- 1School of Psychology, Beijing Sport University, Beijing, China
- 2Department of Psychology, Gdañsk University of Physical Education and Sport, Gdańsk, Poland
- 3Institute of Psychology, University of Gdañsk, Gdańsk, Poland
- 4Institute of Psychology, Jagiellonian University, Kraków, Poland
Objective: Body-image disturbance and eating disorders are significant physical and mental health problems in China. Attitudes toward the body are thought to work in conjunction with other established risk factors for dietary pathology, which include body dissatisfaction, dieting, and negative effects. Negative appearance evaluation may be valuable for extending our understanding of measuring factors and potential causal relationships associated with body image and eating problems. Therefore, this study aimed to determine the association between negative appearance evaluation and a combination of eating attitudes and sociocultural attitudes toward appearance and the mediating effect of negative appearance evaluation on the relationship between eating attitudes and sociocultural attitudes toward appearance.
Methods: We invited 339 Chinese adults to undergo the Eating Attitudes Test (EAT-26), the Fear of Negative Appearance Evaluation Scale (FNAES), and the Sociocultural Attitudes toward Appearance (SATAQ-3) scale, and used AMOS 24.0 for model construction and mediating effects testing.
Results: There was a significant positive correlation between EAT-26 scores and FNAES (p < 0.001) and SATAQ-3 scores (p < 0.001), and all dimensions except internalization general were significantly positively correlated (p < 0.05). There was a significant positive correlation between FNAES and SATAQ-3 scores for all dimensions (p < 0. 01). There was no significant direct effect of eating attitude on sociocultural attitude toward appearance; however, there was a significant mediating effect of fear of negative appearance evaluation.
Conclusion: Our results demonstrate that negative appearance evaluation fully mediates the relationship between eating attitudes and sociocultural attitudes toward appearance. An individual’s attitude toward eating affects negative body perceptions and thus their perception of their own body shape. Our exploration of the specific effects of eating attitudes on body perception provides a psychological basis for guidance and developing interventions regarding attitudes toward the body.
Introduction
An eating disorder is a type of mental disorder that is characterized by abnormal eating habits or a group of abnormal eating behaviors and negatively impacts physical and mental health (1, 2). Abnormal eating behaviors include reduced physical fitness, altered body weight and body fat percentage, and poor bone health (3). Moreover, eating disorders are a major cause of physical and mental health problems among young women (4). The main clinical manifestations are bulimia nervosa, anorexia nervosa, and binge-eating disorder, and the main subclinical manifestations are diet and bulimia (5, 6). Clinical eating disorders are relatively rare and primarily develop and evolve from subclinical eating disorders, which are highly common. Subclinical eating disorders affect 60% of girls and 30% of boys (7).
It has been shown that when individuals are faced with stressful events, have long-term distorted cognition of physique or body shape, or are affected by negative emotions, they are prone to abnormal eating attitudes, which often manifest as overeating, dieting, and other eating problems (8–10). Eating attitudes are a series of cognitive, emotional, and behavioral tendencies of individuals who consider eating as an object. In severe cases, these tendencies can develop into a clinical eating disorder, such as bulimia nervosa, anorexia nervosa, and binge-eating disorder (11). The Eating Attitudes Test (EAT-26) is a reliable and valid instrument that provides an objective measure of the symptoms of anorexia nervosa (12). Furthermore, the EAT-26 may be considered the most appropriate tool as an outcome measure for clinical groups or as a screening tool for high-risk groups for anorexia nervosa in non-clinical settings (13). It is influenced by external stimuli, situations, and the individuals themselves (14).
Individuals with eating disorders are prone to negative self-evaluation, which results in a deformed body image (15, 16). The most prominent psychological problems in individuals with eating disorders are related to their attitudes toward thinness and food. The heavier their weight, the stronger their desire to be thin, and the greater the difficultly in controlling excessive eating. However, underlying these specific attitudes toward body shape and eating, patients with eating disorders may also have other psychological problems, such as pursuing perfection and fear of growth and maturity (17, 18). According to Garner et al. (19), individuals with abnormal eating attitudes may have distortions in body image and inner feelings, which are accompanied by psychophysiological symptoms, such as negative body self, unreasonable eating, and irregular sleep. Previous research has shown that the total score of eating is positively correlated with the fat subscale score of the Negative Physical Self Scale, which indicates that individuals with a high eating attitude score are more likely to have an eating disorder and a more negative cognition of their body (20). Chen (21) showed that anorexia nervosa patients have negative cognitive eating disorders and body image disorders; they are not satisfied with their current body mass and may even have a cognitive bias toward their already low body mass index (BMI). However, patients with anorexia nervosa may overestimate their body weight due to visual distortions (22). Moreover, based on stereotypes about weight, people with eating disorders have double standards that lead to a distorted evaluation or characterization of their external image (23). Furthermore, personality types have been shown to influence individuals’ perceptions of body satisfaction and body image (24). There is also evidence that overvaluation of low body weight and fear of weight gain cannot be explained by general cognition, rather, they require individual judgments (26). In other words, patients do not exhibit changes in physical representations in general; instead, they present with top-down cognitive-emotional distortions in evaluations of their own bodies (27).
In 1962, Bruch first proposed that anorexia nervosa patients have body-image disorder, and numerous reports have since reported similar findings. Body-image disturbances are usually associated with eating disorders (28). Body image disorder is a distorted understanding of one’s image, which is caused by social, psychological, or biological factors (29). A disturbance in body image is an individual’s cognitive maladjustment of their body, which usually leads to negative emotional experiences (30). Thompson et al. (31) proposed the definition, “a persistent report of dissatisfaction, concern, and distress that is related to an aspect of appearance… [and] some degree of impairment in social relations, social activities, or occupational functioning” (p. 11). Body-image disturbances are particularly prominent among female college students and include dissatisfaction with body shape, skin color, height, and other aspects (32), which leads to low self-esteem, anxiety, and depression due to public self-consciousness (33). The Fear of Negative Appearance Evaluation Scale [FNAES; (34)] is used to assess apprehension about appearance evaluation and determines the degree to which people experience apprehension at the prospect of being evaluated negatively for their appearance. It was developed by modifying items from the Brief Fear of Negative Evaluation Scale (35) and creating novel items that index apprehension toward a negative appearance evaluative experience.
Thomas et al. (34) and Leary (35) speculated that fear of negative appearance evaluation (FNAE) and fear of negative evaluation (FNE) are related to sociocultural factors. Various disparate influences have received attention in the field of body image disturbances and eating disorders, including interpersonal and sociocultural factors such as negative appearance-related feedback (teasing), modeling of dieting and body image concerns by parents and peers, elevated tendencies to compare one’s appearance to others, sexual abuse, sexual harassment, and internalization of media images and messages (36, 37). Furthermore, investigating the more specific FNAE may be valuable for extending recent work regarding the identification of factors that are associated with, and potentially the cause of, body image and eating problems (51).
