
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 12 September 2022
Sec. ADHD
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.834356
Objective: Attention-deficit/hyperactivity disorder (ADHD) is associated with a high prevalence of anxiety disorders in children and adolescents. The reasons for this association are poorly understood. Preliminary findings with young adults have suggested that executive functions and functional impairment may mediate the relationship between symptoms of ADHD and mixed anxiety and depressive symptoms. The objective of this study was to explore whether ADHD symptoms, executive functions and functional impairment predict anxiety in a clinical adolescent population. In addition, we investigated the possible mediating role of executive functions and functional impairment in this relationship.
Method: One hundred adolescents with ADHD and their parents completed the ADHD Rating Scale IV (ADHD RS-IV), the Behavior Rating Inventory of Executive Function (BRIEF), and the Weiss Functional Impairment Rating Scale (WFIRS) in relation to an RCT study. The adolescents also completed the Screen for Child Anxiety-Related Emotional Disorders (SCARED). Analyses were conducted using regression and a serial multiple mediator model.
Results: In the regression analyses, parent-rated ADHD symptoms were unable to predict anxiety, but ADHD inattention symptoms predicted anxiety in the self-ratings. Executive dysfunction and functional impairment predicted anxiety in both the parent- and self-reports. In the mediation analyses ADHD symptoms alone did not predict anxiety, but executive dysfunction mediated this relationship as expected. Functional impairment mediated this relationship indirectly through executive functions. The results were similar in the parent- and self- reports.
Conclusion: The results pinpoint executive dysfunction as an important treatment target for alleviating anxiety in adolescents with impairing ADHD symptoms.
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders in childhood (1) and is characterized by developmentally inappropriate levels of inattention, hyperactivity and impulsivity that lead to impairment in at least one life domain (2). Through adolescence, symptoms of ADHD typically impair functioning in various contexts, such as school, social settings, and emotional wellbeing. Comorbid psychiatric conditions are common in this patient group, and anxiety, depression, conduct disorders and substance misuse are among the most common disorders (3–5). Although pharmacological treatment for ADHD has shown beneficial effects on core ADHD symptoms as well as improvements in functional impairment and health-related quality of life (6, 7), the lack of data on longer-term treatment effects makes it unclear whether the changes in health-related quality of life are mediated by symptom changes, changes in functional impairment or other factors.
Anxiety disorders (ADs) are among the most prevalent disorders in child and adolescent populations, and ADHD and AD are comorbid with each other in 25–50% of cases (8–10). This comorbidity rate is greater than chance and is still present after controlling for overlapping symptoms, such as difficulty concentrating and restlessness (11, 12). The presence of both disorders is associated with more attentional problems, school fears and lower social competence than the presence of either ADHD or anxiety alone (8). While there is evidence of a prospective relationship between ADHD and AD across development, the reasons for this association are still unclear. Previous studies have suggested a specific relationship between the ADHD inattentive type and anxiety (9, 13, 14). Similarly, ADHD patients with sluggish (slow) cognitive speed have shown more internalizing symptoms, such as anxiety and depression, than patients with the hyperactive or combined subtype of ADHD (15, 16). Jensen et al. (17) found that anxiety reported in ADHD populations may differ from anxiety in non-ADHD populations, with concerns about competency and performance being the more common components rather than specific phobias per se. This form of anxiety has been suggested to arise primarily when one's cognitive processing abilities are overwhelmed by the demands of the environment (18). Following from this, two possible factors linking ADHD and anxiety are executive functions (EFs) and functional impairment. EFs represent higher-order cognitive processes that help us achieve our daily goals (19–21). EFs are mainly supported by the prefrontal cortex and typically include planning skills, response inhibition, mental flexibility, working memory, initiation and set shifting (22). Dysfunctional EFs may prevent the acquisition and implementation of skills, leading to difficulties handling everyday challenges related to academic functioning (23), interpersonal problems (24), and mental health (25–27). Although dysfunctional EFs are common in ADHD and have been hypothesized to underlie the functional impairments related to this disorder (28, 29), these cognitive dysfunctions are not restricted to ADHD but are rather common in various psychiatric disorders, including mood disorders and ADs (30, 31).
Previous research with university students with ADHD has demonstrated that executive functions may predict functional impairments. Dvorsky and Langberg (32) showed that executive functions, including motivation and emotional regulation skills mediated the association between ADHD symptoms and overall daily functioning. They also found organizational skills to mediate the association between ADHD symptoms and academic achievement rated by grade point average. Dorr and Armstrong (33) found that high executive functions were related to lower levels of functional impairment in patients with low ADHD symptoms, but high EF was not associated with low functional impairment in a sample of university students with a high level of ADHD symptoms. Research conducted with adolescents with ADHD has demonstrated that dysfunctional EFs are related to multiple domains of impairment even after controlling for symptoms of ADHD (23, 34). In particular, the metacognitive aspects of EFs (e.g., mental flexibility, planning and organization) have proven salient for school functioning and homework completion in this age group (34, 35). As children and adolescents with ADHD experience functional impairment in multiple domains, including school, the social arena and family life, they are also more vulnerable to developing low self-esteem. In addition, they are more often involved in risky behavior than their non-ADHD peers (36). Since functional impairment and the accompanying feeling of incompetence may trigger stress and anxiousness, it is important to explore the role of functional impairment in the ADHD- anxiety relationship, as this may guide our understanding of underlying mechanisms for this association and help us develop more targeted treatment interventions for this patient group.
To our knowledge, only one published study has explored the relationship between symptoms of ADHD and mixed anxiety and depressive symptoms with a particular emphasis on EFs and functional impairment. In this study, EFs and functional problems explained 42 to 53% of the variance in mixed anxiety and depressive symptoms in a population of university students (37). A limitation of this study was the lack of a systematic diagnostic assessment in the population.
The aim of the present study was thus to explore whether ADHD symptoms, executive dysfunction and functional impairment predict anxiety in a clinical adolescent population. Specifically, we hypothesize that the effect of ADHD symptoms on anxiety is to some extent mediated through EF or functional impairment (see Figure 1). Based on previous results (37), we expected both EFs and functional impairment to have a mediating effect on the ADHD-anxiety relationship.
