
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Psychiatry , 10 March 2022
Sec. Psychopathology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.830218
This article is part of the Research Topic Violent Relationships: Acute and Long-term Implications View all 8 articles
Experiencing traumatic events has a high lifetime prevalence ranging between 60.7 and 76.2% across different countries (1). Exposure to traumatic events is associated with a higher risk for various mental disorders such as posttraumatic stress disorder (2, 3), which are related to high individual and societal costs (4). The development of interventions to prevent adverse mental health consequences following traumatic event exposure is therefore of vital importance. This, however, requires detailed knowledge about the underlying biological and psychological mechanisms involved in the association between traumatic events and psychopathology. Various risk factors at different levels have already been described in the last decades (5). Biological risk factors include genetic and epigenetic variations (6), alterations in the function of the hypothalamic pituitary adrenal (HPA) axis (7, 8) and the autonomic nervous system (9) as well as changes in brain structure and functioning (10). Psychological risk factors include impairments in cognitive abilities (11) and specific personality traits such as high trait anxiety (12) and maladaptive emotion regulation (13). Social risk factors include impaired interpersonal relations and stigmatization (14, 15). Further, clinical risk factors such as mental health history as well as previous traumatic experiences may also increase the risk for psychopathology after trauma exposure (16). Most of these factors are supposed to be associated with risk of psychopathology independent of the type of traumatic event. However, it is likely that specific traumatic events are associated with different constellations of risk factors, which has so far received little attention in the existing literature. Importantly, traumatic events explicitly include not only events that are personally experienced but also events that are witnessed by an observer (17). This includes witnessing someone being seriously hurt, seeing atrocities or witnessing dead bodies. Witnessed traumatic events are among the most frequent traumatic experiences (1). They are also of high current relevance in the contexts of natural disasters, terrorist attacks and military crises (16, 18, 19). The fact that individuals can develop psychopathological reactions to events that are actually experienced by others raises the question how the suffering of others is being processed. Based on theoretical models and findings from social cognition and neuroscience research, we propose that socio-affective and socio-cognitive mechanisms are involved in the processing and pathological consequences of witnessing traumatic events and could contribute to a better understanding of adverse reactions to this type of traumatic events.
There is solid evidence for the tendency to psycho-physiologically resonate with others' stress responses (20). This linkage with an observed individual that is experiencing adverse events can be associated with stress reactions in the observer (21, 22). Importantly, this linkage between target and observer has been closely related to the constructs of empathy and perspective-taking (also referred to as Theory of Mind or mentalizing). Empathy denotes the sharing of another person's emotions and can thus be defined as an affective state in an observer that is isomorphic to an observed person's affective state (23). Perspective-taking enables the reasoning about and understanding of others' mental states, including their emotions (24) and can modulate empathic responding (25). Adaptive social interaction critically depends on these capacities to understand and feel with others and most empirical evidence associates perspective-taking and empathy with positive health outcomes. Empathy is associated with better relationship quality (26), greater professional satisfaction (27), and emotional self-efficacy (28), with all of these factors being associated with positive mental health (29). Empathy is also proposed to be a healthy and efficient method of interpersonal emotion regulation (30). More specifically, there is first evidence that empathy is related to resilience after secondary exposure to traumatic events (31). On the other hand, there is also evidence for a relationship between empathy and adverse mental health symptoms such as depression (32) and anxiety (33). Moreover, empathy was found to be related to secondary trauma in caregivers (34, 35) and physicians (36, 37) and also with higher levels of traumatic stress symptoms (38, 39). Thus, it can be assumed that empathic responding is only an initial processing step that can be followed by diverging socio-affective and socio-cognitive functions, representing two distinct pathways resulting in either negative or positive mental health outcomes (Figure 1).
