- 1Centre for Medical Ethics, University of Oslo, Oslo, Norway
- 2Faculty of Health Sciences, Oslo Metropolitan University, Oslo, Norway
- 3Mental Health Services, Akershus University Hospital, Lørenskog, Norway
- 4Institute of Clinical Medicine, University of Oslo, Oslo, Norway
- 5Department of Health Psychology, Jagiellonian University Medical College, Krakow, Poland
- 6National Centre for Suicide Research and Prevention, Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Objective: The Staff Attitude to Coercion Scale (SACS) was developed to assess mental health care staff's attitudes to the use of coercion in treatment. The staff's attitudes to the use of coercion may also influence their willingness to engage in professional development projects aimed at reducing use of coercion. This study systematically reviews the existing evidence related to the measurement properties of the SACS in papers published since the publication of SACS in 2008.
Methods: Seven databases were searched for studies published until October 2021 assessing the measurement properties of SACS or using SACS. All original studies reporting data relevant for the assessment of measurement properties of the SACS were eligible for inclusion. The methodological quality of the studies was assessed and rated using the COnsensus-based Standard for the selection of health Measurement INstruments (COSMIN).
Results: Of the 81 identified publications, 13 studies with a total of 2,675 respondents met the inclusion criteria. Most studies reported data on structural validity and internal consistency, with high methodological quality, but there were almost no data on any other measurement properties.
Conclusion: We found evidence for adequate structural validity and internal consistency of the SACS, while other important measurement properties were not addressed in any of the reviewed studies. Caution is needed when interpreting results of the SACS in terms of aspects such as reliability, criterion validity and measurement error. The relationship between staff attitudes to coercion and the actual use of coercion also remains unclear and needs to be further investigated.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42021239284.
Introduction
The use of coercion in health care is ethically problematic and challenge the fundamental health care principle of respect for patient autonomy (1, 2). All over the world there are initiatives to minimize its use (3–6). Health care professionals need to critically reflect upon and morally justify each use of coercive interventions (7, 8). Several studies have shown considerable variation in use of coercive measures both, in one country and between different countries (9–11). These differences are not yet fully explained (12–14). Based on differences in the use of coercive practices among different countries, regions, and hospitals, some of the variation can be attributed to differences in staff attitudes to the use of coercion (15). Attitudes can be defined as a psychological tendency that is expressed through evaluating an entity with a normative degree of either positivity or negativity, based on experience (16). Attitudes do influence behavior, but the connection between attitudes and behavior is complex, and may depend on situational factors. The connection has not been fully mapped yet, and the relationship may also depend on the subject of the attitude (17).
In recent years, attitudes to the use of coercive interventions in mental health care have evolved, with increased focus on user participation, respect for autonomy, and human rights (6). Differences in staff attitudes to the use of coercion may explain why some wards and hospitals have attempted to reduce the use of coercion, while others have not made the same effort (4, 18). Staff attitudes to coercion may also influence the amount of coercion used and reveal the reasons for using coercion in treatment and the dynamics involved.
It is therefore important to have a validated questionnaire for assessing staff attitudes to coercion in mental health care. In 2008, Husum et al. developed and published the Staff Attitude toward Coercion Scale (SACS) for this purpose (19). SACS measures staff attitudes toward use of coercive practices in mental health care. SACS was developed as a short 15-item questionnaire with normative attitudes toward use of coercion. It consists of statements about the use of coercion, about how the participant thinks about it, and whether the participant considers coercive interventions necessary. Using factor analysis, the questionnaire divided staff attitudes to coercion into three groups: the view that use of coercion may offend (critical attitude); the view that coercion is necessary for care and security reasons (pragmatic attitude); and the view of coercion as a valid form of treatment (positive attitude). These items are scored on a five-point Likert scale, from 1 = strongly disagree to 5 = strongly agree.
The SACS is to our knowledge the only instrument measuring staff attitudes to coercion, and the instrument has now been used worldwide and translated into several languages, including German, Polish, Chinese, Japanese, Italian, Turkish and Arabic, indicating a potential for cross-cultural applicability. The questionnaire has also been used in some populations with other participants, like patients and caregivers. However, to the best of our knowledge, no systematic review has been performed to assess the measurement properties of the scale. To date, there has been no attempt to examine the results of its use in practice and research, and no meta-analysis has been done.
This review aims to gather results relevant for measurement evaluation of the SACS questionnaire. Assessing measurement characteristics is essential for comparing results from different countries and populations. In particular, the aim of this study was to conduct a systematic review of the measurement properties of SACS using the COSMIN Risk of Bias checklist (20–23). The following review questions were considered.