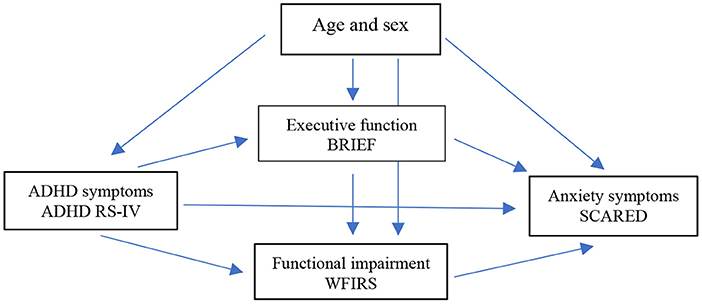
Figure 1. Hypothetic relationships among ADHD symptoms, functional impairment, executive dysfunction, and anxiety symptoms with the accompanying measurements. Age and sex are potential confounders.
This observational study was conducted in Mid-Norway. The data were derived from a randomized controlled trial (RCT) examining the efficacy of cognitive behavioral group therapy as a follow-up treatment in a sample of adolescents with ADHD who previously received a short psychoeducational intervention and were medicated but still presented impairing ADHD symptoms (38). We refer readers to this published study and the study protocol for more details about the procedures (38, 39). Recruitment and data collection began in February 2017, and the last data were collected in September 2019. Written informed consent was obtained from the adolescents and from parents for participants under 16 years of age. The questionnaires were completed under the surveillance of a research assistant. Parent-rated questionnaires were completed by the primary caregiver, usually the mother. The study was approved by the Regional Committee for Medical and Health Research Ethics in Southeast Norway (2015/2115). The present study uses baseline data from the RCT.
See Table 1 for the participant characteristics. The participants were between the ages of 14 and 18 years and were recruited from two outpatient child and adolescent psychiatry (CAP) units at St. Olavs Hospital. The participants had received a prior diagnosis of hyperkinetic disorder by a certified psychologist or a psychiatrist according to the International Statistical Classification of Disease and Related Health Problems (ICD-10) criteria (40). The assessment and diagnosis of hyperkinetic disorder requires a thorough clinical assessment, including a developmental history, a somatic assessment, and an examination of comorbid psychiatric disorders, and the use of questionnaires to assess ADHD symptoms (ADHD rating scale), which were completed by adolescents, parents, and teachers. The diagnostic criteria for hyperkinetic disorder in ICD-10 resemble the criteria for ADHD combined presentation in the Diagnostic and Statistical Manual of Mental Disorder 5th edition (DSM-5). According to Norwegian ADHD guidelines (41), hyperkinetic disorder may also be diagnosed in patients with severe inattention symptoms, similar to the DSM-5 ADHD inattentive type. At study enrolment, each participant was interviewed with the Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version (Kiddie-SADS-PL) at the CAP units to confirm the ADHD symptoms and assess psychiatric comorbidity. The ADHD symptoms were confirmed by a parent rater within the last 3 years of inclusion for 94% of the population. Ninety-one percent of the participants were receiving pharmacological treatment for ADHD. Ninety-two percent had previously received a short psychoeducational intervention of 1–5 h, which typically consisted of information about ADHD diagnosis, symptoms, causes, and treatment options delivered by the patient‘s clinician to the patient with and/or without parents. Parents and a schoolteacher of each participant were also offered a standardized full-day lecture, with information about ADHD, pharmacotherapy, psychosocial interventions, and school interventions. Seventy-two percent of the participants attended this lecture. All the participants had previously had a collaborative meeting with the patient‘s parents and a schoolteacher to discuss supportive measures in school. These interventions were all completed before the baseline collection of data used in the present study.
The socioeconomic status (SES) of the participants refers to the highest level of education reported by one or both parents (n = 75, 75%). This information was retrieved from the participants‘ medical records. Nineteen percent reported that they had an education lower than elementary school or 1–2 years of high school (0–11 years), seven percent completed high school and/or 1 year of training after high school (12–13 years), thirty percent had an academy or university degree for up to 4 years (14–15 years), and nineteen percent confirmed an academy/ university degree for 4 years or more (16 years and more).
The ADHD Rating Scale IV (ADHD RS-IV) (42) was used to measure the ADHD symptoms of the participants. We used the parent and self-report versions in this study. The ADHD RS-IV is an 18-item scale that assesses nine symptoms of inattention and nine symptoms of hyperactivity. The items correspond to the DSM-5 ADHD diagnostic criteria, including the combined and predominantly inattentive and hyperactive presentations. Item responses are scored from 0 = not at all to 3 = very often, with higher scores indicating more symptoms. The questionnaire has been validated for patients with ADHD aged 6–18 years across several European countries, including Norway, with impressive evidence for cross-factorial cultural validity, internal consistency, and convergent and divergent validity (43). Cronbach's α = 0.78 to 0.81 on the ADHD RS-IV parent version and 0.80 to 0.84 on the self-report version were reported in the present study.
The Screen for Child Anxiety-Related Emotional Disorders (SCARED) (44) was used to measure anxiety symptoms. The SCARED is a 41-item self-report screening instrument that measures anxiety symptoms in children and adolescents aged 8 to 18 years. In addition to a total scale score, the instrument contains five subscales representing diagnostic symptoms of panic disorder, generalized anxiety, separation anxiety, social phobia, and school phobia. Item responses are scored from 0 = not at all to 2 = often, and a total score ≥ 25 may indicate the presence of an anxiety disorder (45). The SCARED has shown good internal consistency and moderate parent-child correlations. The instrument is sensitive to detecting specific and/or comorbid anxiety diagnoses in children and adolescents (45). A study among Norwegian high school students found acceptable internal consistency (Cronbach‘s α = 0.62 to 0.87) for the SCARED subscales (46). Cronbach‘s α = 0.95 for the SCARED total score was reported in the current study.
The Behavior Rating Inventory of Executive Function (BRIEF) (22) assesses EF behaviors in children and adolescents at home and at school. The BRIEF includes an 86-item parent version (BRIEF-P) for children and adolescents aged 6–18 years and an 80-item self-report (BRIEF-SR) for children and adolescents aged 11–18 years (47). Both questionnaires contain a metacognitive index (MI), a behavior regulation index (BRI) and a global executive composite (GEC) score that represents the total scale score. The BRIEF-P and BRIEF-SR contain the following MI subscales: working memory, planning/organizing, organization of material and task completion. The BRI includes the following subscales: inhibit, shift and emotional control. Item responses are scored from 0 = not true to 2 = very true, with higher scores representing more severe dysfunction. According to the BRIEF manual, a total T-score above 65 indicates executive dysfunction. In this study, we used the MI, BRI and GEC scores. The BRIEF-P has shown good psychometric properties in a Norwegian child and adolescent population (48). Fallmyr and Egeland (48) found the Norwegian and American norms to be compatible, the questionnaire showed a good ability to discriminate between a normative population and a clinical ADHD population, and the internal consistency was acceptable (Cronbach's α = 0.76 to 0.92). The BRIEF-SR has shown acceptable psychometric properties in an American adolescent population, with α = 0.96 for the GEC and α = 0.72 to 0.96 for the clinical scales. Interrater reliability between the GEC of the BRIEF-P and the GEC of the BRIEF-SR was strong (r = 0.56) (47).
