
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 24 February 2022
Sec. Psychological Therapy and Psychosomatics
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.821468
This article is part of the Research TopicPsychocardiology: Exploring the Brain-Heart InterfaceView all 27 articles
 Nicole Lepsy1†
Nicole Lepsy1† Madelaine-Rachel Dering1†
Madelaine-Rachel Dering1† Jan Fuge2
Jan Fuge2 Tanja Meltendorf2
Tanja Meltendorf2 Marius M. Hoeper2
Marius M. Hoeper2 Ivo Heitland1
Ivo Heitland1 Jan C. Kamp2
Jan C. Kamp2 Da-Hee Park2
Da-Hee Park2 Manuel J. Richter3
Manuel J. Richter3 Henning Gall3
Henning Gall3 Hossein A. Ghofrani3,4
Hossein A. Ghofrani3,4 Dietmar Ellermeier5
Dietmar Ellermeier5 Hans-Dieter Kulla6
Hans-Dieter Kulla6 Karen M. Olsson1,2‡
Karen M. Olsson1,2‡ Kai G. Kahl1*‡
Kai G. Kahl1*‡Introduction: Chronic thromboembolic pulmonary hypertension (CTEPH) is a potentially life-threatening condition associated with high morbidity and mortality. However, advances in medical, surgical and interventional treatment have markedly improved the outcome of patients with CTEPH. Additional factors potentially influencing quality of life (QoL) and outcome in CTEPH are yet to be defined. Child maltreatment is a major risk factor for unfavorable behavioral, mental as well as physical health outcomes and has been associated with decreased QoL. To date, no study assessed the impact of childhood trauma in patients with CTEPH.
Methods: Patients with CTEPH were invited to complete the Childhood Trauma Questionnaire (CTQ). Data were compared to prevalence data from the German population. Mental well-being was assessed using the Hospital Anxiety and Depression Scale (HADS) and quality of life was measured using the WHO Quality of Life Questionnaire (WHOQOL). Furthermore, lifestyle factors and physical health parameters were studied.
Logistic regression analysis was used to investigate a possible impact of child maltreatment on markers of disease severity.
Results: One-hundred and seven patients with CTEPH completed the CTQ. These patients reported higher rates of emotional abuse and physical abuse and emotional neglect compared to the German population while rates of physical neglect and sexual abuse did not differ between patients and German population with prevalence of 20.6% for emotional abuse, 20% for physical abuse, 22% for emotional neglect, 46% for physical neglect, and 6% for sexual abuse in patients with CTEPH. Higher CTQ scores were associated with anxiety symptoms as well as negatively associated with QoL. No direct impact of childhood trauma on CTEPH severity was found.
Conclusion: We found a higher rate of child maltreatment in patients with CTEPH in comparison to the German population. Correlations suggest moderate associations between CTQ scores and mental health and QoL. Child maltreatment had no significant impact on disease severity. Further investigation on proper interventions to support affected patients is needed.
Chronic thromboembolic pulmonary hypertension (CTEPH) is a chronic disease occurring as a possible complication after pulmonary embolism. There are several entities of pulmonary hypertension (PH), categorized into five groups by the World Health Organization (WHO). Of these, CTEPH is designated as WHO group 4.1 (1). In CTEPH, unresolved thromboembolic material leads to the occlusion of pulmonary arteries and progressive pulmonary vascular remodeling resulting in elevated pressure and resistance in the pulmonary vascular bed (2). As a consequence, patients are initially experiencing rather unspecific symptoms like progressive dyspnea on exertion and fatigue as well as syncope and signs of right heart failure in advanced disease (3). With pulmonary endarterectomy (PEA) as surgical treatment, CTEPH became a potentially curable disease for operable patients. The 3-year survival rate increased from estimated 40–90% in patients who underwent surgery. While the majority of operable patients can be cured or achieve functional improvement, residual or recurrent CTEPH might be present (4, 5). Further on, about one half of patients with CTEPH is considered inoperable and therefore receiving lifelong medical treatment and interventional therapy if possible (6, 7). Despite improvements in treatment and increased life expectancy, quality of life is impaired in comparison to the general population (8, 9), and concomitant mental disorders have shown to be associated with impaired physical health (10). Taking these results into account, other factors, increasing the risk of impaired quality of life, physical health and developing mental disorders, are of scientific interest. One of the factors potentially associated with disease coping and QoL is child maltreatment, which is associated with a various number of negative outcomes in adulthood. Child maltreatment is defined as abuse and neglect experienced by children through their parents or other caretakers potentially causing them harm. It is divided into five subtypes of sexual abuse, physical abuse, and neglect as well as emotional abuse and neglect (11). Global prevalence rates for subtypes of child maltreatment are being reported as 12.7% for sexual abuse, 22.6% for physical abuse, 36.3% for emotional abuse, 16.3% for physical neglect, and 18.4% for emotional neglect (12) as well as about one third of a German representative population sample experiencing at least one type of child maltreatment (13). The impact of child maltreatment on developing mental health issues was considered by various studies. Experiencing one or multiple types of child maltreatment is associated with a higher risk for developing depression (14–16), anxiety and eating disorders (14) as well as personality disorders (17–19). In particular, the association between borderline personality disorder and childhood maltreatment is reported in current literature (20), for instance the earlier onset of the disorder in adults who experienced maltreatment through childhood in comparison to those who did not report maltreatment experiences (21). Furthermore, Marchetti et al. (22) were able to identify two personality profiles mediating the association between childhood maltreatment and borderline personality disorder. With one profile being characterized by a high tendency of self-criticism and the other of self-criticism in combination with dependency, they were able to suggest therapy addressing the specific traits, for example cognitive behavioral therapy, compassion focused therapy and schema therapy. Different forms of general health risk factors were found to be associated as well. Experiencing child maltreatment increases the risk for obesity, smoking, and risky sexual behavior (14, 23, 24) as well as alcohol abuse (16). While all of the subtypes are associated with negative health outcomes, a dose-response relationship was shown in more severe health outcomes through co-occurrence of different subtypes (15, 18, 23, 25). In addition to the aforementioned impacted factors, child maltreatment increases the risk of developing physical health issues. The experience of child maltreatment is associated with a higher risk of developing type 2 diabetes (26) with its association being partly mediated by obesity, smoking and high blood pressure (27, 28). It is related with a higher risk of developing chronic obstructive pulmonary disease (COPD) as well (26, 29) and with respiratory diseases in general (30, 31). Furthermore, a higher risk of developing cardiovascular disease is described (32) with higher risk of heart failure (25) and mortality in general (33). Decreased quality of life, higher ratings for anxiety and depression, and a lower cardiac function were found in patients with congenital heart disease who had experienced child maltreatment (34). To the best of our knowledge, this is the first study assessing child maltreatment in patients with CTEPH and the association of its intensity with measures of CTEPH severity, mental well-being and quality of life. Additionally, we assessed the prevalence of child maltreatment using the Childhood Trauma Questionnaire (CTQ) and compared it with the prevalence of the general German population.