Appearance-ideal internalization and appearance pressures are empirically supported risk factors for body image disturbance and disordered eating in Western countries (39, 40). The sociocultural theory has been shown to be a useful framework for exploring how environmental influences contribute to body image concerns (31). The Sociocultural Attitudes toward Appearance Questionnaire (SATAQ-3) is used to document an individual’s recognition of their awareness of a societal influence, alongside the endorsement/acceptance of the prevailing message of an internalization of the touted standard (41). Research findings consistently support the strong relationship between sociocultural influences and body dissatisfaction (42). Several studies have shown that thin-ideal internalization and perceived appearance pressures are uniquely associated with and predict body dissatisfaction. Girard et al. (43) emphasized the usefulness of sociocultural models in understanding women’s body image, which includes their drive for thinness and muscularity concerns. As Knauss et al. (44) expected, internalization, pressure, and BMI contribute to the prediction of body dissatisfaction in boys and girls; moreover, girls internalize media body ideals to a greater extent and feel more pressure from media to conform to this ideal than do boys. In the model by Lovering et al. (45), sociocultural pressure from the media, partners, and peer variables significantly predict body image and eating concerns through the mediating effect of the latent thin-ideal variable (i.e., internalization of the thin-ideal and appearance comparisons), and of the four pathways, the pathway between the media influence variable to the thin-ideal variable was the strongest (45). Exploring the Tripartite Influence Model of body dissatisfaction in postpartum women. There is strong evidence for significant relationships among the putative risk factors, mediators (internalization, comparisons, and peer suppression of feelings), and criterion variables (body dissatisfaction, drive for thinness, bulimic symptoms, and self-esteem) (46). Peer influences, body-image dissatisfaction, eating dysfunction, and self-esteem in adolescent girls. Appearance-ideal internalization refers to the acceptance of culturally endorsed appearance ideals (e.g., thinness for females and muscularity for males) as one’s personal appearance standard (47), whereas perceived pressures can be defined as the feeling of being encouraged to modify one’s physical appearance to reach such ideals (48). A meta-analysis revealed that the emphasis of mass media on the beauty of being slim is significantly related to body image disorder in college students (especially women) (49). In addition, other studies have found that the likelihood of females developing an eating disorder is positively correlated with the degree of recognition of social values (50).
In summary, this study hypothesized that there are two stages of the effect of dietary attitudes on sociocultural attitudes toward appearance. In the first stage, a disorder of dietary attitudes activates FNAE. In the second stage, FNAE eventually affects sociocultural attitudes toward appearance. Therefore, this study hypothesized that: (1) there is a relationship between negative appearance evaluation and sociocultural attitudes toward appearance, and (2) FNAE plays a complete mediating role in the influence of eating attitudes on sociocultural attitudes toward appearance.
Materials and Methods
Participants and Procedure
Participants were 339 healthy people (176 female, 163 male) from various regions of China who were invited to complete the questionnaires. The average age of participants was 31.06 years (range = 18–72 years, standard deviation [SD] = 11.87 years), and mean BMI was 22.24 (range = 14.5–37.2, SD = 3.86). Inclusion criteria were: aged ≥18 years, Chinese nationality, residence in China, and no physical disability or somatic diseases that prevent physical activity. Criteria were verified according to responses to questions on sociodemographic data and health, which allowed for the determination of the exclusion factors.
During the data collection period, 632 participants completed the survey in Chinese. We excluded 201 returned questionnaires from the analysis because of errors in completing the questionnaires (incomplete data) and respondents who had a nationality other than Chinese. A further 92 questionnaires were excluded because the inclusion criteria were not fulfilled.
The procedure carried out in this study consisted of an online survey conducted as part of an international research project registered on ClinicalTrials.gov.1 This study used data collected from a Chinese population between July 20, 2020, and November 24, 2020, during the period of the global pandemic situation. The work was carried out according to the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The protocol was approved by the Ethics Board for Research Projects at the Institute of Psychology, University of Gdańsk, Poland (decision no. 33/2020). The questionnaires that formed this study took around 30 min to complete. All survey participants provided electronic informed consent before registration.
Instruments
Fear of Negative Appearance Evaluation Scale
The FNAES (51) was used to assess women’s apprehension toward appearance evaluations. The FNAES contained six items (e.g., I’m worried about what people think of my appearance), which were scored on a five-point Likert scale, from definitely disagree to definitely agree. Higher scores indicated greater FNAE. Cronbach’s alpha for the FNAES in the present study was 0.93.
The Eating Attitudes Test
The EAT-26 was used to assess subjects on their cognitive, emotional, and behavioral tendencies regarding diet (19). It comprised 26 items that measured three factors: dieting, bulimia, and food preoccupation (abbreviated as bulimia), and oral control. In this study, scale scores were calculated using screening scores. Questions 1 to 25 were scored as never/rarely/sometimes = 0, often = 1, usually = 2, or always = 3, and question 26 was scored in the opposite way. Higher scores represent more severe eating attitudes and behavioral problems. A total score ≥20 indicated the possible presence of an eating disorder. Cronbach’s alpha for the EAT-26 in the present study was 0.72.
The Sociocultural Attitudes Toward Appearance Questionnaire-3
The SATAQ-3 (48) was used to assess participants’ sociocultural attitudes toward appearance. The SATAQ-3 is a 30-item measure comprising four subscales: internalization general, internalization athlete, perception of pressure, and information. Each item was scored on a five-point Likert scale, from definitely disagree to definitely agree.
The information subscale consisted of nine items, which were used to measure recognition of the social importance of beauty ideals in the media (e.g., magazine advertisements are an important source of information about fashion and “being attractive”). The pressure subscale consisted of seven items, which were used to measure perceived stress to meet the Western ideal displayed by the media (e.g., I’ve felt pressure from television or magazines to have a perfect body). The internalization general subscale consisted of nine items, which were used to measure the internalization of the thin ideal (e.g., I compare my body to the bodies of people who are on television, and I do not care if my body looks like the body of people who are on television). The internalization athlete subscale consisted of five items, which were used to measure the internalization of the sports ideal (e.g., I try to look like sports athletes and I wish I looked as athletic as sports stars). Previous studies have shown that the SATAQ-3 has high internal consistency in female college students and patients with eating disorders. Cronbach’s alpha for the SATAQ-3 in the present study was 0.88.
Data Analysis
Data analysis was performed using SPSS 26.0 and AMOS 24.0. T-tests or one-way analyses of variance (ANOVAs) were used to compare scores between participants with different demographic information. Pearson correlation analysis was used to explore relationships between FNAES, EAT-26 (dieting, bulimia and food preoccupation, and oral control), and SATAQ-3 (information, pressure, internalization general, and internalization athlete) scores. In addition, AMOS 24.0 was used to clarify the influencing path of participants’ eating attitudes and sociocultural attitudes toward appearance on external apprehension toward appearance evaluations. Bootstrapping was used to test the mediating effect of apprehension toward appearance evaluations on the relationship between eating attitudes and external sociocultural attitudes toward appearance. A p < 0.05 was considered statistically significant.
