
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 05 April 2022
Sec. Addictive Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.838700
This article is part of the Research TopicDiscounting Models in Behavioral Health Economics and Quantitative Health Psychology, Volume IIView all 5 articles
Background: Binge eating disorder (BED) as a public health problem has been included in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Akin to addictive disorders, impulsivity-related neuropsychological constructs might be potentially involved in the onset and development of BED. However, it remains unclear which facets of impulsivity are connected to overeating and binge eating behaviors among non-clinical populations. The present study aimed to detect the relationship between impulsivity and binge eating both on the personality-trait and behavioral-choice levels in undiagnosed young adults.
Methods: Fifty-eight individuals with probable BED and 59 healthy controls, matched on age, gender, and educational level, were assessed by using a series of self-report measurements, including the Barratt Impulsiveness Scale (BIS-11), UPPS-P Impulsive Behaviors Scale (UPPS-P), Delay Discounting Test (DDT), and Probability Discounting Test (PDT).
Results: Multivariate analysis of variance models revealed that compared with healthy controls, the probable BED group showed elevated scores on the BIS-11 Attentional and Motor impulsiveness, and on the UPPS-P Negative Urgency, Positive Urgency, and Lack of Perseverance. However, the probable BED subjects had similar discounting rates on the DDT and PDT with healthy controls. Regression models found that Negative Urgency was the only positive predictor of binge eating behavior.
Conclusions: These findings suggested that typical facets of trait impulsivity, which have been recognized in addictive disorders, were associated with binge eating in young adults, whereas choice impulsivity was not aberrantly seen in the same probable BED sample. This study might promote a better understanding of the pathogenesis of BED.
Binge eating disorder (BED) is characterized by overwhelming eating desire with recurrent episodes of binge eating (at least once a week during the last 3 months) and lack of control over binge-eating behavior (1). BED has been included as a separate category within the Feeding and Eating Disorders in the latest version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (2). The lifetime prevalence for BED in adults is about 2%, with women having a higher risk than men (3). The prevalence of BED among obese adolescents aged 12–17 years has been reported over 30% in recent literature (4). Generally, adolescents and young adults have a high risk for BED due to their immature cognitive control abilities (5, 6). Interestingly, although most studies focused on clinical samples of BED, some data showed that in non-clinical populations with a normal body mass index (BMI), over-eating behavior could also be seen with an increase in the risk of developing into BED in these young adults (7, 8). Nevertheless, it remains unclear which neuropsychological constructs might be potentially linked to BED among general adolescents and young adults.
Impulsivity is a hallmark feature in various mental disorders including addictive behaviors, as well as in so-called “food addiction”, which has been largely controversial (8). Many studies suggested that impulsivity might be a vulnerability trait for both behavioral and substance-related addictions (9–11). Importantly, individuals with BED and substance abusers shared similar intense cravings, disinhibition over the intake of foods or drugs, and altered reward sensitivity (12, 13). Therefore, impulsivity might also play a part in the processes of BED. However, the relationship between impulsivity and BED remains to be further understood.
Impulsivity refers to a tendency to act without careful thinking or to react prematurely (14, 15). Although impulsivity is a multifaceted construct, at least two different connotations of impulsivity may be separately detected with different measurements (16). Specifically, personality-level trait impulsivity is usually measured by self-report scales such as the Barratt Impulsiveness Scale (BIS-11) (17), while behavioral-level choice impulsivity is mostly assessed by reward discounting tasks such as the Delay-discounting Test (DDT) (18).
Trait impulsivity is a stable and inheritable feature with self-reported attributions of self-regulatory ability (19). Many previous studies have linked trait impulsivity to binge eating behaviors in clinical patients with BED (20, 21). Nevertheless, these samples always had high comorbidity with attention-deficit/hyperactivity disorder (ADHD) (22), anxiety disorders (23), and substance use disorders (24), which might lead to confounding results when detecting the relationship between impulsivity and BED. Moreover, limited data on the associations of trait impulsivity and BED have been incongruous among general populations. Some data suggested that heightened impulsivity was found in young adults with BED compared to healthy controls (25–28), while other studies showed no group differences (29, 30). Findings were also inconsistent when specific facets of impulsive traits were taken into account (31, 32). One prior study found that Attentional, Motor, and Non-planning Impulsiveness were significantly related to binge eating in normal-weighted women (27), while another study showed that only Attentional and Motor Impulsiveness were elevated in obese patients with overeating (30).
Comparatively, choice impulsivity is considered an irrational decision-making process influenced by motivations and affects (33, 34). Meta-analyses have demonstrated that increased choice impulsivity might be particularly relevant to BED (35–37). Clinical patients with BED, including both normal-weighted and over-weighted, displayed steeper delay discounting than healthy controls on the DDT (38, 39). Nonetheless, it is unclear whether this aberrant delay discounting was truly connected to BED itself or rooted in the comorbid psychiatric disorders in these clinical patients (40). Despite little evidence, several studies with non-clinical samples revealed that adults with BED exhibited steeper delay discounting compared to controls (41, 42). However, negative results also showed that BED individuals and healthy controls had no differences on delay discounting tasks (43, 44). Regarding probability discounting, limited studies suggested that obese women with BED tended to discount probabilistic rewards less steeply than healthy controls (45, 46), though our prior data displayed similar probability discounting in young adults with and without BED (47). Therefore, more studies are needed to elucidate the relationship between binge-eating behaviors and choice impulsivity in general populations.