(1) Summarize and evaluate the available evidence regarding the measurement properties and use of the Staff Attitude to Coercion Scale (SACS) in health care settings.
(2) Assess the reliability and validity of the SACS as reported in these studies.
(3) Examine the performance and factorial invariance of the three SACS dimension ratings across subgroups [e.g., defined as populations from different countries; different professional groups; differences between other populations (patients and carers) and across time].
Methods
This systematic review was carried out following the “COnsensus-based Standards for the selection of health Measurement Instruments” (COSMIN) (20, 22, 23) and the “Preferred Reporting Items for Systematic reviews and Meta-Analyses” (PRISMA) guidelines (24).
The review protocol was registered with PROSPERO (Record ID = CRD42021239284).
Criteria for Selecting Studies
All original studies reporting data relevant for the assessment of measurement properties of the SACS were eligible for inclusion. There were no restrictions on setting or publication language. The systematic review includes studies reporting data from any eligible SACS measures on one or more of the domains defined by the consensus-based standard for the selection of health measurement instruments (COSMIN) taxonomy: reliability (internal consistency, test-retest reliability, inter-rater reliability, and measurement error); validity (content validity, construct validity, cross-cultural validity, predictive validity, criterion validity, and structural validity); responsiveness; and interpretability (20, 22).
Strategies for the Identification of Studies
All relevant studies that met the inclusion criteria were identified by searching the following seven electronic databases: MEDLINE by EBSCOhost, PsycINFO by APA PsycNET, Embase by Elsevier, CINAHL by EBSCOhost, Web of Science by Thomson Reuters, Google Scholar, and OpenGrey. The following terms were used in the search for studies: SACS, Staff attitude to coercion scale, Staff attitude toward coercion scale, Staff's normative attitudes toward coercion. Studies published between 2008 and October 2021 were considered. The full search string is attached as Appendix 1. A trained librarian at the hospital library conducted the search. In addition, researchers who had asked for permission to use the scale were also contacted and asked for their results.
Study Screening and Selection
The selection of studies was made by two review teams (JL with TLH, and JS with TLH). Each review team reviewed half of the articles. A third reviewer (TR) was involved when there was discrepancy between the two reviewers. Any discrepancies regarding selection were resolved by consensus. First, titles and abstracts were screened for eligibility. Then, the full text of the potentially relevant studies was read to decide whether the study met the selection criteria. Studies that did not fulfill all the inclusion criteria were excluded, and the reason for exclusion was noted. A flow chart of the selection process is presented in Figure 1.
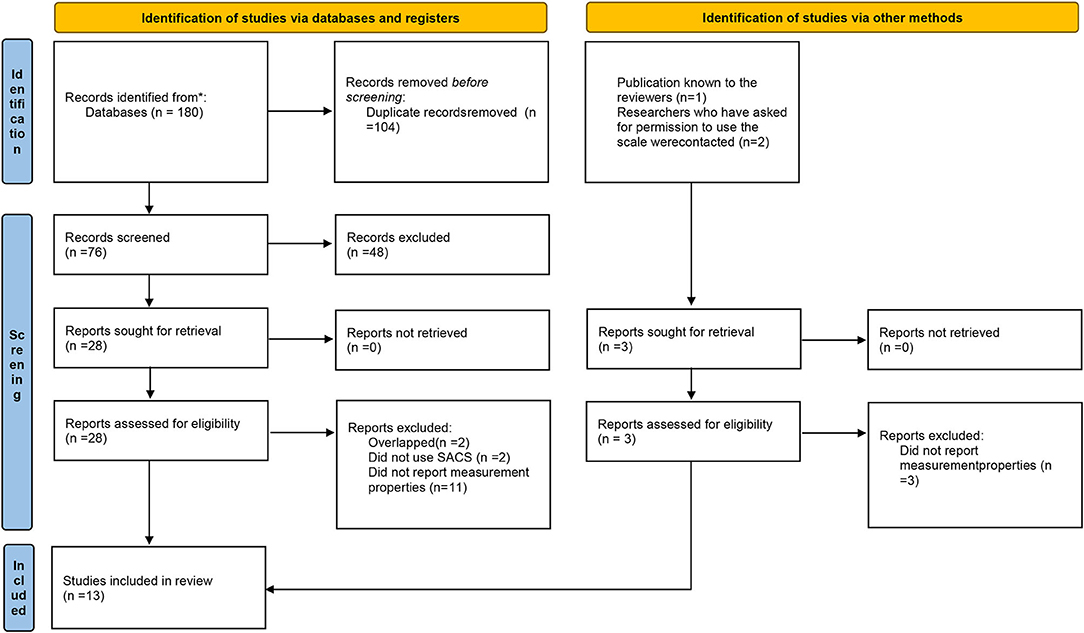
Figure 1. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers and other sources. *Number of records identified from each database is presented in the Appendix 1 in the description of the database search. From: Page et al. (24). For more information, visit: http://www.prisma-statement.org/.
