- 1Departments of Psychiatry, Chonnam National University Medical School, Gwangju, South Korea
- 2Departments of Radiology, Chonnam National University Medical School, Gwangju, South Korea
Objectives: This report aims to introduce a rare case of a dramatic recovery by donepezil with a patient with schizophrenia who suffered from remaining psychotic symptoms despite proper treatment and had a cognitive impairment by carbon monoxide (CO) poisoning sequelae.
Case report: A 38-year-old male who developed schizophrenia 2 years ago had attempted suicide via CO inhalation due to his uncontrolled symptoms. He was hospitalized with delayed neurological sequelae (DNS). Though hyperbaric oxygen therapy (HBOT) was applied 10 times, his cognitive impairment did not recover. Surprisingly, with 5–10 mg donepezil, both cognitive function and the psychotic symptoms of the patient remarkably improved.
Conclusion: This case showed a good response of donepezil for a patient with schizophrenia and CO-induced DNS after ineffective HBOT. Although the mechanism of the phenomenon is unclear, it can be possible reasons that the neuroprotective effect of donepezil and white matter insult by CO poisoning.
Introduction
The lifetime risk of suicide rate among patients with schizophrenia is approximately 14.1% in the global population, and 26.8% of individuals with schizophrenia attempt suicide (1, 2), and the psychotic symptoms, as well as paranoid delusions and commanding hallucinations, are associated with a high risk of suicide (3).
Carbon monoxide (CO) poisoning by burning charcoal is one of the most popular methods of suicide (4). The symptoms of CO poisoning range from slight headache and anxiety to the most severe manifestations such as urinary/stool incontinence, inability to walk, and cognitive impairment (5). Delayed neurological sequelae (DNS) can be developed according to the duration of CO exposure. It can be defined as severe neuropsychiatric symptoms developed after 2–40 days of lucidity in patients with CO poisoning (6–8). Although hyperbaric oxygen therapy (HBOT) is commonly applied to patients with DNS there are no randomized trials showing improvement of neuropsychological symptoms by HBOT in patients with CO poisoning (9, 10).
Few available treatments are for DNS, despite proposed treatments including steroids, aspirin, cerebral vasodilators, bromocriptine, L-dopa, barbiturates, and dextroamphetamine (9, 11–15). Several case reports recently found that acetylcholinesterase inhibitors (AchEIs) were effective in cognitive impairment (16, 17). Interestingly, we experienced an episode of a patient with schizophrenia and CO-induced DNS who responded well to donepezil after unsuccessful HBOT. This case gives an example as the first report for a patient with schizophrenia using donepezil for DNS.
Case report
A 38-year-old male diagnosed with schizophrenia is currently in partial remission. He had visited the hospital for 2 years to treat psychotic symptoms including auditory hallucinations and persecutory delusions. These symptoms had developed a week before his first visit to the hospital. He had no family history related to psychiatric or other medical conditions. He worked in a large company after graduating from college. On being diagnosed with schizophrenia, he took medicines: amisulpride 800 mg, procyclidine 5 mg, propranolol 80 mg, and diazepam 2 mg. His psychotic symptoms were improved after medication, while auditory hallucinations remained unchanged. He reported that he found it hard to work because the voices reproached him. After consulting a doctor, he stopped the work for a moment due to aggravated symptoms. Although the doctor recommended him admission for controlling residual hallucinations, he insisted on keeping outpatient clinic treatment.
With uncontrolled residual psychotic symptoms, he attempted suicide by inhaling charcoal fumes. He was taken to an emergency room at a hospital and underwent symptomatic care, not HBOT, for CO poisoning and rhabdomyolysis. A month later, severe cognitive dysfunction occurred to him. It was composed of memory decline, gait disturbance, and ataxia at the time of admission. He showed marked deterioration of visuospatial function; he stated that he lost all sense of direction. In a clock-drawing test performed on the day of evaluation, he could not tell the hour hand from the minute hand and could not draw the hour hand (as dictated by a doctor; Figure 1).
