- 1Faculty of Medicine of Tunis, Tunis El Manar University, Tunis, Tunisia
- 2The Tunisian Center of Early Intervention in Psychosis, Department of Psychiatry Ibn Omrane, Razi Hospital, Tunis, Tunisia
- 3School of Medicine and Medical Sciences, Holy Spirit University of Kaslik, Jounieh, Lebanon
- 4Psychology Department, College of Humanities, Effat University, Jeddah, Saudi Arabia
- 5Research Department, Psychiatric Hospital of the Cross, Jal Eddib, Lebanon
- 6College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Bahrain
- 7Department of Psychiatry, Ministry of Health, Manama, Bahrain
There is strong evidence that sleep disturbances are commonly experienced by people with psychosis. Evidence has also shown that sleep disturbances are present since the very early stages of the disease, even during the pre-diagnostic phase. More recently, research involving young individuals at ultra-high risk (UHR) for psychosis documented frequent occurrence of sleep disturbances in this group. The very early onset of sleep disturbances in the course of psychosis has drawn attention to the possible links between sleep parameters and the risk of psychosis. To date, the nature of sleep disturbances characterizing the UHR stage remains unclear, with available studies having yielded mixed findings. In this regard, we performed this review to update the body of literature on the nature of sleep disturbances, their underlying mechanisms, their clinical and functional consequences, the prevention and intervention strategies in the at-risk for psychosis population. Our findings provided further support to the presence of disturbed sleep in UHR individuals as evidenced by subjective and objective sleep measures such as polysomnography, sleep electroencephalograms, and actigraphy. Reviewing the possible mechanisms underlying the relationship between sleep and psychosis emphasized its complex and multifactorial nature which is yet to be determined and understood. Further research is warranted to determine which facets of sleep disturbances are most detrimental to this specific population, and to what extent they can be causal factors or markers of psychosis.
Introduction
Sleep is an essential biological function that results from a complex interaction between neurobiological, hormonal, and homeostatic processes. Sleep disturbances are highly prevalent worldwide, affecting one out of five adult people in the community (1). In particular, there is strong evidence that sleep disturbances are experienced to a higher extent by people with psychosis than healthy individuals (2, 3). Substantial sleep problems are reported by up to 80% patients with psychosis in remission (2, 4), are linked to impaired cognitive and functional capacities (5), and contribute to a significant decrease in life expectancy (6). Evidence has also shown that sleep disturbances are present since the very early stages of the disease (7), even during the pre-diagnostic phase (8, 9). More recently, research involving young individuals at ultra-high risk (UHR) for psychosis documented frequent occurrence of sleep disturbances in this group (10, 11). The very early onset of sleep disturbances in the course of psychosis has drawn attention to the possible links between sleep parameters and the risk of psychosis; and has led some authors to suggest that sleep problems are not causally related to chronic symptoms or medication but rather appear to be promising biomarkers of the disease (7, 12). The UHR state refers to the presence of one of the following: attenuated psychotic symptoms, brief limited intermittent psychotic episode, and genetic risk and deterioration syndrome (i.e., trait vulnerability with marked decline in functioning) (13). Being able to intervene during the UHR stage through targeting modifiable factors, such as sleep, offers the opportunity to be more impactful on outcomes by resorting to simpler, more personalized and less harmful treatments (14–16). However, the nature of sleep disturbances characterizing the UHR stage remains unclear, with available studies having yielded mixed findings (10). In addition, potential mechanisms involved in the association between sleep and psychosis etiology are still largely unknown (17). We could find only one previous review that included data prior to February 2020 to examine sleep disturbances in the UHR state, with the specific goal of exploring the relationships between sleep and psychotic symptoms, functioning and quality of life (18). Some interesting new studies have emerged since then [e.g., (19–22)]. This, along with the identified knowledge gaps, have motivated the present review aiming at synthetizing the existing literature to update and extend our understanding of: (1) the nature of sleep disturbances, (2) their underlying mechanisms, (3) their clinical and functional consequences, as well as (4) the prevention and intervention strategies in the at-risk for psychosis population.
