
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 15 December 2022
Sec. Aging Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1091042
This article is part of the Research Topic Resilience in Chronic Disease, volume II View all 8 articles
Introduction: Prenatal psychological distress is prevalent during pregnancy. This study aimed to estimate the associations among fear of childbirth, resilience and psychological distress.
Methods: A total of 1,060 Chinese pregnant women were enrolled from Be Resilient to Postpartum Depression (ChiCTR2100048465) and the following instruments were administered to them: Childbirth Attitudes Questionnaire, Connor-Davidson Resilience Scale, Perceived Social Support Scale, General Self-Efficacy Scale, Adverse Childhood Experience scale and Hospital Anxiety and Depression Scale. A dominance, a response surface analysis and a moderated mediation analysis were performed.
Results: In terms of psychological distress, resilience and fear of childbirth could explain 41.6% (0.148/0.356) and 33.1% (0.118/0.356), respectively. Pregnant women with high resilience-low fear of childbirth had significantly lower levels of psychological distress than those with low resilience-high fear of childbirth. The indirect effects of fear of childbirth on psychological distress through resilience was significantly (B = 0.054, 95% CI 0.038 to 0.070). The interactions between fear of childbirth and adverse childhood experiences (β = 0.114, 95% CI −0.002 to 0.231, p = 0.054) and between resilience and adverse childhood experiences (β = −0.118, 95% CI −0.222 to −0.012, p < 0.05) were significant.
Conclusion: Resilience, fear of childbirth and adverse childhood experiences may be three important factors to psychological distress in Chinese pregnant women.
Depression and anxiety, termed here “psychological distress” are a health issue for pregnant women, that are associated with negative repercussions in the offspring and maternal health (1–3).
Psychological distress is globally reported for pregnant women due to all kinds of challenges and changes (4) and a recent meta-analysis reported that the pooled prevalence of anxiety and depression was 30.5% and 25.6%, respectively (5).
Previous studies have found that psychological distress are related to socio-demographic factors and psychological variables. In terms of socio-demographics, family economic status, education level, occupation, and pregnancy planning status have been confirmed to be significantly associated with psychological distress (6–8). Moreover, research has shown self-efficacy to be negatively correlated with fear of childbirth (FOC) and psychological distress but positively correlated with resilience (9–11). Meanwhile, it’s been confirmed that social support is essential for the development of resilience and can act as a buffer against FOC and psychological distress (12–15). However, FOC is a particularly important risk factor for psychological distress among these psychological variables. A cohort study of 545 participants found that pregnant women with a high degree of FOC are more likely to have elevated psychological distress (16).
Adverse childhood experiences (ACEs) are characterized by exposure to abuse, neglect, and family dysfunction (17). It has been widely proved that ACEs had long-term impact on health status later in life, such as substance use patterns, coronary heart disease, depressive symptoms, post-traumatic stress disorder and so on (18–21). For pregnant women, a wealth of existing evidence has indicated ACEs confer risk to psychological distress during pregnancy (22–24). Even though the literature on the effects of FOC and ACEs on maternal psychological distress is robust, researchers commonly ignore protective and positive factors, such as resilience.
Resilience is a dynamic process that represent one’s ability to adapt successfully to challenges and to thrive in the face of adversity (25, 26). Prior studies suggested that resilience has a protective effect on psychological distress during pregnancy (27–29). Furthermore, in a Chinese study involving 646 pregnant women has shown that resilience was negatively associated with FOC (30). Meanwhile, a recent research found that resilience served as a moderator between ACEs and psychological distress among pregnant women (22). However, the researches measuring resilience in Chinese pregnant women and related effects on psychological distress are still scarce. The potential relationship of FOC, resilience, ACEs and psychological distress has not been systematically examined among pregnant women in previous studies. Therefore, this study hypothesized that
(1) FOC and resilience would be significant predictors of psychological distress;
(2) Resilience mediated the association between FOC and psychological distress;
(3) ACEs may play a moderation role among FOC, resilience and psychological distress.
One thousand and sixty pregnant women in our ongoing Be Resilient to Postpartum Depression (BRPD) cohort were recruited between January 2022 and April 2022. Fifty-eight were excluded due to missing questionnaires, resulting in a final sample of 1002 (response rate 94.5%). The inclusion criteria were: (1) more than 18 years old; (2) pregnancy confirmed by ultrasonography; (3) could communicate fluently in Mandarin; (4) willing to participate in this study. The exclusion criteria was: (1) women with mental illness; (2) plan to terminate pregnancy. Written consent was obtained before the formal investigation.
Based on previous literature (6, 31), we collected demographics (age, academic degree, marital status, working status, monthly average income, place of residence) and pregnancy-related information (maternity type, pregnancy type, weeks of pregnancy).
The Childbirth Attitudes Questionnaire (CAQ), used to evaluate fear related to childbirth, was developed by Lowe (32). The CAQ contains 16 items and 4 dimensions (baby-related, pain and injury-related, general and personal control-related, medical interventions and hospital care-related fears). The sum score ranges from 16 to 64, with higher scores indicating more severe FOC. The validity and reliability of the Chinese version of the CAQ has been validated in pregnant women in China (14, 33). The Cronbach’s alpha for CAQ in the present study was 0.950.
The 25-item Connor-Davidson Resilience Scale (CD-RISC) was developed by Connor and Davidson (34) and a 10-item version was later shortened and validated by Campbell-Sills and Stein (35). The Chinese version of CD-RISC 10 (36) consists of 10 items and ranges from 0 to 40, with higher scores indicating higher resilience levels. This scale has been successfully administered in our previous studies (37–41). The Cronbach’s alpha in the present study was 0.921.
The Perceived Social Support Scale (PSSS) was used to measure perceived support from family, friends, and others (42). It is a 7-Likert scale (1–7, definitely disagree to definitely agree) with high scores indicating a high level of social support. The Chinese version has been shown to have good reliability and validity in the maternal population (43, 44). The Cronbach’s alpha in the present study was 0.957.
The General Self-efficacy Scale (GSES) was developed by Zhang and Schwarzer (45), and the Chinese version has been proved to be reliable when employed in Chinese pregnant women (10, 11). The scale includes 10 items and is rated on a 4-point-Likert scale ranging from 10 to 40. A higher score indicates a higher degree of self-efficacy. The Cronbach’s alpha for GSES in the present study was 0.943.
Adverse Childhood Experience scale (ACE) was used to measured adverse childhood experiences during the respondent’s first 18 years of life (46). It includes 10 items under three categories: household dysfunction (5 items), abuse (3 items) and neglect (2 items) and were binary (yes vs. no). We categorized adverse childhood experiences into dichotomous outcomes – not experienced (score = 0, coded as 0) and experienced (score ≥ 1, coded as 1). The Chinese version of the ACEs scale was translated by Dr. David Yeung (47) and has been widely used in ACE researches (48, 49).
