
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry, 28 February 2022
Sec. Schizophrenia
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.768586
This article is part of the Research TopicAutism and Schizophrenia: Neurodevelopmental, Transdiagnostic, Dimensional ConstructsView all 5 articles
 Michele Ribolsi1*
Michele Ribolsi1* Federico Fiori Nastro2,3
Federico Fiori Nastro2,3 Martina Pelle2,3
Martina Pelle2,3 Caterina Medici2,3
Caterina Medici2,3 Silvia Sacchetto2,3
Silvia Sacchetto2,3 Giulia Lisi4
Giulia Lisi4 Assia Riccioni5
Assia Riccioni5 Martina Siracusano6
Martina Siracusano6 Luigi Mazzone5
Luigi Mazzone5 Giorgio Di Lorenzo2,3,7
Giorgio Di Lorenzo2,3,7There is strong evidence for the existence of a high comorbidity between autism and psychosis with percentages reaching up to 34. 8% and several significant implications for treatment and prognosis of these patients. However, the identification of comorbid psychosis in patients with Autism Spectrum Disorder represents a complex challenge from a psychopathological point of view, in particular in patients with greater deficits in verbal communication. Intercepting the onset of a psychotic breakdown in autism may be very difficult, both disorders in fact occur along a phenotypic continuum of clinical severity and in many cases, psychotic symptoms are present in an attenuated form. In this paper, we reviewed the available scientific literature about comorbidity between psychosis and autism, focusing our attention on four specific dimensions: delusions, hallucinations, negative symptoms, and clinical course. The aim of this paper is to provide clinical tools to identify these psychotic phenomena in autistic patients, even when they occur in their attenuated form.
If historically schizophrenia and autism were judged to be closely related (1), subsequently, through epidemiological studies, these two syndromes have been reconsidered as two distinct entities, each with its own characteristics, clinical course, and typical onset (2–6). However, there is a growing number of studies that focus their attention on the link between schizophrenia and autism spectrum disorders (ASD), finding significant overlaps in genetic studies, neuroimaging data, clinical signs, and cognitive features (7–10). There is strong evidence for the existence of high rates of comorbidity between autism and psychosis (11). According to literature, up to 34.8% of the patients with a diagnosis of ASD can show psychotic symptoms and, similarly, autistic traits have been reported in schizophrenia patients (SCZ) in a percentage ranging between 3.6 and 60% (12).
Autism spectrum disorder is composed by different levels of complexity, with frequent comorbidity with intellectual disability (13) and recently, there is growing attention on the behavioral equivalents of schizophrenia in people with intellectual disability and autism spectrum disorder (14).
Both ASD and SCZ occur along a phenotypic continuum of clinical severity and are susceptible to common environmental risk factors such as advanced paternal age, pregnancy and birth complications, migration status (12).
Precisely because of this high comorbidity rate between ASD and SCZ, many authors hypothesized the existence of a significant psychotic vulnerability in patients with neurodevelopmental disorders: in particular, impairments in information processing are common in ASD and may favor the risk for a transition to psychosis (12). The expression of autistic core symptoms may vary significantly among ASD patients and may be influenced by the disorder's age of onset. Moreover, psychotic and autistic subthreshold or attenuated symptoms, can make even more difficult to recognize the two comorbid disorders (11).
In this paper, we analyze from a clinical and phenomenological point of view the occurrence of psychosis or attenuated psychotic symptoms in ASD individuals. In particular, we discuss the clinical presentation of four dimensions that must be considered crucial to recognize psychosis in ASD: (1) delusions, (2) hallucinations, (3) negative symptoms, and (4) clinical course of both disorders.
Delusions are defined as “fixed beliefs that are not amenable to change in light of conflicting evidence” (15). According to Jaspers (16), there are three crucial criteria to define delusions: (1) subjective certainty, incomparable to other convictions; (2) imperviousness to counterarguments; (3) implausibility of content. Hallucination represents “the intimate conviction of actually perceiving a sensation for which there is no external object” (17) while negative symptoms are represented by blunted affect, alogia, asociality, anhedonia, and avolition (18).
We chose these three symptoms to identify the presence of psychosis in autism. Negative symptoms have been considered pivotal symptoms of psychosis since the early description of Kraepelin and Bleuler. On the contrary, delusions and hallucinations may theoretically also be present in non-schizophrenic clinical pictures, for example in mood disorders with psychotic manifestations. However, they are an essential element for the detection of the attenuated psychotic syndrome. Finally, the evaluation of the clinical course represents an anamnestic element that allows distinguishing autism complicated by comorbid psychosis from early-onset psychosis or schizophrenia.
In the conclusion section, we suggested some psychopathological elements useful to detect attenuated psychotic symptoms in ASD subjects.
A systematic review was conducted based on studies published in English databases from January 1, 1970, to August 1, 2021, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
We searched the following English databases: PubMed and SCOPUS.
We used a search strategy based on a combination of the following terms: [(autism) AND (psychosis) OR (schizophrenia) OR (delusions) OR (hallucinations) OR (negative symptoms)] AND [(asperger) AND (psychosis) OR (schizophrenia) OR (delusions) OR (hallucinations) OR (negative symptoms)].
Four independent reviewers screened the literature collected and decided whether a study met the inclusion criteria of the review.
The inclusion criteria were: (1) Time: the systematic review included published articles (without language restrictions) conducted between January 1, 1970, and August 1, 2021; (2) Study participants: we selected papers that studied patients with Schizophrenia Spectrum Disorders and Autism Spectrum Disorders with or without psychotic features; (3) Studies that evaluated the degree of four clinical dimensions: hallucinations, delusions, negative symptoms, and clinical course of both disorders. Theoretical or speculative papers on this topic of high level were included, too.
Delusions are fixed beliefs that are not amenable to change in light of conflicting evidence (15). The false belief is not accounted for by the person's cultural or religious background or his or her level of intelligence (19).
Karl Jaspers in his masterpiece, Allgemeine Psychopathologie (16), proposed three crucial criteria to define delusions: (1) subjective certainty, incomparable to other convictions; (2) imperviousness to counterarguments; (3) implausibility of content. Although it is commonly considered one of the main features of Schizophrenia Spectrum Disorder, delusional beliefs can be recognized in different psychiatric conditions: bipolar disorder, major depressive disorder with psychotic features, neurological and medical disorders like dementia, delirium, or drug intoxication (20), and finally, ASD (21).
The presence of delusional beliefs, suspiciousness, and paranoid ideation (22, 23) in autistic children is reported since the early descriptions of Autism and labeled by different authors as schizophrenia-like states (24), borderline conditions (25–27), or severe disturbances of ego development (28). The most common delusional beliefs in ASD individuals are expansive (29), persecutory and passivity delusions, delusion of reference (30) or delusion of thought insertion and withdrawal (31) and “unusual idea” (32).
In some cases, it is not easy to distinguish between “childish fantasies” and delusional beliefs (33). In this regard, Eugene Bleuler in 1950 explained “autistic thinking” as an infantile wish to avoid unsatisfying realities and replace them with imagination and hallucinations. On the contrary, Michael Rutter (34) claimed that ‘the autistic child has a deficiency of fantasy rather than an excess'. So, according to the authors, the word autism may refer to someone who fantasized excessively or someone who did not fantasize at all (35).
Along this line of research, a central question is whether ASD children are able to distinguish between their subjective perceptions and reality. If we assume that the autistic condition implies an intrinsic difficulty in distinguishing between fantasy and reality, the recognition of a delusion in these patients becomes a very complex psychopathological task (36).