This cross-sectional observational study enrolled patients diagnosed with CTEPH in two German pulmonary hypertension referral centers (Hannover Medical School and University of Gießen and Marburg). Local institutional boards (Nr. 8540_BO_K_2019 for Hannover and Nr. 21119 for Giessen and Marburg) approved the study. Inclusion criteria were a diagnosis of CTEPH (WHO Group 4.1) (1, 35), age ≥ 18 years, and mental as well as physical capability of completing all questionnaires in German. Participants were excluded if they did not answer all questionnaires. A current or lifetime psychiatric diagnosis was not considered an exclusion criterium. Four hundred and ninety-three patients (309 from Hannover, 184 from Gießen) were contacted by mail after being identified for meeting the criteria from the databases of both referral centers. Recruitment took place from December 2019 until May 2021. One hundred and seven participants were recruited. All participants provided written informed consent (see Figure 1). The results presented here are part of a larger examining psychosocial factors in patients with CTEPH. We here focused on adverse childhood experiences and its impact on mental well-being and healthy lifestyle.
The Childhood Trauma Questionnaire (CTQ) (36) is a screening instrument retrospectively assessing experiences of child maltreatment including the subscales sexual abuse, physical abuse, emotional abuse, physical neglect and emotional neglect. In this study, the German short version (37, 38) was used, consisting of 28 items rated on a Likert-scale from 1 (never true) to 5 (very often true). Besides the five aforementioned subscales being measured by five items each, there are three additionally items measuring the tendency to minimize experienced maltreatment. Wingenfeld et al. (38) reported high internal consistency for emotional abuse, emotional neglect, physical abuse and sexual abuse (Cronbachs α ≥ 0.89) but not for physical neglect (Cronbachs α = 0.62). In order to measure the prevalence of each subtype, thresholds based on Walker et al. (39) were used, which were used in the prevalence study of the general German population as well (13). In accordance with Walker et al. (39), we utilized a threshold score of 10 for emotional abuse, of 15 for emotional neglect, of 8 for physical abuse, of 9 for physical neglect and of 8 for sexual abuse.
In order to measure the participants' mental well-being, the Hospital Anxiety and Depression scale (HADS) (40) was used assessing symptoms of anxiety and depression. The German version shows high internal consistency for both scales (Cronbachs α = 0.8) (41). Quality of life was investigated with the short version of the WHO Quality of Life Questionnaire (WHOQOL-BREF) (42). Internal consistency (Cronbachs Alpha) for the subscales of the German version range between α = 0.59 and α = 0.91 (43). Furthermore, anthropometric data (age, weight, height, and body mass index) as well as lifestyle factors (alcohol consumption, exercise, and smoking) and socio-demographic information (education, employment) were assessed. Exercise was defined on a scale from 1 (no sport exercise at all) to 6 (sport exercise more than three times a week). Alcohol consumption was measured in drinks per week.
The participants were interviewed by a trained interviewer using the structured clinical interview for DSM-5 (SCID-5; German translation) (44). The interview was conducted either face to face or via telephone depending on the preferences of the participants. The SCID-5 consists of a semi structured interview using questions based on the diagnostic criteria for psychiatric disorders of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (45). The results of these interviews were used for a psychiatric characterization of the participants as reported elsewhere (46) and to control for possible confounders.
Body mass index (BMI), lung function tests including WHO functional class (WHO-FC), serum levels of the N-terminal fragment of pro brain natriuretic peptide (NT-proBNP), 6-min walk distance (6MWD) and the diffusion capacity of the lungs for carbon monoxide (DLCO) were used for the clinical assessments. These parameters were assessed at the time of the study while the hemodynamic parameters were assessed at time of the diagnosis.