Methods
In the present mini-review, we performed a literature search using electronic databases (i.e., Pub Med, Web of Science, and Scopus). All studies have been selected according to the following criteria: (1) original peer-reviewed articles written in English, with no time period limits; (2) study samples comprising individuals (aged 12–35 years old) defined as meeting UHR criteria based on the presence of attenuated psychotic symptoms, genetic risk, and functional deterioration; as ascertained by structured clinical interviews [e.g., the Comprehensive Assessment of the At Risk Mental State (CAARMS) (23); the Structured Interview for Prodromal Symptoms (SIPS) (24), the Structured Clinical Interview for DSM Disorders (SCID) (25)]; and (3) studies providing data on sleep disturbances in UHR individuals as assessed using either subjective or objective measures. The articles were selected using cross-matched keywords combination: [At-Risk Mental State [OR] Clinical high risk state [OR] Ultra-high risk [OR] prodromal state [OR] prepsychotic phase [OR] psychosis risk [OR] emergent psychosis [OR] early psychosis) [AND] (sleep [OR] sleep disorders [OR] sleep problems [OR] sleep disturbances [OR] sleep quality [OR] insomnia [OR] sleepiness [OR] circadian rhythm [OR] chronotype [OR] polysomnography [OR] actigraphy]. In addition, a backward search and a Google search were conducted in order to detect any other possible missing relevant research studies or unpublished (gray) literature.
The nature of sleep disturbances in UHR individuals
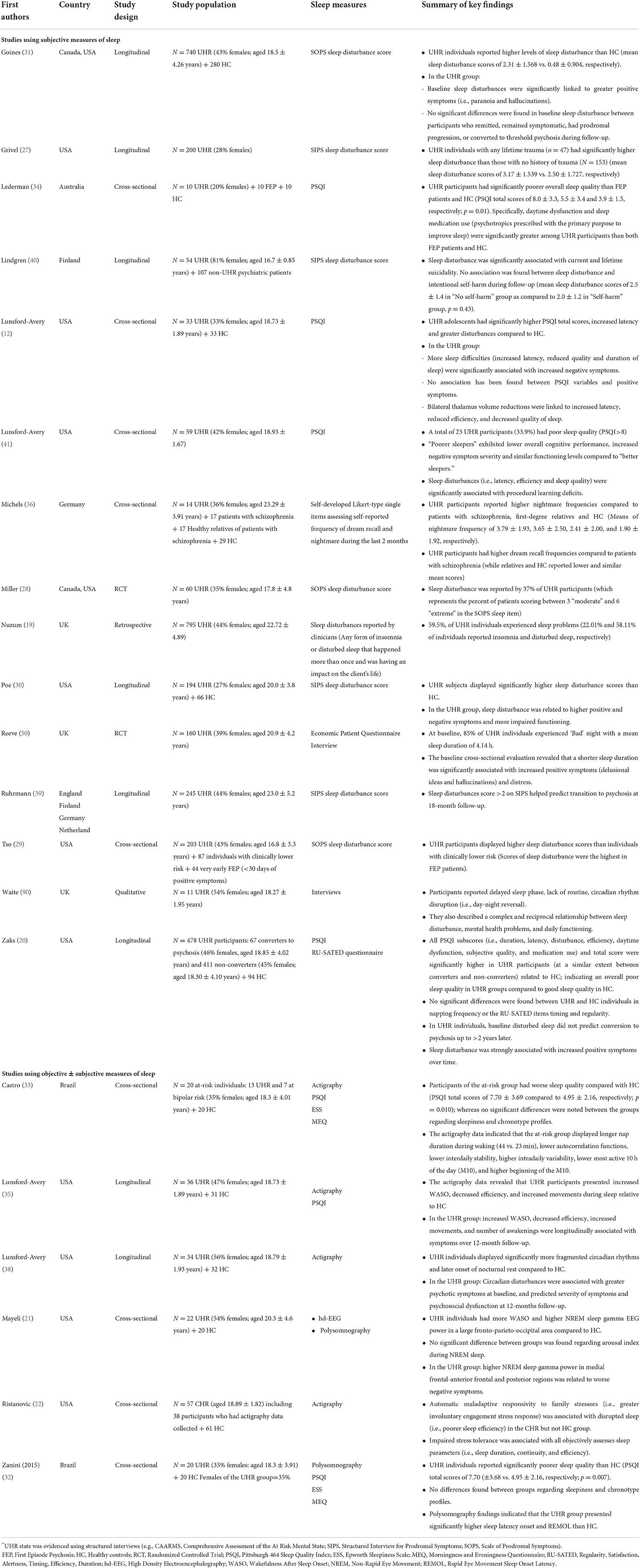
There are two ways to measure sleep disturbances; one is subjective through self-reported [e.g., PSQI (26)] or interviewer-reported [e.g., Scale of Prodromal Symptoms (SOPS)/Structured Interview for Psychosis-Risk Syndromes (SIPS) sleep disturbance items (24)] sleep questionnaires, and the other is objective (e.g., sleep parameters/architecture according to actigraphy or polysomnography). As such, this section will be divided into two parts; the first part reports findings on subjective sleep disturbances, while the second one includes characteristics of objective sleep assessments for UHR individuals (see Table 1 for further details on key findings of the reviewed studies).