Most reports about ASD children who develop delusional ideas (30, 37) are characterized by at least two features 1984 (38): a sufficient cognitive level and an adequate communicative ability. These are necessary for the children to express their own thoughts and for the clinician for the evaluation of children's delusions. Unfortunately, the majority of autistic children show an important communication deficit, including mutism and intellectual disability (21). In several cases, it is reported how much may be difficult for these patients to describe their delusions and for the clinicians to identify and classify them (30). For this reason, some authors have hypothesized to investigate the presence of delusional ideas also through drawings (36).
However, according to Jaspers' definition of delusions (16), it is not possible to evaluate this clinical phenomenon in non-verbal subjects. As Jaspers reports, “delusion is communicated in judgments.” “Subjective certainty,” one of the three parameters to define a delusion, can only be assessed verbally. In this sense, the search for delusional phenomena should be carried out only in communicative subjects, with a sufficient cognitive level.
Therefore, most studies have focused on the presence of psychotic symptoms in ASD subjects without intellectual disability and with good language skills (39).
People with a diagnosis of ASD have difficulties in interpreting subtle social cues, probably because of a Theory of Mind (ToM) deficit, an impairment in the ability to represent the intentions and beliefs of others (40). Both SCZ and ASD subjects frequently present ToM impairments (41–43).
According to Frith (44), ASD children may never acquire ToM abilities, whereas individuals with schizophrenia may have an intact ability to mentalize until their first breakdown. Other authors suggested that, even if impairments in mentalization are clear in both autism and childhood-onset schizophrenia, there are significant differences between the two clinical groups (45, 46). In particular, it has been shown that high-functioning ASD patients are more impaired in affective ToM (verbal faux-pas test) than SCZ subjects (46).
While some studies found no correlation between ToM abilities and the severity of paranoid beliefs (47, 48), other authors have highlighted a possible different quality between the “autistic” paranoia and the “schizophrenic” paranoia. While in ASD subjects, the delusional beliefs may result from the confusion of not understanding the rules and the coordinates of common social interactions (46), in SCZ patients, delusions originate from the aberrant interpretation of others' mental states (44). Compared to ASD, SCZ subjects present a greater hostility bias and paranoid ideation may be considered as the result of hostile attributions (49).
In this regard, several reports have investigated the role of attributional style in the development of paranoia (48). We know that external attributions for negative events and greater internal attributions for positive events may represent a risk factor for the development of paranoia and persecutory delusions (50).
Compared to SCZ subjects, the link between attributional style, paranoid ideation, and mentalization is more controversial in ASD subjects. According to some studies, there is a specific association between (ToM) deficits and paranoia in both ASD and SCZ people (51). An interesting study showed that Asperger subjects have higher levels of paranoia with lower scores on a measure of ToM, supporting the hypothesis that ToM deficits may predispose to persecutory ideas (47). Surprisingly, the authors found no differences in attributional style between ASD individuals and healthy controls (47).
A certain tendency to perceive oneself as an object of social discrimination, potentially vulnerable to judgment, and control by others has been observed in both SCZ patients (52) and Asperger Syndrome patients (47) (see Table 1).
Hallucination is one of the most relevant symptoms in psychiatry. According to Esquirol, hallucination is “the intimate conviction of actually perceiving a sensation for which there is no external object” (17). Hallucinations, in particular the auditory ones, have been closely linked to schizophrenia (53) and constitute one of the 5 key symptoms of criterion A for the diagnosis of schizophrenia according to DSM-5 (15). Hallucinations have been described also in other psychiatric and medical conditions, drugs or alcohol abuse, and non-clinical people (54). ASD individuals often experience, describe, and exhibit unusual patterns of sensation and, according to DSM 5, sensory anomalies are a core symptom for a diagnosis of ASD (15). However, in clinical practice, it is di?cult to discern between sensory issues presenting in ASD individuals and hallucinations, with significant implications for treatment, prognosis and access to services (55).
Findings from standardized parent questionnaires indicate that up to 95% of individuals with ASD show high frequencies of sensory behaviors compared to non-ASD controls (56). With the expression “sensory behavior” we refer to: (a) over-responsivity (exaggerated, rapid onset, and/or prolonged reactions); (b) under-responsivity (unawareness or slow response) to sensory input; (c) seeking behavior, i.e., craving of, and interest in sensory experiences that are prolonged or intense) (57–59).
Interestingly, the frequency of sensory behaviors reported from parents and caregivers seems to vary across age groups and to be linked to mental age.
A meta-analysis from Ben-Sasson (56) shows an increase in sensory behaviors up to age 6–9 years, and a decrease thereafter, compared to non-autistic children. Authors speculate that these symptoms may become more expressed during school age since children typically have to face an increasing demand for independence and the complication of social and physical environment. A true increase of symptoms can, moreover, be reported in the same phase (56). The impact of IQ level on sensory symptoms in autistic people is not clear. Baranek (58) found that sensory symptoms reported by caregivers were negatively related to mental age. A possible explanation is that caregivers may likely underestimate sensory processing problems in children with autism who are less verbally competent (58). In an article by Leekam et al. (60), no significant difference was reported between high functioning and low functioning individuals while other studies have highlighted more total sensory symptoms in younger and lower IQ individuals than older and higher IQ ones (60).
ASD patients frequently suffer from “anomalous perceptual experiences” (APEs) compared to normal controls (61, 62). For example, perceptions of sounds without a visible source are commonly reported, such as hearing a train 5–10 min before it passes or hearing sounds all around (63, 64).
APEs refer to perceptual and hallucinatory experiences and they are similar to the clinical phenomena commonly associated with psychosis (voices, perceptual distortions, “out-of-body” experiences) (62). Like psychotic patients, ASD patients describe these experiences as intrusive and stressful (62).
Despite being reported also in very young children with ASD (56), first-hand descriptions of APEs have usually been given by high-functioning adults (63, 64), scarce information is available about the nature of perception determining abnormal behaviors in younger and low-functioning subjects.
ASD people reveal that these experiences can be very disturbing or frightening and can impact their daily life and social functioning. Sometimes, ASD individuals are aware that their sensory-perceptual experiences are different from those of non-autistic individuals (64). In this regard, it must be specified that APEs need to be considered psychotic phenomena only if they're interpreted in a delusional way by ASD patients or if their source is attributed to the outside world.
Describing proper sensory processing might be difficult for autistic patients, mainly because of their deficits in verbal communication and their language impairment (65). As concretism can be present, investigating hallucinations in a person with ASD can result in confounding answers [e.g., “Do you hear voices when no one is there?” “Yes (on the radio)”] (66). What is more, the patients can describe their somatic complaints in unusual ways: a patient who was suffering from headache described his condition saying that “his head was bleeding” (55).
Symptoms misdiagnosed as psychotic, when considered in the context of the developmental disorder, could be better understood as part of it more than the signal of a co-occurring psychosis (55, 67). Given the deficit of language and communication, emotional recognition, social reciprocity, stereotypic interest, theory of mind, and central coherence, Dossetor (67) claims that reliability in this clinical group can be a serious problem in distinguishing true hallucinations from imagination, memories, illusions, and pseudo-hallucinations.
Autistic children reporting “verbal hallucinations,” sometimes have difficulties in recognizing whether they hear their own voice or that of another person and often aren't able to report the specific words or sentences that the voices might be saying (55, 67). For example, a child described auditory hallucinations that sometimes told him to kill himself or other people and that tend to worsen when he felt under stress: a better assessment suggested that he was not truly psychotic but was having pseudo-hallucinations. With therapeutic (not pharmacologic) intervention, he started to recognize that these voices were from his imagination and started to consider them less frightening until they disappeared (67).
