative appraisal, catastrophizing, and hypervigilance (16–20). These factors promote the maintenance and exacerbation of symptoms and contribute to comorbid psychiatric disorders, increased distress, functional disability, social withdrawal, and reduced quality of life (21–24).
Avoidance has highly relevant treatment implications, providing a foundation for therapeutic interventions following associative learning principles (25–27), particularly exposure-based treatments based on fear extinction within the framework of cognitive behavioral therapy (CBT) (28–30). The main aim of exposure is to help patients to confront themselves to cues and contexts they fear and avoid, and to endure their fears and corresponding behavioral, emotional, and cognitive responses (31). Systematic exposure demonstrably reduces anxiety-relevant symptoms and improves functional abilities (30–33). According to recent findings, extinction effects are initiated by a violation of the patients' dysfunctional expectancies (34, 35). Therefore, during exposure, patients are often encouraged to refrain from engaging in avoidance and safety behaviors, providing an opportunity to experience fear-correcting situations (36–38).
Despite this outstanding relevance in the transition from acute threat to chronic disease, persistence of symptoms, and therapeutic interventions, for a long time avoidance has not received the attention owed in experimental research (39), particularly in the context of psychosomatic medicine. Attempts to investigate avoidance in experimental pain research have more recently been made (40, 41), and avoidance and safety behaviors have been identified as crucial mechanisms of action in CBT for patients suffering from disorders of gut-brain interaction (42, 43). However, experimental approaches often fall short with respect to validity criteria and do not adequately translate into clinical contexts (27, 44–47), and systematic empirical investigations in psychosomatic disorders are still widely lacking.
We herein selectively highlight experimental considerations and clinical implications of avoidance behaviors in the context of psychosomatic disorders with a particular focus on frequently co-occurring pain conditions, disorders of the gut-brain axis, and anxiety disorders (48). We discuss chances but also methodological and conceptual challenges in establishing clinically-relevant experimental models to elucidate avoidance behaviors, underlying mechanisms, and their role in long-term effects of CBT for anxiety and psychosomatic disorders.
A Conceptual Framework of Learning and Extinction
Avoidance is embedded within a conceptual framework of associative learning governed by principles of classical and operant conditioning. Fear conditioning provides an excellent model for investigating the development and maintenance of a wide range of pathologies, including but not limited to anxiety and pain (47, 49–51).
Classical fear conditioning (Figure 1A) occurs through learning about the association between a neutral stimulus and an aversive event, e.g., a symptom, the unconditioned stimulus (US), which inherently elicits a defensive response (unconditioned response; UR), such as fear. Once established, this association renders the initially neutral stimulus a conditioned stimulus (CS), which now has acquired emotional value itself and is capable to trigger a response resembling the UR, the conditioned response (CR) (52, 53). According to the FAM, conditioned fear promotes multifaceted cognitive, emotional, and behavioral responses, including protective safety and avoidance behaviors. Avoidance and its short-term consequences, however, can initiate a second crucial learning process assumed to contribute to the transition from adaptive behavior to pathology, namely operant conditioning (54).
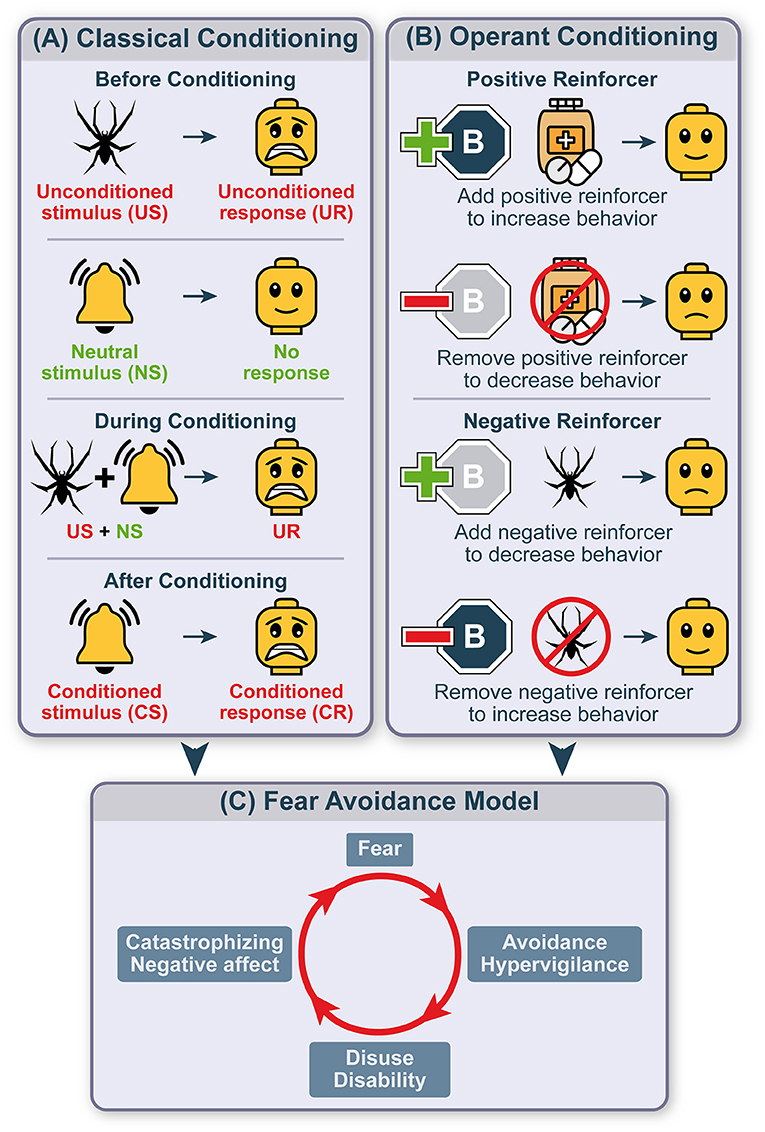
Figure 1. Avoidance within the conceptual framework of learning theory. Schematic depiction of avoidance embedded within the conceptual framework of classical conditioning initiating a fear response and mechanisms of operant conditioning fueling avoidance and maintaining maladaptive behaviors. Classical conditioning (A) refers to learning of an association between two stimuli. The unconditioned stimulus (US) naturally and automatically evokes an unconditioned response (UR) while neutral stimuli (NS) usually evoke no response. When associating the unconditioned with the neutral stimulus, the individual will display the unconditioned response. This association will turn the neutral into a conditioned stimulus (CS) evoking a conditioned response (CR). After a CS-US relationship is established, the behavior of an individual will be adapted based on its consequences. This operant conditioning (B) is formed by adding or removing a reinforcing stimulus that increases or decreases the probability of a specific behavior to occur in the future. A positive reinforcer increases the probability to show a certain behavior while its withdrawal discourages it. Adding a negative reinforcer decreases behavior while removing the negative reinforcer encourages the behavior to be displayed. These two processes combine to form a vicious circle of fear avoidance (C). Upon the encounter of a fear-relevant stimulus, a vicious circle of fear avoidance is initiated by increasing attentional resources to potential sources of threat (hypervigilance), disuse and disability and exaggerating negative thoughts and affect (catastrophizing), thereby preventing the encounter with the feared stimulus and corrective measures.