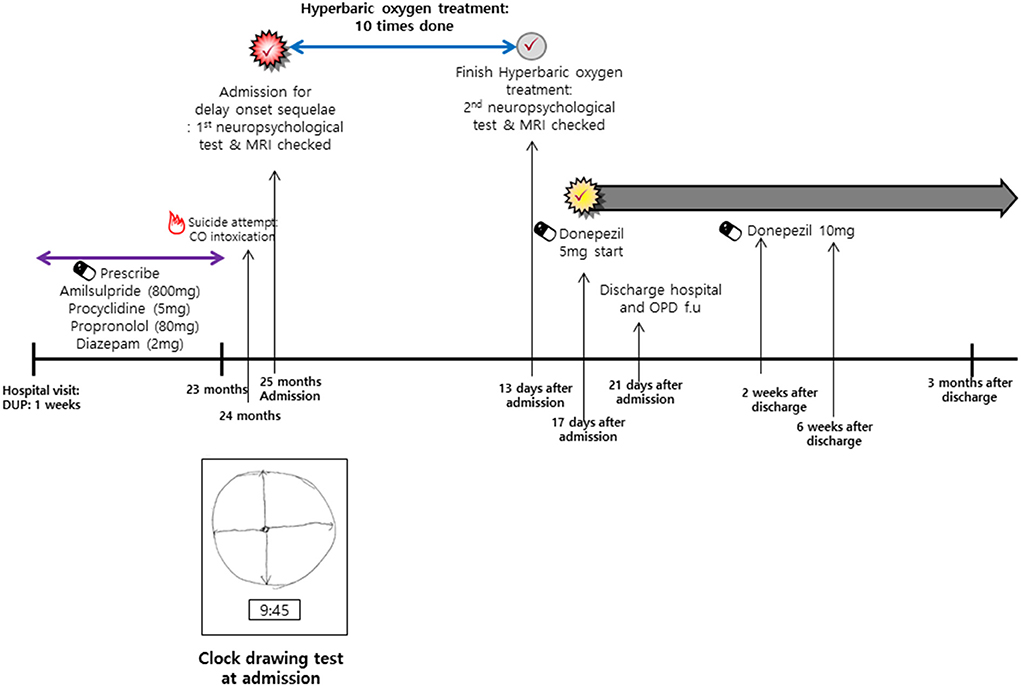
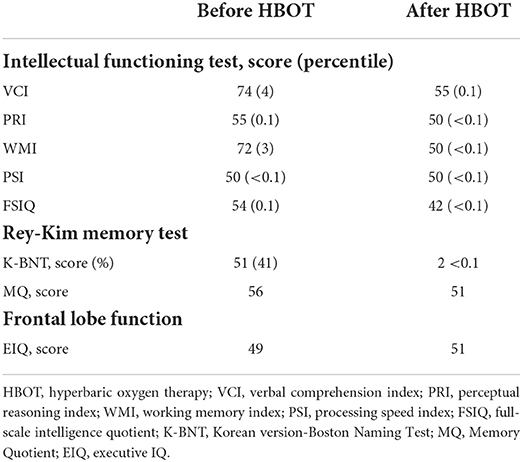
Figure 1. Timeline of clinical course before and after CO intoxication. PANSS, Positive and Negative Syndrome Scale; MINI, Mini-International Neuropsychiatric Interview; CGI-S, Clinical Global Impressions- Severity; CGI-I, Clinical Global Impressions-Improve.