Subjective sleep disturbances in UHR individuals
Most of the existing studies found that sleep disturbances were highly prevalent in UHR individuals based on the structured interviews SIPS/SOPS sleep disturbance scores (27–30); and were reported to a greater extent by UHR groups compared to clinically lower risk patients (29) and healthy volunteers (30, 31). Beyond general sleep disturbances, some previous studies documented worse overall sleep quality (according to higher PSQI scores) in UHR individuals as compared to healthy controls (12, 20, 32–34), and even to first episode psychosis (FEP) patients (34). In particular, UHR individuals displayed longer sleep latency (i.e., the amount of time between reclining in bed and the onset of sleep) (12, 32, 35), shorter sleep duration in hours per night (20), greater daily sleep disturbances (e.g., night time and early morning awakenings) (12), greater daytime dysfunction due to sleepiness (20, 34), and increased sleep medication use (20, 34). Conversely, other studies did not find any differences in self-reported sleep latency (34) sleep duration (12, 34) and sleepiness scores (33) between UHR subjects and healthy controls. One prior research showed that UHR respondents exhibited significantly higher self-reported nightmare frequencies compared to healthy controls, and more dream recall frequencies compared to patients with schizophrenia (36). Finally, two studies using the Morningness and Eveningness Questionnaire (MEQ) (37) found no significant differences in self-reported chronotype profiles between UHR and healthy individuals (32, 33).
Objective sleep disturbances in UHR individuals
We could find only two polysomnography studies, which revealed that the UHR group presented significantly more Wake After Sleep Onset (WASO) (21) and increased sleep latency (i.e., more difficulty falling asleep) than HC (32). Zanini et al. (32) did not find significant differences in the polysomnographic sleep efficiency percentages, WASO scores, and total sleep time and of UHR participants relative to controls. The actigraphy data indicated that UHR individuals experienced increased WASO, decreased efficiency (22), increased night time movements (35), longer daytime nap duration (33), more fragmented circadian rhythms (33, 38) and later onset of nocturnal rest (38) compared to healthy controls. Based on sleep high density-Electroencephalography (hd-EEG) recordings, Mayeli et al. (21) found that UHR participants presented increased EEG gamma activity during non-rapid eye movement sleep in a large fronto-parieto-occipital area compared to controls.
Summary of past subjective and objective studies
In sum, previous studies highlighted a wide range of both subjectively and objectively assessed sleep disturbances in UHR individuals, including increased sleepiness, daytime naps, sleep latency, night time movements, nightmares, and a disrupted circadian rhythm. Overall, studies using subjective measures were more represented in the existing literature than those using objective measures, and mainly focused on general sleep disturbance [non-specific sleep disturbance severity scales of the SIPS/SOPS; n = 7 studies (27–31, 39, 40)], sleep quality [SPSQI; n = 7 studies (12, 20, 32–35, 41)], sleepiness [ESS; n = 2 (32, 33)], and chronotype [MEQ; n = 2 studies (32, 33)]. However, yet no studies assessed insomnia symptoms in UHR subjects using self-report measures [e.g., Insomnia Severity Index (42), Athens Insomnia Scale (43)]; despite having shown to be prevalent and severe in patients with psychosis (44, 45). We could identify only six previous studies using objective sleep measures; four of them used Actigraphy (33, 35, 38) and two used polysomnography (21, 32). All these studies involved small sample sizes (20–38 UHR individuals), and four of them had a cross-sectional design. These identified gaps may limit the conclusions drawn from the current review, and contribute to give an insight to future research in this field. Additional long-term cohort observation studies using objective sleep parameters and large sample sizes to better represent the UHR population are still very needed. It is also important that we draw attention to the fact that all studies in this topic have been performed in Western countries. Research from other parts of the world would be highly informative and should be encouraged.
