- School of Psychology, HSE University, Moscow, Russia
Background: There is extensive available research on the relationship between fear of COVID-19 pandemic and physical symptoms. This study was the first to examine the cyberchondria and COVID-19 preventive behavior as mediators of this relationship.
Methods: A cross-sectional study was conducted from October to December 2021, during the fourth wave of the COVID-19 pandemic in Russia. The participants were 2,011 Russian-speaking volunteers aged 18 years and older. They completed questionnaires on somatic burden, cyberchondria, COVID-19 preventive behavior, and fear of COVID-19 pandemic. Mediation analysis was used to explore the mediating roles of cyberchondria and preventive behavior in the relationship between fear of COVID-19 and somatic burden.
Results: Fear of COVID-19 positively predicted somatic burden, cyberchondria, and COVID-19 preventive behavior. Mediation analysis showed that the relationship between fear of COVID-19 pandemic and somatic burden was mediated by cyberchondria (effect = 0.08, bootstrapping SE = 0.01, bootstrapping 95% CI [0.08, 0.12]), but not COVID-19 preventive behavior (effect = 0.02, bootstrapping SE = 0.01, bootstrapping 95% CI [0.00, 0.05]).
Conclusion: The findings suggest that cyberchondria had negative effects on somatic burden during the COVID-19 pandemic. The knowledge of the mediating role of cyberchondria may be used by health care workers when consulting persons with physical health complaints and psychosomatic disorders.
Introduction
The COVID-19 pandemic has challenged the mental and physical health of the population in all countries. Many people have experienced a relapse of chronic and psychiatric diseases (1), residual physical and cognitive effects (2), emotional exhaustion (3), psychological distress (4), posttraumatic stress disorder (5), psychosomatic burden (6), stigmatization, discrimination (7), isolation, loneliness, and concerns about their health and future (8).
One of the most common effects of pandemic is fear of COVID-19, found in 18–45% of persons in the general population (9, 10). Numerous studies showed that fear of COVID-19 is triggered by feeling of isolation from others and those close friends and family members who are infected with the SARS-CoV-2 (11), weak basic beliefs in goodness and justice of the world around (12), chronic illnesses, perception of bad government response to a pandemic (13), media exposure, intolerance of uncertainty, health anxiety, perceived risk for loved ones, economic consequences, and health care systems overload (14). Females, younger adults, urban residents, divorcees, healthcare workers, quarantined persons, persons suspected of being infected, and persons with mental disorders were at increased risk for fear of COVID-19 (15).
Fear of COVID-19, cyberchondria, and preventive behavior
Not surprisingly, fear of COVID-19 can greatly alter human behavior, especially as it relates to health and safety. Pre-pandemic research showed that more than 50% of Internet users receive medical information through online news, newspapers, and magazines (16). These trends worsened during the COVID-19 pandemic, triggering an increase in health anxiety and a search for information about a mysterious and frightening infection (17). Persons with a high fear of pandemic often search the Internet for information about COVID-19 disease, so fear of COVID-19 was closely associated with cyberchondria (18–20).
Because fear of COVID-19 can change health-related behavior, it can also influence adherence to preventive measures. Since the World Health Organization declared the COVID-19 pandemic, governments of various countries have developed preventive behaviors including hand hygiene, wearing facemasks, social distancing, working from home, and avoiding any non-essential local and international travel (21). Persons with chronic diseases (22), greater COVID-19 threat appraisal (23), sufficient knowledge about the pandemic (24), greater government trust (25), greater health literacy and access to COVID-19 information sources (26), greater positive perception of social media, e-government services and information (27) observed preventive behavior more frequently and intensively.
Fear of COVID-19 has activated preventive behavior (28–30). This trend is highlighted among vulnerable persons, such as pregnant females (31), older persons (32), and persons with mental disorders (33). With long-term observation of the relationship between fear of COVID-19 and preventive behavior, it is clear that this tendency may be significant during a severe, but not mild COVID-19 outbreak period (34).