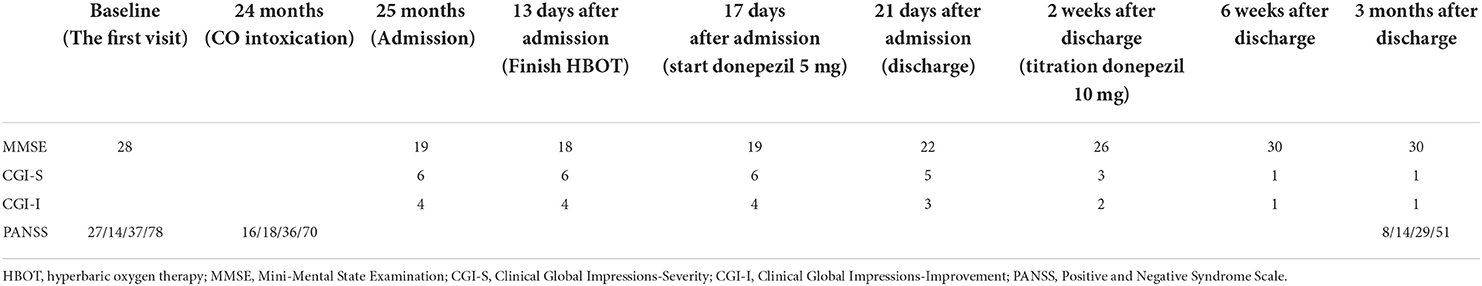
Due to his deteriorated state, physicians decided to apply HBOT and taper psychotropic medications. Brain magnetic resonance imaging (MRI) and a neuropsychological test were executed to confirm his structural and functional brain conditions before therapy. The tests were repeated after 10 times HBOT. The treatment schedule is shown in Figure 1. Pre-and-post-HBOT data are shown in Table 1. In short, HBOT did not change his brain structure and function (Figure 2 and Table 1).
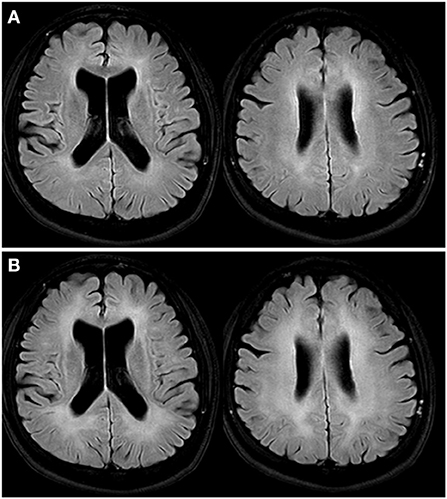
Figure 2. Brain MRI T2 fluid-attenuated inversion recovery image. (A) Initially, it shows bilateral symmetric confluent high signal intensities in periventricular white matters of cerebral hemispheres, which are compatible with delayed CO encephalopathy. (B) After HBOT shows increases in the extent of confluent high signal intensities in bilateral cerebral periventricular and subcortical white matter. MRI, magnetic resonance imaging; CO, carbon monoxide; HBOT, hyperbaric oxygen therapy.
We used the scale Positive and Negative Syndrome Scale (PANSS), Clinical Global Impressions-Severity (CGI-S), Clinical Global Impressions-Improvement (CGI-I), and Mini-Mental State Examination (MMSE) to assess the psychotic symptoms and cognitive dysfunction (18–21). Despite continuous treatment, the overall patient's cognitive function and psychiatric status had been unchanged without worsening during the 10 times HBOT sessions. Changes in symptoms through pre-and-post therapy are shown in Table 2. He was somewhat inconsistent and ambiguous when discussing his underlying psychotic symptoms. For getting more information on him, we had a retrospective interview with a caregiver. Regardless of HBOT, mild to moderate psychotic symptoms and very severe depression were found consistently.
We prescribed donepezil 5 mg once daily to him; after 4 days, the MMSE score improved from 19 to 22. He explained that his subjective cognitive decline had improved by ~70% at the time of discharge. He had no difficulty in activities of daily living and gradually improved with gait. Despite the short-term treatment donepezil seemed to be effective. The dose was increased to 10 mg daily to improve cognition further. He could deal with household matters without any other's help. His MMSE score was 30; additionally, he stated that psychotic symptoms had disappeared as increasing the dose of donepezil. Three months after discharge, remaining on donepezil, he is mentally stable and has returned to work. Supplementary Figure 1 shows a change in scores on the Clinician-Rated Dimensions of Psychosis Symptom Severity (Dimensional) scale in the DSM-5 (22), both the psychotic and cognitive symptoms.
Discussion
We report a case of a patient with schizophrenia in which DNS and functional impairment following CO poisoning improved greatly after a prescription of donepezil hydrochloride, an AchEI. Before donepezil treatment, he had undergone HBOT for 10 sessions which did not improve DNS. His cognitive function increased dramatically on donepezil, such that he has been able to return to work.