In this study both, IBM SPSS Statistics 28.0 (IBM Corp., Armonk, NY, USA) and STATA 13.0 (StataCorp LP, College Station, Texas, USA) statistical software, were used for data-analysis. Depending on its appropriation, either mean and standard deviation (SD) or median and interquartile range (IQR) were used for showing continuous variables. Furthermore, and unless indicated otherwise, n and percent (%) are used for categorical variables. Chi-square tests were used in order to compare prevalence rates of the different types of child maltreatment in CTEPH patients and a general German population presented by Iffland and colleagues (13). Associations between general child maltreatment (total CTQ score), the child maltreatment subtypes (CTQ sub scores), mental well-being (HADS and WHOQOL), and the aforementioned lifestyle factors were analyzed performing partial correlation adjusted for age and gender. The relationship between child maltreatment (total CTQ score) and physical functioning of CTEPH patients (WHO-Functioning class) was assessed through logistic regression analysis. Mildly symptomatic patients (WHO-FC I/II) and patients with more severe symptoms (WHO-FC III/IV) were compared. P < 0.05 were considered statistically significant.
The final sample of this study consisted of 107 patients with mean age of 65 ± 14 years (range, 31–86). There was no significant sex difference between participants who experienced child maltreatment and who did not. None of the participants had current symptoms or a diagnosis of a post-traumatic stress disorder. Most patients (56%) were classified as WHO FC I/II and only 3% as WHO FC IV. For further characteristics (see Table 1).
Fifty-seven percent of the participants had experienced at least one type of child maltreatment. 20.6% reported to have experienced emotional abuse. Furthermore, 19.6% reported physical abuse, 21.5% emotional neglect, 45.8% physical neglect, and 5.6% sexual abuse. Significantly higher rates of emotional abuse [p ≤ 0.001] physical abuse [p = 0.020] and emotional neglect [p = 0.028] were found compared to the general German population (13). Prevalence rates of physical neglect [p = 0.598] and sexual abuse did not differ [p = 0.791] (see Table 2).
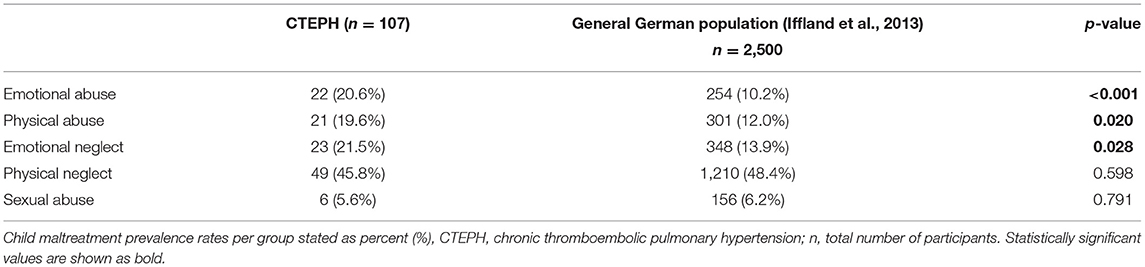
Table 2. Prevalence of child maltreatment and its subtypes of CTEPH in comparison to data from the general German population.
The total CTQ-score was correlated with anxiety symptoms of patients with CTEPH. It was negatively correlated with overall QoL and physical QoL. Emotional abuse was negatively correlated with overall QoL. Emotional neglect correlated with anxiety symptoms and showed negative correlation with physical QoL.
Physical abuse was not correlated with any aspects. Physical neglect correlated with anxiety symptoms and was negatively correlated with physical QoL. Sexual abuse was negatively correlated with overall QoL as well as physical QoL (see Table 3).

Table 3. Partial correlation (Spearman's r) of CTQ-Scores in CTEPH with HADS, QoL, Lifestyle, and WHO FC adjusted for age and gender.
Using a logistic regression model to evaluate the association between child maltreatment and the severity of CTEPH at the time of the study, we defined WHO FC as depended variable with WHO FC I and II being considered asymptomatic and WHO FC III and IV being considered symptomatic. CTQ total score was defined as the independent variable. The model was statistically not significant [p = 0.650]. Therefore, the CTQ total score was not associated with the severity of CTEPH defined by WHO FC class.
In this study, we investigated the prevalence of childhood maltreatment and its association with mental well-being, quality of life, and physical health in patients with CTEPH. More than half of the patients with CTEPH had experienced at least one subtype of childhood maltreatment with physical neglect being the most frequent subtype followed by emotional neglect and emotional abuse. While the prevalence of sexual abuse and physical neglect did not differ from prevalence rates in the general German population, the prevalence of emotional abuse, emotional neglect, and physical abuse were higher in patients with CTEPH. The relatively high rates of different kinds of childhood maltreatment in CTEPH could possibly be explained by changing parenting patterns during past decades. Parenting behavior, which is now considered abusive, was considered acceptable earlier on (47). Our patients had a mean age of 65 years, were born during the 1950s and educated by parents who themselves were survivors of the second world war. Being traumatized after experiencing a war was described to contribute to the next generations' childhood trauma (48, 49). In addition to that, parenting behavior was associated with being passed on from one generation to the other referred to as intergenerational transmission, increasing the likelihood of experiencing childhood maltreatment from former maltreated parents (47). Therefore, the experienced parental trauma and the parenting behavior based on old standards may have contributed to the higher prevalence rates of child maltreatment in this cohort. The high but not significantly different prevalence of physical neglect is reported to be especially apparent in the older German population due to growing up after the Second World War and suffering from privation (50).
Overall childhood maltreatment had a negative impact on general and physical QoL and was positively associated with anxiety symptoms. Furthermore, the subtypes emotional neglect and physical neglect were positively associated with anxiety symptoms as well. Emotional abuse and sexual abuse had a negative impact on overall QoL. Emotional neglect, physical neglect, and sexual abuse had a negative impact on physical QoL. A relationship between child maltreatment and the degree of physical impairment could not be identified.