Results
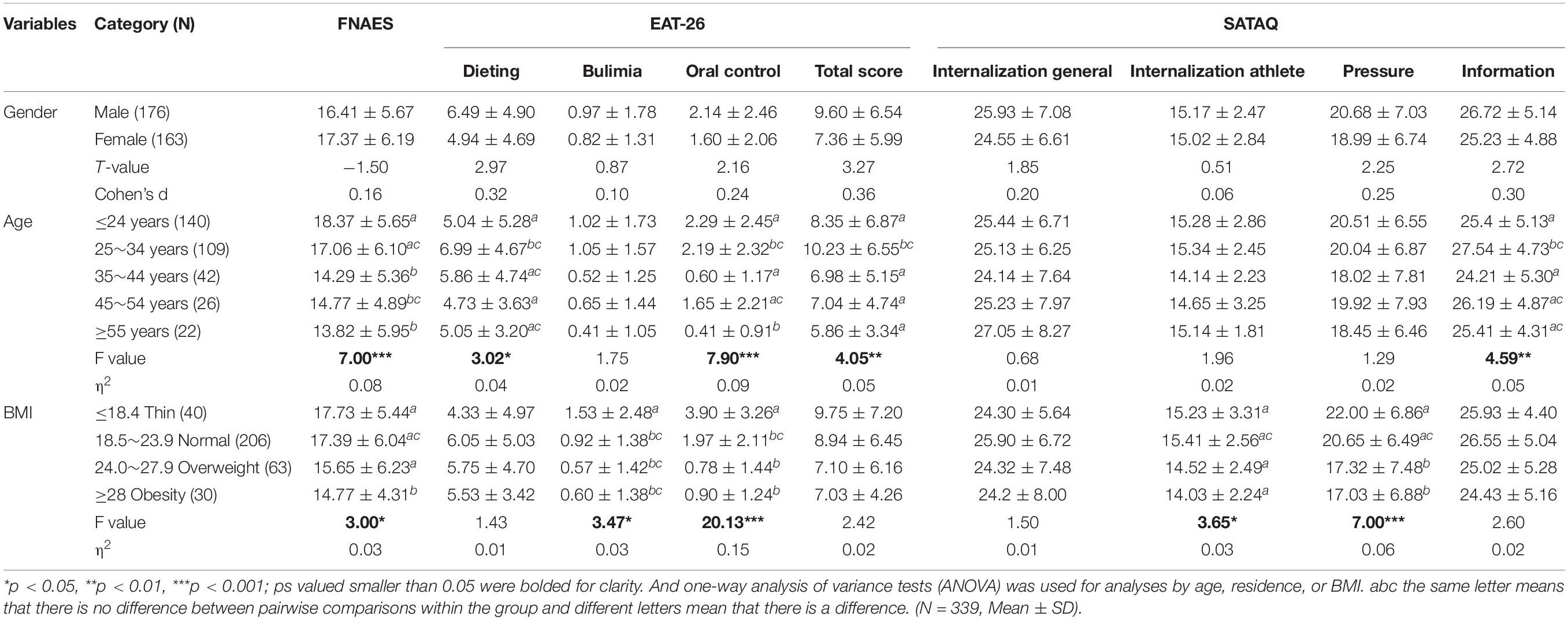
Table 1 shows the differences between the selected demographic variable groups for the FNAES, EAT-26, and SATAQ-3 scores. The mean FNAES score was higher in females (17.37 ± 6.19) than in males (16.41 ± 5.67). Females scored lower than men on the EAT-26 for both total and all dimension scores. SATAQ-3 scores showed similar patterns as the FNAES and EAT-26 scores; however, there were no significant differences.
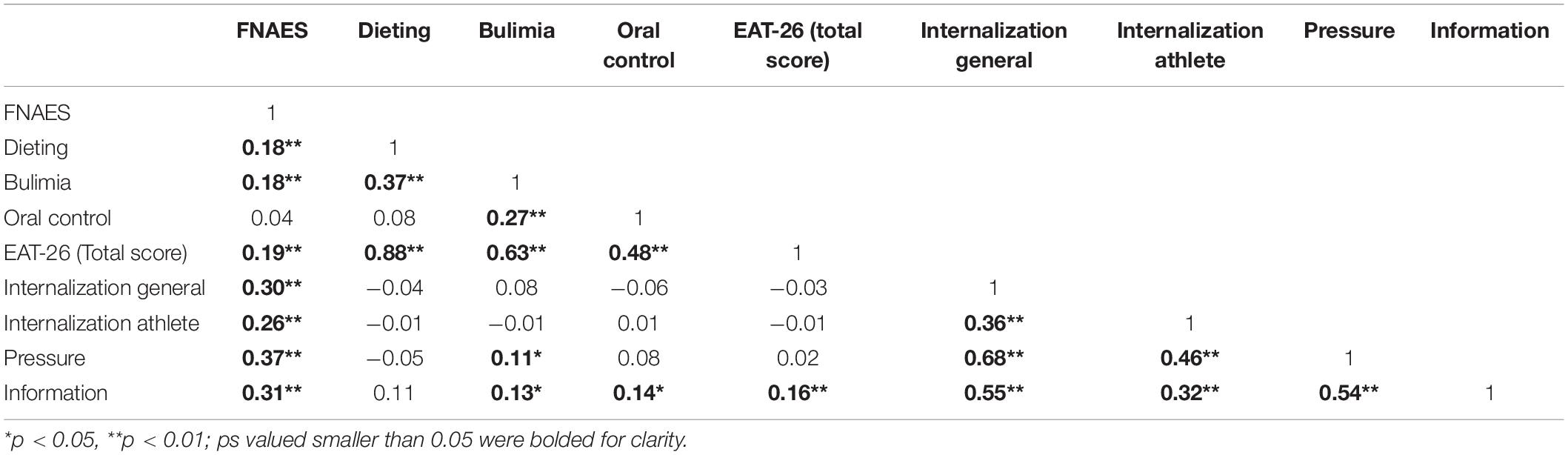
Pearson correlation analysis showed that FNAES score was positively correlated with the dieting (r = 0.18, p < 0.01), bulimia (r = 0.18, p < 0.01), and total score (r = 0.19, p < 0.05) of the EAT-26, and internalization general (r = 0.30, p < 0.01), internalization athlete (r = 0.26, p < 0.01), pressures (r = 0.37, p < 0.01), and information (r = 0.31, p < 0.01) of the SATAQ-3. In addition, the bulimia score was positively correlated with the pressures (r = 0.11, p < 0.05) and information scores (r = 0.13, p < 0.05), the oral control score was positively correlated with the information score (r = 0.14, p < 0.05), and the total score was positively correlated with the information score (r = 0.16, p < 0.01) (Table 2).
The structural equation models built using the EAT-26 score as the independent variable, SATAQ-3 score as the dependent variable, and FNAES score as the mediating variable (Figure 1) showed that the model had a good fit (χ2/df = 2.831, AGFI = 0.931, CFI = 0.945, GFI = 0.966, IFI = 0.946, RMSEA = 0.074, SRMR = 0.045, TLI = 0.915). Furthermore, the standardized path coefficients showed that the EAT-26 score significantly predicted the FNAES score (β = 0.21, p < 0.01), and the FNAES score significantly predicted the SATAQ-3 score (β = 0.41, p < 0.01) (Figure 1).
