- 1Department of Rehabilitation Psychology and Psychotherapy, Institute of Psychology, University of Freiburg, Freiburg, Germany
- 2Department of Health Psychology, Institute of Psychology, Leuphana University Lueneburg, Lueneburg, Germany
- 3Department of Psychiatry and Psychotherapy, Faculty of Medicine, Medical Center–University of Freiburg, Freiburg, Germany
- 4Department of Clinical Psychology and Psychotherapy, Institute of Psychology and Education, Ulm University, Ulm, Germany
Refugees are exposed to multiple stressors affecting their mental health. Given various barriers to mental healthcare in the arrival countries, innovative healthcare solutions are needed. One such solution could be to offer low-threshold treatments, for example by culturally adapting treatments, providing them in a scalable format, and addressing transdiagnostic symptoms. This pilot trial examined the feasibility, acceptance, and preliminary effectiveness of a culturally adapted digital sleep intervention for refugees. Sixty-six refugees participated, with 68.2% of them seeking psychological help for the first time. Only three participants did not show clinically significant insomnia severity, 93.9% reported past traumatic experiences. Participants were randomly assigned to the intervention group (IG) or the waitlist control group (CG). Insomnia severity, measured by the Insomnia Severity Index, and secondary outcomes (sleep quality, fear of sleep, fatigue, depression, wellbeing, mental health literacy) were assessed at baseline, 1 and 3 months after randomization. The self-help intervention included four modules on sleep hygiene, rumination, and information on mental health conditions associated with sleep disturbances. 66.7% of the IG completed all modules. Satisfaction with the intervention and its perceived cultural appropriateness were high. Linear multilevel analyses revealed a small, non-significant intervention effect on insomnia severity of Hedge's g = 0.28 at 3-months follow-up, comparing the IG to the CG [F2, 60 = 0.88, p = 0.421]. This non-confirmatory pilot trial suggests that low-threshold, viable access to mental healthcare can be offered to multiple burdened refugees by culturally adapting an intervention, providing it in a scalable format, and addressing a transdiagnostic symptom.
Introduction
The United High Commissioner for Refugees (UNHCR) reports on 82.4 million forcibly displaced people in the end of 2020, including 34.4 million people displaced abroad1 (1). This poses challenges on healthcare systems in the arrival countries (2–5), mainly because refugees are exposed to many stressors before, during, and after flight (6, 7). The many stressors influence refugee's mental health (8–10) and, correspondingly, the prevalence of trauma-associated disorders such as posttraumatic stress disorder or depression is enhanced (11–14). However, there is a mental health treatment gap (15): Individual barriers (e.g., language barriers, somatic concept of mental health, stigmatization) (16, 17) and structural barriers (e.g., lack of treatment resources or financing opportunities) (18, 19) hinder refugees from seeking help for mental disorders. To overcome mental healthcare barriers, various approaches have been proposed (20, 21), among them (a) using scalable and low-threshold treatment formats, (b) addressing somatically perceived and transdiagnostic symptoms, and (c) culturally adapting treatments.
Concerning (a) the use of scalable and low-threshold treatment formats (22–24), digital interventions are suggested to be easier to access for refugees than face-to-face treatments (25–27), as they are anonymous, resource saving, and flexible in use regarding time and place (28–30). With numerous evidence of efficacy in western populations (31–33), findings on the efficacy of digital interventions among refugees are inconsistent: Whereas a digital intervention to reduce posttraumatic stress disorder did not yield a significant effect in a randomized controlled trial (34), results of two conducted randomized controlled pilot trials indicated significant effects of the digital interventions in reducing depressive symptoms (35, 36). (b) Addressing somatically perceived and transdiagnostic symptoms might be another option to overcome barriers among refugees (37–39). Mental distress is often linked with somatic symptoms in refugee's countries of origin (40), and somatic mental health concepts are prevalent (41, 42). Sleep disturbances as a somatically perceived mental health problem are frequently reported (43–45), which suggests that they could be an accepted way to express mental distress among refugees. Moreover, sleep disturbances are a transdiagnostic symptom (46, 47) and, herewith, often associated with other mental health conditions among refugees (48, 49). Indeed, treating sleep disturbances–also via digital interventions–has been shown to reduce associated mental disorders such as depression and posttraumatic stress disorder (50–54). To date, only two studies evaluated effects of interventions on sleep disturbances, with one study showing a positive effect of relaxation music on sleep quality in refugees (55), and a pilot trial indicating an improved insomnia severity following a transdiagnostic digital intervention (35).
Barriers could be further reduced by (c) culturally adapting treatments, that is by considering refugees' contexts and strains in their treatment (56, 57). Thereby, it appears relevant to adapt interventions in a systematic way (58), which is enabled by frameworks of culturally adapting face-to-face treatments (59–61) and scalable and low-threshold interventions (62–64). Culturally adapting face-to-face treatments seems to enhance their acceptance and efficacy among populations that differ from the original target groups (65, 66). Similarly, culturally adapted digital interventions are shown to be effective in reducing mental disorders (64, 67). However, only few digital interventions have been culturally adapted for refugees (68–71), with the efficacy of some interventions being indicated in randomized controlled pilot trials (35, 36).
Combining the three illustrated approaches to overcome mental healthcare barriers among refugees, we culturally adapted a digital sleep intervention. A randomized controlled pilot trial was conducted to evaluate the feasibility, acceptance, and preliminary effectiveness of the resulting eSano Sleep-e intervention among refugees, which should allow drawing conclusions on conducting a final randomized controlled trial. Thereby, we aimed to investigate
1. whether refugees adhered to the intervention;
2. whether refugees were satisfied with the intervention and perceived it as culturally appropriate; and
3. whether preliminary evaluations indicate that the intervention improved insomnia severity and other sleep associated and mental health conditions in refugees.
Materials and Methods
Study Design, Participants, and Procedure
This is a randomized controlled pilot trial with an intervention group (IG) receiving access to the eSano Sleep-e intervention and a waitlist control group (CG). The study was registered in the German Clinical Trial Register (identifier: DRKS00018949). Deviating from the registration protocol, more than the 40 initially planned participants were included [the planned number based on the Consolidated Standards of Reporting Trials (CONSORT) guidelines for pilot and feasibility studies (72) and an assumed dropout rate of 20% (73)], due to (a) adjustments in the study procedure after the first enrolments of participants and (b) a high response following a last recruitment wave. Furthermore, recruitment was expanded from personal recruitment in Freiburg, Germany, to an online recruitment all over German-speaking countries, due to the restrictions in contacting people in person resulting from the Covid-19 pandemic. The study was approved by the commissioner for data protection and the local Ethics Committee at the University of Freiburg, Germany (no. 475/19) and was carried out in accordance with the Declaration of Helsinki. The CONSORT guidelines and their extension for randomized pilot and feasibility studies were followed for reporting this trial (http://www.consort-statement.org) (72, 74).
The study was conducted online in German and English language. Recruitment was carried out from March 2020 to February 2021 and took place mainly in Germany, with a small part also in Austria, Switzerland, and Liechtenstein. The last follow-up assessment was completed in July 2021. Emails, posts, and flyers referring to the study homepage were distributed through diverse recruitment channels. Among the channels were institutions working with refugees (e.g., universities, refugee support services, psychosocial centres for refugees), (social) media (newsletters, Twitter, Facebook), personal contacts and on-site advertisement (e.g., refugee accommodations). On the study homepage (https://esano.klips-ulm.de/de/trainings/schlafprobleme-sleep-problems/sleep-e/), interested participants could get detailed information on the study procedure, and they were provided a link to study registration.
After registering and signing the digital informed consent, participants were emailed a link to the baseline assessment (T1). Here, inclusion criteria for study participation were assessed, which were (1) age ≥ 18 years, (2) sufficient English or German language skills, (3) access to an internet device, (4) flight background. The only exclusion criterion was suicidality, unless the participant was in secured primary care. No cut-off for the severity of sleep disturbances was used as inclusion criterion so to obtain information on who might be interested in using the intervention, regardless of meeting clinical symptoms. This should also allow participation of refugees with subclinical symptoms to facilitate an initial and transdiagnostic access to mental healthcare. Eligible participants were randomized 1:1 to the IG or the waitlist CG after completing the baseline assessment. Randomization was conducted by an independent researcher not further involved in the study, using an automatic randomization software (https://www.sealedenvelope.com), applying permuted block randomization with randomly varying block sizes of two and four. Randomized participants were emailed information on the further study procedure. Participants of the IG received immediate access to the intervention after randomization; participants of the CG received access to the same intervention after completing the final assessment, following a waiting period with no intervention provided. Follow-up assessments took place 1 month (T2) and 3 months after randomization (T3). Participants received reminders to complete pending assessments. After T3, participants had the chance to win a 50€ Amazon voucher.
