
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 25 April 2022
Sec. Child and Adolescent Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.617941
This article is part of the Research TopicEmotional Dysregulation in Children and Adolescents View all 21 articles
 Mercedes M. Bock1,2*†
Mercedes M. Bock1,2*† Theres Graf1†
Theres Graf1† Verena Woeber3,4†
Verena Woeber3,4† Oswald D. Kothgassner1†
Oswald D. Kothgassner1† Arne Buerger5†
Arne Buerger5† Paul L. Plener1,6†
Paul L. Plener1,6†Introduction: Emotion dysregulation is a common challenge pertaining to numerous psychiatric disorders in adolescence and is associated with increased morbidity and mortality. Dialectical Behavior Therapy for Adolescents (DBT®-A) has been shown to be an effective treatment, especially in the reduction of self-harm and suicidality. Measures in relation to the COVID-19 pandemic set strict limits on physical contacts with patients. In order to continuously provide evidence-based specialized care to patients suffering from emotion dysregulation, we offered two online DBT®-A skill groups in a video-group-call format.
Objective: We aimed at assessing our online DBT®-A skills groups, collect according up- and downsides, and form a basis for advancement of this form of treatment provision. Also, the impact of the COVID-19 pandemic on patients was assessed.
Methods: A physical DBT®-A skill group was switched to a video-group-call format and a second group was initiated de novo online. After five sessions, patients engaged in structured group discussions to reflect experiences. Discussion content was analyzed via Inductive Category Formation within the Framework of Qualitative Content Analysis.
Results: Patients unanimously found the COVID-19 pandemic challenging, but also reported differentially on its impact. Downsides were balanced by subjective “gains” in time and a perceived reduction in stress. Technical problems of the online format were discussed, but did not limit the positive experience of still receiving treatment. Patients of both online DBT®-A skill groups valued the offer, felt connected, and reported benefits from the treatment. The transition group additionally discussed changes in structure and content of the group sessions after the switch to online meetings and reflected differential functions of the group.
Discussion: Although the sample size is small, and conclusions are drawn from Inductive Qualitative Content Analysis, the presented results are of interest. In our investigation, video-group-calls were both safe and beneficial for patients. This alternative to physical meetings is not only interesting for further waves of the current pandemic but also for service provision in remote areas with limited access to specialized care. Further research is needed to challenge and refine our results and to explore extensions to “basic” video-group-calls, such as “break-out sessions,” blended therapy, or real-time supervision within an online session.
Emotion dysregulation is seen as a trans-diagnostic factor with negative impact on various domains of psychopathology in adolescents (1), although specifics could be identified in the subgroup of patients suffering from borderline personality disorder (BPD) (2). Deficits in emotion regulation are associated with social impairment (3) and, consequently, contribute negatively to the level of psychosocial functioning. Additionally, typical behavioral manifestations of emotion dysregulation, such as self-harm, suicidal ideation, eating disorder behaviors, or substance (ab)use, are associated with increased morbidity and mortality (4–7). According to international standards, Dialectical Behavior Therapy for Adolescents (DBT®-A) is an evidence-based treatment for these patients, especially concerning the reduction of self-harm (8–11). DBT-A is a manualized treatment tailored for application in outpatient settings (12–14). Full DBT®-A treatment comprises weekly individual sessions, concurrent participation in a DBT®-A skills group, telephone coaching, consultation team, and family work (13, 15). Specific strategies taught within the skills group component of DBT®-A are mindfulness, distress tolerance, interpersonal effectiveness, emotion regulation, and “walking the middle path” (strategies connecting teens and caregivers).
In integrating the above with results from first observations on the impact of the COVID-19 pandemic on patients suffering from mental health disorders, the continued provision of evidence-based care is of utmost importance. So far, data clearly indicate disproportional consequences of the COVID-19 pandemic (16–18), even a potentially increased suicide risk (18), and an increase of adversities (19) in patients suffering from mental health disorders.