Assessing the Risk of Bias
For assessing the measurement properties of SACS we used the COSMIN Risk of Bias checklist (21, 22). In their 10 steps for conducting a systematic review of patient-reported outcome measurements the COSMIN group defines the evaluation of measurement properties in three steps [step five to seven in Figure 1 in (22)] using the COSMIN Risk of Bias checklist: evaluate content validity, evaluate internal structure (structural validity, internal consistency, cross-cultural validity/measurement invariance), and evaluate the remaining instrument properties (reliability, measurement error, criterion validity, hypothesis testing for construct validity, responsiveness) (21, 22).
Using the checklist, two reviewers independently assessed the methodological quality of measurement properties reported in each study with discrepancies in assessment resolved by consensus. For this review of a single instrument, already developed, we did not rate the studies on content validity. Each of the eight other measurement properties were rated on a four-point scale (inadequate, doubtful, adequate, very good) according to the definitions and instructions in the COSMIN manual (20, 22). The rating inadequate is also used when a study has not examined or reported a property when this could have been done for the instrument.
Data Extraction and Analyses
Two reviewers (JL and JS) extracted the data, and a third reviewer checked the data being extracted (TLH). Data related to internal consistency (Cronbach's alpha), structural validity (factor analysis, correlations), reliability (ICC, Cohen's kappa), and responsiveness (correlations) were collected. In cases of uncertainty about the extracted data, another reviewer (TR) was consulted. For further definition of the measurement constructs, please refer to the COSMIN manual.
Results
Study Selection
Our search resulted in 81 hits, which were reviewed at the title and abstract level. Altogether, 31 studies were read in full text. Finally, 13 studies were included, while the rest were excluded, with reasons for exclusion at the full text level given in Figure 1.
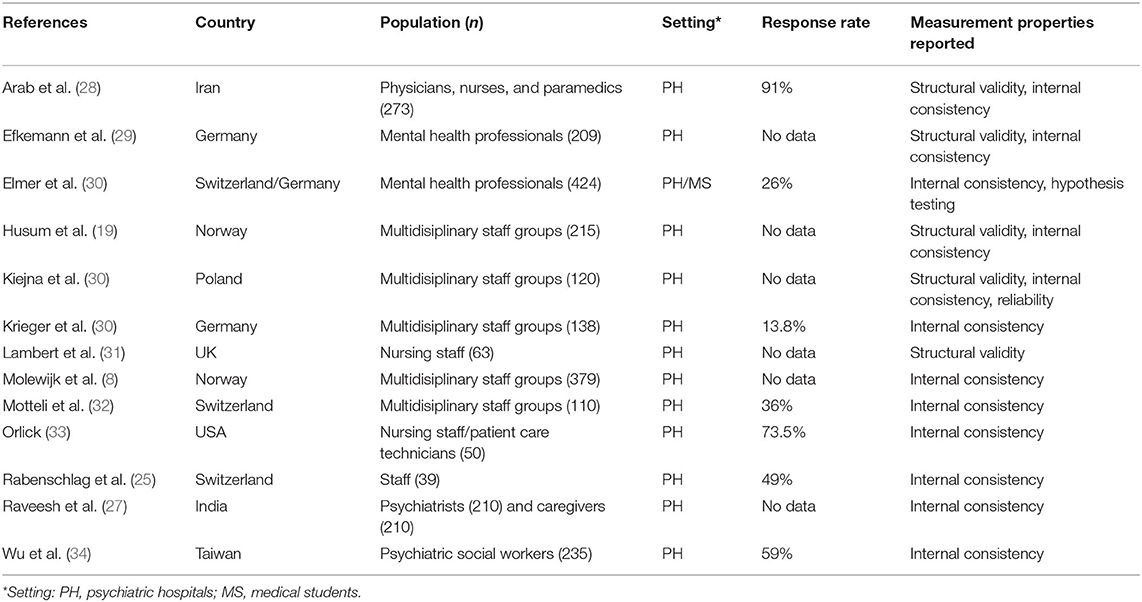
Study Population Demographics
The 13 included studies had between 39 (25) and 424 participants (26), with a total of 2,675 respondents. The studies were from eight different countries and used six different language versions. All populations included mental health professionals, either mixed or grouped by profession. The only exception was one population of 210 caregivers (27) (Table 1).