For both Van Schalkwyk et al. (55) and Dossetor (67) it is remarkable that these peculiar symptoms in autistic children tend to improve when interventions to manage anxiety and reduce stressful situations are provided, while few or no improvement can be seen when antipsychotic medications are started. On the contrary, authors would consider the existence of a condition of comorbidity when a more abrupt onset of sustained auditory hallucinations and disorganized behavior is noticed and this symptom represents a marked worsening from baseline; moreover, prognosis depends more on the use of antipsychotic medications, than on changes in structure or environmental factors (55).
Negative symptoms are represented by blunted affect, alogia, asociality, anhedonia, and avolition (18).
They are difficult to assess (68); Andreasen (69–72), they poorly respond to antipsychotics (73, 74), and they are associated with poor functional outcome (75, 76).
Unlike hallucinations and delusions, which are transdiagnostic symptoms, negative symptoms represent a core feature of psychosis and may only be present in schizophrenia or schizoaffective disorder. This is the reason why the history of negative symptoms is sharply related to the history of “Schizophrenia.”
Even before Morel coined the term “Dementia Praecox” (1845), in 1809 John Haslam (77) described a kind of disorder occurring in youth, characterized by “considerably blunted sensibility”: “they do not bear the same affection towards their parents and relations,” “they become unfeeling to kindness and careless to reproof.” Later, Emil Kraepelin (78) identified a broad panel of abnormalities referred to attention, thought, language, volition, and affect that might occur in most but not all patients. Kraepelin's term “Verblödung” corresponds to affective “flattening” or “blunting” rather than to intellectual dementia (79).
In 1911, Bleuler (1) identified “pathognomonic” symptoms for SCZ, these symptoms have to be present in each patient with SCZ and they are also known as Bleuler 4 As': disturbances of affect, associations, ambivalence, and autism. A Bleuler's student, Eugen Minkowski, introduced the “loss of contact with reality” as a key point of schizophrenia and proposed the distinction between two types of schizophrenic autism: “rich or florid autism” (autisme riche) and “poor autism” (autisme pauvre), which was characterized by affective and cognitive “poverty” (80).
At the same time, in France, Dide and Giraud introduced the concept of Athymhormia, from Greek Thimòs “the emotion and affect” and Ormào “the vital force” (81). They considered the loss of vitality and affectivity (“perte de l'élan vital et de l'affectivité”) as necessary and sufficient elements to characterize schizophrenia.
The dichotomy between positive and negative symptoms kept being enriched thanks to further research proposed by Jackson et al. (82), Crow et al. (83), Crow (84, 85), Andreasen and Olsen (86), and Andreasen (87). Moreover, in the late 1980s, renewing Kraepelin's description of schizophrenia's “fundamental processes,” W.T. Carpenter hypothesized a new refined terminology differentiating negative symptoms in Deficit and Non-Deficit symptoms. Deficit symptoms are primary, they are enduring traits that persist during and between the periods of positive symptoms exacerbation (88). Consequently, Carpenter proposed a new schizophrenia subtype called “Deficit Syndrome” when primary negative symptoms are prominent. Recently a new and revived interest in Negative Symptoms has occurred in order to solve unanswered questions regarding pathophysiology and outcome of schizophrenia (89–91).
Similarities between autism and schizophrenia were recognized since the time of Bleuler and Kanner (92). Only from the early 1970s they have been conceptualized as two distinct disorders (34, 93).
Therefore, differentiating schizophrenia negative symptoms from autistic symptoms represents a pivotal but complicated task even for expert psychiatrists (94, 95).
For example, both social interaction and social communication deficits are frequent in schizophrenia patients as a result of their negative symptoms; at the same time, these are considered key clinical symptoms in ASD (96).
Moreover, the lack of emotional reciprocity in ASD can be confused with the “blunted” affect in schizophrenia.
On one hand, for what concerns “emotional reciprocity,” it is a diagnostic criterion for ASD. Nonetheless, DSM 5 does not precisely explain what reciprocity means, but it only provides anecdotal descriptions such as “not actively participating in simple social play or games,” “preferring solitary activities,” or “involving others in activities only as tools or “mechanical” aid”' (97). ICD-10 illustrated the correspondent diagnostic criteria as follows: “inadequate appreciation of socio-emotional cues, as shown by a lack of responses to other people's emotions and/or a lack of modulation of behaviour according to social context and, especially, a lack of socio-emotional reciprocity” (98).
On the other hand, blunted affect is defined as a “decrease in the expression of emotion and reactivity to events as observed during the spontaneous or elicited expression of emotion (facial and vocal expression and expressive gestures)” (18) and it manifests itself as a characteristic impoverishment of emotional expression, reactivity, and feeling (86).
According to us, to better differentiate these two concepts, it can be hypothesized that ASD subjects can present “poverty in reciprocity” (which can be similar to the “decrease in the expression of emotion and reactivity” of affective flattening) but also an inappropriateness of reciprocity (which is more typical of autism).
Furthermore, also restricted and repetitive behaviors in ASD can be easily misunderstood as a symptom of schizophrenia (99), even if a recent study reported that, in psychosis, a pervasive involvement in special interests or repetitive behaviors is much less common (100).
Restricted and repetitive behaviors might also be present in the co-occurrence of schizophrenia and obsessive-compulsive disorder (OCD); according to a recent review (101) around 30% of patients with SCZ display obsessive-compulsive symptoms (OCSs). What is more, OCSs are considered an identification criterion of an at-risk mental state according to the Comprehensive Assessment of At-Risk Mental State (CAARMS) (102).
Some considerations may help in differentiating these symptoms in Autism and Schizophrenia:
-while in ASD patients, OCSs are present from early childhood (1–3 years of life), in psychotic patients OCSs make their first appearance usually in adolescence (this is the reason why the CAARMS has introduced OCSs in the evaluation of the at-risk mental states).
-while repetitive behaviors in autistic patients are usually a-finalistics, in psychotic patients they may be linked to the prevalent ideation, sometimes of delusional intensity.
The clinical course represents a key element for the differential diagnosis between autism and psychosis.
The natural course of SCZ is extremely heterogeneous and generally considered unpredictable (103). The onset of SCZ is usually between the late adolescence and the mid-30s (96) and it follows a prodromal state in which social impairment, atypical interests and unusual beliefs have already occurred. Onset before adolescence is rare (104).
By contrast, ASD is an early onset (12–24 months of age) lifelong condition characterized by persistent deficits in social communication, as well as restricted and repetitive patterns of behavior (96).
Many parents are concerned about affected children's development by age 1, but most of them are worried by age 2 (105). In a minority of cases, about 20%, parents report some period of normal development followed by loss of skills. The clinical significance of regression continues to be debated (106, 107).
A relevant clinical problem is the distinction between autism and childhood-onset schizophrenia (COS) (108).
Childhood-onset schizophrenia (COS) is a rare, chronic mental illness that is diagnosed in children before 13 years of age (109). Children with COS often show premorbid disturbances in social, motor, and language domains with comorbid learning disabilities and mood or anxiety disorders (110).
Additionally, almost one-third of patients meet the criteria for ASD before the onset of COS (111). The outcome of COS is influenced by the presence and severity of these mentioned developmental abnormalities (112) and a few studies suggested that the severity of these deficits may represent a premorbid phenotype for COS (113).
How often a premorbid COS is sufficiently severe to be confused with ASD during childhood?
