- 1Department of Psychiatry, WHO Collaborating Centre for Mental Health Research and Capacity-Building, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 2Centre for Innovative Drug Development and Therapeutics Trial for Africa, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 3Department of Psychiatry and Mental Health, Muhimbili University of Health and Allied Science, Dar es Salaam, Tanzania
- 4Department of Family Medicine and Primary Care, Faculty of Health Sciences, Witwatersrand University, Johannesburg, South Africa
- 5Department of Epidemiology and Biostatistics, Muhimbili University of Health and Allied Science, Dar es Salaam, Tanzania
- 6Centre for Global Mental Health, Health Service and Population Research Department and WHO Collaborating Centre for Mental Health and Training, Institute of Psychiatry, Psychology, and Neuroscience, King's College University, London, United Kingdom
Introduction: Alcohol use disorder (AUD) is among the leading cause of morbidity and mortality in sub-Saharan Africa. Despite this, AUD is often not detected in health care settings, which contributes to a wide treatment gap. Integrating services for mental, neurological, and substance use disorders in general health care settings is among the recommended strategies to narrow this treatment gap. This scoping review aimed to map the available evidence on integration of AUD interventions in general health care settings in sub–Saharan Africa.
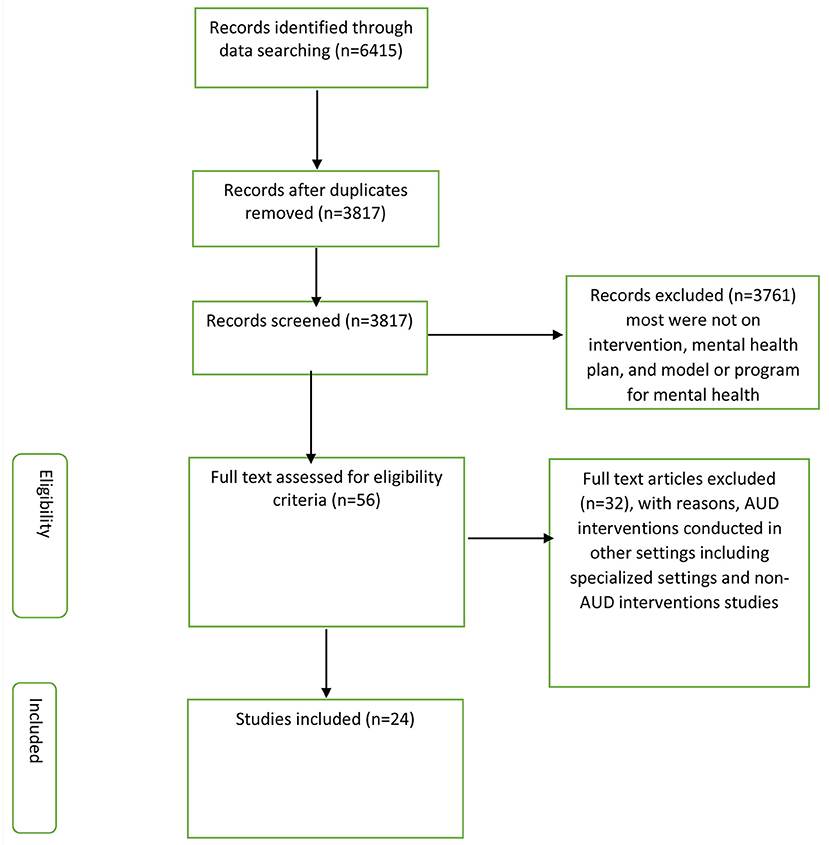
Methods: We searched four databases (PubMed, PsycINFO, CINAHL, and Africa Wide Information) for publications up to December 2020. The search strategy focused on terms for alcohol use, alcohol interventions, and sub-Saharan African countries. Studies that reported AUD interventions in general health care settings in sub–Saharan Africa were eligible for inclusion. Over 3,817 potentially eligible articles were identified. After the removal of duplicates and screening of abstracts, 56 articles were included for full article review. Of these, 24 papers reporting on 22 studies were eligible and included in a narrative review.
Results: Of the 24 eligible articles, 19 (80%) described AUD interventions that were being delivered in general health care settings, 3 (12%) described plans or programs for integrating AUD interventions at different levels of care, including in health facilities, and 2 (8%) studies reported on AUD interventions integrated into general health care settings.
Conclusions: This review shows that there is limited evidence on the integration of AUD interventions in health care settings in sub-Saharan Africa. There is an urgent need for studies that report systematically on the development, adaptation, implementation, and evaluation of integrated AUD interventions in health care settings in sub-Saharan Africa.
Introduction
Alcohol Use Disorder (AUD) is defined as a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using alcohol despite significant alcohol-related problems (1). AUD accounts for about 5.1% of all disability-adjusted life years (DALYs) and 5.3% of all deaths globally (2). AUD is also a risk factor for many diseases, injuries, and social issues including child neglect and violence (2). In addition, AUD negatively impacts the economic wellbeing of both individuals and society at large (2).
