- 1Department of Experimental Psychology, Utrecht University, Utrecht, Netherlands
- 2Department of Clinical Psychology, Utrecht University, Utrecht, Netherlands
- 3Department of Youth and Family, Utrecht University, Utrecht, Netherlands
- 4Huijs GGZ, Den Bosch, Netherlands
Background: The use of oral contraceptives (OCs) has been associated with increased incidences of anxiety and depression, for which adolescents seem to be particularly vulnerable. Rather than looking at singular outcomes, we examined whether OC use is associated with depressive and anxiety symptom trajectories from early adolescence into early adulthood.
Materials and Methods: Data from 178 girls were drawn from the Research on Adolescent Development and Relationships (RADAR-Y) younger cohort study. We used assessments on 9 waves from age 13 until 24. Developmental trajectories of ratings on the Reynolds Adolescent Depression Scale (RADS-2) and the Screen for Child Anxiety Related Emotional Disorders (SCARED) were compared between never and ever users of OCs.
Results: Never users showed increases in depressive and anxiety symptoms in late adolescence, whereas OC users showed a stable level of symptoms throughout adolescence. This effect remained after adjusting for baseline differences between groups in romantic relationships, sexual debut, educational level, smoking, drinking, and drug use. Age of OC use onset did not significantly predict symptom development.
Conclusions: OC use in adolescence was related to an altered developmental trajectory of internalizing symptoms, in which OC users did not show an increase in depressive and anxiety symptoms in late adolescence, whereas never users did. The question remains whether this altered symptom trajectory can be considered a protective effect of OC use on psychopathology. Additional research is needed to improve our understanding of the long-term consequences of OC use on mental health.
Introduction
The oral contraceptive pill (OC; “the pill”) has been on the market for half a century, is used by about 100 million women world-wide, and is one of the most extensively studied pills in the history of medicine (1, 2). In countries such as the Netherlands, about one in five adolescent girls use OCs to prevent pregnancy, alleviate dysmenorrhea, and/or treat acne (3, 4). Whereas, the physical side effects of OCs have been subject to a considerable amount of research, a surprising lack of knowledge exists about its effects on affect, including effects on affect-related brain function (5–7). Some studies suggest that women taking OCs will not be subjected to adverse emotional changes (8, 9), or might even experience a protective effect on their mental health (10–14). However, in recent large observational studies OC use has been associated with higher depressive symptoms (15–17), use of antidepressants (17, 18), and an increased risk of suicide (19). Evidence regarding OCs and anxiety has been limited, with some studies showing that OC use is associated with the onset of anxiety symptoms (20, 21), and lower efficacy of exposure-based therapy (22, 23).
The mixed findings have raised doubts about whether the association of OC use with mood deterioration is due to hormonal disruption. The OC pill contains synthetic versions of the hormones estradiol (E) and progesterone (P) and suppresses natural gonadal hormone production (2). Since natural fluctuations of E and P have been associated with emotion regulatory functioning and mood, OC use may result in emotion dysregulation and internalizing symptoms (6). On the other hand, the different outcomes could merely result from existing and unmeasured group differences between OC users and non-users that make OC users inherently more at risk of psychopathology beyond any influence of OC hormones (24). For instance, behavioral and social factors, such as earlier sexual debut, age at menarche, and smoking, have been identified as confounders for both OC use and depression (8, 25, 26).
Additionally, the conflicting evidence may be especially prominent in studies of only adult OC users, as studies including information on adolescent OC use find adolescents to be particularly vulnerable to developing mood symptoms and disorders after OC use (15–17, 27). This finding may be explained by the absence of the survivor bias effect in first time adolescent OC users compared to adult women with possible previous OC experiences. Then again, adolescent OC users may also be more susceptible to the change in hormonal milieu after starting OCs. Adolescence is considered to be a vulnerable period for the development of depression and anxiety disorders (28–30), with girls being twice as likely to experience depressive and anxiety symptoms compared to boys (31, 32). During this developmental period, the gonadal hormones are at the forefront of brain development (33), and hormonal disruptions are therefore likely to affect brain development and mental health in the long run (34). Given that adolescent girls use OCs at an increasingly younger age and for purposes beyond contraception (3), it is important to gain more insight into the effects of OC's on mental health in adolescence.
Whereas depression in adolescents taking OCs has been the focus in some previous longitudinal studies, the effect of adolescent OC use was mostly assessed retrospectively. Therefore, the present study aimed to examine OC's effect on both depression and anxiety symptoms throughout adolescence. Our study also goes beyond prior research by modeling OC effects on the depressive and anxiety symptom trajectories from early adolescence into early adulthood. These symptom trajectories may be more sensitive to OCs effect than assessing clinical diagnoses and differences in singular outcomes. This allows examining the effect of OC use on symptom development over time while taking the naturally fluctuating development of internalizing symptoms into account. Data were used from a longitudinal data set in the Netherlands on adolescent development. Whereas, baseline information before OC onset is often unavailable in prior work, the current dataset allowed us to include measurements on mental health and adolescent developmental markers over the course of several years before and after OC onset. We used this information to a) examine the relationship between OC use and depression and anxiety symptom development throughout adolescence and into early adulthood, b) explore the effect of age of OC onset on these symptom trajectories, and c) identify possible confounders and risk factors in adolescent development of an effect of OC use on internalizing symptoms.
Materials and Methods
Participants and Procedure
Participants were drawn from the ongoing Research on Adolescent Development and Relationships (RADAR-Y) young population cohort study (35). They were recruited in schools in the province of Utrecht and four cities the Netherlands in 2006. After the first assessment, participants we used in the present study were followed up for nine measurement waves up to 2017. At the first assessment, 214 adolescent girls were included with a mean age of 13.01 years (SD = 0.44). Until age 18, measurements were done annually; afterwards (after wave 6) they were done biannually. From this sample only participants were included who provided information on oral contraceptive use. Thirty-five participants had missing data on contraceptive use. Four participants used other forms of hormonal contraceptives (e.g., injection or intrauterine device), of which 3 girls had used OCs prior to the current alternative contraceptive. The final sample consisted of 178 native Dutch girls, with a mean age of 12.99 (SD = 0.43) at Wave 1 and 23.83 (SD = 0.43) at Wave 9. Most participants had a medium or high socioeconomic status (SES) (85.4%).