Owing to restrictions set to ensure minimum spreading of SARS-CoV-2, not only in everyday life, but also in clinical routine suffered critical cuts. Limits especially concerned physical contacts, which were reduced to an absolute minimum (i.e., emergency presentations in the psychiatric context). Given the need to continuously serve patients despite these restrictions, a lot of effort went into provision of services through other means of care, such as telehealth interventions (20). In the need of the moment and given changes in several legal regulations, many departments of child and adolescent psychiatry conducted an ad hoc switch from face-to-face to teletherapy to continuously serve their current outpatients (21). Although the preexisting body of literature on telemental health, many countries stepped into this venture without preparation because of lack of legal frameworks and lacking prior approval on the conductance of teletherapy by legal authorities and professional organizations (22). Even in countries with regulations and formal licensing procedures, such as the United States, many therapists were unexperienced in using telemental health (23). Sampaio et al. could show that around half of the mental health professionals in their survey were concerned about data safety when using telemental health.
In order to ensure continuation of high-quality, evidence-based services, especially in expectance of further waves of the current pandemic, we aimed at systematically evaluating patients' experiences with our DBT-A skill group in the newly established video group call format via structured group discussions and consecutive qualitative analyses1. Sampaio et al. argued that around 50% of mental health professionals expressed concerns about their ability to handle emergency situations in a telemental health setting (23), which is of special interest for our research because the population investigated herein were “at risk” patients (self-harm, suicidality).
Little et al. (24) argued that qualitative methodology is suitable to address and assess patients' perceptions of DBT®. Since presentation, discussion and training of behavioral, cognitive, and emotional skills serve as one of the main therapeutic tools in overcoming pervasive emotion dysregulation (25, 26), we decided to focus on this component. Also, Linehan et al. (27) could show that skills training alone leads to better results concerning the frequency of self-harm than individual DBT®, as well as overall similar rates concerning other symptoms of BPD addressed within therapy (e.g., suicidal ideations, suicide attempts). The aim of this small open trial was, thus, to assess practicability and record potential adverse effects of DBT®-A skills training in a video group call format. Thoughts and ideas expressed by our patients, as well as insights gained in the process, were deemed to form the base for further steps, especially concerning positive lessons, but also flipsides of this form of treatment conductance. Although this is especially relevant in case of further waves of the COVID-19 pandemic, results might also be helpful concerning potential applications in other situations, such as service provision in remote areas with limited access to specialized care.
Of five patients participating in our physical group, four decided to continue online. All four patients completed the online “cycle.” Although all patients gave consent to study participation, only three engaged in the investigative group discussion (one patient had a colliding appointment).
Six patients showed interest and started in our second de novo online group. Of these six patients, one dropped out after two sessions because she felt the content was not the right fit for her, and one left the group after three sessions because of repeated technical problems (unstable internet connection). The remaining four patients gave consent to study participation, but only three were online at the time of the investigative group discussion. One patient had technical problems during the discussion and, thus, could not continuously contribute. Concerning dropouts, we saw no difference to our physical groups. The dropout rates we observed in our sample were at the lower end of rates reported in other studies (28, 29). Also, dropout rates were equal in both online groups, which is of interest because the module, and thus, content differed. This is in line with the observations of Landes et al. (28).
All patients received concurrent psychiatric treatment (case management and psychopharmaceuticals) and individual psychotherapy before, as well as during the COVID-19 pandemic (during lockdown per telephone or video call). Patients were between 14 and 18 years old and mainly female. The leading diagnoses were BPD, depressive disorder, or anxiety disorder (diagnoses according to ICD-10). Non-BPD patients met at least three BPD criteria.
Given the need to continuously offer specialized care in times of COVID-19-associated restrictions on physical contact, our clinic's DBT®-A team decided to create an online offer. DBT®-A skill group sessions were conducted in a video group call format. Skype for Business (Skype Communications SARL, Luxembourg) was used as platform conforming to Austrian data safeguarding measures. The respective session link was always sent via email a day before the session.