The current study aimed to further detect the associations between impulsivity and binge eating among non-treatment-seeking samples. The Barratt Impulsiveness Scale-11 (BIS-11) and UPPS-P Impulsive Behaviors Scale (UPPS-P) were used to measure trait impulsivity, and the Delay Discounting test (DDT) and Probability Discounting test (PDT) were used to assess choice impulsivity, comparing probable BED subjects with healthy controls. It was generally hypothesized that heightened trait impulsivity and choice impulsivity would be linked to BED, as possible risk factors or vulnerability markers for binge eating behaviors.
Participants were recruited through posters from a local university in Guiyang, China. Power analyses (48) were conducted to determine a target sample size (Cohen' s d = 0.4, α = 0.05, 1 – β = 0.8, F tests, G*Power), with a minimum sample size of 52 (at least n = 26 in each group). All subjects were invited to provide demographic information and complete a series of self-report questionnaires in the laboratory. Inclusion criteria included: (1) 18–25 years of age, and (2) willingness to participate in this study. Exclusion criteria included: (1) past or current severe psychiatric disorders (e.g., schizophrenia, bipolar disorder), (2) a history of illegal psychoactive substance use (e.g., cocaine, heroin, amphetamine), (3) brain trauma or neurological diseases, and (4) severe somatic diseases or special physical conditions that were inappropriate (e.g., menstrual period for women), all of which were evaluated by self-reports.
Probable BED status was estimated by using the Chinese version of the Binge Eating Scale (BES) (47), on which a total score of ≥18 indicates probable binge eating disorder (49). Finally, the probable BED group (pBED) consisted of 58 subjects (mean age = 19.34 ± 1.15 years; 10 men, 17.24%; mean BES score = 21.60 ± 3.29) according to the BES scores. The healthy controls (HCs) included 59 subjects, matched on age, gender, and educational level with the probable BED group (mean age = 19.12 ± 0.77 years; 10 men, 16.94%; mean BES score = 5.47 ± 2.22). All subjects gave informed consent and were compensated with a gift equal to RMB ¥50. The current study was reviewed and approved by the Human Research Ethics Committee at the Guizhou Medical University. The proposed study design, recruitment process, and our plans to compensate the participants were in accordance with the Declaration of Helsinki.
A brief self-report questionnaire was employed to collect demographic data of the subjects, including age, gender, ethnicity, and home locality. Standard procedures were used to measure weight and height, and then body mass index (BMI) was calculated as weight divided by the square of height (i.e., kg/m2). The participants also reported their smoking and drinking behaviors in the past 30 days on two questions (“Have you smoked at least one cigarette in the past 30 days?” and “Did you take at least one drink in the past 30 days?”).
The Binge Eating Scale (BES) (47, 50, 51), was used to screen binge eating behavior. The BES is a 16-item self-report questionnaire designed to assess behavioral, emotional, and cognitive symptoms of binge eating. Items were rated on a five-point Likert scale from 0 (not at all) to 4 (very much), with a total score ranging from 0 to 46. Higher total scores indicate more severe binge eating problems, with a score of ≥18 indicating probable binge eating disorder (BED) (49, 51). The Cronbach's α was 0.863 in this study.
Participants completed the Barratt Impulsiveness Scale (BIS-11) (17), a 30-item self-report inventory that measures impulsive personality in terms of three factors: Motor Impulsiveness, Attentional Impulsiveness, and Non-planning Impulsiveness. Items were rated on a four-point Likert scale. A higher score of each dimension indicates a higher level of trait impulsivity. The Cronbach's α for the BIS-11 was 0.796 in this study. Subjects also completed the UPPS-P Impulsive Behaviors Scale (UPPS-P) (15, 52), a 59-item self-report questionnaire used to assess five dimensions of impulsive personality: Sensation Seeking, Lack of Premeditation, Lack of Perseverance, Negative Urgency, and Positive Urgency. Items were rated on a four-point Likert scale. The Cronbach's α for the UPPS-P was 0.878.
The Delay Discounting Test (DDT) and Probability Discounting Test (PDT) were used to evaluate choice impulsivity. Both tasks were designed to evaluate discounting degrees of hypothetical monetary rewards. The DDT (18) is a fixed serial of a 27-item choice questionnaire between a smaller immediate monetary reward and a larger delayed monetary reward. For the DDT, k parameter indicates the degree of delay discounting, calculated by the equation: V = A/(1 + kD). In this equation, V refers to the individual subjective value of the delayed reward, A is the nominal amount of the delayed reward, and D is the length of the delay. A higher k indicates a higher degree of delay discounting. The PDT (53) is a three-part monetary choice questionnaire, with 10 items in each part. Participants were told to choose between a smaller amount of monetary reward obtained for sure and a larger amount of monetary reward obtained probabilistically (e.g., “$20 for sure” vs. “10% chance of obtaining $80”). The h parameter is calculated by the hyperbolic equation: V = A/(1 + hθ). In this equation, V refers to the present subjective value of the probabilistic reward A. A lower h value implies that the probabilistic rewards are less steeply discounted, suggesting a reduction in risk aversion. The k and h values were log-transformed in analyses.