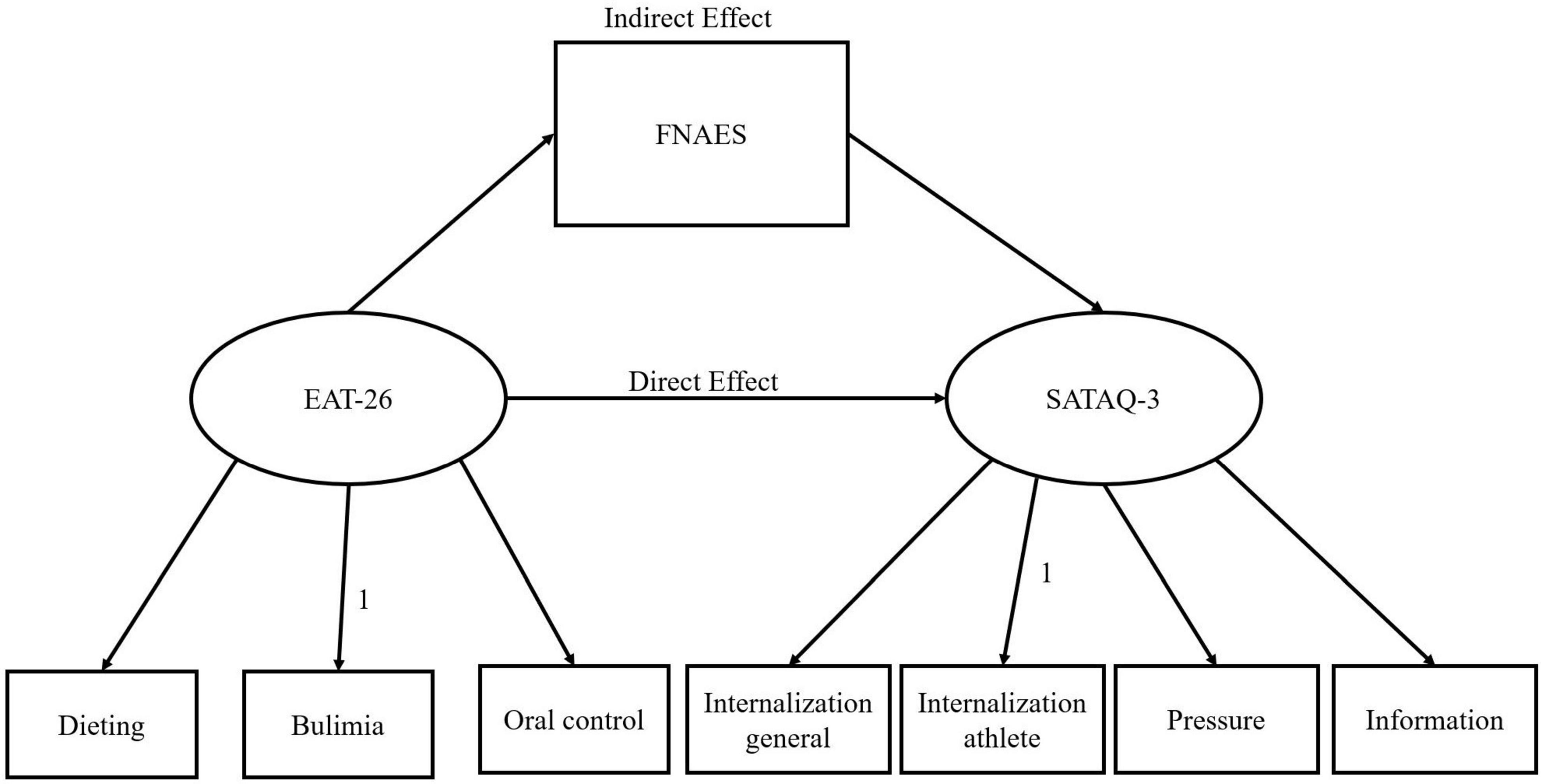
Figure 1. Path analysis of the relationship between FNAES, EAT-26, and SATAQ-3 scores of the participants.
The results of the mediation effect indicated that the mediating effect was significant; however, the direct effect was not significant. Apprehension toward appearance evaluations played a complete mediating role between eating attitudes and sociocultural attitudes toward appearance, and the mediation effect accounted for 70.09% of the total effect (Table 3).
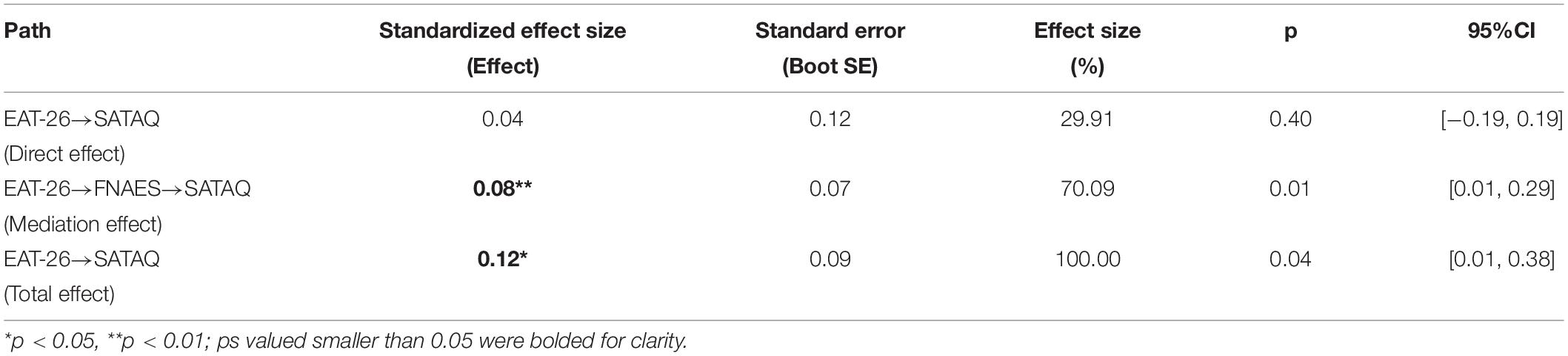
Table 3. Bootstrap analysis of the mediation effect size and significance test of FNAES in EAT-26 and SATAQ.
Discussion
The present study examined the association between negative appearance evaluation and a combination of eating attitudes and sociocultural attitudes toward appearance. We also explored the mediating effect of negative appearance evaluation on the relationship between eating attitudes and sociocultural attitudes toward appearance. Overall, the data suggested that negative appearance evaluation is associated with sociocultural attitudes toward appearance. Specifically, those who report eating disorders demonstrated higher levels of sociocultural attitudes toward appearance. Negative appearance evaluation scores significantly mediated the relationship between eating attitudes and sociocultural attitudes toward appearance.