Operant conditioning or instrumental learning involves positive and negative reinforcers impacting the probability to execute behaviors based on their previous consequences (Figure 1B) (55–57). The presence of a positive reinforcer motivates the maintenance of a shown behavior, its absence, or removal reduces the probability to show this behavior in the future. Reversely, the occurrence of a negative reinforcer punishes performed behavior, resulting in its reduction. Finally, if a negative reinforcer is removed following a certain behavior, the behavioral strategy is strengthened. This last mechanism is considered key for the development and persistence of avoidance behaviors. Specifically, avoidance can instantly provide relief from states of fear, stress, and negative affect as significant negative reinforcers, and is thereby retained and even increasingly used as a behavioral response (46). Avoidance can be further used as a source of information, asserting that if avoidance was beneficial and relieving there must have been danger, and may thereby feed the original fear. Consequently, fear may prevail, resulting in the perpetuation of maladaptive avoidance, increased attention to threatening stimuli (hypervigilance), disuse and disability, catastrophizing, and negative affectivity (Figure 1C).
This two-stage theory of classical and operant conditioning, despite conceptual criticism (6), has been applied to panic disorder (58, 59), post-traumatic stress disorder (37, 60–62), phobias (63–65), social anxiety (66, 67), and chronic pain (68, 69). Common to all these conditions, sustained maladaptive avoidance behaviors prevent the individual from experiencing corrective situations that could rededicate a feared stimulus, such as a bodily symptom, as non-threatening, and can thus hamper fear extinction.
Extinction learning allows the formation of a new memory trace that inhibits the expression of previously acquired CS-US associations (70, 71). Exposure therapy follows the basic principles of extinction to support the development of new adaptive emotional, cognitive, and behavioral responses (28, 30). Importantly, extinguished threat responses may return under certain circumstances, such as with mere passage of time (“spontaneous recovery”), a context change (“renewal effect”), or an unexpected confrontation with the US (“reinstatement”). These return of fear phenomena may underlie relapse, posing major challenges to CBT (72, 73). As safety and avoidance behaviors during exposure therapy might compromise extinction learning (74) and can persist following experimental extinction training (75), they could also increase the risk of return of fear after successful exposure-based treatments (76).
It is therefore crucial to advance our understanding of avoidance behaviors, their underlying mechanisms, and their role in extinction-based treatments to both refine theoretical models and optimize therapeutic interventions for anxiety and psychosomatic disorders.
Clinical Implications of Avoidance in Psychosomatic Medicine
The principles of learning theory and the key role of avoidance are increasingly recognized within biopsychosocial disease models and have been successfully translated into extinction-based interventions in various psychiatric and psychosomatic conditions. Inspired by their wide application in anxiety disorders (30, 32, 36, 77), exposure therapy has been established as an integral part of multimodal interventions for disorders characterized by disturbed interoception (78), including chronic pain (38, 54, 79, 80), disorders of the gut-brain axis, particularly irritable bowel syndrome (IBS) (48, 81–84), but also for body image disturbances and eating disorders (85–88), substance abuse and addiction (89–91).
Evidence supports the association between elevated levels of avoidance and pathology in these conditions (27, 41, 48, 78, 82), rendering avoidance a cardinal symptom and major target of CBT. In contrast to experimental settings, avoidance and safety behaviors in clinical populations are much more complex and highly patient- and disease-specific, ranging from refraining to enter a basement in spider phobia over lifting a suitcase only with severe tension in chronic low back pain to avoiding food consumption before a train ride in IBS. Therefore, it is crucial to individually tailor exposure therapy, which is often graded according to the patient's own threat hierarchy (48, 82).
From a clinical perspective, it is important to distinguish avoidance from safety behaviors and to adapt respective therapeutic approaches (2, 46, 92, 93). Safety behavior describes the endurance of a threat only when strategies aiming to prevent harm are simultaneously executed, such as calming self-talk, while avoidance aims at preventing the occurrence of the threatening stimulus itself, e.g., abstaining from feared situations, and eliminating a confrontation altogether. Accordingly, if avoidance is the disorder's maintaining factor, patients are encouraged to confront themselves with and approach the feared stimulus, optimally in different contexts to foster extinction generalization. To reduce safety behaviors, however, therapy should rather focus on the patient's strategies when being confronted with the feared object or situation.
In this manner, exposure therapy can demonstrably directly target maladaptive avoidance and safety behaviors in anxiety- and stress-related psychosomatic disorders (29, 40, 48, 82, 94, 95), which maintain symptom-related anxiety and contribute to symptom severity. Meanwhile, it is a matter of current debate whether adaptive and maladaptive use of avoidance behaviors should be dissociated, which may impact upon treatment outcome (96, 97). Specifically, avoidance behavior is often discouraged during exposure as it is considered to prevent a violation of dysfunctional expectancies (34, 35), thereby interfering with fear reduction and consequently maintaining symptoms or resulting in a return of fear (98). However, accumulating evidence suggests that avoidance does not necessarily hamper exposure therapy (99–101), may even facilitate its efficacy (102–104), and can enhance treatment acceptability and tolerability (105, 106). Therefore, understanding the process dynamics and considering adaptive characteristics of avoidance and safety behaviors appears crucial, as it may help to understand interindividual differences in risk of relapse.
Challenges in Experimental Research on Avoidance
Despite the crucial impact of avoidance and safety behaviors in the development and maintenance of symptoms and the efficacy of therapeutic approaches, avoidance has long been widely neglected in experimental research (39), particularly in psychosomatic disorders. Recent advances have sparked renewed interest in the behavioral, neuroscientific, and clinical aspects of avoidance (2, 107, 108). However, several novel approaches have provoked criticism regarding validity criteria and translation into clinical reality (27, 44–47).
Commonly utilized experimental models often do not sufficiently represent the complex and nuanced dimensions of avoidance behaviors and their underlying learning processes in clinical populations. Emerging research has started to tackle this challenge with multifaceted translational approaches. Innovative examples range from the implementation of clinically-relevant, interoceptive visceral pain during associative learning (20, 109–111), over the use of immersive and interactive exposure techniques through virtual reality in phobias, anxiety disorders, and PTSD (112, 113), to a variation of the effort required to avoid movements using a robotic arm to address pain-related avoidance (114–116).
Likewise, a major pitfall in experimental avoidance research in humans is its operationalization as a dichotomous rather than continuous variable. In contrast to animal studies allowing a comprehensive evaluation of avoidance from subtle to excessive behaviors (117, 118), this complex phenomenon is often reduced to simple button presses indicating an evaluative decision to avoid or not to avoid an imminent outcome in human research (46). Attempts to overcome this lack of face validity have been made by including behavioral measures such as eye (119) and motion tracking (120) or by implementing a gradual admission of aversive outcomes (121).
Avoidance and safety behaviors can instantly relieve fear and distress and prevent the experience of an expected threat. As such, they serve as short-term rewards, motivating future performance. However, in pathology, excessive avoidance often results in a loss of long-term rewarding experiences, such as the engagement in social interactions, physical, or recreative activities. These avoidance costs contributing to deficits in quality of life are widely ignored in experimental research (118). One reason is likely the challenge to operationalize clinically-relevant costs in experimental settings. Avoidance costs, if considered, often involve instant monetary gains and losses (122–125). These approaches show low phenomenological validity, as they do not relate to the disease under investigation, cannot capture long-term costs of avoidance, and do not take interindividual variability in the value of costs into account. Innovative novel approaches, however, have been promising to address some of these concerns, incorporating the effort the individual is willing to put into avoiding an aversive US or targeting the relevance of avoidance costs in experimental approaches (114, 115, 126).