Intervention
The used brief digital sleep intervention eSano Sleep-e was culturally adapted from GET.ON recovery, a cognitive behavioral digital intervention developed for German teachers showing large effects in reducing sleep disturbances (75–77). Adaptions were conducted between October 2017 and February 2020 and the procedure was based on the heuristic framework for the cultural adaptation of interventions [Barrera and Castro (60); illustrated in Supplementary Table 1.1]. Information on components to culturally adapt were gained in a literature review on culturally adapting digital interventions for mental disorders (64), and in a user experience study in which suggestions of inadequate intervention components were gathered in interviews with refugees and healthcare providers working with refugees (78). Adaptations included content adaptations (e.g., use relatable example characters with similar problems, expand psychoeducational elements, offer intervention in simplified German and English language) and methodological adaptations (e.g., use videos and images instead of text, provide intervention in a mobile format, shorten intervention). An overview on the components that have been culturally adapted is presented in Supplementary Table 1.2.
The intervention was accessible through the Minddistrict platform (https://www.minddistrict.com) in both a browser and mobile-based format. It consisted of four modules, which were recommended to be completed within 4 weeks. It took 30–45 min to complete all contents of one module; a module could be completed as a whole or broken down into different units. Contents aimed at normalizing mental health problems, promoting health behavior, and facilitating access to the health system. They included psychoeducation on sleep difficulties, rumination, and information on associated mental health conditions; sleep hygiene rules; exercises to deal with rumination; links to further mental healthcare options; and relaxation exercises (see Table 1). Information was mainly delivered via videos with experts and example characters and could be consolidated with exercises. Exemplary pages of the intervention are illustrated in Supplementary Table 2. The progress of each participant could be monitored on the platform, and when a module was completed, the next module was activated. In case a participant had not worked on the module for more than a week, they were reminded to do so via email, WhatsApp message, or phone call. No therapeutic guidance was provided.
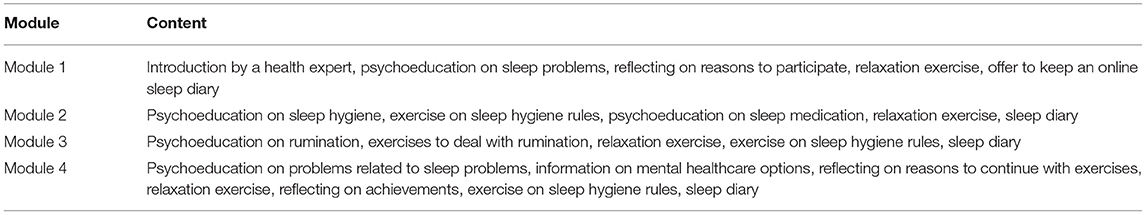
Table 1. Contents of the four modules of the culturally adapted digital sleep intervention eSano Sleep-e.
Outcomes
Data was assessed via online self-report questionnaires and usage data from the intervention platform. At baseline, sociodemographic variables and medical and psychosocial treatments were assessed, and traumatic experiences as well as alcohol and drug consumption were screened with questions from the structured clinical interview for DSM-5 (79).
Adherence to the Intervention
Adherence to the intervention was evaluated by the mean (standard deviation, SD) of completed modules among the participants of the IG, as well as the rates of non-starters and completers. Data was derived from the intervention platform.
Acceptance of the Intervention
Acceptance outcomes included intervention satisfaction and its perceived cultural appropriateness. They were measured at T3 within those participants of the IG who had started the intervention at that time. Satisfaction with the intervention was assessed with the Client Satisfaction Questionnaire adapted for Internet Interventions (80) (CSQ-I; 8 items; scale 1–4; range 8–32, with a higher score indicating higher satisfaction; excellent McDonald's Ω = 0.95, excellent α = 0.95 in current sample). Perceived cultural appropriateness of the intervention was assessed with the self-developed Cultural Appropriateness Questionnaire, which was developed from a previous version (81) (CAQ; 21 items representing 4 subscales: structure, 7 items; design, 3 items; language, 2 items; content, 9 items; scale 1–5; total score range 21–105, with a higher score indicating higher perceived cultural appropriateness; acceptable α = 0.79 in current sample).
Effectiveness of the Intervention
The primary outcome was insomnia severity, measured by the Insomnia Severity Index (ISI) (82). Seven items are answered on a five-point Likert scale (0–4). The total score ranges from 0 to 28, with a higher score indicating higher insomnia severity. The internal consistency is excellent (Cronbach's α = 0.90); in the current sample, Cronbach's α was good (α = 0.84).
Several secondary outcomes were measured. Sleep quality was assessed with the Pittsburgh Sleep Quality Index (83) (PSQI; 19 items representing 7 components; scale 0–3; range 0–21, with a higher score indicating poorer sleep quality; good α = 0.83, questionable α = 0.63 in current sample). Fear of Sleep was assessed with the Fear of Sleep Inventory–Short Form (84) (FOSI-SF; 13 items; scale 0–4; range 0–52, with a higher score indicating higher fear of sleep; excellent α = 0.93, excellent α = 0.93 in current sample). Fatigue was assessed with the Multidimensional Fatigue Inventory (85) (MFI; 20 items representing 5 subscales with 4 items each: general fatigue, physical fatigue, reduced activity, reduced motivation, mental fatigue; scale 0–4; subscale score range 0–16, with a higher score indicating higher fatigue; good average α = 0.84, questionable α = 0.67 in current sample). Depressive symptoms were assessed with the Patient Health Questionnaire−9 item version (86) (PHQ-9; 9 items; scale 0–3; range 0–27, with a higher score indicating more severe depressive symptoms; good α = 0.89, good α = 0.88 in current sample). General wellbeing was assessed with the Refugee Health Screener−15, screening common mental disorders in refugees (posttraumatic stress disorder, anxiety, and depression) (87) (RHS-15; 14 items; scale 0–4; total score range 0–56, with a higher score indicating lower general wellbeing; excellent α = 0.92, excellent α = 0.91 in current sample). Mental health literacy was assessed with the Mental Health Literacy Questionnaire in young adults (88) (MHLQ; 29 items; scale 1–5; range 29–145, with a higher score indicating higher mental health literacy; good α = 0.84, good α = 0.87 in current sample). Literacy was assessed among four dimensions: knowledge on mental health problems, stereotypes, first aid skills, and self-help strategies.
Negative Effects of the Intervention
At T3, negative effects of the intervention were assessed within the IG with the Negative Effects Questionnaire, self-adapted to digital interventions (89, 90) [NEQ; 18 items; 3 scales per item: I. endorsement of a specific effect, scale 1 (yes), 0 (no); II. negativity of the effect, scale 0–4, with a higher score indicating a higher negativity; III. attribution of the effect, scale 1 (treatment), 0 (other circumstances)]. Negative effects represent five factors: symptoms, stigma, and hopelessness regarding mental health, dependency and perceived deficiencies regarding treatment.
Statistical Analyses
Client satisfaction, perceived cultural appropriateness, adherence to the intervention, and negative effects of the intervention are illustrated descriptively.
Effectiveness analyses were performed using SPSS Statistics 27, and based on the intention-to-treat principle and on a two-side significance level of 5%. Intervention effects on the primary and secondary outcomes at T2 and T3 were investigated by means of linear multilevel analyses, with time (T1, T2, T3) on level 1 and individual participants on level 2 (random intercept, fixed slope; diagonal variance structure). This analytical procedure was chosen as it allows for the simultaneous analysis of time and group effects (91). Missing values were estimated in the multilevel analyses. The factors group (IG vs. CG) and time of assessment (T1, T2, T3) as well as their interaction were included into the models on the outcomes, with the interaction indicating group differences in the respective outcome over time. Post-hoc pairwise group comparisons were conducted at T2 and T3 separately. Standardized between-group effect sizes with their 95% confidence intervals (CI) were calculated (Hedges' g) for T2 and T3 by dividing the model-based estimated group mean difference by the corrected pooled SD (92). Due to the pilot character of the trial, p-values are only reported for analyses on the primary outcome. In addition to the intention-to-treat analyses, per protocol analyses were conducted analyzing the intervention effect on the primary outcome, including only those participants of the IG that had completed the main part of the intervention at the time of T3.
We conducted stepwise multiple regression analyses to examine whether acceptance of and adherence to the digital intervention predicted changes in the primary or secondary outcomes from T1 to T3. Perceived cultural appropriateness, client satisfaction, and number of completed modules at the time of T3 were used as predictors.