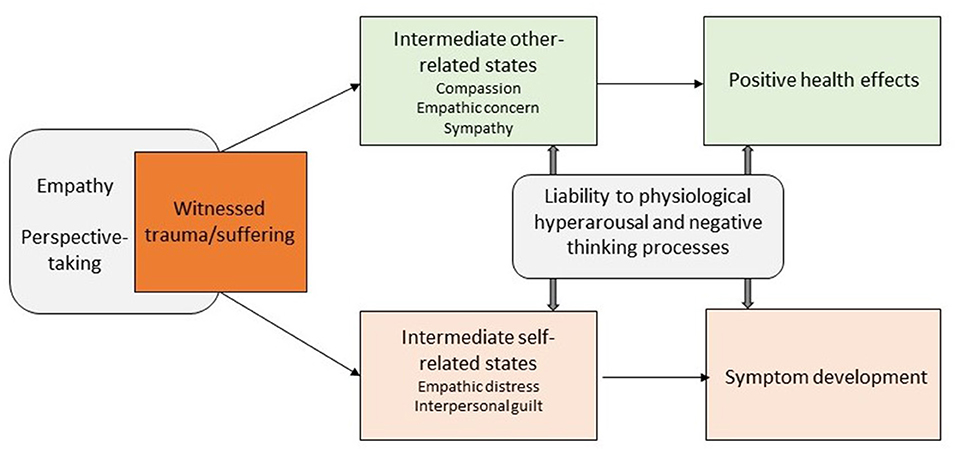
Figure 1. Proposed socio-affective and socio-cognitive mechanism and pathways in the processing of witnessed traumatic events [based on (37, 41)].
As described above, empathy and perspective-taking may lead the observer to feel positive, caring emotions for the suffering other (upper path in Figure 1). These emotions, which form intrinsically other-related states (40), have been studied as compassion, empathic concern or sympathy. Training studies have shown that compassion can be cultivated, increasing not only subjective reports of positive affect toward others, but also prosocial helping behavior (41, 42). As for compassion, it is conceptualized as a qualitatively different state than empathic distress, one that can be actively generated (43). It may be explicitly cultivated as is done, for instance, in compassion focused therapy (44). It may also arise spontaneously, but not automatically when there is no empathic distress (45, 46). Compassion also varies greatly in untrained individuals, with stronger compassionate responding being again associated with more prosocial behavior (47). Furthermore, trait levels of (self-) compassion have been related to stress-buffering and anti-depressant effects (48) and were associated with mental health and recovery from adverse events (49, 50) and with lower PTSD symptoms after witnessed trauma (51). For the context of traumatic stress research, these results suggest that these other-related states may be promising candidates that could partially explain resilience after witnessing of traumatic events.
A second possible outcome of initial perspective-taking and empathic sharing of another's suffering is, however, an elevated risk of adverse reactions including symptom development (lower path in Figure 1). Recent theoretical models (37) suggest that developmental trajectories from empathic tendencies to symptom development encompass two intermediate conditions: empathic distress and interpersonal guilt. In contrast to the other-related states described above, empathic distress and interpersonal guilt are negative states that are intrinsically self-related. Because it shares the negative valence with the initial empathic response to others' suffering, empathic distress may be viewed as an excessive form of empathy and is characterized by increased arousal, stress responses and fear (52). Interpersonal guilt could be viewed as a maladaptive form of cognitive empathy that is driven by excessive concerns, such as unreasonable beliefs that one is responsible for alleviating the suffering of others (53). Both empathic distress and interpersonal guilt may contribute to a higher risk of later psychopathology (41, 54, 55). Thus, in the context of witnessing trauma, empathic distress and interpersonal guilt may be important mediators of adverse reactions and psychopathological symptoms.
The association between empathy and mental health is likely to be non-linear with moderate levels being related to beneficial and high levels to adverse outcomes (37). In addition, previous research suggests that the outcome of empathic responding is further moderated by (1) liability to physiological hyperarousal and (2) liability to negative thinking processes (see Figure 1). Liability to high physiological arousal characterized by alterations in basal endocrine (e.g., basal cortisol secretion) and autonomic changes (e.g., heart rate variability) has been associated with symptom development after exposure to direct and observed stressful experiences (7, 56, 57). Liability to negative thinking processes includes the predisposition to self-focused rumination and poor regulation of cognitive processes (e.g., cognitive inflexibility, impaired ability to suppress negative thoughts) conceptualized as stable traits. They have been associated with poor coping and symptom development in the context of stress exposure and witnessed trauma (58–60). Taken together, these findings suggest that empathic distress and its adverse consequences might be the result of a liability to empathic sensitivity which interacts with a liability to physiological hyperarousal and negative thinking processes.