An even broader challenge is to index avoidance behaviors in both experimental and clinical settings alike. A patient with interoceptive visceral pain may perform a feared activity—yet does this with massive tension and hypervigilance, which can be difficult to identify and quantify as maladaptive behavior. There are various questionnaires and Behavioral Approach Tests (BATs) to quantify avoidance in clinical research and to evaluate the progress of behavioral treatments. However, several methodological weaknesses limit the psychometric and clinical utilization of these assessments (127), as they may partly depend on the instructions used and are prone to demand effects (128, 129). Likewise, available questionnaires in the context of chronic pain were often developed prior to the conceptual FAM and therefore lack construct validity, relevant cut-off scores, and responsiveness to treatment progress (130, 131).
Finally, avoidance is an instinctive survival behavior in response to environmental threats (132). Translating this evolutionarily hardwired protective response driven by severe fear of harm into experimental settings in human research has tight ethical boundaries. Most studies rely on instructed avoidance behavior and likely fail to capture the core mechanisms underlying avoidance as overt behavior (75, 133, 134). To target this issue, pain research addressed costly pain-related fear and avoidance more directly by implementing operant learning paradigms (115, 135, 136), documenting that sustained avoidance behavior is continued despite being no longer adaptive, and can even increase fear and pain sensitivity (137). It further underscores a key role of threat-related uncertainty, which has recently been identified as a putative vulnerability factor for maladaptive avoidance behavior (138), and may constitute a promising target for behavioral treatments in psychosomatic disorders (115).
From theoretical and clinical perspectives alike, expanding research on avoidance behavior is of key relevance to further elucidate the mechanisms and clinical implications of classical and operant learning, extinction, and the return of fear in psychosomatic disorders.
Chances and Future Directions
To advance future research, it is crucial to validly address dysfunctional avoidance behavior and to foster a reciprocal translation between basic and clinical research through clinically-relevant experimental models. These should integrate behavioral approaches based on associative learning with cognitive theories of avoidance beliefs and schemas (139, 140). Not least in light of a need for individually-tailored CBT in anxiety- and stress-related disorders, it is key to acknowledge interindividual variability in aversive learning and memory, warranting more insight into putative moderating and mediating factors, and approaching predictions of specific avoidance patterns (6, 141).
For example, sex differences play an important role with women being more likely to engage in avoidance behaviors than men following traumatic events (142), in agoraphobia (143, 144), and in healthy individuals encountering panic-relevant (145) and phobic situations (146). Likewise, healthy women demonstrate longer avoidance duration and continue avoidant behavior during extinction (147), well in line with clinical data showing a higher female prevalence for anxiety disorders (148, 149), chronic pain (150), and IBS (151). Further, individual personality traits seem to influence the propensity to display maladaptive avoidance behavior. For example, evidence supports a relationship between intolerance of uncertainty, as well as neuroticism and avoidance (138, 152), being linked to higher fear avoidance both in healthy volunteers (153) and in clinical populations (154).
Experimental research further suggests that competing goals and goal prioritization in favor of reward seeking rather than threat avoidance attenuates the tendency to engage in avoidance behaviors (124, 155). Psychosomatic disorders are characterized by approach-avoidance conflicts following a continuum between the subjectively perceived threat and associated costs (156). While particularly anxious individuals tend to avoid a feared stimulus, associating the feared stimulus with higher rewards or avoidance costs may foster approach motivation (157) and promote fear extinction (158). Before a therapeutic intervention can be successful, it therefore appears crucial to evaluate and systematically implement what is rewarding to the individual to terminate dysfunctional and motivate more functional behaviors and non-avoidant decisions, which are demonstrably associated with less avoidance behavior post-treatment (123, 159).
Following theoretical accounts of learning, avoidance behaviors acquire inhibitory properties and are therefore presumed to interfere with fear extinction (76). Besides the need for further empirical testing of these assumptions (41, 160), it appears promising to target the extinction of maladaptive avoidance behaviors in CBT independent of the conditioned fear association (33, 161), particularly in patients who show excessive avoidance and those at risk to discontinue treatment. First experimental studies demonstrate that the extinction of avoidance behavior is facilitated by reducing the partial reinforcement rate of avoidance (133) and by increasing the effort (114, 158) or costs of an avoidance response (75, 162). These approaches may reduce the likelihood to express maladaptive avoidance behavior during exposure, paving the way for the successful extinction of conditioned threat associations.
Finally, approaches in experimental and clinical research alike should aim at bridging the gap between models applied in laboratory settings and patients' clinical reality and to more closely integrate the concepts of the FAM into the broad field of psychosomatic medicine. To achieve this goal, clinically-relevant and phenomenologically valid models are needed, capturing different facets as well as the specificity of fear and avoidance in psychosomatic disease, as first innovative attempts in the fields of muscoskeletal (115, 135–137, 163) and interoceptive visceral pain (20, 110, 111, 164, 165) have previously demonstrated. These experimental settings provide an ideal opportunity to overcome some common limitations of avoidance research, and to operationalize and assess the complex phenomenon of avoidance in its multiple facets, incorporating behavioral, cognitive, but also neural levels (39). Rather than artificial losses, clinically-relevant avoidance costs appear promising here, such as the previously implemented increased efforts to achieve a goal (135, 158) or a loss of predictability, which increases fear and uncertainty and can demonstrably affect pain-related fear and interoceptive pain experiences (111, 164, 166).
Albeit selective, this brief overview highlights key factors of relevance in experimental and clinical avoidance research in the context of anxiety- and stress-related disease. Future work in the field could, inspired and governed by associative learning principles, help shed light on mechanisms underlying different facets of adaptive and maladaptive avoidance as “the good, the bad, and the ugly” in pathology and therapy and pave the way toward refined tailored treatments for patients with psychosomatic disorders.
Author Contributions
MW, SE, and AI acquired funding. FL, AI, and MW wrote the manuscript with input from all authors. SE made significant contributions to all parts of the manuscript. All authors approved the final version of the manuscript.