The reported negative association between childhood maltreatment and overall and physical QoL is in line with other studies (51–53). Mechanistically, it has been suggested that child maltreatment leads to biological and behavioral maladaptation, which interfere with the development of necessary skills to cope with obstacles later in life (54). The behavioral changes are associated with the development of maladaptive schemas in reaction to child maltreatment (55, 56). These schemas are hypothesized to negatively impact the way of dealing with wearing situations in adulthood, with little or no improvement over time (57). In addition to the maladaptive schemas, childhood maltreatment is characterized as increasing the risk of the disrupted ability to recognize and verbalize one's emotions, called alexithymia, increasing the risk of psychopathology (19, 58, 59). Furthermore, emotional dysregulation in general is associated with the experience of childhood maltreatment (60, 61) affecting the psychological well-being negatively by maladaptive coping with obstacles (62). The latter is explained with the need of a primary caretaker as role model in order to learn adequate emotion regulation and problem oriented coping strategies, which children, who experience childhood maltreatment, most likely do not have (63). In contrast maltreatment increases the probability of learning emotional coping strategies through the maltreating caretaker, characterized as avoidance of stressful situations as well as the suppression of emotions in general and the expression of negative emotions already during childhood and adolescence (61, 64) and later in adulthood with increased risk of engaging in substance use (65). The possible presence of maladaptive schemas, the lack of functional coping strategies with stressful events and the resulting impact on self-esteem and interaction might be responsible for the negative association between childhood maltreatment and QoL (54, 55). The association between child maltreatment and anxiety symptoms in this cohort is supported by previous research (14, 34, 66, 67). The likelihood of developing anxiety after experiencing child maltreatment might be explained through an altered stress response. Changes in stress related systems [e.g., hypothalamus-pituitary-adrenal (HPA) axis, autonomic nervous system, serotonin transporter gene] tend to increase the anxiety sensitivity (68, 69). As CTEPH is a potentially life-threatening disease and debilitating symptoms as dyspnea are present, the increased anxiety sensitivity might be considered as a reason for the associations found in this study.
We did not find an association between child maltreatment of any kind and depressive symptoms as well as with other health risk factors such as BMI, smoking, low exercise and alcohol consumption. The result contrasts with the high prevalence rates of maltreatment found in this cohort and the strong association described between the aforementioned factors and child maltreatment in other cohorts (14, 16, 23, 54, 70). Additionally, we did not find an association between physical abuse and QoL, which is in contrast to other studies pointing out the influence of physical abuse on QoL (54). The lacking associations might be explained by the low number of participants in our study, masking the effects of childhood maltreatment on psychological and behavioral factors. A further possible explanation could be resilience as it was reported to lower the risk of developing depression after the experience of child maltreatment (71). Resilience is defined as adaptation to adverse experiences, showing at least average functioning in various domains and an absence of pathology (72). It is viewed as a dynamic process which therefore does not exclude the possibility of functioning in some domains while not in others (73). The absence of the association with common health risk factors and depressive symptoms in this study might be explainable by enough protective factors within the participants to cope in a functional way with the experienced trauma instead of engaging in maladaptive behavior as smoking, low exercise, and alcohol consumption. Further investigation on the effect of childhood maltreatment and resilience simultaneously might help to further elucidate the mechanism between resilience on the one hand and maladaptation on the other hand.
Moreover, the absence of a direct impact of child maltreatment on the severity of CTEPH might be explainable with resilience as well as the underlying mechanisms and risk factors for developing CTEPH. Wegman and Stetler (31) described the association of child maltreatment with cardiovascular and respiratory diseases with a greater risk to engage in health risking behavior as smoking and consuming alcohol. Other studies described this mediating effect as well (25, 26) which could be missing in this cohort due to the lack of association between childhood maltreatment and the aforementioned health risk behaviors. Another reason for the missing impact of childhood maltreatment on CTEPH severity might refer to the dose-response relationship. Studies who investigated on the mental and physical health outcome of participants who experienced child maltreatment reported an increased risk especially in association with the co-occurrence of different subtypes (15, 23, 25, 26). In contrast to that, more than half of the participants who reported child maltreatment in this study, had experienced not more than one subtype, and less than one third had experienced three or more subtypes. Further studies with a larger sample might be needed to further investigate on the relationship between child maltreatment and severity of CTEPH.
In comparison to the general German population, three out of five maltreatment subtypes were present with higher prevalence in our CTEPH cohort. This implies the question whether childhood maltreatment might be associated with the development of CTEPH later in life. A possible link between childhood maltreatment and thromboembolic events might be seen via alterations of the inflammatory response. In fact, inflammation is linked to the development of CTEPH besides other risk factors such as acute pulmonary embolism, medical interventions (e.g., splenectomy and ventriculoarterial shunt) and plasmatic factors (74). Inflammatory markers like the C-reactive protein (CRP) were shown to be increased in comparison to healthy controls (75). As CRP was found to be associated with childhood trauma as well (76), changes in the inflammatory response could mediate the effect between child maltreatment and developing CTEPH. Molecular changes in maltreated individuals are associated with epigenetic changes in response to the experienced trauma. Alterations in DNA methylation are associated with altered gene expression, influencing for example the stress response and inflammatory processes (77, 78). Further studies on the mediating effect of epigenetic alterations due to child maltreatment associating it with CTEPH patients may be needed to clarify the exact relationship.