Measures
Oral Contraceptive Use
Current and past use of OC was determined via self-report at Wave 6 with the question: “which (hormonal) contraceptive do you currently use?” Participants could indicate when the first intake of their current contraceptive occurred [in months and years, which previous (other) contraceptive they had used, and which dates they started and stopped (in months and years)]. No information was available on OC type. Girls who reported no previous or current OC use were defined as never users of OCs. Ever users of OCs were defined as girls who reported to use OCs currently or previously. Follow up analyses used age of OC onset (n = 137), which was determined by age, date of assessment, and date of onset OC use. Early OC users were defined as users with first intake of OCs before the age of 15 and late OC users were defined as starting OC use at age 15 or older. The age of 15 was selected as a cutoff to separate early and middle/late adolescence into groups comparable in size (n = 33 for early users, n = 44 for late users).
Depression
Depressive symptoms were assessed by the Dutch adjusted version of the Reynolds Adolescent Depression Scale, 2nd ed. (RADS-2) (36). The RADS-2 is a self-report measure developed to measure cognitive, motor, somatic and interpersonal depressive symptoms in adolescents. The scale consists of 23 items (the anhedonia subscale was not administered on Waves 2-6) on a 4-point Likert scale ranging from 1 (almost never) to 4 (most of the time), with a minimum score of 23 and maximum score of 92. Items are part of the subscales dysphoric mood, negative self-evaluation, and somatic complaints. In this study, the scale showed good internal consistency across all waves, with a Cronbach's alpha of 0.93. A previous study has shown good psychometric properties for the RADS-2 in adolescents (37).
Anxiety
Anxiety symptoms were assessed with the Screen for Child Anxiety Related Emotional Disorders (SCARED) (38). The SCARED is a self-report instrument designed to measure anxiety symptoms in children and adolescents. The SCARED consists of 38 items scored on a 3-point Likert scale ranging from 1 (almost never) to 3 (often), with a minimum score of 38 and maximum score of 114. The scale assesses the subscales somatic/panic, general anxiety, separation anxiety, social phobia, and school phobia. The internal consistency for the SCARED was good across all waves, with a Cronbach's alpha of 0.93. Multiple previous studies have shown the SCARED has good psychometric properties (38–40).
Covariates
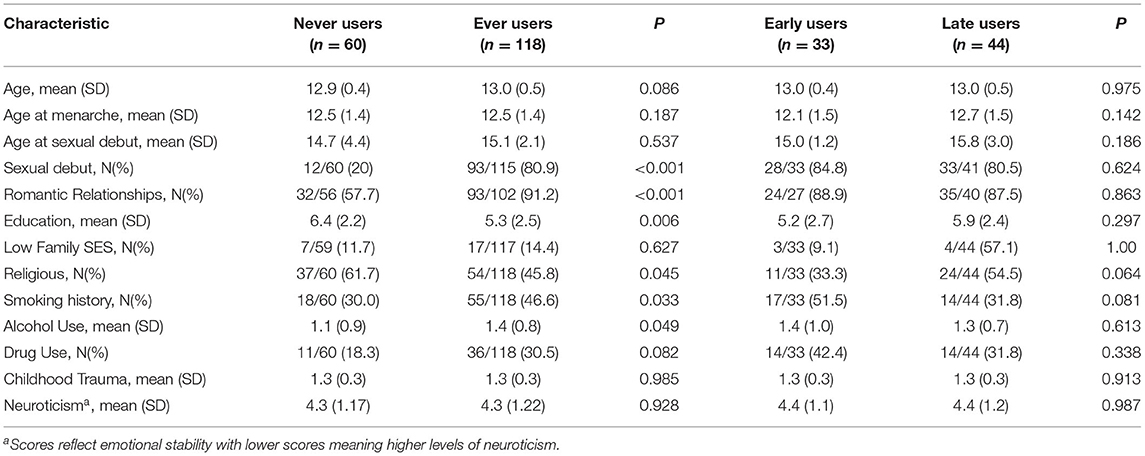
First, covariates were selected if they had previously been associated with OC use and/or internalizing symptoms: age at menarche (25), (age at) sexual debut [yes/no] (25), romantic relationships [yes, no] (41), smoking history [no, yes] (26), religion [not religious, religious] (42), alcohol use [0-5, no alcohol this past month to alcohol every day this month] (43), hard drug use [no, yes] (44), childhood trauma [Childhood Trauma Questionnaire (CTQ)] (45), neuroticism [BIG5] (46), educational level [wave 3] (47), and SES [low, middle/high] (48). Next, the variables that were significantly different between never and ever OC users (or never, early, and late users) were included in the analyses (Table 1). These were sexual debut (p < 0.001), romantic relationships (p < 0.001), education (p = 0.006), religion (p = 0.045), alcohol use (p = 0.049), smoking history (p = 0.033) and drug use (p = 0.082 for never/ever, p = 0.040 for never/early/late).
Analyses
Descriptive statistics were computed for all OC groups (never users, ever users, early users and late users). Growth curve models were used to describe the effect of OC use on the developmental trajectories of both depressive and anxiety symptoms (49). First, a best-fit model was determined that best captured the observed symptom changes in different developmental periods for both depressive and anxiety symptoms. This was done by comparing the chi-square difference (Δχ2) in log likelihood (-2LL) of a one-slope model, two slope model or three slope model with age centered by subtracting 16 from the original values (to compare slopes for early and late adolescence). The one-slope model assumed a linear relationship between age and anxiety or depressive symptoms, where the two-slope model fitted two slopes before and after age 16. The three-slope model plotted one slope for early adolescence (<14 years), one slope for middle to late adolescence (14–18 years), and one slope for young adulthood (> 18 years). The best fitting model used two age slopes to model the development of symptoms from age 13–24.