A sound investigation of potential socio-affective mechanisms of witnessed trauma including its moderators requires experimental designs to be able to manipulate the independent variable (witnessed trauma) and to take into account the existence of potential confounding factors. In recent years, laboratory models of witnessed trauma such as the trauma film paradigm have been developed and successfully implemented in various studies (61). However, it must be considered that the external validity of such trauma analog studies is limited. Therefore, there is a need to test hypotheses also with other study designs such as prospective cohort studies or cohort studies in recently trauma exposed individuals. To elucidate which factors contribute to either beneficial or adverse pathways of empathic processes after witnessed trauma, a social cognitive and affective neuroscience approach could also be particularly valuable (62). Perspective-taking, empathy, compassion and empathic distress are dissociable on interindividual, intraindividual developmental and neural levels (63, 64). Perspective-taking activates regions in the temporoparietal junction and anterior and posterior midline structures (65), while different networks are involved in sharing different emotions. For sharing others pain and negative emotions in general, it is especially the anterior insula, anterior cingulate cortex, and amygdala that are involved (46). Empathic distress may include activation change in the anterior insula and cingulate cortex, but also in the amygdala and hippocampus as has been shown for first-hand stress experience (66, 67). Compassion, in contrast, activates a network typically involved in positive affect and reward processing including the ventral striatum and medial orbitofrontal cortex (47). Probing the neural responding to witnessing traumatic events would enable the objective assessment of perspective-taking, empathic affect sharing, compassion and empathic distress as potential predictors of later symptom development. In addition to neuroimaging methods, there are well-validated and reliable paradigms for behavioral assessments of socio-cognitive and socio-affective processes such as compassion, empathic concern and perspective-taking (theory of mind) (68). For instance, the EmpaToM task presents videos of short autobiographic narrations that vary in emotion and perspective-taking demands (68, 69). These enable the assessment of socio-affective and -cognitive functioning with meaningful variability in health and psychopathology that also relates to everyday functioning (70, 71). Lastly, genetic contributions might be a valuable target to explain differences in empathic sensitivity (37) and could serve as potential biological risk markers.
Witnessed traumatic events are highly prevalent and can cause high individual and societal burden. In addition to known risk factors for symptom development, socio-affective, and socio-cognitive mechanisms could play a crucial role for the processing of such events. Perspective-taking and empathic responding are initial processing steps, followed by diverging socio-affective functions, which are associated with either negative or positive affective and health outcomes. Although these proposed trajectories are still merely theoretical and evidence supporting the specificity of the suggested mechanisms beyond known concepts of risk and resilience is scarce, they present highly valuable targets for future research. Confirming different socio-affective pathways, their dissection on the neural level and the identification of biological and psychological factors that contribute to these different pathways could improve the prediction of adverse reactions to witnessed trauma.
ST developed the concept and wrote the paper. CW contributed to the writing of the paper and revised the paper for important intellectual content. MM revised the paper for important intellectual content. PK contributed to the concept and revised the paper for important intellectual content. All authors approved the final manuscript for publication.