Results
Participants
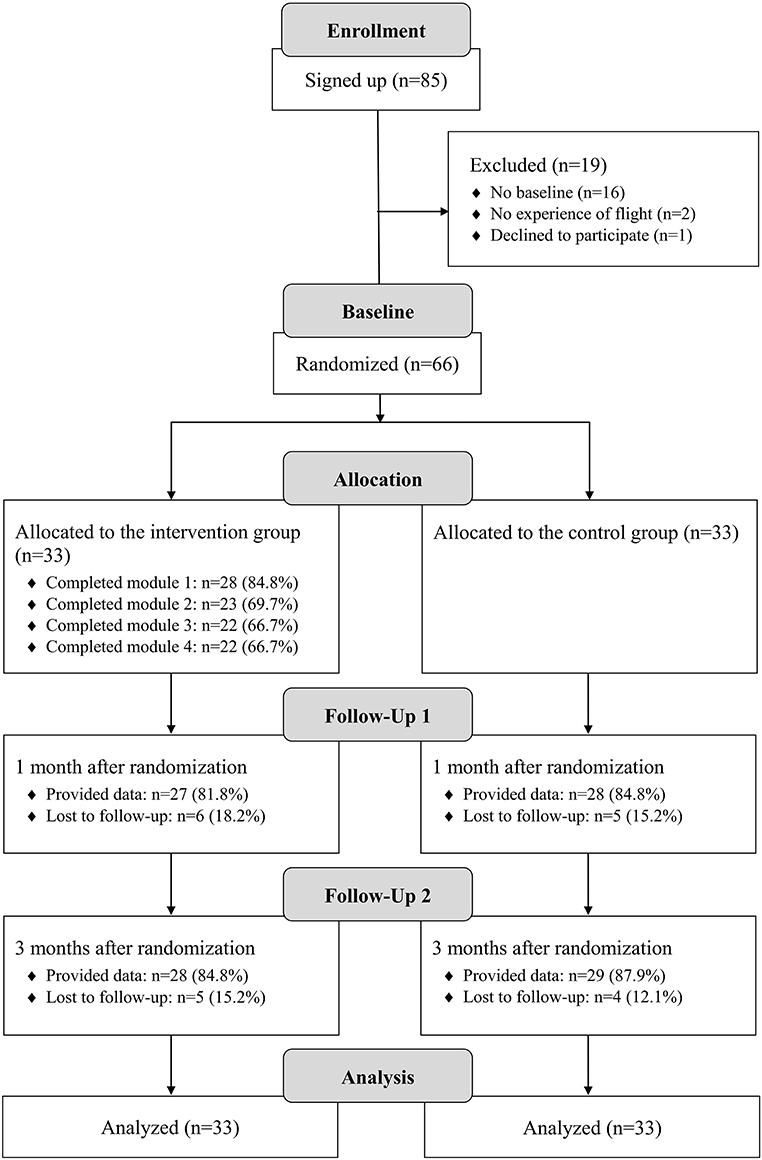
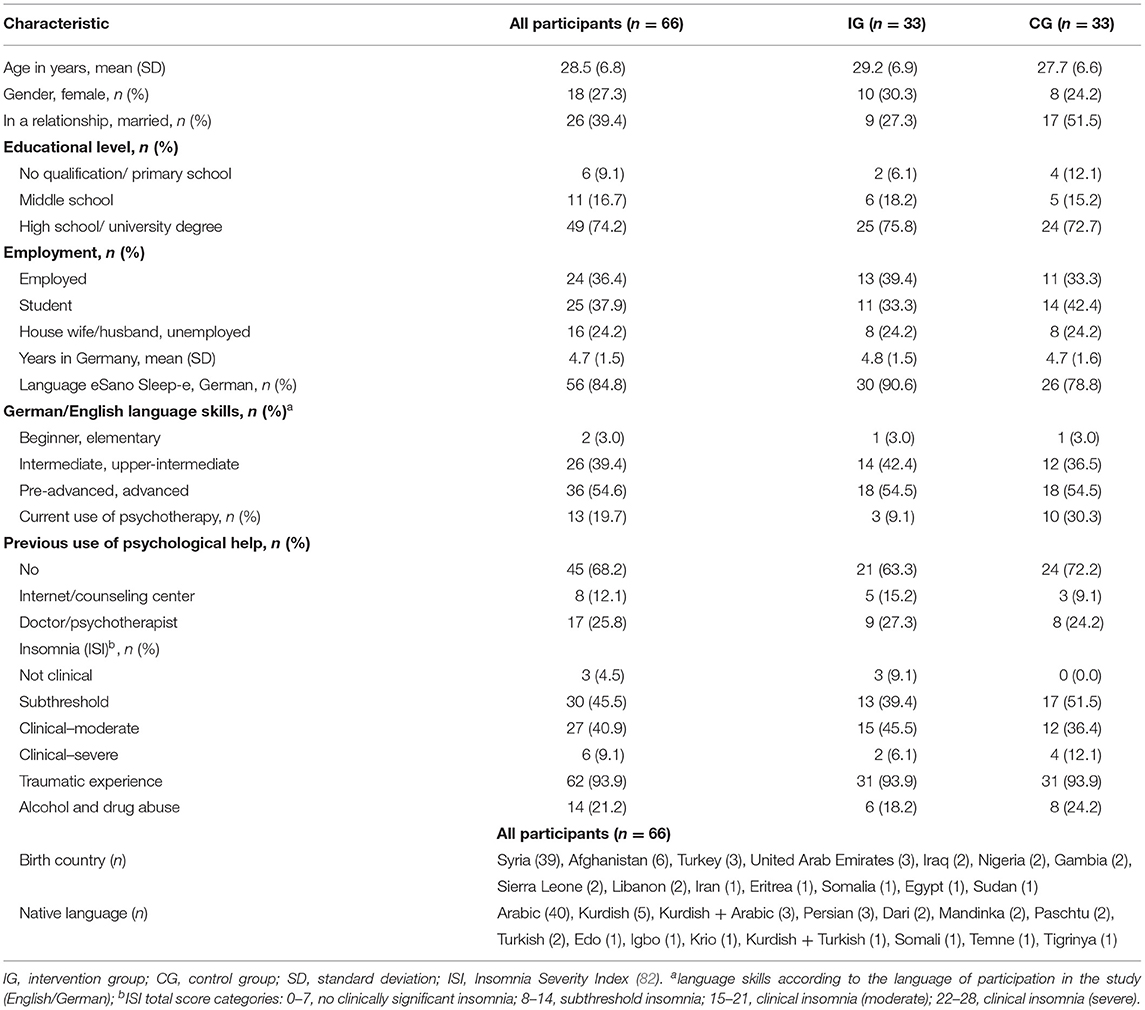
Figure 1 shows the participants' flow. Sixty-six participants were randomized to the IG (n = 33) and CG (n = 33). Their sociodemographic characteristics are illustrated in Table 1. Eighteen participants (27.3%) were female. The mean (SD) age was 28.5 (6.8) years, ranging from 18 to 49 years. Participants were from 14 nationalities, with the majority coming from Syria (n = 39, 59.1%). In total, 58 (87.9%) of the participants were from countries in the orient, the remaining 8 (12.1%) from sub-Saharan African countries. Participants spoke 15 different native languages, with 43 (65.2%) having Arabic as (one of) their native language. 36.4% of the participants (n = 24) were currently employed, 37.9% (n = 25) were enrolled at a university. Thirteen participants (19.7%) were in current psychotherapeutic treatment, 45 (68.2%) had never sought psychological help before. Regarding baseline symptomatic, three participants did not show clinically significant insomnia severity; 30 (45.5%) showed subclinical insomnia severity, and 33 (50.0%) showed clinical insomnia severity. Sixty-two participants (93.9%) reported past traumatic experiences, 14 (21.2%) reported alcohol or drug abuse.
Sociodemographic data (Table 2) and baseline symptoms (Tables 3, 4) did not differ substantially between the IG and CG, except for the number of participants being in therapeutic treatment [IG: 3 (9.1%); CG: 10 (30.3%)]. Neither did the study dropout rates differ between the groups [IG: 6 (18.2%), CG: 5 (15.2%) dropout at T3]. Differences between participants who completed T3 (n = 57) and those who dropped out of the study (n = 9), or between participants of the IG who completed the training (n = 22) and those who did not (n = 11) were revealed concerning language abilities, level of education, and student status. Rates of lower language skills and lower educational level were higher among participants who did not complete T3 or the intervention, whereas rates of higher language skills and higher educational level were enhanced among participants who completed T3 and the intervention. Similarly, the number of university students was higher among study and intervention completers than among non-completers. Detailed information on the revealed group differences are presented in Supplementary Table 3.