Hospital Anxiety and Depression Scale (HADS), developed by Zigmond and Snaith (50), was used to assess psychological distress levels, including two dimensions: anxiety (7 items) and depression (7 items). It employs a 4-point scoring method (0–3) yielding a total score range of 0-42, with higher scores representing a higher degree of psychological distress (51). The Chinese version of HADS has been approved to be reliable (52, 53). The Cronbach’s alpha for HADS in the present study was 0.816.
First, descriptive analysis was used to describe the demographics and pregnancy-related information. In addition, Pearson’s correlation analysis was performed to determine the relationships among resilience, perceived social support, self-efficacy, fear of childbirth and psychological distress.
Second, dominance analysis was conducted in order to determine the relative importance of resilience, perceived social support, self-efficacy, and fear of childbirth on psychological distress in this study. In this analysis all the model predictors were compared to each other and ranked by their relative importance (54). Dominance analysis is based on estimating an △R2 value for all possible subset models, so we conducted 37 regression analyses to compare predictors’ weight.
Third, polynomial regression with moderated response surface analysis (RSA) was performed to test the congruent and discrepant effects of pregnant women’s resilience and fear of childbirth on their psychological distress level (55). This regression consists of ten predictors: (1) resilience, (2) FOC, (3) resilience *resilience, (4) resilience * FOC, (5) FOC * FOC 2, (6) ACE, (7) ACE * resilience, (8) ACE * FOC, (9) ACE * resilience * resilience, (10) ACE * resilience * FOC, (11) ACE * FOC * FOC.
Fourth, Harman’s one-factor model was adopted to estimate potential existence of the common method variance [CMV, (56)]. Then, the mediator role of resilience was evaluated between FOC and psychological distress through the PROCESS macro (Model 4) of SPSS.
Fifth, a moderation analysis was employed to examine the moderating role of ACE on the associations among fear of childbirth, resilience and psychological distress through the PROCESS macro (Model 5, 7, 14) of SPSS.
R 3.3.2 (57) and SPSS 26.0 (IBM Corp., Armonk, NY, United States) were used for all statistical analyses.
The present study was part of BRPD (Registration number: ChiCTR2100048465) and was approved by the ethics review committee of the participating hospital (No: K-2022-024). The participants were reassured that their personal data would be kept confidentially and used for academic research anonymously.
Among the 1002 women in the present study, the mean age was 29.59 years (SD = 4.16), and 95.1% of pregnant women were married. More than half (67.9%) were in employment status and one in ten had an unplanned pregnancy. Other details were demonstrated in Table 1.
The results of the dominance analysis of four predictors (model 1, P = 4, Table 2) including resilience (X1), perceived social support (X2), self-efficacy (X3) and FOC (X4), showed that resilience, perceived social support, self-efficacy and FOC accounted for 33.0% (0.125/0.379), 18.7% (0.071/0.379), 19.0% (0.072/0.379) and 29.3% (0.111/0.379) of the total variance, respectively. A further dominance analysis (model 2, P = 3, Table 3) revealed that resilience (41.6% of the total variance) was the strongest predictor to psychological distress, followed by FOC (33.1% of the known variance) and self-efficacy (25.3% of the known variance). Thus, resilience, FOC and psychological distress were included in the following response surface analysis.
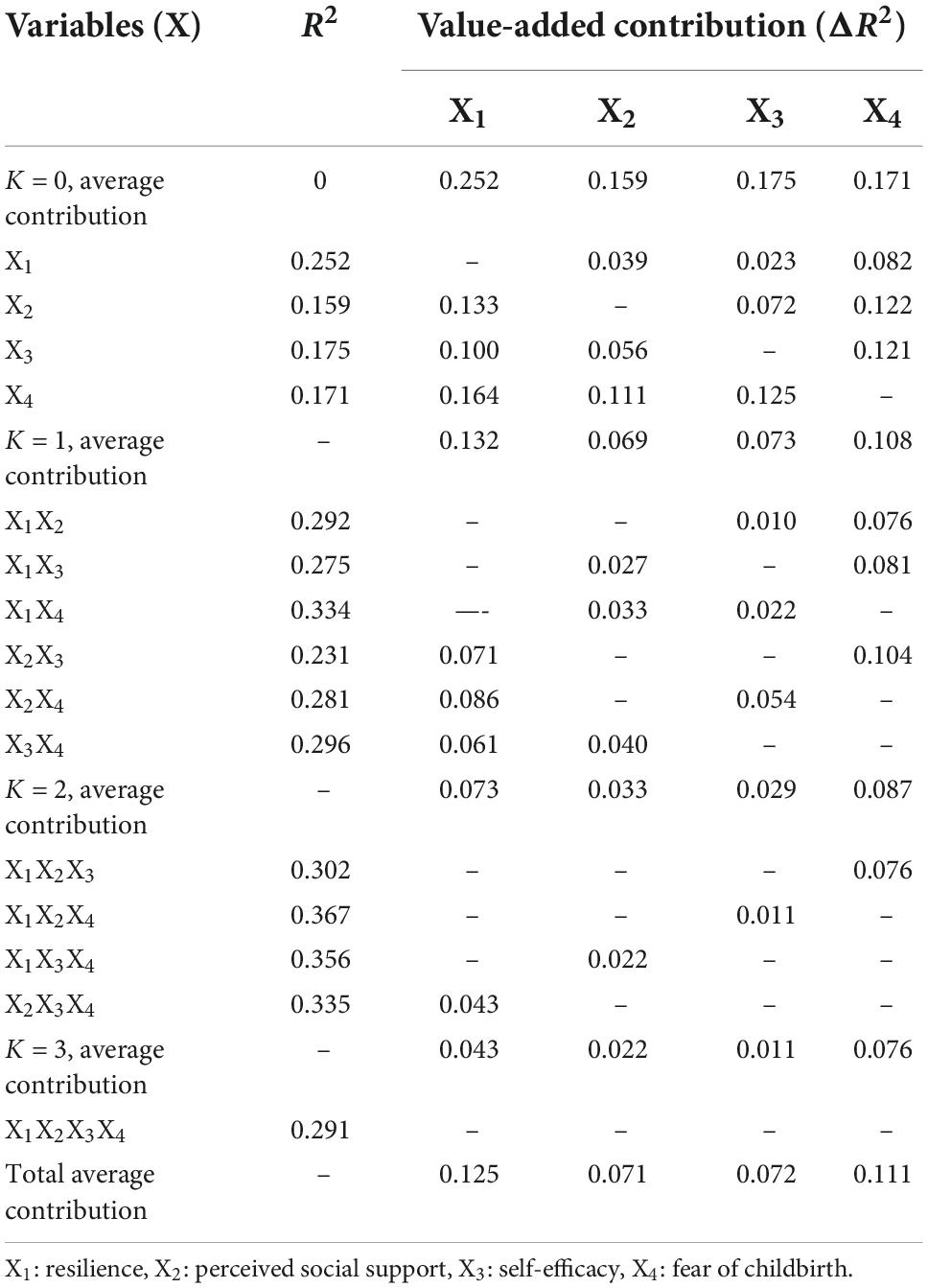
Table 2. When P = 4, the value-added contribution, average contribution and total average contribution of each predictor variable.

