
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 02 February 2022
Sec. Mood Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.803639
 Ju-Yeon Lee1
Ju-Yeon Lee1 Robert Stewart2,3
Robert Stewart2,3 Hee-Ju Kang1
Hee-Ju Kang1 Ju-Wan Kim1
Ju-Wan Kim1 Min Jhon1
Min Jhon1 Sung-Wan Kim1
Sung-Wan Kim1 Il-Seon Shin1
Il-Seon Shin1 Jae-Min Kim1*
Jae-Min Kim1*Objectives: This study was performed to investigate the roles of childhood abuse and social support in predicting short- and long-term pharmacological treatment outcomes in outpatients with depressive disorders in a naturalistic 1-year prospective design.
Methods: Patients were recruited at a university hospital in South Korea between March 2012 and April 2017. Subjects with stepwise pharmacotherapy (switching, augmentation, combination, and mixture of these approaches) included 1246 patients at 12-week points in the acute treatment response and 1,015 patients at 12-months in the long-term treatment response. Remission was defined as Hamilton Depression Rating Scale score ≤ 7. Exposure to three types of childhood abuse (physical, emotional, and sexual) before the age of 16 and perceived social support were assessed at baseline.
Results: Individual associations of childhood abuse were associated with poorer treatment outcomes in the 12-month long-term phase, and no significant individual associations were found for social support level with any period outcome. In combination, any child abuse, emotional abuse, and physical abuse were significantly associated with long-term 12-month remission rate in the presence of higher level of social support after adjustment with significant interaction terms. However, no significant interactions were found with sexual abuse.
Conclusion: Synergistic interactive effects of child abuse and social support levels on treatment outcomes in depressive patients were found during long-term pharmacotherapy. Thus, depressed patients with a history of childhood abuse may require specialized clinical approaches, including social support, to enhance the long-term treatment outcomes.
Childhood abuse increases the risk of the development of depression in adulthood (1, 2). Childhood abuse is associated with the severity of adult depression and leads to elevated risk of early onset, recurrent, and chronic depression (3). Various forms of childhood abuse, including emotional, physical, and sexual abuse, are notably prevalent in the general population, with 53.4% of adults in an epidemiological study having experienced at least one form of child abuse in childhood (4). Relative to other forms of child abuse, sexual abuse has received the most empirical attention (5), but there is as yet no consensus on which type(s) of child abuse can specifically predict depression in adulthood.
Childhood abuse has been discussed as an important factor influencing not only the course of depression but also treatment response to pharmacotherapy for adult depression. A meta-analysis of previous studies showed that depressive patients with a history of childhood abuse showed a poorer outcome of pharmacological treatment compared to those without a history of child abuse (odds ratio = 1.26, 95% CI = 1.01–1.56) (6). However, the treatment periods of related studies included in this meta-analysis varied from weeks to several months. Especially, studies with short-term (12-week) treatment revealed that childhood abuse was not associated with response to antidepressants alone (7, 8). Other than the study period, there were also differences in consideration of potential covariates that could contribute to the association between childhood abuse and treatment outcome (9, 10). A study on the interaction between childhood abuse and time over a 12-week course of pharmacotherapy indicated that probability of remission increased significantly faster over time for patients without a history of clinically significant abuse compared to those with such a history (9). They suggested that the gap in remission rates according to time may be due to psychosocial issues beyond medication effects. Therefore, there is a need for investigation into psychosocial moderators that could affect treatment outcomes over time in adults with a history of childhood abuse.
Social support, which refers to an individual's sense that they are cared about and held in positive regard by those in their support networks, is an important psychosocial factor related to the associations between a history of childhood abuse and mental health outcomes (10–12). Previous studies showed that social support buffered the impact of child abuse on risk of depression in adulthood (13–15). Perceived social support was suggested to be associated with reduced pathogenic effects of life stress and to be a protective factor against current depression among adults with a history of childhood adversity (16–18). A prospective cohort study reported that social support played a significant role in moderating the relationship between childhood abuse and subsequent depression in adulthood (19). The importance of social support in affecting disease outcomes was suggested to involve physiological as well as psychosocial mechanisms (20). However, to our knowledge, there have been no previous studies regarding the role of social support as a moderator of a history of child abuse on depression treatment outcomes during antidepressant pharmacotherapy.
The present study was performed to examine whether there is a critical period in which childhood abuse as a predictor of poorer outcome affects antidepressant treatment response during the long-term phase, to examine the interactive effects of childhood abuse and social support on the treatment outcome during pharmacotherapy, and to determine whether there are differences in these associations according to type of child abuse. To address these issues, we analyzed the impact of predictors based on a longitudinal study involving both acute (12 weeks) and continuation phases (12 months) of long-term stepwise pharmacotherapy.
This study was carried out as a component of the MAKE Biomarker discovery for Enhancing anTidepressant Treatment Effect and Response (MAKE BETTER) program. Details of the study have been published as a design paper (21) and registered with cris.nih.go.kr (identifier: KCT0001332). To reflect real-world treatment settings, participants were enrolled regardless of depression subtype or physical comorbidity. Treatment interventions were also conducted in a naturalistic fashion in determining the type, dose, and regimen of antidepressant and other medications, considering patient preference as well as clinician decisions, but were guided by pre-planned measurements and time points. After a 3-week antidepressant monotherapy period, the next treatment steps with alternative strategies could be initiated every 3 weeks during the acute treatment phase (3, 6, 9, and 12 weeks), and every 3 months during the continuation treatment phase (6, 9, and 12 months). All data on sociodemographic and clinical characteristics at baseline and treatment-related variables at follow-ups were obtained using a structured clinical report form (CRF) by clinical research coordinators who were blinded to treatment modalities. These staff were trained in CRF implementation and data collection methods by the research psychiatrists. Patients' data were recorded on a CRF, registered on the website of the MAKE BETTER study (http://icreat.nih.go.kr/icreat/webapps/com/hismainweb/jsp/cdc_n2.live) within 3 days, and monitored by data management center personnel. The population in this study is the same as in the previous our study which was carried out as a component of MAKE Biomarker discovery for Enhancing anTidepressant Treatment Effect and Response (MAKE BETTER) program, and the methods might be some overlap with previous study (22). However, in this study, we investigated the roles of childhood abuse and social support in predicting short- and long-term pharmacological treatment outcomes compared to previous study that investigated predictors of relapse in an outpatient clinical sample with depressive disorders receiving stepwise pharmacotherapy based on early clinical decision-making, applying a naturalistic 24-month prospective design.