The final growth curve model assessed within-subject variation using a random intercept and the two age slopes. In the crude models, between-subject variation was modeled by fixed effects for OC use [never/ever]. The age slopes and two-way interaction effects of OC use and both slopes were included to estimate whether the course of depressive and anxiety symptoms differed according to OC use. The adjusted models included the covariates romantic relationships, sexual debut, educational level, religion, alcohol use, drug use, and smoking history as fixed effects. This resulted in two crude and two adjusted models for OC use effects on depressive and anxiety symptoms, respectively. All growth curve analyses were performed using PROC MIXED in SAS 9.4 (SAS Inc, Cary, NC).
Follow-up analyses grouped OC use as never, early (<15 years), or late (≥ 15 years) users to examine the effect of age of OC onset on mood development. Additionally, sensitivity analyses were conducted by restructuring the data using age of OC onset in a 2-slope model, setting the slopes to before and after OC onset (slopes before and after the mean age of OC onset for never users). Modeling the effect of OC use based on age of OC onset rather than centered age resulted in similar main results (see Supplementary Table 1 and Supplementary Figure 1). The main growth curve models that used age to model depressive and anxiety symptoms had more power than models using OC onset, because 41 participants had missing data for date of OC onset.
Results
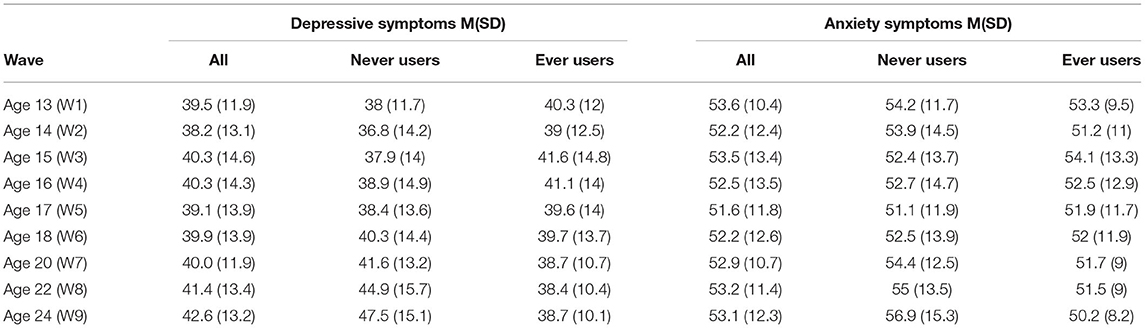
Of the total sample of 178 girls, 60 reported they have never used hormonal contraceptives before and 118 reported they have used OCs. Of the OC users, 6 girls were not currently using OCs but had used them in the past, and the other 112 were currently using OCs. For 77 girls, the age of OC use onset could be determined; the other 41 girls had missing data for date of OC onset. The mean age of OC onset was 14.9 (SD = 1.6). Of the OC users, 33 were considered early users and 44 considered late users. Table 1 displays the descriptive statistics for never and ever users of OC and for early and late users. OC users were more likely to have had romantic relationships and their sexual debut. Additionally, OC users had a lower level of education, and were more likely to have smoked, have drunk alcohol and be non-religious compared to never users. In Supplementary Table 2 the correlations between the descriptive characteristics and internalizing symptoms are listed. Table 2 describes the means and standard deviations of depressive and anxiety symptoms of the final sample at each wave. Supplementary Table 3 lists the correlations between anxiety and depression for each wave.
Anxiety and Depressive Symptom Trajectories
The best fit model that was used to determine the effect of OC use on symptom development throughout adolescence modeled symptom trajectories over two slopes before and after 16 years for both depression [χ2(6) = 875.9, AIC = 9997.2, BIC = 10020.7] and anxiety [χ2(6) = 846.9, AIC = 9010.2, BIC = 9033.7]. For the depressive symptoms, there was no significant main effect of slope 1 (ß = 0.02, p = 0.0.947). For the whole sample, depressive symptoms significantly increased in late adolescence (ß = 0.38, p = 0.027).
The development of anxiety symptoms in adolescence did not show significant main effects of slopes. Anxiety symptoms remained stable in early (ß = −0.43, p = 0.147) and late adolescence (ß = 0.08, p = 0.613).
OC Use and Anxiety and Depressive Symptoms
The trajectories over time for depression and anxiety are shown in Figure 1. Table 3 shows the model fit, standardized regression coefficients and standard errors of the models. Depressive symptoms showed an overall increase in late adolescence with a significant main effect of slope 2 (p = 0.003). There was a significant interaction effect of slope 2 and OC use (p < 0.001): never users of OC showed an increase in depressive symptoms in late adolescence, whereas OC users showed a stable trajectory of depressive symptoms throughout adolescence and young adulthood. The model adjusted for covariates showed similar results, with a significant main effect of age slope 2 (p = 0.001) and a significant interaction effect of age slope 2 and OC use (p < 0.001), indicating a general increase in depressive symptoms in late adolescence for girls and women who have never used OCs.