Adherence to the Intervention
Participants of the IG completed a mean of 2.9 (SD = 1.7) modules, which equals 72.0% of the intervention. Five participants (15.2%) did not start the intervention, 22 participants (66.7%) completed all modules (see Figure 1). At the time of T3, the mean of completed modules was 2.8 (SD = 1.7; 69.7%), with six participants (18.2%) not having started the intervention. Twenty participants (60.6%) had completed all modules at that time, and an additional two participants had completed three modules.
Acceptance of the Intervention
Intervention satisfaction among the participants of the IG who started the intervention was found to be high with a mean CSQ-I score of M = 24.0 (SD = 6.6). The lowest rate of agreement was revealed in the statement “The training has met my needs,” which 15 participants (57.7%) partly or totally agreed with. The highest rate of agreement was shown in the statements “The training helped me deal with my problems more effectively,” “In an overall, general sense, I am satisfied with the training,” and “I would come back to such a training if I were to seek help again,” which 19 participants (71.4%) partly or totally agreed with, respectively. Details on the ratings are shown in Supplementary Table 4.
Perceived cultural appropriateness was shown to be high with a mean CAQ global score of M = 79.3 (SD = 10.3). All four subscales yielded high mean scores, with language being the scale with the lowest ratings (70.0% of total score) and structure being the scale with the highest ratings (77.4%). The lowest perceived appropriateness was shown on the item “It would have been better for me to do the training in my native language,” which 23.1% (strongly) supported. The highest appropriateness was shown on the item “I think the training looks good,” which 88.5% (strongly) supported. Details on the ratings are displayed in the Supplementary Table 5.
Effectiveness of the Intervention
Primary Outcome
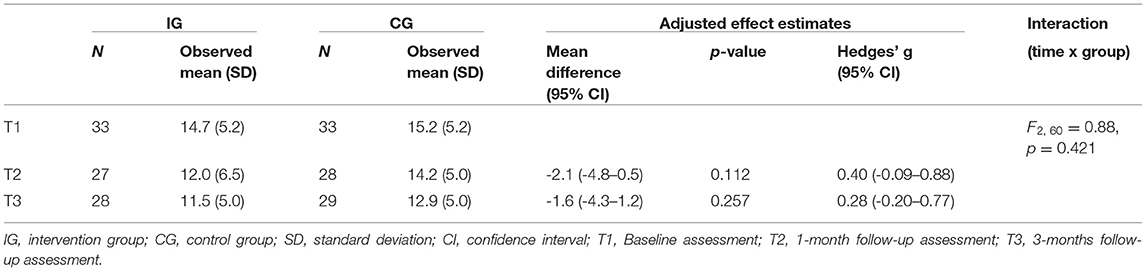
Multilevel analyses of the ISI are illustrated in detail in Table 3, Figure 2. No significant group x time interaction was shown. At T1, the IG showed an insomnia severity of M = 14.7 (SD = 5.2) and the CG of M = 15.2 (SD = 5.2). At T2, a mean of M = 12.0 (SD = 6.5) in the IG and of M=14.2 (SD = 5.0) in the CG was observed, with a non-significant estimated mean difference of -2.1 (95% CI, -4.8 to 0.5, p = 0.112) and an effect size of g = 0.40. At T3, a mean of M = 11.5 (SD = 5.0) was observed in the IG and a mean of M = 12.9 (SD = 5.0) in the CG, with a non-significant estimated mean difference of -1.6 (95% CI, -4.3 to 1.2, p = 0.257) and an effect size of g = 0.28.
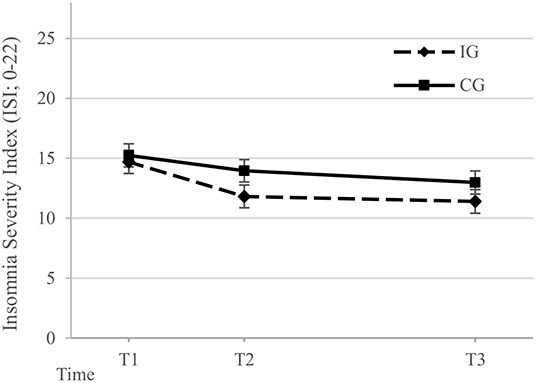
Figure 2. Model-based estimates of the Insomnia Severity Index scores (82) in the intervention group (IG) and control group (CG) at Baseline (T1), 1-month follow-up assessment (T2), and 3-months follow-up assessment (T3). The model includes the factors time, group, and their interaction. The error bars represent the estimated standard error of the mean.
Per protocol analyses on the primary outcome were conducted including only those 22 participants of the IG that had completed at least three modules of the intervention at the time of T3. Analyses revealed a non-significant group x time interaction effect. Between-group mean differences of insomnia severity at T2 with -2.4 (95% CI, -5.2 to 0.4) and T3 with -1.9 (95% CI, -4.9 to 1.2) were non-significant, revealing effect sizes of g = 0.49 and g = 0.35, respectively. Detailed results are illustrated in Supplementary Table 6.
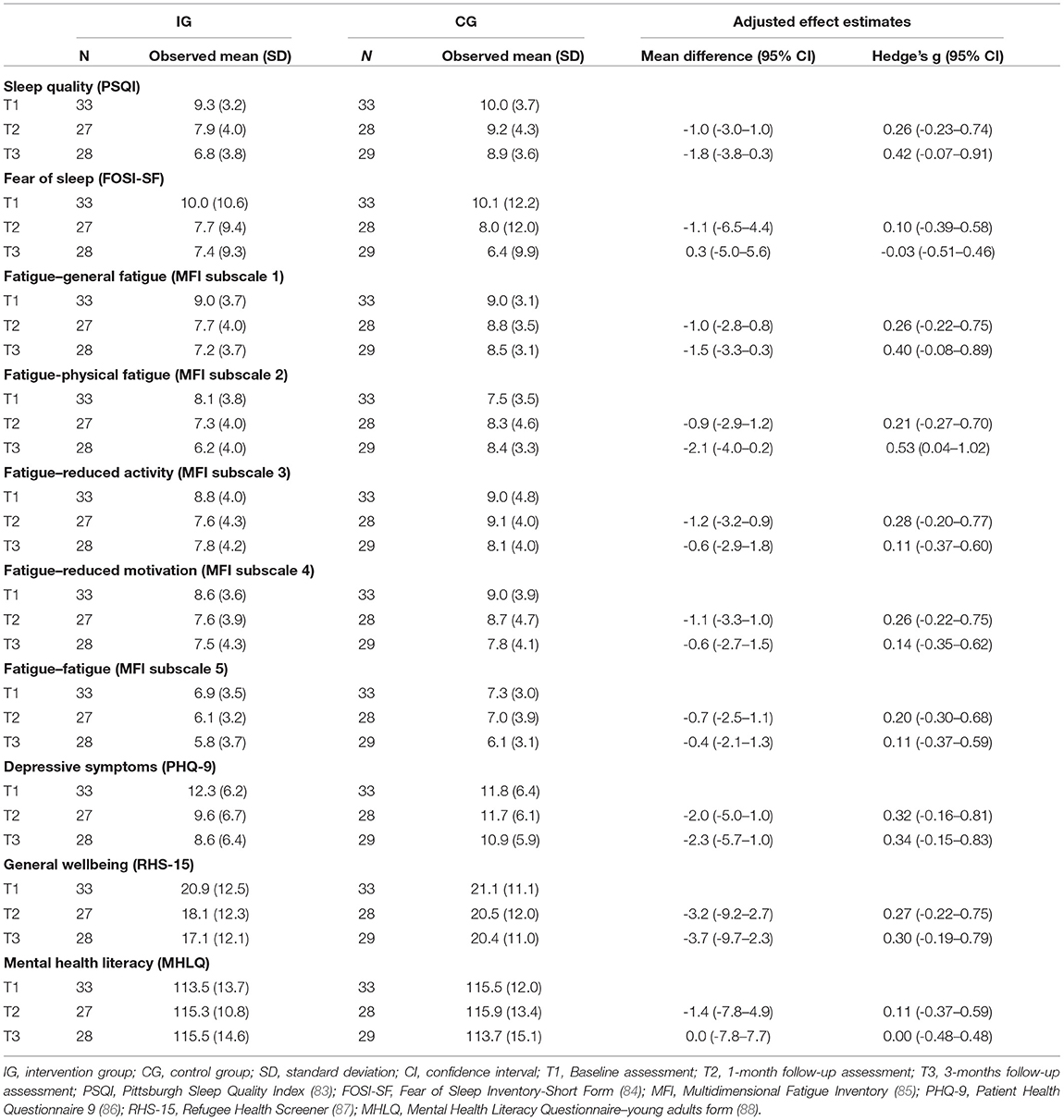
Secondary Outcomes
Table 4 presents all means and SD of the secondary outcomes. For the subscale physical fatigue of the MFI, a significant group x time interaction effect was shown with F2, 54= 4.97, p = 0.010, revealing a significant estimated mean difference at T3 between the IG and CG of -2.1 (95% CI, -4.0 to -0.2, p < 0.05; g = 0.53).