Diagnostic difficulties are more common in the early phase of these disorders when symptoms are less distinguished.
One of the key difficulties in differentiating COS and ASD is to disentangle true psychotic hallucinations and delusions from the child's imaginative play (114, 115). For example, having imaginary friends is a common situation for children which may be mistaken for psychosis. Similarly, the expressing of children with poor or underdeveloped language skills may be confused with the disorganized thought of SCZ (114).
ASD diagnoses have been reported in COS, in particular we refer to Pervasive Development Disorder Not Otherwise Specified (PDD-NOS) (111) or Multiple Complex Developmental Disorder (MCDD) (99, 116–118).
In a clinical case reported by Hatila and Solanki (119), the patient (an Indian 26 years old male) was diagnosed with ASD (DSM-IV-TR criteria) at the age of 4. Then, at the age of 6, he was sent to a special school, from which he was later withdrawn due to aggressive behavior. In adolescence, he presented with unprovoked aggressive behavior, hallucinatory behavior, irrelevant talk and disturbed sleep. A diagnosis of paranoid schizophrenia comorbid with ASD was performed. In this case, there was a history of birth insult, which is underestimated as a possible risk factor for both ASD and SCZ (119).
Keller et al. (120) proposed to operate a differential diagnosis between psychotic disorders and ASD. The key points are the following:
1. the investigation in the early years of some typical traits like interaction and communication difficulties, stereotyped behaviors, selective interests, and the sensorial alteration typical of ASD;
2. the evaluation of the psychotic symptoms within their context of appearance and the search for the cause of these symptoms in a literal reading of the external reality, typical of the ASD;
3. the evaluation of the symptoms typical of schizophrenia, in particular Schneider's first-rank symptoms (e.g., thoughts echoes, sounds coming from thoughts, hearing voices under the form of dialogues and replies to patient questions, hearing voices that accompany the patient's actions, diffusions of the thoughts, delirious perception, and tendency to follow impulses).
If the recognition of psychotic symptoms in ASD patients is, by itself, a psychopathological challenge, the detection of attenuated psychotic symptoms in ASD adolescents is an even more complex task, because of the existing overlap between autistic symptoms and subclinical psychotic symptoms.
According to the North American Prodrome Longitudinal Study, 2.6% of young individuals at clinical high risk for psychosis (CHR) present a comorbid developmental disorder (121).
ASD, CHR, and First Episode Psychosis (FEP) share developmental impairments in communication and social functioning, FEP and CHR can be considered in an imaginary midway between healthy subjects and ASD for what concerns the impairments related to social communication and awareness (122).
Furthermore, correlations between autistic symptoms and schizotypal traits (referential thinking, paranoid thinking, constricted affect, social affect, odd speech, eccentric behavior) have been found in individuals with ASD (99, 123). From this perspective, ASD patients will frequently match UHR trait risk factors.
A recent study compared baseline characteristics, clinical profiles, and conversion to psychosis outcomes between young individuals at clinical high risk for psychosis (CHR) who presented with or without a prior ASD diagnosis during the second phase of the North American Prodrome Longitudinal Study (124). However, positive symptoms and all other negative symptoms appear quite similar in individuals with CHR with and without comorbid ASD. Secondly, individuals with ASD do not show a higher risk for converting to psychosis, when compared to other individuals with CHR (124).
Currently, the evaluation of attenuated psychotic symptoms in autistic patients is usually performed using the same tools available for non-ASD patients.
In our opinion, this aspect needs to be discussed more in detail for several clinical reasons.
Firstly, the “level 3” of the “unusual thought of content” dimension of the Scale of Prodromal Symptoms (SOPS) stands for a moderate intensity and it is the “threshold” severity level for an attenuated psychotic symptom. It is described as: “Unanticipated mental events/beliefs that cannot be dismissed and are also irritating and/or worrisome. A sense that unexpected experiences are somehow meaningful because they won't go away.”
It is not easy from a clinical point of view, for a psychiatrist, to understand whether an ASD patient is able to recognize whether a mental event/belief is “unanticipated” or not. Likewise, it is sometimes difficult to define whether, and in what way, a mental event may be meaningful for an ASD patient.
ASD patients may find it difficult to understand their own mental states and to explain whether certain mental events or beliefs are unanticipated or not; they will not easily be able to describe if these mental events or beliefs happen to acquire a more intense meaning, a necessary precondition for the building of a delusion.
In this sense, the extension “tout court” to ASD patients of the classic tools used for the investigation of at risk mental states (SIPS / SOPS, CAARMS) can be controversial.
We must consider the possibility that the investigation of the presence of attenuated psychotic symptoms should be evaluated within a more global assessment of the subject's autistic psychopathology.
An attenuated psychotic symptom cannot be “added” or removed from a patient's symptom framework as if it was an object. As Parnas argues, psychotic symptoms “are subjected to the processes of conceptualization and verbalization, both embedded in the interpersonal context of the psychiatric interview” (125). The interpersonal context between a psychiatrist and an ASD adolescent is very different from the one with healthy help-seeking adolescents.
The recognition of psychosis in patients with ASD represents a complex psychopathological challenge.
In Table 2, we have summarized the basic differences between ASD and SCZ patients for the detection of delusions, hallucinations, and negative symptoms.
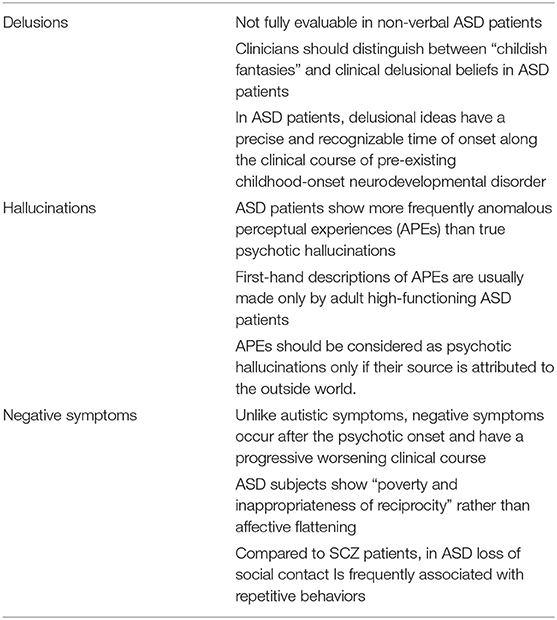
Table 2. Basic differences between ASD and SCZ patients for the detection of delusions, hallucinations, and negative symptoms.
The term “psychosis” has various definitions. Generally, this term refers to a “loss of contact from reality” (NHS).
For Minkowski autism is an expression of the loss of vital contact with reality and represents the fundamental psychopathological disturbance in schizophrenia (80).
The modern definition of autism essentially consists of two clinical aspects: (1) persistent deficit in social communication and social interaction and (2) patterns of restricted, repetitive behavior, interests, or activities. Rather than a loss of contact with reality, in ASD patients we observe a loss of social contact, or a form of social detachment (126).
Recognizing a “loss of contact with reality” (psychosis) in patients suffering from a form of social detachment (autism) can be very complex.
The correct identification of the three fundamental dimensions of psychosis (Delusion, Hallucinations, Negative Symptoms) and an evaluation of the clinical course of the two disorders may be useful to recognize psychotic comorbidity in patients with ASD.
The identification of delusional, hallucinatory, or negative symptoms, is not easy in patients as complex as patients with ASD.