Data analysis was performed with the Statistical Package for the Social Sciences for Windows, Version 22.0 (SPSS Inc., Chicago, IL, USA). Chi-Square tests were used to test group differences on categorical variables (i.e., ethnicity, gender, home locality). t-Tests were adopted to analyze group differences on BMI and age. Multivariate analysis of variance (mANOVA) models were used to compare task scores between the two groups. Partial correlations were tested between the BIS-11, UPPS-P, DDT, PDT, and BES scores, controlling for age, BMI, gender, ethnicity, home locality, smoking, and drinking status. In addition, a multivariate linear regression analysis was conducted to test the effects of impulsivity measures on BES scores, and logistic regression analyses were tested for the predictive effects of impulsivity scores on binge eating behavior. According to the standardized variance inflation factor (VIF), multi-collinearity was not a problem for any variable in these regression models (VIF < 10). Significance was defined as p < 0.05, two-tailed.
Table 1 illustrated the demographics and task scores of the two groups. The pBED group had a higher BMI than the HCs (t = 4.18, p = 0.001). No between-group differences were found for age (p = 0.214), ethnicity (p = 0.649), gender (p = 0.967), or home locality (p = 0.872).
On the BIS-11, the mANOVA models revealed significant between-group differences on Attention Impulsiveness [F(1,114) = 21.061, p = 0.001, = 0.156] and Motor Impulsiveness [F(1,114) = 8.043, p = 0.005, = 0.066], but not on Non-Planning Impulsiveness [F(1,114) = 2.971, p = 0.087]. Post-hoc comparisons found that the pBED group had higher scores on Attentional Impulsiveness (Md = 2.669, p = 0.001, Cohen's d = 0.853) and Motor Impulsiveness (Md = 1.753, p = 0.005, Cohen's d = 0.514) than the HCs.
On the UPPS-P, the mANOVA models showed significant between-group differences on Negative Urgency [F(1,114) = 44.711, p = 0.001, = 0.282], Lack of Perseverance [F(1,114) = 7.419, p = 0.007, = 0.061], and Positive Urgency [F(1,114) = 19.421, p = 0.001, = 0.146], but not on Lack of Premeditation [F(1,114) = 0.416, p = 0.520) or Sensation Seeking (F(1,114) = 0.256, p = 0.614]. Post-hoc comparisons displayed that pBED group had higher scores on Negative Urgency (Md = 5.662, p = 0.001, Cohen's d = 1.241), Lack of Perseverance (Md = 1.712, p = 0.007, Cohen' s d = 0.504), and Positive Urgency (Md = 4.855, p = 0.001, Cohen' s d = 0.817) than HCs.
On the DDT, the mANOVA models displayed no significant between-group differences on the log-transformed k-value [F(1,114) = 1.176, p = 0.280]. On the PDT, the mANOVA models found no significant between-group differences on the log-transformed h values of the Part A [F(1,114) = 3.681, p = 0.058], Part B [F(1,114) = 0.044, p = 0.835] or Part C [F(1,114) = 0.183, p = 0.670].
As seen in Table 2, significant positive correlations were detected between the BES scores and BIS-11 Attentional Impulsiveness, Motor Impulsiveness, Non-planning Impulsiveness, UPPS-P Negative Urgency, Lack of Perseverance, and Positive Urgency scores (rp = 0.23–0.60, ps < 0.05). Nevertheless, no significant correlations were detected between the BES scores and UPPS-P Lack of Premeditation, Sensation Seeking, DDT k-value (log-transformed), and PDT h-values (log-transformed) of the three parts.
The multivariate linear regression analyses were used to test the effect of BIS-11, UPPS-P, DDT, and PDT scores on BES scores, with a two-step design. BMI was entered in step 1 as the control variable, and the impulsivity scores were entered in step 2 as the predictor variables. Table 3 displayed that only UPPS-P Negative Urgency positively predicted BES scores, after controlling for the effect of BMI [F (13, 103) = 7.03, p < 0.001; ΔR2 = 0.37, p < 0.001].
The binary logistic regression models were conducted to examine the effects of the impulsivity scores on binge-eating behavior. A two-step design was used: BMI was entered in step 1 as the control variable, and the three dimensions of BIS-11 (Attentional Impulsiveness, Motor Impulsiveness, and Non-planning Impulsiveness), five dimensions of UPPS-P (Negative Urgency, Lack of Premeditation, Lack of Perseverance, Sensation Seeking, and Positive Urgency), DDT k-value (log-transformed), and PDT h values (log-transformed) were entered in step 2. Table 4 revealed that only Negative Urgency positively predicted binge eating behavior (OR = 1.54, p < 0.001, NagelkerkeR2 = 0.650 for the model).
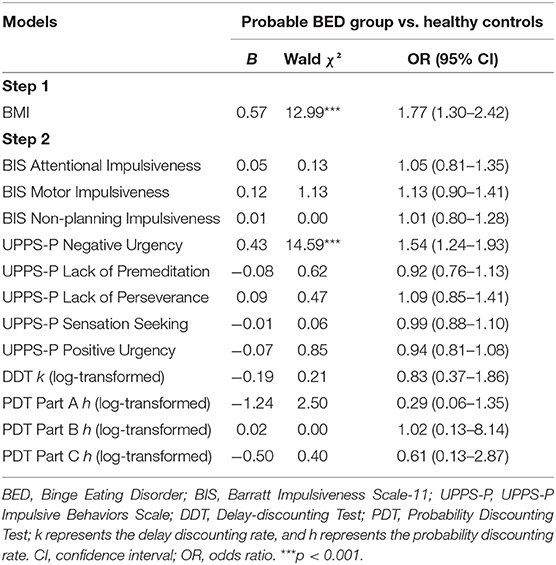
Table 4. Logistic regression analyses of impulsivity scores on binge eating controlling for BMI (N = 117).