Table 3. When P = 3, the value-added contribution, average contribution and total average contribution of each predictor variable.
In the absence of ACEs, the result of the response surface analysis was presented in Figure 1A. Along the congruence line X = Y, psychological distress in the posterior corner (high FOC - high resilience) was significantly lower than that in the anterior corner (low FOC -low resilience), indicating that when the FOC was balanced with their resilience, pregnant women’s psychological distress level was lowest in the double-high combination. Along the discrepancy line X = –Y, psychological distress in the left corner of the graph (low FOC - high resilience) was significantly lower than those in the right corner of the graph (high FOC - low resilience), indicating that resilience had a more positive effect on psychological distress than the negative effect of FOC. A similar pattern emerged in pregnant women who experienced ACEs (Figure 1B). Besides, pregnant women with ACEs reported higher levels of psychological distress compared to those without ACEs.
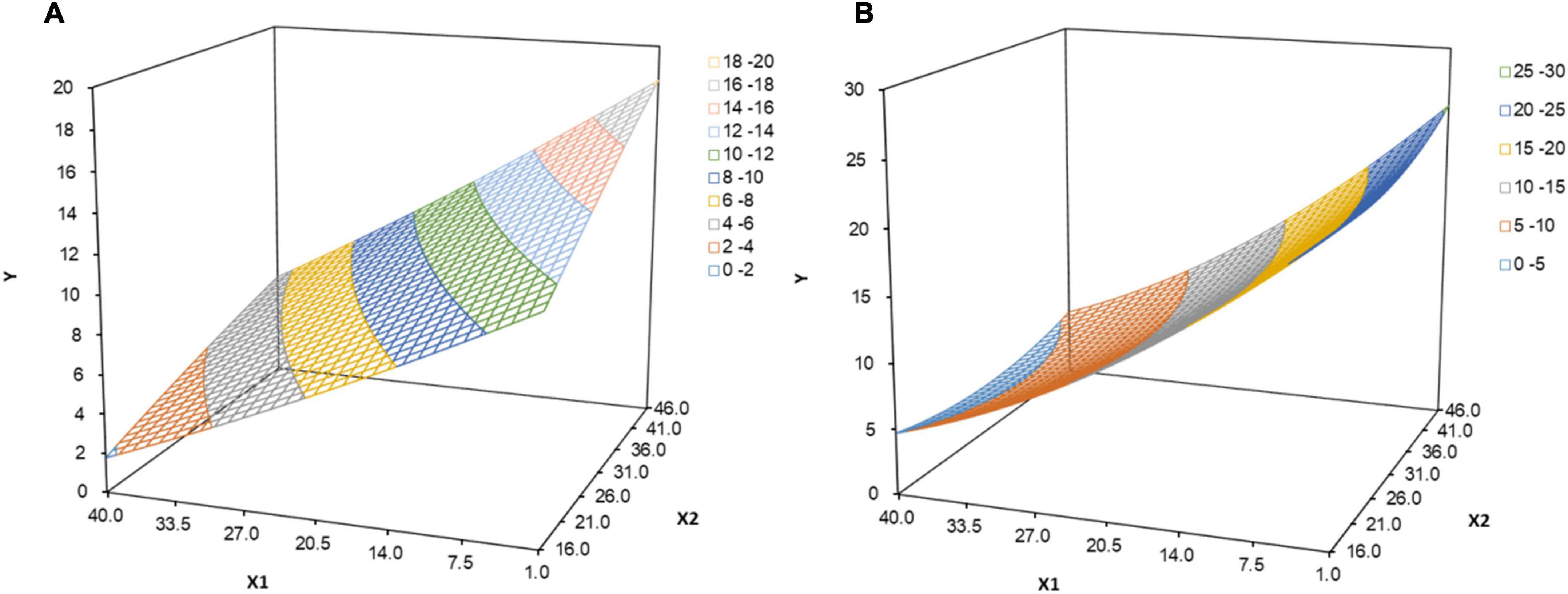
Figure 1. (A) In the absence of adverse childhood experiences, the effect of resilience and fear of childbirth on psychological distress. X1: resilience, X2: fear of childbirth, Y: psychological distress. (B) When having adverse childhood experiences, the effect of resilience and fear of childbirth on psychological distress. X1: resilience, X2: fear of childbirth, Y: psychological distress.
The variance explained by the first factor was 27.6% and did not reach 50%, so the common method bias was negligible. Psychological distress was significantly correlated with resilience (r = –0.516, P < 0.001) and FOC (r = 0.438, P < 0.001). Other information was summarized in Figure 2A. Figure 2B revealed that FOC was negatively associated with resilience (β = –0.182, P < 0.001); resilience had a significant impact on anxiety (β = –0.124, P < 0.001, Figure 3A), depression (β = –0.170, P < 0.001) and psychological distress (β = –0.295, P < 0.001, Figure 3C). In Figure 2C, the indirect effect of FOC through resilience on psychological distress were significant (B = 0.054, SEBoot = 0.008, 95%CI: 0.08, 0.014), including anxiety (B = 0.023, SEBoot = 0.004, 95%CI: 0.016, 0.030, Figure 3B) and depression (B = 0.031, SEBoot = 0.005, 95%CI: 0.022, 0.041, Figure 3D).