The Weiss Functional Impairment Rating Scale parent-report (WFIRS-P) and self-report (WFIRS-S) versions (49) assess functional impairment in different domains typically affected in ADHD. The WFIRS-P and WFIRS-S consist of 50 and 69 items, respectively, divided into six and seven domains of impairment. The domains include family, school and learning, life skills, self-concept, social activities, and risky activities. The WFIRS-P and WFIRS-S are not parallel forms, but there are many parallel items. Item responses are scored from 0 = not at all to 3 = very often and 4 = not applicable, with higher scores indicating more impairment. In this study, a total mean score was calculated, representing the sum of the mean domain scores. Items with a missing or “not applicable” response were omitted. Any domain with a mean score > 1.5, two items with a score ≥ 2, or one item with a score = 3 is considered clinically impaired. The WFIRS scales have shown acceptable psychometric properties in a Norwegian adolescent ADHD population (50). In the present study, Cronbach's α was r = 0.62 to 0.88 for the WFIRS-P subscales and 0.70 to 0.92 for the WFIRS-S subscales.
We conducted regression analyses to analyse the individual contributions of parent-rated and self-rated ADHD symptoms, executive dysfunction, and functional impairment to the severity of adolescent-rated anxiety symptoms in separate analyses. First, the ADHD RS-IV total score; the ADHD RS inattentive and the hyperactivity subscale scores; the BRIEF GEC, BRI and MI indices; and the WFIRS total score were entered one by one as independent variables, with the SCARED total score as the dependent variable. Second, to explore which of the subscales or indices from the ADHD RS-IV and the BRIEF questionnaire that predict anxiety the most while controlling for the other questionnaire subscale, we carried out two separate regression analyses: first with the two ADHD RS-IV subscales simultaneously and second with the two BRIEF indices simultaneously. Multicollinearity was checked to avoid high correlations (r =0.70 and above) between the independent variables, as recommended by Dormann et al. (51). The normality of residuals was checked by visual inspection of QQ plots.
To explore whether EFs and functional impairment act as mediators in the association between ADHD symptoms and anxiety, we conducted a serial multiple mediator model recommended by Hayes (52) using the PROCESS macro for IBM SPSS (www.processmacro.org). The PROCESS command generates bootstrap confidence intervals (CIs) for all indirect effects as well as possible pairwise comparisons between indirect effects. We used 5,000 bootstrap samples. The ADHD RS total score was entered as the predictor variable (X), the BRIEF GEC score was entered as the first mediator (M1), and the WFIRS total score was entered as the second parallel mediator (M2) (see Figures 2, 3). The adolescent- rated SCARED total score was the outcome variable in both mediation analyses. The analyses were conducted using parent- and self-report questionnaires in separate analyses. Age and sex were considered confounders and entered as covariates in all the analyses. In addition, we carried out supplementary analyses also adjusting for IQ and SES. These analyses were restricted to the 62 participants in the regression analyses and 58 and 52 participants in the mediation analyses using parent- and self-reports, respectively, with available data on these variables. The estimated effects were essentially the same (data not shown). Missing data were handled using single imputation on scales using the mean score if 70% or more of the questions were answered. Otherwise, the outcome of that specific questionnaire for that participant was treated as missing. For the rest, we handled missing data using available case analyses, including in each analysis the cases with data on the variables in the analysis. We report 95% CIs where relevant. To reduce the risk of false-positive findings due to multiple hypotheses, two-sided p-values ≤ 0.01 are regarded as significant. This approach is suggested by Lydersen (53). Statistical analyses were conducted using SPSS 26.
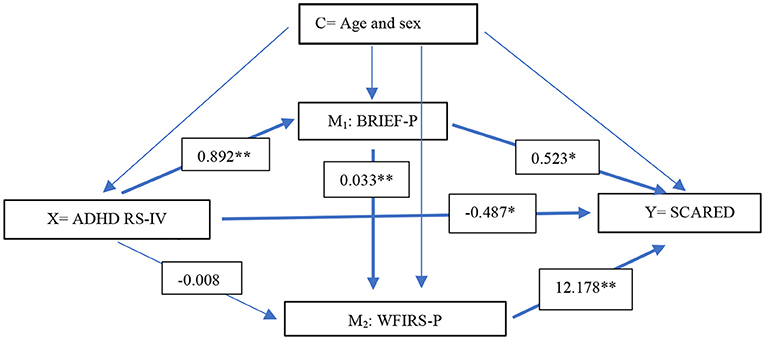
Figure 2. Regression coefficients for the associations between parent-report measures of ADHD RS-IV and SCARED (self-report) with BRIEF and WFIRS as possible mediators. Age and sex were considered confounders (n = 90). X predictor, Y dependent variable, C confounder, M1 mediator 1, M2 mediator 2. ADHD RS-IV Attention-Deficit/Hyperactivity Disorder Rating Scale, BRIEF-P Behavior Rating Inventory of Executive Function Parent version, WFIRS Weiss Functional Impairment Rating Scale. ** p < 0.005, * p < 0.05.
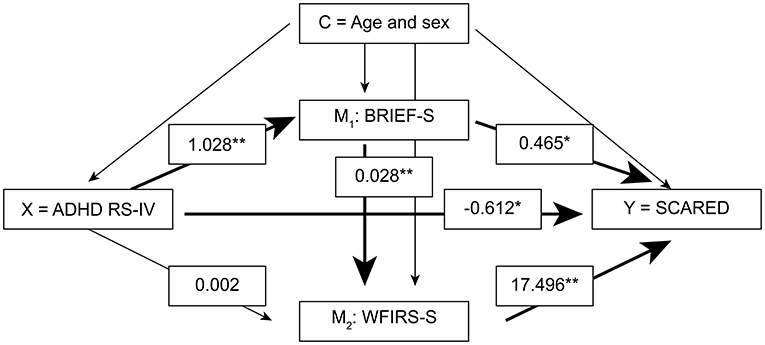
Figure 3. Regression coefficients for the associations between self-report measures of ADHD RS-IV and SCARED with BRIEF and WFIRS as possible mediators. Age and sex were considered confounders (n = 81). X predictor, Y dependent variable, C confounder, M1 mediator 1, M2 mediator 2, ADHD RS-IV Attention-Deficit/Hyperactivity Disorder Rating Scale, BRIEF-S Behavior Rating Inventory of Executive Function Self-report, WFIRS Weiss Functional Impairment Rating Scale Self-report. ** p < 0.005, * p < 0.05.