Effects of COVID-19 fear on somatic burden
In a broad sense, somatic burden occurs as a physiological reaction to strong emotional impressions. A person in a state of fear may have elevated blood pressure, pulse, and respiration, which decrease when the fear passes, but remain when a person experiences permanent or persistent fear and can not express it in emotion or behavior (35). Fear of COVID-19 refers to these permanent or persistent emotional disturbances due to the duration of dangerous and life-threatening circumstances, Therefore, persons who expressed greater fear of COVID-19 had more severe and frequent somatic symptoms (36–38).
The present study
Obviously, the relationship between fear of COVID-19 and somatic burden can be mediated by various phenomena, but so far only the buffering effect of perceived social support has been studied (38). Considering the relationship between fear of COVID-19 and somatic burden, as well as the relationship between fear of COVID-19, cyberchondria, and preventive behavior, it has been suggested that cyberchondria and preventive behavior may mediate the relationship between fear of COVID-19 and somatic burden.
Based on previous empirical highlights (22, 37–39), it has been hypothesized that fear of COVID-19, cyberchondria, and preventive behavior would be positively associated with somatic burden (H1). Also, it seemed obvious to suggest that both cyberchondria and preventive behavior positively mediate the relationship between fear of COVID-19 and somatic burden (H2). This hypothesis was based on the relationship between cyberchondria and somatic burden found before the pandemic (40), and the fact that frequent primary health care attendance is typical for persons with somatic symptom disorder (41). The proposed multiple mediation model is presented in Figure 1.
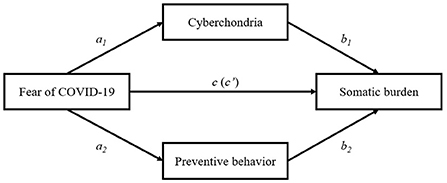
Figure 1. Proposed multiple mediation model; Direct and indirect effects of COVID-19 fear on somatic burden. c – total effect; c' – direct effect.
Materials and methods
Sample and procedure
The data were collected in December 2021. The participants were recruited from a community sample with the support of the Russian survey company Anketolog. This company sent out letters to its subscribers inviting them to take part in the study. The only criterion was 18 years of age or older. Volunteers who responded to the invitation gave written informed consent, filled out a questionnaire, and received a financial reward for participating in the study. A sample consisted of 2,011 volunteers (1,335 females and 676 males) aged 18–80 years old (M = 40.91, Mdn = 40, SD = 10.57).
Evaluation instruments
Somatic burden was evaluated with the Somatic Symptoms Scale-8 (SSS-8). The SSS-8 is an 8-item scale developed (42) and adapted into Russian (43) to measure somatic burden through eight somatic complaints. Symptoms are scored on a five-point response option from 0 (“not bothered at all”) to 4 (“bothered very much”). Cronbach's alpha was 0.83 in the current study.
Fear of COVID-19 was evaluated with the Fear of COVID-19 Scale (FCV-19S). The FCV-19S is a 7-item scale developed (44) and adapted into Russian (45) to measure psychological and physiological responses to fear associated with SARS-CoV-2 and COVID-19 pandemic. Responses range from 1 (“strongly disagree”) to 5 (“strongly agree”). Cronbach's alpha was 0.83 in the current study.
Cyberchondria was evaluated with the Cyberchondria Severity Scale-12 (CSS-12). The CSS-12 is a 12-item scale developed (46) and adapted (47) to measure excessive, compulsive, and distressing searches for health information on the Internet. Each statement is rated from 1 (“never”) to 5 (“always”). Cronbach's alpha was 0.95 in the current study.
Preventive behavior was evaluated with the COVID-19 Preventive Behavior Index (CPBI). The CPBI is a 10-item scale developed (21) to measure preventive behaviors aimed at reducing exposure to SARS-CoV-2 and COVID-19 pandemic. Responses range from 1 (“strongly disagree”) to 5 (“strongly agree”). In the current study, the CPBI was translated into Russian with a standardized procedure (48). The translated Russian version of the CPBI showed acceptable reliability (Cronbach's alpha was 0.86) and factor validity (χ2 = 492.655, df = 33, p < 0.001, TLI = 0.918, CFI = 0.940, RMSEA = 0.083 [0.077–0.090]).