Funding
This work was funded by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG), SFB 1280 Extinction Learning (316803389—Projects A10, A12, and A13).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Öhman A, Mineka S. Fears, phobias, and preparedness : toward an evolved module of fear and fear learning. Psychol Rev. (2001) 108:483–522. doi: 10.1037/0033-295X.108.3.483
2. Le Doux J, Daw ND. Surviving threats: neural circuit and computational implications of a new taxonomy of defensive behaviour. Nat Rev Neurosci. (2018) 19:269–82. doi: 10.1038/nrn.2018.22
3. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. (2000) 85:317–32. doi: 10.1016/S0304-3959(99)00242-0
4. Lethem J, Slade PD, Troup JD, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception–I. Behav Res Ther. (1983) 21:401–8. doi: 10.1016/0005-7967(83)90009-8
5. Crombez G, Eccleston C, Van Damme S, Vlaeyen JWS, Karoly P. Fear-avoidance model of chronic pain. Clin J Pain. (2012) 28:475–83. doi: 10.1097/AJP.0b013e3182385392
6. Krypotos A-M, Effting M, Kindt M, Beckers T. Avoidance learning: a review of theoretical models and recent developments. Front Behav Neurosci. (2015) 9:189. doi: 10.3389/fnbeh.2015.00189
7. Vlaeyen JWS, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. (2016) 157:1588–9. doi: 10.1097/j.pain.0000000000000574
8. Leeuw M, Goossens MEJB, Linton SJ, Crombez G, Boersma K, Vlaeyen JWS. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. (2007) 30:77–94. doi: 10.1007/s10865-006-9085-0
9. Vangronsveld K, Peters M, Goossens M, Linton S, Vlaeyen J. Applying the fear-avoidance model to the chronic whiplash syndrome. Pain. (2007) 131:258–61. doi: 10.1016/j.pain.2007.04.015
10. Alappattu MJ, Bishop MD. Psychological factors in chronic pelvic pain in women: relevance and application of the fear-avoidance model of pain. Phys Ther. (2011) 91:1542–50. doi: 10.2522/ptj.20100368
11. Elsenbruch S, Benson S, Koenen LR, Labrenz F, Icenhour A. From gut feelings to memories of visceral pain. Neuroforum. (2020) 26:171–7. doi: 10.1515/nf-2020-0016
12. Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain. (2008) 9:883–91. doi: 10.1016/j.jpain.2008.05.005
13. Katz J, Rosenbloom BN, Fashler S. Chronic pain, psychopathology, and DSM-5 somatic symptom disorder. Can J Psychiatry. (2015) 60:160–7. doi: 10.1177/070674371506000402
14. Dersh J, Polatin PB, Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med. (2002) 64:773–86. doi: 10.1097/00006842-200209000-00010
15. Fond G, Loundou A, Hamdani N, Boukouaci W, Dargel A, Oliveira J, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. (2014) 264:651–60. doi: 10.1007/s00406-014-0502-z
16. Lee JE, Kim SH, Shin SK, Wachholtz A, Lee JH. Attentional engagement for pain-related information among individuals with chronic pain: the role of pain catastrophizing. Pain Res Manag. (2018) 2018:6038406. doi: 10.1155/2018/6038406
17. van Vliet CM, Meulders A, Vancleef LMG, Vlaeyen JWS. The opportunity to avoid pain may paradoxically increase fear. J Pain. (2018) 19:1222–30. doi: 10.1016/j.jpain.2018.05.003
18. Labrenz F, Knuf-Rtveliashvili S, Elsenbruch S. Sex differences linking pain-related fear and interoceptive hypervigilance: attentional biases to conditioned threat and safety signals in a visceral pain model. Front Psychiatry. (2020) 11:197. doi: 10.3389/fpsyt.2020.00197
19. Elsenbruch S, Wolf OT. Could stress contribute to pain-related fear in chronic pain? Front Behav Neurosci. (2015) 9:340. doi: 10.3389/fnbeh.2015.00340
20. Icenhour A, Petrakova L, Hazzan N, Theysohn N, Merz CJ, Elsenbruch S. When gut feelings teach the brain to fear pain: context-dependent activation of the central fear network in a novel interoceptive conditioning paradigm. Neuroimage. (2021) 238:118229. doi: 10.1016/j.neuroimage.2021.118229
21. Pincus T, Morley S. Cognitive-processing bias in chronic pain: a review and integration. Psychol Bull. (2001) 127:599–617. doi: 10.1037/0033-2909.127.5.599
22. van Ryckeghem DML, Noel M, Sharpe L, Pincus T, Van Damme S. Cognitive biases in pain : an integrated functional – contextual framework. Pain. (2019) 160:1489–93. doi: 10.1097/j.pain.0000000000001508
23. Elsenbruch S. Abdominal pain in Irritable Bowel Syndrome: a review of putative psychological, neural and neuro-immune mechanisms. Brain Behav Immun. (2011) 25:386–94. doi: 10.1016/j.bbi.2010.11.010
24. Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. (2007) 133:581–624. doi: 10.1037/0033-2909.133.4.581
25. Hooten WM. Chronic pain and mental health disorders: shared neural mechanisms, epidemiology, and treatment. Mayo Clin Proc. (2016) 91:955–70. doi: 10.1016/j.mayocp.2016.04.029
26. Treanor M, Barry TJ. Treatment of avoidance behavior as an adjunct to exposure therapy: insights from modern learning theory. Behav Res Ther. (2017) 96:30–6. doi: 10.1016/j.brat.2017.04.009
27. Pittig A, Treanor M, LeBeau RT, Craske MG. The role of associative fear and avoidance learning in anxiety disorders: gaps and directions for future research. Neurosci Biobehav Rev. (2018) 88:117–40. doi: 10.1016/j.neubiorev.2018.03.015
28. Paredes D, Morilak DA. A Rodent model of exposure therapy: the use of fear extinction as a therapeutic intervention for PTSD. Front Behav Neurosci. (2019) 13:46. doi: 10.3389/fnbeh.2019.00046
29. Hofmann SG, Hay AC. Rethinking avoidance: toward a balanced approach to avoidance in treating anxiety disorders. J Anxiety Disord. (2018) 55:14–21. doi: 10.1016/j.janxdis.2018.03.004
30. Foa EB, McLean CP. The efficacy of exposure therapy for anxiety-related disorders and its underlying mechanisms: the case of OCD and PTSD. Annu Rev Clin Psychol. (2016) 12:1–28. doi: 10.1146/annurev-clinpsy-021815-093533
31. Craske MG, Hermans D, Vervliet B, Craske MG. State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Philos Trans R Soc Lond B Biol Sci. (2018) 373:20170025. doi: 10.1098/rstb.2017.0025
32. Kaczkurkin AN, Foa EB. Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues Clin Neurosci. (2015) 17:337–46. doi: 10.31887/DCNS.2015.17.3/akaczkurkin
33. Dymond S. Overcoming avoidance in anxiety disorders: the contributions of Pavlovian and operant avoidance extinction methods. Neurosci Biobehav Rev. (2019) 98:61–70. doi: 10.1016/j.neubiorev.2019.01.007
34. Declercq M, De Houwer J, Baeyens F. Evidence for an expectancy-based theory of avoidance behaviour. Q J Exp Psychol. (2008) 61:1803–12. doi: 10.1080/17470210701851214
35. Lovibond P. Fear and Avoidance: an integrated expectancy model. In: Craske M, Hermans D, Vansteenwegen D, editors. Fear and Learning: From Basic Processes to Clinical Implications. Washington, DC: American Psychological Association (2006). p. 117–32. doi: 10.1037/11474-006