Our study has two major clinical implications. First, donepezil may be useful for treating DNS caused by CO poisoning (whereas HBOT was ineffective). The underlying cause of DNS after CO poisoning remains unclear but may be due to diffuse demyelination of the cerebral white matter (23–25). Hippocampal nicotinic acetylcholinergic neurons were dysfunctional in an animal model of DNS induced by CO poisoning (26). Donepezil exerts anti-inflammatory and neuroprotective effects (27–29). However, the effects of donepezil on DNS are not known; randomized controlled trials are needed. Second, before attempting suicide, the patient reported severe auditory hallucinations despite adequate medication. When we interviewed the patient after he had been started on donepezil, his cognitive function was observed to have improved markedly, and all psychiatric symptoms including the auditory hallucinations had disappeared. Earlier case reports found that psychiatric symptoms before CO poisoning, as well as DNS symptoms, persisted in some patients but disappeared in others after starting on donepezil (16, 17, 30). Underlying psychiatric symptoms improved only in patients with mood disorders; they persisted in those with other psychotic symptoms, although cognitive function improved in all patients. Meanwhile, there was one case of schizophrenia with the delusion that responded to donepezil augmented with antipsychotics (31). However, the only use of donepezil to improve psychotic symptoms has been hard to find any reports. Our findings differ; the DNS and psychotic symptoms disappeared completely after we prescribed donepezil without antipsychotics. The disappearance of psychotic symptoms that did not completely respond to earlier (pre-DNS) medications may be explained as follows. First, increasing evidence suggests that the cerebral white matter is involved in the pathophysiology of schizophrenia (32, 33). In this case, white matter abnormalities caused by DNS may have improved the psychiatric symptoms. Second, the neuroprotective effect of donepezil might improve psychiatric symptoms. Third, the suicide attempt per se may have exerted a psychological effect, possibly improving the psychotic symptoms. However, further study is warranted. In particular, any future recurrence of psychotic symptoms will be clinically relevant.
Despite the demonstration of a clear effect of donepezil in a patient with schizophrenia and CO-induced DNS this paper has limitations. First, we could not conclude what mechanism is underlying this phenomenon. Second, we could not find similar cases elsewhere. Third, In this case, when the patient came to the emergency room of our hospital, it had been a month since CO intoxication occurred, and acute blood samples, including a percentage of carboxyhemoglobin, could not be obtained. However, delayed encephalopathy of CO intoxication had been confirmed from the brain MRI readings performed at our hospital. Accordingly, it could diagnose through the correlation between the medical history and diagnosis at the time of inhalation and the patient's clinical symptoms and images.
We described a patient with schizophrenia and CO-induced DNS who responded well to donepezil after ineffective HBOT. Further studies are warranted to confirm the long-term efficacy of donepezil for improving cognitive function and psychotic symptoms in patients with schizophrenia, particularly after CO intoxication.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Had full access to all of the data in the study and take responsibility for the data: S-HB, J-WK, and J-MK. Study concept and design: J-WK and S-WK. Drafting of the manuscript: J-WK and J-MK. Critical revision of the manuscript for important intellectual content: J-WK, YYL, J-YK, S-WK, and J-MK. Administrative, technical, or material support: YYL and J-YK. Study supervision: S-WK and J-MK. All authors contributed to the article and approved the submitted version.
Funding
The study was funded by a grant of National Research Foundation of Korea Grant [NRF-2020M3E5D9080733] and [NRF-2020R1A2C2003472].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1071417/full#supplementary-material
Supplementary Figure S1. Changes in scores on the Clinician-Rated Dimensions of Psychosis Symptom Severity (Dimensional) scale in the DSM-5.