ST and PK are supported by the German Research Foundation (TR1489/1-1, KA 4412/2-1, KA 4412/4-1, KA 4412/5-1, and CRC940/C07).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. (2016) 46:327–43. doi: 10.1017/S0033291715001981
2. Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, et al. Cumulative traumas and risk thresholds: 12-month PTSD in the World Mental Health (WMH) surveys. Depress Anxiety. (2014) 31:130–42. doi: 10.1002/da.22169
3. McLaughlin KA, Koenen KC, Friedman MJ, Ruscio AM, Karam EG, Shahly V, et al. Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biol Psychiatry. (2015) 77:375–84. doi: 10.1016/j.biopsych.2014.03.028
4. Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. (2000) 61:4–14. doi: 10.4088/JCP.v61n0713e
5. DiGangi JA, Gomez D, Mendoza L, Jason LA, Keys CB, Koenen KC. Pretrauma risk factors for posttraumatic stress disorder: a systematic review of the literature. Clin Psychol Rev. (2013) 33:728–44. doi: 10.1016/j.cpr.2013.05.002
6. Duncan LE, Cooper BN, Shen H. Robust findings from 25 years of PTSD genetics research. Curr Psychiatry Rep. (2018) 20:1–9. doi: 10.1007/s11920-018-0980-1
7. Steudte-Schmiedgen S, Stalder T, Schönfeld S, Wittchen H-U, Trautmann S, Alexander N, et al. Hair cortisol concentrations and cortisol stress reactivity predict PTSD symptom increase after trauma exposure during military deployment. Psychoneuroendocrinology. (2015) 59:123–33. doi: 10.1016/j.psyneuen.2015.05.007
8. Trautmann S, Muehlhan M, Kirschbaum C, Wittchen HU, Höfler M, Stalder T, et al. Biological stress indicators as risk markers for increased alcohol use following traumatic experiences. Addict Biol. (2018) 23:281–90. doi: 10.1111/adb.12487
9. Schneider M, Schwerdtfeger A. Autonomic dysfunction in posttraumatic stress disorder indexed by heart rate variability: a meta-analysis. Psychol Med. (2020) 50:1937–48. doi: 10.1017/S003329172000207X
10. Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. (2007) 164:1476–88. doi: 10.1176/appi.ajp.2007.07030504
11. Germine LT, Joormann J, Passell E, Rutter LA, Scheuer L, Martini P, et al. Neurocognition after motor vehicle collision and adverse post-traumatic neuropsychiatric sequelae within 8 weeks: initial findings from the AURORA study. J Affect Disord. (2021) 298:57–67. doi: 10.1016/j.jad.2021.10.104
12. Jakšić N, Brajković L, Ivezić E, Topić R, Jakovljević M. The role of personality traits in posttraumatic stress disorder (PTSD). Psychiatr Danubina. (2012) 24:256–66.
13. Seligowski AV, Lee DJ, Bardeen JR, Orcutt HK. Emotion regulation and posttraumatic stress symptoms: a meta-analysis. Cogn Behav Ther. (2015) 44:87–102. doi: 10.1080/16506073.2014.980753
14. Thomas S, Hummel KV, Schäfer J, Wittchen HU, Trautmann S. The role of harassment and group cohesion for depressive and anxiety symptoms. Can J Behav Sci. (2021). doi: 10.1037/cbs0000283. [Epub ahead of print].
15. Thomas S, Hummel K, Schäfer J, Wittchen HU, Trautmann S. Harassment and its association with depressive symptoms and suicidal behavior: the role of perceived stigma and non-disclosure. Psychol Serv. (2021). doi: 10.1037/ser0000610. [Epub ahead of print].
16. Kessler RC, Rose S, Koenen KC, Karam EG, Stang PE, Stein DJ, et al. How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO World Mental Health Surveys. World Psychiatry. (2014) 13:265–74. doi: 10.1002/wps.20150
17. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Edn. Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
18. Holman EA, Garfin DR, Silver RC. Media's role in broadcasting acute stress following the Boston Marathon bombings. Proc Nat Acad Sci USA. (2014) 111:93–8. doi: 10.1073/pnas.1316265110
19. Monfort E, Afzali MH. Traumatic stress symptoms after the November 13th 2015 terrorist attacks among young adults: the relation to media and emotion regulation. Compr Psychiatry. (2017) 75:68–74. doi: 10.1016/j.comppsych.2017.02.015