Analytic strategy
All data analyses were performed using jamovi 1.6.15 and IBM SPSS Statistics 27.0. Descriptive statistics were tested using means and standard deviations. Bivariate relations between measured variables were assessed with Pearson correlations. A p-value of 0.05 or lower was considered statistically significant. Mediation model was conducted using Hayes' Process with Model 4. It examined cyberchondria and preventive behavior as mediators in the relationship between fear of COVID-19 and somatic burden. Statistical significance of the indirect effects were established using the bootstrapping method based on 10,000 resamples. The indirect effect was considered significant if the confidence intervals were entirely above or below zero (49).
Results
Preliminary analysis
Table 1 presents descriptive statistics and Pearson's correlation coefficients for all measured variables. Somatic burden was positively related to fear of COVID-19, cyberchondria, and preventive behavior. Fear of COVID-19 was positively correlated with cyberchondria and preventive behavior. Finally, cyberchondria was positively associated with preventive behavior during the COVID-19 pandemic.
Mediation analysis
A multiple mediation analysis was used to examine whether cyberchondria and preventive behavior mediate the relationship between fear of COVID-19 and somatic burden (Figure 2). There was a significant positive effect of COVID-19 fear on cyberchondria (a1: β = 0.33, SE = 0.04, p < 0.001), and on preventive behavior (a2: β = 0.46, SE = 0.03, p < 0.001). Cyberchondria (b1: β = 0.25, SE = 0.01, p < 0.001) was positively related to somatic burden, whereas preventive behavior (b2: β = 0.04, SE = 0.01, p = 0.115) had non-significant effect on somatic burden. The total effect of COVID-19 fear on somatic burden was significant (c: β = 0.27, SE = 0.03, p < 0.001), and after entering cyberchondria and preventive behavior into the model, the direct effect of COVID-19 fear on somatic burden remained significant (c': β = 0.17, SE = 0.03, p < 0.001). Using the bootstrapping procedure (10,000 resamples), the analysis showed that indirect effect of COVID-19 fear on somatic burden through cyberchondria was significant (effect = 0.08, bootstrapping SE = 0.01, bootstrapping 95% CI [0.08, 0.12]), whereas indirect effect of COVID-19 fear on somatic burden through preventive behavior was non-significant (effect = 0.02, bootstrapping SE = 0.01, bootstrapping 95% CI [0.00, 0.05]).
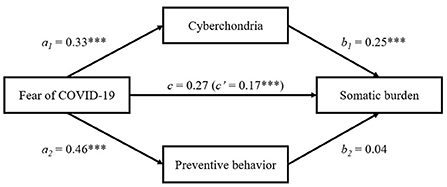
Figure 2. Mediation effects of cyberchondria and preventive behavior in the relationship between COVID-19 fear and somatic burden. All coefficients are standardized. c – total effect; c' – direct effect; ***p < 0.001.
Discussion
This study was aimed to examine two research hypotheses: (H1) the relationship between fear of COVID-19, cyberchondria, and preventive behavior would be positively associated with somatic burden; (H2) cyberchondria and preventive behavior positively mediate the relationship between fear of COVID-19 and somatic burden. Firstly, the results of correlation analysis showed that somatic burden was positively correlated with fear of COVID-19, cyberchondria, and preventive behavior. This fully confirmed H1. Secondly, the results of mediation analysis indicated that the relationship between fear of COVID-19 and somatic burden was mediated by cyberchondria, but not preventive behavior. This partially supported H2.
These findings are consistent with previous highlights that somatic burden is associated with cyberchondria (40) and fear of COVID-19 (38). Cyberchondria was a positive mediator in the relationship between fear of COVID-19 and somatic burden, that is, when it grows, fear of COVID-19 leads to increased somatization. During the COVID-19 pandemic, cyberchondria was linked to many negative conditions including health anxiety, anxiety about a pandemic, depressive symptoms, obsessive-compulsive symptoms, and problematic usage of the Internet (50). Since somatic symptoms in general practice are more prevalent than anxiety and depressive symptoms (51), the current findings emphasize the fragility of psychosomatic well-being and its dependence on fear of COVID-19 mediated by the destructive power of cyberchondria.