Recognizing the pathway that leads to a delusion, therefore the moment of its onset, the phases preceding the definition of the delusional construction, etc., may be very complex in ASD patients. While in healthy subjects, the construction of a delusion occurs through a clear rupture with the usual meanings that the patient gives to external reality, in ASD patients it is necessary to recognize this same moment along with a pre-existing impairment in social interaction.
For what concerns the evaluation of psychotic comorbidity in ASD patients, a central issue definitely is the identification of attenuated psychotic symptoms during the transition phase, from adolescence to adulthood. Not surprisingly, there is a growing literature on this topic. To recognize attenuated psychotic symptoms in these patients is essential to prevent or treat earlier the development of psychotic comorbidity.
Foss-Feig et al. (124) show a similar level of core psychotic symptoms in ASD + UHR patients and in the so-called “normotypical” UHR patients. The authors conclude that “baseline psychosis symptoms, predictors of risk for conversion, and ultimate conversion rates are similar in patients with Clinical High Risk with and without ASD.”
In our opinion, these findings need to be confirmed in larger studies.
It would be useful to verify whether there are autistic symptoms within the spectrum, that are associated with a greater risk of conversion to psychosis. The great heterogeneity of the clinical manifestations within the autistic spectrum does not allow universal conclusions to be drawn.
Similarly, the different quality of psychotic symptoms in autistic patients compared to healthy subjects should be studied in depth.
For example, due to the lower hostility bias and the reduced tendency to external attribution of ASD patients compared to psychotic subjects, a lower amount of persecutory delusions should be expected. Likewise, it is necessary to investigate which role concretism plays in ASD patients for what concerns psychotic development.
We hypothesize that the assessment of psychotic risk should be carried out with highly refined diagnostic tools and within the clinical history of the autistic subject.
In this sense, the “tout court” extension of the classic tools for UHR assessment (SIPS/SOPS, CAARMS) deserves further studies.
The tools used so far for the assessment of self-disorders (Examination of Anomalous Self-Experience, EASE) could play a crucial role since they allow the identification of core symptoms of psychosis. A clinical tool, able to recognize the rupture of the ego boundaries and, consequently, the clinical manifestations of the self-disorders within the clinical history of an ASD subject, could certainly be more refined than a tool that allows the identification of an isolated single symptom, for example, an isolated or recurring hallucinatory experience. A psychotic phenomenon, delusional, or hallucinatory, has a more solid clinical value if this is contextualized within the framework of the ego experience disorders. There is still a long way to go.
MR, FF, MP, CM, LM, and GD contributed to study the literature on the topic and wrote the paper. GL, MS, and AR contributed to study the literature on the topic and supervised the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
3. Konstantareas MM, Hewitt T. Autistic disorder and schizophrenia: diagnostic overlaps. J Autism Dev Disord. (2001) 31:19–28. doi: 10.1023/A:1005605528309
4. Kastner A, Begemann M, Michel TM, Everts S, Stepniak B, Bach C, et al. Autism beyond diagnostic categories: characterization of autistic phenotypes in schizophrenia. BMC Psychiatry. (2015) 15:115. doi: 10.1186/s12888-015-0494-x
5. Crespi BJ. Revisiting Bleuler: relationship between autism and schizophrenia. Br J Psychiatry. (2010) 196:495. doi: 10.1192/bjp.196.6.495
6. Parnas J, Bovet P. Autism in schizophrenia revisited. Compr Psychiatry. (1991) 32:7–21. doi: 10.1016/0010-440X(91)90065-K
7. Volkmar FR, McPartland JC. From Kanner to DSM-5: autism as an evolving diagnostic concept. Annu Rev Clin Psychol. (2014) 10:193–212. doi: 10.1146/annurev-clinpsy-032813-153710
8. Skokauskas N, Gallagher L. Psychosis, affective disorders and anxiety in autistic spectrum disorder: prevalence and nosological considerations. Psychopathology. (2010) 43:8–16. doi: 10.1159/000255958
9. de Lacy N, King BH. Revisiting the relationship between autism and schizophrenia: toward an integrated neurobiology. Annu Rev Clin Psychol. (2013) 9:555–87. doi: 10.1146/annurev-clinpsy-050212-185627
10. Deste G, Barlati S, Gregorelli M, Lisoni J, Turrina C, Valsecchi P, et al. Looking through autistic features in schizophrenia using the PANSS Autism Severity Score (PAUSS). Psychiatry Res. (2018) 270:764–8. doi: 10.1016/j.psychres.2018.10.074
11. Kincaid DL, Doris M, Shannon C, Mulholland C. What is the prevalence of autism spectrum disorder and ASD traits in psychosis? A systematic review. Psychiatry Res. (2017) 250:99–105. doi: 10.1016/j.psychres.2017.01.017
12. Chisholm K, Lin A, Abu-Akel A, Wood SJ. The association between autism and schizophrenia spectrum disorders: a review of eight alternate models of co-occurrence. Neurosci Biobehav R. (2015) 55:173–83. doi: 10.1016/j.neubiorev.2015.04.012
13. Mazza M, Pino MC, Keller R, Vagnetti R, Attanasio M, Filocamo A, et al. Qualitative differences in attribution of mental states to other people in autism and schizophrenia: what are the tools for differential diagnosis? J Autism Dev Disord. (2021) 52:1283–98. doi: 10.1007/s10803-021-05035-3
14. Bakken TL. Behavioural equivalents of schizophrenia in people with intellectual disability and autism spectrum disorder: A selective review. Int J Dev Disabil. (2021) 67:310–7. doi: 10.1080/20473869.2021.1925402
15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Dsm-5. American Psychiatric Publishing, Incorporated (2013). doi: 10.1176/appi.books.9780890425596
17. Esquirol E, Hunt EK. Mental Maladies; A Treatise on Insanity Philadelphia: Lea and Blanchard (1845). doi: 10.1097/00000441-184507000-00020
18. Kirkpatrick B, Fenton WS, Carpenter WT. Jr. , Marder SR The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. (2006) 32:214–9. doi: 10.1093/schbul/sbj053
19. Kiran C, Chaudhury S. Understanding delusions. Ind Psychiatry J. (2009) 18:3–18. doi: 10.4103/0972-6748.57851
20. Bebbington P, Freeman D. Transdiagnostic extension of delusions: schizophrenia and beyond. Schizophr Bull. (2017) 43:273–82. doi: 10.1093/schbul/sbw191
21. Dykens E, Volkmar F, Glick M. Though disorder in high-functioning autistic adults. J Autism Dev Disord. (1991) 21:291–301. doi: 10.1007/BF02207326