36. Pittig A, van den Berg L, Vervliet B. The key role of extinction learning in anxiety disorders: behavioral strategies to enhance exposure-based treatments. Curr Opin Psychiatry. (2016) 29:39–47. doi: 10.1097/YCO.0000000000000220
37. Foa EB, Kozak MJ. emotional processing of fear. Exposure to corrective information. Psychol Bull. (1986) 99:20–35. doi: 10.1037/0033-2909.99.1.20
38. Gatzounis R, den Hollander M, Meulders A. Optimizing long-term outcomes of exposure for chronic primary pain from the lens of learning theory. J Pain. (2021) 22:1315–27. doi: 10.1016/j.jpain.2021.04.012
39. Le Doux JE, Moscarello J, Sears R, Campese V. The birth, death and resurrection of avoidance: a reconceptualization of a troubled paradigm. Mol Psychiatry. (2017) 22:24–36. doi: 10.1038/mp.2016.166
40. Volders S, Boddez Y, De Peuter S, Meulders A, Vlaeyen JWS. Avoidance behavior in chronic pain research: a cold case revisited. Behav Res Ther. (2015) 64:31–7. doi: 10.1016/j.brat.2014.11.003
41. Meulders A. Fear in the context of pain: lessons learned from 100 years of fear conditioning research. Behav Res Ther. (2020) 131:103635. doi: 10.1016/j.brat.2020.103635
42. Ljótsson B. What are the mechanisms of psychological treatments for irritable bowel syndrome? J Psychosom Res. (2019) 118:9–11. doi: 10.1016/j.jpsychores.2019.01.003
43. Hesser H, Hedman-Lagerlöf E, Lindfors P, Andersson E, Ljótsson B. Behavioral avoidance moderates the effect of exposure therapy for irritable bowel syndrome: a secondary analysis of results from a randomized component trial. Behav Res Ther. (2021) 141:103862. doi: 10.1016/j.brat.2021.103862
44. Scheveneels S, Boddez Y, Vervliet B, Hermans D. The validity of laboratory-based treatment research: bridging the gap between fear extinction and exposure treatment. Behav Res Ther. (2016) 86:87–94. doi: 10.1016/j.brat.2016.08.015
45. Cain CK. Avoidance problems reconsidered. Curr Opin Behav Sci. (2019) 26:9–17. doi: 10.1016/j.cobeha.2018.09.002
46. Krypotos AM, Vervliet B, Engelhard IM. The validity of human avoidance paradigms. Behav Res Ther. (2018) 11:99–105. doi: 10.1016/j.brat.2018.10.011
47. Beckers T, Krypotos AM, Boddez Y, Effting M, Kindt M. What's wrong with fear conditioning? Biol Psychol. (2013) 92:90–6. doi: 10.1016/j.biopsycho.2011.12.015
48. Keefer L, Ballou SK, Drossman DA, Ringstrom G, Elsenbruch S, Ljótsson B, et al. Rome working team report on brain-gut behavior therapies for disorders of gut-brain interaction. Gastroenterology. (2022) 162:300–15. doi: 10.1053/j.gastro.2021.09.015
49. Dunsmoor JE, Paz R. Fear generalization and anxiety: behavioral and neural mechanisms. Biol Psychiatry. (2015) 78:336–43. doi: 10.1016/j.biopsych.2015.04.010
50. Mansour AR, Farmer MA, Baliki MN, Apkarian AV. Chronic pain: the role of learning and brain plasticity. Restor Neurol Neurosci. (2014) 32:129–39. doi: 10.3233/RNN-139003
51. Lissek S, van Meurs B. Learning models of PTSD: theoretical accounts and psychobiological evidence. Int J Psychophysiol. (2015) 98:594–605. doi: 10.1016/j.ijpsycho.2014.11.006
53. Watson JB, Rayner R. Conditioned emotional reactions. J Exp Psychol. (1920). 3:1–14. doi: 10.1037/h0069608
54. Vlaeyen JWSS, Crombez G. Behavioral conceptualization and treatment of chronic pain. Annu Rev Clin Psychol. (2020) 16:187–212. doi: 10.1146/annurev-clinpsy-050718-095744
55. Skinner BF. The Behavior of Organisms: An Experimental Analysis. The Behavior of Organisms: An Experimental Analysis. Oxford: Appleton-Century (1938).
56. Skinner B. Operant behavior. In: Honig W, editor. Areas of Research and Application. New York, NY: Appleton-Century-Crofts (1966). p. 12–32.
57. Staddon JER, Cerutti DT. Operant conditioning. Annu Rev Psychol. (2003) 54:115–44. doi: 10.1146/annurev.psych.54.101601.145124
58. Barlow DH, Craske MG, Cerny JA, Klosko JS. Behavioral treatment of panic disorder. Behav Ther. (1989). 20:261–82. doi: 10.1016/S0005-7894(89)80073-5
59. Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychol Rev. (2001) 108:4–32. doi: 10.1037/0033-295X.108.1.4
60. Ousdal OT, Huys QJ, Milde AM, Craven AR, Ersland L, Endestad T, et al. The impact of traumatic stress on Pavlovian biases. Psychol Med. (2018) 48:327–36. doi: 10.1017/S003329171700174X
61. VanElzakker MB, Kathryn Dahlgren M, Caroline Davis F, Dubois S, Shin LM. From Pavlov to PTSD: the extinction of conditioned fear in rodents, humans, and anxiety disorders. Neurobiol Learn Mem. (2014) 113:3–18. doi: 10.1016/j.nlm.2013.11.014
62. Hassija CM, Gray MJ. Behavioral interventions for trauma and posttraumatic stress disorder. Int J Behav Consult Ther. (2007) 3:166–75. doi: 10.1037/h0100797
63. Davey GC. Classical conditioning and the acquisition of human fears and phobias: a review and synthesis of the literature. Adv Behav Res Ther. (1992) 14:29–66. doi: 10.1016/0146-6402(92)90010-L
64. Siddle DA, Bond NW. Avoidance learning, Pavlovian conditioning, and the development of phobias. Biol Psychol. (1988) 27:167–83. doi: 10.1016/0301-0511(88)90048-8
65. Merckelbach H, de Jong PJ, Muris P, van Den Hout MA. The etiology of specific phobias: a review. Clin Psychol Rev. (1996) 16:337–61. doi: 10.1016/0272-7358(96)00014-1
66. Abraham A, Hermann C. Biases in probabilistic category learning in relation to social anxiety. Front Psychol. (2015) 6:1218. doi: 10.3389/fpsyg.2015.01218
67. Stevens S, Peters A, Abraham A, Hermann C. Enhanced avoidance behavior in social anxiety: evidence from a probabilistic learning task. J Behav Ther Exp Psychiatry. (2014) 45:39–45. doi: 10.1016/j.jbtep.2013.07.007
68. Cordier L, Diers M. Learning and unlearning of pain. Biomedicines. (2018) 6:67. doi: 10.3390/biomedicines6020067
69. Flor H, Knost B, Birbaumer N. The role of operant conditioning in chronic pain: an experimental investigation. Pain. (2002) 95:111–8. doi: 10.1016/S0304-3959(01)00385-2
70. Bouton ME. Context and behavioral processes in extinction. Learn Mem. (2004) 11:485–94. doi: 10.1101/lm.78804
71. Bouton ME, Maren S, McNally GP. Behavioral and neurobiological mechanisms of pavlovian and instrumental extinction learning. Physiol Rev. (2021) 101:611–81. doi: 10.1152/physrev.00016.2020
72. Bouton ME. Context, ambiguity, and unlearning: sources of relapse after behavioral extinction. Biol Psychiatry. (2002) 52:976–86. doi: 10.1016/S0006-3223(02)01546-9
73. Vervliet B, Craske MG, Hermans D. Fear extinction and relapse: state of the art. Annu Rev Clin Psychol. (2013) 9:215–48. doi: 10.1146/annurev-clinpsy-050212-185542