To the best of our knowledge, the present study was the first to examine the associations between trait impulsivity, choice impulsivity, and binge-eating behavior in non-clinical samples. The results supported our hypotheses that individuals with probable binge eating disorder (pBED) might have elevated impulsive personality traits than the healthy controls. Specifically, the probable BED subjects showed higher levels of trait impulsivity on the BIS-11 (i.e., Attentional Impulsiveness, Motor Impulsiveness) and UPPS-P (i.e., Negative Urgency, Lack of Perseverance, Positive Urgency). However, the probable BED group had a normal level of choice impulsivity both on the DDT and the PDT, compared with the healthy controls. Significant positive correlations were found between BES scores and most trait impulsivity scores, including BIS-11 Attentional Impulsiveness, Motor Impulsiveness, Non-planning Impulsiveness, UPPS-P Negative Urgency, Lack of Perseverance, and Positive Urgency. More importantly, regression models showed that only Negative Urgency positively predicted binge eating behavior as a potential risk factor. These findings suggested that different impulsivity facets were separately associated with BED, and certain trait impulsivity (Negative Urgency) might be considered a hallmark for BED in non-clinical young adults.
Increased impulsivity has been proposed as a phenotype for addictive disorders as well as within the clinical obesity spectrum, and it might also increase the onset of BED (12). However, few studies have focused on the relationship between impulsivity and binge eating in non-treatment-seeking individuals with normal weight. The current study investigated the associations of trait impulsivity, choice impulsivity, and binge-eating behavior in common populations (i.e., young adult college students). The data showed that individuals with probable BED had elevated scores on measurements of trait impulsivity (i.e., Attentional Impulsiveness, Motor Impulsiveness, Negative Urgency, Lack of Perseverance, and Positive Urgency), consistent with previous reports on BED (54–57) and addictive disorders (58, 59).
Furthermore, positive correlations were detected between the BES scores and these impulsivity scores (Table 2). However, only Negative Urgency displayed the main effect as a significant indicator for binge-eating behavior in the regression models (Tables 3, 4). These findings suggested that elevated Negative Urgency might represent a preclinical susceptibility marker for binge eating disorder, although longitudinal studies are needed to clarify whether Negative Urgency precedes the onset of binge eating behavior or as a consequence of BED. Nevertheless, our first direct evidence in the non-treatment-seeking populations showed that specific trait of impulsivity (i.e., Negative Urgency) was overtly enhanced in binge-eating behavior (60–62). Negative Urgency reflects a typical tendency to act impulsively under the condition of extreme negative emotions (63). Individuals with elevated Negative Urgency seemed more likely to be involved into binge eating in order to deal with negative emotions, and as a result, their binge-eating behaviors would be further reinforced or deteriorated (64). Our results increased new knowledge to the current literature that Negative Urgency could play a key role for binge eating even in the non-clinical samples, as a possible susceptible hallmark of binge-eating behavior, which should promote a better understanding of the pathogenesis of BED. More interestingly, the proposed “Emotional Regulation Model” of BED emphasized that negative emotions might serve as a trigger component for binge eating, and impulsivity could possibly offer one explanation for the cause of binge eating triggered by negative emotions (65). In this respect, Negative Urgency might potentially represent a characteristic trait of impulsivity linking negative emotions to binge eating behavior that individuals with BED might react to binge eating with dysfunctional emotion regulation strategy due to their high level of impulsivity (65). If this is the case, it would be of help to further develop innovative therapeutic approaches for BED. Indeed, a recent study found that food-related impulsivity measured by laboratory tasks could be reduced by cognitive behavioral interventions and suggested that such clinical treatments might also be effective in modifying trait impulsivity associated with negative emotional states (e.g., Negative Urgency) in patients with BED (66). Nevertheless, further evidence-based experiments and clinical trials are warranted to verify the possible role of Negative Urgency both in the onset and development of binge eating behavior and in the treatment outcomes among different samples of binge eating disorder.
On the other side, the probable BED group did not show an aberrant pattern of choice impulsivity. The data revealed that individuals with probable BED performed similarly with the healthy controls on the Delay Discounting Test (DDT) and the Probability Discounting Test (PDT). Moreover, the DDT k value and PDT h-values were not significantly associated with or predictive of binge eating (Tables 2–4). Previous studies found that obese women with BED had higher discounting degrees of delayed rewards (67), and addictive drug abusers displayed a lower risk aversion compared to matched controls (68, 69). Among clinical samples of BED as well as those of obesity without BED, reduced reward processing in the striatal and amygdala regions indicated motivational hypofunction to non-food rewards (70, 71). Nonetheless, a longitudinal study showed that the ventromedial prefrontal cortex (vmPFC) activation did not display a significant effect on the severity of binge-eating behaviors in adolescent girls (72). Therefore, more parallel studies should be conducted to investigate the processes of delay gratification and risk aversion in both clinical and non-clinical samples of BED in the future. Meanwhile, a notable question related to choice impulsivity in BED should be taken into consideration that these two tasks (i.e., DDT and PDT) mainly contain hypothetical monetary rewards as the stimulus, which might reduce the suitability and validity of these tasks used in binge eating (37). Previous studies using non-monetary rewards on the DDT found evidence of increased choice impulsivity in BED individuals, with the largest effect sizes observed for food rewards (41). Thus, focus on food-related impulsivity should be paid more attention to in the investigation and might be conducive to better understanding the pathology of BED (12, 73).
