- 1Acupuncture Department, National Hospital of Traditional Medicine, Hanoi, Vietnam
- 2Department of Biostatistics, School of Medicine, Virginia Commonwealth University, Richmond, VA, United States
- 3Traditional Medicine Hospital, Ministry of the Public Security, Hanoi, Vietnam
- 4U Buou Hospital, Bac Giang City, Vietnam
- 5Son Uyen General Hospital, Bac Giang City, Vietnam
- 6Lady Reading Hospital, Peshawar, Pakistan
Introduction: This study aims to assess the requirement for anxiety and depression treatment for patients with coronavirus disease 2019 (COVID-19) in medical camps in Bac Giang province, Vietnam. This information can help improve the government policy to reduce anxiety and depression in patients with COVID-19.
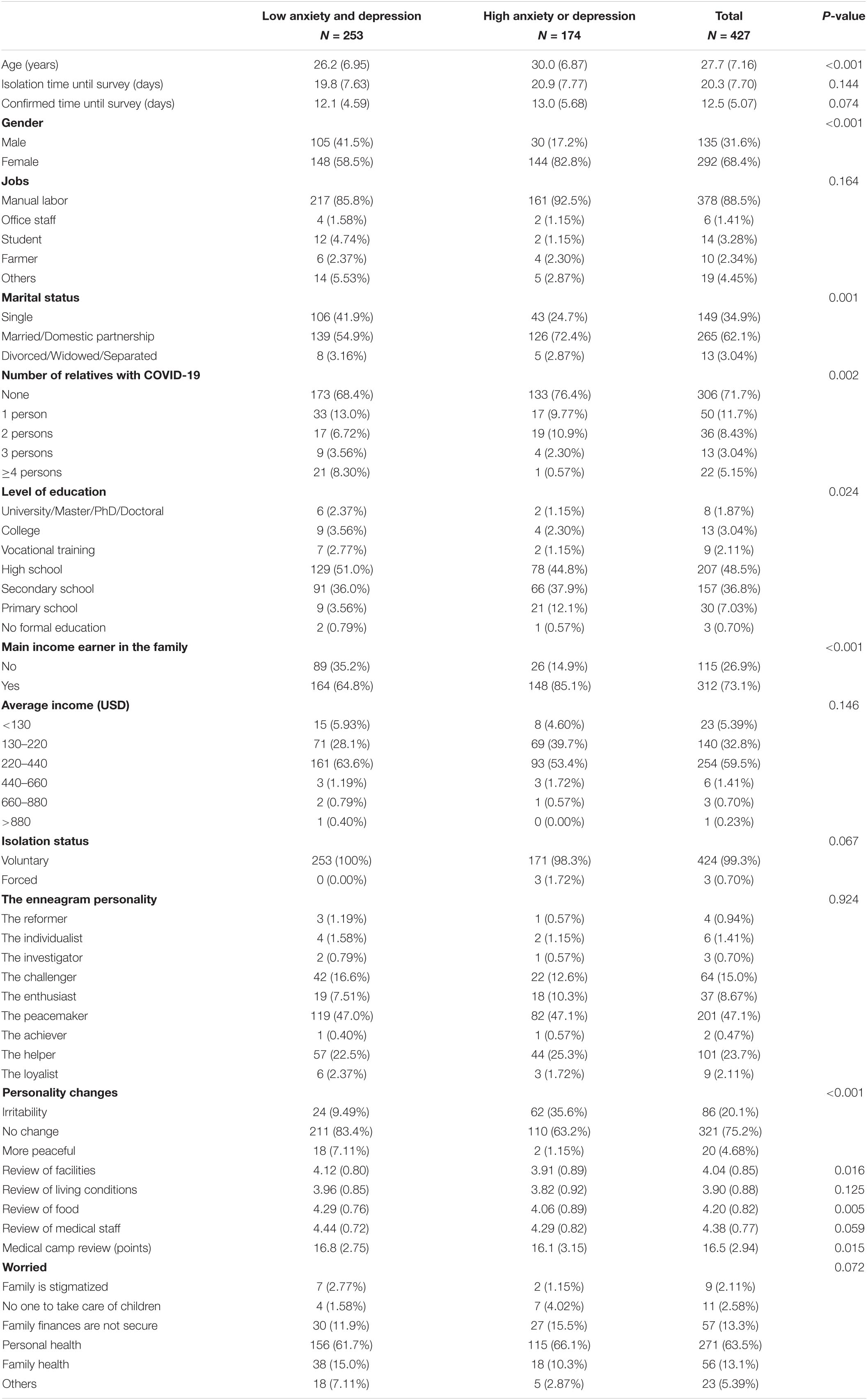
Methods: A total of patients with 427 COVID-19 participated in the survey conducted from 5 to 15 June 2021 in Bac Giang province. The survey included 17 questions about the general characteristics of the patients, 15 questions to assess common COVID-19 symptoms, the Patient Health Questionnaire-9 (PHQ-9), and General Anxiety Disorder-7 (GAD-7) scores, and four questions to assess hospital reviews, including facilities, food, medical staff, and living conditions. Logistics regression analyses were conducted to assess the association between COVID-19 symptoms and high anxiety and depression (HAD) status.