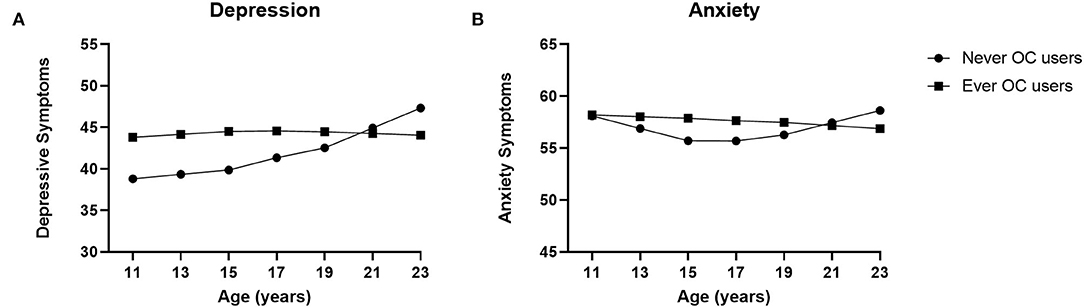
Figure 1. Oral Contraceptive (OC) use and anxiety and depression modeled symptom trajectories. Growth curve models for the depressive and anxiety symptoms for never users of oral contraceptives (OCs) and ever users of OCs. (A) In late adolescence depression scores increased significantly for never users, whereas OC users showed stable depression scores throughout adolescence. (B) An increase in anxiety symptoms toward late adolescence was significant only for never users of OCs, with stable levels of anxiety symptoms for OC users. Means are adjusted for romantic relationships, sexual debut, education level, religion, smoking history, alcohol use, and drug use.

Table 3. Model fit, standardized regression coefficients and standard errors of fixed and random effects as predictors of development of depressive and anxiety symptoms with never and ever users of oral contraceptives.
In the crude model for anxiety symptoms, only the interaction effect between slope 2 and OC use was significant (p = 0.023). Again, an increase toward the end of adolescence and young adulthood was seen only for never users of OCs (Table 2). OC users showed a slight decrease of anxiety symptoms in late adolescence. Adjusting for the covariates showed similar results, with a significant interaction effect of age slope 2 and OC use (p = 0.020).
Age of OC Use and Anxiety and Depressive Symptoms
Grouping OC use into early and late users resulted in the developmental courses depicted in Figure 2 (see Supplementary Table 4 for model fit, standardized regression coefficients and standard errors of the models). For depressive symptoms, results only showed a significant interaction between age slope 2 and OC use (p < 0.001). An increase in depressive symptoms was shown for never users of OCs in late adolescence (> 16 years). Late pill users showed a stable trajectory throughout adolescence and early pill users showed a decrease in depressive symptoms after the age of 16. This effect remained after full adjustment for all covariates (p < 0.001).
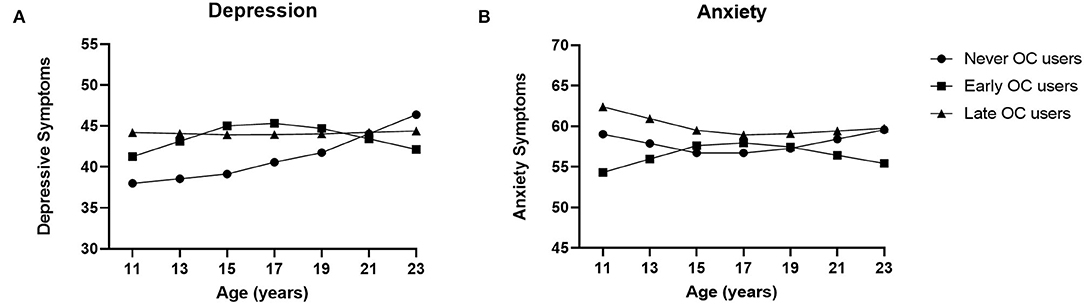
Figure 2. Oral Contraceptive (OC) use, age of onset, and anxiety and depression modeled symptom trajectories. Growth curve models for the depressive and anxiety symptoms for never, early (<15 years), and late (≥15 years) users of oral contraceptives (OCs). (A) Never users increased significantly in depressive symptoms in late adolescence, whereas late pill users had a stable trajectory throughout adolescence and early pill users decreased in symptoms after age 16. (B) Never, early and late OC users did not show significantly different anxiety symptom trajectories in adolescence. Means are adjusted for sexual debut, romantic relationships, education level, religion, smoking history, alcohol use, and drug use.
The growth model for anxiety did not show significant effects of age or OC use, the interaction effect of age slope 2 and OC use had a p-value of 0.112. Adjusting for covariates resulted in the same non-significant interaction effect of age slope 2 and OC use (p = 0.099).
Sensitivity Analyses
The sensitivity analysis using a 2-slope model before and after OC onset showed similar effects as the main models comparing never and ever users, see Supplementary Table 1 and Supplementary Figure 1. A significant increase in symptoms for never users in late adolescence was seen for both depressive (p = 0.002) and anxiety (p = 0.028) symptoms. When considering age of OC onset, the interaction effects were similar (p = 0.006 for depression, p = 0.086 for anxiety) compared to the models using age to model the slopes. However, in these models the slopes for early and late OC use did not differ from each other (p > 0.05) but only from never users (p < 0.05).
Discussion
This study found an altered symptom trajectory of anxiety and depressive symptoms for OC users in late adolescence. Specifically, OC users showed a stable course of depressive and anxiety symptoms throughout adolescence whereas never users showed an increase of internalizing symptoms in late adolescence. When adjusting the developmental trajectories for baseline differences between groups (romantic relationships, sexual debut, educational level, smoking, drinking, and drug use) the effects of OC use remained significant. Furthermore, comparing development before and after OC use resulted in the same effects. That is, no change in symptom development between groups was found before start of OC use, whereas OC users showed a more stable course after OC onset without the increase in symptoms seen on never OC users. Earlier start of OC use even showed a decrease in depressive symptom development after the age of 16, but this effect disappeared when taking the development before and after OC onset into account.
This apparent “protective” role of OC use on internalizing symptoms has been found previously (8, 10–14, 50). In these studies, women using OCs showed lower prevalence of depressive symptoms (12, 13), Major Depressive Disorder (MDD), Generalized Anxiety Disorder (GAD) and Panic Disorder (PD) (10), and even lower risk of past-year suicide attempts (12) compared to non-users. This could be due to a stabilizing effect of OC use on hormonal fluctuations of E and P throughout the menstrual cycle and its co-occurring stabilization of mood variability (51).