Studies conducted in sub-Saharan Africa (SSA) have shown that approximately one in five people attending health care facilities meet the criteria for AUD (3–7). AUD in the African setting is associated with injuries (5, 8), physical and mental health problems (9), as well as direct and indirect adverse effects on HIV disease progression (6), barriers to seeking professional help, stigma, and a low tendency to seek help (9, 10). Even though the magnitude and factors associated with AUD are substantial, AUD appears to be rarely detected by health care providers (11) leading to a wide treatment gap (9, 11–13). This gap is particularly marked in low-income and lower-middle-income countries (9, 11, 12).
The World Health Organization (WHO) mental health Gap Action Program (mhGAP) intervention guidelines support the integration of services for people with mental health, substance use, and neurological disorders into general and primary health care as a means of narrowing the treatment gap (14–16). In SSA, interventions for AUD have been reported in various general health care settings (3, 17–27), including services for people with HIV or other sexually transmitted diseases (9, 10, 13–16, 18, 21), antenatal and postnatal care (19, 27–29), care for people with tuberculosis (30, 31), inpatient and outpatient care (20, 26, 32–35). Some of these studies have further reported on implementation outcomes (e.g., feasibility or acceptability) of interventions for AUD in general health care settings (7, 36–38). However, evidence on the integration of AUD interventions into general health care settings has not been synthesized.
In response to this gap, in this scoping review, we mapped the available evidence on the integration of interventions for people with AUD attending general health care facilities in SSA.
Methods
Design
We conducted a scoping review of published articles that described or evaluated interventions, service models, plans, or programs for integrating care for people with AUD in general health care facilities in SSA.
A scoping review can be undertaken to map the key concepts underpinning a research area as well as to clarify working definitions, and/or the conceptual boundaries of a topic (39). This study was guided by Arksey and O'Malley's (39) scoping review methodological framework. Furthermore, the study team followed the PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) checklist and explanation (40). Based on the WHO technical report on the integration of health services, we have defined integration as a range of services/interventions for alcohol use disorder integrated into the work of general health care workers in general health care settings (41).
This study is part of formative work to adapt and pilot an integrated intervention model for people with AUD in primary healthcare in rural Tanzania (42).
Search Strategies
We reviewed published literature on interventions for AUD integrated into general health care settings in SSA. The search was conducted using the following electronic databases: PubMed, PsychINFO, CINAHL, and Africa Wide Information. We included studies published from the inception of databases to December 2020 (Supplementary Material). The rationale for this was that no previous review on integration of interventions for people with AUD attending general health care facilities in SSA had been conducted. We also anticipated that older studies would still have potential relevance. All types of study designs were included.
Two reviewers (DM and JF) independently screened the titles and abstracts of citations identified through the search strategy, and thereafter full articles, to select studies that met inclusion criteria. Disagreements between the screeners were resolved by a joint discussion, without the need for the involvement of senior co-investigators.
Inclusion Criteria
(i) We included studies that reported on any interventions for AUD conducted among people attending general health care facilities in SSA.
(ii) Studies with any methodology (quantitative, qualitative, mixed) were included.
Exclusion Criteria
(i) Studies that reported on interventions for AUD in other settings, for example, in specialist settings were excluded.
(ii) Systematic reviews and meta-analyses studies were excluded, but the individual studies included within these papers were assessed for eligibility.
Extraction of the Data
A pre-tested data extraction form was used to extract the information needed for this review. A pre-test was conducted with five articles to assess if all the required information would be captured. The following information was extracted:
(i) author, (ii) country in which the study was conducted, (iii) year the study was conducted, (iv) year of publication, (v) study population and type of health care service, (vi) type of AUD interventions, (vii) primary outcome/s, and (viii) integration status of AUD intervention.
Results
Identified Papers
In this review, 24 articles were eligible for the synthesis of information. Figure 1 presents the overall process of searching the potential articles included in this review. The review yielded 6,415 citations, out of which 2,598 (40%) were duplicates. We screened titles and abstracts of 3,817 citations and identified 56 citations for full article review. Of these, we excluded 32 articles that did not report on AUD interventions or reported on AUD interventions from settings other than general health care.
We present the review findings as follows:
(i) the underlying study design, (ii) targeted population and type of health care service, (iii) region of sub-Saharan Africa where the study took place, (iv) publication year, (v) primary outcome, and (vi) AUD intervention.
Study Designs of the Included Studies
Most of the studies were randomized controlled trials (n = 15), followed by mixed-method study designs (n = 7), cohort study design (n = 1), and cross-sectional survey (n = 1).
Health Care Service and Targeted Population
Most studies were of AUD interventions integrated within HIV care or services for other sexually transmitted diseases (n = 10), or in general clinical services (n = 10), with the remainder conducted in the context of emergency services (n = 3) and tuberculosis care/clinics (n = 1).