Results: A logistic regression analysis evaluated the risk factors in need of intervention. Our study showed that lower hospital review scores (odd ratio = 0.98; 95% confident interval = 0.97–0.99) were found to be a risk needing intervention. It was also identified that older patients (odd ratio = 1.1; 95% confident interval = 1.03–1.18), women (odd ratio = 1.31; 95% confident interval = 1.09–1.31), patients who were primary income earners in the family (odd ratio = 1.15; 95% confident interval = 1.03–1.28), patients who had headaches (odd ratio = 1.16; 95% confident interval = 1.06–1.21), and patients who had joint pain (odd ratio = 1.17; 95% confident interval = 1.06– 1.3) were risk factors for HAD status.
Conclusion: Our research shows that every 10-year age increase was associated with a 10% increase in the likelihood of HAD status. Study subjects being primary income earners were also associated with a 15% increased risk of having HAD status. This study showed that a decrease in family income due to COVID-19 caused an increase in high-level anxiety/depression status.
Introduction
On 1 December 2019, the first patient infected with severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) was reported in Wuhan, China, and was described with strange pneumonia (1, 2). While complex transmission mechanisms had often been mentioned for SARS-CoV-2, such as surface contact and fecal-oral or airborne transmission (3, 4), the main transmission would in fact be direct human-to-human (3, 4). Four months after the first infected patients, SARS-CoV-2 had spread globally and became a humanitarian disaster (5, 6).
Although the first COVID-19 death occurred on 22 January, 2020, in Wuhan, China, the Vietnamese government immediately took strong measures to control the situation. Early decisions included social distancing and the isolation of all infected and suspected cases. This allowed Vietnam to control the average daily number of infections to about 6.2 cases. Centralized isolation measures significantly reduced the spread of infection sources. Bac Giang province was under such control for more than 4 months. The fourth wave of COVID-19 at the end of April 2021, consisting of the Delta variant of the virus, caused an outbreak in Bac Giang province. According to a report, authorities were required to isolate 5,779 F0 patients who were inflected by COVID-19, and 43,469 F1 cases who were in close contact with infected patients for 14 days (7). With merely nine hospitals in the province, only patients with severe symptoms were admitted. To meet the need for isolation, 326 medical camps were established (7), making use of sports halls, schools, factories, and so forth. However, these camps had inadequate facilities and limited living conditions. In addition, evidence showed that isolation were associated with psychological effects (8, 9). Our study was designed to assess the status of anxiety and depression in the medical camps in Bac Giang. Such an assessment could provide information regarding factors influencing the situation, which, in turn, could improve government policy to reduce depression and anxiety in patients with COVID-19.
Materials and Methods
Study Design and Participants
This study with a cross-sectional descriptive study was conducted in medical camps in Bac Giang province from 5 to 15 June 2021. The study excluded participants in Bac Giang Province Hospital, patients under 18 years old, and patients who refuse to download the ZALO app. We randomly selected isolated patients and conducted an online survey through Google Forms. After that, we communicated with the patients through the ZALO app to track their symptoms.