The 100 participants included 57 females and 43 males; the mean age was 15.8 years (SD = 1.3). When collecting the data, ninety-one percent of the participants were stably taking ADHD medication. Nevertheless, sixty-six percent of participants met the DSM-5 criteria for an ADHD diagnosis (35% predominantly inattentive presentation and 31% combined presentation), and 33% presented subthreshold symptoms of ADHD (all ADHD medicated). Fifty-three percent of the participants had at least one current comorbid condition; among them, 37% had an AD according to the DSM-5 criteria (see Table 1).
The results from the regression analyses using parent-ratings of the ADHD RS-IV, the BRIEF and the WFIRS to predict anxiety symptoms measured with the SCARED self-report, controlling for age and sex, are presented in Table 2. In step 1, neither the ADHD total score, nor the subscale scores were able to predict anxiety. All the BRIEF indices, including the GEC (p = 0.002), the BRI (p = 0.010) and the MI (p = 0.003) significantly predicted anxiety, as did the WFIRS total score (p < 0.001).
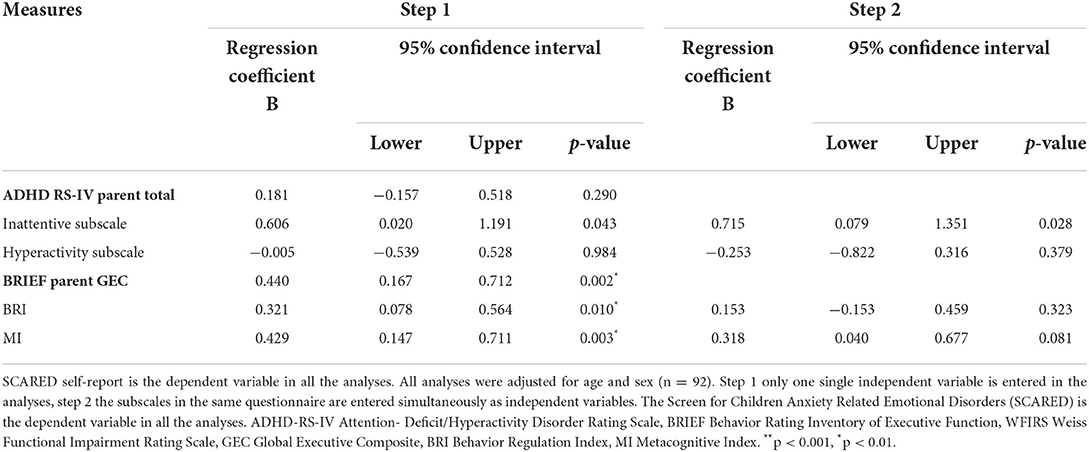
Table 2. Results from regression analysis using the parent-rated ADHD RS-IV, BRIEF and WFIRS measures as independent variables entered in two steps.
In step 2 of Table 2, we examined the ability of the ADHD RS-IV subscale scores and the BRIEF indices to predict anxiety when controlling for age, sex, and the companion subscale or index score. The results showed that neither the ADHD subscales nor the BRIEF indices were able to predict anxiety when controlling for age, sex, and the companion subscale.
The results from the regression analyses using self-ratings of the ADHD RS-IV, the BRIEF and the WFIRS to predict anxiety symptoms measured with SCARED, controlling for age and sex, are presented in Table 3. In step 1, the ADHD inattentive subscale score was significantly able to predict anxiety (p = 0.002). Among the BRIEF indices, the GEC, MI, and BRI predicted anxiety (p ≤ 0.001), as did the total score of the WFIRS (p < 0.001).
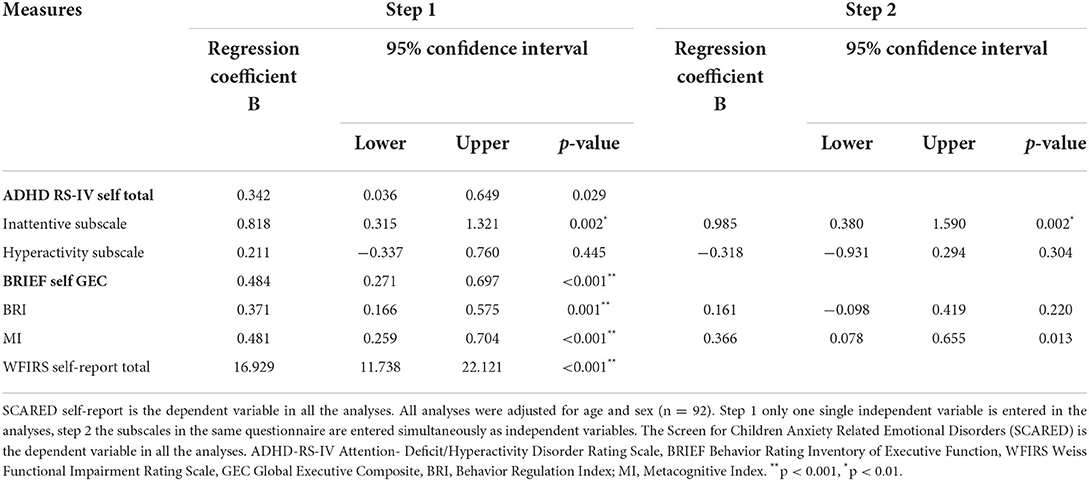
Table 3. Results from regression analyses using self-report measures of the ADHD RS-IV, BRIEF and WFIRS measures entered as independent variables in two steps.
In step 2 of Table 3, we examined the ability of the ADHD RS-IV subscale scores and the BRIEF indices to predict anxiety when controlling for age, sex, and the companion subscale or index score. The results showed that the ADHD inattention score was able to predict anxiety when controlling for the hyperactive subscale score. The BRIEF indices were unable to predict anxiety when controlling for each other.