Sub-Saharan Africa Regions Where Interventions Were Implemented
Most of the studies were implemented in the southern African region (n = 12) and eastern region (n = 10), with two studies conducted in the central region, and one in the western region.
Publication Year of the Interventions
Most studies were published from the years 2010 to 2020 (n = 20), while three studies were reported from the years 2000 to 2010. Only one study was published before the year 2000.
Integrated Interventions for AUD in General Health Care Settings
We found several studies describing AUD interventions delivered in general health settings in SSA. However, for most of these studies, we could not be certain if those interventions were integrated into these services. In addition to that, we also found studies that reported frameworks and plans for integrated interventions for the mental health services that also included AUD care as one component. Based on this observation we have reported our results in three categories: (i) studies that described interventions for AUD, (ii) studies that described plans or frameworks for integrated AUD interventions, and (iii) studies that reported the integration status of AUD interventions in general health care settings.
Interventions for AUD in General Health Care Settings
Table 1 describes the interventions for AUD that have been applied in general health care settings in SSA, which included: (i) interventions which were based on motivational interviewing techniques (n = 15), (ii) interventions focused on identification of alcohol use (n = 8), (iii) interventions which applied cognitive behavior therapy (n = 3), (iv) interventions that focused on risk/behavioral reduction counseling (n = 1), and (v) interventions that applied problem solving skills (n = 1).
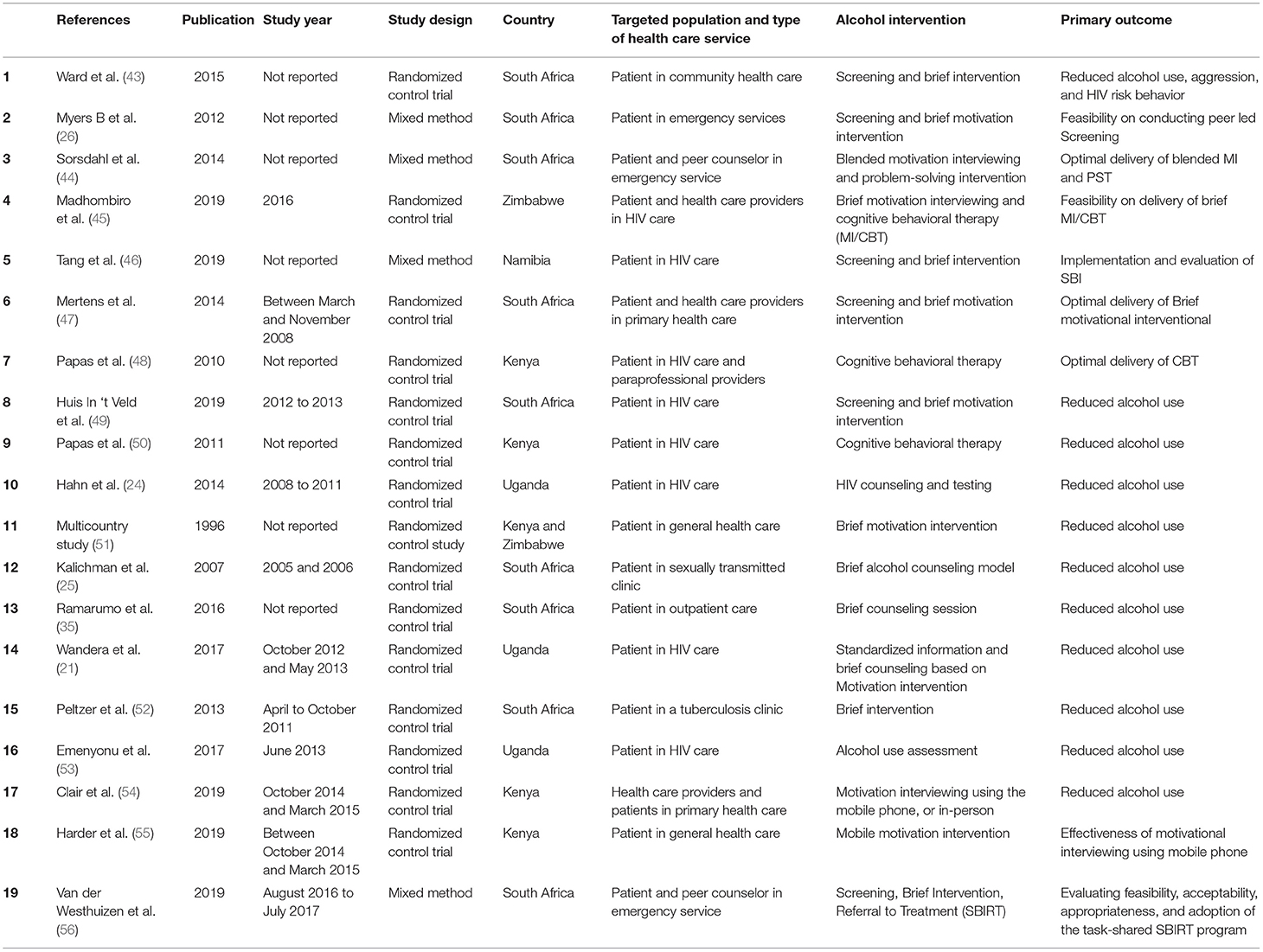
Table 1. Description of interventions for alcohol use disorder in Sub Saharan Africa general health care settings.