Questionnaire Design
The survey included 17 questions about the general characteristics of the patients, 15 questions to assess common symptoms, the Patient Health Questionnaire-9 (PHQ-9), and General Anxiety Disorder-7 (GAD-7) scores. Categories of depression symptoms were defined as low depression (PHQ-9 score 0–9) and high depression (PHQ-9 score ≥ 10) (10). Categories of anxiety symptoms were defined as low anxiety (GAD-7 score 0–9) and high anxiety (GAD-7 score ≥ 10) (11). The low anxiety and depression (LAD) group included patients with low anxiety or low depression. In contrast, the high anxiety and depression (HAD) group included patients with moderate and severe anxiety or moderate and severe depression (moderate or severe). Finally, the survey participants graded the medical camps based on four criteria: facilities, food, medical staff, and living conditions on a 5-level Likert scale (1: very poor; 5: very good).
Statistics Analysis
The Shapiro-Wilk test was conducted to test the normal distribution hypothesis for continuous variables. Comparisons were made using a t-test for continuous variables with normal distribution, and the Mann-Whitney U test for continuous variables with non-normal distribution. Data were presented as the number of patients (percent) for categorical variables. The Chi-square test (if the expected value in cell > 5) and the Fisher exact test (if the expected value in cell < 5) were conducted for categorical variables to compare baseline characteristics between the study groups (intervention and non-intervention). The correlation between Patient Health Questionnaire-9 and General Anxiety Disorder-7 was determined. Univariate and multivariate logistics regressions were conducted to evaluate the odds ratio (OR) and 95% confidence interval (95% CI) of factors between the intervention group and the non-intervention group. All hypotheses were tested as two tails, with a p-value < 0.05 considered statistically significant. Statistical analyses were performed using RStudio version 3.6.2.