Several limitations should be noted in the current study. Firstly, this study was a cross-sectional design in nature, and thus could not draw a causal conclusion between these impulsivity aspects and BED. Moreover, the samples mainly consisted of young adult college students and the results could not be generalized to clinical samples with serious binge-eating problems. Future research should investigate the relationship of specific trait impulsivity (e.g., Negative Urgency) with binge-eating behaviors in more severe clinical patients with BED. Thirdly, given that our study mostly focused on some limited aspects of impulsivity (i.e., trait impulsivity and choice impulsivity) measured by self-report scales, these findings should be interpreted more carefully because of the possible subjective bias, and other important facets of impulsivity (e.g., inhibitory control) should be investigated using more objective tasks. Especially, impulsivity is a quite complex and multidimensional theoretical concept (9), with diverse measurements probably evaluating differentiated facets of impulsivity. In our study, the BIS-11 and UPPS-P used are basically self-report questionnaires about different types of trait impulsivity that may reflect enduring impulsivity constructs, while the DDT and PDT are monetary reward-based decision-making tasks assessing behavioral choice impulsivity that may measure rather the current state of impulsive behaviors (e.g., delay discounting) (19, 74). As a result, the very low correlations between trait impulsivity (BIS-11, UPPS-P) and choice impulsivity (DDT, PDT) scores in this study (Table 2) further indicated that these two types of impulsivity could be largely uncorrelated and represent distinct pathways and processes of impulsivity (74). Therefore, more intensive studies are needed to further uncover the underlying mechanisms of these impulsivity categories connected to binge eating and other disorders. In addition to these points, another potential limitation should also be noted in the current study that the classification of probable BED was based on the BES scores without standard clinical diagnoses for BED. Thus, these participants were in fact undiagnosed non-clinical samples, although they might experience binge-eating behaviors and problems in the routine daily life. In the meantime, possible compensatory behaviors that could be associated with binge eating were not evaluated and excluded in the subjects, considering certain conditions such as life stress and negative emotions (e.g., depression, anxiety) are important risk factors for BED (75). Future similar studies should consider more standard diagnoses and compensatory behaviors.
Despite these limitations, the present study firstly looked into the associations between various aspects of impulsivity and binge-eating behavior in non-clinical samples of probable BED with a case-control design. Our results indicated that Attentional Impulsiveness, Motor Impulsiveness, Negative Urgency, Lack of Perseverance, and Positive Urgency were elevated in probable BED, and in particular, Negative Urgency was the only positive predictor of binge eating behavior. These findings suggested that typical facets of trait impulsivity, which have been recognized in addictive disorders, were associated with binge eating in young adults, while choice impulsivity was not aberrantly seen in the same probable BED sample.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee at the Guizhou Medical University. The patients/participants provided their written informed consent to participate in this study.
W-SY designed the study, wrote the protocols, directed the study, and wrote the first draft of the manuscript. D-HZ performed the main data analysis and assisted in writing the first draft of the manuscript. M-ML contributed to the assessments and data collection. All authors contributed to this article and have approved the final manuscript.
This study was supported by the National Natural Science Foundation of China (Nos: 32060195 and 31560284) to W-SY.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors are thankful for all the participants in this study.
1. Pasold TL, McCracken A, Ward-Begnoche WL. Binge eating in obese adolescents: emotional and behavioral characteristics and impact on health-related quality of life. Clin Child Psychol Psychiatry. (2014) 19:299–312. doi: 10.1177/1359104513488605
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
3. Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. (2013) 73:904–14. doi: 10.1016/j.biopsych.2012.11.020
4. Stabouli S, Erdine S, Suurorg L, Jankauskiene A, Lurbe E. Obesity and eating disorders in children and adolescents: the bidirectional link. Nutrients. (2021) 13:4321. doi: 10.3390/nu13124321