Associations between sleep disturbances and clinical/functional outcomes in UHR individuals
Sleep disturbances have proven to be associated with various negative outcomes in patients with early and chronic psychosis, including heightened psychotic symptom severity, greater suicidality, increased cognitive deficits, as well as impaired functioning and quality of life (11, 46, 47). In this section, we propose to review the available research on the effects of sleep disturbances on various clinical and functioning outcomes in UHR individuals.
Associations between sleep disturbances and clinical outcomes
A limited amount of research has specifically addressed the contribution of sleep disturbances to psychotic symptoms in UHR individuals (11, 48–50). Some studies found that several disrupted sleep parameters at baseline (e.g., increased WASO, reduced efficiency, heightened night-time movements and more awakenings, lowered sleep time, fragmented circadian rhythm) were significant longitudinal predictors of the later severity of positive (35, 38, 50) and negative (38) psychotic symptoms. A recent longitudinal study (20) tracked sleep during 8 months in 478 UHR individuals, and showed that sleep disturbance was strongly and prospectively linked to increased psychotic symptoms (positive, negative, disorganized, and general) over time. Lunsford-Avery et al. (35) found that both baseline self-reported and actigraphic-measured sleep disturbance (i.e., decreased sleep efficiency, increased WASO, greater number of awakenings, and increased movements) helped predict the longitudinal course of positive symptoms specifically in UHR individuals; whereas no significant correlation has been found between actigraphic variables and negative symptoms over time. More particularly, findings from a large retrospective study from the UK demonstrated a specific association between sleep problems and greater perceptual abnormality frequency and severity in young UHR individuals (19). Similarly, Goines et al. (31) pointed to the specific effect of hallucinations on sleep over other attenuated psychotic symptoms. While these two studies (19, 31) suggested that perceptual abnormalities may lead to sleep disturbances in UHR individuals, other authors claimed a reversed pattern of association (51); highlighting the need for additional studies to elucidate the direction and nature of this relationship.
To summarize, the majority of the existing longitudinal studies cited above agreed that sleep disturbances are associated with subsequent psychotic symptoms exacerbation, which may in turn lead to poor mental health and functional outcomes even in individuals recovering from their at-risk state (52, 53). However, the observed impact of sleep disturbance on psychotic symptoms evolution over time is still unclear mainly due to a lack of longitudinal studies (20), which highlights the need for further investigations.
Associations between sleep disturbances and functional outcomes
Sleep problems have been consistently shown to impact cognitive processes and daytime functioning (54). Severe cognitive deficits and subsequent daily functional impairment are common outcomes in UHR youth, regardless of eventual conversion to threshold psychosis (53, 55, 56). Some cross-sectional evidence suggested that sleep disturbances are associated with more psychosocial dysfunctioning (30, 41). However, to date, little attention has been paid to the prospective relationship between sleep and functional outcomes in UHR individuals (10). One longitudinal research by Lunsford-Avery et al. found that objectively assessed circadian rhythm disruption at baseline predicted worse psychosocial functioning levels at 12-months follow up (38). More recently, Nuzum et al. (19) investigated 795 clinical records of UHR patients and found that sleep problems predicted worse follow-up levels of social functioning. Although sleep is a potentially modifiable factor (57, 58), that when treated could substantially and independently improve functional outcomes (59), its impact on functioning, quality of life and overall wellbeing in UHR states remain largely understudied (10). Therefore, further studies allowing a deeper understanding of the pathways linking sleep to developmental and long-term outcomes in UHR youth are required.