Ethical Consideration
The ethics committee approved all procedures of Traditional Medicine Hospital-Ministry of Public Security, Hanoi, Vietnam (No.664/QD-YHCT). Consent forms were attached to the survey questionnaire, and the patients only took the survey after accepting the terms of the study.
Results
A total of 427 patients with COVID-19 participated in this study, with a response rate of 64.2%. Men made up 31.6% of the participants, while women made up 68.4%. The mean participant age was 27.7 (standard deviation = 7.16). Moreover, 174 patients (40.7%) were identified as HAD. Figure 1 shows a positive correlation between PHQ-9 and GAD-7 scores. Specifically, the proportion of patients with a GAD-7 score greater than or equal to 10 and a PHQ-9 score less than 10 is relatively low.
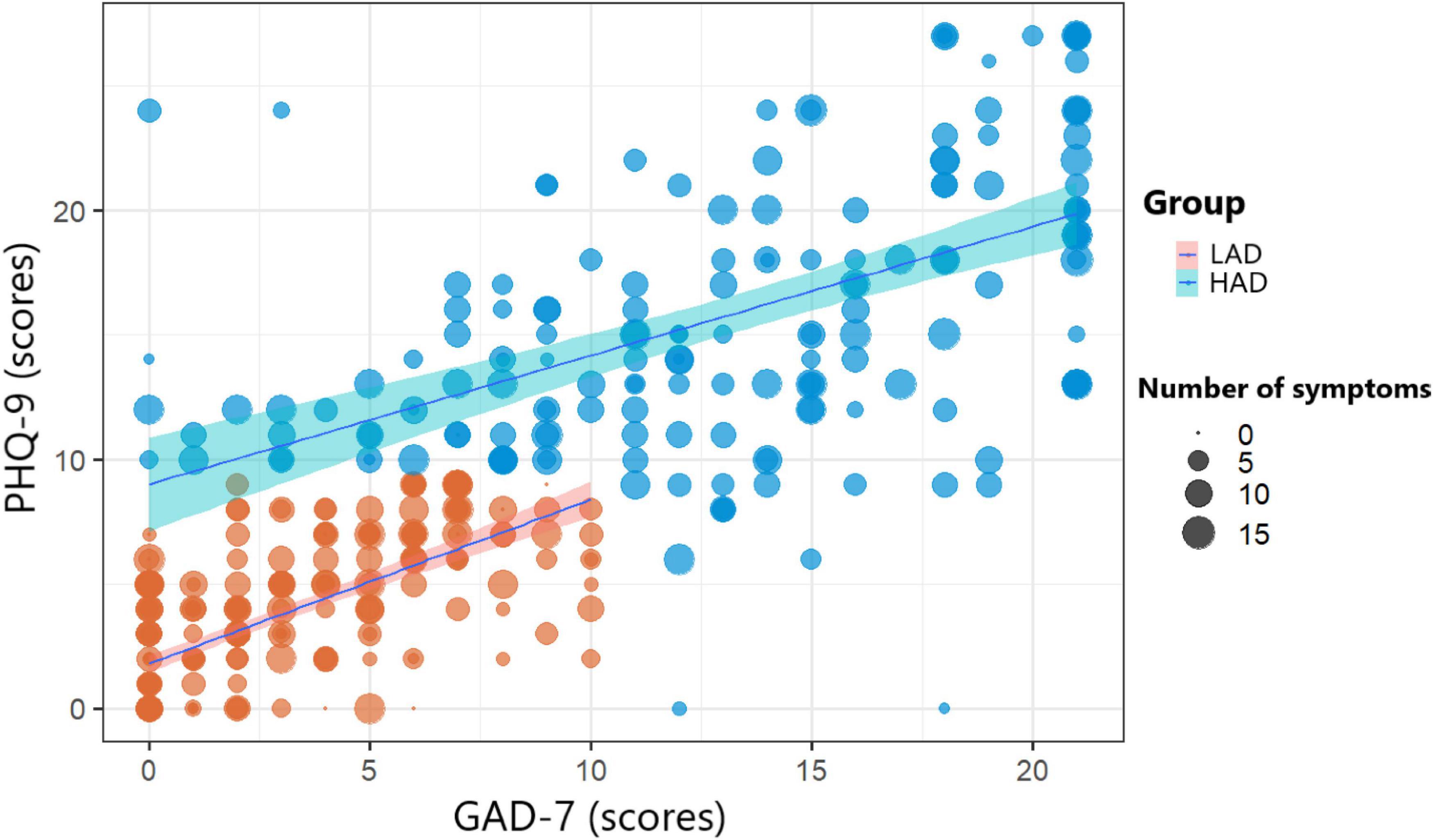
Figure 1. Correlation between General Anxiety Disorder-7 (GAD) and Patient Health Questionnaire-9 (PHQ) scores according to anxiety and depression status and number of symptoms.
According to Table 1, the mean age of the subjects in the HAD group was 30 (6.87), which was statistically significantly higher than in the LAD group, whose mean age was 26.2 (6.95). In the HAD group, 82.8% of the patients were women, compared to the 58.5% in the LAD group. Furthermore, in the HAD group, 85.1% of patients were defined as primary workers in the family, which was significantly higher than in the LAD group (68.4%). According to the personality changes criterion, the HAD group had a significantly higher rate of irritability; 35.6% compared to the 9.49% of the LAD group. The LAD group evaluated facilities, food, living conditions, and medical staff higher than the HAD group. In particular, statistical significance was found between the two groups in facilities (p-value = 0.016) and food (p-value = 0.005).