Regression coefficients presenting the direct effects between the parent-rated variables are presented in Figure 2. The total direct and indirect effects between the variables are presented in Supplementary Table S4. The direct effect of ADHD symptoms predicting anxiety was negative but significant (coefficient = −0.487, p = 0.048); thus, a low ADHD symptom score significantly predicted more severe symptoms of anxiety when EFs and functional impairment were controlled for. The first indirect effect of only EF mediating the association between ADHD symptoms and anxiety was significantly positive (coefficient = 0.466, CI 0.013 to 1.024). Thus, levels of ADHD symptoms predicted levels of executive dysfunction, which again mediated the severity of anxiety symptoms. The second indirect effect was through levels of functional impairment only, which was negative and non-significant (coefficient = −0.101, CI:−0.275 to 0.0241). The third indirect effect of executive dysfunction and functional impairment in serial (X- M1- M2-Y) was positive and significant (coefficient = 0.362, CI: 0.087 to 0.665); thus, the association between ADHD symptoms and anxiety seems to be mediated by EFs affecting functional impairment, which in turn mediates symptoms of anxiety. This was found regardless of age, sex, IQ, and SES.
Regression coefficients presenting the direct effects between the self-rated variables are presented in Figure 3. The total direct and indirect effects between the variables are presented in Supplementary Table S5. The results from the self-report measures were similar to the results from the parent reports, showing a negative but significant direct effect of ADHD symptoms predicting anxiety (coefficient = −0.612, p = 0.007). The first indirect effect via executive dysfunction alone was positive and significant (coefficient = 0.478, CI: 0.025 to 0.947), while the second indirect effect via functional impairment alone was non-significant (coefficient = 0.035, CI:−0.199 to 0.261). The serial indirect effect of executive dysfunction and functional impairment on the association between ADHD and anxiety was positive and significant (coefficient = 0.501, CI: 0.203 to 0.889), and the results were similar to the analyses with the parent reports.
Children and adolescents with ADHD have an increased risk of comorbid ADs compared to their non-ADHD peers. In addition, anxiety symptoms tend to have an earlier onset, be more severe and be frequently associated with other psychiatric conditions (54, 55). Although the comorbidity rates of ADHD and ADs are well documented, the etiology of these associations is poorly understood. As such, the first aim of the current study was to examine whether parent- and self-rated ADHD symptoms, executive dysfunction and functional impairment were able to predict anxiety in a clinical population of adolescents with symptoms of ADHD. Overall, the main patterns were similar in the adolescent and parent reports, with stronger associations in the self-reports. This finding was as expected, considering that anxiety is an internalizing disorder and that only the adolescents reported anxiety symptoms. Among the self-rated ADHD symptom scores, only the inattention domain predicted anxiety, while hyperactivity symptoms were unable to predict anxiety. This was found regardless of age and sex and is in line with previous studies showing inattention symptoms to be more strongly associated with anxiety than hyperactivity (14, 56). On the other hand, none of the parent-rated ADHD symptom scores were able to predict anxiety. This was somewhat surprising and might suggest that parents are less sensitive in capturing this symptom association, perhaps because of the less overt nature of both inattention symptoms and anxiety symptoms. On the other hand, only including a self-report measure of anxiety could have affected this finding.
Among the EFs, both the global executive composite (GEC), the behavioral regulation index (BRI) and the metacognitive index (MI) were able to predict anxiety in both self- and parent-reports. Neither the BRI nor the MI index was significantly able to predict anxiety over and above the other BRIEF index when controlling for age and sex. The behavioral regulation index reflects both emotional dysregulation, mental inflexibility and impulsivity. An association between emotional dysregulation and anxiety would be expected. In addition, an association between mental inflexibility and anxiousness has previously been found in studies examining measures of shifting and updating using neurocognitive measures on clinical and non-clinical samples of anxious children and adolescents (57–59). Impulsivity, on the other hand, has previously been shown to be inversely associated with anxiety, with studies showing less inhibited children and adolescents presenting lower symptoms of anxiety than more inhibited children (60, 61). More detailed subgroup analyses are recommended to explore these associations further.
The metacognitive index includes cognitive functions such as working memory, task completion, planning and organization, and organization of materials, all skills strongly related to school performance and the attainment of future goals. As such, it is reasonable to link experienced difficulties in these areas with both low self-esteem and lack of control, which again may increase anxiousness. Finally, the functional impairment score, representing self-concept, social activities, school functioning, life skills and risky activities, predicted anxiety in both the parent- and self-reports. In sum, both executive dysfunction related to behavior regulation and metacognitive functions and functional impairment may be important to assess when working with adolescents with ADHD and comorbid anxiety.
The second aim of this study was to explore the roles of executive dysfunction and functional impairment as possible mediators in the ADHD-anxiety relationship. The results from the mediation analyses showed that ADHD symptoms alone were unable to predict anxiety when controlling for executive dysfunction and functional impairment. Executive dysfunction mediated the ADHD-anxiety pathway, as expected; thus, more ADHD symptoms significantly predicted more severe executive dysfunction, which mediated the severity of anxiety symptoms. This pattern was found when controlling for age and sex and was similar in both parent- and self-reports, strengthening the validity of the result. This result was similar to a previous study (37) where EFs and functional impairment explained most of the variance in combined anxiety and depressive symptoms in college students with ADHD. Another recent study found that EFs and anxiety/depression significantly mediate the relationship between ADHD and quality of life (62). Together, these results suggest that executive dysfunctions rather than ADHD symptoms per se may lead to comorbid anxiety or mood disorders and difficulties in daily life. In the current study, ADHD symptoms alone were unable to predict functional impairment, but functional impairment predicted anxiety. Functional impairment was thus unable to mediate the ADHD-anxiety relationship by itself but acted as a mediator through EFs. Executive dysfunction has previously been linked to functional impairment in both school and social settings in children and adolescents with ADHD (63, 64). Rosellȯ et al. (65) found impulsivity/emotional lability as well as planning and organizing to be significant predictors of functional impairment in family, social, academic, and risky activity areas in young adults with ADHD. Shift and working memory marginally predicted impairment in the same areas. These findings suggest executive dysfunction to be an important target in the prevention of functional impairment across several life domains.