Prediction of Effectiveness of the Intervention
Regression analyses investigating the influence of the CSQ-I, the CAQ, and the number of completed modules at T3 on the primary outcome did not yield significant results. Among the secondary outcomes, scores of the PSQI, the FOSI, the PHQ, the RHS, and some subscales of the MFI were significantly predicted by CSQ-I or CAQ scores. None of the outcomes was significantly predicted by the adherence to the intervention. Results are illustrated in Supplementary Table 7.
Negative Effects of the Intervention
All in all, 98 negative effects were reported that occurred during study participation (M = 3.8, SD = 3.5), of which 12 (12.2%) were reported to be caused by the intervention, and 86 (87.8%) were reported to be caused by other circumstances. Concerning the negative effects caused by the intervention, three related to the factor symptoms, with slightly, moderately, or strongly worsened symptoms; five related to the factor deficiencies, revealing slightly or moderately perceived deficiencies of the intervention; one related to the factor dependency, with a moderate dependency on the intervention; two related to the factor stigma, with a moderate or strong stigma in relation to the intervention; and one related to the factor hopelessness, with a moderate hopelessness due to the intervention. Details on negative effects are displayed in Supplementary Table 8.
Discussion
This is the first trial investigating a digital sleep intervention in refugees. Thereby, three low-threshold approaches were combined to engage refugees: using a scalable digital format for the intervention, addressing somatically perceived and transdiagnostic sleep disturbances, and culturally adapting the intervention. The findings of this non-confirmatory trial indicate that the self-help intervention holds the potential to provide multiple burdened refugees with initial access to mental health treatment. So, on the one hand, although there were no inclusion criteria to the study regarding a cut-off for insomnia severity, only three of 66 participants showed no clinically significant insomnia severity based on the ISI (82). Moreover, 93.9% participants reported from previously endured traumata, 89.4% showed at least mild depressive symptoms, and 77.3% revealed current mental health problems. On the other hand, more than two-thirds (68.2%) of the participants never had used psychological help before.
The particular target group of burdened and underserved refugees showed high satisfaction with, perceived appropriateness of, and adherence to the digital sleep intervention, with rates comparable to the original intervention (77, 81). Importantly, the intervention did not seem to cause any serious negative effects. However, in this non-confirmatory pilot trial, intervention effects on insomnia severity were shown to be non-significant and small, with g = 0.40 after 1 month, and g = 0.28 after 3 months comparing the IG to the waitlist CG. Of note, the power to find significant insomnia severity differences was 1-β = 0.35 at T2 and 1-β = 0.20 at T3. Nevertheless, effects are smaller than the revealed large effects of the culturally non-adapted versions (77, 81). Effects on the secondary outcomes were also mostly small. A moderate effect was revealed only on reducing physical fatigue, which fits the assumed somatic mental health concept of refugees (93). High improvements in the CG might have leveled out between group differences, possibly due to an increased use of psychotherapeutic treatment among the CG (30.3% of the CG vs. 9.1% of the IG). Furthermore, the intervention was developed as a brief, psychoeducative health promotion intervention, not comprising recommended and effective components of sleep treatment that require high self-motivation and are demanding for users (e.g., sleep restriction and stimulus control) (94). This approach was chosen because the primary goal of the intervention was to provide refugees with initial access to healthcare, to be followed by more intensive treatment for sleep disturbances or other mental health conditions (37, 95, 96).
When interpreting the results, two aspects should be taken into account. First, a large proportion of participants had high levels of education and language skills, and the intervention dropout rate seemed higher among participants with lower levels of education and language skills. Second, almost three-quarters (72.7%) of the IG participants needed to be motivated to start or continue with the intervention at least three times, and intervention completion took long (average days of completion: 46, range 12 to 107). This may suggest that the intervention completion was difficult and required skills that could mainly be fulfilled among highly educated refugees, which may be an easier-to-reach subgroup of refugees.
To increase adherence, acceptance, and effectiveness in refugees with a lower level of education, it might be necessary to further adapt the intervention. (1) As suggested by the results of the CAQ, the intervention should be translated into native languages of refugees. (2) As access to the intervention was shown to be difficult by the frequent reminders on starting the intervention, the intervention should be provided on an easy-to-access platform with lower technical demands. In addition to reminders, persuasive design principles aiming at user engagement may be promising in this regard (97). (3) More guidance should be provided to support the refugees on technical or other demands, as guidance is known to improve intervention adherence and effectiveness (33, 98). After such a refinement of the cultural adaptation, its acceptance and effectiveness should be compared with the present version of the intervention in a sufficiently powered randomized controlled trial (63, 67, 99), or in randomized factorial trials (100, 101). These allow the modification of single intervention components (e.g., language modifications) and thereby the comparison of the specific effect of the suggested refinements of cultural adaptation to understand mechanisms of change more precisely (102, 103), and may thus be a fruitful next step in further developing the present intervention. In addition to a further adaptation of the intervention, the study conduction should be optimized: (1) Questionnaires that have been developed and evaluated for refugees and are available in their native languages ought to be applied (87); and (2), more in-person recruitment should be used, so that refugees with a lower level of education and technical familiarity can be reached (104).
The conducted pilot trial had several limitations. First, due to the pilot character of the trial, the sample size and, thus, the power to detect clinical significant effects was limited. Second, the digital sleep intervention and study participation material was only available in English or German. This posed high demands on (possible) participants, potentially hindering interested refugees with higher language barriers from participating in the study and the intervention. Third, along with this, a large part of the participants had a high level of education, which does not adequately reflect the situation of refugees, herewith indicating a selection bias and, thus, a limited generalisability. Fourth, a large proportion of Syrian refugees participated in the study. Although this roughly maps the distribution of refugees in Germany, the generalisability for refugees from other countries of origin is limited. Fifth, the used self-report questionnaires to assess the effectiveness and acceptability of the intervention were largely not evaluated for the target population, with exception of the RHS-15 (87). This lack of evaluation or possibly also of cultural appropriateness for refugees might be linked with the revealed questionable internal consistency of some questionnaires (PSQI; MFI). Sixth, no information on the participants' thoroughness in completing the intervention was gained; however, before activating the following module, it was verified that the main parts of a module had been visited. Seventh, we did not differentiate between refugees with regard to, for example, length of stay in Germany or country of origin. However, such aspects may influence the need of culturally adapting digital interventions and, herewith, the effectiveness of such interventions (105) and should thus be considered in a future randomized trial.
Conclusions
In conclusion, this pilot trial indicated that providing a treatment in a digital format, targeting transdiagnostic sleep disturbances, and conducting a cultural adaptation resulted in an intervention that seemed feasible to establish initial healthcare access for hard-to-reach, burdened refugees. Acceptance and adherence levels were high, and no serious negative effects due to the intervention were reported. However, this non-confirmatory pilot trial indicated only a small, non-significant intervention effect on improving insomnia severity. Evaluating a refined cultural adaptation focusing on language, intervention complexity, and engagement strategies may be a promising next step toward bridging the mental health treatment gap for refugees.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee at the University of Freiburg, Germany. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KSpa, JB, and LS conceived the study conceptualization and design. DL provided the intervention template GET.ON recovery, KSpa and LS adapted the intervention content, HB provided access to the intervention platform. KSpi provided expertise in sleep problems and treatment. KSpa and EH collected data, conducted the statistical analyses, and wrote the draft of the manuscript. HB, JB, and LS supervised the work. All authors contributed to the manuscript revision, read, and approved the submitted version.
Funding
KSpa is supported by the German Academic Scholarship Foundation. The article processing charge was funded by the University of Freiburg in the funding programme Open Access Publishing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank all of the study participants, as well as the organisations distributing the information on the study. Further thanks go to Layla Humpert, Annika Weiser, and Viktoria Boeckle for their assistance in recruitment and data acquisition.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.832196/full#supplementary-material
Abbreviations
CAQ, Cultural Appropriateness Questionnaire; CG, control group; CI, confidence interval; CSQ-I, Client Satisfaction Questionnaire adapted to Internet interventions; FOSI-SF, Fear of Sleep Inventory-Short Form; IG, intervention group; ISI, Insomnia Severity Index; MFI, Multidimensional Fatigue Inventory; MHLQ, Mental Health Literacy Questionnaire young adults form; NEQ, Negative Effects Questionnaire; PHQ, Patient Health Questionnaire; PSQI, Pittsburgh Sleep Quality Index; RHS, Refugee Health Screener; SD, standard deviation; UNHCR, United Nations High Commissioner for Refugees.