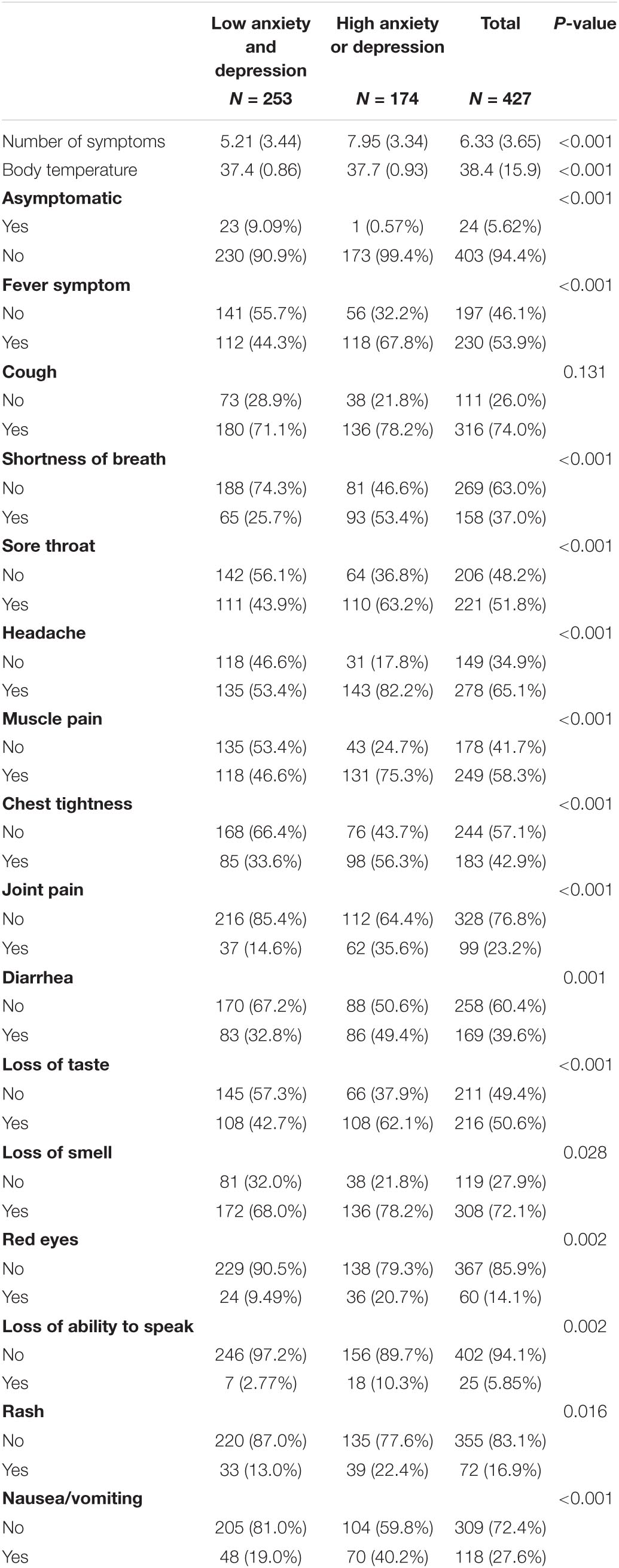
The HAD group had a significantly higher rate of symptoms than the LAD group, except for cough symptoms. According to Table 2, asymptomatic patients in the LAD group were 9.09%, approximately 16 times higher than in the HAD group. However, the difference between the two groups was not statistically significant in terms of cough symptoms (p = 0.131).
As shown in Table 3, HAD status was significantly higher among older patients, women, main income earners, and those suffering from shortness of breath, headaches, joint pain, and loss of speaking ability. Moreover, patients with loss of speaking ability have higher odd ratios of needing interventions than patients without this loss (OR = 1.39; 95% CI = 1.15–1.70). Besides these factors, hospitals with higher review scores had fewer patients in the HAD group (OR = 0.98; 95% CI = 0.96–1). According to the results of multiple binary logistic regression analysis evaluating the risk factors in need of intervention, lower hospital review scores (OR = 0.98; 95% CI = 0.97–0.99) were found to be a risk for needing intervention, while older patients (OR = 1.1; 95% CI = 1.03–1.18), women (OR = 1.31; 95% CI = 1.09–1.31), patients who were main income earners (OR = 1.15; 95% CI = 1.03–1.28), patients who had headaches (OR = 1.16; 95% CI = 1.06–1.21), and patients who had joint pain (OR = 1.17; 95% CI = 1.06–1.3) were identified as risk factors for HAD status.