This study has several strengths. First, this was the first study to explore the mediating effect of EFs and functional impairment on the ADHD-anxiety relationship in a clinical adolescent population. Second, we included ADHD patients with common psychiatric comorbidities, which increases the generalizability of the results to a clinical CAP setting. Third, the use of both parent- and self-report measures improves the validity of the results. Finally, males and females were equally represented among the participants, which is positive when controlling for the possible moderating effect of sex on the ADHD-anxiety relationship. This study also has several limitations. First, most of the participants (91.0%) were on ADHD medication when completing the questionnaires; thus, the results may not be representative of adolescents with ADHD who are not on medication. Second, the participants showed subthreshold ADHD symptoms, which may limit the generalizability to participants with more severe symptoms. Third, data on ADHD symptoms, executive functions and functional impairments were restricted to parent- and self-report questionnaires. The additional use of neurocognitive measures and computer tests to assess inattention symptoms and executive functions could have added valuable supplemental information in this study. Fourth, a high correlation between the main index scores (see Supplementary Table S6) indicates some conceptual overlap between the EF and functional impairment questionnaires. The two measures, however, also represent distinct, non-overlapping problem areas, making each questionnaire valuable as a clinical assessment instrument. Fifth, since this is a cross-sectional observational study, we have no longitudinal data to explore different developmental pathways related to the included variables. Moreover, the inclusion of only quantitative data limits an in-depth understanding of the origin and consequence of the different associations between cognitive functions/ADHD symptoms, functional impairments, and anxiety in this adolescent population. The inclusion of qualitative methods, such as interviewing parents and adolescents about life conditions, symptom development, psychosocial treatment and medication effects, could improve our knowledge of these associations for different patient groups and is recommended for use in future studies.
In this study, ADHD inattention symptoms, executive functions and functional impairment predicted anxiety in a clinical adolescent population with ADHD symptoms. ADHD core symptoms were, however, not able to predict anxiety when controlling for executive functions and functional impairment in a mediation analysis. Executive dysfunction acted as a substantial mediator in this relationship, while functional impairment mediated this relationship only through EFs. This result pinpoints executive dysfunction as an important treatment target in alleviating anxiety in adolescents with impairing ADHD symptoms. Thus, the additional assessment of EFs using a broadband questionnaire such as the BRIEF parent- and self-report versions is recommended when assessing ADHD and comorbid disorders in adolescent populations. The results also suggest that adolescents with ADHD with normal EFs may have a lower risk of experiencing anxiety. These results improve our knowledge of the association between ADHD and anxiety in a clinical ADHD population. More studies are needed to replicate these findings across different age groups.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Regional Committee for Medical and Health Research Ethics in Southeast Norway (2015/2115). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
TN, PT, and SL supervised A-LH. A-LH drafted the paper and performed the statistical analyses with the supervision of SL. All authors contributed to the research design, provided substantial contributions to the paper, and read and approved the final version of the manuscript.
The study was funded by a PhD grant to A-LH by the Regional Centre for Child and Youth Mental Health and Child Welfare (RKBU), Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology (NTNU). The study received additional funding from the Child and Adolescent Psychiatric Clinic, St. Olav's University Hospital; the Regional Network for Autism, ADHD, and Tourette syndrome, Mid-Norway Health Trust; the National Research Network for ADHD, Ullevål University Hospital, Oslo; and the Regional Competence Network for ADHD, RKBU, NTNU.
The authors are grateful for the contribution of Eirin-Katrine Støkkan and her support in gathering patient data. The authors also thank the patients and parents participating in the study.
Authors A-LH, AS, and TN have received a speaker's fee and a travel honorarium from Medice during the last 3 years. Author PT has received speakers fee from Medice and Takeda within last 3 years. Author PT has received royalties from several publishers for books on ADHD and related disorders.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.834356/full#supplementary-material
ADHD, Attention-deficit/hyperactivity disorder; ADHD-RS IV, ADHD Rating Scale IV; BRIEF, The Behavior Rating Inventory of Executive Function; CAP, Child and Adolescent Psychiatry; CI, Confidence Intervals; EF, Executive Functions; GAD, Generalized Anxiety Disorder; SCARED, The Screen for Child Anxiety-Related Emotional Disorders; WFIRS-P/-S, Weiss Functional Impairment Rating Scale parent-report/self-report versions.
1. Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. (2019) 144:e20192528. doi: 10.1542/peds.2019-2528
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Publishing (2013). doi: 10.1176/appi.books.9780890425596
3. Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med. (2006) 36:167–79. doi: 10.1017/S0033291705006410
4. Powell V, Riglin L, Hammerton G, Eyre O, Martin J, Anney R, et al. What explains the link between childhood ADHD and adolescent depression? investigating the role of peer relationships and academic attainment. Eur Child Adolesc Psychiatry. (2020) 29:1581–91. doi: 10.1007/s00787-019-01463-w
5. Reale L, Bartoli B, Cartabia M, Zanetti M, Costantino MA, Canevini MP, et al. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry. (2017) 26:1443–57. doi: 10.1007/s00787-017-1005-z
6. Chang Z, Ghirardi L, Quinn PD, Asherson P, D'Onofrio BM, Larsson H. Risks and benefits of attention-deficit/hyperactivity disorder medication on behavioral and neuropsychiatric outcomes: a qualitative review of pharmacoepidemiology studies using linked prescription databases. Biol Psychiatry. (2019) 86:335–43. doi: 10.1016/j.biopsych.2019.04.009
7. Coghill D. The impact of medications on quality of life in attention-deficit hyperactivity disorder: a systematic review. CNS Drugs. (2010) 24:843–66. doi: 10.2165/11537450-000000000-00000
8. Bowen R, Chavira DA, Bailey K, Stein MT, Stein MB. Nature of anxiety comorbid with attention deficit hyperactivity disorder in children from a pediatric primary care setting. Psychiatry Res. (2008) 157:201–9. doi: 10.1016/j.psychres.2004.12.015
9. March JS, Swanson JM, Arnold LE, Hoza B, Conners CK, Hinshaw SP, et al. Anxiety as a predictor and outcome variable in the multimodal treatment study of children with ADHD (MTA). J Abnorm Child Psychol. (2000) 28:527–41. doi: 10.1023/A:1005179014321
10. Steinhausen HC, Nøvik TS, Baldursson G, Curatolo P, Lorenzo MJ, Rodrigues Pereira R, et al. Co-existing psychiatric problems in ADHD in the ADORE cohort. Eur Child Adolesc Psychiatry. (2006) 15:I25–I9. doi: 10.1007/s00787-006-1004-y
11. Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. (1999) 40:57–87. doi: 10.1111/1469-7610.00424
12. Tannock R. Attention-deficit disorders and comorbidities in children, adolescents, and adults. In: Brown T, editor. Attention-Deficit/Hyperactivity Disorders With Anxiety Disorders. Washington, DC: American Psychiatric Press (2000). p. 125–70.