74. Volders S, Meulders A, De Peuter S, Vervliet B, Vlaeyen JWS. Safety behavior can hamper the extinction of fear of movement-related pain: an experimental investigation in healthy participants. Behav Res Ther. (2012) 50:735–46. doi: 10.1016/j.brat.2012.06.004
75. Vervliet B, Indekeu E. Low-cost avoidance behaviors are resistant to fear extinction in humans. Front Behav Neurosci. (2015) 9:351. doi: 10.3389/fnbeh.2015.00351
76. Lovibond PF, Mitchell CJ, Minard E, Brady A, Menzies RG. Safety behaviours preserve threat beliefs: protection from extinction of human fear conditioning by an avoidance response. Behav Res Ther. (2009) 47:716–20. doi: 10.1016/j.brat.2009.04.013
77. Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther. (2014) 58:10–23. doi: 10.1016/j.brat.2014.04.006
78. Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, et al. Interoception and mental health: a roadmap. Biol Psychiatry Cogn Neurosci Neuroimaging. (2018) 3:501–13. doi: 10.1016/j.bpsc.2018.04.007
79. Flack F, Stahlschmidt L, Dobe M, Hirschfeld G, Strasser A, Michalak J, et al. Efficacy of adding interoceptive exposure to intensive interdisciplinary treatment for adolescents with chronic pain: a randomized controlled trial. Pain. (2018) 159:2223–33. doi: 10.1097/j.pain.0000000000001321
80. Schemer L, Schroeder A, Ørnbøl E, Glombiewski JA. Exposure and cognitive-behavioural therapy for chronic back pain: an RCT on treatment processes. Eur J Pain. (2019) 23:526–38. doi: 10.1002/ejp.1326
81. Craske MG, Wolitzky-Taylor KB, Labus J, Wu S, Frese M, Mayer EA, et al. A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behav Res Ther. (2011) 49:413–21. doi: 10.1016/j.brat.2011.04.001
82. Kinsinger SW. Cognitive-behavioral therapy for patients with irritable bowel syndrome: current insights. Psychol Res Behav Manag. (2017) 10:231–7. doi: 10.2147/PRBM.S120817
83. Ljótsson B, Hesser H, Andersson E, Lackner JM, El Alaoui S, Falk L, et al. Provoking symptoms to relieve symptoms: a randomized controlled dismantling study of exposure therapy in irritable bowel syndrome. Behav Res Ther. (2014) 55:27–39. doi: 10.1016/j.brat.2014.01.007
84. Ballou S, Keefer L. Psychological interventions for irritable bowel syndrome and inflammatory bowel diseases. Clin Transl Gastroenterol. (2017) 8:e214. doi: 10.1038/ctg.2016.69
85. Schaumberg K, Reilly EE, Gorrell S, Levinson CA, Farrell NR, Brown TA, et al. Conceptualizing eating disorder psychopathology using an anxiety disorders framework: evidence and implications for exposure-based clinical research. Clin Psychol Rev. (2021) 83:101952. doi: 10.1016/j.cpr.2020.101952
86. Butler RM, Heimberg RG. Exposure therapy for eating disorders: a systematic review. Clin Psychol Rev. (2020) 78:101851. doi: 10.1016/j.cpr.2020.101851
87. Murray SB, Treanor M, Liao B, Loeb KL, Griffiths S, Le Grange D. Extinction theory and anorexia nervosa: deepening therapeutic mechanisms. Behav Res Ther. (2016) 87:1–10. doi: 10.1016/j.brat.2016.08.017
88. Cardi V, Leppanen J, Mataix-Cols D, Campbell IC, Treasure J. A case series to investigate food-related fear learning and extinction using in vivo food exposure in anorexia nervosa: a clinical application of the inhibitory learning framework. Eur Eat Disord Rev. (2019) 27:173–81. doi: 10.1002/erv.2639
89. Byrne SP, Haber P, Baillie A, Giannopolous V, Morley K. Cue exposure therapy for alcohol use disorders: what can be learned from exposure therapy for anxiety disorders? Subst Use Misuse. (2019) 54:2053–63. doi: 10.1080/10826084.2019.1618328
90. Mellentin AI, Skøt L, Nielsen B, Schippers GM, Nielsen AS, Stenager E, et al. Cue exposure therapy for the treatment of alcohol use disorders: a meta-analytic review. Clin Psychol Rev. (2017) 57:195–207. doi: 10.1016/j.cpr.2017.07.006
91. Back SE, Killeen T, Badour CL, Flanagan JC, Allan NP, Ana ES, et al. Concurrent treatment of substance use disorders and PTSD using prolonged exposure: a randomized clinical trial in military veterans. Addict Behav. (2019) 90:369–77. doi: 10.1016/j.addbeh.2018.11.032
92. Pittig A, Wong AHK, Glück VM, Boschet JM. Avoidance and its bi-directional relationship with conditioned fear: mechanisms, moderators, and clinical implications. Behav Res Ther. (2020) 126:103550. doi: 10.1016/j.brat.2020.103550
93. Mobbs D. The ethological deconstruction of fear(s). Curr Opin Behav Sci. (2018) 24:32–7. doi: 10.1016/j.cobeha.2018.02.008
94. Craske MG, Stein MB, Eley TC, Milad MR, Holmes A, Rapee RM, et al. Anxiety disorders. Nat Rev Dis Prim. (2017) 3:17024. doi: 10.1038/nrdp.2017.24
95. Vervliet B, Raes F. Criteria of validity in experimental psychopathology:application to models of anxiety and depression. Psychol Med. (2013) 43:2241–4. doi: 10.1017/S0033291712002267
96. Blakey SM, Abramowitz JS. The effects of safety behaviors during exposure therapy for anxiety: critical analysis from an inhibitory learning perspective. Clin Psychol Rev. (2016) 49:1–15. doi: 10.1016/j.cpr.2016.07.002
97. Goetz AR, Davine TP, Siwiec SG, Lee H-J. The functional value of preventive and restorative safety behaviors: a systematic review of the literature. Clin Psychol Rev. (2016) 44:112–24. doi: 10.1016/j.cpr.2015.12.005
98. Salkovskis PM, Clark DM, Hackmann A, Wells A, Gelder MG. An experimental investigation of the role of safety-seeking behaviours in the maintenance of panic disorder with agoraphobia. Behav Res Ther. (1999) 37:559–74. doi: 10.1016/S0005-7967(98)00153-3
99. Rachman S, Radomsky AS, Shafran R. Safety behaviour: a reconsideration. Behav Res Ther. (2008) 46:163–73. doi: 10.1016/j.brat.2007.11.008
100. Wolitzky KB, Telch MJ. Augmenting in vivo exposure with fear antagonistic actions: a preliminary test. Behav Ther. (2009) 40:57–71. doi: 10.1016/j.beth.2007.12.006
101. Milosevic I, Radomsky AS. Safety behaviour does not necessarily interfere with exposure therapy. Behav Res Ther. (2008) 46:1111–8. doi: 10.1016/j.brat.2008.05.011
102. Goetz AR, Lee H-J. The effects of preventive and restorative safety behaviors on a single-session of exposure therapy for contamination fear. J Behav Ther Exp Psychiatry. (2015) 46:151–7. doi: 10.1016/j.jbtep.2014.10.003
103. Hood HK, Antony MM, Koerner N, Monson CM. Effects of safety behaviors on fear reduction during exposure. Behav Res Ther. (2010) 48:1161–9. doi: 10.1016/j.brat.2010.08.006
104. Milosevic I, Radomsky AS. Keep your eye on the target: safety behavior reduces targeted threat beliefs following a behavioral experiment. Cognit Ther Res. (2013) 37:557–71. doi: 10.1007/s10608-012-9483-2
105. Levy HC, Radomsky AS. Safety behaviour enhances the acceptability of exposure. Cogn Behav Ther. (2014) 43:83–92. doi: 10.1080/16506073.2013.819376