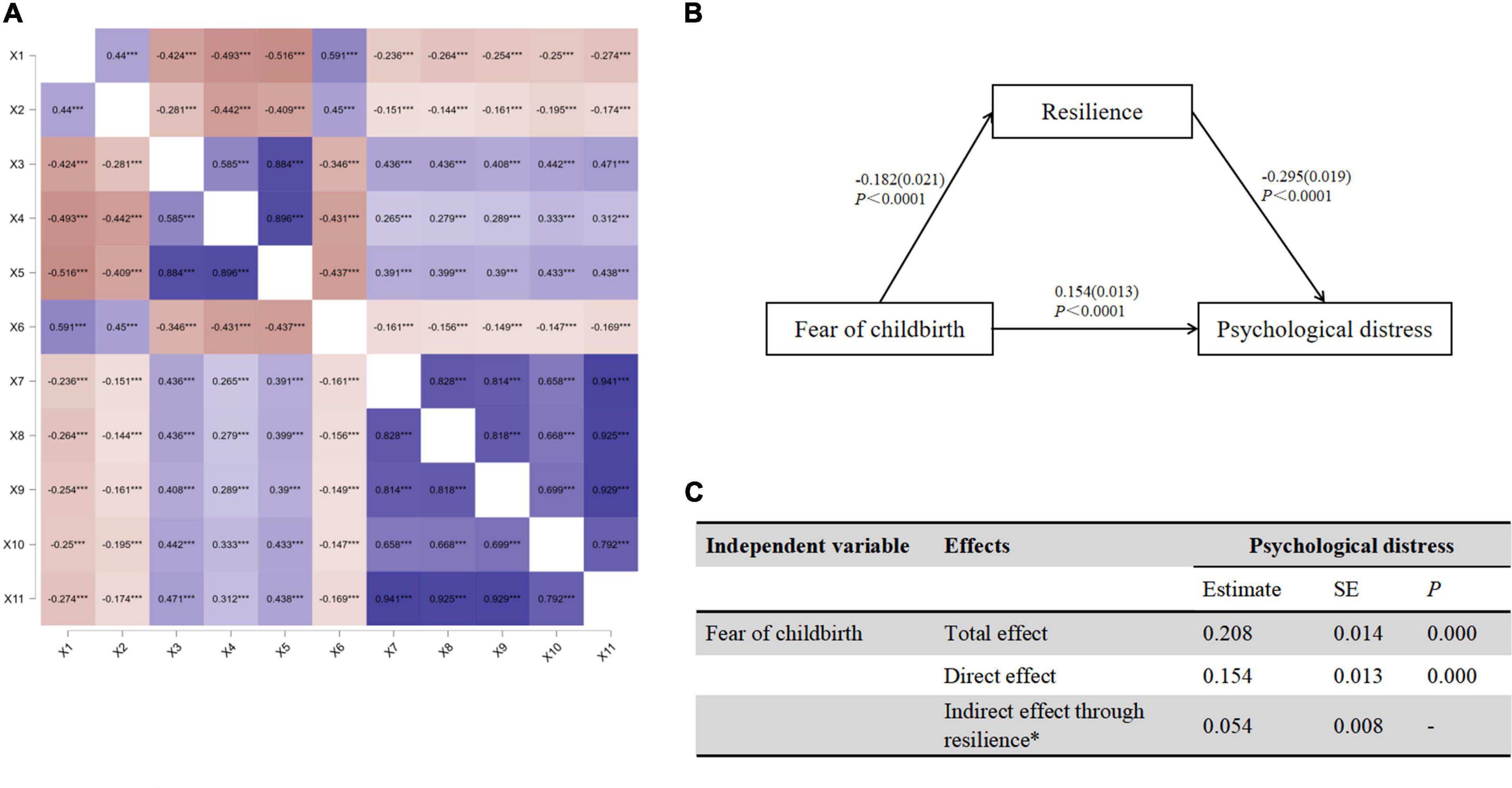
Figure 2. (A) Correlations between variables. (B) The mediating effect of resilience on psychological distress. (C) Direct and indirect (mediation) effect of resilience on psychological distress. X1: resilience, X2: perceived social support, X3: anxiety, X4: depression, X5: psychological distress, X6: self-efficacy, X7: baby-related FOC, X8: general and personal control-related FOC, X9: pain and injury-related FOC, X10: medical interventions and hospital care-related FOC, X11: Fear of childbirth. ***Correlation is significant at the 0.001 level.

Figure 3. (A) The mediating effect of resilience on anxiety. (B) Direct and indirect (mediation) effect of resilience on anxiety. (C) The mediating effect of resilience on depression. (D) Direct and indirect (mediation) effect of resilience on depression.
The results of the moderation analysis were depicted in Tables 4–6. The interaction of FOC and ACEs was not significant (B = –0.036, 95%CI: –0.104 to 0.031, P = 0.291, Table 4), indicating that ACEs did not moderate the relationship between FOC and psychological distress. The significant moderation effect of ACEs was recognized (B = 0.114, 95%CI: –0.002 to 0.231, P = 0.054, Table 5) and visualized in the simple slopes test (Bno = –0.195, P < 0.001; Byes = –0.084, P = 0.140, Figure 4A). In Table 6, ACEs could significantly moderate the association between resilience and psychological distress (Bno = –0.276, P < 0.001; Byes = –0.393, P < 0.001, Figure 4B).
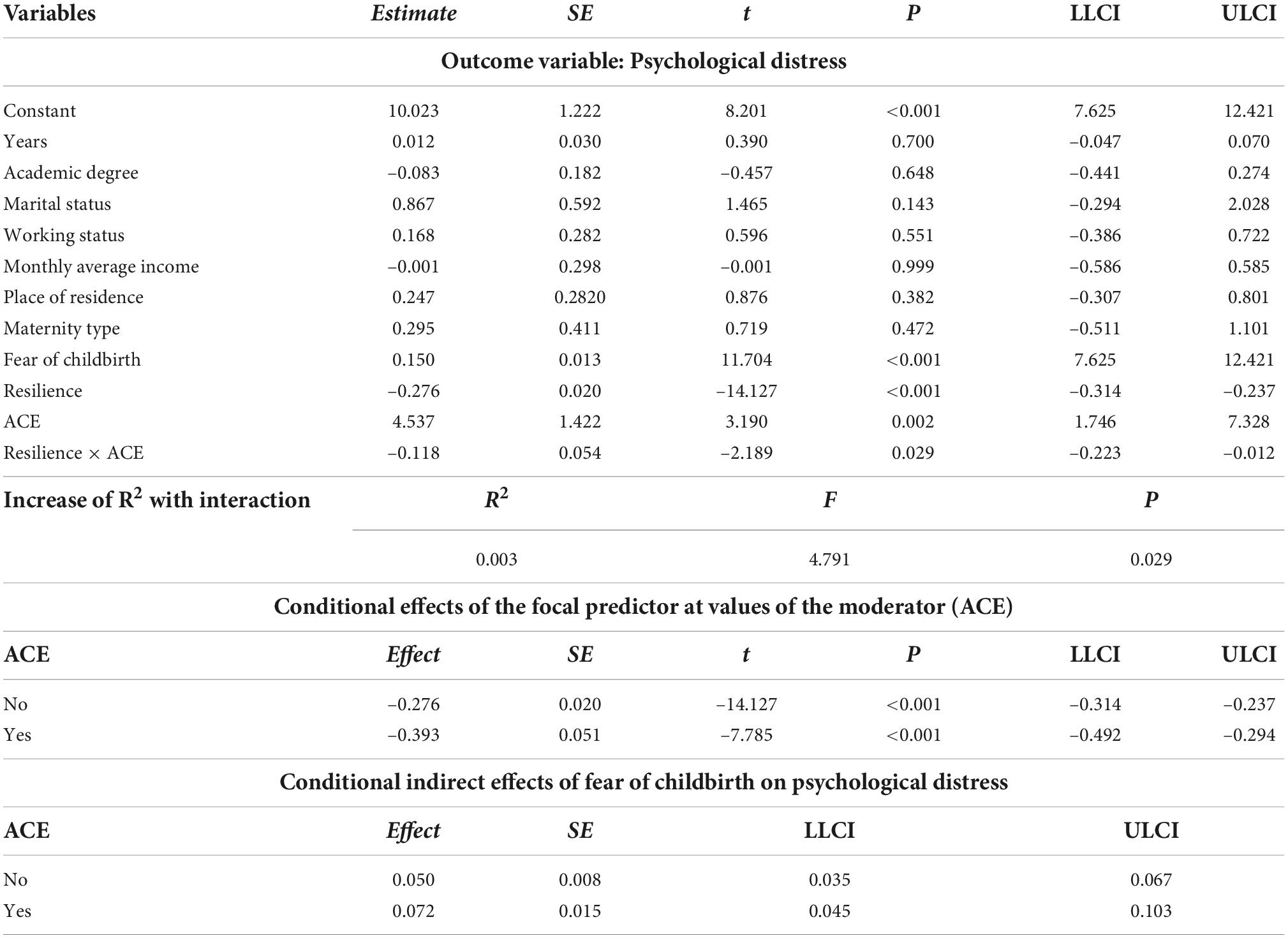
Table 6. The moderated effect of ACEs on the association between resilience and psychological distress.