Programs for Integrated AUD Interventions
This included district mental health plans (n = 2) and a program intervention guide (n = 1) for integrated mental health services that included AUD (Table 2). The implementation outcomes [such as acceptability and feasibility (58)] for the integrated mental health services that included AUD were also reported in these studies. Strategies that facilitated the implementation of AUD care within integrated mental health services at different levels of care (community, general health facility, health system organization) were also reported. The following implementation strategies were reported: (i) engaging mental health stakeholders from inception to enhance their ownership and commitment, (ii) conducting sensitization workshops (37, 38), (iii) training clinical staff (36–38), (iv) supervising decision support and supporting staff well-being (3–37, 59), and leveraging available resources and existing systems (36–38). In addition, these studies identified individual and structural bottlenecks for implementing integrated mental health services including AUD (36, 38).
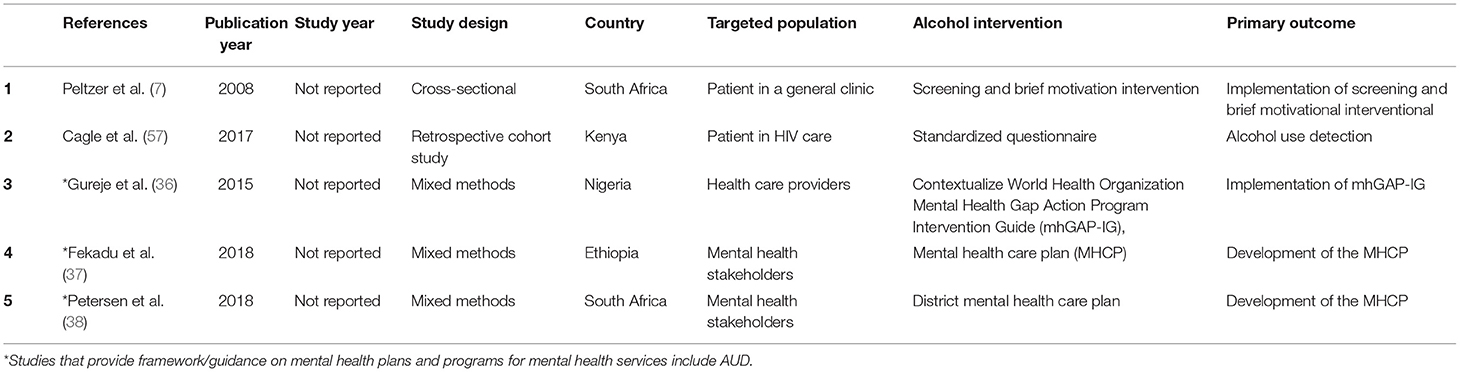
Table 2. Description of integrated interventions, mental health plan and program for alcohol use disorder in Sub Saharan Africa general health care settings.
Integrated Interventions for AUD in General Health Care Settings
This included routine screening or inquiring about alcohol use disorder (n = 1), and screening and brief intervention (SBI) for AUD (n = 1) (Table 2). These studies aimed to assess routine screening for alcohol use for people living with HIV during enrollment in the HIV clinic (57) and implementation of an alcohol screening and brief intervention in 18 primary health care services (7). The study found nine clinics had good and nine had poor SBI implementation. To improve routine implementation of SBI, the study recommended that more attention needs to be paid to training, clinic organization, and addressing the attitudes of health care providers.
Discussion
In this review, we found only two studies that described and reported on the integration status of AUD interventions in general health care settings in SSA (7, 57). Importantly, we identified several studies detailing the mental health plans and programs based on integrated interventions for mental health services that include AUD (36–38). Our review findings are in keeping with previous reviews that reported a paucity of interventions to address problematic alcohol use in SSA (60, 61). Our findings reflect the low priority accorded to expanding access to care for AUD indicated in the World Health Organization (WHO) report on alcohol and health in low and middle-income countries (2). In that WHO report, treatment coverage for AUD is low and national alcohol policies are scarce in SSA.