5. Hornberger LL, Lane MA, Committee Committee on Adolescence. Identification and management of eating disorders in children and adolescents. Pediatrics. (2021) 147:e2020040279. doi: 10.1542/peds.2020-040279
6. Marzilli E, Cerniglia L, Cimino S. A narrative review of binge eating disorder in adolescence: prevalence, impact, and psychological treatment strategies. Adolesc Health Med Ther. (2018) 9:17–30. doi: 10.2147/AHMT.S148050
7. Lowe MR, van Steenburgh J, Ochner C, Coletta M. Neural correlates of individual differences related to appetite. Physiol Behav. (2009) 97:561–71. doi: 10.1016/j.physbeh.2009.04.001
8. Rømer Thomsen K, Callesen MB, Hesse M, Kvamme TL, Pedersen MM, Pedersen MU, et al. Impulsivity traits and addiction-related behaviors in youth. J Behav Addict. (2018) 7:317–30. doi: 10.1556/2006.7.2018.22
9. Dalley JW, Robbins TW. Fractionating impulsivity: neuropsychiatric implications. Nat Rev Neurosci. (2017) 18:158–71. doi: 10.1038/nrn.2017.8
10. Davis C, Cohen A, Davids M, Rabindranath A. Attention-deficit/hyperactivity disorder in relation to addictive behaviors: a moderated-mediation analysis of personality-risk factors and sex. Front Psychiatry. (2015) 6:47. doi: 10.3389/fpsyt.2015.00047
11. Homberg JR, Karel P, Verheij MM. Individual differences in cocaine addiction: maladaptive behavioural traits. Addict Biol. (2014) 19:517–28. doi: 10.1111/adb.12036
12. Giel KE, Teufel M, Junne F, Zipfel S, Schag K. Food-related impulsivity in obesity and binge eating disorder-a systematic update of the evidence. Nutrients. (2017) 9:1170. doi: 10.3390/nu9111170
13. Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. (2016) 44:125–39. doi: 10.1016/j.cpr.2016.02.001
14. Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev. (2004) 28:343–51. doi: 10.1016/j.neubiorev.2004.03.007
15. Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Pers Individ Dif. (2001) 30:669–89. doi: 10.1016/S0191-8869(00)00064-7
16. Waltmann M, Herzog N, Horstmann A, Deserno L. Loss of control over eating: a systematic review of task based research into impulsive and compulsive processes in binge eating. Neurosci Biobehav Rev. (2021) 129:330–50. doi: 10.1016/j.neubiorev.2021.07.016
17. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. (1995) 51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1
18. Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. (1999) 128:78–87. doi: 10.1037/0096-3445.128.1.78
19. MacKillop J, Weafer J, C Gray J, Oshri A, Palmer A, de Wit H. The latent structure of impulsivity: impulsive choice, impulsive action, and impulsive personality traits. Psychopharmacology. (2016) 233:3361–70. doi: 10.1007/s00213-016-4372-0
20. Kollei I, Rustemeier M, Schroeder S, Jongen S, Herpertz S, Loeber S. Cognitive control functions in individuals with obesity with and without binge-eating disorder. Int J Eat Disord. (2018) 51:233–40. doi: 10.1002/eat.22824
21. Michael ML, Juarascio A. Elevated cognitive dietary restraint mediates the relationship between greater impulsivity and more frequent binge eating in individuals with binge-spectrum eating disorders. Eat Weight Disord. (2021) 26:2795–800. doi: 10.1007/s40519-021-01153-0
22. Karaca S, Saleh A, Canan F, Potenza MN. Comorbidity between behavioral addictions and attention deficit/hyperactivity disorder: a systematic review. Int J Ment Health Addict. (2017) 15:701–24. doi: 10.1007/s11469-016-9660-8
23. Welch E, Jangmo A, Thornton LM, Norring C, von Hausswolff-Juhlin Y, Herman BK, et al. Treatment-seeking patients with binge-eating disorder in the Swedish national registers: clinical course and psychiatric comorbidity. BMC Psychiatry. (2016) 16:163. doi: 10.1186/s12888-016-0840-7
24. Bogusz K, Kopera M, Jakubczyk A, Trucco EM, Kucharska K, Walenda A, et al. Prevalence of alcohol use disorder among individuals who binge eat: a systematic review and meta-analysis. Addiction. (2021) 116:18–31. doi: 10.1111/add.15155
25. Guerrieri R, Nederkoorn C, Stankiewicz K, Alberts H, Geschwind N, Martijn C, et al. The influence of trait and induced state impulsivity on food intake in normal-weight healthy women. Appetite. (2007) 49:66–73. doi: 10.1016/j.appet.2006.11.008
26. Khairallah C, Zoghbi M, Richa S, Bou Khalil R. Disgust, impulsivity and depressive dimensions in subjects at risk for bulimia nervosa and/or binge eating disorder. Asian J Psychiatr. (2019) 39:32–4. doi: 10.1016/j.ajp.2018.11.019
27. Lyke JA, Spinella M. Associations among aspects of impulsivity and eating factors in a nonclinical sample. Int J Eat Disord. (2004) 36:229–33. doi: 10.1002/eat.20025
28. Solomon-Krakus S, Uliaszek AA, Bagby RM. Evaluating the associations between personality psychopathology and heterogeneous eating disorder behaviors: a dimensional approach. Personal Disord. (2020) 11:249–59. doi: 10.1037/per0000358
29. Fields SA, Sabet M, Reynolds B. Dimensions of impulsive behavior in obese, overweight, and healthy-weight adolescents. Appetite. (2013) 70:60–6. doi: 10.1016/j.appet.2013.06.089