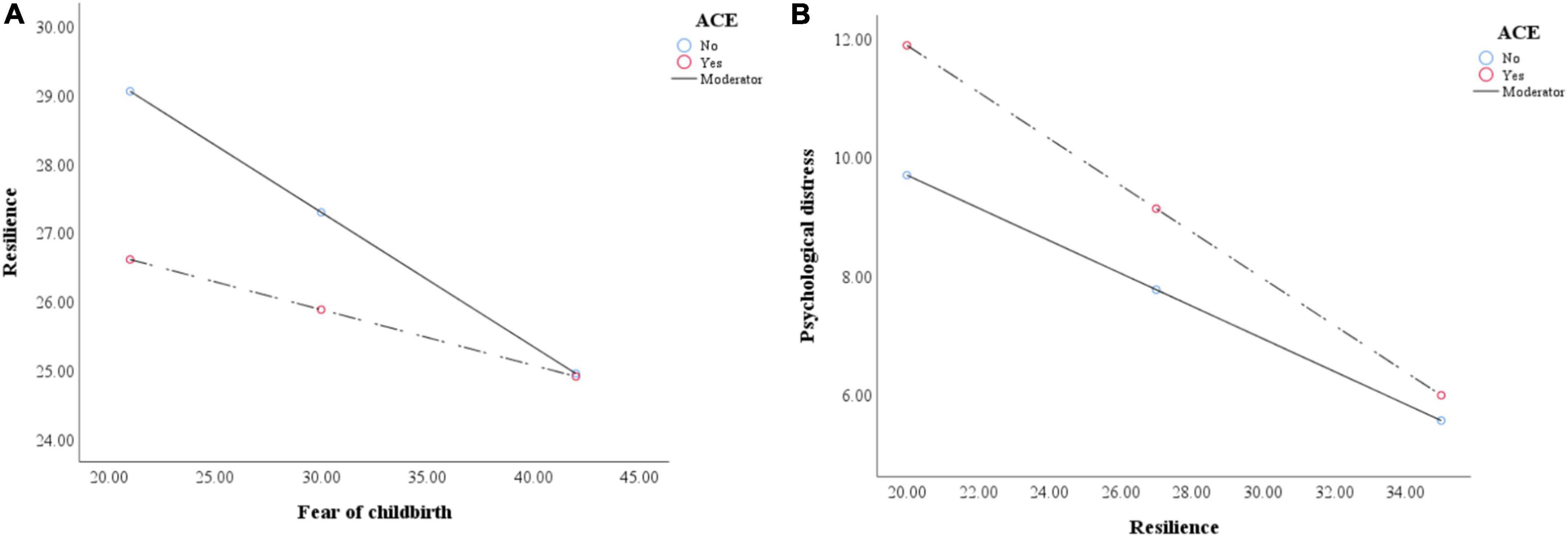
Figure 4. (A) The interaction between fear of childbirth and ace on resilience. (B) The interaction between resilience and ace on psychological distress.
The current study examined the associations among FOC, resilience, ACEs and psychological distress in Chinese pregnant women. Specifically, we utilized dominance analysis, response surface analysis and moderated mediation model to test the effects of FOC, resilience, and ACEs on psychological distress.
First, FOC was positively associated with psychological distress in the current study, which was consistent with previous literature (58, 59). As FOC is defined as severe fear, anxiety or concern specifically in relation to childbirth (60), it may not be surprising that psychological distress was associated with higher FOC. However, the reasons for FOC are complex and unique and women with high to severe FOC is not recognized in maternity care in many countries. Hence, identifying pregnant women with high FOC may be the first step to help them build confidence in giving birth and improve their mental health.
Second, response surface results indicated that when resilience and FOC were congruent and high, pregnant women’s psychological distress level is significantly lower than the low resilience -low FOC model. In other words, a high level of FOC could be buffered by high resilience and pregnant women’s mental health will not be severely damaged. Furthermore, the effects of discrepancy in resilience and FOC on psychological distress suggested that low resilience – high FOC leads to higher psychological distress, while high resilience – low FOC promotes better mental health, indicating that resilience plays a significant role. These results were consistent with Huang’s findings (30) that pregnant women with high resilience may actively use their own psychological resources to reduce fear and ultimately maintain better mental health.
Third, the mediation model showed that resilience significantly mediated the relationship between FOC and psychological distress, which was partially confirmed in previous research (11). According to the pathway of FOC → resilience → psychological distress, it is essential that strategies to promote resilience in pregnant women need to be developed and implemented to counter the impact of FOC on psychological distress. There already exist resilience-enhancing programs for pregnant women. For instance, Witteveen et al. developed a guided self-help ACT-based program for pregnant and the psychological distress symptoms were alleviated (61). In addition, resilience-based interventions have also been trialed on patients. For example, Ye et al. developed the program Be Resilient to Breast Cancer to promote breast cancer patients’ resilience, resulting in increased quality of life and hope (62–68). These successful programs could be adapted and utilized for pregnant women.
Fourth, ACEs was confirmed as a moderator among FOC, resilience and psychological distress. On the one hand, FOC had a stronger negative effect on resilience in pregnant women with ACEs compared to those without ACEs, indicating that ACEs contributed to reduced resilience, which was consistent with prior studies (69–71). On the other hand, when pregnant women have experienced childhood trauma, the protective effects of resilience are diminished, leading to them more prone to psychological distress. Our findings support the growing literature acknowledging the long-term and severe impact of ACEs on psychological distress (72, 73). So, it is crucial to incorporate ACEs screening into prenatal care.
In general, pregnant women with ACEs, high FOC and low resilience are more likely to experience severe psychological distress, which should be addressed through early identification and intervention.