Regarding the conception of this study, limitations have to be acknowledged. Child maltreatment was assessed with the CTQ, which is based on self-report and retrospection making a recall bias possible (13, 79). Furthermore, out of the contacted CTEPH patients, only 22% responded and were included into the assessment. Hence, the sample size was low in comparison to other studies focusing on the consequences of childhood maltreatment [e.g., (25, 33)]. One contributor to the low response rate may have been the higher age of our patient population compared to other studies. Furthermore, the motivation to participate might have been limited as many of the patients were no longer followed at their PH center (especially those who had undergone successful PEA surgery). In addition, the questionnaires had been sent out without personal advance notice from their PH physicians.
In conclusion, more than half of our patients with CTEPH had experienced at least one type of child maltreatment. A history of child maltreatment had a negative impact on QoL and was associated with anxiety symptoms. In order to improve the treatment of patients with CTEPH, the presence of experienced childhood maltreatment should be considered. Further studies are needed to assess tools that may help patients to cope better with the consequences of CTEPH.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee, Hannover Medical School, Hannover Germany and Ethics Committee, University Medical Center Gießen und Marburg, Marburg, Germany. The patients/participants provided their written informed consent to participate in this study.
NL, JF, MH, KK, KO, and M-RD were responsible for study design, implementation of the study, statistical analysis, data interpretation, and drafting the manuscript. NL and M-RD were responsible for conducting the interviews. NL, JF, and M-RD did data collection. JK, MR, and HGa implementation of the study. IH, D-HP, HGh, DE, JK, MR, HGa, TM, and H-DK were responsible for study design, data interpretation, and revising the manuscript. All authors contributed to the article and approved the submitted version.
This work was funded by the German Center for Lung Research (DZL).
MH has received honoraria for lectures and/or consultations from Acceleron, Actelion, Bayer, GSK, Janssen, MSD and Pfizer, and all outside the present study. D-HP has received honoraria for lectures and/or consultationsf rom Janssen. HGa has received personal fees from Actelion, personal fees from AstraZeneca, personal fees from Bayer, personal fees from BMS, personal fees from GSK, personal fees from Janssen-Cilag, personal fees from Lilly, personal fees from MSD, personal fees from Novartis, personal fees from OMT, personal fees from Pfizer, personal fees from United Therapeutics, outside the submitted work. HGh has received fees from Actelion, Bayer, Gilead, GSK, MSD, Pfizer and United Therapeutics, outside the present work. KK has received honoraria forconsultations and/or lectures from Eli Lilly, Janssen, Lundbeck, Neuraxpharm, Otsuka, Pfizer, Servier, Schwabe, Takeda and Trommsdorff/Ferrer, Alexion, and CannaXan (advisory board). KO has received honoraria for lectures and/or consultations from Acceleron, Actelion, Bayer, GSK, Janssen, MSD, United Therapeutics and Pfizer, and all outside the present study. H-DK was employed by Pulmonale Hypertonie eV.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We wish to thank all patients who participated in this project. Furthermore, we wish to thank the German Center for Lung Research (DZL) for their cooperation as well as ‘Pulmonale Hypertonie e.V' for their support.
1. Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. (2015). ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. (2016) 37:67–119. doi: 10.1093/eurheartj/ehv317
2. Wilkens H, Konstantinides S, Lang I, Bunck A, Gerges M, Gerhardt F, et al. Chronisch thromboembolische pulmonale Hypertonie: Empfehlungen der Kölner Konsensus Konferenz 2016. Dtsch Med Wochenschr. (2016) 141:S62–S9. doi: 10.1055/s-0042-114529
3. Hoeper MM, Madani MM, Nakanishi N, Meyer B, Cebotari S, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Lancet Respir Med. (2014) 2:573–82. doi: 10.1016/S2213-2600(14)70089-X
4. Cannon JE, Su L, Kiely DG, Page K, Toshner M, Swietlik E, et al. Dynamic risk stratification of patient long-term outcome after pulmonary Endarterectomy: results from the United Kingdom national cohort. Circulation. (2016) 133:1761–71. doi: 10.1161/CIRCULATIONAHA.115.019470
5. Hoeper MM, Ghofrani HA, Grünig E, Klose H, Olschewski H, Rosenkranz S. Pulmonary hypertension. Dtsch Arzteblatt Int. (2017) 114:73–84. doi: 10.3238/arztebl.2016.0073
6. Olsson KM, Wiedenroth CB, Kamp J-C, Breithecker A, Fuge J, Krombach GA, et al. Balloon pulmonary angioplasty for inoperable patients with chronic thromboembolic pulmonary hypertension: the initial German experience. Eur Respir J. (2017) 49:1602409. doi: 10.1183/13993003.02409-2016
7. Kramm T, Wilkens H, Fuge J, Schäfers H-J, Guth S, Wiedenroth CB, et al. Incidence and characteristics of chronic thromboembolic pulmonary hypertension in Germany. Clin Res Cardiol. (2018) 107:548–53. doi: 10.1007/s00392-018-1215-5
8. Ivarsson B, Hesselstrand R, Rådegran G, Kjellström B. Health-related quality of life, treatment adherence and psychosocial support in patients with pulmonary arterial hypertension or chronic thromboembolic pulmonary hypertension. Chron Respir Dis. (2019) 16:1479972318787906. doi: 10.1177/1479972318787906
9. Mathai SC, Ghofrani HA, Mayer E, Pepke-Zaba J, Nikkho S, Simonneau G. Quality of life in patients with chronic thromboembolic pulmonary hypertension. Eur Respir J. (2016) 48:526–37. doi: 10.1183/13993003.01626-2015
10. Tajima H, Kasai H, Tanabe N, Sugiura T, Miwa H, Naito A, et al. Clinical characteristics and prognosis in patients with chronic thromboembolic pulmonary hypertension and a concomitant psychiatric disorder. Pulm Circ. (2019) 9:1–9. doi: 10.1177/2045894019836420
11. Leeb RT, Paulozzi LJ, Melanson C, Simon TR, Arias I. CHILD MALTREATMENT SURVEILLANCE: uniform definitions for Public Health and Recommended Data Elements (Version 1.0). Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2008).
12. Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, van Ijzendoorn MH. The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Review. (2015) 24:37–50. doi: 10.1002/car.2353
13. Iffland B, Brähler E, Neuner F, Häuser W, Glaesmer H. Frequency of child maltreatment in a representative sample of the German population. BMC Public Health. (2013) 13:980. doi: 10.1186/1471-2458-13-980
14. Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. (2012) 9:e1001349. doi: 10.1371/journal.pmed.1001349
15. Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, et al. Adverse childhood experiences and adult risk factors for age-related disease depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. (2009) 163:1135–43. doi: 10.1001/archpediatrics.2009.214
16. Merrick MT, Ford DC, Ports KA, Guinn AS, Chen; Jieru, Klevens J, et al. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention - 25 states, 2015-2017. Morb Mortal Weekly Rep. (2019) 68:999–1005. doi: 10.15585/mmwr.mm6844e1
17. Cirasola A, Hillman S, Fonagy P, Chiesa M. Mapping the road from childhood adversity to personality disorder: the role of unresolved states of mind. Pers Mental Health. (2017) 11:77–90. doi: 10.1002/pmh.1365
18. Hengartner M, Ajdacic-Gross V, Rodgers S, Müller M, Rössler W. Childhood adversity in association with personality disorder dimensions: new findings in an old debate. Eur Psychiatry. (2013) 28:476–82. doi: 10.1016/j.eurpsy.2013.04.004
19. Berenbaum H. Childhood abuse, alexithymia and personality disorder. J Psychosom Res. (1996) 41:585–95. doi: 10.1016/S0022-3999(96)00225-5
20. Steele K, Townsend M, Grenyer B. Parenting and personality disorder: an overview and meta-synthesis of systematic reviews. PLoS One. (2019) 14:e0223038. doi: 10.1371/journal.pone.0223038
21. Bozzatello P, Rocca P, Bellino S. Trauma and psychopathology associated with early onset BPD: an empirical contribution. J Psychiatr Res. (2020) 131:54–9. doi: 10.1016/j.jpsychires.2020.08.038
22. Marchetti D, Musso P, Verrocchio M, Manna G, Kopala-Sibley D, De Berardis D, et al. Childhood maltreatment, personality vulnerability profiles, and borderline personality disorder symptoms in adolescents. Dev Psychopathol. (2021) 26:1–14. doi: 10.1017/S0954579420002151
23. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults the Adverse Childhood Experiences (ACE) study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
24. Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. (2017) 2:e356–e66. doi: 10.1016/S2468-2667(17)30118-4
25. Ho FK, Celis-Morales C, Gray SR, Petermann-Rocha F, Lyall D, Mackay D, et al. Child maltreatment and cardiovascular disease: quantifying mediation pathways using UK Biobank. BMC Med. (2020) 18:143. doi: 10.1186/s12916-020-01603-z
26. Clemens V, Huber-Lang M, Plener PL, Brähler E, Brown RC, Fegert JM. Association of child maltreatment subtypes and long-term physical health in a German representative sample. Eur J Psychotraumatol. (2018) 9:1510278. doi: 10.1080/20008198.2018.1510278
27. Shields ME, Hovdestad WE, Pelletier C, Dykxhoorn JL, O'Donnell SC, Tonmyr L. Childhood maltreatment as a risk factor for diabetes: findings from a population-based survey of Canadian adults. BMC Public Health. (2016) 16:879. doi: 10.1186/s12889-016-3491-1
28. Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. (2008) 121:e1240–e9. doi: 10.1542/peds.2007-2403
29. Shields ME, Hovdestad WE, Gilbert CP, Tonmyr LE. Childhood maltreatment as a risk factor for COPD: findings from a population-based survey of Canadian adults. Int J COPD. (2016) 11:2641–50. doi: 10.2147/COPD.S107549
30. Goodwin RD, Stein MB. Association between childhood trauma and physical disorders among adults in the United States. Psychol Med. (2004) 34:509–20. doi: 10.1017/S003329170300134X
31. Wegman HL, Stetler C. A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosom Med. (2009) 71:805–12. doi: 10.1097/PSY.0b013e3181bb2b46
32. Clemens V, Bürgin D, Huber-lang M, Plener PL, Brähler E, Fegert JM. The interplay between child maltreatment and stressful life events during adulthood and cardiovascular problems -a representative study. J Clin Med. (2021) 10:3937. doi: 10.3390/jcm10173937
33. Pierce JB, Kershaw KN, Kiefe CI, Jacobs DR, Sidney S, Merkin SS, et al. Association of childhood psychosocial environment with 30-year cardiovascular disease incidence and mortality in middle age. J Am Heart Assoc. (2020) 9:e015326 doi: 10.1161/JAHA.119.015326
34. Proskynitopoulos PJ, Heitland I, Glahn A, Bauersachs J, Westhoff-Bleck M, Kahl KG. Prevalence of child maltreatment in adults with congenital heart disease and its relationship with psychological well-being, health behavior, and current cardiac function. Front Psychiatry. (2021) 12:686169. doi: 10.3389/fpsyt.2021.686169
35. Galiè N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. (2009) 30:2493–537. doi: 10.1183/09031936.00139009
36. Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Selfreport Manual. Texas: The Psychological Corporation (1998).
37. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Neglect. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
38. Wingenfeld K, Spitzer C, Mensebach C, Grabe HJ, Hill A, Gast U, et al. The German version of the Childhood Trauma Questionnaire (CTQ): preliminary psychometric properties. Psychother Psychosom Med Psychol. (2010) 60:442–50. doi: 10.1055/s-0030-1247564
39. Walker EA, Gelfand A, Katon WJ, Koss MP, von Korff M, Bernstein D, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. (1999) 107:332–9. doi: 10.1016/S0002-9343(99)00235-1
40. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
41. Herrmann-Lingen C, Buss U, Snaith RP. Hospital Anxiety and depression Scale - Deutsche Version. In: Snaith vRP, Zigmond AS, Deutsche Adaptation der Hospital Anxiety and Depression Scale (HADS). 4th ed. Göttingen: Hogrefe (2011).
42. THE WHOQOL GROUP. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. (1998) 28:551–8. doi: 10.1017/S0033291798006667
43. Angermeyer MC, Kilian R, Matschinger H. WHOQOL-100 und WHOQOL-BREF: Handbuch für die deutschsprachigen Versionen der WHO Instrumente zur Erfassung von Lebensqualität, 1st Edn. Göttingen: Hogrefe (2000).
44. Beesdo-Baum K, Zaudig M, Wittchen H-U. Strukturiertes Klinisches Interview für DSM-5-Störungen - Klinische Version. In: First MB, Williams JBW, Karg RS, Spitzer RL, editors. Deutsche Bearbeitung des Structured Clinical Interview for DSM-5 Disorders - Clinician Version von. 1st Edn. Göttingen: Hogrefe (2019).
46. Dering M-R, Lepsy N, Fuge J, Meltendorf T, Hoeper MM, Heitland I, et al. Prevalence of mental disorders in patients with chronic thromboembolic pulmonary hypertension. Front Psychiatry. (2022) 13:821466. doi: 10.3389/fpsyt.2022.821466
47. Assink M, Spruit A, Schuts M, Lindauer R, van der Put CE, Stams GJJM. The intergenerational transmission of child maltreatment: a three-level meta-analysis. Child Abuse Neglect. (2018) 84:131–45. doi: 10.1016/j.chiabu.2018.07.037
48. Yehuda R, Halligan SL, Grossman R. Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Dev Psychopathol. (2001) 13:733–53. doi: 10.1017/S0954579401003170
49. Castro-Vale I, Severo M, Carvalho D, Mota-Cardoso R. Intergenerational transmission of war-related trauma assessed 40 years after exposure. Ann Gen Psychiatry. (2019) 18:14. doi: 10.1186/s12991-019-0238-2
50. Häuser W, Schmutzer G, Brähler E, Glaesmer H. Misshandlungen in Kindheit und Jugend: Ergebnisse einer Umfrage in einer repräsentativen Stichprobe der Deutschen Bevölkerung. Dtsch Ärzteblatt Int. (2011) 108:287–94. doi: 10.3238/arztebl.2011.0287
51. Afifi TO, Enns MW, Cox BJ, de Graaf R, ten Have M, Sareen J. Child abuse and health-related quality of life in adulthood. J Nervous Mental Dis. (2007) 195:797–804. doi: 10.1097/NMD.0b013e3181567fdd
52. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. (2009) 373:68–81. doi: 10.1016/S0140-6736(08)61706-7
53. Corso PS, Edwards VJ, Fang X, Mercy JA. Health-related quality of life among adults who experienced maltreatment during childhood. Am J Public Health. (2008) 98:1094–100. doi: 10.2105/AJPH.2007.119826
54. Weber S, Jud A, Landolt MA. Quality of life in maltreated children and adult survivors of child maltreatment: a systematic review. Qual Life Res. (2016) 25:237–55. doi: 10.1007/s11136-015-1085-5
55. Pilkington PD, Bishop A, Younan R. Adverse childhood experiences and early maladaptive schemas in adulthood: a systematic review and meta-analysis. Clin Psychol Psychother. (2021) 28:569–84. doi: 10.1002/cpp.2533