However, these findings contradict the evidence that vaccination against SARS-CoV-2 infection was not predicted by somatic symptoms (52), and persons with high psychosomatic burden are more concerned about their health and visit health care facilities more often (53). Obviously, vaccination against SARS-CoV-2 adherence is more difficult for persons than complying with self-preventive measures. A recent study has shown that vaccine acceptance is positively associated with COVID-19-related anxiety and fears of infection and health-related consequences, whereas social and economic fears are negatively correlated with vaccination willingness (54).
This explains why persons with high socio-economic risks refuse vaccination against SARS-CoV-2. Young persons with high risk for HIV reported wearing facemasks, washing hands, and staying six feet apart, but about one-third of them reported that they would not be vaccinated (55). Refusal or hesitation to vaccinate increased with financial instability (56), working far from the capital (57), lower education background, and uncertainty about the ability of the health care system to treat patients with COVID-19 (58). The non-contributing effect of preventive behavior can be explained by poor knowledge of COVID-19 (59), beliefs in COVID-19 conspiracy theories (60), poor COVID-19 risk perception (61), and skepticism about the virus due to the distrust in politicians and medical scientists (62).
Limitations and future research
There are several limitations and future perspectives in this study. First, this study was cross-sectional. Previous research suggested that cyberchondria played a moderating role in behavior changes and the growth of concerns regarding the COVID-19 between the first and the second wave of the pandemic (63). To draw conclusions on causal effects, future research must rely on longitudinal data. Second, the findings were obtained in a population sample and cannot be generalized to clinical groups. There is evidence that fear of COVID-19, cyberchondria, and somatization differ between healthy persons and patients with mental and physical diseases (64–66). The patterns found should be examined in clinical groups including patients with somatoform disorders. Third, the relationship between fear of COVID-19 and somatic burden can be mediated by some other characteristics. Future research could explore the relationship between fear of COVID-19, cyberchondria, and psychosomatic burden in a broader biopsychosocial approach. Finally, somatic burden was assessed in this study based on self-report instruments. Although previous research has shown that subjective body complaints can be interpreted as a sign of somatization (67), future studies could examine medical records and health care utilization for a clearer perspective.
Conclusion
In conclusion, this study contributes to the growing body of knowledge about the relationship between fear of COVID-19 and somatic burden mediated by cyberchondria, but not preventive behavior. It is hoped that changes in the fear of COVID-19 and somatization severity may reduce the burden of cyberchondria, and with low cyberchondria, fear of COVID-19 would not be as destructive to psychosomatic well-being.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Review Board, HSE University (minutes of the meeting of October 25, 2021). The patients/participants provided their written informed consent to participate in this study.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mutlu E, Anil Yagcioglu EA. Relapse in patients with serious mental disorders during the COVID-19 outbreak: a retrospective chart review from a community mental health center. Eur Arch Psychiatry Clin Neurosci. (2021) 271:381–3. doi: 10.1007/s00406-020-01203-1