22. Darr GC, Worden FG. Case report twenty-eight years after an infantile autistic disorder. Am J Orthopsychiatry. (1951) 21:559–70. doi: 10.1111/j.1939-0025.1951.tb00012.x
23. Wolff S, Barlow A. Schizoid personality in childhood: a comparative study of schizoid, autistic and normal children. J Child Psychol Psychiatry. (1979) 20:29–46. doi: 10.1111/j.1469-7610.1979.tb01704.x
24. Mahler MS, Ross JR Jr, De Fries Z. Clinical studies in benign and malignant cases of childhood psychosis (schizophrenia-like). Am J Orthopsychiatry. (1949) 19:295–305. doi: 10.1111/j.1939-0025.1949.tb05149.x
25. Ekstein R, Wallerstein J. Observations on the psychotherapy of borderline and psychotic children. Psychoanal Study Child. (1956) 11:303–11. doi: 10.1080/00797308.1956.11822790
26. Geleerd ER. Borderline states in childhood and adolescence. Psychoanal Study Child. (1958) 13:279–95. doi: 10.1080/00797308.1958.11823183
27. Singer MB. Fantasies of a borderline patient. Psychoanal Study Child. (1960) 15:310–56. doi: 10.1080/00797308.1960.11822581
28. Weil AP. Certain severe disturbances of EGO development in childhood. Psychoanal Study Child. (1953) 8:271–87. doi: 10.1080/00797308.1953.11822772
29. Abell F, Hare DJ. An experimental investigation of the phenomenology of delusional beliefs in people with Asperger syndrome. Autism. (2005) 9:515–31. doi: 10.1177/1362361305057857
30. Clarke D, Baxter M, Perry D, Prasher V. The diagnosis of affective and psychotic disorders in adults with autism: seven case reports. Autism. (1999) 3:149–64. doi: 10.1177/1362361399003002005
31. Tantam D. Asperger Syndrome in Adulthood. Autism and Asperger syndrome. New York, NY: Cambridge University Press (1991). p. 147–83. doi: 10.1017/CBO9780511526770.005
32. Szatmari P. Asperger's syndrome: diagnosis, treatment, and outcome. Psychiatr Clin North Am. (1991) 14:81–93. doi: 10.1016/S0193-953X(18)30326-5
33. Rutter M, Lockyer L. five to fifteen year follow-up study of infantile psychosis. I Description of sample. Br J Psychiatry. (1967) 113:1169–82. doi: 10.1192/bjp.113.504.1169
34. Rutter M. Childhood schizophrenia reconsidered. J Autism Child Schizophr. (1972) 2:315–37. doi: 10.1007/BF01537622
35. Evans B. How autism became autism: the radical transformation of a central concept of child development in Britain. Hist Human Sci. (2013) 26:3–31. doi: 10.1177/0952695113484320
36. Bisagni F. Delusional development in child autism at the onset of puberty: vicissitudes of psychic dimensionality between disintegration and development. Int J Psychoanal. (2012) 93:667–92. doi: 10.1111/j.1745-8315.2012.00596.x
37. Gillberg C. Asperger's syndrome and recurrent psychosis–a case study. J Autism Dev Disord. (1985) 15:389–97. doi: 10.1007/BF01531783
38. Petty LK, Ornitz EM, Michelman JD, Zimmerman EG. Autistic children who become schizophrenic. Arch Gen Psychiatry. (1984) 41:129–35. doi: 10.1001/archpsyc.1984.01790130023003
39. Volkmar FR, Cohen DJ, Paul R. An evaluation of DSM-III criteria for infantile autism. J Am Acad Child Psychiatry. (1986) 25:190–7. doi: 10.1016/S0002-7138(09)60226-0
40. Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind” ? Cognition. (1985) 21:37–46. doi: 10.1016/0010-0277(85)90022-8
41. Bora E, Yucel M, Pantelis C. Theory of mind impairment in schizophrenia: meta-analysis. Schizophr Res. (2009) 109:1–9. doi: 10.1016/j.schres.2008.12.020
42. Chung YS, Barch D, Strube M. A meta-analysis of mentalizing impairments in adults with schizophrenia and autism spectrum disorder. Schizophr Bull. (2014) 40:602–16. doi: 10.1093/schbul/sbt048
43. Bliksted V, Videbech P, Fagerlund B, Frith C. The effect of positive symptoms on social cognition in first-episode schizophrenia is modified by the presence of negative symptoms. Neuropsychology. (2017) 31:209–19. doi: 10.1037/neu0000309
44. Frith CD. The Cognitive Neuropsychology of Schizophrenia: Classic Edition. Psychology Press (2015). doi: 10.4324/9781315785011
45. Pilowsky T, Yirmiya N, Arbelle S, Mozes T. Theory of mind abilities of children with schizophrenia, children with autism, and normally developing children. Schizophr Res. (2000) 42:145–55. doi: 10.1016/S0920-9964(99)00101-2
46. Tin LNW, Lui SSY, Ho KKY, Hung KSY, Wang Y, Yeung HKH, et al. High-functioning autism patients share similar but more severe impairments in verbal theory of mind than schizophrenia patients. Psychol Med. (2018) 48:1264–73. doi: 10.1017/S0033291717002690
47. Blackshaw AJ, Kinderman P, Hare DJ, Hatton C. Theory of mind, causal attribution and paranoia in Asperger syndrome. Autism. (2001) 5:147–63. doi: 10.1177/1362361301005002005
48. Craig JS, Hatton C, Craig FB, Bentall RP. Persecutory beliefs, attributions and theory of mind: comparison of patients with paranoid delusions, Asperger's syndrome and healthy controls. Schizophr Res. (2004) 69:29–33. doi: 10.1016/S0920-9964(03)00154-3
49. Pinkham AE, Harvey PD, Penn DL. Paranoid individuals with schizophrenia show greater social cognitive bias and worse social functioning than non-paranoid individuals with schizophrenia. Schizophr Res Cogn. (2016) 3:33–8. doi: 10.1016/j.scog.2015.11.002
50. Kaney S, Bentall RP. Persecutory delusions and attributional style. Br J Med Psychol. (1989) 62(Pt 2):191–8. doi: 10.1111/j.2044-8341.1989.tb02826.x
51. Corcoran R, Mercer G, Frith CD. Schizophrenia, symptomatology and social inference - investigating theory of mind in people with schizophrenia. Schizophr Res. (1995) 17:5–13. doi: 10.1016/0920-9964(95)00024-G
52. Smari J, Stefansson S, Thorgilsson H. Paranoia, self-consciousness, and social cognition in schizophrenics. Cognitive Ther Res. (1994) 18:387–99. doi: 10.1007/BF02357512
54. Waters F, Fernyhough C. Hallucinations: a systematic review of points of similarity and difference across diagnostic classes. Schizophr Bull. (2017) 43:32–43. doi: 10.1093/schbul/sbw132
55. Van Schalkwyk GI, Peluso F, Qayyum Z, McPartland JC, Volkmar FR. Varieties of misdiagnosis in ASD: an illustrative case series. J Autism Dev Disord. (2015) 45:911–8. doi: 10.1007/s10803-014-2239-y
56. Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E, et al. A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. J Autism Dev Disord. (2009) 39:1–11. doi: 10.1007/s10803-008-0593-3
57. Baker AE, Lane A, Angley MT, Young RL. The relationship between sensory processing patterns and behavioural responsiveness in autistic disorder: a pilot study. J Autism Dev Disord. (2008) 38:867–75. doi: 10.1007/s10803-007-0459-0
58. Baranek GT, David FJ, Poe MD, Stone WL, Watson LR. Sensory Experiences Questionnaire: discriminating sensory features in young children with autism, developmental delays, and typical development. J Child Psychol Psychiatry. (2006) 47:591–601. doi: 10.1111/j.1469-7610.2005.01546.x