Sleep disturbance as a risk factor for transition to psychosis
It is well-established that a proportion of UHR individuals will convert later to a clinical psychosis (60, 61). Although evidence showing that sleep disturbances are present in UHR individuals before any psychosis onset (8, 31, 32, 39), there has been very limited interest so far on how abnormal sleep patterns may contribute to the transition risk (20). The first attempt to use sleep disturbances in the prediction of transition to psychosis was performed by Ruhrmann et al. (39) through a large prospective European study (39), and documented sleep as a strong predictive factor of transition from subthreshold to full-threshold psychosis over 18 months of follow-up (39). Inconsistent findings have emerged thereafter; with some studies showing that sleep problems represented a risk indicator for both the persistence and/or exacerbation of psychotic symptoms over time (35, 62); while others found no significant effect of sleep on psychosis transition (20, 30, 31). More recently, Nuzum et al. (19) found that, despite a lack of significant association between sleep parameters and transition to psychosis, sleep disturbances were significantly correlated with a shorter time to transition in UHR individuals converted to psychosis. Zaks et al. (20) suggested that disrupted sleep patterns may act as risk factors for transition only in aggregation with other potential factors. Overall, the pathways between sleep and psychosis are rather complex and have been hypothesized to be bidirectional (63). The eventual role that sleep would play in the development and progress of psychotic symptoms raises the question of its underlying mechanisms of the effects of sleep on the pathogenesis of psychosis (11, 49, 64). We propose to address this question in the next section.
Explaining mechanisms of the relation sleep disturbances–psychosis
The implication of sleep on the development and progress of psychosis has attracted a growing interest during the last years. A key hypothesis that has particularly received attention is the presence of structural brain abnormalities and neural development alterations which may likely lead to sleep alterations, and in turn psychotic symptoms, from the very early stages of psychosis (64). Structural brain alterations in the thalamic region are involved in both human sleep dysregulation (65), and the etiopathogeny of schizophrenia (66, 67). A thalamic volume reduction is noted early during the course of psychotic disorders, and exacerbates as the disease progresses (68). In this regard, a study by Lunsford-Avery et al. revealed that UHR individuals had a reduced bilateral thalamic volume that significantly related to poorer sleep quality (12). A recent review suggested that aberrant thalamic function could result in sleep spindle deficits and altered EEG microstate dynamics (69). These alterations [e.g., increased non-rapid eye movement gamma EEG activity (21)] have been previously reported in UHR individuals, and could, in turn, represent “potent endophenotypes” and “vulnerability factors” for psychosis (69). This brings us back to the hypothesis stated earlier by Feinberg (70), that the great rearrangement of brain function and structure occurring during early adolescence, including maturational changes in EEG sleep patterns (i.e., decline in EEG amplitude), may have resulted from a decrease in cortical synaptic density, which may in turn underlie the emergence of schizophrenia. In this line of research, a relevant hypothesized biological mechanism underlying the effect of sleep on psychosis risk is a defective synaptic transmission. Acetylcholine has been shown to play a major role in both sleep and hallucinatory phenomena (71). As such, it has been suggested that sleep deprivation can be a direct cause of hallucinations and progression toward psychosis due to cholinergic depletion (51).
Other explaining mechanisms for the association between sleep and subsequent psychosis have been identified, such as negative affects (i.e., depression and anxiety) (72–74), endocrine dysfunction due to exposure to psychosocial and biological stress, and cognitive deficits (64). In this regard, some biological markers have been found to interfere with both psychosis proneness and sleep disturbances through a stress-induced activation of the hypothalamic–pituitary–adrenal (HPA) axis, including elevated cortisol levels (75, 76) and pro-inflammatory cytokines (77, 78). Interestingly, an increased reactivity to stress has recently been found to directly affect sleep in the UHR stage. For instance, Ristanovic et al. (22) found that maladaptive responsivity to family stressors and impaired stress tolerance were associated with disrupted sleep as assessed objectively in UHR subjects. Another previous study (41) suggested a pathway in which sleep problems amplify stress indirectly through a negative effect on cognition.
All the above-mentioned factors would interplay and together contribute to sleep disturbances and psychosis in vulnerable young people, highlighting “a possible role for sleep dysfunction within a neurodevelopmental diathesis–stress model for schizophrenia” (64). In sum, despite increased efforts to elucidate the complex relationship sleep-psychosis, a long way remains ahead before understanding what mechanisms are behind the observed patterns of relationships between these two constructs.