Structural Validity
We identified five studies assessing structural validity (19, 28–31). Four of these studies reported data from factor analysis (19, 28–30), while one reported correlations between the subscales (31).
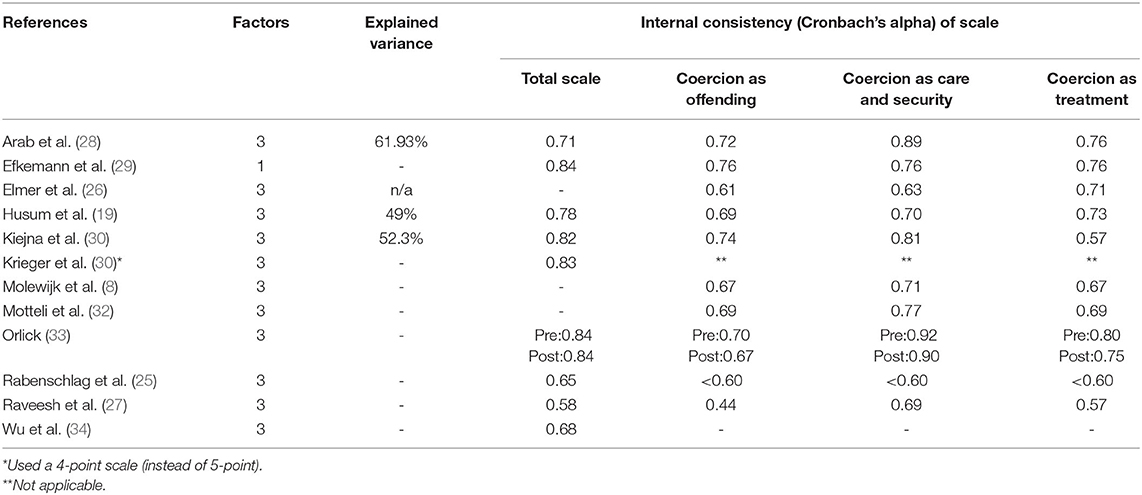
Husum et al. (19) was the first study in this category and reported three factors representing the underlying theoretical structure and explaining 49.1% of the variance. This finding was later replicated (28, 30). Arab et al. found that the three factors explained 61.93% of the variance, while Kiejna et al. found that they explained 52.3% of the variance.
Efkemann et al. reported four factors meeting the common factor analysis criteria of eigenvalue <1; however, the last factor was only marginally larger than one. A scree plot inspection indicated that a three-factor solution might better represent the underlying structure. When testing the original three-factor solution reported by Husum et al. (19), however, they found that not all items corresponded to the original factor solution, and that some items loaded on two factors. As a final test of the internal structure, they did a factor analysis with only one factor. This also seemed to represent an adequate solution, as all items loaded higher than 0.4 on this factor.
The study reporting subscale correlations found that the “coercion as offending” subscale correlated to 0.34 with the “coercion as care and security” subscale and to −0.12 with the “coercion as treatment” subscale. The “coercion as care and security” and the “coercion as treatment” subscales correlated to 0.65 (31) (Table 2).
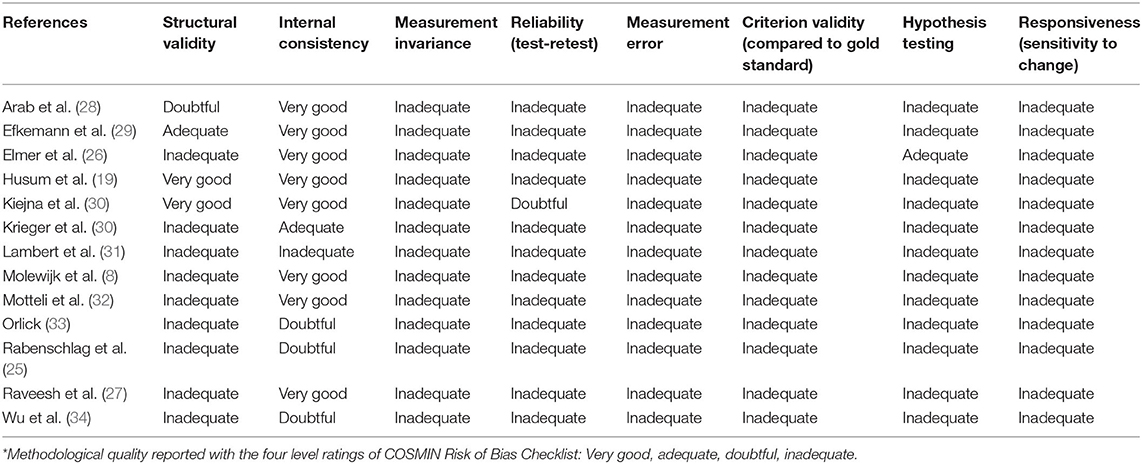
The studies investigating structural validity were overall of good methodological quality; two studies were rated very good and one adequate, fair (Table 3).