These findings both support and extend previous literature regarding the relationship between sociocultural attitudes toward appearance and adaptive eating patterns. Women are at higher risk of eating disorders, especially women in college, and have the highest prevalence of eating disordered behaviors (40, 52). The sex difference might be attributed to biological, psychodynamic, and sociocultural factors (53). However, there was no significant difference in eating attitudes between different BMI groups, except for bulimia and oral control subscale scores. Furthermore, those aged 25–34 years had the highest average score on this scale. Current research on eating disorders is focused on adolescents (7, 54–56), and there is a lack of large-scale cross-sectional studies on the age of onset of eating disorders, which may be a useful research direction in the future. This study showed that there was no significant difference in negative image ratings between men and women. However, there were significant differences in the evaluation of one’s own image among different age groups; the perception of one’s appearance and physique became more negative with age. As women approach midlife, the pressures that came from body monitoring and surveillance (57) begin prior to middle age. These pressures may become more salient during the aging process (58, 59). In addition to the social ideal of being beautiful and slim in women of all ages, middle-aged women also face age-related pressures, such as the need to avoid wrinkles and other visible signs of aging (60–62). These increasing pressures may develop into concerns about appearance, which increases the fear of negative appearance judgment and results in greater dissatisfaction with their body (63). Scores differed significantly between BMI groups, whereby people with a lower BMI tended to have a more negative evaluation of their appearance. This was not consistent with the results of previous studies. Studies have found that the FNAES does not significantly correlate with BMI (51). This discrepancy may be due to cultural differences between China and the West; moreover, the pursuit of thinness for a prolonged period may lead people with a lower BMI to be less satisfied with their appearance. Notably, the impact of the coronavirus 19 (COVID-19) outbreak is a problem that cannot be ignored. The COVID-19 outbreak threatened public physical health while having a profound impact on the public’s mental health (64, 65). Indeed, several self-reported studies have suggested that dietary restrictions or compensatory behaviors were further exacerbated during the outbreak (66). Moreover, recent questionnaire data suggests that the epidemic had a similar negative impact on people’s diet under certain conditions, whereby symptoms became more severe in patients with eating disorders (67). In addition, under the strict control conditions of the COVID-19 pandemic in China, such effects may have been amplified, which likely affected individuals’ perception of their external image. To some extent, this may have influenced a more negative view of their external image, which can lead to cognitive biases that are ultimately reflected in sociocultural attitudes.
This study also found a positive correlation between eating attitudes and FNAE, which is consistent with previous research. Several studies have investigated eating disorders in both men and women and found that those with eating disorders have a higher incidence of emotional disorders (68–73). Furthermore, satisfaction with body image is significantly different from that of the control group (53), demonstrating clear body dissatisfaction in this group (74, 75). FNAE, which is defined as social anxiety and distress due to their appearance negatively evaluated, has been found to be predictive of eating disorders above and beyond other body image variables (51). Patients with eating disorders may be more worried about their appearance being negatively evaluated. Indeed, clinical samples of women with eating disorders report higher levels of fear of negative evaluation than that of controls (76). Social appearance anxiety (i.e., fear of negative evaluation of one’s appearance) and general fear of negative evaluation have each been proposed as risk factors for eating disorders. It is possible that treating FNAE may reduce eating disorder symptoms (77).
Fear of negative appearance evaluation scale was also associated with sociocultural attitudes toward appearance, and we observed a correlation between eating attitudes and information. Because of the cultural differences between the West and China, people have different sociocultural attitudes toward appearance, which affects the generalization of our results. Slimness is an ideal criterion for female attractiveness in China (78), and girls who do not conform to this philosophy are more likely to receive negative feedback, experience physical dissatisfaction, and perform inappropriate compensatory behaviors to reduce the difference between their own and the ideal body shape (78). Moreover, there is a stronger cultural premium on appearance and attractiveness as defining attributes of femininity in China (79). In Western culture, objectification theory (80) suggests that Western societies sexually objectify the female body, which leads women to feel as if they are constantly being valued (or devalued) according to their appearance. Internalization of media images and messages (36, 81) may lead to the onset and maintenance of body image disturbance and eating disorders (47, 82). The external pressure and information that constantly instill the concept of beauty may influence eating attitudes toward gaining social recognition of “beauty” through dieting and other behaviors.
Our findings contribute to evidence suggesting that the relationship between eating attitudes and sociocultural attitudes toward appearance is mediated by negative appearance evaluation. van den Berg et al. (83) reported that girls exhibit internalization of the ideal body and feel more pressure from the media than boys. When girls have a strong negative image of their bodies, there is a greater internalizing effect when they see “plus-size” models or “slim” pictures that suggest that slim models represent beauty, and a negative self-image reinforces this perception. The age range of participants in this study was largely focused on adolescence and the period of transition from adolescence to middle age. Body image concerns usually begin and increase during early adolescence and decrease in younger adulthood; thus, it affects mental health at different stages of life. The type and extent of body image disturbance vary with age, race, peers, family, and sociocultural influences. The development of negative body image disorders is considered to be the strongest determinant of sociocultural influences, and body dissatisfaction is considered to be a predictor of eating disorders because adolescents do not accept the “ideal body.” Furthermore, current research suggests that body dissatisfaction is associated with an increased tendency to initiate unhealthy eating behaviors, for which girls are at higher risk than boys (84). Notably, the present study was conducted in adolescents without a diagnosis of eating disorders in a non-clinical setting. In an earlier study, Furnham et al. (85) observed that males and females had comparable levels of body dissatisfaction, but in opposite directions: 41% of males wanted to be thinner, whereas 22% of females wanted to gain weight. Thus, underweight men seem to be dissatisfied with their bodies, whereas underweight women seem to be very satisfied (86). Although both men and women desire physical perfection, gaining weight and attaining the ideal body should be achieved through exercise and weight training and not only via diet control (87). However, the idea of achieving the socio-cultural perception of a perfect body, combined with girls’ dissatisfaction with their bodies, can exacerbate inappropriate eating behaviors and increase their risk of developing eating disorders (88). Many individuals with eating disorders are undiagnosed (89) and thus do not receive the necessary support and training. Adolescence is a time when individuals are highly vulnerable psychologically; therefore, it is important to provide the necessary support to enable them to develop into healthy adults. Adolescents require education around perceiving their bodies in a healthy way and how to filter messages in the mass media to prevent negative effects. In a previous study, Posavac et al. (90) observed that female students with a negative self-image who received psycho-educational instruction in media analysis were less likely to make social comparisons and less vulnerable to the negative effects of “thin” images of beauty than students who did not receive such instruction. Individuals with a positive body image tend to filter and reject unrealistic images in the media to protect their body image (91).
The current study has several limitations worth noting. First, the age distribution of our sample was 18–34 years and is thus not representative of the general population; however, body image concerns are a key issue for this population, as eating disorders and associated pathology are common in this age group. In addition, the study design was cross-sectional; therefore, no longitudinal conclusions can be drawn about the relationships between these variables. These variables should be examined in the future using a prospective design to monitor sociocultural attitudes toward appearance and assess perceptions of eating attitude and negative appearance evaluation over time, particularly during the transition from adolescence to middle age. Despite these limitations, the current study provides useful insight into the relationships between eating attitudes, perceptions of one’s own body shape, and the factors associated with this social context in the Chinese population. We found that differing perceptions of external body shape can be effective predictors of eating behavior and social perception. Overall, studies on diet and related body image factors (internalized and perceived body acceptance) should be continued to improve the health of Chinese populations and combat eating disorders and weight-related diseases.
Conclusion
Our results suggest that negative appearance ratings fully mediate the effect between dietary attitudes and sociocultural attitudes toward appearance. An individual’s eating attitudes influence negative body perceptions, which in turn affects the perception of their body shape. Our findings on the specific effects of dietary attitudes on body perception provide a psychological basis to guide and develop interventions on attitudes toward the body. Given the current cultural climate in which women’s and men’s bodies are constantly being objectified and censored, and recognizing the social importance of media (e.g., magazines and advertisements) in determining the ideals of beauty, there is a crucial need to identify the factors that influence individuals’ sociocultural attitudes toward appearance. In addition, studies using diverse age groups may help understand how these issues and behaviors manifest.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Board for Research Projects at the Institute of Psychology, University of Gdańsk, Poland. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HF, ML, MLa, BI, and YY: conceptualization. RW, ML, MLa, and YG: methodology. HF, JL, ML, MLa, BI, and SG: investigation. RW, YG, XW, and HF: writing – original draft preparation. RW, MLa, ML, BI, YG, XW, and HF: writing – review and editing. ML and MLa: supervision. ML: project administration. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by the Fundamental Research Funds for the Central Universities of China (Nos. 2020030 to HF and 20212032 to RW), the Polish National Agency for Academic Exchange under the Urgency Grants program (BPN/GIN/2021/1/00010/U/00001 to ML).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord. (2010) 40:293–309. doi: 10.1002/eat.20369
2. World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 11th ed. (2019). Available online at: https://icd.who.int/ (accessed Septermber 4, 2021).
3. Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. (2006) 19:438–43. doi: 10.1097/01.yco.0000228768.79097.3e
4. Hoek HW, Hoeken DV, Katzman MA. Epidemiology and Cultural Aspects of Eating Disorders. Hoboken, NJ: John Wiley & Sons, Ltd (2016).
5. Chen H, Gao X. The body-image disturbance of college students’ and its influential factors. Health Med Res Pract. (2005) 2:26–9.
6. Izydorczyk B. Body Image in Eating Disorders: Clinical Diagnosis and Integrative Approach to Psychological Treatment. Milton Park: Taylor & Francis (2022). doi: 10.4324/9781003251088
7. Eisenberg ME, Neumark-Sztainer D. Friends’ dieting and disordered eating behaviors among adolescents five years later: findings from project eat. J Adolesc Health. (2010) 47:67–73. doi: 10.1016/j.jadohealth.2009.12.030
8. Haase AM, Prapavessis H, Owens RG. Perfectionism, social physique anxiety and disordered eating: a comparison of male and female elite athletes. Psychol Sport Exerc. (2002) 3:209–22. doi: 10.1016/S1469-0292(01)00018-8
9. Lipowska M, Lipowski M. Narcissism as a moderator of satisfaction with body image in young women with extreme underweight and obesity. PLoS One. (2015) 10:e0126724. doi: 10.1371/journal.pone.0126724
10. Izydorczyk B, Truong Thi Khanh H, Lipowska M, Sitnik-Warchulska K, Liziñczyk S. Psychological risk factors for the development of restrictive and bulimic eating behaviors: a polish and Vietnamese comparison. Nutrients. (2021) 13:910. doi: 10.3390/nu13030910
11. Liu Y, Chen JZ, Jiang M. Psychotherapy for bulimia nervosa. Chin J Clin Psychol. (2013) 3:467–70. doi: 10.16128/j.cnki.1005-3611.2013.03.043
12. Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. (1979) 9:273–9. doi: 10.1017/s0033291700030762
13. Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. (1982) 12:871–8. doi: 10.1017/s0033291700049163
14. Wagner RV, Sherwood JT. The study of attitude change. 2nd ed. In: Zhang ZG, Jin SH editors. Social Psychology. Beijing: People’s Education Press (2008). p. 195–6.
15. Chen QY, Fu DD, Chen W, Wang JP. Influence of self- esteem in eating disorders: the mediation effect of body dissatisfaction. Chin J Clin Psychol. (2007) 15:290–2.
16. Meule A. Interactive effects between flexible and rigid control of eating behavior on body weight: a moderated serial multiple mediation model. Health Psychol Rep. (2017) 5:314–22. doi: 10.5114/hpr.2017.70206
17. Zhang WH, Zhang DR, Qian Y. Psychological characteristics of patients with eating disorders. Chin Ment Health J. (2006) 20:596–9.
18. Tucholska K, Gulla B, Grabowska A, Major P. Time perspective, future anxiety, and hope for success in individuals awaiting bariatric surgery. Health Psychol Rep. (2022) 10. doi: 10.5114/hpr.2021.105259
19. Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. (1982) 12:871–8. doi: 10.1017/S0033291700049163
20. Wang BY, Chen JZ, Liu Y, Liu J, Guo T. Validity and reliability of the Chinese version of the eating attitudes test in Chinese college students. Chin Ment Health J. (2015) 29:150–5.
21. Chen LN. Study of personality characteristics, eating attitudes and coping styles in patients with anorexia nervosa. J Clin Psychosom Dis. (2015) 4:100–3. doi: 10.3969/j.issn.1672-187X.2015.04.033-0097-04
22. Mölbert SC, Thaler A, Mohler BJ, Streuber S, Romero J, Black MJ, et al. Assessing body image in anorexia nervosa using biometric self-avatars in virtual reality: attitudinal components rather than visual body size estimation are distorted. Psychol Med. (2018) 48:642–53. doi: 10.1017/S0033291717002008
23. Voges MM, Giabbiconi CM, Schöne B, Waldorf M, Hartmann AS, Vocks S. Gender differences in body evaluation: do men show more self-serving double standards than women? Front Psychol. (2019) 10:544. doi: 10.3389/fpsyg.2019.00544
24. Hye LJ, Kwon SH. Research on body satisfaction and interest in body image by personality type. Korean Hum Image Design. (2021) 3:59–71.
25. Behrens SC, Meneguzzo P, Favaro A, Teufel M, Skoda E-M, Lindner M, et al. Weight bias and linguistic body representation in anorexia nervosa: findings from the BodyTalk project. Eur Eat Disord Rev. (2021) 29:204–15. doi: 10.1002/erv.2812
26. Mergen J, Keizer A, Koelkebeck K, van den Heuvel MRC, Waner H. Women with anorexia nervosa do not show altered tactile localization compared to healthy controls. Psychiatry Res. (2018) 267:446–54. doi: 10.1016/j.psychres.2018.06.007
27. Su XL. Prevalence of eating disorders, affecting factors and preventive measures. J Environ Hyg. (2008) 35:240–4.
28. Ryan JK. Eating Disorders [EB]. (2019). Available online at: https://ssl.adam.com/content.aspx?productId=10&pid=10&gid=000049&site=slu.adam.com&login=SLUC3551 (accessed Septermber 2, 2021).