References
1. Lu L, Dong M, Zhang L, Zhu XM, Ungvari GS, Ng CH, et al. Prevalence of suicide attempts in individuals with schizophrenia: a meta-analysis of observational studies. Epidemiol Psychiatr Sci. (2020) 29:e39. doi: 10.1017/S2045796019000313
2. Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health. (2018) 15:1425. doi: 10.3390/ijerph15071425
3. Grover LE, Jones R, Bass NJ, McQuillin A. The differential associations of positive and negative symptoms with suicidality. Schizophr Res. (2022) 248:42–9. doi: 10.1016/j.schres.2022.07.016
4. Huang CC, Ho CH, Chen YC, Hsu CC, Wang YF, Lin HJ, et al. Impact of hyperbaric oxygen therapy on subsequent neurological sequelae following carbon monoxide poisoning. J Clin Med. (2018) 7:349–61. doi: 10.3390/jcm7100349
5. Pepe G, Castelli M, Nazerian P, Vanni S, Panta MD, Gambassi F, et al. Delayed neuropsychological sequelae after carbon monoxide poisoning: predictive risk factors in the Emergency Department. A retrospective study. Scand J Trauma Resusc Emerg Med. (2011) 19:16–23. doi: 10.1186/1757-7241-19-16
6. Rose JJ, Wang L, Xu Q, McTiernan CF, Shiva S, Tejero J, et al. Carbon monoxide poisoning: pathogenesis, management, and future directions of therapy. Am J Respir Crit Care Med. (2017) 195:596–606. doi: 10.1164/rccm.201606-1275CI
7. Hsiao CL, Kuo HC, Huang CC. Delayed encephalopathy after carbon monoxide intoxication–long-term prognosis and correlation of clinical manifestations and neuroimages. Acta Neurol Taiwan. (2004) 13:64–70.
8. Oh S, Choi SC. Acute carbon monoxide poisoning and delayed neurological sequelae: a potential neuroprotection bundle therapy. Neural Regen Res. (2015) 10:36–8. doi: 10.4103/1673-5374.150644
9. Lee HF, Mak SC, Chi CS, Hung DZ. Hyperbaric oxygen for carbon monoxide poisoning-induced delayed neuropsychiatric sequelae. Zhonghua Yi Xue Za Zhi. (2001) 64:310–4.
10. Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. (2011) 2011:CD002041. doi: 10.1002/14651858.CD002041.pub3
11. Min SK. A brain syndrome associated with delayed neuropsychiatric sequelae following acute carbon monoxide intoxication. Acta Psychiatr Scand. (1986) 73:80–6. doi: 10.1111/j.1600-0447.1986.tb02671.x
12. Starkstein SE, Berthier ML, Leiguarda R. Psychic akinesia following bilateral pallidal lesions. Int J Psychiatry Med. (1989) 19:155–64. doi: 10.2190/AE1Q-QY7B-LU2F-GJHF
13. Jaeckle RS, Nasrallah HA. Major depression and carbon monoxide-induced Parkinsonism: diagnosis, computerized axial tomography, and response to L-dopa. J Nerv Ment Dis. (1985) 173:503–8. doi: 10.1097/00005053-198508000-00009
14. Norris Jr CR, Trench JM, Hook R. Delayed carbon monoxide encephalopathy: clinical and research implications. J Clin Psychiatry. (1982) 43:294–5.
15. Smallwood P, Murray GB. Neuropsychiatric aspects of carbon monoxide poisoning: a review and single case report suggesting a role for amphetamines. Ann Clin Psychiatry. (1999) 11:21–7. doi: 10.3109/10401239909147044
16. Wang P, Zeng T, Chi ZF. Recovery of cognitive dysfunction in a case of delayed encephalopathy of carbon monoxide poisoning after treatment with donepezil hydrochloride. Neurol India. (2009) 57:481–2. doi: 10.4103/0028-3886.55596
17. Yanagiha K, Ishii K, Tamaoka A. Acetylcholinesterase inhibitor treatment alleviated cognitive impairment caused by delayed encephalopathy due to carbon monoxide poisoning: two case reports and a review of the literature. Medicine. (2017) 96:e6125. doi: 10.1097/MD.0000000000006125
18. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
19. Pinna F, Deriu L, Diana E, Perra V, Randaccio RP, Sanna L, et al. Clinical Global Impression-severity score as a reliable measure for routine evaluation of remission in schizophrenia and schizoaffective disorders. Ann Gen Psychiatry. (2015) 14:6–13. doi: 10.1186/s12991-015-0042-6
20. Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry. (2007) 4:28–37.