Nevertheless, the identified studies indicated that it is possible to implement integrated mental health services, including AUD care, in general, health care settings in SSA. This is similar to findings from a brief review of integrating interventions for AUD into clinical practice in high-income settings (62). These studies demonstrated that AUD care, as a component of integrated mental health care, can achieve a positive and significant impact on clinical outcomes for people with AUD (36, 38). Additionally, these studies also identified various strategies that may facilitate the implementation of AUD components of an integrated mental health care program. These strategies included methods to improve detection, support decision making, improve staff wellbeing, and ensure proper program management and supportive supervision (36–38). These findings align with a previous review on strategies to facilitate integrated care for people with alcohol problems (63).
Individual and structural bottlenecks to the implementation of integrated interventions for mental health services including AUD were also identified. These findings are in keeping with results from a review of barriers and facilitators to implementing screening and brief intervention for alcohol misuse in high-income country settings (64).
This scoping review had some limitations. We were not able to document policy level examples of integration of AUD, and we did not search the gray literature where program evaluations may be available. The reasons for omitting a gray literature search was largely due to feasibility, but also reflected our concerns that some gray literature may not be published online or the uniform resource locator (URL)/website may not be stable, older documents may not be archived, and format and citation information could be inconsistent.
It is likely that other examples of integration of AUD interventions in general health care exist but have not been reported and, therefore, could not be detected by this scoping review.
Conclusions
This review has highlighted the paucity of studies on integrated interventions for AUD in general health care settings in sub-Saharan Africa. There is an urgent need for studies that report systematically on the development, or adaptation, implementation, and evaluation of integrated AUD interventions in health care settings in sub- Saharan Africa.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
DM developed the study design with contribution from JF, CH, CM, and ST. DM and JF carried out the article's systematic searching, screening, and eligibility checking. DM performed data analysis with contribution from JF. DM wrote the manuscript draft. All authors took part in the interpretation of the data, reviewed the draft, provided important intellectual materials, and agreed on the final draft.
Funding
DM acknowledges support from the Centre for Innovative Drug Development and Therapeutics Trial for Africa (CDT-Africa), a World Bank Africa Centre of excellence at Addis Ababa University as part of her training fellowship.
Author Disclaimer
The opinions in this paper are those of the authors and do not reflect the views of CDT-Africa.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.822791/full#supplementary-material
References
1. American Psychiatric Association. Diagnostic and Statistical Manual Of Mental Disorders 5th ed. (2013). doi: 10.1176/appi.books.9780890425596
2. World Health Organization. Global Status Report on Alcohol and Health. Geneva: World Health Organization (2018).
3. Parry CD, Kekwaletswe C, Shuper PA, Nkosi S, Myers BJ, Morojele NK. Heavy alcohol use in patients on highly active antiretroviral therapy: What responses are needed? S Afr Med J. (2016) 106:567–8. doi: 10.7196/SAMJ.2016.v106i6.10639
4. Hahn JA, Emenyonu NI, Fatch R, Muyindike WR, Kekiibina A, Carrico AW, et al. Declining and rebounding unhealthy alcohol consumption during the first year of HIV care in rural Uganda, using phosphatidyl ethanol to augment self-report. Addiction. (2016) 111:272–9. doi: 10.1111/add.13173
5. Forson PK, Gardner A, Oduro G, Bonney J, Biney EA, Oppong C, et al. Frequency of alcohol use among injured adult patients presenting to a Ghanaian emergency department. Ann Emerg Med. (2016) 68:492–500. doi: 10.1016/j.annemergmed.2016.04.033
6. Kader R, Seedat S, Govender R, Koch JR, Parry CD. Hazardous and harmful use of alcohol and/or other drugs and health status among South African patients attending hiv clinics. AIDS Behav. (2014) 18:525–34. doi: 10.1007/s10461-013-0587-9
7. Peltzer K, Matseke G, Azwihangwisi M, Babor T. Evaluation of alcohol screening and brief intervention in routine practice of primary care nurses in Vhembe district, South Africa. Croat Med J. (2008) 49:392–401. doi: 10.3325/cmj.2008.3.392
8. Staton CA, Vissoci JRN, Toomey N, Abdelgadir J, Chou P, Haglund M, et al. The impact of alcohol among injury patients in Moshi, Tanzania: a nested case-crossover study. BMC Public Health. (2018) 18:275. doi: 10.1186/s12889-018-5144-z
9. Zewdu S, Hanlon C, Fekadu A, Medhin G, Teferra S. Treatment gap, help-seeking, stigma and magnitude of alcohol use disorder in rural Ethiopia. Subst Abuse Treat Prev Policy. (2019) 14:4. doi: 10.1186/s13011-019-0192-7
10. Nalwadda O, Rathod SD, Nakku J, Lund C, Prince M, Kigozi F. Alcohol use in a rural district in Uganda: findings from community-based and facility-based cross-sectional studies. Int J Ment Health Syst. (2018) 12:12. doi: 10.1186/s13033-018-0191-5
11. Rathod SD, Silva MJD, Ssebunnya J, Breuer E, Murhar V, Luitel NP, et al. Treatment contact coverage for probable depressive and probable alcohol use disorders in four low- and middle-income country districts: the PRIME cross-sectional community surveys. PLoS ONE. (2016) 11:e0162038. doi: 10.1371/journal.pone.0162038
12. Luitel NP, Jordans MJD, Kohrt BA, Rathod SD, Komproe IH. Treatment gap and barriers for mental health care: a cross-sectional community survey in Nepal. PLoS ONE. (2017) 12:e0183223. doi: 10.1371/journal.pone.0183223
13. Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. (2004) 82:858–66.