The present study has some limitations. First, all the collected data is self-reported, so recall bias and social desirability bias may exist. Second, conclusions derived from this study are based on Chinese pregnant women and these findings should be replicated in other populations with different backgrounds. Third, the cross-sectional design limits the ability for causal inference among these four variables, and a longitudinal study should be conducted to replicate these findings. An ongoing 2 year follow-up assessment of this cohort (Be Resilient to Postpartum Depression, BRPD) will provide additional insights in the future. Fourth, several potential confounders, such as intimate partner violence, sleep quality and mindfulness level are not considered in the moderated mediation model due to heavy scale burden, which may result in biased estimations of associations.
Fear of childbirth (FOC) directly impacts psychological distress, and resilience significantly mediates the relationship between FOC and psychological distress. ACEs significantly moderates the association between FOC and psychological distress as well as the relationship between resilience and psychological distress. Reducing FOC while promoting resilience and early screening of ACEs may be useful targets for relieving psychological distress level among pregnant women in China.
The data that support the findings of this study are available on request from the corresponding authors. The data are not publicly available due to privacy or ethical restrictions.
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine (No. K-2022-024). The patients/participants provided their written informed consent to participate in this study.
XM: conceptualization, data curation, methodology, software, and writing – original draft. RM: software, validation, and methodology. YLL: investigation, software, and methodology. XW and QC: investigation and resources. YJL: resources and supervision. ZY: supervision and writing – review and editing. All authors contributed to the article and approved the submitted version.
This research was funded by grants from National Natural Science Foundation of China (Nos. 72274043 and 71904033), Young Elite Scientists Sponsorship Program by CACM (No. 2021-QNRC2-B08), Humanity and Social Science Foundation of Department of Education of Guangdong Province (No. 2020WTSCX009), Humanity and Social Science Foundation of Guangzhou (No. 2021GZGJ57), Guangdong Research Center for TCM Service and Industrial Development, Guangzhou University of Chinese Medicine (2022ZDA03), and Humanity and Social Science Foundation of Guangzhou University of Chinese Medicine (No. 2021SKYB07).
We thank nurse directors from participating universities for supporting data collection and all the participants for completing surveys.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Vehmeijer F, Guxens M, Duijts L, El Marroun H. Maternal psychological distress during pregnancy and childhood health outcomes: a narrative review. J Dev Origins Health Dis. (2019) 10:274–85. doi: 10.1017/S2040174418000557
2. Isgut M, Smith AK, Reimann ES, Kucuk O, Ryan J. The impact of psychological distress during pregnancy on the developing fetus: biological mechanisms and the potential benefits of mindfulness interventions. J Perinat Med. (2017) 45:999–1011. doi: 10.1515/jpm-2016-0189
3. Krawczak EM, Minuzzi L, Hidalgo MP, Frey BN. Do changes in subjective sleep and biological rhythms predict worsening in postpartum depressive symptoms? A prospective study across the perinatal period. Arch Womens Ment Health. (2016) 19:591–8. doi: 10.1007/s00737-016-0612-x
4. Ghaffar R, Iqbal Q, Khalid A, Saleem F, Hassali MA, Baloch NS, et al. Frequency and predictors of anxiety and depression among pregnant women attending tertiary healthcare institutes of Quetta City, Pakistan. BMC Womens Health. (2017) 17:51. doi: 10.1186/s12905-017-0411-1
5. Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res. (2021) 300:113912. doi: 10.1016/j.psychres.2021.113912
6. Sari O, Dağcıoğlu BF, Akpak YK, Yerebatmaz N, Ýleri A. Planned and unplanned pregnancy and its association with coping styles and life quality. Health Care Women Int. (2021) 1–11. doi: 10.1080/07399332.2021.1932895
7. Van de Loo K, Vlenterie R, Nikkels SJ, Merkus P, Roukema J, Verhaak CM, et al. Depression and anxiety during pregnancy: the influence of maternal characteristics. Birth. (2018) 45:478–89. doi: 10.1111/birt.12343
8. Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord. (2016) 191:62–77. doi: 10.1016/j.jad.2015.11.014
9. Çitak Bilgin N, Cos̨kun H, Cos̨kuner Potur D, Ýbar Aydın E, Uca E. Psychosocial predictors of the fear of childbirth in Turkish pregnant women. J Psychosom Obstet Gynaecol. (2021) 42:123–31. doi: 10.1080/0167482X.2020.1734791
10. Zhou WS, Zhu XD, Li SJ, Zheng BH, Yu YH, Xu HL, et al. Does the presence of anxiety and depression symptoms mediate the association between family functions and self-efficacy in pregnant women in the third trimester?: a community-based cross-sectional survey. Front Psychiatry. (2021) 12:726093. doi: 10.3389/fpsyt.2021.726093
11. Ma R, Yang F, Zhang L, Sznajder KK, Zou C, Jia Y, et al. Resilience mediates the effect of self-efficacy on symptoms of prenatal anxiety among pregnant women: a nationwide smartphone cross-sectional study in China. BMC Pregnancy Childbirth. (2021) 21:430. doi: 10.1186/s12884-021-03911-5
12. Zhang H, Zhao Q, Cao P, Ren G. Resilience and quality of life: exploring the mediator role of social support in patients with breast cancer. Med Sci Monit. (2017) 23:5969–79. doi: 10.12659/msm.907730
13. Kishore MT, Satyanarayana V, Ananthanpillai ST, Desai G, Bhaskarapillai B, Thippeswamy H, et al. Life events and depressive symptoms among pregnant women in India: moderating role of resilience and social support. Int J Soc Psychiatry. (2018) 64:570–7. doi: 10.1177/0020764018789193
14. Zhou X, Liu H, Li X, Zhang S. Fear of childbirth and associated risk factors in healthy pregnant women in northwest of China: a cross-sectional study. Psychol Res Behav Manag. (2021) 14:731–41. doi: 10.2147/PRBM.S309889
15. Corno G, Villani D, de Montigny F, Pierce T, Bouchard S, Molgora S. The role of perceived social support on pregnant women’s mental health during the COVID-19 pandemic. J Reprod Infant Psychol. (2022) 1–15. doi: 10.1080/02646838.2022.2042799