20. Engert V, Linz R, Grant JA. Embodied stress: the physiological resonance of psychosocial stress. Psychoneuroendocrinology. (2019) 105:138–46. doi: 10.1016/j.psyneuen.2018.12.221
21. Buchanan L, Bushroe K, Malthaner L, McCarthy T, Zhao S, Hade E, et al. Test accuracy of the screening tool for early predictors of post-traumatic stress disorder for post-injury mental health in a managed-medicaid population. J Pediatr. (2019) 210:127–33. doi: 10.1016/j.jpeds,.2019.03.016
22. Hein G, Singer T. I feel how you feel but not always: the empathic brain and its modulation. Curr Opin Neurobiol. (2008) 18:153–8. doi: 10.1016/j.conb.2008.07.012
23. De Vignemont F, Singer T. The empathic brain: how, when and why? Trends Cogn Sci. (2006) 10:435–41. doi: 10.1016/j.tics.2006.08.008
25. Lamm C, Batson CD, Decety J. The neural substrate of human empathy: effects of perspective-taking and cognitive appraisal. J Cogn Neurosci. (2007) 19:42–58. doi: 10.1162/jocn.2007.19.1.42
26. Coutinho JF, Silva PO, Decety J. Neurosciences, empathy, and healthy interpersonal relationships: recent findings and implications for counseling psychology. J Couns Psychol. (2014) 61:541. doi: 10.1037/cou0000021
27. Halpern J. What is clinical empathy? J Gen Intern Med. (2003) 18:670–4. doi: 10.1046/j.1525-1497.2003.21017.x
28. Goroshit M, Hen M. Does emotional self-efficacy predict teachers' self-efficacy and empathy? J Educ Train Stud. (2014) 2:26–32. doi: 10.11114/jets.v2i3.359
29. Wacker R, Dziobek I. Preventing empathic distress and social stressors at work through nonviolent communication training: a field study with health professionals. J Occup Health Psychol. (2018) 23:141. doi: 10.1037/ocp0000058
30. Zaki J. Integrating empathy and interpersonal emotion regulation. Annu Rev Psychol. (2020) 71:517–40. doi: 10.1146/annurev-psych-010419-050830
31. Morice-Ramat A, Goronflot L, Guihard G. Are alexithymia and empathy predicting factors of the resilience of medical residents in France? Int J Med Educ. (2018) 9:122. doi: 10.5116/ijme.5ac6.44ba
32. Zhang W, Li H, Gong Y, Ungar M. Stressful events and depression among Chinese adolescents: the mitigating role of protective factors. Sch Psychol Int. (2013) 34:501–13. doi: 10.1177/0143034312472760
33. Gambin M, Sharp C. Relations between empathy and anxiety dimensions in inpatient adolescents. Anxiety Stress Coping. (2018) 31:447–58. doi: 10.1080/10615806.2018.1475868
34. Kim K. To feel or not to feel: empathy and physician burnout. Acad Psychiatry. (2018) 42:157–8. doi: 10.1007/s40596-017-0871-5
35. Ogińska-Bulik N, Juczyński Z, Michalska P. The mediating role of cognitive trauma processing in the relationship between empathy and secondary traumatic stress symptoms among female professionals working with victims of violence. J Interpers Violence. (2020) 37:1197–225. doi: 10.1177/0886260520976211
36. Mottaghi S, Poursheikhali H, Shameli L. Empathy, compassion fatigue, guilt and secondary traumatic stress in nurses. Nurs Ethics. (2020) 27:494–504. doi: 10.1177/0969733019851548
37. Tone EB, Tully EC. Empathy as a “risky strength”: a multilevel examination of empathy and risk for internalizing disorders. Dev Psychopathol. (2014) 26:1547–65. doi: 10.1017/S0954579414001199
38. Arnold TC. An evolutionary concept analysis of secondary traumatic stress in nurses. Nursing Forum. (2020) 55:149–56. doi: 10.1111/nuf.12409
39. Sheen K, Slade P, Spiby H. An integrative review of the impact of indirect trauma exposure in health professionals and potential issues of salience for midwives. J Adv Nurs. (2014) 70:729–43. doi: 10.1111/jan.12274
40. Zickfeld JH, Schubert TW, Seibt B, Fiske AP. Empathic concern is part of a more general communal emotion. Front Psychol. (2017) 8:723. doi: 10.3389/fpsyg.2017.00723
41. Klimecki O, Singer T. Empathic distress fatigue rather than compassion fatigue: Integrating findings from empathy research in psychology and social neuroscience. In: Oakley B, Knafo A, Madhavan G, Wilson DS, editors. Pathological Altruism. Oxford University Press (2012). p. 368–83.