Patients of the current DBT®-A skill group and patients new to DBT®-A, as well as all respective parents/guardians, were asked individually, per telephone or video call, whether they would participate in an online format. Two separate DBT®-A online skill groups were offered. Group 1 was transited from an existing physical group to online meetings after a COVID-19-associated break of 3 weeks (time needed for organization, preparation of technology, checking compliance to data safety regulations). Group 2 was initiated de novo online 3 weeks after the onset of Group 1. Lockdown measures were still active at the time.
Two group discussions, conceptualized to evaluate each of the online DBT®-A skill groups, were conducted online via Cisco WebEx (Webex Communications Deutschland GmbH, Germany).
Ethical approval for this investigation was granted by the institutional review board of the Medical University of Vienna (#1540/2020), and patients and guardians gave written consent prior to study participation.
DBT®-A skill group contracts were adapted so as to suit online sessions and were signed by all patients. The following methods and materials were used: (1) presentation of content by skill trainers, (2) group discussions engaging all patients, (3) chat function where applicable (e.g., group tasks), (4) worksheets (distributed via email), (5) shared files for continued group work (e.g., collective PowerPoint presentations for collection of skills manageable within the set restrictions, which were conducted with enthusiasm and creativity by the patients and the trainers, and which were presented and discussed in the next session), and (6) peer feedback. Session structure was defined so as to follow the same basic routine for both groups, although specific content varied between the two groups. This variation was owed to the fact that the first of the two online DBT®-A skill groups was transited from an existing physical group and, thus, already had prior knowledge on a range of skills, while the second group started de novo online. In order to follow the need of the moment, we decided to align content around the current module (group 1 → emotion regulation, group 2 → distress tolerance), but integrate specific content according to patients' current needs, thus, sometimes giving the group the lead and reacting spontaneously including skills from other modules. Basic session structure and specific content per group and appointment for the first five sessions (evaluation after session 5) are listed in Tables 1, 2, respectively. Upon onset of the online format, the DBT®-A team was unsure about session length (presence groups lasted for 90 min including a 15-min break), so that this was openly discussed with participants from group 1, who by then all had experience with distance learning. Consensus was reached at a session length of 60 min. In order to ensure patient safety, each patient had to name a contact (mostly parent) beforehand, who could be reached in case of emergency (this emergency procedure actually never had to be used). Contact details of patients and emergency contacts were kept “ready to use” by both skill trainers. Additionally, patients were informed that in case of emergency (acute tension, need for immediate support/action) one of the two trainers would continue the session alone, and the other would be available in a separate online meeting or via telephone.2 Sessions were prepared in a separate, weekly online meeting by the two DBT®-A skill trainers. Each session was followed by a reflection of the trainers directly after the end of the respective session. Supervision via telephone conference by an external supervisor was well-established and continued during the pandemic crisis and the according DBT®-A online format.
To our knowledge, a video group call format of a DBT® (-A) skill group has not yet been evaluated, so this investigation was set up as an exploratory pilot study. Due to the novelty of the situation, only limited prior knowledge on its effects on adolescents suffering from mental health disorders (especially emotion dysregulation, self-harm, and suicidal ideations), and a limited number of participants, we opted for a purely qualitative evaluation in the form of online group discussions and according analyses. Separate discussions were planned for each of the two online DBT®-A skills groups at our clinic after five sessions of skill training. Details of the study were explained to patients and guardians separate from details concerning the skill training sessions, and written informed consent was obtained. The group discussion sessions were configurated by a qualified research fellow and senior resident in Child and Adolescent Psychiatry, who was not involved in the treatment of the respective patients. Session links were sent per email to all participants by one of the skill trainers. At the beginning of the group discussion sessions, both skill trainers were present and introduced the moderator of the discussion. The skills trainers then logged out of the respective session and stayed available as background support per telephone or video call for any acute situations or technical problems. Immediately after the end of the respective discussions, the moderator left the meeting, and the skill trainers took over to resume and round up.