Patients with depressive disorders were consecutively recruited from March 2012 to April 2017 from those who had visited the outpatient psychiatric department of (removed for review) Hospital. All inclusion instances represented new treatment episodes, i.e., taking newly initiated antidepressant treatment, regardless of whether depressive symptoms were first-onset or recurrent. As the primary objective of the MAKE BETTER study was to discover predictive markers for antidepressant treatment response, all participants were enrolled with consent to receive antidepressant-based treatment approaches only. Inclusion criteria were: age > 7 years; diagnosis of major depressive disorder (MDD), dysthymic disorder, or depressive disorder not otherwise specified (NOS), using the Mini-International Neuropsychiatric Interview (MINI) (23), a structured diagnostic psychiatric interview based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria (24); Hamilton Depression Rating Scale (HAMD) (25) score ≥14; able to complete questionnaires, understand the objective of the study, and sign the informed consent form. Exclusion criteria were as follows: unstable or uncontrolled medical condition; unable to complete the psychiatric assessment or comply with the medication regimen due to severe physical illness; current or lifetime DSM-IV diagnosis of bipolar disorder, schizophrenia, schizoaffective disorder, schizophreniform disorder, psychotic disorder NOS, or other psychotic disorder; history of organic psychosis, epilepsy, or seizure disorder; history of anticonvulsant treatment; hospitalization for any psychiatric diagnosis other than depressive disorder (e.g., alcohol/drug dependence); electroconvulsive therapy received for the current depressive episode; and pregnant or breastfeeding. All participants reviewed the consent form and provided written informed consent. For participants aged under 16, written consent was obtained from a parent or legal guardian, and written assent was obtained from the participant. All patients gave written informed consent to participate in the study and use their data. The study was approved by the Ethics Commission of the Chonnam National University Hospital Institutional Review Board as it uses de-identified data. It was registered at cris.nih.go.kr (identifier: KCT0001332).
History of childhood abuse was assessed with the Nemesis Childhood Trauma Interview (26). In this semi-structured interview, participants were asked whether they had ever experienced emotional or psychological, physical, or sexual abuse before the age of 16. Emotional abuse was evaluated by asking, “Were you emotionally or psychologically abused, meaning being yelled at, falsely punished, subordinated to your siblings or being blackmailed?”; physical abuse was evaluated by asking, “Were you abused physically, meaning being hit, kicked, beaten up, or other types of physical abuse?”; and sexual abuse was evaluated by asking, “Were you sexually abused, meaning being touched or having to touch someone in a sexual way or pressured into sexual contact against your will?” As these forms of abuse often occur together (27, 28), a broad definition of “childhood abuse” (having at least one type of abuse) was used for the primary analysis. In this study, participants who had experienced more than one of the three types of child abuse were classified as the “present” group. In the present study, the Cronbach's α values was 0.67, indicating reliable internal consistency.
Social support was evaluated by the Multidimensional Scale of Perceived Social Support (MSPSS) (29). The MSPSS is a brief measure of a respondent's perception of the social support that they receive from three different sources: a significant other, family, and friends, and consists of 12 items rated on a seven-point Likert-type scale (1, very strongly disagree; 7, very strongly agree). The possible score range is between 12 and 84, with higher scores indicating higher degree of perceived social support. As there is no standard cutoff, the total scores of scales were dichotomized at the median into low and high social support groups. Previous study found that the Korean version of the MSPSS was valid and useful for assessing social support in the Korean population (30).
The sociodemographic characteristics examined consisted of age, sex, number of years of formal education, marital status (currently married or not), cohabitation status (living alone or not), religion (religious observance or not), occupation (currently employed or not), and monthly income (above or below 2000 USD). The clinical characteristics evaluated were diagnoses of depressive disorders as outlined above with certain specifiers, age at onset and duration of illness(es), number of previous depressive episodes, duration of present episode, family history of depression, and number of concurrent physical disorders (applying a questionnaire enquiring about 15 different systems or disorders).
Assessment scales for investigating symptoms and function were administered. Depressive and anxiety symptoms were evaluated by the Hospital Anxiety Depression Scale-Depression subscale (HADS-D) and anxiety subscale (HADS-A) (31), respectively; quality of life by the EuroQol-5D (EQ-5D) (32); functioning level by the Social and Occupational Functioning Assessment Scale (SOFAS) (24); number of stressful life events by the Life Experiences Survey (LES) (33); subjective perception of stress by the Perceived Stress Scale (PSS) (34); psychological resilience by the Connor-Davidson Resilience Scale (CDRS) (35); and screening for alcohol-related problems by the Alcohol Use Disorders Identification Test (AUDIT) (36). Higher scores on HADS-D, HADS-A, EQ-5D, LES, PSS, and AUDIT and lower scores on SOFAS and CDRS indicate more severe symptomatology. All scales had been formally translated into the Korean language. In addition, their validity and reliability had been confirmed with acceptable levels in Korean setting (37–42).
Details of the treatment in this study have been published previously (21, 43). Prior to commencement of treatment, a comprehensive review was made of the patients' clinical manifestations (e.g., psychotic and anxiety symptoms), severity of illness, physical comorbidities and medication profiles, and history of previous treatments. Minimal and maximal dosages of pharmacological agents were determined considering existing treatment guidelines (44, 45). In the first treatment step, patients received antidepressant treatment, taking into consideration these data and treatment guidelines (45–47), for 3 weeks. The antidepressants used were bupropion, desvenlafaxine, duloxetine, escitalopram, fluoxetine, mirtazapine, paroxetine, sertraline, venlafaxine, and vortioxetine. After the first antidepressant monotherapy treatment step, the next step of pharmacotherapy was administered every 3 weeks during the acute treatment phase (3, 6, 9, and 12 weeks with a 3-day allowable window) and every 3 months during the continuation treatment phase (6, 9, and 12 months with a 7-day allowable window), whenever needed. At the end of each step, overall effectiveness and tolerability were reviewed prior to proceeding with measurement-based next-step treatments. In cases of insufficient improvement (HAMD score reduction <30% from baseline) or intolerable side effects, patients were instructed to choose whether they would prefer to remain in the current step or enter the next step strategy with switching (S), augmentation (A), combination (C), S + A, S + C, A + C, and S + A + C treatment. Patients were also allowed to receive next-step treatment if they showed sufficient improvement (HAMD score reduction ≥30% from baseline) with absence/tolerable side effects. To determine the treatment strategies, each patient's preference was given priority to maximize medication compliance and treatment outcomes (48). The antidepressants switched or combined were bupropion, desvenlafaxine, duloxetine, escitalopram, fluoxetine, mirtazapine, paroxetine, sertraline, venlafaxine, and vortioxetine. Augmented drugs were buspirone, lithium, triiodothyronine, and atypical antipsychotics, including aripiprazole, risperidone, olanzapine, quetiapine, and ziprasidone.