16. Nath S, Lewis LN, Bick D, Demilew J, Howard LM. Mental health problems and fear of childbirth: a cohort study of women in an inner-city maternity service. Birth. (2021) 48:230–41. doi: 10.1111/birt.12532
17. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/s0749-3797(98)00017-8
18. Davis JP, Tucker JS, Stein BD, D’Amico EJ. Longitudinal effects of adverse childhood experiences on substance use transition patterns during young adulthood. Child Abuse Negl. (2021) 120:105201. doi: 10.1016/j.chiabu.2021.105201
19. Deschênes SS, Kivimaki M, Schmitz N. Adverse childhood experiences and the risk of coronary heart disease in adulthood: examining potential psychological, biological, and behavioral mediators in the Whitehall II cohort study. J Am Heart Assoc. (2021) 10:e019013. doi: 10.1161/JAHA.120.019013
20. Iob E, Lacey R, Steptoe A. Adverse childhood experiences and depressive symptoms in later life: longitudinal mediation effects of inflammation. Brain Behav Immun. (2020) 90:97–107. doi: 10.1016/j.bbi.2020.07.045
21. Chang X, Jiang X, Mkandarwire T, Shen M. Associations between adverse childhood experiences and health outcomes in adults aged 18-59 years. PLoS One. (2019) 14:e0211850. doi: 10.1371/journal.pone.0211850
22. Young-Wolff KC, Alabaster A, McCaw B, Stoller N, Watson C, Sterling S, et al. Adverse childhood experiences and mental and behavioral health conditions during pregnancy: the role of resilience. J Womens Health. (2019) 28:452–61. doi: 10.1089/jwh.2018.7108
23. Racine N, Devereaux C, Cooke JE, Eirich R, Zhu J, Madigan S. Adverse childhood experiences and maternal anxiety and depression: a meta-analysis. BMC Psychiatry. (2021) 21:28. doi: 10.1186/s12888-020-03017-w
24. Abe Y, Sirichokchatchawan W, Sangkomkamhang U, Satthapisit S, Maes M. Adverse childhood experiences combined with emotional and physical abuse by the partner predict antenatal depression. J Affect Disord. (2022) 298(Pt A):194–201. doi: 10.1016/j.jad.2021.10.099
25. Masten AS, Barnes AJ. Resilience in children: developmental perspectives. Children. (2018) 5:98. doi: 10.3390/children5070098
26. Gagnon AJ, Stewart DE. Resilience in international migrant women following violence associated with pregnancy. Arch Womens Ment Health. (2014) 17:303–10. doi: 10.1007/s00737-013-0392-5
27. Chasson M, Taubman-Ben-Ari O, Abu-Sharkia S. Jewish and Arab pregnant women’s psychological distress during the COVID-19 pandemic: the contribution of personal resources. Ethn Health. (2021) 26:139–51. doi: 10.1080/13557858.2020.1815000
28. Lubián López DM, Butrón Hinojo CA, Arjona Bernal JE, Fasero Laiz M, Alcolea Santiago J, Guerra Vilches V, et al. Resilience and psychological distress in pregnant women during quarantine due to the COVID-19 outbreak in Spain: a multicentre cross-sectional online survey. J Psychosom Obstet Gynaecol. (2021) 42:115–22. doi: 10.1080/0167482X.2021.1896491
29. Zhang L, Yang X, Zhao J, Zhang W, Cui C, Yang F, et al. Prevalence of prenatal depression among pregnant women and the importance of resilience: a multi-site questionnaire-based survey in mainland China. Front Psychiatry. (2020) 11:374. doi: 10.3389/fpsyt.2020.00374
30. Huang J, Huang J, Li Y, Liao B. The prevalence and predictors of fear of childbirth among pregnant Chinese women: a hierarchical regression analysis. BMC Pregnancy Childbirth. (2021) 21:643. doi: 10.1186/s12884-021-04123-7
31. Wang YN, Yuan ZJ, Leng WC, Xia LY, Wang RX, Li ZZ, et al. Role of perceived family support in psychological distress for pregnant women during the COVID-19 pandemic. World J Psychiatry. (2021) 11:365–74. doi: 10.5498/wjp.v11.i7.365
32. Lowe NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. J Psychosom Obstet Gynaecol. (2000) 21:219–24. doi: 10.3109/01674820009085591
33. Liu S, Jin Y, Li H, Zeng T, Zhou G, Yu L, et al. Associations of musical activities and positive affect with fear of childbirth: a structural equation modeling approach. Front Public Health. (2022) 10:906996. doi: 10.3389/fpubh.2022.906996
34. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
35. Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the connor-davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. (2007) 20:1019–28. doi: 10.1002/jts.20271
36. Ye ZJ, Qiu HZ, Li PF, Chen P, Liang MZ, Liu ML, et al. Validation and application of the Chinese version of the 10-item Connor-Davidson resilience scale (CD-RISC-10) among parents of children with cancer diagnosis. Eur J Oncol Nurs. (2017) 27:36–44. doi: 10.1016/j.ejon.2017.01.004
37. Mei X, Wang H, Wang X, Wu X, Wu J, Ye Z. Associations among neuroticism, self-efficacy, resilience and psychological distress in freshman nursing students: a cross-sectional study in China. BMJ Open. (2022) 12:e059704. doi: 10.1136/bmjopen-2021-059704
38. Mei XX, Wang HY, Wu XN, Wu JY, Lu YZ, Ye ZJ. Self-efficacy and professional identity among freshmen nursing students: a latent profile and moderated mediation analysis. Front Psychol. (2022) 13:779986. doi: 10.3389/fpsyg.2022.779986
39. Mei XX, Wu XN, Wang HY, Wu JY, Wang XQ, Ye ZJ. Heterogeneity in psychological resilience and mental health among newly graduated nursing students: a latent profile and generalized additive model analysis. Psychol Res Behav Manag. (2022) 15:597–606. doi: 10.2147/PRBM.S348661
40. Chen HL, Wang HY, Lai SF, Ye ZJ. The associations between psychological distress and academic burnout: a mediation and moderation analysis. Psychol Res Behav Manag. (2022) 15:1271–82. doi: 10.2147/PRBM.S360363
41. Wu X, Lu Y, Zhang Q, Wang H, Sun X, Han H, et al. Stress/resource complex, sense of coherence and professional identity among nursing students: a latent profile and mediation analysis. Psychol Res Behav Manag. (2022) 15:2409–20. doi: 10.2147/PRBM.S378088
42. Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55:610–7. doi: 10.1080/00223891.1990.9674095
43. Gao LL, Sun K, Chan SW. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery. (2014) 30:532–8. doi: 10.1016/j.midw.2013.06.007
44. Li Y, Long Z, Cao D, Cao F. Social support and depression across the perinatal period: a longitudinal study. J Clin Nurs. (2017) 26:2776–83. doi: 10.1111/jocn.13817
45. Zhang JX, Schwarzer R. Measuring optimistic self-beliefs: a Chinese adaptation of the general self-efficacy scale. Psychologia. (1995) 38:174–81. doi: 10.1080/09515089508573160
46. Centers for Disease Control and Prevention. About the CDC-Kaiser ACE Study. Atlanta, GA: Center for Disease Control and Prevention (2022).