Discussions were conceptualized, moderated, and analyzed by a qualified research fellow and senior resident in Child and Adolescent Psychiatry, who was not involved in the treatment of the respective patients. The format of a group discussion, due to the shared background of the patients following the ideas of Bohnsack (30), was chosen because perceptions and opinions of participants were interpreted as being results of the process of the groups per se and were, thus, deemed to be best accessible via discussion within the established groups. Discussions followed the structure stimulus→discussion → “exmanent” questioning3→directive phase→protocol. Stimuli are understood as input material to start off the process of discussion. Most frequently, statements, videos, audio files, or pictures are being used. The main discussion is understood as exchange between the participants without intervention of the moderator. When the discussion is “exhausted,” i.e., there are no more novel contributions or long pauses, the moderator steps in to ask questions that have not been addressed by the participants, but are of relevance for the research in question. The directive phase of the discussion serves clarification; contradictory statements are being picked up by the moderator, and participants are asked for further input.
The stimulus presented in this study were verbal captions of the current situation and varied slightly between the two groups, so as to additionally encompass the fact that the transition group already had a good working alliance before the start of the online treatment, while the de novo online group had to manage this process online.
In light of the novelty of the situation and the consequent lack of prior information, in-depth qualitative analysis of discussion content was open and exploratory, applying Inductive Category Formation within the framework of Qualitative Content Analysis (Mayring) (31). Analysis was supported by the standard computerized qualitative data analysis tool ATLAS.ti 8 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). A summary description of the according analytical steps is presented in Table 3.
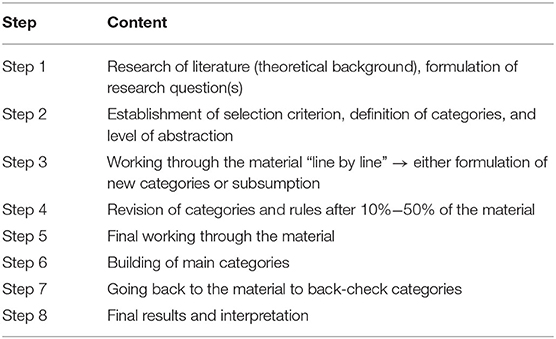
Table 3. Summary description of Inductive Category Formation (Qualitative Content Analysis) (31).
Content of the group discussions varied between the two groups, whereby group 1 engaged in a more in-depth discussion on specifics of teletherapy and benefits from the skill group, in general, and especially in times of the COVID-19 pandemic, while group 2 stayed on a more superficial level and rather focused on differential impacts of the pandemic.
Patients of both groups unanimously agreed upon the challenging character of the current situation and the need to engage in adjustment processes [“It, like, happened all at once, it was simply there, it was so overwhelming.”].4 Both groups expressed up- and downsides of lockdown measures and associated restrictions. Main themes on the positive side were the feeling of having more time (for relaxation, for reflection, for the family) [“All of a sudden I had time, time that I never had before.”] and experiencing less stress. Patients also mentioned the perception of now valuing things more (“little” things, freedom, contacts) [“I've learned to appreciate every-day life things a lot more.”], and the feeling of confronting and experimenting more (affective states, emotions and respective skills); in their view mainly attributed to fewer distractions [“The situation implied that I could not run away from my feelings that much, because I just had less distraction. Obviously, that wasn't always comfortable, but it made me get to know my emotions and deal with them.”]. Flipsides named were restrictions concerning typically applied coping strategies, boredom, self-isolation [“It was just so easy to self-isolate.”], decreased mood, less drive, and the missing of physical contacts (both in the sense of seeing them for real and being touched) with friends.
Complaints about technical problems and specific challenges of teletherapy as such, especially video calls, did not relate to group membership. Only one patient (group 1) expressed frustration concerning problems with the internet connection, but said that this was easily circumventable by intermittent use of the chat function. Additionally, one patient from group 1 and one patient from group 2 expressed overall discomfort. Issues raised were irritation due to constantly seeing oneself (video in small display window) and the feeling of potentially being overheard by family members and consequently being less open. At the same time, both of these patients stated that they valued the offer as an alternative to not being able to receive specialized treatment at all. Both clearly stated to have benefitted a lot and would just prefer real-life contacts. On the other hand, one patient mentioned feeling more comfortable with the video call setting, due to not having to hide wounds and scars, because only her head and chest could be seen. This patient added that she found it easier to apply skills in case of distress during the sessions because of the opportunity to turn off the camera for a short time.