14. Funk M, Saraceno B, Drew N, Faydi E. Integrating mental health into primary healthcare. Ment Health Fam Med. (2008) 5:5–8.
15. Ferreira-Borges C, Parry CDH, Babor TF. Harmful Use of Alcohol: A Shadow over Sub-Saharan Africa in Need of Workable Solutions. Int J Environ Res Public Health. (2017) 14:346. doi: 10.3390/ijerph14040346
16. Mhgap Intervention Guide For Mental Neurological And Substance Use Disorders In Non-Specialized Health Settings. Geneva: World Health Organization (2017).
17. Jaquet A, Wandeler G, Nouaman M, Ekouevi DK, Tine J, Patassi A, et al. Alcohol use, viral hepatitis, and liver fibrosis among HIV-positive persons in West Africa: a cross-sectional study. J Int AIDS Soc. (2017) 20:21424. doi: 10.7448/IAS.20.1.21424
18. Soboka M, Tesfaye M, Feyissa GT, Hanlon C. Alcohol use disorders and associated factors among people living with HIV who are attending services in southwest Ethiopia. BMC. (2014) 7:828. doi: 10.1186/1756-0500-7-828
19. Sania A, Brittain K, Phillips TK, Zerbe A, Ronan A, Myer L, et al. Effect of alcohol consumption and psychosocial stressors on preterm and small-for-gestational-age births in HIV-infected women in South Africa: a cohort study. BMJ Open. (2017) 7:e014293. doi: 10.1136/bmjopen-2016-014293
20. Bhana A, Rathod SD, Selohilwe O, Kathree T, Petersen I. Characteristics and correlates of alcohol consumption among adult chronic care patients in North West Province, South Africa. S Afr Med J. (2017) 107:636–42. doi: 10.7196/SAMJ.2017.v107i7.12131
21. Wandera B, Tumwesigye NM, Nankabirwa JI, Kambugu AD, Parkes-Ratanshi R, Mafigiri DK, et al. Alcohol consumption among HIV-infected persons in a large urban HIV clinic in Kampala Uganda: a constellation of harmful behaviors. PLoS ONE. (2015) 10:e0126236. doi: 10.1371/journal.pone.0126236
22. Medley A, Seth P, Pathak S, Howard AA, DeLuca N, Matiko E, et al. Alcohol use and its association with HIV risk behaviors among a cohort of patients attending HIV clinical care in Tanzania, Kenya, and Namibia. AIDS Care. (2014) 26:1288–97. doi: 10.1080/09540121.2014.911809
23. Martinez P, Andia I, Emenyonu N, Hahn JA, Hauff E, Pepper L, et al. Alcohol use, depressive symptoms and the receipt of antiretroviral therapy in Southwest Uganda. AIDS Behav. (2008) 12:605–12. doi: 10.1007/s10461-007-9312-x
24. Hahn JA, Fatch R, Wanyenze RK, Baveewo S, Kamya MR, Bangsberg DR, et al. Decreases in self-reported alcohol consumption following HIV counseling and testing at Mulago Hospital, Kampala, Uganda. BMC Infect Dis. (2014) 14:403. doi: 10.1186/1471-2334-14-403
25. Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in cape town, South Africa. J Acquir Immune Defic Syndr. (2007) 44:594–600. doi: 10.1097/QAI.0b013e3180415e07
26. Myers B, Stein DJ, Mtukushe B, Sorsdahl K. Feasibility and acceptability of screening and brief interventions to address alcohol and other drug use among patients presenting for emergency services in Cape Town, South Africa. Adv Prev Med. (2012) 2012:569153. doi: 10.1155/2012/569153
27. Rotheram-Borus MJ, Tomlinson M, Roux IL, Stein JA. Alcohol use, partner violence, and depression: a cluster randomized controlled trial among urban South African mothers over 3 Years. Am J Prev Med. (2015) 49:715–25. doi: 10.1016/j.amepre.2015.05.004
28. Namagembe I, Jackson LW, Zullo MD, Frank SH, Byamugisha JK, Sethi AK. Consumption of alcoholic beverages among pregnant urban ugandan women. Matern Child Health J. (2010) 14:492–500. doi: 10.1007/s10995-009-0500-3
29. English L, Mugyenyi GR, Ngonzi J, Kiwanuka G, Nightingale I, Koren G, et al. Prevalence of ethanol use among pregnant women in southwestern Uganda. J Obstet Gynaecol Can. (2015) 37:901–2. doi: 10.1016/S1701-2163(16)30027-5
30. Kendall EA, Theron D, Franke MF, van Helden P, Victor TC, Murray MB, et al. Alcohol, hospital discharge, and socioeconomic risk factors for default from multidrug resistant tuberculosis treatment in Rural South Africa: a retrospective cohort study. PLoS ONE. (2013) 8:e83480. doi: 10.1371/journal.pone.0083480