2. Jaywant A, Vanderlind WM, Alexopoulos GS, Fridman CB, Perlis RH, Gunning FM. Frequency and profile of objective cognitive deficits in hospitalized patients recovering from COVID-19. Neuropsychopharmacol. (2021) 46:2235–40. doi: 10.1038/s41386-021-00978-8
3. Barello S, Caruso R, Palamenghi L, Nania T, Dellafiore F, Bonetti L, et al. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: an application of the job demands-resources model. Int Arch Occup Environ Health. (2021) 94:1751–61. doi: 10.1007/s00420-021-01669-z
4. Lorant V, Smith P, Van den Broeck K, Nicaise P. Psychological distress associated with the COVID-19 pandemic and suppression measures during the first wave in Belgium. BMC Psychiatry. (2021) 21:112. doi: 10.1186/s12888-021-03109-1
5. Tarsitani L, Vassalini P, Koukopoulos A, Borrazzo C, Alessi F, Di Nicolantonio C, et al. Post-traumatic stress disorder among COVID-19 survivors at 3-month follow-up after hospital discharge. J Gen Intern Med. (2021) 36:1702–7. doi: 10.1007/s11606-021-06731-7
6. Yi J, Kang L, Li J, Gu J. A key factor for psychosomatic burden of frontline medical staff: occupational pressure during the COVID-19 pandemic in China. Front Psychiatry. (2020) 11:590101. doi: 10.3389/fpsyt.2020.590101
7. Sangma RD, Kumar P, Nerli LM, Khanna AM, Vasavada DA, Tiwari DS. Social stigma and discrimination in Coronavirus Disease-2019 survivors and its changing trend: a longitudinal study at tertiary care center Gujarat, India. Asian J Soc Health Behav. (2022) 5:68–74. doi: 10.4103/shb.shb_12_22
8. Patil S, Datar M, Shetty J, Naphade N. Psychological consequences and coping strategies of patients undergoing treatment for COVID-19 at a tertiary care hospital: a qualitative study. Asian J Soc Health Behav. (2021) 4:62–8. doi: 10.4103/shb.shb_5_21
9. Doshi D, Karunakar P, Sukhabogi JR, Prasanna JS, Mahajan SV. Assessing coronavirus fear in Indian population using the fear of COVID-19 scale. Int J Ment Health Addict. (2021) 19:2383–91. doi: 10.1007/s11469-020-00332-x
10. Šljivo A, Kačamaković M, Quraishi I, Kulenović AD. Fear and depression among residents of Bosnia and Herzegovina during COVID-19 outbreak - internet survey. Psychiatr Danub. (2020) 32:266–72. doi: 10.24869/psyd.2020.266
11. Mistry SK, Ali ARMM, Akther F, Yadav UN, Harris MF. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob Health. (2021) 17:47. doi: 10.1186/s12992-021-00698-0
12. Gritsenko VV, Reznik AD, Konstantinov VV, Marinova TY, Khamenka NV, Isralowitz R. Fear of coronavirus disease (COVID-19) and basic personality beliefs. Clin Psychol Special Edu. (2020) 9:99–118. doi: 10.17759/cpse.2020090205 (In Russ.).
13. Cerda AA, García LY. Factors explaining the fear of being infected with COVID-19. Health Expect. (2022) 25:506–12. doi: 10.1111/hex.13274
14. Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J Anxiety Disord. (2020) 74:102258. doi: 10.1016/j.janxdis.2020.102258
15. Quadros S, Garg S, Ranjan R, Vijayasarathi G, Mamun MA. Fear of COVID 19 infection across different cohorts: a scoping review. Front Psychiatry. (2021) 12:708430. doi: 10.3389/fpsyt.2021.708430
16. Hashemi SGS, Hosseinnezhad S, Dini S, Griffiths MD, Lin CY, Pakpour AH. The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID-19 among Iranian online population. Heliyon. (2020) 6:e05135. doi: 10.1016/j.heliyon.2020.e05135
17. Kizilkurt OK, Yilmaz A, Noyan CO, Dilbaz N. Health anxiety during the early phases of COVID-10 pandemic in Turkey and its relationship with postpandemic attitudes, hopelessness, and psychological resilience. Perspect Psychiatr Care. (2021) 57:399–407. doi: 10.1111/ppc.12646
18. Jungmann SM, Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: which factors are related to coronavirus anxiety? J Anxiety Disord. (2020) 73:102239. doi: 10.1016/j.janxdis.2020.102239
19. Wu X, Nazari N, Griffiths MD. Using fear and anxiety related to COVID-19 to predict cyberchondria: cross-sectional survey study. J Med Internet Res. (2021) 23:26285. doi: 10.2196/26285