Remission was defined as HAMD score ≤ 7. The main outcome measures were remission at 12 weeks and at 12 months.
Between-group comparisons of baseline sociodemographic, clinical, and treatment-related characteristics according to the presence of any childhood abuse were analyzed using the t-test or χ2 test, as appropriate. The same comparisons were repeated between groups with lower social support vs. higher social support. Considering these associations and collinearity between the variables, covariates were considered in later adjusted analyses. The individual associations of childhood abuse and social support groups with the 12-week and 12-month remission status were analyzed in logistic regression models before and after adjusting for potential covariates. Interactive effects of childhood abuse and social support on the 12-week and 12-month remission status were analyzed using multinomial logistic regression tests after adjustment for potential covariates. All statistical tests were two-sided with p < 0.05 taken to indicate statistical significance. Statistical analyses were performed using IBM SPSS Statistics (version 25; IBM, Chicago, IL).
Patient recruitment and flow are described in Figure 1. Of 1,262 patients evaluated at baseline, 1,246 (98.7%) were followed up at least once during the 12-week acute treatment phase, and comprised the sample analyzed for acute treatment outcomes. There were no significant differences in any baseline characteristic between the 1,246 patients included and 16 remaining patients (all p > 0.6).
After the acute treatment phase, 1,015 (81.5%) were followed up at least once during the treatment period, and comprised the sample analyzed for continuation treatment outcome. Attrition at 12 months was significantly associated with unemployed status and higher EQ-5D scores at baseline.
Characteristics were compared by presence of any childhood abuse in Table 1, which was significantly associated with younger age, male sex, higher education, unmarried status, no religion, and low monthly income. With regard to depression characteristics, the presence of childhood abuse was significantly associated with atypical features, early onset, longer duration of illness, greater number of depressive episodes, longer duration of present episode, family history of depression, and concurrent physical disorders. In addition, the presence of childhood abuse was significantly associated with higher baseline scores on HADS-A, LES, PSS, and AUDIT, and lower scores on both CDRS and MSPSS. There were significant group-related differences in treatment steps after 12 weeks. Characteristics were compared again according to the social support level using MSPSS (Supplementary Table S1). Lower social support was significantly associated with unmarried status, no religion, unemployed status, diagnosis of MDD, earlier age at onset, longer duration of illness, greater number of depressive episodes, longer duration of present episode, higher scores on HADS-D, HADS-A, and PSS, and lower scores on both SOFAS and CDRS. Considering these associations and collinearity between the variables, the following covariates were selected for further adjusted analyses: age, sex, atypical features, number of depressive episodes, duration of present episode, family history of depression, HADS-A, LES, and AUDIT scores, and treatment step.
Remission up to 12 weeks and up to 12 months were observed in 43.3 and 70.4% of cases, respectively. The individual associations of history of childhood abuse and social support group with the 12-week and 12-month remission status are shown in Table 2. All types of childhood abuse showed no association with acute 12-week remission in both unadjusted and adjusted analyses. However, all types of childhood abuse showed associations with long-term 12-month remission before and after adjustment. Higher social support was significantly associated with acute 12-week remission in unadjusted analyses, but this association lost significance after adjustment. There were no significant associations between social support and long-term 12-month remission in both unadjusted and adjusted analyses.
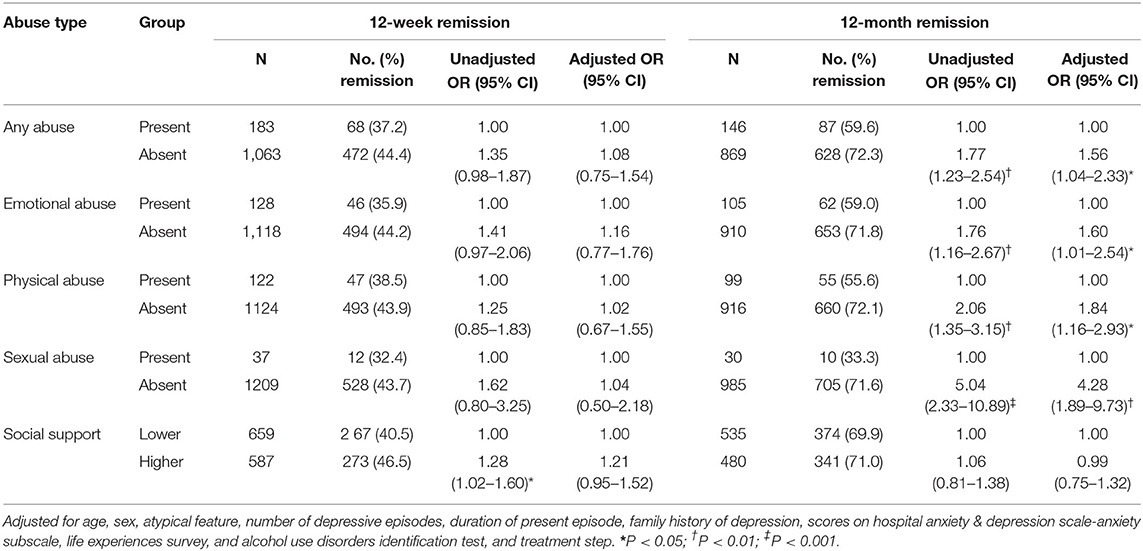
Table 2. Individual associations of reported childhood abuse and social support levels with remissions on 12-week and 12-month.
The interactive effects of history of childhood abuse and social support levels on the 12-week remission status are shown in Figure 2. No significant interactive associations were found between each childhood abuse type and social support levels on the acute 12-week remission rate. Figure 3 shows the interactive effects of history of childhood abuse and social support levels on the 12-month remission status. Presence of both a history of child abuse and low level of social support was associated with the lowest long-term 12-month remission rates. Of these associations, interaction terms between any child abuse, emotional abuse, and physical abuse and baseline social support on remission rate were significant (p = 0.020, 0.009, and 0.023, respectively). However, no significant interactions were found with sexual abuse (p = 0.301).