42. Trautwein F-M, Kanske P, Böckler A, Singer T. Differential benefits of mental training types for attention, compassion, and theory of mind. Cognition. (2020) 194:104039. doi: 10.1016/j.cognition.2019.104039
43. Singer T, Klimecki OM. Empathy and compassion. Curr Biol. (2014) 24:R875–8. doi: 10.1016/j.cub.2014.06.054
44. Gilbert P. Introducing compassion-focused therapy. Adv Psychiatr Treat. (2009) 15:199–208. doi: 10.1192/apt.bp.107.005264
45. Engen HG, Singer T. Compassion-based emotion regulation up-regulates experienced positive affect and associated neural networks. Soc Cogn Affect Neurosci. (2015) 10:1291–301. doi: 10.1093/scan/nsv008
46. Kanske P, Böckler A, Trautwein F-M, Singer T. Dissecting the social brain: introducing the EmpaToM to reveal distinct neural networks and brain-behavior relations for empathy and theory of mind. Neuroimage. (2015) 122:6–19. doi: 10.1016/j.neuroimage.2015.07.082
47. Ashar YK, Andrews-Hanna JR, Dimidjian S, Wager TD. Empathic care and distress: predictive brain markers and dissociable brain systems. Neuron. (2017) 94:1263–73. doi: 10.1016/j.neuron.2017.05.014
48. Trzeciak S, Roberts BW, Mazzarelli AJ. Compassionomics: hypothesis and experimental approach. Med Hypotheses. (2017) 107:92–7. doi: 10.1016/j.mehy.2017.08.015
49. Raque-Bogdan TL, Ericson SK, Jackson J, Martin HM, Bryan NA. Attachment and mental and physical health: self-compassion and mattering as mediators. J Couns Psychol. (2011) 58:272. doi: 10.1037/a0023041
50. Spandler H, Stickley T. No hope without compassion: the importance of compassion in recovery-focused mental health services. J Mental Health. (2011) 20:555–66. doi: 10.3109/09638237.2011.583949
51. Moss J, Roberts MB, Shea L, Jones CW, Kilgannon H, Edmondson DE, et al. Healthcare provider compassion is associated with lower PTSD symptoms among patients with life-threatening medical emergencies: a prospective cohort study. Intens Care Med. (2019) 45:815–22. doi: 10.1007/s00134-019-05601-5
52. Eisenberg N, Shea CL, Carlo G, Knight GP. Empathy-related responding and cognition: A “chicken and the egg” dilemma. In: Kurtines WM, Gewirtz JL, editors, Handbook of Moral Behavior and Development, Vol. 1. Princeton, NJ: Lawrence Erlbaum Associates (1991). p. 63–88.
53. Oakley B, Knafo A, Madhavan G, Wilson DS. Pathological Altruism. Oxford University Press (2011). doi: 10.1093/acprof:oso/9780199738571.001.0001
54. Haag A-C, Zehnder D, Landolt MA. Guilt is associated with acute stress symptoms in children after road traffic accidents. Eur J Psychotraumatol. (2015) 6:29074. doi: 10.3402/ejpt.v6.29074
55. Trautmann S, Reineboth M, Trikojat K, Richter J, Hagenaars MA, Kanske P, et al. Susceptibility to others' emotions moderates immediate self-reported and biological stress responses to witnessing trauma. Behav Res Ther. (2018) 110:55–63. doi: 10.1016/j.brat.2018.09.001
56. Muscatell KA, Eisenberger NI. A social neuroscience perspective on stress and health. Soc Pers Psychol Compass. (2012) 6:890–904. doi: 10.1111/j.1751-9004.2012.00467.x
57. Trautmann S, Kräplin A, Dieterich R, Richter J, Muehlhan M. The role of childhood trauma and stress reactivity for increased alcohol craving after induced psychological trauma: an experimental analogue study. Psychopharmacology. (2018) 235:2883–95. doi: 10.1007/s00213-018-4979-4
58. Abramson LY, Alloy LB, Hankin BL, Haeffel GJ, MacCoon DG, Gibb BE. Cognitive vulnerability-stress models of depression in a self-regulatory and psychobiological context. In: Gotlib IH, Hammen CL, editors, Handbook of Depression. New York, NY: The Guilford Press (2002). p. 268–294.