13. Biederman J, Petty C, Fried R, Fontanella J, Doyle AE, Seidman LJ, et al. Impact of psychometrically defined deficits of executive functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry. (2006) 163:1730–8. doi: 10.1176/ajp.2006.163.10.1730
14. Koyuncu A, Ertekin E, Yüksel Ç, Aslantaş Ertekin B, Çelebi F, Binbay Z, et al. Predominantly inattentive type of ADHD is associated with social anxiety disorder. J Atten Disord. (2014) 19:856–64. doi: 10.1177/1087054714533193
15. Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, et al. The internal, external, and diagnostic validity of sluggish cognitive tempo: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. (2016) 55:163–78. doi: 10.1016/j.jaac.2015.12.006
16. Hartman CA, Willcutt EG, Rhee SH, Pennington BF. The relation between sluggish cognitive tempo and DSM-IV ADHD. J Abnorm Child Psychol. (2004) 32:491–503. doi: 10.1023/B:JACP.0000037779.85211.29
17. Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, et al. ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry. (2001) 40:147–58. doi: 10.1097/00004583-200102000-00009
18. Schachar R, Tannock R, Marriott M, Logan G. Deficient inhibitory control in attention deficit hyperactivity disorder. J Abnorm Child Psychol. (1995) 23:411–37. doi: 10.1007/BF01447206
19. Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. (1997) 121:65–94. doi: 10.1037/0033-2909.121.1.65
20. Biederman J, Petty CR, Fried R, Doyle AE, Spencer T, Seidman LJ, et al. Stability of executive function deficits into young adult years: a prospective longitudinal follow-up study of grown up males with ADHD. Acta Psychiatr Scand. (2007) 116:129–36. doi: 10.1111/j.1600-0447.2007.01008.x
21. Bloemen AJP, Oldehinkel AJ, Laceulle OM, Ormel J, Rommelse NNJ, Hartman CA. The association between executive functioning and psychopathology: general or specific? Psychol Med. (2018) 48:1787–94. doi: 10.1017/S0033291717003269
22. Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function Professional Maual. Odessa, Florida: Psychological Assessment Resources (2000). doi: 10.1076/chin.6.3.235.3152
23. Miller M, Nevado-Montenegro AJ, Hinshaw SP. Childhood executive function continues to predict outcomes in young adult females with and without childhood-diagnosed ADHD. J Abnorm Child Psychol. (2012) 40:657–68. doi: 10.1007/s10802-011-9599-y
24. Sprague J, Verona E, Kalkhoff W, Kilmer A. Moderators and mediators of the stress-aggression relationship: executive function and state anger. Emotion. (2011) 11:61–73. doi: 10.1037/a0021788
25. Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. (2009) 23:315–36. doi: 10.1037/a0014708
26. Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychol Bull. (2013) 139:81–132. doi: 10.1037/a0028727
27. Snyder HR, Kaiser RH, Whisman MA, Turner AEJ, Guild RM, Munakata Y. Opposite effects of anxiety and depressive symptoms on executive function: the case of selecting among competing options. Cogn Emot. (2014) 28:893–902. doi: 10.1080/02699931.2013.859568
28. Barkley RA, Fischer M. Predicting impairment in major life activities and occupational functioning in hyperactive children as adults: self-reported executive function (EF) deficits versus EF tests. Dev Neuropsychol. (2011) 36:137–61. doi: 10.1080/87565641.2010.549877
29. Barkley RA. The executive functions and self-regulation: an evolutionary neuropsychological perspective. Neuropsychol Rev. (2001) 11:1–29. doi: 10.1023/A:1009085417776
30. Millan MJ, Agid Y, Brüne M, Bullmore ET, Carter CS, Clayton NS, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. (2012) 11:141–68. doi: 10.1038/nrd3628
31. Snyder HR, Miyake A, Hankin BL. Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Front Psychol. (2015) 6:328. doi: 10.3389/fpsyg.2015.00328
32. Dvorsky MR, Langberg JM. Predicting impairment in college students with ADHD: the role of executive functions. J Atten Disord. (2019) 23:1624–36. doi: 10.1177/1087054714548037
33. Dorr MM, Armstrong KJ. Executive functioning and impairment in emerging adult college students with ADHD symptoms. J Atten Disord. (2019) 23:1759–65. doi: 10.1177/1087054718787883
34. Langberg JM, Dvorsky MR, Evans SW. What specific facets of executive function are associated with academic functioning in youth with attention-deficit/hyperactivity disorder? J Abnorm Child Psychol. (2013) 41:1145–59. doi: 10.1007/s10802-013-9750-z
35. Jacobson LA, Williford AP, Pianta RC. The role of executive function in children's competent adjustment to middle school. Child Neuropsychology. (2011) 17:255–80. doi: 10.1080/09297049.2010.535654
36. Franke B, Michelini G, Asherson P, Banaschewski T, Bilbow A, Buitelaar JK, et al. Live fast, die young? a review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. (2018) 28:1059–88. doi: 10.1016/j.euroneuro.2018.08.001
37. Mohamed SMH, Börger NA, Van der Meere JJ. Executive and daily life functioning influence the relationship between ADHD and mood symptoms in university students. J Atten Disord. (2020) 25:1731–42. doi: 10.1177/1087054719900251
38. Haugan AJ, Sund AM, Young S, Thomsen PH, Lydersen S, Nøvik TS. Cognitive behavioural group therapy as addition to psychoeducation and pharmacological treatment for adolescents with ADHD symptoms and related impairments: a randomised controlled trial. BMC Psychiatry. (2022) 22:375. doi: 10.1186/s12888-022-04019-6
39. Novik TS, Haugan AJ, Lydersen S, Thomsen PH, Young S, Sund AM. Cognitive-behavioural group therapy for adolescents with ADHD: study protocol for a randomised controlled trial. BMJ Open. (2020) 10:e032839. doi: 10.1136/bmjopen-2019-032839
40. World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth revision. World Health Organization (1992).
41. Helsedirektoratet. ADHD Nasjonal faglig retningslinje 2016. (2018). Available online at: https://www.helsedirektoratet.no/retningslinjer/adhd (accessed October 27, 2020).