48. Fung HW, Ross CA, Yu CK, Lau EK. Adverse childhood experiences and dissociation among Hong Kong mental health service users. J Trauma Dissoc. (2019) 20:457–70. doi: 10.1080/15299732.2019.1597808
49. Huang C, Yang M, Geng Y, Chen Y, Cheung SP, Deng G, et al. Adverse childhood experiences and mindfulness in Chinese college students during the COVID-19 pandemic. Front Psychiatry. (2021) 12:619128. doi: 10.3389/fpsyt.2021.619128
50. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
51. Leung CM, Ho S, Kan CS, Hung CH, Chen CN. Evaluation of the Chinese version of the hospital anxiety and depression scale. a cross-cultural perspective. Int J Psychosom. (1993) 40:29–34.
52. Zhang J, Yang Z, Wang X, Li J, Dong L, Wang F, et al. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J Clin Nurs. (2020) 29:4020–9. doi: 10.1111/jocn.15425
53. Chen W, Li J, Peng S, Hong S, Xu H, Lin B, et al. Association of total thyroidectomy or thyroid lobectomy with the quality of life in patients with differentiated thyroid cancer with low to intermediate risk of recurrence. JAMA Surg. (2022) 157:200–9. doi: 10.1001/jamasurg.2021.6442
54. Azen R, Budescu DV. The dominance analysis approach for comparing predictors in multiple regression. Psychol Methods. (2003) 8:129–48. doi: 10.1037/1082-989x.8.2.129
55. Barranti M, Carlson EN, Côté S. How to test questions about similarity in personality and social psychology research: description and empirical demonstration of response surface analysis. Soc Psychol Pers Sci. (2017) 8:465–75. doi: 10.1177/1948550617698204
56. Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
57. R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing (2019).
58. Jha P, Larsson M, Christensson K, Svanberg AS. Fear of childbirth and depressive symptoms among postnatal women: a cross-sectional survey from Chhattisgarh, India. Women Birth. (2018) 31:e122–33. doi: 10.1016/j.wombi.2017.07.003
59. Koc AE, Colak S, Colak GV, Pusuroglu M, Hocaoglu C. Investigating fear of childbirth in pregnant women and its relationship between anxiety sensitivity and somatosensory amplification. J Obstet Gynaecol. (2021) 41:217–23. doi: 10.1080/01443615.2020.1732894
60. Saisto T, Halmesmäki E. Fear of childbirth: a neglected dilemma. Acta obstet Gynecol Scand. (2003) 82:201–8.
61. Witteveen AB, Henrichs J, Walker AL, Bohlmeijer ET, Burger H, Fontein-Kuipers Y, et al. Effectiveness of a guided ACT-based self-help resilience training for depressive symptoms during pregnancy: study protocol of a randomized controlled trial embedded in a prospective cohort. BMC Pregnancy Childbirth. (2020) 20:705. doi: 10.1186/s12884-020-03395-9
62. Liang, MZ, Tang Y, Knobf MT, Molassiotis A, Chen P, Hu GY, et al. Resilience index improves prediction of 1-year decreased quality of life in breast cancer. J Cancer Surv. (2022). doi: 10.1007/s11764-022-01239-3 [Epub ahead of print].
63. Ye ZJ, Zhang Z, Tang Y, Liang J, Sun Z, Hu GY, et al. Resilience patterns and transitions in the be resilient to breast cancer trial: an exploratory latent profile transition analysis. Psychooncology. (2021) 30:901–9. doi: 10.1002/pon.5668
64. Ye ZJ, Zhang Z, Zhang XY, Tang Y, Chen P, Liang MZ, et al. State or trait? Measuring resilience by generalisability theory in breast cancer. Eur J Oncol Nurs. (2020) 46:101727. doi: 10.1016/j.ejon.2020.101727
65. Ye ZJ, Zhang Z, Zhang XY, Tang Y, Liang J, Sun Z, et al. Effectiveness of adjuvant supportive-expressive group therapy for breast cancer. Breast Cancer Res Treat. (2020) 180:121–34. doi: 10.1007/s10549-020-05526-4
66. Ye ZJ, Peng CH, Zhang HW, Liang MZ, Zhao JJ, Sun Z, et al. A biopsychosocial model of resilience for breast cancer: a preliminary study in mainland China. Eur J Oncol Nurs. (2018) 36:95–102. doi: 10.1016/j.ejon.2018.08.001
67. Ye ZJ, Qiu HZ, Liang MZ, Liu ML, Li PF, Chen P, et al. Effect of a mentor-based, supportive-expressive program, be resilient to breast cancer, on survival in metastatic breast cancer: a randomised, controlled intervention trial. Br J Cancer. (2017) 117:1486–94. doi: 10.1038/bjc.2017.325
68. Ye ZJ, Liang MZ, Qiu HZ, Liu ML, Hu GY, Zhu YF, et al. Effect of a multidiscipline mentor-based program, be resilient to breast cancer (BRBC), on female breast cancer survivors in mainland China-a randomized, controlled, theoretically-derived intervention trial. Breast Cancer Res Treat. (2016) 158:509–22. doi: 10.1007/s10549-016-3881-1
69. Chen Y, Hua K, Huang C, Zhou G, Wang J. Adverse childhood experiences and psychological well-being in Chinese college students: moderated mediation by gender and resilience. Front Psychiatry. (2021) 12:710635. doi: 10.3389/fpsyt.2021.710635
70. Morgan CA, Chang YH, Choy O, Tsai MC, Hsieh S. Adverse childhood experiences are associated with reduced psychological resilience in youth: a systematic review and meta-analysis. Children. (2021) 9:27. doi: 10.3390/children9010027
71. Wang Z, Lohrmann DK, Buu A, Lin HC. Resilience as a mediator between adverse childhood experiences and prescription opioid misuse among U.S. adults. Subst Use Misuse. (2021) 56:484–92. doi: 10.1080/10826084.2021.1879148
72. Clements-Nolle K, Waddington R. Adverse childhood experiences and psychological distress in juvenile offenders: the protective influence of resilience and youth assets. J Adolesc Health. (2019) 64:49–55. doi: 10.1016/j.jadohealth.2018.09.025
Keywords: fear of childbirth, resilience, psychological distress, dominance analysis, response surface analysis, moderated mediation analysis, pregnant women
Citation: Mei XX, Mei RR, Liu YL, Wang XQ, Chen QW, Lei YJ and Ye ZJ (2022) Associations among fear of childbirth, resilience and psychological distress in pregnant women: A response surface analysis and moderated mediation model. Front. Psychiatry 13:1091042. doi: 10.3389/fpsyt.2022.1091042
Received: 06 November 2022; Accepted: 28 November 2022;
Published: 15 December 2022.
Edited by:
Bochao Cheng, Sichuan University, ChinaReviewed by:
Zhenwei Dai, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaCopyright © 2022 Mei, Mei, Liu, Wang, Chen, Lei and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youjin Lei, bGVpeW91amluMTczM0AxNjMuY29t; Zengjie Ye, emVuZ2ppZXllQHFxLmNvbQ==
†These authors have contributed equally to this work
‡ORCID: Xiaoxiao Mei, orcid.org/0000-0003-2721-5784
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.