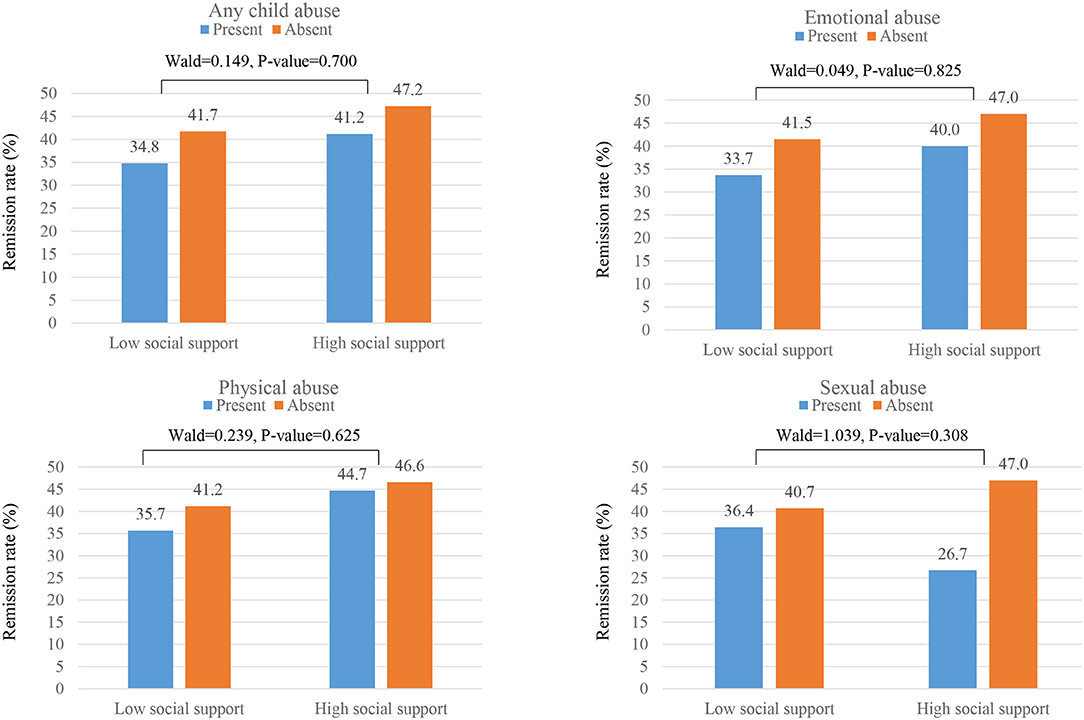
Figure 2. Interactive effects of childhood abuse and social support levels on 12-week remission rates. Interaction terms (Wald and P-value statistics) were calculated after adjustment for age, sex, atypical feature, number of depressive episodes, duration of present episode, family history of depression, scores on Hospital Anxiety & Depression Scale-anxiety subscale, Life experiences survey, and alcohol use disorders identification test, and treatment step.
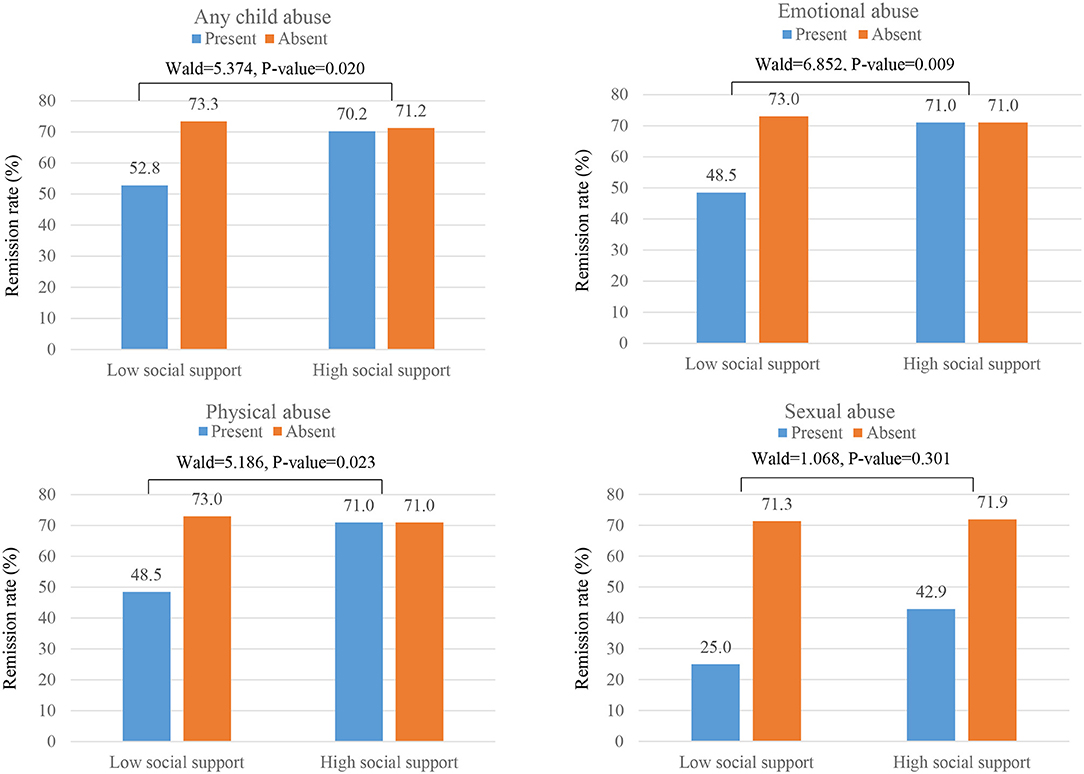
Figure 3. Interactive effects of childhood abuse and social support levels on 12-month remission rates. Interaction terms (Wald and P-value statistics) were calculated after adjustment for age, sex, atypical feature, number of depressive episodes, duration of present episode, family history of depression, scores on Hospital Anxiety & Depression Scale-anxiety subscale, Life experiences survey, and alcohol use disorders identification test, and treatment step.
The principal findings of this study were that childhood abuse before the age of 16 is associated with poorer 12-month long-term pharmacological treatment outcomes in patients with depressive disorders, but not in the 12-week acute treatment phase in adulthood. Furthermore, in analyzing the effects of the interaction of each type of childhood abuse and the level of social support on remission, we found interactive effects of history of childhood abuse and social support level on the long-term 12-month remission status. However, no interaction effect was found with sexual abuse.