42. DuPaul GJ, Anastopoulos AD, Power TJ, Reid R, Ikeda MJ, McGoey KE. Parent ratings of attention-deficit/hyperactivity disorder symptoms: factor structure and normative data. J Psychopathol Behav Assess. (1998) 20:83–102. doi: 10.1023/A:1023087410712
43. Dopfner M, Steinhausen HC, Coghill D, Dalsgaard S, Poole L, Ralston SJ, et al. Cross-cultural reliability and validity of ADHD assessed by the ADHD rating scale in a Pan-European study. Eur Child Adolesc Psychiatry. (2006) 15:I46–55. doi: 10.1007/s00787-006-1007-8
44. Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. (1997) 36:545–53. doi: 10.1097/00004583-199704000-00018
45. Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. (1999) 38:1230–6. doi: 10.1097/00004583-199910000-00011
46. Ingul JM, Klöckner CA, Silverman WK, Nordahl HM. Adolescent school absenteeism: modelling social and individual risk factors. Child Adolesc Ment Health. (2012) 17:93–100. doi: 10.1111/j.1475-3588.2011.00615.x
47. Guy SC, Isquith PK, Gioia GA. Behavior Rating Inventory of Executive Function-Self-Report Version Professional Manual. Odessa, FL: Psychological Aassessment Resources (2004).
48. Fallmyr O, Egeland J. Psychometric properties of the Norwegian version of BRIEF-for children from 5 to 18 years old. Tidsskrift for Norsk Psykologforening. (2011) 48:339–43.
49. Canadian Attention Deficit Hyperactivity Disorder Resource Alliance. Canadian ADHD Practice Guidelines. Toronto, ON: CADDRA (2011).
50. Haugan AJ, Sund AM, Thomsen PH, Lydersen S, Nøvik TS. Psychometric properties of the weiss functional impairment rating scale parent and self-reports in a Norwegian clinical sample of adolescents treated for ADHD. Nord J Psychiatry. (2020) 75:63–72. doi: 10.1080/08039488.2020.1795252
51. Dormann CF, Elith J, Bacher S, Buchmann C, Carl G, Carré G, et al. Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. (2013) 36:27–46. doi: 10.1111/j.1600-0587.2012.07348.x
52. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Second ed. New York, London: Guilford Press (2017).
53. Lydersen S. Adjustment of p-values for multiple hypotheses. Tidsskriftet Den norske legeforening (2021). doi: 10.4045/tidsskr.21.0357
54. D'Agati E, Curatolo P, Mazzone L. Comorbidity between ADHD and anxiety disorders across the lifespan. Int J Psychiatry Clin Pract. (2019) 23:238–44. doi: 10.1080/13651501.2019.1628277
55. Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. (2017) 17:302. doi: 10.1186/s12888-017-1463-3
56. Newcorn JH, Halperin JM, Jensen PS, Abikoff HB, Arnold LE, Cantwell DP, et al. Symptom profiles in children with ADHD: effects of comorbidity and gender. J Am Acad Child Adolesc Psychiatry. (2001) 40:137–46. doi: 10.1097/00004583-200102000-00008
57. Toren P, Sadeh M, Wolmer L, Eldar S, Koren S, Weizman R, et al. Neurocognitive correlates of anxiety disorders in children: a preliminary report. J Anxiety Disord. (2000) 14:239–47. doi: 10.1016/S0887-6185(99)00036-5
58. Visu-Petra L, Stanciu O, Benga O, Miclea M, Cheie L. Longitudinal and concurrent links between memory span, anxiety symptoms, and subsequent executive functioning in young children. Front Psychol. (2014) 5:443. doi: 10.3389/fpsyg.2014.00443
59. Castagna PJ, Calamia M, Roye S, Greening SG, Davis TE. The effects of childhood inattention and anxiety on executive functioning: inhibition, updating, and shifting. Atten Defic Hyperact Disord. (2019) 11:423–32. doi: 10.1007/s12402-019-00306-7
60. Schatz DB, Rostain AL. ADHD with comorbid anxiety: a review of the current literature. J Atten Disord. (2006) 10:141–9. doi: 10.1177/1087054706286698
61. Maric M, Bexkens A, Bögels SM. Is clinical anxiety a risk or a protective factor for executive functioning in youth with ADHD? a meta-regression analysis. Clin Child Fam Psychol Rev. (2018) 21:340–53. doi: 10.1007/s10567-018-0255-8
62. Zhang SY, Qiu SW, Pan MR, Zhao MJ, Zhao RJ, Liu L, et al. Adult ADHD, executive function, depressive/anxiety symptoms, and quality of life: a serial two-mediator model. J Affect Disord. (2021) 293:97–108. doi: 10.1016/j.jad.2021.06.020
63. Sjöwall D, Thorell LB. Functional impairments in attention deficit hyperactivity disorder: the mediating role of neuropsychological functioning. Dev Neuropsychol. (2014) 39:187–204. doi: 10.1080/87565641.2014.886691
64. Tseng WL, Gau SSF. Executive function as a mediator in the link between attention-deficit/hyperactivity disorder and social problems. J Child Psychol Psychiatry. (2013) 54:996–1004. doi: 10.1111/jcpp.12072
65. Roselló B, Berenguer C, Baixauli I, Mira Á, Martinez-Raga J, Miranda A. Empirical examination of executive functioning, ADHD associated behaviors, and functional impairments in adults with persistent ADHD, remittent ADHD, and without ADHD. BMC Psychiatry. (2020) 20:134. doi: 10.1186/s12888-020-02542-y
Keywords: attention-deficit/hyperactivity disorder, executive functions, functional impairment, adolescents, anxiety
Citation: Haugan A-LJ, Sund AM, Thomsen PH, Lydersen S and Nøvik TS (2022) Executive functions mediate the association between ADHD symptoms and anxiety in a clinical adolescent population. Front. Psychiatry 13:834356. doi: 10.3389/fpsyt.2022.834356
Received: 13 December 2021; Accepted: 22 August 2022;
Published: 12 September 2022.
Edited by:
Kerstin Jessica von Plessen, Centre Hospitalier Universitaire Vaudois (CHUV), SwitzerlandReviewed by:
Javier Fenollar Cortés, Loyola University Andalusia, SpainCopyright © 2022 Haugan, Sund, Thomsen, Lydersen and Nøvik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anne-Lise Juul Haugan, YW5uZS1saXNlLmouaGF1Z2FuQG50bnUubm8=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.