20. Yalçin I, Boysan M, Eşkisu M, Çam Z. Health anxiety model of cyberchondria, fears, obsessions, sleep quality, and negative affect during COVID-19. Curr Psychol. (2022). doi: 10.1007/s12144-022-02987-2
21. Breakwell GM, Fino E, Jaspal R. The COVID-19 Preventive Behaviors Index: development and validation in two samples from the United Kingdom. Eval Health Prof. (2021) 44:77–86. doi: 10.1177/0163278720983416
22. Islam JY, Vidot DC, Camacho-Rivera M. Determinants of COVID-19 preventive behaviors among adults with chronic diseases in the USA: an analysis of the nationally representative COVID-19 impact survey. BMJ Open. (2021) 11:e044600. doi: 10.1136/bmjopen-2020-044600
23. Šurina S, Martinsone K, Perepjolkina V, Kolesnikova J, Vainik U, RuŽa A, et al. Factors related to COVID-19 preventive behaviors: a structural equation model. Front Psychol. (2021) 12:676521. doi: 10.3389/fpsyg.2021.676521
24. Gutu B, Legese G, Fikadu N, Kumela B, Shuma F, Mosisa W, et al. Assessment of preventive behavior and associated factors towards COVID-19 in Qellam Wallaga Zone, Oromia, Ethiopia: a community-based cross-sectional study. PLoS One. (2021) 16:e0251062. doi: 10.1371/journal.pone.0251062
25. Ozdemir S, Ng S, Chaudhry I, Finkelstein EA. Adoption of preventive behavior strategies and public perceptions about COVID-19 in Singapore. Int J Health Policy Manag. (2022) 11:579–91. doi: 10.34172/IJHPM.2020.199
26. Sánchez-Arenas R, Doubova SV, González-Pérez MA, Pérez-Cuevas R. Factors associated with COVID-19 preventive health behaviors among the general public in Mexico City and the State of Mexico. PLoS One. (2021) 16:e0254435. doi: 10.1371/journal.pone.0254435
27. Mat Dawi N, Namazi H, Maresova P. Predictors of COVID-19 preventive behavior adoption intention in Malaysia. Front Psychol. (2021) 12:616749. doi: 10.3389/fpsyg.2021.616749
28. Alijanzadeh M, Ahorsu DK, Alimoradi Z, Mahmoudi N, Griffiths MD, Lin C-Y, et al. Fear of COVID-19 and trust in the healthcare system mediates the association between individual's risk perception and preventive COVID-19 behaviors among Iranians. Int J Environ Res Public Health. (2021) 18:12146. doi: 10.3390/ijerph182212146
29. Chung GKK, Strong C, Chan YH, Chung RYN, Chen JS, Lin YH, et al. Psychological distress and protective behaviors during the COVID-19 pandemic among different populations: Hong Kong general population, Taiwan healthcare workers, and Taiwan outpatients. Front Med. (2022) 9:800962. doi: 10.3389/fmed.2022.800962
30. Roberts JA, David ME. Improving predictions of COVID-19 preventive behavior: development of a sequential mediation model. J Med Internet Res. (2021) 23:23218. doi: 10.2196/23218
31. Ahorsu DK, Imani V, Lin C-Y, Timpka T, Broström A, Updegraff JA, et al. Associations between fear of COVID-19, mental health, and preventive behaviors across pregnant women and husbands: an actor-partner interdependence modelling. Int J Ment Health Addict. (2022) 20:68–82. doi: 10.1007/s11469-020-00340-x
32. Pakpour AH, Liu CH, Hou WL, Chen YP, Li YP, Kuo YJ, et al. Comparing fear of COVID-19 and preventive COVID-19 infection behaviors between Iranian and Taiwanese older people: early reaction may be a key. Front Public Health. (2021) 9:740333. doi: 10.3389/fpubh.2021.740333
33. Chang KC, Strong C, Pakpour AH, Griffiths MD, Lin CY. Factors related to preventive COVID-19 infection behaviors among people with mental illness. J Formos Med Assoc. (2020) 119:1772–80. doi: 10.1016/j.jfma.2020.07.032
34. Kuo YJ, Chen YP, Wang HW, Liu C, Strong C, Saffari M, et al. Community outbreak moderates the association between COVID-19-related behaviors and COVID-19 fear among older people: a one-year longitudinal study in Taiwan. Front Med. (2021) 8:756985. doi: 10.3389/fmed.2021.756985
35. Satsangi AK, Brugnoli MP. Anxiety and psychosomatic symptoms in palliative care: from neuro-psychobiological response to stress, to symptoms' management with clinical hypnosis and meditative states. Ann Palliat Med. (2018) 7:75–111. doi: 10.21037/apm.2017.07.01