This study included a sample of outpatients with depressive disorder from a naturalistic prospective pharmacological treatment protocol. Our findings were broadly inconsistent with previous studies reporting the association between childhood adversity and lack of remission in short-term (12 weeks) treatment (6). However, two studies of 12-month treatment outcomes showed that childhood abuse was associated with non-remission after a medication trial (49, 50) which was consistent with our 12-month results. As the present study is the first long-term study assessing both acute and late phases to report changes in the predictive value of child abuse for pharmacological treatment, our findings could provide a more integrated and expanded understanding in the context of previous research. Some studies exploring time to remission within several weeks indicated that there were differences in remission rates over time, and that childhood abuse was associated with longer time to remission across treatments (51, 52). From these findings, we can make assumptions about other mediators that impact the response to drug response in depressed patients with childhood abuse in the long-term rather than the short-term. A cross-sectional study to evaluate the 1-year outcome of depression during pharmacotherapy reported that coping with interpersonal stress rather than history of abuse was a significant long-term (1 year later) predictor of remission (49). Interpersonal events and their responses are factors that could change in the long-term along with responses to medications, and we speculate that they may have influenced long-term remission rather than acute remission via interaction with child abuse.
This speculation is an observation in the present study, which showed there was a significant interaction between perceived social support and childhood abuse and effects on remission of depression. With regard to treatment outcome, this is the first study to identify social support as a mediator of the association between childhood abuse and pharmacological outcome in the long-term. There are several possible explanations for the significant interactive effects of social support during drug therapy. First, it is possible that social support serves as an active coping strategy during pharmacological treatment (53). Perceived social support in contrast to received social support, defined as the actual provision of support, is the cognitive evaluation of being connected to others and knowing that support is available (54). Individual differences in cognitive processing of the abusive experience rather than the abuse itself may predict later psychological adjustment (54). This perceived social support can also be viewed as a coping strategy involving the effective use of a social support system, such as sharing feelings with family and friends and of talking to others about one's problems (55). The coping strategy regarding effective use of a social support system would involve sufficient communication between patients and healthcare providers and actively seeking change during drug therapy, and may be specifically associated with positive treatment outcome. Second, social support may confer resilience to chronic stress, such as child abuse, by modifying the physiological status, which may be associated with antidepressant treatment response. There is an emerging literature linking social support and neurobiological pathways, including cardiovascular, neuroendocrine, and immune systems (20). In particular, evidence for a gene–environment interaction involving social support suggested that social support may confer resilience to stress by moderating serotonin transporter (5-HTT) gene expression in maltreated children (56). Childhood abuse may increase the risk of depressive disorder through alteration of the HPA axis and CRF circuits in the brain (57). An animal study suggested that early life adversity and serotonin transporter gene variation interacted at the level of the adrenal gland to affect the adult HPA axis (58). Our findings suggest that social support may modify serotonin function, which enhances antidepressant response by affecting the regulation of HPA dysfunction due to early childhood adversity. Based on these results, we assume that social support during drug therapy modulates the risk of a history of child abuse by affecting coping strategies or neurobiological changes in the long-term rather than acute phase. These coping modalities and physiological changes via social support could be expected over a long-term of several months rather than short-term.
However, we found no interactive effects of sexual abuse and social support level on the long-term 12-month remission status. Childhood abuse may be one decisive source of heterogeneity that may also depend on trauma type (59). Some studies have suggested that specific types of abuse rather than a general history of trauma moderate pharmacological treatment response (60). Specifically, a previous study suggested that the buffering effect of social support on depression appeared to be diminished with increasing severity or complexity of maltreatment history (61). Child sexual abuse often co-occurs within the context of other types of family dysfunction, social deprivation, and physical and emotional abuse (62, 63). Considering the interaction between these additional stressors, the apparent association between child sexual abuse and adult depression is complex (63, 64). The findings of the present study suggest that the experience of sexual abuse may overpower the buffering effect of social support typically perceived, even during pharmacotherapy. Several studies have suggested that neurobiological consequences in adults who have experienced child sexual abuse are distinct from those of other types of abuse. A study of the HPA axis indicated that only sexual abuse during childhood, but not other types of child abuse, was correlated with cortisol dysfunction in pharmacological challenge tests in adults with posttraumatic stress disorder (65). Adults who had experienced childhood sexual abuse were shown to have cortical thinning, especially in regions of the primary somatosensory cortex, whereas adults who had experienced emotional abuse showed cortical thinning in regions of self-evaluation (66). These specific neurobiological consequences of childhood sexual abuse may have influenced the pharmacological response in a manner distinct from other types of child abuse by interacting with social support. Our findings suggest that appropriate social support interventions during medication for depressed patients with a history of sexual abuse cannot be expected to have a positive impact on the pharmacological outcomes. On the other hand, the findings of the present study bolster the idea that specific types of social support could exhibit effects on depression according to the type of child abuse. Previous research showed that actual parental support, but not cognitive appraisals or coping strategies, was predictive of resilience in victims of sexual abuse (67). That is, our findings suggest that perceived social support may not be beneficial in relation to the type of sexual abuse during medication for depression. Instead, patients with a history of sexual abuse may have better treatment outcomes by the provision of actual social support rather than facilitating cognitive appraisals about subjective social support. Therefore, research on whether such actual social support may have an impact on remission in depressed patients with a history of sexual abuse is required. In addition, special attention has been paid to ensuring the identification and provision of different types and sources of social support.
In addition, our findings agree with those of previous studies indicating that childhood abuse is associated with a pernicious course of depression, including early onset and greater number and persistence of depressive episodes (68, 69). In this study, no individual associations of social support level with the 12-week and 12-month remission status were found after adjusting for covariates. There are conflicting reports in the literature on the influence of social support on various health outcomes. Some researchers suggested that social support has a direct protective effect against depression (70), whereas others suggested that social support indirectly influences depression outcome via coping, communication, and self-esteem (71, 72). Our findings support the indirect effects of social support on treatment outcome in depressive patients. Future research should examine further the mechanisms affecting treatment outcomes during pharmacotherapy through social support and its relationship to childhood abuse.
The strengths of this study were that the sample size was larger and the follow-up period was longer than previous studies on this issue, and a range of covariates were considered in the analysis. However, this study had several limitations. First, as depressed patients in this study reported childhood abuse retrospectively, this information was vulnerable to the effects of recall and mood. In addition, the relatively small number of subjects with a history of sexual abuse compared to other types of childhood abuse may have underpowered the significant interactions with social support on remission status. However, several recent studies have found retrospective reports to be consistent with prospective designs (73, 74), and depressed individuals' reports of childhood abuse are stable despite changes in clinical state (75, 76). Second, follow-up rates for long-term treatment were relatively low compared with those for the acute treatment phase. Previous studies suggested that subjects with a history of childhood adversity are also more likely to drop out of treatment (77). Therefore, it is necessary to investigate the differences between types of child abuse among individuals who dropped out in the early phase and those of participants who remained until long-term follow-up. Third, as this study had a naturalistic design, treatment was decided by patient preference under physician's guidance rather than by a determined protocol; therefore, interphysician variability may have influenced the outcomes. Fourth, we did not assess the specific period associated with childhood abuse. Some studies suggested that specific periods (e.g., pre-pubertal age) of sensitivity to child abuse distinctly moderate the later response to pharmacotherapy (78). More work in the timing of childhood abuse and associated treatment outcomes is warranted.