56. Young JE, Klosko JS, Weishaar ME. Schema Therapy: A Practitioner's Guide. New York, NY: Guilford Press (2003).
57. Blissett J, Walsh J, Harris G, Jones C, Leung N, Meyer C. Different core beliefs predict paternal and maternal attachment representations in young women. Clin Psychol Psychother. (2006) 13:163–71. doi: 10.1002/cpp.482
58. Brown S, Fite PJ, Stone K, Bortolato M. Accounting for the associations between child maltreatment and internalizing problems: the role of alexithymia. Child Abuse Neglect. (2016) 52:20–8. doi: 10.1016/j.chiabu.2015.12.008
59. Brown S, Fite PJ, Stone K, Richey A, Bortolato M. Associations between emotional abuse and neglect and dimensions of alexithymia: the moderating role of sex. Psychol Trauma. (2018) 10:300–8. doi: 10.1037/tra0000279
60. Jennissen S, Holl J, Mai H, Wolff S, Barnow S. Emotion dysregulation mediates the relationship between child maltreatment and psychopathology: a structural equation model. Child Abuse Neglect. (2016) 62:51–62. doi: 10.1016/j.chiabu.2016.10.015
61. Gruhn MA, Compas BE. Effects of maltreatment on coping and emotion regulation in childhood and adolescence: a meta-analytic review. Child Abuse Neglect. (2020) 103:104446. doi: 10.1016/j.chiabu.2020.104446
62. De Berardis D, Fornaro M, Orsolini L, Ventriglio A, Vellante F, Di Giannantonio M. Emotional dysregulation in adolescents: implications for the development of severe psychiatric disorders, substance abuse, and suicidal ideation and behaviors. Brain Sci. (2020) 10:1–5. doi: 10.3390/brainsci10090591
63. Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Soc Dev. (2007) 16:361–88. doi: 10.1111/j.1467-9507.2007.00389.x
64. VanMeter F, Handley ED, Cicchetti D. The role of coping strategies in the pathway between child maltreatment and internalizing and externalizing behaviors. Child Abuse Neglect. (2020) 101:104323. doi: 10.1016/j.chiabu.2019.104323
65. Wolff S, Holl J, Stopsack M, Arens E, Höcker A, Staben K, et al. Does emotion dysregulation mediate the relationship between early maltreatment and later substance dependence? Findings of the CANSAS Study. Eur Addict Res. (2016) 22:292–300. doi: 10.1159/000447397
66. Simon NM, Herlands NN, Marks EH, Mancini C, Letamendi A, Li Z, et al. Childhood maltreatment linked to greater symptom severity and poorer quality of life and function in social anxiety disorder. Depress Anxiety. (2009) 26:1027–32. doi: 10.1002/da.20604
67. Karatekin C, Almy B, Mason SM, Borowsky I, Barnes A. Mental and physical health profiles of maltreated youth. Child Abuse Neglect. (2018) 84:23–33. doi: 10.1016/j.chiabu.2018.07.019
68. Karatsoreos IN, McEwen BS. Psychobiological allostasis: resistance, resilience and vulnerability. Trends Cogn Sci. (2011) 15:576–84. doi: 10.1016/j.tics.2011.10.005
69. Stein MB, Schork NJ, Gelernter J. Gene-by-environment (serotonin transporter and childhood maltreatment) interaction for anxiety sensitivity, an intermediate phenotype for anxiety disorders. Neuropsychopharmacology. (2008) 33:312–9. doi: 10.1038/sj.npp.1301422
70. Gardner MJ, Thomas HJ, Erskine HE. The association between five forms of child maltreatment and depressive and anxiety disorders: a systematic review and meta-analysis. Child Abuse Neglect. (2019) 96:104082 doi: 10.1016/j.chiabu.2019.104082
71. Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Neglect. (2007) 31:211–29. doi: 10.1016/j.chiabu.2007.02.004
72. Walsh WA, Dawson J, Mattingly MJ. How are we measuring resilience following childhood maltreatment? Is the research adequate and consistent? what is the impact on research, practice, and policy? Trauma Violence Abuse. (2010) 11:27–41. doi: 10.1177/1524838009358892
73. Afifi TO, Macmillan HL. In review resilience following child maltreatment: a review of protective factors. Can J Psychiatry. (2011) 56:266–72. doi: 10.1177/070674371105600505
74. Kim NH, Lang IM. Risk factors for chronic thromboembolic pulmonary hypertension. Eur Respir Rev. (2012) 21:27–31. doi: 10.1183/09059180.00009111
75. Quarck R, Nawrot T, Meyns B, Delcroix M. C-Reactive protein. A new predictor of adverse outcome in pulmonary arterial hypertension. J Am Coll Cardiol. (2009) 53:1211–8. doi: 10.1016/j.jacc.2008.12.038
76. Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. (2016) 21:642–9. doi: 10.1038/mp.2015.67
77. Cicchetti D, Hetzel S, Rogosch FA, Handley ED, Toth SL. An investigation of child maltreatment and epigenetic mechanisms of mental and physical health risk. Dev Psychopathol. (2016) 28:1305–17. doi: 10.1017/S0954579416000869
78. Parade SH, Huffhines L, Daniels TE, Stroud LR, Nugent NR, Tyrka AR. A systematic review of childhood maltreatment and DNA methylation: candidate gene and epigenome-wide approaches. Transl Psychiatry. (2021) 11:134. doi: 10.1038/s41398-021-01207-y
Keywords: chronic thromboembolic pulmonary hypertension, pulmonary hypertension, childhood maltreatment, childhood trauma questionnaire, CTQ, CTEPH, quality of life
Citation: Lepsy N, Dering MR, Fuge J, Meltendorf T, Hoeper MM, Heitland I, Kamp JC, Park DH, Richter MJ, Gall H, Ghofrani HA, Ellermeier D, Kulla HD, Olsson KM and Kahl KG (2022) Childhood Maltreatment, Mental Well-Being, and Healthy Lifestyle in Patients With Chronic Thromboembolic Pulmonary Hypertension. Front. Psychiatry 13:821468. doi: 10.3389/fpsyt.2022.821468
Received: 24 November 2021; Accepted: 31 January 2022;
Published: 24 February 2022.
Edited by:
Francesco Monaco, Azienda Sanitaria Locale Salerno, ItalyReviewed by:
Domenico De Berardis, Azienda Usl Teramo, ItalyCopyright © 2022 Lepsy, Dering, Fuge, Meltendorf, Hoeper, Heitland, Kamp, Park, Richter, Gall, Ghofrani, Ellermeier, Kulla, Olsson and Kahl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai G. Kahl, a2FobC5rYWlAbWgtaGFubm92ZXIuZGU=
†These authors have contributed equally to this work
‡These authors share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.