Footnotes
1. ^This number includes refugees and asylum-seekers, further referred to as refugees.
References
1. UNHCR. Global Trends: forced displacement in 2020. UNHCR The UN Refugee Agency (2021). Available online at: https://www.unhcr.org/60b638e37/unhcr-global-trends-2020
2. Lindert J, Carta MG, Schäfer I, Mollica RF. Refugees mental health - a public mental health challenge. Eur J Public Health. (2016) 26:374–5. doi: 10.1093/eurpub/ckw010
3. Silove D, Ventevogel P, Rees S. The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry. (2017) 16:130–9. doi: 10.1002/wps.20438
4. Wylie L, Van Meyel R, Harder H, Sukhera J, Luc C, Ganjavi H, et al. Assessing trauma in a transcultural context: challenges in mental health care with immigrants and refugees. Public Health Rev. (2018) 39:22. doi: 10.1186/s40985-018-0102-y
5. Bajbouj M, Panneck P, Winter S-M, Ajami C, Alabdullah J, Benedikt Burger M, et al. A central clearing clinic to provide mental health services for refugees in Germany. Front Public Heal. (2021) 9:635474. doi: 10.3389/fpubh.2021.635474
6. Müller M, Khamis D, Srivastava D, Exadaktylos AK, Pfortmueller CA. Understanding refugees' health. Semin Neurol. (2018) 38:152–62. doi: 10.1055/s-0038-1649337
7. Steel JL, Dunlavy AC, Harding CE, Theorell T. The psychological consequences of pre-emigration trauma and post-migration stress in refugees and immigrants from Africa. J Immigr Minor Heal. (2017) 19:523–32. doi: 10.1007/s10903-016-0478-z
8. Sangalang CC, Becerra D, Mitchell FM, Lechuga-Peña S, Lopez K, Kim I. Trauma, post-migration stress, and mental health: a comparative analysis of refugees and immigrants in the United States. J Immigr Minor Heal. (2019) 21:909–19. doi: 10.1007/s10903-018-0826-2
9. Hou WK, Liu H, Liang L, Ho J, Kim H, Seong E, et al. Everyday life experiences and mental health among conflict-affected forced migrants: a meta-analysis. J Affect Disord. (2020) 264:50–68. doi: 10.1016/j.jad.2019.11.165
10. Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: a systematic review. Front Psychiatry. (2018) 9:433. doi: 10.3389/fpsyt.2018.00433
11. Turrini G, Purgato M, Ballette F, Nosè M, Ostuzzi G, Barbui C. Common mental disorders in asylum seekers and refugees: umbrella review of prevalence and intervention studies. Int J Ment Health Syst. (2017) 11:51. doi: 10.1186/s13033-017-0156-0
12. Henkelmann J-R, de Best S, Deckers C, Jensen K, Shahab M, Elzinga B, et al. Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych Open. (2020) 6:e68. doi: 10.1192/bjo.2020.54
13. Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med. (2020) 17:e1003337. doi: 10.1371/journal.pmed.1003337
14. Hoell A, Kourmpeli E, Salize HJ, Heinz A, Padberg F, Habel U, et al. Prevalence of depressive symptoms and symptoms of post-traumatic stress disorder among newly arrived refugees and asylum seekers in Germany: systematic review and meta-analysis. BJPsych Open. (2021) 7:e93. doi: 10.1192/bjo.2021.54
15. Satinsky E, Fuhr DC, Woodward A, Sondorp E, Roberts B. Mental health care utilisation and access among refugees and asylum seekers in Europe: a systematic review. Health Policy. (2019) 123:851–63. doi: 10.1016/j.healthpol.2019.02.007
16. Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. (2006) 23:325–48. doi: 10.1093/fampra/cmi113
17. Kiselev N, Morina N, Schick M, Watzke B, Schnyder U, Pfaltz MC. Barriers to access to outpatient mental health care for refugees and asylum seekers in Switzerland: the therapist's view. BMC Psychiatry. (2020) 20:1–14. doi: 10.1186/s12888-020-02783-x
18. van der Boor CF, White R. Barriers to accessing and negotiating mental health services in asylum seeking and refugee populations: the application of the candidacy framework. J Immigr Minor Heal. (2020) 22:156–74. doi: 10.1007/s10903-019-00929-y
19. Byrow Y, Pajak R, Specker P, Nickerson A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: a systematic review. Clin Psychol Rev. (2020) 75:101812. doi: 10.1016/j.cpr.2019.101812
20. Patel V, Chowdhary N, Rahman A, Verdeli H. Improving access to psychological treatments: lessons from developing countries. Behav Res Ther. (2011) 49:523–8. doi: 10.1016/j.brat.2011.06.012
21. Trilesnik B, Altunoz U, Wesolowski J, Eckhoff L, Ozkan I, Loos K, et al. Implementing a need-adapted stepped-care model for mental health of refugees: preliminary data of the state-funded project “Refukey”. Front Psychiatry. (2019) 10:688. doi: 10.3389/fpsyt.2019.00688
22. Munz D, Melcop N. The psychotherapeutic care of refugees in Europe: treatment needs, delivery reality and recommendations for action. Eur J Psychotraumatol. (2018) 9:1476436. doi: 10.1080/20008198.2018.1476436
23. Koesters M, Barbui C, Purgato M. Recent approaches to provision of mental healthcare in refugee populations. Curr Opin Psychiatry. (2018) 31:368–72. doi: 10.1097/YCO.0000000000000428
24. World Health Organization. Scalable Psychological Interventions For People In Communities Affected By Adversity–A New Area Of Mental Health And Psychosocial Work at WHO. Geneva (2017).
25. Rubeis G. [Digital interventions for refugees Challenges, opportunities, and perspectives of agency]. Ethik der Medizin. (2021) 33:335–52. doi: 10.1007/s00481-021-00621-6
26. Muñoz RF, Bunge EL, Chen K, Schueller SM, Bravin JI, Shaughnessy EA, et al. Massive open online interventions: a novel model for delivering behavioral health services worldwide. Clin Psychol Sci. (2016) 4:194–205. doi: 10.1177/2167702615583840
27. Giacco D, Priebe S. Mental health care for adult refugees in high-income countries. Epidemiol Psychiatr Sci. (2018) 27:109–16. doi: 10.1017/S2045796017000609
28. Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Why are health care interventions delivered over the internet? a systematic review of the published literature. J Med Internet Res. (2006) 8:e10. doi: 10.2196/jmir.8.2.e10
29. Carroll KM, Rounsaville BJ. Computer-assisted therapy in psychiatry: be brave - it's a new world. Curr Psychiatry Rep. (2010) 12:426–32. doi: 10.1007/s11920-010-0146-2
30. Andersson G, Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. (2014) 13:4–11. doi: 10.1002/wps.20083
31. Andersson G, Titov N, Dear BF, Rozental A, Carlbring P. Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry. (2019) 18:20–8. doi: 10.1002/wps.20610
32. Rigabert A, Motrico E, Moreno-Peral P, Resurrección DM, Conejo-Cerón S, Cuijpers P, et al. Effectiveness of online psychological and psychoeducational interventions to prevent depression: systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev. (2020) 82:101931. doi: 10.1016/j.cpr.2020.101931
33. Karyotaki E, Efthimiou O, Miguel C, Bermpohl FMG, Furukawa TA, Cuijpers P, et al. Internet-based cognitive behavioral therapy for depression: a systematic review and individual patient data network meta-analysis. JAMA Psychiatry. (2021) 78:361–71. doi: 10.1001/jamapsychiatry.2020.4364
34. Roehr S, Jung FU, Pabst A, Grochtdreis T, Dams J, Nagl M, et al. A self-help app for Syrian refugees with posttraumatic stress (Sanadak): randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9:e24807. doi: 10.2196/24807
35. Lindegaard T, Seaton F, Halaj A, Berg M, Kashoush F, Barchini R, et al. Internet-based cognitive behavioural therapy for depression and anxiety among Arabic-speaking individuals in Sweden: a pilot randomized controlled trial. Cogn Behav Ther. (2020) 50:47–66. doi: 10.1080/16506073.2020.1771414
36. Heim E, Abi Ramia J, Abi Hana R, Burchert S, Carswell K, Cornelisz I, et al. Step-by-step: feasibility randomised controlled trial of a mobile-based intervention for depression among populations affected by adversity in Lebanon. Internet Interv. (2021) 24:100380. doi: 10.1016/j.invent.2021.100380
37. Tay AK, Miah MAA, Khan S, Badrudduza M, Morgan K, Balasundaram S, et al. Theoretical background, first stage development and adaptation of a novel Integrative Adapt Therapy (IAT) for refugees. Epidemiol Psychiatr Sci. (2019) 29:e47. doi: 10.1017/S2045796019000416
38. Koch T, Ehring T, Liedl A. Effectiveness of a transdiagnostic group intervention to enhance emotion regulation in young Afghan refugees: a pilot randomized controlled study. Behav Res Ther. (2020) 132:103689. doi: 10.1016/j.brat.2020.103689
39. Murray LK, Haroz E, Dorsey S, Kane J, Bolton PA, Pullmann MD. Understanding mechanisms of change: an unpacking study of the evidence-based common-elements treatment approach (CETA) in low and middle income countries. Behav Res Ther. (2020) 130:103430. doi: 10.1016/j.brat.2019.103430