The importance of considering relevant confounders when studying OC side effects is shown by these aforementioned studies. They showed that controlling for confounders (including age, BMI, physical activity, chronic disease, number of sexual partners) rendered results non-significant for the protective effects of OCs on psychopathology (8, 10), most likely because OC use in these studies was associated with increased health-promoting behavior (12). In our study, the stabilizing effect of OC use on internalizing symptoms remained after adjustment for relevant risk factors. However, OC use in our study was associated with increased risk behavior for (mental) health problems. Namely, OC users had a lower educational level, were more likely to have had romantic relationships, their sexual debut, a history of smoking, and were heavier drinkers. These are behaviors that are generally associated with an increased risk of internalizing disorders (26, 43, 44). Our results may therefore better fit with the buffer perspective on risky behavior, which suggests that experimenting with alcohol and drugs may not be detrimental per se but can be part of developmentally normative activities (52–54). Beyond the covariates regarding risky behavior that were included in this study, OC use may function as an overall indicator of a more outgoing and social lifestyle with OC users representing the typically developing teenagers. As interpersonal difficulties are considered correlates and risk factors for internalizing disorders such as depression (55), the increased socialization of OC users could buffer the increased depression and anxiety symptoms in late adolescence seen in non-users. However, if these groups are to be considered inherently and substantially different, with OC users reflecting the more normative developing adolescents, it could be expected that the groups showed a significant difference in development before OC onset. This was, however, not the case.
Both our raw and modeled data show an overall increase for depressive symptoms in late adolescence, which is in line with previous studies using the same dataset that have shown an increase in internalizing symptoms in late adolescence for boys and girls (56–58). In the study by Nelemans et al. (57), the results for girls showed a larger intercept and less steep incline in depressive symptoms in late adolescence compared to boys. This would imply a more stable course of symptoms over time in girls, which is possibly an effect of higher baseline levels for girls in general or due to the contribution of OC users. The first inclination would be to interpret the finding of a decrease in internalizing symptoms for OC users in late adolescence as protective. Conversely, the increase in symptoms at the end of adolescence could be considered beneficial and part of developmentally appropriate behavior (59), especially because this increase is seen in both boys and girls (57). Adolescence is a developmental period in which internal changes and external challenges result in higher turmoil than in either childhood or adulthood (60). This significant transition period requires adolescents to adapt to the developmental tasks of that period and provides an opportunity to attain psychological autonomy in adulthood (61). As such, OC use may prevent adolescents from learning to express a range of emotions and developing adequate coping strategies.
Our finding that earlier age of OC onset in adolescence strengthens the effect of OCs on depressive symptoms builds on previous research showing that considering age of OC onset is essential when studying mood related side effects of OC use (15–17, 27). However, this effect disappeared when group differences were assessed after OC onset rather than according to age. The previous effect may then be explained by duration of use, as earlier OC users automatically became longer OC users. The effect of age of OC onset may also not be of added value in this study as only adolescent OC users were included, but remains an important factor to be considered when studying adult OC users.
Strengths, Limitations and Future Directions
In our study we were able to analyze symptom trajectories as a function of OC use over time, which may give more information about effects on mental health than comparing outcomes at any one given time point. The current dataset entailed extensive information regarding adolescent development, which made it possible to include and correct for relevant characteristics predictive of mental health in those years. The methodological challenges when examining OC use on mental health symptoms include problems such as survivor bias and confounding. Our study included information on previous OC use, so we were able to include ever users rather than just current users. Additionally, we were able to correct for most known confounders for both internalizing symptoms and OC use after which the effects remained significant.
Nevertheless, methodological limitations of epidemiological studies like this one are that confounding by unmeasured variables remains a possibility and causality cannot be inferred. For example, our data did not have information on premenstrual symptoms (PMS) or non-contraceptive reasons for using OCs such as acne reduction. The potential protective effect of OCs on mental health may be due to the reduction of hormonal fluctuations, so the positive effects of OC use may be reserved for women who suffer from the hormonal fluctuations of the menstrual cycle and experience a high degree of premenstrual symptoms and related internalizing symptoms that are alleviated by the stabilizing effects of OCs (11). In addition, future research should consider social functioning as a possible buffer in OC users for future psychopathology. Lastly, the contribution of sexual orientation to the increase in internalizing symptoms in never users should be explored. Non-heterosexual girls will be less likely to start OCs and are at increased risk of developing internalizing symptoms in adolescence (62, 63).
It should also be noted that current and past OC use was based on self-report, and was not confirmed by medical reports. Age of onset of OC use could therefore be subject to inaccuracies. Additionally, information on OC use was only assessed at wave 6 when participants were, on average, 18 years old. Participants starting OC use at a later age may have been wrongly classified as “never” users. However, the vast majority of OC users were probably classified correctly at wave 6, because Dutch girls start OC use on average at age 16 (4). Moreover, a wrongful classification would only mean an underestimation of the stabilizing effect seen in OC users. Removing the wrongfully classified OC users from the never user group would also remove the dampening effect seen in OC users from the already increased symptom trajectories seen in never users. In a sensitivity analysis shown in Supplementary Table 5, analyzing only waves 1 through 6 (without 7–9), we found similar results for depression symptoms with significant group differences in late adolescence. Therefore, despite increased differences between groups in standard deviations, the pill effect on depressive symptoms remains apparent in late adolescence. However, the increase in anxiety symptoms in late adolescence for never users rendered insignificant when analyzing only waves 1 through 6. This further showed that the effect of OC use on anxiety symptoms was inconsistent in our sample and depends on the method of analysis (never/ever use, never/early/late use, crude/adjusted, number of waves). Another limitation was the lack of information on type and dose of OC. Considering the different androgenic properties of possible progestins in OCs, different effects on mood are possible and important to consider (7).