21. Kang YW, Na DL, Hahn SH. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. (1997) 15:300–8.
22. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing (2013). doi: 10.1176/appi.books.9780890425596
23. Lapresle J, Fardeau M. The central nervous system and carbon monoxide poisoning. II Anatomical study of brain lesions following intoxication with carbon monoxide (22 cases). Prog Brain Res. (1967) 24:31–74. doi: 10.1016/S0079-6123(08)60181-8
24. Ginsberg MD, Myers RE, McDonagh BF. Experimental carbon monoxide encephalopathy in the primate. II Clinical aspects, neuropathology, and physiologic correlation. Arch Neurol. (1974) 30:209–16. doi: 10.1001/archneur.1974.00490330017003
25. Kim JH, Chang KH, Song IC, Kim KH, Kwon BJ, Kim HC, et al. Delayed encephalopathy of acute carbon monoxide intoxication: diffusivity of cerebral white matter lesions. AJNR Am J Neuroradiol. (2003) 24:1592–7.
26. Ochi S, Abe M, Li C, Mori Y, Ishimaru T, Yoshino Y, et al. The nicotinic cholinergic system is affected in rats with delayed carbon monoxide encephalopathy. Neurosci Lett. (2014) 569:33–7. doi: 10.1016/j.neulet.2014.03.054
27. Akasofu S, Kimura M, Kosasa T, Sawada K, Ogura H. Study of neuroprotection of donepezil, a therapy for Alzheimer's disease. Chem Biol Interact. (2008) 175:222–6. doi: 10.1016/j.cbi.2008.04.045
28. Field RH, Gossen A, Cunningham C. Prior pathology in the basal forebrain cholinergic system predisposes to inflammation-induced working memory deficits: reconciling inflammatory and cholinergic hypotheses of delirium. J Neurosci. (2012) 32:6288–94. doi: 10.1523/JNEUROSCI.4673-11.2012
29. Hwang J, Hwang H, Lee HW, Suk K. Microglia signaling as a target of donepezil. Neuropharmacology. (2010) 58:1122–9. doi: 10.1016/j.neuropharm.2010.02.003
30. Tseng WT, Yeh JY, Lane HY, Lin CH. Effects of donepezil on cognition and global functioning in patients with delayed encephalopathy after carbon monoxide poisoning: a case series. Psychiatry Clin Neurosci. (2019) 73:348. doi: 10.1111/pcn.12841
31. Halder A, Panchami N, Harshe G. A case of schizophrenia with Capgras delusion responded to donepezil. Indian J Psychiatry. (2022) 64:219–20. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_972_21
32. Levitt JJ, Alvarado JL, Nestor PG, Rosow L, Pelavin PE, McCarley RW, et al. Fractional anisotropy and radial diffusivity: diffusion measures of white matter abnormalities in the anterior limb of the internal capsule in schizophrenia. Schizophr Res. (2012) 136:55–62. doi: 10.1016/j.schres.2011.09.009
Keywords: suicide, carbon monoxide, delayed neurological sequelae, donepezil, schizophrenia
Citation: Baek S-H, Kim J-W, Lee YY, Kim J-Y, Kim S-W and Kim J-M (2022) Case report: Recovery of hallucinations and cognitive impairment after administration of donepezil in a patient with schizophrenia and carbon monoxide poisoning. Front. Psychiatry 13:1071417. doi: 10.3389/fpsyt.2022.1071417
Received: 16 October 2022; Accepted: 07 November 2022;
Published: 18 November 2022.
Edited by:
Massimo Tusconi, University of Cagliari, ItalyReviewed by:
Steinn Steingrimsson, Sahlgrenska University Hospital, SwedenMaryam Akhgari, Iranian Legal Medicine Organization, Iran
Copyright © 2022 Baek, Kim, Lee, Kim, Kim and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sung-Wan Kim, c3draW1AY2hvbm5hbS5hYy5rcg==; Jae-Min Kim, am1raW1AY2hvbm5hbS5hYy5rcg==
†These authors have contributed equally to this work
 Seon-Hwa Baek
Seon-Hwa Baek Ju-Wan Kim1†
Ju-Wan Kim1† Sung-Wan Kim
Sung-Wan Kim Jae-Min Kim
Jae-Min Kim