Patients reported on having learned to recognize and label different emotions and affective states, as well as behavioral patterns. They also valued the discussion of specific strategies to deal with according distress. Patients from both groups mentioned that they were able to amplify their coping repertoire. Additionally, the interactive character and the chance to give and receive peer feedback, which patients perceived as strongly supporting transfer into everyday application of specific skills, was mentioned as beneficial [“It was so positive that we could discuss ideas and provide potential solutions within the group, so we really could give and take.”].
Reports from group 1 were more elaborated and integrated perceptions of differential changes in the structure and content of group sessions after the transition to the online format, as well as individually perceived functions of the group as such. To use the words of one of the patients, the group provided “familiarity within the unfamiliar.” Details of the compiled categories are depicted in Figure 1. To summarize the analysis, patients of the transition group benefitted from continuation of established therapy and assigned a range of subjective functions of the group as such. The transition into an online setting worked for all of these patients and was reflected in the context of “change”; situational adaptions were mirrored in perceptions of changed structure and content of the group sessions. One of our patients summarized: “The mundane structure I was used to and, due to Corona, did not have anymore, was filled with this subtle but very helpful appointment.”
Concerning the level of psychosocial functioning, all patients managed to stay socially integrated (with all limits imposed by the set restrictions) and to keep up with school, i.e., all patients made their grades; one even the school ending exam (“Matura”).
The COVID-19-pandemic had, and still has, a huge impact on people worldwide and not only demanded adaptions from individuals and systems but also required immense situational adjustment. Specific subpopulations, such as individuals suffering from psychiatric disorders, have been suspected to have an increased risk of deterioration in their mental health status, although limited data are available differentially evaluating potential consequences of the crisis (32, 33). All else put aside, current outpatients were confronted with the fact that measures set to ensure minimum spreading of SARS-CoV-2 imposed considerable changes in the availability of established treatment, ranging from treatment pause to an ad hoc switch to teletherapy (e.g., telephone, video calls). Data on the provision of DBT® and consequences for patients suffering from BPD during COVID-19 suggest serious consequences, especially reduced numbers treated and changes in structure and content of therapy (34). Although teletherapy generally seems to be beneficial (35, 36), many countries were unprepared for it due to lacking legal frameworks, lacking prior approval on the conductance of teletherapy by legal authorities and professional organizations, and lacking clarity concerning cost coverage or reimbursement (22). Interestingly, even in countries with preexisting regulations on tele (mental) health, such as the United States, many mental health professionals had not used telemental health before the outbreak of the COVID-19 pandemic, whereby data safety and a lack of preparedness for handling emergency situations seem to have been the main concerns (23). Regulations in our country precluded video-calls as a legitimate treatment alternative so that the patients assessed in this study had no prior experience with teletherapeutic offers. When offered the option to participate in an internet-based video call format, only one patient from our ongoing physical group declined, so that we could assess the transition aspect—face to face switched to teletherapy—in this established group. Additionally, we invited patients new to us and to DBT-A to join a second de novo online skill group, which enabled us to assess the process of forming a group online and explore challenges in conveying DBT®-A skills via this format.
Concerning participation, we lost two patients due to dropouts. This number did not differ from recorded dropouts in our physical groups and is in line with rates reported in other studies (29).