30. Kelly NR, Cotter EW, Mazzeo SE. Examining the role of distress tolerance and negative urgency in binge eating behavior among women. Eat Behav. (2014) 15:483–9. doi: 10.1016/j.eatbeh.2014.06.012
31. Meule A, Platte P. Facets of impulsivity interactively predict body fat and binge eating in young women. Appetite. (2015) 87:352–7. doi: 10.1016/j.appet.2015.01.003
32. Steward T, Mestre-Bach G, Vintró-Alcaraz C, Agüera Z, Jiménez-Murcia S, Granero R, et al. Delay discounting of reward and impulsivity in eating disorders: from anorexia nervosa to binge eating disorder. Eur Eat Disord Rev. (2017) 25:601–6. doi: 10.1002/erv.2543
33. Cardinal RN, Pennicott DR, Sugathapala CL, Robbins TW, Everitt BJ. Impulsive choice induced in rats by lesions of the nucleus accumbens core. Science. (2001) 292:2499–501. doi: 10.1126/science.1060818
34. Evenden JL. Varieties of impulsivity. Psychopharmacology. (1999) 146:348–61. doi: 10.1007/PL00005481
35. Guillaume S, Gorwood P, Jollant F, Van den Eynde F, Courtet P, Richard-Devantoy S. Impaired decision-making in symptomatic anorexia and bulimia nervosa patients: a meta-analysis. Psychol Med. (2015) 45:3377–91. doi: 10.1017/S003329171500152X
36. Wu M, Giel KE, Skunde M, Schag K, Rudofsky G, de Zwaan M, et al. Inhibitory control and decision making under risk in bulimia nervosa and binge-eating disorder. Int J Eat Disord. (2013) 46:721–8. doi: 10.1002/eat.22143
37. Carr MM, Wiedemann AA, Macdonald-Gagnon G, Potenza MN. Impulsivity and compulsivity in binge eating disorder: A systematic review of behavioral studies. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 110:110318. doi: 10.1016/j.pnpbp.2021.110318
38. Bartholdy S, Rennalls S, Danby H, Jacques C, Campbell IC, Schmidt U, et al. Temporal Discounting and the Tendency to Delay Gratification across the Eating Disorder Spectrum. Eur Eat Disord Rev. (2017) 25:344–50. doi: 10.1002/erv.2513
39. Müller A, Brandl C, Kiunke W, Georgiadou E, Horbach T, Köhler H, et al. Food-independent tendency to disadvantageous decisions in obese individuals with regular binge eating. Compr Psychiatry. (2014) 55:64–70. doi: 10.1016/j.comppsych.2013.08.010
40. Amlung M, Marsden E, Holshausen K, Morris V, Patel H, Vedelago L, et al. Delay discounting as a transdiagnostic process in psychiatric disorders: a meta-analysis. JAMA psychiatry. (2019) 76:1176–86. doi: 10.1001/jamapsychiatry.2019.2102
41. Manwaring JL, Green L, Myerson J, Strube MJ, Wilfley DE. Discounting of various types of rewards by women with and without binge eating disorder: evidence for general rather than specific differences. Psychol Rec. (2011) 61:561–82. doi: 10.1007/BF03395777
42. Weller RE, Cook EW, Avsar KB, Cox JE. Obese women show greater delay discounting than healthy-weight women. Appetite. (2008) 51:563–9. doi: 10.1016/j.appet.2008.04.010
43. Davis C, Patte K, Curtis C, Reid C. Immediate pleasures and future consequences. A neuropsychological study of binge eating and obesity. Appetite. (2010) 54:208–13. doi: 10.1016/j.appet.2009.11.002
44. Mole TB, Irvine MA, Worbe Y, Collins P, Mitchell SP, Bolton S, et al. Impulsivity in disorders of food and drug misuse. Psychol Med. (2015) 45:771–82. doi: 10.1017/S0033291714001834
45. Svaldi J, Brand M, Tuschen-Caffier B. Decision-making impairments in women with binge eating disorder. Appetite. (2010) 54:84–92. doi: 10.1016/j.appet.2009.09.010
46. Voon V, Morris LS, Irvine MA, Ruck C, Worbe Y, Derbyshire K, et al. Risk-taking in disorders of natural and drug rewards: neural correlates and effects of probability, valence, and magnitude. Neuropsychopharmacology. (2015) 40:804–12. doi: 10.1038/npp.2014.242
47. Yan WS, Zhang RR, Lan Y, Li ZM, Li YH. Questionnaire-based maladaptive decision-coping patterns involved in binge eating among 1013 college students. Front Psychol. (2018) 9:609. doi: 10.3389/fpsyg.2018.00609
48. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/BF03193146
49. Ricca V, Mannucci E, Moretti S, Di Bernardo M, Zucchi T, Cabras PL, et al. Screening for binge eating disorder in obese outpatients. Compr Psychiatry. (2000) 41:111–5. doi: 10.1016/S0010-440X(00)90143-3
50. Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. (1982) 7:47–55. doi: 10.1016/0306-4603(82)90024-7
51. Greeno CG, Marcus MD, Wing RR. Diagnosis of binge eating disorder: discrepancies between a questionnaire and clinical interview. Int J Eat Disord. (1995) 17:153–60. doi: 10.1002/1098-108X(199503)17:2<153::AID-EAT2260170208>3.0.CO;2-V
52. Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM. On the validity and utility of discriminating among impulsivity-like traits. Assessment. (2007) 14:155–70. doi: 10.1177/1073191106295527
53. Madden GJ, Petry NM, Johnson PS. Pathological gamblers discount probabilistic rewards less steeply than matched controls. Exp Clin Psychopharmacol. (2009) 17:283–90. doi: 10.1037/a0016806