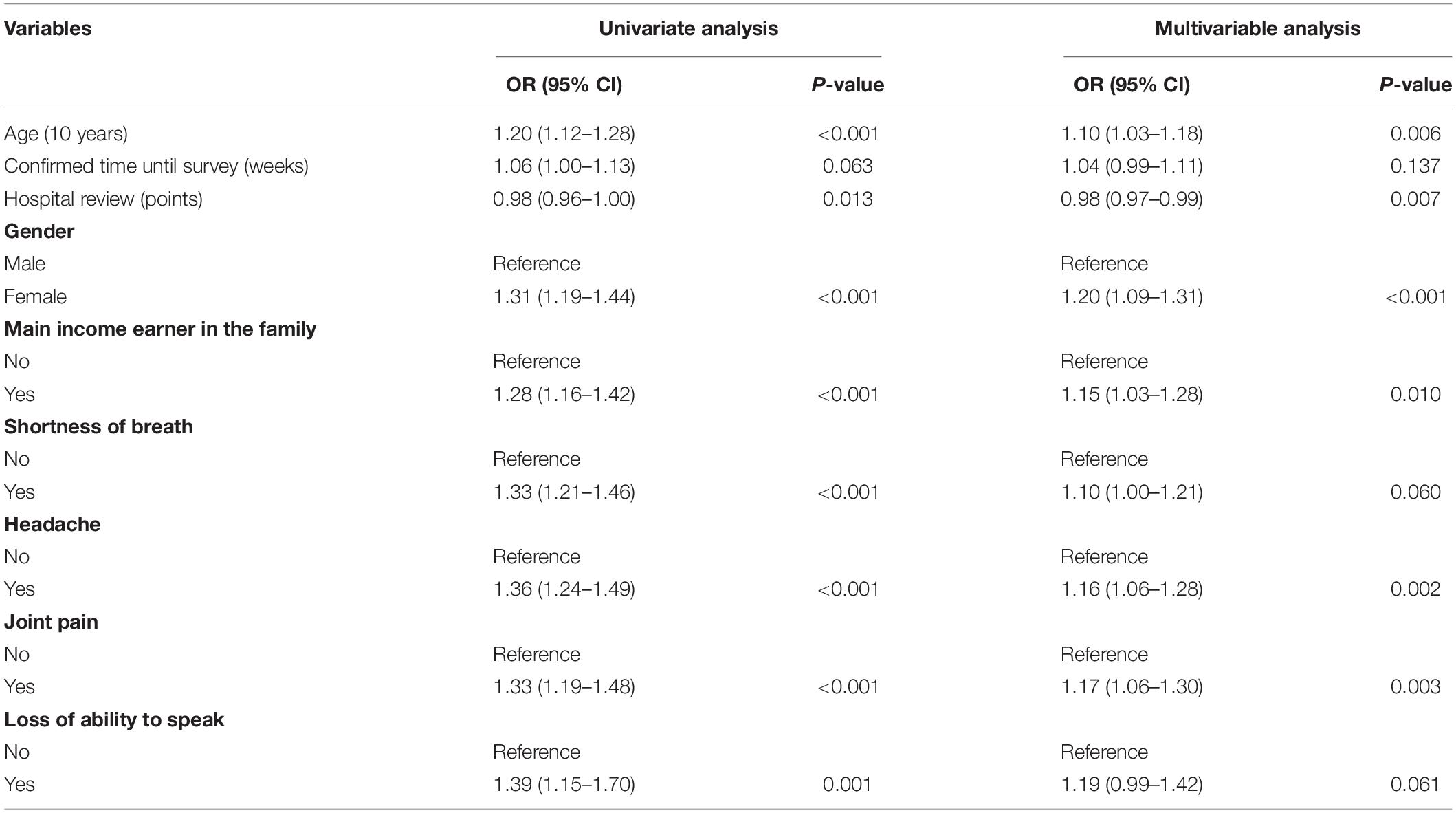
Table 3. Multivariable regression related to indications for high anxiety and depression (HAD) status.
Discussion
In the face of complicated developments of the COVID-19 epidemic in Vietnam, the government has taken an uncompromising approach to the centralized isolation of all confirmed cases. The measure has shown apparent effectiveness in controlling the COVID-19 outbreak. However, our study showed that the isolation process significantly impacted mental health. Symptoms of COVID-19 were positively correlated with depression and anxiety. Our study showed that age, confirmed cases until the survey, gender, being primary income earners, shortness of breath, headaches, joint pain, and loss of speaking ability were significantly associated with the likelihood of having HAD status. Furthermore, the medical camp review was significantly associated with reduction in LAD status. Our study points to the necessity of depression and anxiety treatment, such as psychological consultations, as well as the establishment of a policy to financially support low-income patients with COVID-19.