Although this study is exploratory, and results are drawn from a small sample, we provided evidence for a differentiated view on the impact of the COVID-19 pandemic on adolescent psychiatric outpatients. Although perceiving the situation as challenging, patients not only named downsides but also numerous positive consequences during lockdown. Concerning technical aspects, the situation was challenging for both therapists and patients, although only one patient elaborated this aspect in the group discussion. As skill trainers, we decided to include the chat function of our video call platform to keep collaboration and exchange going in case of problems, which was valued by participants (e.g., a note that a patient will turn off the camera in case of the need to apply skills during the session, unstable internet connection, or quality problems with video and sound). Patients of the transition group could also be evaluated concerning the perception and acceptance of changes in content and structure. The feedback was very positive concerning both changes in content and structure. Patients stated that the sessions became more interactive than the physical meetings, and they especially valued extensive peer discussions and peer feedback, which we encouraged in order to give room for group exchange on pandemic-related topics. This “togetherness” was also directly addressed in the group discussions. Interestingly, also group 2, who only got to know each other online, stated feeling “connected” and also put emphasis on the group providing an anchor, something to hold onto.
Regarding patient safety, a meeting was arranged, and in consent with the patient, the patient's individual therapist was contacted in order to ensure continued treatment. One patient dropped out after the third session because her internet connection failed repeatedly, and she was neither able to interact, nor to follow the content.
Generalization of results is limited by the sample size and characteristics, the exploratory character, and the consequently applied qualitative methodology. Also, only five sessions of the online DBT®-A skill group have been evaluated.
Despite the abovementioned limitations, in our assessment, DBT®-A skill training via internet-based video group call proved to be safe and beneficial for adolescents with emotion dysregulation. This result is especially relevant since many therapists are concerned about their ability to handle emergency situations in a telemental health setting (23). Our results indicate that an online format might be an alternative to face-to-face group sessions if these are not possible. This is obviously interesting concerning future situations of quarantine, especially further waves of the current pandemic, but potentially also for service provision in remote areas, where highly specialized treatment often is not available.
In spite of the encouraging character of these results, further research is necessary to challenge and refine our findings, especially in the sense of a direct comparison of online vs. face-to-face DBT®-A skill groups, to assess suitability as alternative to or augmentation of face-to-face treatment in a more general context aside from quarantine. Despite the availability of smartphones and internet connection, technical difficulties, especially concerning speed and stability of the connection, have been raised by our patients, so that investment in enhancing availability of adequate technologies is necessary. Additionally, extensions of the video group call format, such as “break-out sessions” (i.e., parallel video sessions) for teamwork, real-time inclusion of an external supervisor or blended therapy has to be considered, in order to further test the potential of this format. Also, combinations with other technologies, such as virtual reality (e.g., Virtual Reality Mindfulness), should be explored within online DBT®(-A) (23).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Review Board of the Medical University of Vienna. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
MB, TG, and PP conceptualized the study. MB and VW conveyed the DBT-A treatment analyzed. TG planned and conducted the focus groups and according qualitative data analyses. MB, AB, OK, and PP all contributed to writing the manuscript. All authors contributed to the article and approved the submitted version.
MB has received research funding from the Medical Scientific Fund of the Mayor of the City of Vienna. PP has received research funding from Lundbeck and Servier. He has received a speaker's honorarium from Shire.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are extremely grateful to our patients for their spirit during the experiment DBT-A skill group online and their enthusiastic participation in its evaluation.
1. ^All patients also had individual therapy, which was not evaluated within this study.
2. ^We twice had to make use of this option. In both cases (once in group 1 and once in group 2), patients could be reached on their smartphones and rejoined the running session.
3. ^“Exmanent” questioning translates into the moderator actively asking about topics that have not yet been addressed, but are relevant to the research question(s).
4. ^For illustration, patient quotes are inserted in square brackets.
1. McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. (2011) 49:544–54. doi: 10.1016/j.brat.2011.06.003
2. Ibraheim M, Kalpakci A, Sharp C. The specificity of emotion dysregulation in adolescents with borderline personality disorder: comparison with psychiatric and healthy controls. Borderline Personal Disord Emot Dysregul. (2017) 4:1. doi: 10.1186/s40479-017-0052-x
3. Bunford N, Evans SW, Langberg JM. Emotion dysregulation is associated with social impairment among young adolescents with ADHD. J Attent Disord. (2018) 22:66–82. doi: 10.1177/1087054714527793
4. Ajetunmobi O, Taylor M, Stockton D, Wood R. Early death in those previously hospitalised for mental healthcare in Scotland: a nationwide cohort study, 1986-2010. BMJ Open. (2013) 3:e002768. doi: 10.1136/bmjopen-2013-002768
5. Scott LN, Pilkonis PA, Hipwell AE, Keenan K, Stepp SD. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: a multi-wave prospective study. Compr Psychiatry. (2015) 58:1–10. doi: 10.1016/j.comppsych.2014.12.011
6. Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. (2016) 46:225–36. doi: 10.1017/S0033291715001804
7. Wolff JC, Thompson E, Thomas SA, Nesi J, Bettis AH, Ransford B, et al. Emotion dysregulation and non-suicidal self-injury: a systematic review and meta-analysis. Eur Psychiatry. (2019) 59:25–36. doi: 10.1016/j.eurpsy.2019.03.004
8. Glenn CR, Esposito EC, Porter AC, Robinson DJ. Evidence base update of psychosocial treatments for self-injurious thoughts and behaviors in youth. J Clin Child Adolesc Psychol. (2019) 48:357–92. doi: 10.1080/15374416.2019.1591281
9. Kothgassner OD, Robinson K, Goreis A, Ougrin D, Plener PL. Does treatment method matter? A meta-analysis of the past 20 years of research on therapeutic interventions for self-harm and suicidal ideation in adolescents. Borderline Personal Disord Emot Dysregul. (2020) 7:9. doi: 10.1186/s40479-020-00123-9
10. McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, et al. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: a randomized clinical trial. JAMA Psychiatry. (2018) 75:777–85. doi: 10.1001/jamapsychiatry.2018.1109
11. Mehlum L, Ramleth RK, Tørmoen AJ, Haga E, Diep LM, Stanley BH, et al. Long term effectiveness of dialectical behavior therapy versus enhanced usual care for adolescents with self-harming and suicidal behavior. J Child Psychol Psychiatry. (2019) 60:1112–22. doi: 10.1111/jcpp.13077
13. Rathus JH, Miller AL. Dialectical behavior therapy adapted for suicidal adolescents. Suicide Life Threat Behav. (2002) 32:146–57. doi: 10.1521/suli.32.2.146.24399
14. Auer AKv, Bohus M editors. Interaktives Skillstraining für Jugendliche mit Problemen der Gefühlsregulation (DBT-A®). Das Therapeutenmanual. 1 ed. Stuttgart, Germany: Schattauer; (2017).
15. Miller AL, Rathus JH, Linehan MM. Dialectical Behavior Therapy® with Suicidal Adolescents. New York: The Guilford Press;. (2017) 346 p.
16. Cui Y, Li Y, Zheng Y, Chinese Chinese Society of C, Adolescent P. Mental health services for children in China during the COVID-19 pandemic: results of an expert-based national survey among child and adolescent psychiatric hospitals. Eur Child Adolesc Psychiatry. (2020) 29:743–8. doi: 10.1007/s00787-020-01548-x
17. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. (2020) 14:20. doi: 10.1186/s13034-020-00329-3
18. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
19. Iob E, Steptoe A, Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatry. (2020) 217:543–6. doi: 10.1192/bjp.2020.130
20. Torous J, Jan Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health. (2020) 7:e18848. doi: 10.2196/18848
21. Witt A, Ordóñez A, Martin A, Vitiello B, Fegert JM. Child and adolescent mental health service provision and research during the Covid-19 pandemic: challenges, opportunities, and a call for submissions. Child Adolesc Psychiatry Ment Health. (2020) 14:19. doi: 10.1186/s13034-020-00324-8