Internal Consistency
This was the most frequently reported measurement property, with 12 studies reporting relevant analysis (8, 19, 25–30, 32–35). Nine studies reported Cronbach's alpha for the entire SACS scale, varying between 0.58 (27) and 0.84 (29, 33). Six of the nine studies (19, 25, 27–30, 33–35) reported alpha above 0.70. Nine studies reported Cronbach's alpha for the “coercion as offending” subscale, varying between 0.44 (27) and 0.76 (29). Four studies reported Cronbach's alpha at or above 0.70 (28–30, 33). Cronbach's alpha for the “coercion as care and security” subscale was reported in nine studies, and varied between 0.63 (26) and 0.89 (28). Seven studies reported Cronbach's alpha at or above 0.7 (8, 19, 25, 27–29, 32–35). Cronbach's alpha for the “coercion as treatment” subscale was reported in nine studies, and varied between 0.57 (27) and 0.80 (33). Five studies reported Cronbach's alpha at or above 0.70 (19, 26, 28, 29, 33) (Table 2). The methodological quality of reporting internal consistency was very good for eight studies, adequate for one, doubtful for three and inadequate for one (Table 3).
Other Measurement Properties
Only two studies reported data on other measurement properties reported in Table 3; Kiejna et al. (30) reported test-retest reliability over 3 weeks and found a correlation of 0.57 between the time points. Elmer et al. (26) investigated the relationship between SACS and attitudes to informal coercion among medical students and health care personnel. They found positive attitudes toward coercion to be negatively associated with recognizing informal coercion. On the other side, personnel viewing coercion as offending recognized coercion more adequately.
Discussion
The SACS has been used in many studies and countries since its development in 2008. This indicates concern in many cultural settings about use of coercion in mental health care. However, to the best of our knowledge, this is the first systematic review of the measurement properties of the SACS.
Structural validity and internal consistency were the most frequently reported measurement characteristics in the identified studies. All studies reported adequate internal consistency. Most studies replicated the original three-factor structure and the correlation between the factors were medium to low as expected. Merging the model into one factor has been considered, but the measurement findings in this review suggest that the three-factor is better fit to the available data. Keeping the three-factor model is supported by another study who found that professionals could be divided in three groups concerning their thoughts about use of seclusion in mental health care. The authors of this study identified three types of professionals: Transformers, Doubters, and Maintainers (36).
While the available data support the SACS as being psychometrically sound, some important data are missing. For example, there are no measurements across more extended periods of time (37), which could be used to assess the sensitivity to change and stability of the SACS. Two test-retests within a 3-week interval indicate that SACS score may vary over time in the same individuals indicating that the SACS may assess dynamic attitudes likely to fluctuate even within relative short time periods.
Testing of criterion validity by comparing SACS to a gold standard is lacking because there are no other instruments on staff attitude to coercion to compare with. There is also very limited research on the relationship between staff attitudes and the use of coercion. Several studies have suggested that there is a relationship between staff attitudes toward use of coercion and actual use of coercive interventions (8, 26, 35, 38–43).
Other studies have found important differences between explicit and implicit attitudes (44). Explicit attitudes are attitudes that the individual himself is aware of, while implicit attitudes are those attitudes that one is not aware of, but can be measured indirectly through, for example, autonomous reactions. The most common approach to measuring explicit attitudes is self-reporting as these are attitudes that the subject is self-aware of. The SACS questionnaire measures only explicit attitudes. One of the studies included in this review had however studied both explicit and implicit attitudes (45). This is also a topic that should be investigated more thoroughly in future studies.
As shown in Table 3, the reporting of measurement properties except structural validity and internal consistency are so far almost non-existent in SACS studies. A major reason for this may be those analyses of factor structure and the internal consistency of scales and subscales are well established and fairly easy to do, while several of the other properties have been more defined as standards more recently and are less established. Some of these also require more demanding design, data collections and data analyses. The detailed and complicated criteria in the COSMIN rating instructions also makes it difficult to have simple descriptions in a table explaining what the ratings mean. Some criteria in the COSMIN Risk of Bias checklist have also been debated, like rating properties of an instrument based on whether the instrument confirms a hypothesis in a study, as it is impossible to assess in one study both the treatment effect and the responsiveness of an instrument (46).