A previous study from Kong et al. (12) showed that the PHQ-9 and GAD-7 scales increase with age for COVID-19 patients. Our findings indicate that every 10-year increase in age was associated with a 10% increase in the likelihood of HAD status. The 1-week increase after the confirmation of COVID-19 was associated with a 4% increased likelihood of having HAD status. These results were similar to Yanyu Hu’s study, which showed that the duration of COVID-19 was associated with a statistically significant increase in GAD-7 and PHQ-9 scores (13). Our results also showed that being female was associated with a 20% increased likelihood of having HAD status. This is similar to a previous study showing that women with COVID-19 have higher depression and anxiety scores than men (14–17).
In the multivariate logistics regression results, the common symptoms of shortness of breath, headaches, and joint pain were significant factors related to the HAD group. Furthermore, study subjects being primary income earners were also associated with a 15% increased risk of having HAD status. Healthcare workers also have an increased chance of exposure to COVID-19 (18). This study showed that a decrease in family income due to COVID-19 led to an increase in high-level anxiety/depression status (19). In other studies, asymptomatic patients at the time of testing accounted for 30.8–51.7% (20, 21); this rate differed from our study (5.62%). However, follow-up studies over time show that the proportion of asymptomatic patients was much lower at about 10.7 (22) to 15.6% (23). This difference could be explained by patients being diagnosed at an early stage when they were not showing any symptoms.
Furthermore, a 1-point increase in the medical camp review was associated with a 2% reduction in the likelihood of having HAD status. During the isolation period, patients with COVID-19 shared a small space with limited facilities with other patients with COVID-19. Therefore, it was not surprising that their satisfaction with the medical camp was significantly associated with reduction in HAD status.
There were some limitations to our study. First, although this study was a random selection of patients through an online format, most of the participants were relatively young (mean age was 27.7); thus, it is necessary to investigate with an older participant pool. Second, there is a lack of follow-up in the study design related to depression and anxiety. Follow-up studies would clarify participants’ levels of depression and anxiety after being COVID-19-free. Third, this study was conducted based on a self-reported questionnaire, which may involve respondents’ bias.
Conclusion
This study indicated that increase in age would increase the likelihood of HAD. The advantage of medical camp has reduced the severity of shortage number of beds in the hospital, low-cost facilities and easy to establish. Moreover, low income and being a primary income earner also increased the risk of having HAD status. Government and policymakers should, thus, offer financial support for low-income patients with COVID-19. Our study further showed that HAD status was correlated with increase in symptoms of COVID-19. Therefore, psychological consultations in Vietnam’s medical camps are necessary to improve patient health conditions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The Ethics Committee approved all procedures of Traditional Medicine Hospital–Ministry of Public Security, Hanoi, Vietnam (No.664/QD-YHCT). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KH, VT, and LV developed the study concept and provided critical revisions. KH, VT, LV, HT, MN, and HN performed the analysis. All authors contributed to draft the manuscript and to the study design and approved the final version of the manuscript for submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
2. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
3. Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. (2020) 382:2081–90. doi: 10.1056/NEJMoa2008457
4. Harrison AG, Lin T, Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. (2020) 41:1100–15. doi: 10.1016/j.it.2020.10.004
5. Acter T, Uddin N, Das J, Akhter A, Choudhury TR, Kim S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci Total Environ. (2020) 730:138996. doi: 10.1016/j.scitotenv.2020.138996
6. Mallah SI, Ghorab OK, Al-Salmi S, Abdellatif OS, Tharmaratnam T, Iskandar MA, et al. COVID-19: breaking down a global health crisis. Ann Clin Microbiol Antimicrob. (2021) 20:35. doi: 10.1186/s12941-021-00438-7
7. Bac Giang Department of Information and Communication.Report: Summary of COVID-19 Prevention and Control in Bac Giang Province (237/BC-BCD). (2021). Available online at: https://stttt.bacgiang.gov.vn/documents/21475/11798496/1633333534577_BC-237.pdf/cfb3182d-5a4f-4372-98b5-f1595c9379cd (accessed June 6, 2021).