54. Claes L, Islam MA, Fagundo AB, Jimenez-Murcia S, Granero R, Agüera Z, et al. The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLoS ONE. (2015) 10:e0126083. doi: 10.1371/journal.pone.0126083
55. Davis C, Levitan RD, Carter J, Kaplan AS, Reid C, Curtis C, et al. Personality and eating behaviors: a case-control study of binge eating disorder. Int J Eat Disord. (2008) 41:243–50. doi: 10.1002/eat.20499
56. Murphy CM, Stojek MK, MacKillop J. Interrelationships among impulsive personality traits, food addiction, and Body Mass Index. Appetite. (2014) 73:45–50. doi: 10.1016/j.appet.2013.10.008
57. VanderBroek-Stice L, Stojek MK, Beach S, vanDellen MR, MacKillop J. Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite. (2017) 112:59–68. doi: 10.1016/j.appet.2017.01.009
58. Smith GT, Cyders MA. Integrating affect and impulsivity: the role of positive and negative urgency in substance use risk. Drug Alcohol Depend. (2016) 163:S3–12. doi: 10.1016/j.drugalcdep.2015.08.038
59. Quintero MJ, Navas JF, Perales JC. The associative underpinnings of negative urgency and its role in problematic gambling behavior. Addict Behav. (2020) 111:106533. doi: 10.1016/j.addbeh.2020.106533
60. Cyders MA, Smith GT. Clarifying the role of personality dispositions in risk for increased gambling behavior. Pers Individ Dif. (2008) 45:503–8. doi: 10.1016/j.paid.2008.06.002
61. Fischer S, Smith GT, Anderson KG. Clarifying the role of impulsivity in bulimia nervosa. Int J Eat Disord. (2003) 33:406–11. doi: 10.1002/eat.10165
62. Kenny TE, Singleton C, Carter JC. An examination of emotion-related facets of impulsivity in binge eating disorder. Eat Behav. (2019) 32:74–7. doi: 10.1016/j.eatbeh.2018.12.006
63. Um M, Whitt ZT, Revilla R, Hunton T, Cyders MA. Shared neural correlates underlying addictive disorders and negative urgency. Brain Sci. (2019) 9:36. doi: 10.3390/brainsci9020036
64. Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. (2007) 75:629–38. doi: 10.1037/0022-006X.75.4.629
65. Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity-a systematic review. Neurosci Biobehav Rev. (2015) 49:125–34. doi: 10.1016/j.neubiorev.2014.12.008
66. Schag K, Leehr EJ, Meneguzzo P, Martus P, Zipfel S, Giel KE. Food-related impulsivity assessed by longitudinal laboratory tasks is reduced in patients with binge eating disorder in a randomized controlled trial. Sci Rep. (2021) 11:8225. doi: 10.1038/s41598-021-87231-w
67. Lavagnino L, Arnone D, Cao B, Soares JC, Selvaraj S. Inhibitory control in obesity and binge eating disorder: a systematic review and meta-analysis of neurocognitive and neuroimaging studies. Neurosci Biobehav Rev. (2016) 68:714–26. doi: 10.1016/j.neubiorev.2016.06.041
68. Fernie G, Cole JC, Goudie AJ, Field M. Risk-taking but not response inhibition or delay discounting predict alcohol consumption in social drinkers. Drug Alcohol Depend. (2010) 112:54–61. doi: 10.1016/j.drugalcdep.2010.05.011
69. Lejuez CW, Aklin W, Bornovalova M, Moolchan ET. Differences in risk-taking propensity across inner-city adolescent ever- and never-smokers. Nicotine Tobacco Res. (2005) 7:71–9. doi: 10.1080/14622200412331328484
70. McClure SM, York MK, Montague PR. The neural substrates of reward processing in humans: the modern role of FMRI. Neuroscientist. (2004) 10:260–8. doi: 10.1177/1073858404263526
71. Simon JJ, Skunde M, Walther S, Bendszus M, Herzog W, Friederich HC. Neural signature of food reward processing in bulimic-type eating disorders. Soc Cogn Affect Neurosci. (2016) 11:1393–401. doi: 10.1093/scan/nsw049
72. Bodell LP, Wildes JE, Goldschmidt AB, Lepage R, Keenan KE, Guyer AE, et al. Associations between neural reward processing and binge eating among adolescent girls. J Adolesc Health. (2018) 62:107–13. doi: 10.1016/j.jadohealth.2017.08.006
73. Schag K, Schönleber J, Teufel M, Zipfel S, Giel KE. Food-related impulsivity in obesity and binge eating disorder-a systematic review. Obesity reviews. (2013) 14:477–95. doi: 10.1111/obr.12017
74. Strickland JC, Johnson MW. Rejecting impulsivity as a psychological construct: a theoretical, empirical, and sociocultural argument. Psychol Rev. (2021) 128:336–61. doi: 10.1037/rev0000263
Keywords: binge eating disorder, impulsivity, discounting task, BIS-11, UPPS-P
Citation: Yan W-S, Zheng D-H and Liu M-M (2022) Trait Impulsivity and Choice Impulsivity in Young Adult Students With Probable Binge Eating Disorder. Front. Psychiatry 13:838700. doi: 10.3389/fpsyt.2022.838700
Received: 18 December 2021; Accepted: 22 February 2022;
Published: 05 April 2022.
Edited by:
Fabien Gierski, Université de Reims Champagne-Ardenne, FranceReviewed by:
Sabrina Julien Sweerts, Université de Reims Champagne-Ardenne, FranceCopyright © 2022 Yan, Zheng and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wan-Sen Yan, eWFud2Fuc2VuQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.