59. Tomchek SD, Dunn W. Sensory processing in children with and without autism: a comparative study using the short sensory profile. Am J Occup Ther. (2007) 61:190–200. doi: 10.5014/ajot.61.2.190
60. Leekam SR, Nieto C, Libby SJ, Wing L, Gould J. Describing the sensory abnormalities of children and adults with autism. J Autism Dev Disord. (2007) 37:894–910. doi: 10.1007/s10803-006-0218-7
61. Horder J, Wilson CE, Mendez MA, Murphy DG. Autistic traits and abnormal sensory experiences in adults. J Autism Dev Disord. (2014) 44:1461–9. doi: 10.1007/s10803-013-2012-7
62. Milne E, Dickinson A, Smith R. Adults with autism spectrum conditions experience increased levels of anomalous perception. PLoS ONE. (2017) 12:e0177804. doi: 10.1371/journal.pone.0177804
63. Cesaroni L, Garber M. Exploring the experience of autism through firsthand accounts. J Autism Dev Disord. (1991) 21:303–13. doi: 10.1007/BF02207327
64. Jones RSP, Quigney C, Huws JC. First-hand accounts of sensory perceptual experiences in autism: a qualitative analysis. J Intellect Dev Dis. (2003) 28:112–21. doi: 10.1080/1366825031000147058
65. Kjelgaard MM, Tager-Flusberg H. An investigation of language impairment in autism: implications for genetic subgroups. Lang Cogn Process. (2001) 16:287–308. doi: 10.1080/01690960042000058
66. Fogler J, Kuhn J, Prock L, Radesky J, Gonzalez-Heydrich J. Diagnostic uncertainty in a complex young man: autism versus psychosis. J Dev Behav Pediatr. (2019) 40:72–4. doi: 10.1097/DBP.0000000000000635
67. Dossetor DR. 'All that glitters is not gold': misdiagnosis of psychosis in pervasive developmental disorders–a case series. Clin Child Psychol Psychiatry. (2007) 12:537–48. doi: 10.1177/1359104507078476
68. Carpenter WT J, Heinrichs DW, Alphs LD. Treatment of negative symptoms. Schizophr Bull. (1985) 11:440–52. doi: 10.1093/schbul/11.3.440
69. Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. Br J Psychiatry. (1989) 155:49–52. doi: 10.1192/S0007125000291496
70. Lewine RR, Fogg L, Meltzer HY. Assessment of negative and positive symptoms in schizophrenia. Schizophr Bull. (1983) 9:368–76. doi: 10.1093/schbul/9.3.368
71. Kirkpatrick B, Buchanan RW, McKenney PD, Alphs LD, Carpenter WT Jr. The Schedule for the Deficit syndrome: an instrument for research in schizophrenia. Psychiatry Res. (1989) 30:119–23. doi: 10.1016/0165-1781(89)90153-4
72. Horan WP, Kring AM, Gur RE, Reise SP, Blanchard JJ. Development and psychometric validation of the Clinical Assessment Interview for Negative Symptoms (CAINS). Schizophr Res. (2011) 132:140–5. doi: 10.1016/j.schres.2011.06.030
73. Aleman A, Lincoln TM, Bruggeman R, Melle I, Arends J, Arango C, et al. Treatment of negative symptoms: where do we stand, and where do we go? Schizophr Res. (2017) 186:55–62. doi: 10.1016/j.schres.2016.05.015
74. Millan MJ, Andrieux A, Bartzokis G, Cadenhead K, Dazzan P, Fusar-Poli P, et al. Altering the course of schizophrenia: progress and perspectives. Nat Rev Drug Discov. (2016) 15:485–515. doi: 10.1038/nrd.2016.28
75. Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. (2012) 11:73–9. doi: 10.1016/j.wpsyc.2012.05.004
76. Rabinowitz J, Levine SZ, Garibaldi G, Bugarski-Kirola D, Berardo CG, Kapur S. Negative symptoms have greater impact on functioning than positive symptoms in schizophrenia: analysis of CATIE data. Schizophr Res. (2012) 137:147–50. doi: 10.1016/j.schres.2012.01.015
77. Haslam J. Illustrations of Madness: Exhibiting a Singular Case of Insanity, and a No Less Remarkable Difference in Medical Opinion: Developing the Nature of Assailment, and the Manner of Working Events: With a Description of the Tortures Experienced by Bomb-bursting, Lobster-cracking, and Lenghthening the Brain. Embellished with a Curious Plate. London: G Hayden (1810).
79. Berrios GE. The History of Mental Symptoms: Descriptive Psychopathology Since the Nineteenth Century. Cambridge: Cambridge University Press (1996). doi: 10.1017/CBO9780511526725
80. Minkowski E. La schizophrÈnie: psychopathologie des schizoÔdes et de schizophrËnes. Paris: Payot & Rivages (2010).
82. Jackson JH, Taylor J, Holmes G, Walshe F. Selected writings of John Hughlings Jackson: evolution and dissolution of the nervous system. In: Speech Various Papers, Addresses, and Lectures. Staples (1958).
83. Crow TJ, Frith CD, Johnstone EC, Owens DGC, Weinberger D, Jed Wyatt R, et al. Atrophy. Lancet. (1980) 315:1129–30. doi: 10.1016/S0140-6736(80)91569-X
85. Crow TJ. The two-syndrome concept: origins and current status. Schizophr Bull. (1985) 11:471–88. doi: 10.1093/schbul/11.3.471
86. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. (1982) 39:789–94. doi: 10.1001/archpsyc.1982.04290070025006
87. Andreasen NC. Positive vs. negative schizophrenia: a critical evaluation. Schizophr Bull. (1985) 11:380–9. doi: 10.1093/schbul/11.3.380
88. Carpenter WT Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. (1988) 145:578–83. doi: 10.1176/ajp.145.5.578
89. Lincoln TM, Dollfus S, Lyne J. Current developments and challenges in the assessment of negative symptoms. Schizophr Res. (2017) 186:8–18. doi: 10.1016/j.schres.2016.02.035
90. Galderisi S, Mucci A, Buchanan RW, Arango C. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry. (2018) 5:664–77. doi: 10.1016/S2215-0366(18)30050-6
91. Kaiser S, Lyne J, Agartz I, Clarke M, Morch-Johnsen L, Faerden A. Individual negative symptoms and domains - relevance for assessment, pathomechanisms and treatment. Schizophr Res. (2017) 186:39–45. doi: 10.1016/j.schres.2016.07.013
93. Kolvin I. Studies in the childhood psychoses. I Diagnostic criteria and classification. Br J Psychiatry. (1971) 118:381–4. doi: 10.1192/bjp.118.545.381
94. Hommer RE, Swedo SE. Schizophrenia and autism-related disorders. Schizophr Bull. (2015) 41:313–4. doi: 10.1093/schbul/sbu188
95. Schmidt SJ, Behar A, Schultze-Lutter F. Asperger syndrome and/or clinical high risk of psychosis? A differential diagnostic challenge. Prax Kinderpsychol Kinderpsychiatr. (2018) 67:274–93. doi: 10.13109/prkk.2018.67.3.274
96. De Crescenzo F, Postorino V, Siracusano M, Riccioni A, Armando M, Curatolo P, et al. Autistic symptoms in schizophrenia spectrum disorders: a systematic review and meta-analysis. Front Psychiatry. (2019) 10:78. doi: 10.3389/fpsyt.2019.00078
97. van Ommeren TB, Begeer S, Scheeren AM, Koot HM. Measuring reciprocity in high functioning children and adolescents with autism spectrum disorders. J Autism Dev Disord. (2012) 42:1001–10. doi: 10.1007/s10803-011-1331-9
98. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization (1993).