A challenge in using the COSMIN method for this systematic review is also that the COSMIN taxonomy is originally developed for the assessment of patient-outcome measures. The SACS measures staff attitudes, which is another kind of phenomenon. In general, the scientific study of staff attitudes in mental health care seems to be scarce, and this field needs to be methodologically developed.
Limitations and Recommendations for Future Research
Limitations in this review could be that the two pairs of assessors that assessed the studies could develop different consensus about how to interpret the findings in the papers. Another possible limitation could be that two of the authors were also involved in the development of the original SACS questionnaire and could possibly be biased. We sought to take this into account by collaborating in pairs with the authors not included in the development of the scale. All authors were also involved in the final quality assurance and interpretation of the findings. It is also a challenge and possible limitation in this review that the validation process differs between different studies and countries. Further the studies have used the scale differently. The SACS was developed and validated 15–20 years ago. While not formally investigated in this review; changes in attitudes to toward coercion in the society at large may indicate that a revision of the SACS item may be warranted.
Conclusion
The SACS is, to our best of knowledge, the only questionnaire measuring staff's attitudes to the use of coercive interventions in mental health services. It is used widely, which demonstrates the need for such a tool. The widespread use also indicates that the tool is perceived as feasible and useful.
The assessment found evidence for adequate validity and internal consistency of the SACS. However, there were very limited support for other important measurement qualities such as reliability, criterion validity and measurement error.
Future research should focus on the stability of these attitudes, whether they are amendable by interventions and the relationship between staff attitudes to coercive interventions and the actual use of coercion. Another related topic is to more thoroughly investigate the relationship between staff's explicit and implicit attitudes toward use of coercion. Further future research could investigate formation of staff attitudes. Staff attitudes to the use of coercive practices may also influence the staff's willingness to engage in projects to reduce the use of coercive interventions. Another possible topic for research is to investigate barriers to engage in projects aimed at reducing use of coercive practices in mental health care.
Until future studies have evaluated more measurement properties of SACS, users of SACS must interpret the results based on the current knowledge of its properties.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
All authors have been involved in the process of assessing the studies for inclusion, analyzing the results, writing article, contributed to the article, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Many thanks to the librarian Åse Marit Hammersbøen at Akershus University Hospital for performing the literature searches.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.744661/full#supplementary-material
References
1. Beauchamp TL. Principles of biomedical ethics. In: Tom L, Beauchamp, James F, editors. Childress Childress. New York, NY: Oxford University Press (1979).
2. UN General Assembly. Convention on the Rights of Persons with Disabilities : resolution / adopted by the General Assembly A/RES/61/106. (2007). Available online at: https://www.refworld.org/docid/45f973632.html (accessed April 2, 2022).
3. Sashidharan SP, Mezzina R, Puras D. Reducing coercion in mental healthcare. Epidemiol Psychiatr Sci. (2019) 28:605–12. doi: 10.1017/S2045796019000350
4. Gooding P, McSherry B, Roper C. Preventing and reducing ‘coercion' in mental health services: an international scoping review of English-language studies. Acta Psychiatr Scand. (2020) 142:27–39. doi: 10.1111/acps.13152
5. Council of Europe. Ending Coercion in Mental Health: The Need for a Human Rights-Based Approach. (2019). Available online at: http://www.europeanrights.eu/public/atti/COE_2158_Recommandations_ENG.pdf
6. Zinkler M, von Peter S. End Coercion in mental health services—toward a system based on support only. Laws. (2019) 8:19. doi: 10.3390/laws8030019
7. Mezzina R, Rosen A, Amering M, Javed A. The practice of freedom: human rights and the global mental health agenda. In: Javed A, Fountoulakis KN, editors. Advances in Psychiatry. Cham: Springer International Publishing (2019). p. 483–515.
8. Molewijk B, Kok A, Husum T, Pedersen R, Aasland O. Staff's normative attitudes towards coercion: the role of moral doubt and professional context-a cross-sectional survey study. BMC Med Ethics. (2017) 18:37. doi: 10.1186/s12910-017-0190-0
9. Sheridan Rains L, Zenina T, Dias MC, Jones R, Jeffreys S, Branthonne-Foster S, et al. Variations in patterns of involuntary hospitalisation and in legal frameworks: an international comparative study. Lancet Psychiatry. (2019) 6:403–17. doi: 10.1016/S2215-0366(19)30090-2
10. Kelly BD. Variations in involuntary hospitalisation across countries. Lancet Psychiatry. (2019) 6:361–2. doi: 10.1016/S2215-0366(19)30095-1
11. Bremnes R, Skui H. [Coercion in mental health in Norway. Status after legal changes in (2017). Report IS-2888]. Oslo: The Norwegian Directorate of Health (2020).