29. Chen H, Jackson T, Huang X. The negative physical self-scale: initial development and validation in samples of Chinese adolescents and young adults. Body Image. (2006) 3:401–12. doi: 10.1016/j.bodyim.2006.07.005
30. Thompson JK, Coovert MD, Stormer SM. Body image, social comparison, and eating disturbance: a covariance structure modeling investigation. Int J Eat Disord. (1999) 26:43–51. doi: 10.1002/(sici)1098-108x(199907)26:1<43::aid-eat6>3.0.co;2-r
31. Cooley E, Toray T. Disordered eating in college freshman women: a prospective study. J Am Coll Health. (2001) 49:229–35. doi: 10.1080/07448480109596308
32. Polivy J, Herman CP. Causes of eating disorders. Annu Rev Psychol. (2002) 53:187–213. doi: 10.1146/annurev.psych.53.100901.135103
33. Thompson JK. Exacting beauty: theory, assessment and treatment of body image disturbance. Behav Res Ther. (1998) 23:94. doi: 10.1037/10312-000
34. Leary MR. A brief version of the fear of negative evaluation scale. Pers Soc Psychol Bull. (1983) 9:371–5. doi: 10.1177/0146167283093007
35. Shisslak CM, Crago M. Risk and protective factors in the development of eating disorders. In: Thompson JK, Smolak L editors. Body Image, Eating Disorders, and Obesity in Youth: Assessment, Prevention, and Treatment. Washington, DC: American Psychological Association. (2001). p. 103–125. doi: 10.1037/10404-004
36. Stice E. Risk factors for eating pathology: recent adBances and future directions. In: Striegel-Moore RH, Smolak L editors. Eating Disorders: Innovative Directions in Research and Practice. Washington, DC: American Psychological Association (2001). p. 51–73. doi: 10.1037/10403-003
37. Stefanile C, Nerini A, Matera C, Schaefer LM, Thompson JK. Validation of an italian version of the sociocultural attitudes towards appearance questionnaire-4-revised (sataq-4r) on non-clinical Italian women and men. Body Image. (2019) 31:48–58. doi: 10.1016/j.bodyim.2019.08.005
38. Izydorczyk B, Sitnik-Warchulska K, Liziñczyk S, Lipowska M. Socio-cultural standards promoted by the mass media as predictors of restrictive and bulimic behavior. Front Psychiatry. (2020) 11:506. doi: 10.3389/fpsyt.2020.00506iers
39. Heinberg LJ, Thompson JK, Stormer S. Development and validation of the sociocultural attitudes towards appearance questionnaire. Int J Eat Disord. (1995) 17:81–9. doi: 10.1002/1098-108X(199501)17:1<81::AID-EAT2260170111>3.0.CO;2-Y
40. Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: a synthesis of research findings. J Psychosom Res. (2002) 53:985–93. doi: 10.1016/s0022-3999(02)00488-9
41. Marilou G, Rodgers RF, Henri C. Prospective predictors of body dissatisfaction, drive for thinness, and muscularity concerns among young women in France: a sociocultural model. Body Image. (2018) 26:103. doi: 10.1016/j.bodyim.2018.07.001
42. Knauss C, Paxton SJ, Alsaker FD. Relationships amongst body dissatisfaction, internalisation of the media body ideal and perceived pressure from media in adolescent girls and boys. Body Image. (2007) 4:353–60. doi: 10.1016/j.bodyim.2007.06.007
43. Lovering ME, Rodgers RF, George JE, Franko DL. Exploring the tripartite influence model of body dissatisfaction in postpartum women. Body Image. (2018) 24:44–54. doi: 10.1016/j.bodyim.2017.12.001
44. Shroff H, Thompson JK. Peer influences, body-image dissatisfaction, eating dysfunction and self-esteem in adolescent girls. J Health Psychol. (2006) 11:533–51. doi: 10.1177/1359105306065015
45. Spangler DL, Stice E. Validation of the beliefs about appearance scale. Cogn Ther Res. (2001) 25:813–27.
46. Thompson JK, Berg P, Roehrig M, Guarda AS, Heinberg LJ. The sociocultural attitudes towards appearance scale-3 (sataq-3): development and validation. Int J Eat Disord. (2004) 35:293–304. doi: 10.1002/eat.10257
47. Groesz LM, Levine MP, Murnen SK. The effect of experimental presentation of thin media images on body satisfaction: a meta-analytic review. Int J Eat Disord. (2002) 31:1–16. doi: 10.1002/eat.10005
49. Lundgren JD, Anderson DA, Thompson JK. Fear of negative appearance evaluation: development and evaluation of a new construct for risk factor work in the field of eating disorders. Eat Behav. (2004) 5:75–84. doi: 10.1016/S1471-0153(03)00055-2
50. Striegel-Moore RH, Silberstein LR, Frensch P, Rodin J. A prospective study of disordered eating among college students. Int J Eat Disord. (1989) 8:499–509. doi: 10.1002/1098-108X(198909)8:5<499::AID-EAT2260080502>3.0.CO;2-A
51. Olivardia R, Pope HG, Mangweth B, Hudson JI. Eating disorders in college men. Am J Psychiatry. (1995) 152:1279–85. doi: 10.1037/e328052004-005
52. Rayner KE, Schniering CA, Rapee RM, Hutchinson DM. A longitudinal investigation of perceived friend influence on adolescent girls’ body dissatisfaction and disordered eating. J Clin Child Adolesc Psychol. (2013) 42:643–56. doi: 10.1080/15374416.2012.743103
53. Hutchinson DM, Rapee RM. Do friends share similar body image and eating problems? The role of social networks and peer influences in early adolescence. Behav Res Ther. (2007) 45:1557–77. doi: 10.1016/j.brat.2006.11.007
54. Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull. (2004) 130:19–65. doi: 10.1037/0033-2909.130.1.19
55. Markey CN, Markey PM. Correlates of young women’s interest in obtaining cosmetic surgery. Sex Roles. (2009) 61:158–66. doi: 10.1007/s11199-009-9625-5
56. Dunaev JL, Schulz JL, Markey CN. Cosmetic surgery attitudes among midlife women: appearance esteem, weight esteem, and fear of negative appearance evaluation. J Health Psychol. (2016) 23:59–66. doi: 10.1177/1359105316642249
57. Gestsdottir S, Svansdottir E, Sigurdsson H, Arnarsson A, Ommundsen Y, Arngrimsson S, et al. Different factors associate with body image in adolescence than in emerging adulthood: a gender comparison in a follow-up study. Health Psychol Rep. (2018) 6:81–93. doi: 10.5114/hpr.2018.71201
58. Chrisler J. Leaks, lumps, and lines stigma and women’s bodies. Psychol Women Q. (2011) 35:202–14. doi: 10.1177/0361684310397698
59. Slevec J, Tiggemann M. Attitudes toward cosmetic surgery in middle-aged women: body image, aging anxiety, and the media. Psychol Women Q. (2010) 34:65–74. doi: 10.1111/j.1471-6402.2009.01542.x
60. Lipowska M, Lipowski M, Olszewski H, Dykalska-Bieck D. Gender differences in body-esteem among seniors: beauty and health considerations. Arch Gerontol Geriatr. (2016) 67:160–70. doi: 10.1016/j.archger.2016.08.006
61. Bailey L, Markey CN, Markey PM, August KJ, Nave CS. Understanding same-sex male and female partners’ restrained eating in the context of their relationships. J Health Psychol. (2015) 20:816–27. doi: 10.1177/1359105315573431
62. Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of covid-19 on the mental health in the general population. QJM. (2020) 113:531–7. doi: 10.1093/qjmed/hcaa201
63. Wilczyñska D, Li J, Yang Y, Fan H, Liu T, Lipowski M. Fear of COVID-19 changes the motivation for physical activity participation: polish-Chinese comparisons. Health Psychol Rep. (2021) 9:138–48. doi: 10.5114/hpr.2021.105007
64. Clark Bryan D, Macdonald P, Ambwani S, Cardi V, Rowlands K, Willmott D, et al. Exploring the ways in which covid-19 and lockdown has affected the lives of adult patients with anorexia nervosa and their carers. Eur Eat Disord Rev. (2020) 28:826–35. doi: 10.1002/erv.2762
65. Monteleone AM, Marciello F, Cascino G, Abbate-Daga G, Anselmetti S, Baiano M, et al. The impact of covid-19 lockdown and of the following “re-opening” period on specific and general psychopathology in people with eating disorders: the emergent role of internalizing symptoms. J Affect Disord. (2021) 285:77–83. doi: 10.1016/j.jad.2021.02.037
66. Sharp CW, Clark SA, Dunan JR, Blackwood D, Shapiro CM. Clinical presentation of anorexia nervosa in males: 24 new cases. Int J Eat Disord. (1994) 15:125–34. doi: 10.1002/1098-108X(199403)15:2<125::AID-EAT2260150204>3.0.CO;2-O
67. Mitchell JE, Goff G. Bulimia in male patients. Psychosomatics. (1984) 25:909–13. doi: 10.1016/S0033-3182(84)72923-9
68. Pope HG, Hudson JI, Jonas JM. Bulimia in men: a series of fifteen cases. J Nerv Ment Dis. (1986) 174:117. doi: 10.1097/00005053-198602000-00008
69. Schneider JA, Agras WS. Bulimia in males: a matched comparison with females. Int J Eat Disord. (1987) 6:235–42. doi: 10.1002/1098-108X(198703)6:2<235::AID-EAT2260060207>3.0.CO;2-A
70. Hudson JI, Pope HG, Jonas JM, Yurgelun-Todd D. Phenomenologic relationship of eating disorders to major affective disorder – sciencedirect. Psychiatry Res. (1983) 9:345–54. doi: 10.1016/0165-1781(83)90008-2
71. Keck PE, Pope HG, Hudson JI, Mcelroy SL, Yurgelun-Todd D, Hundert EM. A controlled study of phenomenology and family history in outpatients with bulimia nervosa. Compr Psychiatry. (1990) 31:275–83. doi: 10.1016/0010-440X(90)90034-P
72. Crisp AH, Burns T, Bhat AV. Primary anorexia nervosa in the male and female: a comparison of clinical features and prognosis. Psychol Psychother Theor Res Pract. (1986) 59:123–32. doi: 10.1111/j.2044-8341.1986.tb02676.x
73. Woodside DB, Garner DM, Rockert W, Garfinkel PE. Eating disorders in males: insights from a clinical and psychometric comparison with female patients. In: Andersen AE editor. Males With Eating Disorders. New York, NY: Brunner (1990).