99. Cochran DM, Dvir Y, Frazier JA. “Autism-plus” spectrum disorders: intersection with psychosis and the schizophrenia spectrum. Child Adolesc Psychiatr Clin N Am. (2013) 22:609–27. doi: 10.1016/j.chc.2013.04.005
100. Larson FV, Wagner AP, Jones PB, Tantam D, Lai MC, Baron-Cohen S, et al. Psychosis in autism: comparison of the features of both conditions in a dually affected cohort. Br J Psychiatry. (2017) 210:269–75. doi: 10.1192/bjp.bp.116.187682
101. Tezenas du Montcel C, Pelissolo A, Schurhoff F, Pignon B. Obsessive-compulsive symptoms in schizophrenia: an up-to-date review of literature. Curr Psychiatry Rep. (2019) 21:64. doi: 10.1007/s11920-019-1051-y
102. Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry. (2005) 39:964–71. doi: 10.1080/j.1440-1614.2005.01714.x
103. Di Michele V, Bolino F. The natural course of schizophrenia and psychopathological predictors of outcome. A community-based cohort study. Psychopathology. (2004) 37:98–104. doi: 10.1159/000078090
104. Miettunen J, Immonen J, McGrath JJ, Isohanni M, Jääskeläinen E. The age of onset of schizophrenia spectrum disorders. In: Age of Onset of Mental Disorders Springer (2019). p. 55–73. doi: 10.1007/978-3-319-72619-9_4
105. Chawarska K, Klin A, Paul R, Macari S, Volkmar F. A prospective study of toddlers with ASD: short-term diagnostic and cognitive outcomes. J Child Psychol Psychiatry. (2009) 50:1235–45. doi: 10.1111/j.1469-7610.2009.02101.x
106. Parr JR, Le Couteur A, Baird G, Rutter M, Pickles A, Fombonne E, et al. Early developmental regression in autism spectrum disorder: evidence from an international multiplex sample. J Autism Dev Disord. (2011) 41:332–40. doi: 10.1007/s10803-010-1055-2
107. Shattuck PT, Durkin M, Maenner M, Newschaffer C, Mandell DS, Wiggins L, et al. Timing of identification among children with an autism spectrum disorder: findings from a population-based surveillance study. J Am Acad Child Adolesc Psychiatry. (2009) 48:474–83. doi: 10.1097/CHI.0b013e31819b3848
108. Naito K, Matsui Y, Maeda K, Tanaka K. Evaluation of the validity of the Autism Spectrum Quotient (AQ) in differentiating high-functioning autistic spectrum disorder from schizophrenia. Kobe J Med Sci. (2010) 56:E116–24.
109. Bartlett J. Childhood-onset schizophrenia: what do we really know? Health Psychol Behav Med. (2014) 2:735–47. doi: 10.1080/21642850.2014.927738
110. Driver DI, Gogtay N, Rapoport JL. Childhood onset schizophrenia and early onset schizophrenia spectrum disorders. Child Adolesc Psychiatr Clin N Am. (2013) 22:539–55. doi: 10.1016/j.chc.2013.04.001
111. Rapoport J, Chavez A, Greenstein D, Addington A, Gogtay N. Autism spectrum disorders and childhood-onset schizophrenia: clinical and biological contributions to a relation revisited. J Am Acad Child Adolesc Psychiatry. (2009) 48:10–8. doi: 10.1097/CHI.0b013e31818b1c63
112. Alaghband-Rad J, McKenna K, Gordon CT, Albus KE, Hamburger SD, Rumsey JM, et al. Childhood-onset schizophrenia: the severity of premorbid course. J Am Acad Child Adolesc Psychiatry. (1995) 34:1273–83. doi: 10.1097/00004583-199510000-00012
113. Watkins JM, Asarnow RF, Tanguay PE. Symptom development in childhood onset schizophrenia. J Child Psychol Psychiatry. (1988) 29:865–78. doi: 10.1111/j.1469-7610.1988.tb00759.x
114. Coghill D, Bonnar S, Seth S, Duke S, Graham J. Child and Adolescent Psychiatry. Oxford, MI: Oxford University Press (2009). doi: 10.1093/med/9780199234998.001.0001
115. Taylor JL. The transition out of high school and into adulthood for individuals with autism and for their families. Int Rev Res Mental Retard. (2009) 38:1–32. doi: 10.1016/S0074-7750(08)38001-X
116. Buitelaar JK, van der Gaag RJ. Diagnostic rules for children with PDD-NOS and multiple complex developmental disorder. J Child Psychol Psychiatry. (1998) 39:911–9. doi: 10.1017/S0021963098002820
117. Towbin KE, Dykens EM, Pearson GS, Cohen DJ. Conceptualizing “borderline syndrome of childhood” and “childhood schizophrenia” as a developmental disorder. J Am Acad Child Adolesc Psychiatry. (1993) 32:775–82. doi: 10.1097/00004583-199307000-00011
118. Xavier J, Vannetzel L, Viaux S, Leroy A, Plaza M, Tordjman S, et al. Reliability and diagnostic efficiency of the Diagnostic Inventory for Disharmony (DID) in youths with Pervasive Developmental Disorder and Multiple Complex Developmental Disorder. Res Autism Spectr Disord. (2011) 5:1493–9. doi: 10.1016/j.rasd.2011.02.010
119. Hatila S, Solanki G. Co-occurrence of autistic spectrum disorder and childhood-onset schizophrenia. Prim Care Companion CNS Disord. (2020) 22:2515. doi: 10.4088/PCC.19l02515
120. Keller R, Piedimonte A, Bianco F, Bari S, Cauda F. Diagnostic characteristics of psychosis and autism spectrum disorder in adolescence and adulthood. A case series. Autism Open Access. (2015) 6:159. doi: 10.4172/2165-7890.1000159
121. Addington J, Piskulic D, Liu L, Lockwood J, Cadenhead KS, Cannon TD, et al. Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophr Res. (2017) 190:90–5. doi: 10.1016/j.schres.2017.03.043
122. Solomon M, Olsen E, Niendam T, Ragland JD, Yoon J, Minzenberg M, et al. From lumping to splitting and back again: atypical social and language development in individuals with clinical-high-risk for psychosis, first episode schizophrenia, and autism spectrum disorders. Schizophr Res. (2011) 131:146–51. doi: 10.1016/j.schres.2011.03.005
123. Barneveld PS, Pieterse J, de Sonneville L, van Rijn S, Lahuis B, van Engeland H, et al. Overlap of autistic and schizotypal traits in adolescents with Autism Spectrum Disorders. Schizophr Res. (2011) 126:231–6. doi: 10.1016/j.schres.2010.09.004
124. Foss-Feig JH, Velthorst E, Smith L, Reichenberg A, Addington J, Cadenhead KS, et al. Clinical profiles and conversion rates among young individuals with autism spectrum disorder who present to clinical high risk for psychosis services. J Am Acad Child Adolesc Psychiatry. (2019) 58:582–8. doi: 10.1016/j.jaac.2018.09.446
125. Fusar-Poli P, Raballo A, Parnas J. What is an attenuated psychotic symptom? On the importance of the context. Schizophr Bull. (2017) 43:687–92. doi: 10.1093/schbul/sbw182
Keywords: autism, psychosis, delusions, hallucinations, negative symptoms
Citation: Ribolsi M, Fiori Nastro F, Pelle M, Medici C, Sacchetto S, Lisi G, Riccioni A, Siracusano M, Mazzone L and Di Lorenzo G (2022) Recognizing Psychosis in Autism Spectrum Disorder. Front. Psychiatry 13:768586. doi: 10.3389/fpsyt.2022.768586
Received: 31 August 2021; Accepted: 03 February 2022;
Published: 28 February 2022.
Edited by:
Sarah Lippe, Université de Montréal, CanadaReviewed by:
Anna Comparelli, Azienda Ospedaliera Sant'Andrea, ItalyCopyright © 2022 Ribolsi, Fiori Nastro, Pelle, Medici, Sacchetto, Lisi, Riccioni, Siracusano, Mazzone and Di Lorenzo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michele Ribolsi, bWljaGVsZS5yaWJvbHNpQHVuaWNhbXB1cy5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.