In conclusion, we found that a history of child abuse predicted poorer pharmacological treatment response in depressed patients in the long-term. This study also indicated interactive effects of a history of childhood abuse and social support level on the long-term 12-month remission status. Notably, the level of social support showed no interactive effect with sexual abuse on the long-term treatment response to antidepressant medication. Our findings highlight the importance of early preventive and therapeutic interventions, and of obtaining information about childhood abuse in routine clinical assessments of adult patients with depression, to identify individuals at high risk of poor response to treatment with antidepressant medications.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Commission of the Chonnam National University Hospital Institutional Review Board (CNUH 2012-014). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
J-MK and RS were involved in the conception and design of the study and responsible for the acquisition of data. J-MK, RS, and J-YL were involved in the analysis and interpretation of data and performed the statistical analysis. J-MK and J-YL drafted the manuscript. H-JK, S-WK, and I-SS revised the manuscript critically for important intellectual content. H-JK, J-WK, and MJ contributed to administrative, technical, or material support. S-WK and I-SS supervised the study. All authors read and approved the final paper.
The study was funded by a grant of National Research Foundation of Korea Grant [NRF-2019M3C7A1031345] to J-MK. RS is part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London, and from the National Institute for Health Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust. RS is also a National Institute for Health Research (NIHR) Senior Investigator.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.803639/full#supplementary-material
1. MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, et al. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. (2001) 158:1878–83. doi: 10.1176/appi.ajp.158.11.1878
2. Mandelli L, Petrelli C, Serretti A. Tildhood trauma and adult depression. Eur Psychiatry. (2015) 30:665–80. doi: 10.1016/j.eurpsy.2015.04.007
3. Klein DN, Kotov R. Course of depression in a 10-year prospective study: evidence for qualitatively distinct subgroups. J Abnorm Psychol. (2016) 125:337–48. doi: 10.1037/abn0000147
4. Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky A. et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. (2010) 67:113–23. doi: 10.1001/archgenpsychiatry.2009.186
5. Infurna MR, Reichl C, Parzer P, Schimmenti A, Bifulco A, Kaess M. Associations between depression and specific childhood experiences of abuse and neglect: a meta-analysis. J Affect Disord. (2016) 190:47–55. doi: 10.1016/j.jad.2015.09.006
6. Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. (2012) 169:141–51. doi: 10.1176/appi.ajp.2011.11020335
7. Asarnow JR, Emslie G, Clarke G, Wagner KD, Spirito A, Vitiello B, et al. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: predictors and moderators of treatment response. J Am Acad Child Adolesc Psychiatry. (2009) 48:330–9. doi: 10.1097/CHI.Ob013e3181977476
8. Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW, Silva SG, et al. Impact of childhood trauma on treatment outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. (2010) 49:132–40. doi: 10.1016/j.jaac.2009.10.007
9. Johnstone JM, Luty SE, Carter JD, Mulder RT, Frampton CM, Joyce PR. Childhood neglect and abuse as predictors of antidepressant response in adult depression. Depress Anxiety. (2009) 26:711–7. doi: 10.1002/da.20590
10. Li ET, Luyten P, Midgley N. Psychological mediators of the association between childhood emotional abuse and depression: a systematic review. Front Psychiatry. (2020) 11:559213. doi: 10.3389/fpsyt.2020.559213
11. Carlson EB, Dalenberg C, Armstrong J, Daniels JW, Loewenstien R, Roth D. Multivariate prediction of posttraumatic symptoms in psychiatric inpatients. J Trauma Stress. (2001) 14:549–67. doi: 10.1023/A:1011164707774
12. Vranceanu A, Hobfoll S, Johnson RJ. Child multi-type maltreatment and associated depression and PTSD symptoms: the role of social support and stress. Child Abuse Negl. (2007) 31:71–84. doi: 10.1016/j.chiabu.2006.04.010
13. Brinker J, Cheruvu VK. Social and emotional support as a protective factor against current depression among individuals with adverse childhood experiences. Prev Med Rep. (2016) 5:127–33. doi: 10.1016/j.pmedr.2016.11.018
14. Cheong EV, Sinnott C, Dahly D, Kearney PM. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open. (2017) 7:e013228. doi: 10.1136/bmjopen-2016-013228
15. Kealy D, Rice SM, Cox DW. Childhood adversity and depressive symptoms among young adults: examining the roles of individuation difficulties and perceived social support. Early Interv Psychiatry. (2020) 14:241–6. doi: 10.1111/eip.12894
16. Evans SE, Steel AL, DiLillo D. Child maltreatment severity and adult trauma symptoms: does perceived social support play a buffering role? Child Abuse Negl. (2013) 37:934–43. doi: 10.1016/j.chiabu.2013.03.005
17. Yang J, Yao S, Zhu X. The impact of stress on depressive symptoms is moderated by social support in Chinese adolescents with subthreshold depression: a multi-wave longitudinal study. J Affect Disord. (2010) 127:113–21. doi: 10.1016/j.jad.2010.04.023
18. Wichers MC, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, et al. Evidence that moment-to-moment variation in positive emotions buffer genetic risk for depression: a momentary assessment twin study. Acta Psychiatr Scand. (2007) 115:451–7. doi: 10.1111/j.1600-0447.2006.00924.x
19. Sperry DM, Widom CS. Child abuse and neglect, social support, and psychopathology in adulthood: a prospective investigation. Child Abuse Negl. (2013) 37:415–25. doi: 10.1016/j.chiabu.2013.02.006
20. Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. (2006) 29:377–87. doi: 10.1007/s10865-006-9056-5
21. Kang HJ, Kim JW, Kim SY, Kim SW, Shin HY, Shin MG. et al. The make biomarker discovery for enhancing antidepressant treatment effect and response (Make Better) study: design and methodology. Psychiatry Investig. (2018) 15:538–45. doi: 10.30773/pi.2017.10.2
22. Kim JM, Stewart R, Kang HJ, Kim JW, Lee HJ, Jhon M, et al. Predictors of relapse following a stepwise psychopharmacotherapy regime in patients with depressive disorders. J Affect Disord. (2021) 293:109–16. doi: 10.1016/j.jad.2021.06.015
23. Sheehan DV. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59:22–33.
24. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Press. (1994).
25. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. (1960) 23:56–62. doi: 10.1136/jnnp.23.1.56
26. de Graaf R, Bijl RV, Ravelli A, Smit F, Vollebergh WAM. Predictors of first incidence of DSM-III-R psychiatric disorders in the general population: findings from the netherlands mental health survey and incidence study. Acta Psychiatr Scand. (2002) 106:303–13. doi: 10.1034/j.1600-0447.2002.01397.x
27. Björkenstam E, Hjern A, Vinnerljung B. Adverse childhood experiences and disability pension in early midlife: results from a Swedish National Cohort Study. Eur J Public Health. (2017) 27:472–7. doi: 10.1093/eurpub/ckw233
28. Hovens JG, Wiersma JE, Giltay EJ, van Oppen P, Spinhoven P, Penninx BW, et al. Childhood life events and childhood trauma in adult patients with depressive, anxiety and comorbid disorders vs. controls. Acta Psychiatr Scand. (2010) 122:66–74. doi: 10.1111/j.1600-0447.2009.01491.x
29. Abbey A, Abramis DJ, Caplan RD. The effects of different sources of social support and interpersonal conflict on emotional well-being. Basic Appl Soc Psych. (1985) 6:111–29. doi: 10.1207/s15324834basp0602_2
30. Park H, Nguyen T, Park H. Validation of multidimensional scale of perceived social support in middle-aged Korean women with diabetes. Asia Pac J Soc Work Dev. (2012) 22:202–13. doi: 10.1080/02185385.2012.691719
31. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
32. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol group. Ann Med. (2001) 33:337–43. doi: 10.3109/07853890109002087
33. Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the life experiences survey. J Consult Clin Psychol. (1978) 46:932–46. doi: 10.1037/0022-006X.46.5.932
34. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
35. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
36. Saunders JB, Aasland OG, Babor TF. de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction. (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
37. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: a comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. (1999) 38:289–96.
38. Lee YK, Nam HS, Chuang LH, Kim KY, Yang HK, Kwon IS, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. (2009) 12:1187–93. doi: 10.1111/j.1524-4733.2009.00579.x
39. Lee JY, Cho MJ, Kwon JS. Global assessment of functioning scale and social and occupational functioning scale. Korean J Psychopharmacol. (2006) 17:122–7.
40. Lee J, Shin C, Ko YH, Lim J, Joe SH, Kim S, et al. The reliability and validity studies of the korean version of the perceived stress scale. Korean J Psychosom Med. (2012) 20:127–34.
41. Baek HS, Lee KU, Joo EJ, Lee MY, Choi KS. Reliability and validity of the korean version of the connor-davidson resilience scale. Psychiatry Investig. (2010) 7:109–15. doi: 10.4306/pi.2010.7.2.109
42. Lee BO, Lee CH, Lee PG, Choi MJ, Namkoong K. Development of Korean version of Alcohol Use Disorders Identification Test (AUDIT-K): Its reliability and validity. J Korean Academy of Addiction Psychiatry. (2000) 4:83–92.
43. Kim JM, Stewart R, Kang HJ, Kim JW, Lee HJ, Jhon M, et al. Short and long-term treatment outcomes of stepwise psychopharmacotherapy based on early clinical decision in patients with depressive disorders. J Affect Disord. (2020) 274:315–25. doi: 10.1016/j.jad.2020.05.002
44. Anderson IM, Ferrier IN, Baldwin RC, Cowen PJ, Howard L, Lewis G, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2000 british association for psychopharmacology guidelines. J Psychopharmacol. (2008) 22:343–96. doi: 10.1177/0269881107088441
45. Bauer M, Pfennig A, Severus E, Whybrow PC, Angst J, Möller HJ. World federation of societies of biological psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry. (2013) 14:334–85. doi: 10.3109/15622975.2013.804195
46. Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 3. Pharmacol Treatm Can J Psychiatry. (2016) 61:540–60. doi: 10.1177/0706743716659417
47. Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand college of psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. (2015) 49:1087–206. doi: 10.1177/0004867415617657
48. Swift JK, Callahan JL. The impact of client treatment preferences on outcome: a meta-analysis. J Clin Psychol. (2009) 65:368–81. doi: 10.1002/jclp.20553
49. Enns MW, Cox BJ. Psychosocial and clinical predictors of symptom persistence vs remission in major depressive disorder. Can J Psychiatry. (2005) 50:769–77. doi: 10.1177/070674370505001206
50. Yrondi A, Aouizerate B, Bennabi D, Richieri R, D'Amato T, Bellivier F, et al. Childhood maltreatment and clinical severity of treatment-resistant depression in a French cohort of outpatients (FACE-DR): one-year follow-up. Depress Anxiety. (2020) 37:365–74. doi: 10.1002/da.22997
51. Klein DN, Arnow BA, Barkin JL, Dowling F, Kocsis JH, Leon AC., et al. Early adversity in chronic depression: clinical correlates and response to pharmacotherapy. Depress Anxiety. (2009) 26:701–10. doi: 10.1002/da.20577
52. Miniati M, Rucci P, Benvenuti A, Frank E, Buttenfield J, Giorgi G, et al. Clinical characteristics and treatment outcome of depression in patients with and without a history of emotional and physical abuse. J Psychiatr Res. (2010) 44:302–9. doi: 10.1016/j.jpsychires.2009.09.008
53. Moos RH, Schaefer JA. Coping resources and processes: current concepts and measures. In: Goldberger A, Breznitz S, editors. Handbook of Stress. Second. New York, NY: The Free Press. (1993). p. 234–57.