After controlling for the aforementioned variables, an effect of OC use on mental health could possibly still be explained by residual confounding by unknown confounders that we could not account for. For example, the confounders could reflect a bigger social buffer effect as mentioned above. At the same time, previous epidemiological studies on OC use and depression have also shown multiple group differences in factors including SES, sexual activity, ethnicity, educational level, BMI, age at menarche, and smoking (8, 15, 16). These recurring group differences point to our sample being representative of the general population.
Our results show the importance of considering age of OC onset when researching mood related effects. However, OC onset data were not available for 41 participants, resulting in more missing data in these analyses compared to the never/ever analyses. Therefore, the results of this analysis have to be interpreted with caution due to lower power and could potentially explain the lack of significant findings with respect to age of OC use onset and anxiety symptom development.
Conclusion
In conclusion, this study underlines the importance of considering OC use in the development of internalizing symptoms from adolescence into adulthood and adds to research showing that OC affects mental health. Our results suggest that OC users show a stable trajectory of anxiety and depressive symptoms throughout adolescence whereas girls who do not use OCs show an increase in internalizing symptoms in late adolescence, even after adjusting for confounders. The stabilizing trajectory in OC users is surprising given that OC users reported more health risk behaviors, but it may reflect a group of typically developing girls. The question is whether this altered symptom trajectory in OC users can be considered as a protective effect of OC use on psychopathology and which developmental pattern can be seen as the normative development of internalizing symptoms in adolescent girls. The answer may lie in future studies predicting adaptive outcomes in later life using the separate developmental trajectories of depressive and anxiety symptoms based on OC use. Given the high number of adolescent girls that start OCs in adolescence (3, 4), additional research is needed to improve our understanding of the long-term consequences of OC use on mental health.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found at: https://doi.org/10.17026/dans-zrb-v5wp (For Waves 1-7, data used for this study are available on request to the corresponding author).
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethical Committees of the Utrecht Medical Center and VU University Medical Center, Netherlands, and the Ethical Committee of the Faculty of Social Science of the Utrecht University, Netherlands. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
AD: formal analysis, writing—original draft, and visualization. SB, SN, EM, IE, JB, and WM: conceptualization and writing—review and editing. LG: formal analysis, conceptualization, writing—original draft, and supervision. All authors contributed to the article and approved the submitted version.
Funding
Data of the RADAR (Research on Adolescent Development and Relationships) study were used. RADAR has been financially supported by main grants from the Netherlands Organization for Scientific Research (GB-MAGW 480-03-005 and GB-MAGW 480-08-006), Stichting Achmea Slachtoffer en Samenleving (SASS), the Netherlands Organization for Scientific Research to the Consortium Individual Development (CID; 024.001.003), a grant of the European Research Council (ERC-2017-CoG - 773023 INTRANSITION), and various other grants from the Netherlands Organization for Scientific Research, VU University Amsterdam, and Utrecht University. IE was funded by a Vici innovational research grant (453–15–005) from the Netherlands Organization for Scientific Research. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.799470/full#supplementary-material
References
2. Petitti DB. Clinical practice. Combination estrogen-progestin oral contraceptives. N Engl J Med. (2003) 349:1443–50. doi: 10.1056/NEJMcp030751
3. Ehrlich E, Gibson T, Mark T. Trends in Prescriptions for Oral Contraceptives Among US Teenagers. Thomson Reuters (2011)/
5. Cobey KD, Buunk AP. Conducting high-quality research on the psychological impact of oral contraceptive use. Contraception. (2012) 86:330–1. doi: 10.1016/j.contraception.2012.01.011
6. Montoya ER, Bos PA. How oral contraceptives impact social-emotional behavior and brain function. Trends Cogn Sci. (2017) 21:125–36. doi: 10.1016/j.tics.2016.11.005
7. Pletzer BA, Kerschbaum HH. 50 years of hormonal contraception—time to find out, what it does to our brain. Front Neurosci. (2014) 8:256. doi: 10.3389/fnins.2014.00256
8. McKetta S, Keyes KM. Oral contraceptive use and depression among adolescents. Ann Epidemiol. (2019) 29:46–51. doi: 10.1016/j.annepidem.2018.10.002
9. Rapkin AJ, Morgan M, Sogliano C, Biggio G, Concas A. Decreased neuroactive steroids induced by combined oral contraceptive pills are not associated with mood changes. Fertil Steril. (2006) 85:1371–8. doi: 10.1016/j.fertnstert.2005.10.031
10. Cheslack-Postava K, Keyes KM, Lowe SR, Koenen KC. Oral contraceptive use and psychiatric disorders in a nationally representative sample of women. Arch Women's Mental Health. (2015) 18:103–11. doi: 10.1007/s00737-014-0453-4