36. Liu S, Liu Y, Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. (2020) 289:113070. doi: 10.1016/j.psychres.2020.113070
37. Shevlin M, Nolan E, Owczarek M, McBride O, Murphy J, Miller JG, et al. COVID-19-related anxiety predicts somatic symptoms in the UK population. Br J Health Psychol. (2020) 25:875–82. doi: 10.1111/bjhp.12430
38. Suhail A, Dar KA, Iqbal N. COVID-19 related fear and mental health in Indian sample: the buffering effect of support system. Curr Psychol. (2021) 41:1–12. doi: 10.1007/s12144-021-01694-8
39. Yuan Y, Deng Z, Chen M, Yin D, Zheng J, Liu Y, et al. Changes in mental health and preventive behaviors before and after COVID-19 vaccination: a propensity score matching (PSM) study. Vaccines (Basel). (2021) 9:1044. doi: 10.3390/vaccines9091044
40. Arsenakis S, Chatton A, Penzenstadler L, Billieux J, Berle D, Starcevic V, et al. Unveiling relationships between cyberchondria and psychopathological symptoms. J Psychiatr Res. (2021) 143:254–61. doi: 10.1016/j.jpsychires.2021.09.014
41. Nazzal Z, Maraqa B, Abu Zant M, Qaddoumi L, Abdallah R. Somatic symptom disorders and utilization of health services among Palestinian primary health care attendees: a cross-sectional study. BMC Health Serv Res. (2021) 21:615. doi: 10.1186/s12913-021-06671-2
42. Gierk B, Kohlmann S, Kroenke K, Spangenberg L, Zenger M, Brähler E, et al. The somatic symptom scale-8 (SSS-8): a brief measure of somatic symptom burden. JAMA Intern Med. (2014) 174:399–407. doi: 10.1001/jamainternmed.2013.12179
43. Zolotareva AA. Factor structure of the Russian version of the Somatic Symptom Scale-8 (SSS-8). Couns Psychol Psychotherapy. (2022) 30:8–20. doi: 10.17759/cpp.2022300302
44. Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID- 19 scale: development and initial validation. Int J Ment Health Addict. (2022) 20:1537–45. doi: 10.1007/s11469-020-00270-8
45. Reznik A, Gritsenko V, Konstantinov V, Khamenka N, Isralowitz R. COVID-19 fear in Eastern Europe: validation of the Fear of COVID-19 Scale. Int J Ment Health Addict. (2021) 19:1903–8. doi: 10.1007/s11469-020-00283-3
46. McElroy E, Kearney M, Touhey J, Evans J, Cooke Y, Shevlin M. The CSS-12: Development and validation of a short-form version of the Cyberchondria severity scale. Cyberpsychol Behav Soc Netw. (2019) 22:330–5. doi: 10.1089/cyber.2018.0624
47. Zolotareva AA. Assessment of cyberchondria: Prospects and limitations. In: Zvereva NV, editor. Diagnostics in Medical (Clinical) Psychology: Traditions and Outlook. Theses and Articles of the 3rd All-Russian Conference with International Participation (2021). p. 260–2.
48. Behr D. Assessing the use of back translation: the shortcomings of back translation as a quality testing method. Int J Soc Res Methodol. (2017) 20:573–84. doi: 10.1080/13645579.2016.1252188
49. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: The Guilford Press (2013).
50. Vismara M, Benatti B, Ferrara L, Colombo A, Bosi M, Varinelli A, et al. A preliminary investigation of cyberchondria and its correlates in a clinical sample of patients with obsessive-compulsive disorder, anxiety and depressive disorders attending a tertiary psychiatric clinic. Int J Psychiatry Clin Pract. (2021) 25:1–12. doi: 10.1080/13651501.2021.1927107
51. Clarke DM, Piterman L, Byrne CJ, Austin DW. Somatic symptoms, hypochondriasis and psychological distress: a study of somatization in Australian general practice. Med J Aust. (2008) 189:560–4. doi: 10.5694/j.1326-5377.2008.tb02180.x
52. Simione L, Vagni M, Gnagnarella C, Bersani G, Pajardi D. Mistrust and beliefs in conspiracy theories differently mediate the effects of psychological factors on propensity for COVID-19 vaccine. Front Psychol. (2021) 12:683684. doi: 10.3389/fpsyg.2021.683684
53. Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry. (2005) 62:903–10. doi: 10.1001/archpsyc.62.8.903
54. Bendau A, Plag J, Petzold MB, Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. (2021) 97:107724. doi: 10.1016/j.intimp.2021.107724
55. Christodoulou J, Fehrenbacher AE, Shaw EH, Vincent EM, Saleska JL. COVID-19 prevention behaviors, trust, and intent to vaccinate among youth at risk for HIV. PLoS One. (2022) 17:e0266321. doi: 10.1371/journal.pone.0266321
56. Muhajarine N, Adeyinka DA, McCutcheon J, Green KL, Fahlman M, Kallio N. COVID-19 vaccine hesitancy and refusal and associated factors in an adult population in Saskatchewan, Canada: evidence from predictive modelling. PLoS One. (2021) 16:e0259513. doi: 10.1371/journal.pone.0259513
57. Zammit N, Gueder AE, Brahem A, Ayouni I, Ghamman R, Fredj SB, et al. Studying SARS-CoV-2 vaccine hesitancy among health professionals in Tunisia. BMC Health Serv Res. (2022) 22:489. doi: 10.1186/s12913-022-07803-y
58. Thanapluetiwong S, Chansirikarnjana S, Sriwannopas O, Assavapokee T, Ittasakul P. Factors associated with COVID-19 vaccine hesitancy in Thai seniors. Patient Prefer Adher. (2021) 15:2389–403. doi: 10.2147/PPA.S334757
59. Feleke BT, Wale MZ, Yirsaw MT. Knowledge, attitude and preventive practice towards COVID-19 and associated factors among outpatient service visitors at Debre Markos compressive specialized hospital, north-west Ethiopia, 2020. PLoS One. (2021) 16:e0251708. doi: 10.1371/journal.pone.0251708
60. Ferreira S, Campos C, Marinho B, Rocha S, Fonseca-Pedrero E, Rocha B. What drives beliefs in COVID-19 conspiracy theories? The role of psychotic-like experiences and confinement-related factors. Soc Sci Med. (2022) 292:114611. doi: 10.1016/j.socscimed.2021.114611
61. Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, Splegelhalter D, et al. COVID-19 risk perception: a longitudinal analysis of its predictors and associations with health protective behaviors in the United Kingdom. J Risk Res. (2021) 24:294–313. doi: 10.1080/13669877.2021.1890637
62. Priniski JH, Holyoak KJ. A darkening spring: how preexisting distrust shaped COVID-19 skepticism. PLoS One. (2022) 17:e0263191. doi: 10.1371/journal.pone.0263191
63. Jokic-Begic N, Lauri Korajlija A, Mikac U. Cyberchondria in the age of COVID-19. PLoS One. (2020) 15:e0243704. doi: 10.1371/journal.pone.0243704
64. Shahini N, Ghasemzadeh M, Javan M, Salimi Z. Evaluation of the COVID-19 pandemic effect on the development of somatic symptoms in patients with mood disorders: a case-control study. New Microbes New Infect. (2021) 43:100917. doi: 10.1016/j.nmni.2021.100917
65. Musche V, Kohler H, Bäuerle A, Schweda A, Weismüller B, Fink M, et al. COVID-19-related fear, risk perception, and safety behavior in individuals with diabetes. Healthcare. (2021) 9:480. doi: 10.3390/healthcare9040480
66. Vismara M, Vitella D, Biolcati R, Ambrosini F, Pirola V, Dell'Osso B, et al. The impact of COVID-19 pandemic on searching for health-related information and cyberchondria on the general population in Italy. Front Psychiatry. (2021) 12:754870. doi: 10.3389/fpsyt.2021.754870
Keywords: somatic burden, fear of COVID-19, cyberchondria, preventive behavior, COVID-19 pandemic
Citation: Zolotareva A (2022) Cyberchondria, but not preventive behavior, mediates the relationship between fear of COVID-19 and somatic burden: Evidence from Russia. Front. Psychiatry 13:1018659. doi: 10.3389/fpsyt.2022.1018659
Received: 13 August 2022; Accepted: 08 September 2022;
Published: 26 September 2022.
Edited by:
Vsevolod Konstantinov, Penza State University, RussiaReviewed by:
Chung-Ying Lin, National Cheng Kung University, TaiwanAndrés Alexis Ramírez Coronel, Catholic University of Cuenca, Ecuador
Nabi Nazari, Lorestan University, Iran
Copyright © 2022 Zolotareva. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alena Zolotareva, alena.a.zolotareva@gmail.com
 Alena Zolotareva
Alena Zolotareva