12. Husum TL, Bjørngaard JH, Finset A, Ruud T. A cross-sectional prospective study of seclusion, restraint and involuntary medication in acute psychiatric wards: patient, staff and ward characteristics. BMC Health Serv Res. (2010) 10:89. doi: 10.1186/1472-6963-10-89
13. Gandré C, Gervaix J, Thillard J, Macé J-M, Roelandt J-L, Chevreul K. Geographic variations in involuntary care and associations with the supply of health and social care: results from a nationwide study. BMC Health Serv Res. (2018) 18:253. doi: 10.1186/s12913-018-3064-3
14. Välimäki M, Yang M, Vahlberg T, Lantta T, Pekurinen V, Anttila M, et al. Trends in the use of coercive measures in Finnish psychiatric hospitals: a register analysis of the past two decades. BMC Psychiatry. (2019) 19:230. doi: 10.1186/s12888-019-2200-x
15. Husum TL. Staff Attitudes and Use of Coercion in Acute Psychiatric Wards in Norway (Dissertation). University of Oslo, Oslo, Norway (2011).
16. Eagly AH, Chaiken S. The advantages of an inclusive definition of attitude. Soc Cogn. (2007) 25:582–602. doi: 10.1521/soco.2007.25.5.582
17. Maio G, Haddock G, Verplanken B. The Psychology of Attitudes and Attitude Change. New York, NY: Sage Publications (2019).
18. Barbui C, Purgato M, Abdulmalik J, Caldas-de-Almeida JM, Eaton J, Gureje O, et al. Efficacy of interventions to reduce coercive treatment in mental health services: umbrella review of randomised evidence. Br J Psychiatry. (2020) 1–11. doi: 10.1192/bjp.2020.144. [Epub ahead of print].
19. Husum TL, Finset A, Ruud T. The staff attitude to coercion scale (SACS): reliability, validity and feasibility. Int J Law Psychiatry. (2008) 31:417–22. doi: 10.1016/j.ijlp.2008.08.002
20. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. (2010) 19:539–49. doi: 10.1007/s11136-010-9606-8
21. Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, et al. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. (2018) 27:1171–9. doi: 10.1007/s11136-017-1765-4
22. Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. (2018) 27:1147–57. doi: 10.1007/s11136-018-1798-3
23. Terwee CB, Prinsen CAC, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. (2018) 27:1159–70. doi: 10.1007/s11136-018-1829-0
24. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
25. Rabenschlag F, Konrad A, Rueegg S, Jaeger M A. recovery-oriented approach for an acute psychiatric ward: is it feasible and how does it affect staff satisfaction? Psychiatr Quart. (2014) 85:225–39. doi: 10.1007/s11126-013-9285-z
26. Elmer T, Rabenschlag F, Schori D, Zuaboni G, Kozel B, Jaeger S, et al. Informal coercion as a neglected form of communication in psychiatric settings in Germany and Switzerland. Psychiatry Res. (2018) 262:400–6. doi: 10.1016/j.psychres.2017.09.014
27. Raveesh BN, Pathare S, Noorthoorn EO, Gowda GS, Lepping P, Bunders-Aelen JG. Staff and caregiver attitude to coercion in India. Indian J Psychiatry. (2016) 58:S221–S9. doi: 10.4103/0019-5545.196847
28. Arab M, Gray S, Hamouzadeh P. Validation of the “staff attitude toward coercion use in treatment of mentally ill patients” questionnaire in selected public psychiatric hospitals of Tehran in 2015. J Hosp. (2017) 16:31–42. Available online at: https://jhosp.tums.ac.ir/browse.php?a_code=A-10-83-3&slc_lang=en&sid=1
29. Efkemann SA, Scholten M, Bottlender R, Juckel G, Gather J A. German version of the staff attitude to coercion scale. Development and empirical validation. Front Psychiatr. (2020) 11:573240. doi: 10.3389/fpsyt.2020.573240
30. Kiejna A, Jakubczyk MH, Gondek TM, Rajba B. Kwestionariusz Postaw Personelu wobec Przymusu (SACS)–polska adaptacja. Psychiatr Pol. (2020) 54:113–24. doi: 10.12740/PP/102438
31. Lambert K, Chu S, Turner P. Professional boundaries of nursing staff in secure mental health services: impact of interpersonal style and attitude toward coercion. J Psychosoc Nurs Ment Health Serv. (2019) 57:16–24. doi: 10.3928/02793695-20180920-05