22. Nittari G, Khuman R, Baldoni S, Pallotta G, Battineni G, Sirignano A, et al. Telemedicine practice: review of the current ethical and legal challenges. Telemed J E Health. (2020) 26:1427–37. doi: 10.1089/tmj.2019.0158
23. Sampaio M, Haro MVN, De Sousa B, Melo WV, Hoffman HG. Therapists make the switch to telepsychology to safely continue treating their patients during the COVID-19 pandemic. Virtual reality telepsychology may be next. Front Virtual Real. (2021) 1:576421. doi: 10.3389/frvir.2020.576421
24. Little H, Tickle A, das Nair R. Process and impact of dialectical behaviour therapy: a systematic review of perceptions of clients with a diagnosis of borderline personality disorder. Psychol Psychother. (2018) 91:278–301. doi: 10.1111/papt.12156
25. Neacsiu AD, Rizvi SL, Linehan MM. Dialectical behavior therapy skills use as a mediator and outcome of treatment for borderline personality disorder. Behav Res Ther. (2010) 48:832–9. doi: 10.1016/j.brat.2010.05.017
26. Zeifman RJ, Boritz T, Barnhart R, Labrish C, McMain S. The independent roles of mindfulness and distress tolerance in treatment outcomes in dialectical behavior therapy skills training. Personal Disord. (2019) 11:181–90. doi: 10.1037/per0000368
27. Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry. (2015) 72:475–82. doi: 10.1001/jamapsychiatry.2014.3039
28. Landes SJ, Chalker SA, Comtois KA. Predicting dropout in outpatient dialectical behavior therapy with patients with borderline personality disorder receiving psychiatric disability. Borderline Personal Disord Emot Dysregul. (2016) 3:9. doi: 10.1186/s40479-016-0043-3
29. Dixon LJ, Linardon J. A systematic review and meta-analysis of dropout rates from dialectical behaviour therapy in randomized controlled trials. Cogn Behav Ther. (2020) 49:181–96. doi: 10.1080/16506073.2019.1620324
30. Bohnsack R. Rekonstruktive Sozialforschung: Einführung in qualitative Methoden. 5 ed. Opladen: Leske Budrich; (2003). 288 p. doi: 10.1007/978-3-322-89614-8
31. Mayring P. Qualitative Inhaltsanalyse. Grundlagen und Techniken. 12 ed. Weinheim: Beltz;. (2015) 152 p.
32. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. (2020) 77:891–2. doi: 10.1001/jamapsychiatry.2020.0894
33. Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:e21. doi: 10.1016/S2215-0366(20)30090-0
34. Lakeman R, Crighton J. The impact of social distancing on people with borderline personality disorder: the views of dialectical behavioural therapists. Issues Ment Health Nurs. (2020) 42:410–6. doi: 10.1080/01612840.2020.1817208
35. Vigerland S, Lenhard F, Bonnert M, Lalouni M, Hedman E, Ahlen J, et al. Internet-delivered cognitive behavior therapy for children and adolescents: a systematic review and meta-analysis. Clin Psychol Rev. (2016) 50:1–10. doi: 10.1016/j.cpr.2016.09.005
Keywords: DBT-A, skills group, COVID-19, emotion dysregulation, teletherapy, online, video
Citation: Bock MM, Graf T, Woeber V, Kothgassner OD, Buerger A and Plener PL (2022) Radical Acceptance of Reality: Putting DBT®-A Skill Groups Online During the COVID-19 Pandemic: A Qualitative Study. Front. Psychiatry 13:617941. doi: 10.3389/fpsyt.2022.617941
Received: 15 October 2020; Accepted: 23 February 2022;
Published: 25 April 2022.
Edited by:
Eva Moehler, Saarland University Hospital, GermanyReviewed by:
Hunter Hoffman, University of Washington, United StatesCopyright © 2022 Bock, Graf, Woeber, Kothgassner, Buerger and Plener. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mercedes M. Bock, bWVyY2VkZXMuaHVzY3NhdmFAbWVkdW5pd2llbi5hYy5hdA==
†ORCID: Mercedes M. Bock orcid.org/0000-0003-0089-5505
Theres Graf orcid.org/0000-0003-3790-4911
Verena Woeber orcid.org/0000-0001-9245-5149
Oswald D. Kothgassner orcid.org/0000-0002-3243-0238
Arne Buerger orcid.org/0000-0002-5203-6510
Paul L. Plener orcid.org/0000-0003-4333-1494
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.