31. O'Connell R, Chishinga N, Kinyanda E, Patel V, Ayles H, Weiss HA, et al. Prevalence and correlates of alcohol dependence disorder among TB and HIV Infected patients in Zambia. PLoS ONE. (2013) 8: e74406. doi: 10.1371/journal.pone.0074406
32. Adias TC, Egerton E, Erhabor O. Evaluation of coagulation parameters and liver enzymes among alcohol drinkers in Port Harcourt, Nigeria. Int J Gen Med. (2013) 6:489–94. doi: 10.2147/IJGM.S43472
33. Peltzer K, Pengpid S. Alcohol use and health-related quality of life among hospital outpatients in South Africa. Alcohol Alcohol. (2012) 47:291–5. doi: 10.1093/alcalc/ags001
34. Steenkamp WC, Botha NJ, Van Der Merwe AE. The prevalence of alcohol dependence in burned adult patients. Burns. (1994) 20:522–5. doi: 10.1016/0305-4179(94)90012-4
35. Ramarumo M, Peltzer K, Khoza LB. Screening and brief intervention of alcohol problems in primary care in South Africa: a brief report. J Psychol Afr. (2016) 26:78–80. doi: 10.1080/14330237.2015.1101282
36. Gureje O, Abdulmalik J, Kola L, Musa E, Yasamy MT, Adebayo K. Integrating mental health into primary care in Nigeria: report of a demonstration project using the mental health gap action program intervention guide. BMC Health Serv Res. (2015) 15:242. doi: 10.1186/s12913-015-0911-3
37. Fekadu A, Hanlon C, Medhin G, Alem A, Selamu M, Giorgis TW, et al. Development of a scalable mental healthcare plan for a rural district in Ethiopia. Br J Psychiatry. (2016) 208:s4–12. doi: 10.1192/bjp.bp.114.153676
38. Petersen I, Fairall L, Bhana A, Kathree T, Selohilwe O, Brooke-Sumner C, et al. Integrating mental health into chronic care in South Africa: the development of a district mental healthcare plan. Br J Psychiatry. (2016) 208:s29–39. doi: 10.1192/bjp.bp.114.153726
39. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
40. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Int Med. (2018) 169:467–73. doi: 10.7326/M18-0850
42. Mushi DP, Hanlon C, Francis JM, Teferra S. Adaptation and piloting of an integrated intervention model for alcohol use disorders in primary healthcare in rural Tanzania: a study protocol. BMJ Open. (2020) 10:e038615. doi: 10.1136/bmjopen-2020-038615
43. Ward CL, Mertens JR, Bresick GF, Little F, Weisner CM. Screening and brief intervention for substance misuse: does it reduce aggression and HIV-related risk behaviours? Alcohol Alcohol. (2015) 50:302–9. doi: 10.1093/alcalc/agv007
44. Sorsdahl K, Myers B, Ward C, Matzopoulos R, Mtukushe B, Nicol A, et al. Screening and brief interventions for substance use in emergency departments in the Western Cape province of South Africa: views of health care professionals. Int J Injury Contr Saf Promot. (2014) 21:236–43. doi: 10.1080/17457300.2013.811267
45. Madhombiro M, Dube B, Dube M, Zunza M, Chibanda D, Rusakaniko S, et al. Intervention for alcohol use disorders at an HIV care clinic in Harare: a pilot and feasibility study. Addict Sci Clin Pract. (2019) 14:1–1. doi: 10.1186/s13722-019-0143-7
46. Tang AM, Hamunime N, Adams RA, Kanyinga G, Fischer-Walker C, Agolory S, et al. Introduction of an alcohol-related electronic screening and brief intervention (eSBI) program to reduce hazardous alcohol consumption in Namibia's antiretroviral treatment (ART) program. AIDS Behav. (2019) 23:3078–92. doi: 10.1007/s10461-019-02648-9
47. Mertens JR, Ward CL, Bresick GF, Broder T, Weisner CM. Effectiveness of nurse-practitioner-delivered brief motivational intervention for young adult alcohol and drug use in primary care in South Africa: a randomized clinical trial. Alcohol Alcohol. (2014) 49:430–8. doi: 10.1093/alcalc/agu030
48. Papas RK, Sidle JE, Martino S, Baliddawa JB, Songole R, Omolo OE, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in western Kenya. AIDS Behav. (2010) 14:669–78. doi: 10.1007/s10461-009-9647-6
49. Huis In ‘t Veld D, Ensoy-Musoro C, Pengpid S, Peltzer K, Colebunders R. The efficacy of a brief intervention to reduce alcohol use in persons with HIV in South Africa, a randomized clinical trial. PLoS ONE. (2019) 14:e0220799. doi: 10.1371/journal.pone.0220799