32. Mötteli S, Hotzy F, Lamster F, Horisberger R, Theodoridou A, Vetter S, et al. Optimistic recovery expectations are associated with critical attitudes toward coercion among mental health professionals. Int J Ment Health. (2020) 49:157–69. doi: 10.1080/00207411.2019.1699338
33. Orlick A. Reducing the use of physical and chemical restraints through enhanced de-escalation training in adult inpatient psychiatry. Dissertation Abst Int Section Sci Eng. (2021) 82. Available online at: https://www.proquest.com/openview/e4d7035de705238602f41f323ee93404/1?pq-origsite=gscholar&cbl=18750&diss=y
34. Wu H-C, Tang IC, Lin W-I, Chang L-H. Professional values and attitude of psychiatric social workers toward involuntary hospitalization of psychiatric patients. J Soc Work. (2013) 13:419–34. doi: 10.1177/1468017311435201
35. Krieger E, Moritz S, Lincoln TM, Fischer R, Nagel M. Coercion in psychiatry: a cross-sectional study on staff views and emotions. J Psychiatr Ment Health Nurs. (2020) 29:29. doi: 10.1111/jpm.12643
36. Van Doeselaar M, Sleegers P, Hutschemaekers G. Professionals' attitudes toward reducing restraint: the case of seclusion in The Netherlands. Psychiatr Quart. (2008) 79:97–109. doi: 10.1007/s11126-007-9063-x
37. Sturgis P, Allum N, Brunton-Smith I. (2009). Attitudes over time: the psychology of panel conditioning. In: Groves RM, Kalton G, Rao JNK, Schwarz N, Skinner, Lynn P, editors. Methodology of Longitudinal Surveys. (2009). doi: 10.1002/9780470743874.ch7
38. Aasland OG, Husum TL, Førde R, Pedersen R. Between authoritarian and dialogical approaches: attitudes and opinions on coercion among professionals in mental health and addiction care in Norway. Int J Law Psychiatry. (2018) 57:106–12. doi: 10.1016/j.ijlp.2018.02.005
39. Bregar B, Skela-Savič B, Plesničar BK. Cross-sectional study on nurses' attitudes regarding coercive measures: the importance of socio-demographic characteristics, job satisfaction, and strategies for coping with stress. BMC Psychiatry. (2018) 18:1–10. doi: 10.1186/s12888-018-1756-1
40. Doedens P, Vermeulen J, Boyette LL, Latour C, de Haan L. Influence of nursing staff attitudes and characteristics on the use of coercive measures in acute mental health services—A systematic review. J Psychiatr Mental Health Nurs. (2020) 27:446–59. doi: 10.1111/jpm.12586
41. Husum TL, Bjørngaard JH, Finset A, Ruud T. Staff attitudes and thoughts about the use of coercion in acute psychiatric wards. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:893–901. doi: 10.1007/s00127-010-0259-2
42. Steinert T, Lepping P, Baranyai R, Hoffmann M, Leherr H. Compulsory admission and treatment in schizophrenia. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:635–41. doi: 10.1007/s00127-005-0929-7
43. Zinkler M, Priebe S. Detention of the mentally ill in Europe–a review. Acta Psychiatrica Scand. (2002) 106:3–8. doi: 10.1034/j.1600-0447.2002.02268.x
44. Verplanken B, Sui J. Habit and identity: behavioral, cognitive, affective, and motivational facets of an integrated self. Front Psychol. (2019) 10:e01504. doi: 10.3389/fpsyg.2019.01504
45. Vandamme A, Wullschleger A, Garbe A, Cole C, Heinz A, Bermpohl F, et al. The role of implicit and explicit staff attitudes in the use of coercive measures in psychiatry. Front Psychiatry. (2021) 12:e699446. doi: 10.3389/fpsyt.2021.699446
Keywords: mental health, staff, attitudes, coercion, psychometrics, systematic review
Citation: Husum TL, Ruud T, Lickiewicz J and Siqveland J (2022) Measurement Properties of the Staff Attitude to Coercion Scale: A Systematic Review. Front. Psychiatry 13:744661. doi: 10.3389/fpsyt.2022.744661
Received: 20 July 2021; Accepted: 22 March 2022;
Published: 28 April 2022.
Edited by:
Bridget Hamilton, The University of Melbourne, AustraliaReviewed by:
Yu-Wei Ryan Chen, The University of Sydney, AustraliaMinna Stolt, University of Turku, Finland
Copyright © 2022 Husum, Ruud, Lickiewicz and Siqveland. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tonje Lossius Husum, dC5sLmh1c3VtQG1lZGlzaW4udWlvLm5v
 Tonje Lossius Husum
Tonje Lossius Husum Torleif Ruud
Torleif Ruud Jakub Lickiewicz
Jakub Lickiewicz Johan Siqveland
Johan Siqveland