40. Morina N, Kuenburg A, Schnyder U, Bryant RA, Nickerson A, Schick M. The association of post-traumatic and postmigration stress with pain and other somatic symptoms: an explorative analysis in traumatized refugees and asylum seekers. Pain Med. (2018) 19:50–9. doi: 10.1093/pm/pnx005
41. Hinton DE, Otto MW. Symptom presentation and symptom meaning among traumatized Cambodian refugees: relevance to a somatically focused cognitive-behavior therapy. Cogn Behav Pract. (2006) 13:249–60. doi: 10.1016/j.cbpra.2006.04.006
42. Rohlof HG, Knipscheer JW, Kleber RJ. Somatization in refugees: a review. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1793–804. doi: 10.1007/s00127-014-0877-1
43. Al-Smadi AM, Tawalbeh LI, Gammoh OS, Ashour A, Tayfur M, Attarian H. The prevalence and the predictors of insomnia among refugees. J Health Psychol. (2019) 24:1125–33. doi: 10.1177/1359105316687631
44. Lies J, Drummond SPA, Jobson L. Longitudinal investigation of the relationships between trauma exposure, post-migration stress, sleep disturbance, and mental health in Syrian refugees. Eur J Psychotraumatol. (2020) 11:1825166. doi: 10.1080/20008198.2020.1825166
45. Jamil H, Hakim-Larson J, Farrag M, Kafaji T, Jamil LH, Hammad A. Medical complaints among Iraqi American refugees with mental disorders. J Immigr Health. (2005) 7:145–52. doi: 10.1007/s10903-005-3671-z
46. Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. (2016) 142:969–90. doi: 10.1037/bul0000053
47. Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. (2008) 12:169–84. doi: 10.1016/j.smrv.2007.08.008
48. Lies J, Jones L, Ho R. The management of post-traumatic stress disorder and associated pain and sleep disturbance in refugees. BJPsych Adv. (2019) 25:196–206. doi: 10.1192/bja.2019.7
49. Lies J, Mellor A, Jobson L, Drummond SPA. Prevalence of sleep disturbance and its relationships with mental health and psychosocial issues in refugees and asylum seekers attending psychological services in Australia. Sleep Heal. (2019) 5:335–43. doi: 10.1016/j.sleh.2019.06.002
50. Furukawa TA, Suganuma A, Ostinelli EG, Andersson G, Beevers CG, Shumake J, et al. Dismantling, optimising, and personalising internet cognitive behavioural therapy for depression: a systematic review and component network meta-analysis using individual participant data. Lancet Psychiatry. (2021) 8:500–11. doi: 10.1016/S2215-0366(21)00077-8
51. Cheng P, Kalmbach DA, Tallent G, Joseph CLM, Espie CA, Drake CL. Depression prevention via digital cognitive behavioral therapy for insomnia: a randomized controlled trial. Sleep. (2019) 42:zsz150. doi: 10.1093/sleep/zsz150
52. Stott R, Pimm J, Emsley R, Miller CB, Espie CA. Does adjunctive digital CBT for insomnia improve clinical outcomes in an improving access to psychological therapies service? Behav Res Ther. (2021) 144:103922. doi: 10.1016/j.brat.2021.103922
53. Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry. (2016) 3:333–41. doi: 10.1016/S2215-0366(15)00536-2
54. Harvey AG, Dong L, Hein K, Yu SH, Martinez AJ, Gumport NB, et al. A randomized controlled trial of the transdiagnostic intervention for sleep and circadian dysfunction (TranS-C) to improve serious mental illness outcomes in a community setting. J Consult Clin Psychol. (2021) 89:537–50. doi: 10.1037/ccp0000650
55. Jespersen KV, Vuust P. The effect of relaxation music listening on sleep quality in traumatized refugees: a pilot study. J Music Ther. (2012) 49:205–29. doi: 10.1093/jmt/49.2.205
56. Bernal G, Jiménez-Chafey MI, Domenech Rodríguez MM. Cultural adaptation of treatments: a resource for considering culture in evidence-based practice. Prof Psychol Res Pract. (2009) 40:361–8. doi: 10.1037/a0016401
57. Schnyder U, Bryant RA, Ehlers A, Foa EB, Hasan A, Mwiti G, et al. Culture-sensitive psychotraumatology. Eur J Psychotraumatol. (2016) 7:31179. doi: 10.3402/ejpt.v7.31179
58. Castro FG, Barrera M, Steiker LKH. Issues and challenges in the design of culturally adapted evidence-based interventions. Annu Rev Clin Psychol. (2010) 6:213–39. doi: 10.1146/annurev-clinpsy-033109-132032
59. Jalal B, Samir SW, Hinton DE. Adaptation of CBT for traumatized Egyptians: examples from culturally adapted CBT (CA-CBT). Cogn Behav Pract. (2017) 24:58–71. doi: 10.1016/j.cbpra.2016.03.001
60. Barrera M, Castro FG. A heuristic framework for the cultural adaptation of interventions. Clin Psychol Sci Pract. (2006) 13:311–6. doi: 10.1111/j.1468-2850.2006.00043.x
61. Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research - issues for the cultural adaptation and development of psychosocial treatments with hispanics. J Abnorm Child Psychol. (1995) 23:67–82. doi: 10.1007/BF01447045
62. Sangraula M, Kohrt BA, Ghimire R, Shrestha P, Luitel NP, Hof EV, et al. Development of the mental health cultural adaptation and contextualization for implementation (mhCACI) procedure: a systematic framework to prepare evidence-based psychological interventions for scaling. Glob Ment Heal. (2021) 8:e6. doi: 10.1017/gmh.2021.5
63. Heim E, Kohrt BA. Cultural adaptation of scalable psychological interventions: a new conceptual framework. Clin Psychol Eur. (2019) 1:e37679. doi: 10.32872/cpe.v1i4.37679
64. Spanhel K, Balci S, Feldhahn F, Bengel J, Baumeister H, Sander LB. Cultural adaptation of internet- and mobile-based interventions for mental disorders: a systematic review. NPJ Digit Med. (2021) 4:128. doi: 10.1038/s41746-021-00498-1
65. Hall GCN, Ibaraki AY, Huang ER, Marti CN, Stice E. A meta-analysis of cultural adaptations of psychological interventions. Behav Ther. (2016) 47:993–1014. doi: 10.1016/j.beth.2016.09.005
66. Anik E, West RM, Cardno AG, Mir G. Culturally adapted psychotherapies for depressed adults: a systematic review and meta-analysis. J Affect Disord. (2021) 278:296–310. doi: 10.1016/j.jad.2020.09.051
67. Harper Shehadeh MJ, Heim E, Chowdhary N, Maercker A, Albanese E. Cultural adaptation of minimally guided interventions for common mental disorders: a systematic review and meta-analysis. JMIR Ment Heal. (2016) 3:e44. doi: 10.2196/mental.5776
68. Abi Ramia J, Harper Shehadeh M, Kheir W, Zoghbi E, Watts S, Heim E, et al. Community cognitive interviewing to inform local adaptations of an e-mental health intervention in Lebanon. Glob Ment Heal. (2018) 5:e39. doi: 10.1017/gmh.2018.29
69. Nygren T, Berg M, Sarkohi A, Andersson G. Development of an internet-based cognitive behavioral therapy self-help program for arabic-speaking immigrants: mixed-methods study. JMIR Res Protoc. (2018) 7:e11872. doi: 10.2196/11872
70. Burchert S, Alkneme MS, Bird M, Carswell K, Cuijpers P, Hansen P, et al. User-centered app adaptation of a low-intensity e-mental health intervention for Syrian refugees. Front Psychiatry. (2019) 9:663. doi: 10.3389/fpsyt.2018.00663
71. Harper Shehadeh MJ, Abi Ramia J, Cuijpers P, El Chammay R, Heim E, Kheir W, et al. Step-by-Step, an e-mental health intervention for depression: a mixed methods pilot study from Lebanon. Front Psychiatry. (2020) 10:986. doi: 10.3389/fpsyt.2019.00986
72. Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. (2016) 355:i5239. doi: 10.1136/bmj.i5239
73. Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS ONE. (2010) 5:e13196. doi: 10.1371/journal.pone.0013196
74. Schulz KF, Altman DG, Moher D, the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Intern Med. (2010) 152:726–32. doi: 10.7326/0003-4819-152-11-201006010-00232
75. Ebert DD, Berking M, Thiart H, Riper H, Laferton JAC, Cuijpers P, et al. Restoring depleted resources: efficacy and mechanisms of change of an internet-based unguided recovery training for better sleep and psychological detachment from work. Heal Psychol. (2015) 34:1240–51. doi: 10.1037/hea0000277
76. Thiart H, Lehr D, Ebert DD, Berking M, Riper H. Log in and breathe out: internet-based recovery training for sleepless employees with work-related strain – results of a randomized controlled trial. Scand J Work Environ Heal. (2015) 41:164–74. doi: 10.5271/sjweh.3478
77. Behrendt D, Ebert DD, Spiegelhalder K, Lehr D. Efficacy of a self-help web-based recovery training in improving sleep in workers: randomized controlled trial in the general working population. J Med Internet Res. (2020) 22:e13346. doi: 10.2196/13346
78. Spanhel K, Schweizer JS, Wirsching D, Lehr D, Baumeister H, Bengel J, et al. Cultural adaptation of internet interventions for refugees: results from a user experience study in Germany. Internet Interv. (2019) 18:100252. doi: 10.1016/j.invent.2019.100252
79. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5 - Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). Arlington, VA: American Psychiatric Association (2015).