54. Cullen FT. Social support as an organizing concept for criminology: presidential address to the academy of criminal justice sciences. Justice Q. (1994) 11:527–59. doi: 10.1080/07418829400092421
55. Runtz MG, Schallow JR. Social support and coping strategies as mediators of adult adjustment following childhood maltreatment. Child Abuse Negl. (1997) 21:211–26. doi: 10.1016/S0145-2134(96)00147-0
56. Kaufman J, Yang BZ, Douglas-Palumberi H, Grasso D, Lipschitz D, Houshyar S, et al. Brain-derived neurotrophic factor–HTTLPR gene interactions and environmental modifiers of depression in children. Biol Psychiatry. (2006) 59:673–80. doi: 10.1016/j.biopsych.2005.10.026
57. Pirnia B, Khosravani V, Maleki F, Kalbasi R, Pirnia K, Malekanmehr P, et al. The role of childhood maltreatment in cortisol in the hypothalamic-pituitary-adrenal (HPA) axis in methamphetamine-dependent individuals with and without depression comorbidity and suicide attempts. J Affect Disord. (2020) 263:274–81. doi: 10.1016/j.jad.2019.11.168
58. van der Doelen RH, Deschamps W, D'Annibale C, Geenen B, Riva MA, Kozicz T, et al. Early life adversity and serotonin transporter gene variation interact at the level of the adrenal gland to affect the adult hypothalamo-pituitary-adrenal axis. Transl Psychiatry. (2014) 4:e409. doi: 10.1038/tp.2014.57
59. Hill J. Developmental perspectives on adult depression. Psychoanal Psychother. (2009) 23:200–12. doi: 10.1080/02668730903227263
60. Shamseddeen W, Asarnow JR, Clarke G, Vitiello B, Wagner KD, Birmaher B, et al. Impact of physical and sexual abuse on treatment response in the Treatment of Resistant Depression in Adolescent Study (TORDIA). J Am Acad Child Adolesc Psychiatry. (2011) 50:293–301. doi: 10.1016/j.jaac.2010.11.019
61. Salazar AM, Keller TE, Courtney ME. Understanding social support's role in the relationship between maltreatment and depression in youth with foster care experience. Child Maltreat. (2011) 16:102–13. doi: 10.1177/1077559511402985
62. Fergusson DM, Horwood LJ, Lynskey MT. Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry. (1996) 35:1365–74. doi: 10.1097/00004583-199610000-00024
63. Mullen PE, King NJ, Tonge BJ. Child sexual abuse: an overview. Behav Change. (2000) 17:2–14. doi: 10.1375/bech.17.1.2
64. Rutter ML. Psychosocial adversity and child psychopathology. Br J Psychiatry. (1999) 174:480–93. doi: 10.1192/bjp.174.6.480
65. Mello MF, Mello AF, Ruiz JE, Fiks JP, Adreoli SB, Bressan RA, et al. The effect of comorbid depression and sexual abuse during childhood on glucocorticoid and mineralocorticoid receptor sensitivity of patients with post-traumatic stress disorder. J Depress Anxiety. (2013) S4:004. doi: 10.4172/2167-1044.S4-004
66. Heim CM, Mayberg HS, Mletzko T, Nemeroff CB, Pruessner JC. Decreased cortical representation of genital somatosensory field after childhood sexual abuse. Am J Psychiatry. (2013) 170:616–23. doi: 10.1176/appi.ajp.2013.12070950
67. Spaccarelli S. Stress, appraisal, and coping in child sexual abuse: a theoretical and empirical review. Psychol Bull. (1994) 116:1–23. doi: 10.1037/0033-2909.116.2.340
68. Comijs HC, van Exel E, van der Mast RC, Paauw A, Oude Voshaar R, Stek ML. Childhood abuse in late-life depression. J Affect Disord. (2013) 147:241–6. doi: 10.1016/j.jad.2012.11.010
69. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. (2017) 210:96–104. doi: 10.1192/bjp.bp.115.180752
70. Praharso NF, Tear MJ, Cruwys T. Stressful life transitions and wellbeing: a comparison of the stress buffering hypothesis and the social identity model of identity change. Psychiatry Res. (2017) 247:265–75. doi: 10.1016/j.psychres.2016.11.039
71. Bámaca-Colbert MY, Tilghman-Osborne EM, Calderón-López S, Moore AM. Perceptions of support from mothers, fathers, and friends: direct and indirect associations with the psychological adjustment of Mexican-origin girls. J Lat Psychol. (2017) 5:142–56. doi: 10.1037/lat0000070
72. Shen Q, Shi Y, Zhang S, Tsamlag L, Wang H, Chang R, et al. How involuntary subordination and social support influence the association between self-esteem and depression: a moderated mediation model. BMC Psychiatry. (2019) 19:390. doi: 10.1186/s12888-019-2330-1
73. Fergusson DM, Horwood LJ, Boden JM. Structural equation modeling of repeated retrospective reports of childhood maltreatment. Int J Methods Psychiatr Res. (2011) 20:93–104. doi: 10.1002/mpr.337
74. Scott KM, McLaughlin KA, Smith DAR, Ellis PM. Childhood maltreatment and DSM-IV adult mental disorders: Comparison of prospective and retrospective findings. Br J Psychiatry. (2012) 200:469–75. doi: 10.1192/bjp.bp.111.103267
75. Lizardi H, Klein DN. Long term stability of parental representations in depressed outpatients utilizing the Parental Bonding Instrument. J Nerv Ment Dis. (2005) 193:183–8. doi: 10.1097/01.nmd.0000154838.16100.36
76. Wilhelm K, Niven H, Parker G, Hadzi-Pavlovic D. The stability of the Parental Bonding Instrument over a 20-year period. Psychol Med. (2005) 35:387–93. doi: 10.1017/S0033291704003538
77. Waller G. Drop-out and failure to engage in individual outpatient cognitive behavior therapy for bulimic disorders. Int J Eat Disord. (1997). 22:35–41. doi: 10.1002/(SICI)1098-108X(199707)22:1<35::AID-EAT4>3.0.CO;2-3
78. Williams LM, Debattista C, Duchemin AM, Schatzberg AF, Nemeroff CB. Childhood trauma predicts antidepressant response in adults with major depression: data from the randomized international study to predict optimized treatment for depression. Transl Psychiatry. (2016) 6:e799. doi: 10.1038/tp.2016.61
Keywords: depression, childhood abuse, social support, pharmacotherapy, treatment outcome
Citation: Lee J-Y, Stewart R, Kang H-J, Kim J-W, Jhon M, Kim S-W, Shin I-S and Kim J-M (2022) Childhood Abuse, Social Support, and Long-Term Pharmacological Treatment Outcomes in Patients With Depressive Disorders. Front. Psychiatry 13:803639. doi: 10.3389/fpsyt.2022.803639
Received: 28 October 2021; Accepted: 07 January 2022;
Published: 02 February 2022.
Edited by:
Yuan-Pang Wang, University of São Paulo, BrazilReviewed by:
Mariusz Stanisław Wiglusz, Medical University of Gdansk, PolandCopyright © 2022 Lee, Stewart, Kang, Kim, Jhon, Kim, Shin and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jae-Min Kim, am1raW1AY2hvbm5hbS5hYy5rcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.