11. Freeman EW, Halbreich U, Grubb GS, Rapkin AJ, Skouby SO, Smith L, et al. An overview of four studies of a continuous oral contraceptive (levonorgestrel 90 mcg/ethinyl estradiol 20 mcg) on premenstrual dysphoric disorder and premenstrual syndrome. Contraception. (2012) 85:437–45. doi: 10.1016/j.contraception.2011.09.010
12. Keyes KM, Cheslack-Postava K, Westhoff C, Heim CM, Haloossim M, Walsh K, et al. Association of hormonal contraceptive use with reduced levels of depressive symptoms: a national study of sexually active women in the United States. Am J Epidemiol. (2013) 178:1378–88. doi: 10.1093/aje/kwt188
13. Toffol E, Heikinheimo O, Koponen P, Luoto R, Partonen T. Hormonal contraception and mental health: results of a population-based study. Hum Reprod. (2011) 26:3085–93. doi: 10.1093/humrep/der269
14. Toffol E, Heikinheimo O, Koponen P, Luoto R, Partonen T. Further evidence for lack of negative associations between hormonal contraception and mental health. Contraception. (2012) 86:470–80. doi: 10.1016/j.contraception.2012.02.014
15. Anderl C, Li G, Chen FS. Oral contraceptive use in adolescence predicts lasting vulnerability to depression in adulthood. J Child Psychol Psychiatry. (2020) 61:148–56. doi: 10.1111/jcpp.13115
16. de Wit AE, Booij SH, Giltay EJ, Joffe H, Schoevers RA, Oldehinkel AJ. Association of use of oral contraceptives with depressive symptoms among adolescents and young women. JAMA Psychiatry. (2020) 77:52–9. doi: 10.1001/jamapsychiatry.2019.2838
17. Skovlund CW, Morch LS, Kessing LV, Lidegaard O. Association of hormonal contraception with depression. JAMA Psychiatry. (2016) 73:1154–62. doi: 10.1001/jamapsychiatry.2016.2387
18. Wirehn AB, Foldemo A, Josefsson A, Lindberg M. Use of hormonal contraceptives in relation to antidepressant therapy: A nationwide population-based study. Eur J Contracept Reproductive Health Care. (2010) 15:41–7. doi: 10.3109/13625181003587004
19. Skovlund CW, Morch LS, Kessing LV, Lange T, Lidegaard O. Association of hormonal contraception with suicide attempts and suicides. Am J Psychiatry. (2018) 175:336–42. doi: 10.1176/appi.ajp.2017.17060616
20. Bengtsdotter H, Lundin C, Gemzell Danielsson K, Bixo M, Baumgart J, Marions L, et al. Ongoing or previous mental disorders predispose to adverse mood reporting during combined oral contraceptive use. Eur J Contracept Reproductive Health Care. (2018) 23:45–51. doi: 10.1080/13625187.2017.1422239
21. Lundin C, Danielsson KG, Bixo M, Moby L, Bengtsdotter H, Jawad I, et al. Combined oral contraceptive use is associated with both improvement and worsening of mood in the different phases of the treatment cycle-A double-blind, placebo-controlled randomized trial. Psychoneuroendocrinology. (2017) 76:135–43. doi: 10.1016/j.psyneuen.2016.11.033
22. Graham BM, Li SH, Black MJ, Ost LG. The association between estradiol levels, hormonal contraceptive use, and responsiveness to one-session-treatment for spider phobia in women. Psychoneuroendocrinology. (2018) 90:134–40. doi: 10.1016/j.psyneuen.2018.02.019
23. Raeder F, Heidemann F, Schedlowski M, Margraf J, Zlomuzica A. No pills, more skills: The adverse effect of hormonal contraceptive use on exposure therapy benefit. J Psychiatr Res. (2019) 119:95–101. doi: 10.1016/j.jpsychires.2019.09.016
24. Robakis T, Williams KE, Nutkiewicz L, Rasgon NL. Hormonal contraceptives and mood: review of the literature and implications for future research. Curr Psychiatry Rep. (2019) 21:57. doi: 10.1007/s11920-019-1034-z
25. Kaltiala-Heino R, Kosunen E, Rimpela M. Pubertal timing, sexual behaviour and self-reported depression in middle adolescence. J Adolesc. (2003) 26:531–45. doi: 10.1016/S0140-1971(03)00053-8
26. Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC. Smoking and major depression. A causal analysis. Arch Gene Psychiatry. (1993) 50:36–43. doi: 10.1001/archpsyc.1993.01820130038007
27. Zettermark S, Perez Vicente R, Merlo J. Hormonal contraception increases the risk of psychotropic drug use in adolescent girls but not in adults: A pharmacoepidemiological study on 800 000 Swedish women. PLoS ONE. (2018) 13:e0194773. doi: 10.1371/journal.pone.0194773
28. Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, Allen NB. Gender differences in anxiety disorders and anxiety symptoms in adolescents. J Abnorm Psychol. (1998) 107:109–17. doi: 10.1037/0021-843X.107.1.109
29. Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. (2008) 9:947–57. doi: 10.1038/nrn2513
30. Steiner M, Dunn E, Born L. Hormones and mood: from menarche to menopause and beyond. J Affect Disord. (2003) 74:67–83. doi: 10.1016/S0165-0327(02)00432-9
31. Hankin BL. Adolescent depression: description, causes, and interventions. Epilepsy Behav. (2006) 8:102–14. doi: 10.1016/j.yebeh.2005.10.012
32. Weiss DD, Last CG. Developmental variations in the prevalence and manifestation of anxiety disorders. Dev Psychopathol Anxiety. (2001) 1:27–42. doi: 10.1093/med:psych/9780195123630.003.0002
33. Sisk CL, Zehr JL. Pubertal hormones organize the adolescent brain and behavior. Front Neuroendocrinol. (2005) 26:163–74. doi: 10.1016/j.yfrne.2005.10.003
34. Cahill L. How does hormonal contraception affect the developing human adolescent brain? Curr Opin Behav Sci. (2018) 23:131–5. doi: 10.1016/j.cobeha.2018.06.015
35. Branje S, Meeus WHJ. Research on Adolescent Development and Relationships (Young Cohort) (2018).
36. Reynolds WM. Reynolds Adolescent Depression Scale: Professional Manual. Psychological Assessment Resources, Inc. (2002).