59. Fu F, Chow A. Traumatic exposure and psychological well-being: the moderating role of cognitive flexibility. J Loss Trauma. (2017) 22:24–35. doi: 10.1080/15325024.2016.1161428
60. Zetsche U, Ehring T, Ehlers A. The effects of rumination on mood and intrusive memories after exposure to traumatic material: an experimental study. J Behav Ther Exp Psychiatry. (2009) 40:499–514. doi: 10.1016/j.jbtep.2009.07.001
61. James EL, Lau-Zhu A, Clark IA, Visser RM, Hagenaars MA, Holmes EA. The trauma film paradigm as an experimental psychopathology model of psychological trauma: intrusive memories and beyond. Clin Psychol Rev. (2016) 47:106–42. doi: 10.1016/j.cpr.2016.04.010
62. Lanius RA, Bluhm RL, Frewen PA. How understanding the neurobiology of complex post-traumatic stress disorder can inform clinical practice: a social cognitive and affective neuroscience approach. Acta Psychiatr Scand. (2011) 124:331–48. doi: 10.1111/j.1600-0447.2011.01755.x
63. Kanske P. The social mind: disentangling affective and cognitive routes to understanding others. Interdiscip Sci Rev. (2018) 43:115–24. doi: 10.1080/03080188.2018.1453243
64. Stietz J, Jauk E, Krach S, Kanske P. Dissociating empathy from perspective-taking: Evidence from intra-and inter-individual differences research. Front Psychiatry. (2019) 10:126. doi: 10.3389/fpsyt.2019.00126
65. Schurz M, Radua J, Tholen MG, Maliske L, Margulies DS, Mars RB, et al. Toward a hierarchical model of social cognition: a neuroimaging meta-analysis and integrative review of empathy and theory of mind. Psychol Bull. (2021) 147:293. doi: 10.1037/bul0000303
66. Dedovic K, Rexroth M, Wolff E, Duchesne A, Scherling C, Beaudry T, et al. Neural correlates of processing stressful information: an event-related fMRI study. Brain Res. (2009) 1293:49–60. doi: 10.1016/j.brainres.2009.06.044
67. Knight LK, Stoica T, Fogleman ND, Depue BE. Convergent neural correlates of empathy and anxiety during socioemotional processing. Front Hum Neurosci. (2019) 13:94. doi: 10.3389/fnhum.2019.00094
68. Tholen MG, Trautwein F-M, Böckler A, Singer T, Kanske P. Functional magnetic resonance imaging (fMRI) item analysis of empathy and theory of mind. Hum Brain Mapp. (2020) 41:2611–28. doi: 10.1002/hbm.24966
69. Kanske P, Böckler A, Trautwein F-M, Parianen Lesemann FH, Singer T. Are strong empathizers better mentalizers? Evidence for independence and interaction between the routes of social cognition. Soc Cogn Affect Neurosci. (2016) 11:1383–92. doi: 10.1093/scan/nsw052
70. Hildebrandt MK, Jauk E, Lehmann K, Maliske L, Kanske P. Brain activation during social cognition predicts everyday perspective-taking: a combined fMRI and ecological momentary assessment study of the social brain. Neuroimage. (2021) 227:117624. doi: 10.1016/j.neuroimage.2020.117624
Keywords: empathy, theory of mind, hyperarousal, negative thinking, traumatic event
Citation: Trautmann S, Wittgens C, Muehlhan M and Kanske P (2022) The Role of Socio-Affective and Socio-Cognitive Mechanisms in the Processing of Witnessed Traumatic Events. Front. Psychiatry 13:830218. doi: 10.3389/fpsyt.2022.830218
Received: 06 December 2021; Accepted: 11 February 2022;
Published: 10 March 2022.
Edited by:
Judith K. Daniels, University of Groningen, NetherlandsReviewed by:
Raffael Kalisch, Johannes Gutenberg University Mainz, GermanyCopyright © 2022 Trautmann, Wittgens, Muehlhan and Kanske. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sebastian Trautmann, c2ViYXN0aWFuLnRyYXV0bWFubkBtZWRpY2Fsc2Nob29sLWhhbWJ1cmcuZGU=; Philipp Kanske, cGhpbGlwcC5rYW5za2VAdHUtZHJlc2Rlbi5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.