80. Boß L, Lehr D, Reis D, Vis C, Riper H, Berking M, et al. Reliability and validity of assessing user satisfaction with web-based health interventions. J Med Internet Res. (2016) 18:e234. doi: 10.2196/jmir.5952
81. Spanhel K, Burdach D, Pfeiffer T, Lehr D, Spiegelhalder K, Ebert DD, et al. Effectiveness of an internet-based intervention to improve sleep difficulties in a culturally diverse sample of international students: a randomised controlled pilot study. J Sleep Res. (2021) 00:e13493. doi: 10.1111/jsr.13493
82. Bastien CH, Valliéres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
83. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
84. Pruiksma KE, Taylor DJ, Ruggero C, Boals A, Davis JL, Cranston C, et al. A psychometric study of the fear of sleep inventory-short form (FoSI-SF). J Clin Sleep Med. (2014) 10:551–8. doi: 10.5664/jcsm.3710
85. Smets EMA, Garssen B, Bonke B, De Haes JCJM. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. (1995) 39:315–25. doi: 10.1016/0022-3999(94)00125-O
86. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
87. Hollifield M, Verbillis-Kolp S, Farmer B, Toolson EC, Woldehaimanot T, Yamazaki J, et al. The refugee health screener-15 (RHS-15): development and validation of an instrument for anxiety, depression, and PTSD in refugees. Gen Hosp Psychiatry. (2013) 35:202–9. doi: 10.1016/j.genhosppsych.2012.12.002
88. Dias P, Campos L, Almeida H, Palha F. Mental health literacy in young adults: adaptation and psychometric properties of the mental health literacy questionnaire. Int J Environ Res Public Health. (2018) 15:1318–30. doi: 10.3390/ijerph15071318
89. Rozental A, Kottorp A, Forsström D, Månsson K, Boettcher J, Andersson G, et al. The negative effects questionnaire: psychometric properties of an instrument for assessing negative effects in psychological treatments. Behav Cogn Psychother. (2019) 47:559–72. doi: 10.1017/S1352465819000018
90. Rozental A, Kottorp A, Boettcher J, Andersson G, Carlbring P. Negative effects of psychological treatments: an exploratory factor analysis of the negative effects questionnaire for monitoring and reporting adverse and unwanted events. PLoS ONE. (2016) 11:e0157503. doi: 10.1371/journal.pone.0157503
91. Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. (2002) 56:588–94. doi: 10.1136/jech.56.8.588
92. Hedges L, Olkin I. Statistical Methods For Meta-Analysis. London: Academic Press Inc. (1985). p. 368.
93. Hinton DE, Jalal B. Guidelines for the implementation of culturally sensitive cognitive behavioural therapy among refugees and in global contexts. Intervention. (2014) 12:78–93. doi: 10.1097/WTF.0000000000000069
94. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. (2017) 26:675–700. doi: 10.1111/jsr.12594
95. Lindegaard T, Kashoush F, Holm S, Halaj A, Berg M, Andersson G. Experiences of internet-based cognitive behavioural therapy for depression and anxiety among Arabic-speaking individuals in Sweden: a qualitative study. BMC Psychiatry. (2021) 21:288. doi: 10.1186/s12888-021-03297-w
96. Lies J, Jobson L, Mascaro L, Whyman T, Drummond SPA. Postmigration stress and sleep disturbances mediate the relationship between trauma exposure and posttraumatic stress symptoms among Syrian and Iraqi refugees. J Clin Sleep Med. (2021) 17:479–89. doi: 10.5664/jcsm.8972
97. Baumeister H, Kraft R, Baumel A, Pryss R, Messner E-M. Persuasive e-health design for behavior change. In: Baumeister H, Montag C, editors. Digital Phenotyping and Mobile Sensing Studies in Neuroscience, Psychology and Behavioral Economics. Cham: Springer (2019). p. 261–76. doi: 10.1007/978-3-030-31620-4_17
98. Moshe I, Terhorst Y, Philippi P, Domhard M, Cuijpers P, Cristea I, et al. Digital interventions for the treatment of depression: a meta-analytic review. Psychol Bull. (2021) 147:749–86. doi: 10.1037/bul0000334
99. Ramos G, Chavira DA. Use of technology to provide mental health care for racial and ethnic minorities: evidence, promise, and challenges. Cogn Behav Pract. (2019). doi: 10.1016/j.cbpra.2019.10.004
100. Bur OT, Krieger T, Moritz S, Klein JP, Berger T. Optimizing the context of support to improve outcomes of internet-based self-help in individuals with depressive symptoms: protocol for a randomized factorial trial. JMIR Res Protoc. (2021) 10:e21207. doi: 10.2196/21207
101. Watkins ER, Newbold A. Factorial designs help to understand how psychological therapy works. Front Psychiatry. (2020) 11:429. doi: 10.3389/fpsyt.2020.00429
102. Domhardt M, Cuijpers P, Ebert DD, Baumeister H. More light? opportunities and pitfalls in digitalized psychotherapy process research. Front Psychol. (2021) 12:544129. doi: 10.3389/fpsyg.2021.544129
103. Domhardt M, Steubl L, Boettcher J, Buntrock C, Karyotaki E, Ebert DD, et al. Mediators and mechanisms of change in internet- and mobile-based interventions for depression: a systematic review. Clin Psychol Rev. (2021) 83:101953. doi: 10.1016/j.cpr.2020.101953
104. Roehr S, Wittmann F, Jung F, Hoffmann R, Renner A, Dams J, et al. Strategies to recruit refugees for intervention studies: lessons learned from the “Sanadak" trial. Psychother Psychosom Med Psychol. (2019) 69:484–9. doi: 10.1055/a-1030-4570
Keywords: culturally sensitive treatment, refugees, healthcare barriers, sleep disturbances, transdiagnostic symptoms, internet-based interventions, low-threshold treatment
Citation: Spanhel K, Hovestadt E, Lehr D, Spiegelhalder K, Baumeister H, Bengel J and Sander LB (2022) Engaging Refugees With a Culturally Adapted Digital Intervention to Improve Sleep: A Randomized Controlled Pilot Trial. Front. Psychiatry 13:832196. doi: 10.3389/fpsyt.2022.832196
Received: 09 December 2021; Accepted: 31 January 2022;
Published: 23 February 2022.
Edited by:
Rahul Shidhaye, Pravara Institute of Medical Sciences, IndiaReviewed by:
Yesim Erim, University of Erlangen-Nuremberg, GermanyNele A. J. De Witte, Thomas More University of Applied Sciences, Belgium
Copyright © 2022 Spanhel, Hovestadt, Lehr, Spiegelhalder, Baumeister, Bengel and Sander. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kerstin Spanhel, a2Vyc3Rpbi5zcGFuaGVsQHBzeWNob2xvZ2llLnVuaS1mcmVpYnVyZy5kZQ==
 Kerstin Spanhel
Kerstin Spanhel Eva Hovestadt1
Eva Hovestadt1 Dirk Lehr
Dirk Lehr Kai Spiegelhalder
Kai Spiegelhalder Harald Baumeister
Harald Baumeister Lasse B. Sander
Lasse B. Sander