37. Osman A, Gutierrez PM, Bagge CL, Fang Q, Emmerich A. Reynolds adolescent depression scale-second edition: a reliable and useful instrument. J Clin Psychol. (2010) 66:1324–45. doi: 10.1002/jclp.20727
38. Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. (1997) 36:545–53. doi: 10.1097/00004583-199704000-00018
39. Hale WW, Crocetti E, Raaijmakers QA, Meeus WH. A meta-analysis of the cross-cultural psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED). J Child Psychol Psychiatry. (2011) 52:80–90. doi: 10.1111/j.1469-7610.2010.02285.x
40. Hale WW, Raaijmakers Q, Muris P, Meeus W. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED) in the general adolescent population. J Am Acad Child Adolesc Psychiatry. (2005) 44:283–90. doi: 10.1097/00004583-200503000-00013
41. La Greca AM, Harrison HM. Adolescent peer relations, friendships, and romantic relationships: Do they predict social anxiety and depression? J Clin Child Adolesc Psychol. (2005) 34:49–61. doi: 10.1207/s15374424jccp3401_5
42. McCullough ME, Larson DB. Religion and depression: a review of the literature. Twin Res. (1999) 2:126–36. doi: 10.1375/twin.2.2.126
43. Boden JM, Fergusson DM. Alcohol and depression. Addiction. (2011) 106:906–14. doi: 10.1111/j.1360-0443.2010.03351.x
44. Hallfors DD, Waller MW, Bauer D, Ford CA, Halpern CT. Which comes first in adolescence—sex and drugs or depression? Am J Prev Med. (2005) 29:163–70. doi: 10.1016/j.amepre.2005.06.002
45. Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. (2008) 33:693–710. doi: 10.1016/j.psyneuen.2008.03.008
46. Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. (2004) 161:631–6. doi: 10.1176/appi.ajp.161.4.631
47. Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med. (2008) 66:1334–45. doi: 10.1016/j.socscimed.2007.12.019
48. Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. (2003) 157:98–112. doi: 10.1093/aje/kwf182
49. Reynolds CA, Finkel D, McArdle JJ, Gatz M, Berg S, Pedersen NL. Quantitative genetic analysis of latent growth curve models of cognitive abilities in adulthood. Dev Psychol. (2005) 41:3–16. doi: 10.1037/0012-1649.41.1.3
50. Duke JM, Sibbritt DW, Young AF. Is there an association between the use of oral contraception and depressive symptoms in young Australian women? Contraception. (2007) 75:27–31. doi: 10.1016/j.contraception.2006.08.002
51. Oinonen KA, Mazmanian D. To what extent do oral contraceptives influence mood and affect? J Affect Disord. (2002) 70:229–40. doi: 10.1016/S0165-0327(01)00356-1
52. Myers MG, Aarons GA, Tomlinson K, Stein MB. Social anxiety, negative affectivity, and substance use among high school students. Psychol Addictive Behav. (2003) 17:277. doi: 10.1037/0893-164X.17.4.277
53. Shedler J, Block J. Adolescent drug use and psychological health: A longitudinal inquiry. Am Psychol. (1990) 45:612. doi: 10.1037/0003-066X.45.5.612
54. Siebenbruner J, Englund MM, Egeland B, Hudson K. Developmental antecedents of late adolescence substance use patterns. Dev Psychopathol. (2006) 18:551–71. doi: 10.1017/S0954579406060287
55. Hames JL, Hagan CR, Joiner TE. Interpersonal processes in depression. Annu Rev Clin Psychol. (2013) 9:355–77. doi: 10.1146/annurev-clinpsy-050212-185553
56. Endedijk HM, Nelemans SA, Schur RR, Boks MPM, van Lier P, Meeus W, et al. The role of stress and mineralocorticoid receptor haplotypes in the development of symptoms of depression and anxiety during adolescence. Front Psychiatry. (2020) 11:367. doi: 10.3389/fpsyt.2020.00367
57. Nelemans SA, Boks M, Lin B, Oldehinkel T, van Lier P, Branje S, et al. Polygenic risk for major depression interacts with parental criticism in predicting adolescent depressive symptom development. J Youth Adolesc. (2021) 50:159–76. doi: 10.1007/s10964-020-01353-4
58. Nelemans SA, Hale WW, Raaijmakers QA, Branje SJ, van Lier PA, Meeus WH. Longitudinal associations between social anxiety symptoms and cannabis use throughout adolescence: the role of peer involvement. Eur Child Adolesc Psychiatry. (2016) 25:483–92. doi: 10.1007/s00787-015-0747-8
59. Granic I. Timing is everything: Developmental psychopathology from a dynamic systems perspective. Dev Rev. (2005) 25:386–407. doi: 10.1016/j.dr.2005.10.005
60. Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. (1997) 278:823–32. doi: 10.1001/jama.1997.03550100049038
61. Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. J Consult Clin Psychol. (2002) 70:6–20. doi: 10.1037/0022-006X.70.1.6
62. D'augelli AR. Mental health problems among lesbian, gay, and bisexual youths ages 14 to 21. Clin Child Psychol Psychiatry. (2002) 7:433–56. doi: 10.1177/1359104502007003039
Keywords: development, adolescence, anxiety, depression, oral contraceptives (OCs)
Citation: Doornweerd AM, Branje S, Nelemans SA, Meeus WHJ, Montoya ER, Engelhard IM, Baas JMP and Gerritsen L (2022) Stable Anxiety and Depression Trajectories in Late Adolescence for Oral Contraceptive Users. Front. Psychiatry 13:799470. doi: 10.3389/fpsyt.2022.799470
Received: 05 November 2021; Accepted: 12 April 2022;
Published: 23 May 2022.
Edited by:
Agnès Lacreuse, University of Massachusetts Amherst, United StatesReviewed by:
Abdul-Rahman Hudaib, Monash Alfred Psychiatry Research Centre, AustraliaPatrizia Porcu, National Research Council (CNR), Italy
Shuliweeh Alenezi, King Saud University, Saudi Arabia
Copyright © 2022 Doornweerd, Branje, Nelemans, Meeus, Montoya, Engelhard, Baas and Gerritsen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anne Marieke Doornweerd, YS5tLmRvb3Jud2VlcmRAdXUubmw=
 Anne Marieke Doornweerd
Anne Marieke Doornweerd Susan Branje
Susan Branje Stefanie A. Nelemans
Stefanie A. Nelemans Wim H. J. Meeus
Wim H. J. Meeus Estrella R. Montoya1,4
Estrella R. Montoya1,4 Joke M. P. Baas
Joke M. P. Baas