106. Milosevic I, Radomsky AS. Incorporating the judicious use of safety behavior into exposure-based treatments for anxiety disorders: a study of treatment acceptability. J Cogn Psychother. (2013) 27:155–74. doi: 10.1891/0889-8391.27.2.155
107. Sangha S, Diehl MM, Bergstrom HC, Drew MR. Know safety, no fear. Neurosci Biobehav Rev. (2020) 108:218–30. doi: 10.1016/j.neubiorev.2019.11.006
108. Krypotos AM, Engelhard IM. Targeting avoidance via compound extinction. Cogn Emot. (2019) 33:1523–30. doi: 10.1080/02699931.2019.1573718
109. Icenhour A, Langhorst J, Benson S, Schlamann M, Hampel S, Engler H, et al. Neural circuitry of abdominal pain-related fear learning and reinstatement in irritable bowel syndrome. Neurogastroenterol Motil. (2015) 27:114–27. doi: 10.1111/nmo.12489
110. Koenen LR, Pawlik RJ, Icenhour A, Petrakova L, Forkmann K, Theysohn N, et al. Associative learning and extinction of conditioned threat predictors across sensory modalities. Commun Biol. (2021) 4:1–17. doi: 10.1038/s42003-021-02008-1
111. Labrenz F, Icenhour A, Schlamann M, Forsting M, Bingel U, Elsenbruch S. From Pavlov to pain: how predictability affects the anticipation and processing of visceral pain in a fear conditioning paradigm. Neuroimage. (2016) 130:104–14. doi: 10.1016/j.neuroimage.2016.01.064
112. Park MJ, Kim DJ, Lee U, Na EJ, Jeon HJ. A literature overview of Virtual Reality (VR) in treatment of psychiatric disorders: recent advances and limitations. Front psychiatry. (2019) 10:505. doi: 10.3389/fpsyt.2019.00505
113. Maples-Keller JL, Yasinski C, Manjin N, Rothbaum BO. Virtual reality-enhanced extinction of phobias and post-traumatic stress. Neurother J Am Soc Exp Neurother. (2017) 14:554–63. doi: 10.1007/s13311-017-0534-y
114. Meulders A, Franssen M, Fonteyne R, Vlaeyen JWS. Acquisition and extinction of operant pain-related avoidance behavior using a 3 degrees-of-freedom robotic arm. Pain. (2016) 157:1094–104. doi: 10.1097/j.pain.0000000000000483
115. Glogan E, Vandael K, Gatzounis R, Meulders A. When do we not face our fears? Investigating the boundary conditions of costly pain-related avoidance generalization. J Pain. (2021) 22:1221–32. doi: 10.1016/j.jpain.2021.03.149
116. van Vliet CM, Meulders A, Vancleef LMG, Vlaeyen JWS. Avoidance behaviour performed in the context of a novel, ambiguous movement increases threat and pain-related fear. Pain. (2021) 162:875–85. doi: 10.1097/j.pain.0000000000002079
117. Kumar V, Bhat ZA, Kumar D. Animal models of anxiety: a comprehensive review. J Pharmacol Toxicol Methods. (2013) 68:175–83. doi: 10.1016/j.vascn.2013.05.003
118. Kirlic N, Young J, Aupperle RL. Animal to human translational paradigms relevant for approach avoidance conflict decision making. Behav Res Ther. (2017) 96:14–29. doi: 10.1016/j.brat.2017.04.010
119. Konovalova I, Antolin J V, Bolderston H, Gregory NJ. Adults with higher social anxiety show avoidant gaze behaviour in a real-world social setting: a mobile eye tracking study. PLoS ONE. (2021) 16:e0259007. doi: 10.1371/journal.pone.0259007
120. Lebowitz ER, François B. Using motion tracking to measure avoidance in children and adults: psychometric properties, associations with clinical characteristics, and treatment-related change. Behav Ther. (2018) 49:853–65. doi: 10.1016/j.beth.2018.04.005
121. Wong AHK, Pittig A. A dimensional measure of safety behavior: a non-dichotomous assessment of costly avoidance in human fear conditioning. Psychol Res. (2021). doi: 10.1007/s00426-021-01490-w. [Epub ahead of print].
122. Hengen KM, Alpers GW. Better safe than wealthy: dysfunctional risk avoidance in spider-fearful individuals. J Anxiety Disord. (2021) 79:102383. doi: 10.1016/j.janxdis.2021.102383
123. Pittig A, Hengen K, Bublatzky F, Alpers GW. Social and monetary incentives counteract fear-driven avoidance: evidence from approach-avoidance decisions. J Behav Ther Exp Psychiatry. (2018) 60:69–77. doi: 10.1016/j.jbtep.2018.04.002
124. Claes N, Karos K, Meulders A, Crombez G, Vlaeyen JWS. Competing goals attenuate avoidance behavior in the context of pain. J Pain. (2014) 15:1120–9. doi: 10.1016/j.jpain.2014.08.003
125. Van Damme S, Van Ryckeghem DML, Wyffels F, Van Hulle L, Crombez G. No pain no gain? Pursuing a competing goal inhibits avoidance behavior. Pain. (2012) 153:800–4. doi: 10.1016/j.pain.2011.12.015
126. Lemmens A, Smeets T, Beckers T, Dibbets P. Avoiding at all costs? An exploration of avoidance costs in a novel Virtual Reality procedure. Learn Motiv. (2021) 73:101710. doi: 10.1016/j.lmot.2021.101710
127. Pincus T, Smeets RJEM, Simmonds MJ, Sullivan MJL. The fear avoidance model disentangled: improving the clinical utility of the fear avoidance model. Clin J Pain. (2010) 26:739–46. doi: 10.1097/AJP.0b013e3181f15d45
128. Bernstein DA, Nietzel MT. Procedural variation in behavioral avoidance tests. J Consult Clin Psychol. (1973) 41:165–74. doi: 10.1037/h0035170
129. Bernstein DA, Nietzel MT. Behavioral avoidance tests: the effects of demand characteristics and repeated measures on two types of subjects. Behav Ther. (1974) 5:183–92. doi: 10.1016/S0005-7894(74)80133-4
130. Lundberg M, Grimby-Ekman A, Verbunt J, Simmonds MJ. Pain-related fear: a critical review of the related measures. Pain Res Treat. (2011) 2011:494196. doi: 10.1155/2011/494196
131. Gatchel RJ, Neblett R, Kishino N, Ray CT. Fear-avoidance beliefs and chronic pain. J Orthop Sports Phys Ther. (2016) 46:38–43. doi: 10.2519/jospt.2016.0601
132. Mobbs D, Hagan CC, Dalgleish T, Silston B, Prévost C. The ecology of human fear: survival optimization and the nervous system. Front Neurosci. (2015) 9:55. doi: 10.3389/fnins.2015.00055
133. Xia W, Dymond S, Lloyd K, Vervliet B. Partial reinforcement of avoidance and resistance to extinction in humans. Behav Res Ther. (2017) 96:79–89. doi: 10.1016/j.brat.2017.04.002
134. Zuj D V, Xia W, Lloyd K, Vervliet B, Dymond S. Negative reinforcement rate and persistent avoidance following response-prevention extinction. Behav Res Ther. (2020) 133:103711. doi: 10.1016/j.brat.2020.103711
135. Glogan E, Gatzounis R, Meulders M, Meulders A. Generalization of instrumentally acquired pain-related avoidance to novel but similar movements using a robotic arm-reaching paradigm. Behav Res Ther. (2020) 124:103525. doi: 10.1016/j.brat.2019.103525
136. Glogan E, Gatzounis R, Vandael K, Franssen M, Vlaeyen JWS, Meulders A. Investigating pain-related avoidance behavior using a robotic arm-reaching paradigm. J Vis Exp. (2020). 3:164. doi: 10.3791/61717
137. van Vliet CM, Meulders A, Vancleef LMG, Meyers E, Vlaeyen JWS. Changes in pain-related fear and pain when avoidance behavior is no longer effective. J Pain. (2020) 21:494–505. doi: 10.1016/j.jpain.2019.09.002