74. Hinrichsen H, Wright F, Waller G, Meyer C. Social anxiety and coping strategies in the eating disorders. Eat Behav. (2003) 4:117–26. doi: 10.1016/S1471-0153(03)00016-3
75. Levinson CA, Rodebaugh TL, White EK, Menatti AR, Weeks JW, Iacovino JM, et al. Social appearance anxiety, perfectionism, and fear of negative evaluation: distinct or shared risk factors for social anxiety and eating disorders? Appetite. (2013) 67:125–33. doi: 10.1016/j.appet.2013.04.002
76. Leung F, Lam S, Sze S. Cultural expectations of thinness in Chinese women. Eat Disord. (2001) 9:339–50. doi: 10.1080/106402601753454903
77. Jackson T, Chen H. Features of objectified body consciousness and sociocultural perspectives as risk factors for disordered eating among late adolescent women and men. J Couns Psychol. (2015) 62:741–52. doi: 10.1037/cou0000096
78. Fredrickson B, Roberts T. Objectification theory. Psychol Women Q. (1997) 21:623–36. doi: 10.1111/j.1471-6402.1997.tb00108.x
79. Stice TE. Thin-ideal internalization: mounting evidence for a new risk factor for body-image disturbance and eating pathology. Curr Dir Psychol Sci. (2001) 10:181–3. doi: 10.1111/1467-8721.00144
80. Smolak L, Thompson JK. Body image, eating disorders, and obesity in youth: assessment, prevention, and treatment. Adolescence. (2009) 44:250–1. doi: 10.1037/11860-000
81. van den Berg P, Paxton SJ, Keery H, Wall M, Guo J, Neumark-Sztainer D. Body dissatisfaction and body comparison with media images in males and females. Body Image. (2007) 4:257–68. doi: 10.1016/j.bodyim.2007.04.003
82. Laporta-Herrero I, Jáuregui-Lobera I, Barajas-Iglesias B, Santed-Germán MÁ. Body dissatisfaction in adolescents with eating disorders. Eat Weight Disord. (2018) 23:339–47. doi: 10.1007/s40519-016-0353-x
83. Furnham A, Badmin N, Sneade I. Body image dissatisfaction: gender differences in eating attitudes, self-esteem, and reasons for exercise. J Psychol Interdiscip Appl. (2002) 136:581–96. doi: 10.1080/00223980209604820
84. Cash TF. The great American shape-up: body-image survey report. Psychol Today. (1986) 20:30–7. doi: 10.1037/e400702009-002
85. Pawłowska A, Lipowska K, Krokosz D. Too masculine for healthcare, too feminine for intense sports: correlation between gender conformity and pro-health behaviours. Baltic J Health Phys Act. (2021) 1(Suppl. 1):29–41. doi: 10.29359/BJHPA.2021.Suppl.1.04
86. Champion H, Furnham A. The effect of the media on body satisfaction in adolescent girls. Eur Eat Disord Rev. (1999) 7:213–28. doi: 10.1002/(SICI)1099-0968(199906)7:3<213::AID-ERV229>3.0.CO;2-W
87. Constaín GA, Ricardo Ramírez C, Rodríguez-Gázquez Mde L, Alvarez Gómez M, Marín Múnera C, Agudelo Acosta C. Diagnostic validity and usefulness of the eating attitudes test-26 for the assessment of eating disorders risk in a Colombian female population. Aten Primaria. (2014) 46:283–9.
88. Posavac HD, Posavac SS, Weigel RG. Reducing the impact of media images on women at risk for body image disturbance: three targeted interventions. Soc Sci Electron Publ. (2005) 20:324–40. doi: 10.1521/jscp.20.3.324.22308
Keywords: sociocultural influence, body image, EAT-26, FNAES, SATAQ 3
Citation: Wang R, Gan Y, Wang X, Li J, Lipowska M, Izydorczyk B, Guo S, Lipowski M, Yang Y and Fan H (2022) The Mediating Effect of Negative Appearance Evaluation on the Relationship Between Eating Attitudes and Sociocultural Attitudes Toward Appearance. Front. Psychiatry 13:776842. doi: 10.3389/fpsyt.2022.776842
Received: 14 September 2021; Accepted: 09 February 2022;
Published: 15 March 2022.
Edited by:
Antoine Bechara, University of Southern California, United StatesReviewed by:
Paolo Meneguzzo, University of Padua, ItalySebastian Lizinczyk, University of Social Sciences and Humanities, Poland
Copyright © 2022 Wang, Gan, Wang, Li, Lipowska, Izydorczyk, Guo, Lipowski, Yang and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongying Fan, ZmFuaHlAYnN1LmVkdS5jbg==; ZmFuX2hvbmd5aW5nQHllYWgubmV0; Mariusz Lipowski, bWFyaXVzei5saXBvd3NraUBhd2YuZ2RhLnBs
 Ruohang Wang
Ruohang Wang Youteng Gan
Youteng Gan Xueyu Wang
Xueyu Wang Jianye Li
Jianye Li Małgorzata Lipowska
Małgorzata Lipowska Bernadetta Izydorczyk
Bernadetta Izydorczyk Shuai Guo
Shuai Guo Mariusz Lipowski
Mariusz Lipowski Yin Yang
Yin Yang Hongying Fan
Hongying Fan