8. Saltzman LY, Hansel TC, Bordnick PS. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol Trauma. (2020) 12(Suppl. 1):S55–7. doi: 10.1037/tra0000703
9. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
10. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ Can Med Assoc J. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
11. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
12. Kong X, Zheng K, Tang M, Kong F, Zhou J, Diao L, et al. Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID-19. MedRxiv [Preprint]. (2020). doi: 10.1101/2020.03.24.20043075
13. Hu Y, Chen Y, Zheng Y, You C, Tan J, Hu L, et al. Factors related to mental health of inpatients with COVID-19 in Wuhan. China. Brain Behav Immun. (2020) 89:587–93. doi: 10.1016/j.bbi.2020.07.016
14. Nie XD, Wang Q, Wang MN, Zhao S, Liu L, Zhu YL, et al. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int J Psychiatry Clin Pract. (2021) 25:109–14. doi: 10.1080/13651501.2020.1791345
15. Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav Immun. (2020) 88:17–27. doi: 10.1016/j.bbi.2020.05.038
16. Htun YM, Thiha K, Aung A, Aung NM, Oo TW, Win PS, et al. Assessment of depressive symptoms in patients with COVID-19 during the second wave of epidemic in Myanmar: a cross-sectional single-center study. PLoS One. (2021) 16:e0252189. doi: 10.1371/journal.pone.0252189
17. Basheti IA, Mhaidat QN, Mhaidat HN. Prevalence of anxiety and depression during COVID-19 pandemic among healthcare students in Jordan and its effect on their learning process: a national survey. PLoS One. (2021) 16:e0249716. doi: 10.1371/journal.pone.0249716
18. Cao J, Tu WJ, Cheng W, Yu L, Liu YK, Hu X, et al. Clinical features and short-term outcomes of 102 patients with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. (2020) 71:748–55. doi: 10.1093/cid/ciaa243
19. Tran BX, Nguyen HT, Le HT, Latkin CA, Pham HQ, Vu LG, et al. Impact of COVID-19 on economic well-being and quality of life of the vietnamese during the National social distancing. Front Psychol. (2020) 11:565153. doi: 10.3389/fpsyg.2020.565153
20. Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility – King County, Washington, March 2020. MMWR Morb Mort Wkly Rep. (2020) 69:377–81. doi: 10.15585/mmwr.mm6913e1
21. Nishiura H, Kobayashi T, Miyama T, Suzuki A, Jung SM, Hayashi K, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. (2020) 94:154–5. doi: 10.1016/j.ijid.2020.03.020
22. Ki M, Task Force for 2019-nCoV. Epidemiologic characteristics of early cases with 2019 novel coronavirus (2019-nCoV) disease in Korea. Epidemiol Health. (2020) 42:e2020007. doi: 10.4178/epih.e2020007
Keywords: depression, COVID-19, anxiety, multiple logistics regression, medical camps
Citation: Trang VTT, Huynh KLA, Truong HT, Nguyen HT, Hoang GT, Dao DQ, Van Vu U, Hassan Z, Nguyen MNH and Truong LV (2022) Predicting Anxiety and Depression Among Patients With COVID-19 in Concentrated Isolation at Medical Camps in Vietnam: A Descriptive Cross-Sectional Study. Front. Psychiatry 13:823586. doi: 10.3389/fpsyt.2022.823586
Received: 27 November 2021; Accepted: 20 April 2022;
Published: 31 May 2022.
Edited by:
Marco Grados, Johns Hopkins Medicine, United StatesReviewed by:
Wen-Jun Tu, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaJelena Vrublevska, Riga Stradiņš University, Latvia
Copyright © 2022 Trang, Huynh, Truong, Nguyen, Hoang, Dao, Van Vu, Hassan, Nguyen and Truong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Le Van Truong, YnMudmFudHJ1b25nQGdtYWlsLmNvbQ==
†These authors share first authorship
 Vu Thi Thu Trang1†
Vu Thi Thu Trang1† Zair Hassan
Zair Hassan Le Van Truong
Le Van Truong