138. Flores A, López FJ, Vervliet B, Cobos PL. Intolerance of uncertainty as a vulnerability factor for excessive and inflexible avoidance behavior. Behav Res Ther. (2018) 104:34–43. doi: 10.1016/j.brat.2018.02.008
139. Leigh E, Clark DM. Understanding social anxiety disorder in adolescents and improving treatment outcomes: applying the cognitive model of Clark and Wells (1995). Clin Child Fam Psychol Rev. (2018) 21:388–414. doi: 10.1007/s10567-018-0258-5
140. Gkika S, Wittkowski A, Wells A. Social cognition and metacognition in social anxiety: a systematic review. Clin Psychol Psychother. (2018) 25:10–30. doi: 10.1002/cpp.2127
141. Lonsdorf TB, Merz CJ. More than just noise: inter-individual differences in fear acquisition, extinction and return of fear in humans - biological, experiential, temperamental factors, and methodological pitfalls. Neurosci Biobehav Rev. (2017) 80:703–28. doi: 10.1016/j.neubiorev.2017.07.007
142. Kessler RC. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. (1995) 52:1048. doi: 10.1001/archpsyc.1995.03950240066012
143. Cameron OG, Hill EM. Women and anxiety. Psychiatr Clin North Am. (1989) 12:175–86. doi: 10.1016/S0193-953X(18)30459-3
144. Turgeon L, Marchand A, Dupuis G. Clinical Features in panic disorder with agoraphobia. J Anxiety Disord. (1998) 12:539–53. doi: 10.1016/S0887-6185(98)00031-0
145. Nillni YI, Berenz EC, Rohan KJ, Zvolensky MJ. Sex differences in panic-relevant responding to a 10% carbon dioxide-enriched air biological challenge. J Anxiety Disord. (2012) 26:165–72. doi: 10.1016/j.janxdis.2011.10.008
146. McLean CP, Hope DA. Subjective anxiety and behavioral avoidance: gender, gender role, and perceived confirmability of self-report. J Anxiety Disord. (2010) 24:494–502. doi: 10.1016/j.janxdis.2010.03.006
147. Sheynin J, Beck KD, Servatius RJ, Myers CE. Acquisition and extinction of human avoidance behavior: attenuating effect of safety signals and associations with anxiety vulnerabilities. Front Behav Neurosci. (2014) 8:323. doi: 10.3389/fnbeh.2014.00323
148. Bangasser DA, Eck SR, Telenson AM, Salvatore M. Sex differences in stress regulation of arousal and cognition. Physiol Behav. (2018) 187:42–50. doi: 10.1016/j.physbeh.2017.09.025
149. Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. (2014) 35:320–30. doi: 10.1016/j.yfrne.2014.05.004
150. Mogil JS, Bailey AL. Sex and gender differences in pain and analgesia. Prog Brain Res. (2010) 186:141–57. doi: 10.1016/B978-0-444-53630-3.00009-9
151. Camilleri M. Sex as a biological variable in irritable bowel syndrome. Neurogastroenterol Motil Off J Eur Gastrointest Motil Soc. (2020) 32:e13802. doi: 10.1111/nmo.13802
152. San Martín C, Jacobs B, Vervliet B. Further characterization of relief dynamics in the conditioning and generalization of avoidance: effects of distress tolerance and intolerance of uncertainty. Behav Res Ther. (2020) 124:103526. doi: 10.1016/j.brat.2019.103526
153. Lommen MJJ, Engelhard IM, van den Hout MA. Neuroticism and avoidance of ambiguous stimuli: better safe than sorry? Pers Individ Dif. (2010) 49:1001–6. doi: 10.1016/j.paid.2010.08.012
154. Ibrahim ME, Weber K, Courvoisier DS, Genevay S. Big five personality traits and disabling chronic low back pain: association with fear-avoidance, anxious and depressive moods. J Pain Res. (2020) 14:745–54. doi: 10.2147/JPR.S237522
155. Claes N, Crombez G, Vlaeyen JWS. Pain-avoidance versus reward-seeking: an experimental investigation. Pain. (2015) 156:1449–57. doi: 10.1097/j.pain.0000000000000116
156. Aupperle RL, Paulus MP. Neural systems underlying approach and avoidance in anxiety disorders. Dialogues Clin Neurosci. (2010) 12:517–31. doi: 10.31887/DCNS.2010.12.4/raupperle
157. Pittig A, Dehler J. Same fear responses, less avoidance: rewards competing with aversive outcomes do not buffer fear acquisition, but attenuate avoidance to accelerate subsequent fear extinction. Behav Res Ther. (2019) 112:1–11. doi: 10.1016/j.brat.2018.11.003
158. Rattel JA, Miedl SF, Blechert J, Wilhelm FH. Higher threat avoidance costs reduce avoidance behaviour which in turn promotes fear extinction in humans. Behav Res Ther. (2017) 96:37–46. doi: 10.1016/j.brat.2016.12.010
159. Pittig A, Alpers GW, Niles AN, Craske MG. Avoidant decision-making in social anxiety disorder: a laboratory task linked to in vivo anxiety and treatment outcome. Behav Res Ther. (2015) 73:96–103. doi: 10.1016/j.brat.2015.08.003
160. Meulders A, Van Daele T, Volders S, Vlaeyen JWS. The use of safety-seeking behavior in exposure-based treatments for fear and anxiety: benefit or burden? A meta-analytic review. Clin Psychol Rev. (2016) 45:144–56. doi: 10.1016/j.cpr.2016.02.002
161. Urcelay GP, Prével A. Extinction of instrumental avoidance. Curr Opin Behav Sci. (2019) 26:165–71. doi: 10.1016/j.cobeha.2019.01.018
162. Pittig A. Incentive-based extinction of safety behaviors: positive outcomes competing with aversive outcomes trigger fear-opposite action to prevent protection from fear extinction. Behav Res Ther. (2019) 121:103463. doi: 10.1016/j.brat.2019.103463
163. Meulders A, Vansteenwegen D, Vlaeyen JWS. The acquisition of fear of movement-related pain and associative learning: a novel pain-relevant human fear conditioning paradigm. Pain. (2011) 152:2460–9. doi: 10.1016/j.pain.2011.05.015
164. Icenhour A, Labrenz F, Ritter C, Theysohn N, Forsting M, Bingel U, et al. Learning by experience? Visceral pain-related neural and behavioral responses in a classical conditioning paradigm. Neurogastroenterol Motil. (2017) 29:e13026. doi: 10.1111/nmo.13026
165. Icenhour A, Kattoor J, Benson S, Boekstegers A, Schlamann M, Merz CJ, et al. Neural circuitry underlying effects of context on human pain-related fear extinction in a renewal paradigm. Hum Brain Mapp. (2015) 36:3179–93. doi: 10.1002/hbm.22837
Keywords: avoidance, psychosomatic medicine, pain, anxiety, associative learning, conditioning, gut-brain axis
Citation: Labrenz F, Woud ML, Elsenbruch S and Icenhour A (2022) The Good, the Bad, and the Ugly—Chances, Challenges, and Clinical Implications of Avoidance Research in Psychosomatic Medicine. Front. Psychiatry 13:841734. doi: 10.3389/fpsyt.2022.841734
Received: 22 December 2021; Accepted: 28 January 2022;
Published: 18 February 2022.
Edited by:
Stephan Zipfel, University of Tübingen, GermanyReviewed by:
Hiu Tin Leung, The University of Hong Kong, Hong Kong SAR, ChinaCopyright © 2022 Labrenz, Woud, Elsenbruch and Icenhour. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adriane Icenhour, QWRyaWFuZS5JY2VuaG91ckBydWhyLXVuaS1ib2NodW0uZGU=
 Franziska Labrenz
Franziska Labrenz Marcella L. Woud
Marcella L. Woud Sigrid Elsenbruch
Sigrid Elsenbruch Adriane Icenhour
Adriane Icenhour