50. Papas RK, Sidle JE, Gakinya BN, Baliddawa JB, Martino S, Mwaniki MM, et al. Treatment outcomes of a Stage 1 cognitive-behavioral trial to reduce alcohol use among HIV-infected outpatients in western Kenya. Addiction. (2011) 106:2156. doi: 10.1111/j.1360-0443.2011.03518.x
51. WHO brief intervention study group. A cross-sectional trial on brief interventions with heavy drinkers. Am J Public Health. (1996) 86:948–55. doi: 10.2105/AJPH.86.7.948
52. Peltzer K, Naidoo P, Louw J, Matseke G, Zuma K, Mchunu G, et al. Screening and brief interventions for hazardous and harmful alcohol use among patients with active tuberculosis attending primary public care clinics in South Africa: results from a cluster randomized controlled trial. BMC Public Health. (2013) 13:1–2. doi: 10.1186/1471-2458-13-699
53. Emenyonu NI, Fatch R, Muyindike WR, Kekibiina A, Woolf-King S, Hahn JA. Randomized study of assessment effects on alcohol use by persons with HIV in rural Uganda. J Stud Alcohol Drugs. (2017) 78:296–305. doi: 10.15288/jsad.2017.78.296
54. Clair V, Rossa-Roccor V, Mokaya AG, Mutiso V, Musau A, Tele A, et al. Peer-and mentor-enhanced web-based training on substance use disorders: a promising approach in low-resource settings. Psychiatr Serv. (2019) 70:1068–71. doi: 10.1176/appi.ps.201900201
55. Harder VS, Musau AM, Musyimi CW, Ndetei DM, Mutiso VN. A randomized clinical trial of mobile phone motivational interviewing for alcohol use problems in Kenya. Addiction. (2020) 115:1050–60. doi: 10.1111/add.14903
56. Van der Westhuizen C, Myers B, Malan M, Naledi T, Roelofse M, Stein DJ, et al. Implementation of a screening, brief intervention and referral to a treatment program for risky substance use in South African emergency centres: a mixed methods evaluation study. PLoS ONE. (2019) 14:e0224951. doi: 10.1371/journal.pone.0224951
57. Cagle A, McGrath C, Richardson BA, Donovan D, Sakr S, Yatich N, et al. Alcohol use and immune reconstitution among HIV-infected patients on antiretroviral therapy in Nairobi, Kenya. AIDS Care. (2017) 29:1192–7. doi: 10.1080/09540121.2017.1281881
58. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
59. Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, Cherry C. Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. J Stud Alcohol. (2004) 65:43442. doi: 10.15288/jsa.2004.65.434
60. Peltzer K. Brief intervention of alcohol problems in Sub-Saharan Africa: a review. J Psychol Afr. (2009) 19:415–22. doi: 10.1080/14330237.2009.10820310
61. Francis JM, Cook S, Morojele NK, Swahn MH. Rarity and limited geographical coverage of individual level alcohol interventions in sub-Saharan Africa: findings from a scoping review. J Subst Use. (2020) 25:11–9. doi: 10.1080/14659891.2019.1664662
62. Agerwala SM, McCance-Katz EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: a brief review. J Psychoactive Drugs. (2012) 44:307–17. doi: 10.1080/02791072.2012.720169
63. Savic M, Best D, Manning V, Lubman DI. Strategies to facilitate integrated care for people with alcohol and other drug problems: a systematic review. Subst Abuse Treat Prev Policy. (2017) 12:19. doi: 10.1186/s13011-017-0104-7
Keywords: alcohol use disorder intervention, integration of intervention for alcohol use disorder, mental health plan, screening, brief intervention, sub-Saharan Africa, general health care
Citation: Mushi D, Francis JM, Moshiro C, Hanlon C and Teferra S (2022) Integration of Alcohol Use Disorder Interventions in General Health Care Settings in Sub-Saharan Africa: A Scoping Review. Front. Psychiatry 13:822791. doi: 10.3389/fpsyt.2022.822791
Received: 26 November 2021; Accepted: 07 February 2022;
Published: 15 March 2022.
Edited by:
Dorothy Newbury-Birch, Teesside University, United KingdomReviewed by:
Suwa Goden Goar, University of Jos, NigeriaJudith Eberhardt, Teesside University, United Kingdom
Copyright © 2022 Mushi, Francis, Moshiro, Hanlon and Teferra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dorothy Mushi, ZG9ycnltdXNoQHlhaG9vLmNvbQ==
 Dorothy Mushi
Dorothy Mushi Joel M. Francis4,5
Joel M. Francis4,5 Charlotte Hanlon
Charlotte Hanlon