Prevention and intervention strategies targeting sleep for UHR individuals
Our review of the literature identified several altered subjective and objective sleep parameters in the at-risk stage of psychosis (10, 16), that have even been hypothesized as causal mechanisms of psychosis development and persistence (49, 79). Sleep is a malleable factor that has been shown to worsen psychotic symptoms when non-treated (20, 35, 62, 72), or reduce them and improve functional outcomes when treated (59, 80). As such, we suggest that although the directionality and the specific mechanisms underlying the relationship sleep-psychosis have not yet been elucidated, treatment of sleep problems has the potential to either reduce the risk of developing psychosis (as a causal factor) (49, 79), or prevent worsening of the disease outcomes (as an effect of prodromal symptoms) (59, 80).
When present, sleep disturbances are recommended to be screened for, monitored and treated according to the DSM-5 recommendations (81). Therefore, we suggest that screening for and addressing sleep disturbances should be a routine practice in early intervention services to help with reducing their clinical and functional impact on young UHR individuals (82). Promoting sleep in this vulnerable population may be a promising intervention target for symptom and functioning improvement (20), and possibly for delay or prevention of transition to psychosis (39, 83).
Sleep management in psychosis has been shown to be limited by several challenges. First, sleep disturbances are often not given the required focus (10) and are thus underestimated and undertreated. Second, clinicians tend to evaluate sleep informally and offer no or inadequate treatment (e.g., pharmacotherapy instead of the recommended first-line psychotherapy) (84, 85). Third, at the present time no consensual recommendations are available for the management of sleep problems in UHR patients. Basic sleep hygiene education has proven to be beneficial in people with psychosis (11, 46). In this regard, some authors demonstrated the benefits of a low cost and simple sleep intervention for early psychosis patients, consisting of sleep hygiene advice along with a provision of a wearable sleep tracker (86). Accumulated evidence has confirmed the effectiveness of the Cognitive Behavioral Therapy for insomnia (CBTi) in UHR states (80, 82, 87). The CBTi has also been proven to have wider benefits by improving depression, anxiety (44, 80, 88), and attenuated psychotic symptoms (44, 80). Other sleep interventions have been specifically designed and tested for use in young UHR people, such as the brief psychological intervention “SleepWell” that targets key sleep parameters (i.e., hyperarousal, sleep pressure, and circadian rhythm), and has yielded promising preliminary results (82). The SleepWell is now being tested in a randomized trial in young patients at ultra-high-risk of psychosis [for further details, see the published protocol (89)].
Conclusion and perspectives
The current review extends our existing knowledge by further highlighting the presence of disturbed sleep in UHR individuals as evidenced by subjective and objective sleep measures such as polysomnography, sleep electroencephalograms, and actigraphy. Reviewing the possible mechanisms underlying the relationship between sleep and psychosis emphasizes its complex and multifactorial nature which is yet to be determined and understood. Our literature search revealed that this topic has attracted relatively scant research attention so far. Nevertheless, the early intervention field is a growing area of research and we expect that studies on sleep and UHR will continue to increase during the coming years. As such, we believe that our Mini review will shed light on the importance of further focusing on this promising avenue of research. Further high-quality longitudinal and experimental research on sleep involving large samples of UHR individuals and using a broad range of sleep parameters is warranted to determine which facets of sleep disturbances are most detrimental to this specific population, and to what extent they can be causal factors or markers of psychosis. This research can help deepen our understanding of the continuum of psychosis vulnerability; and inform psychosis-risk prediction models as well as prevention and early intervention programs.
Author contributions
FF-R wrote the first draft. SH, MC, and HJ provided intellectual contributions to strengthening the manuscript. All authors were involved in revising the manuscript and approved the final version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ohayon MM. Epidemiological overview of sleep disorders in the general population. Sleep Med Res. (2011) 2:1–9. doi: 10.17241/smr.2011.2.1.1
2. Kaskie RE, Graziano B, Ferrarelli F. Schizophrenia and sleep disorders: links, risks, management challenges. Nat Sci Sleep. (2017) 9:227–39. doi: 10.2147/NSS.S121076
3. Rowland LM, Wickwire EM. A wake-up call: assess and treat sleep disorders in early psychosis. Schizophr Bull. (2019) 45:265–6. doi: 10.1093/schbul/sby187
4. Meyer N, Faulkner SM, McCutcheon RA, Pillinger T, Dijk D-J, MacCabe JH. Sleep and circadian rhythm disturbance in remitted schizophrenia and bipolar disorder: a systematic review and meta-analysis. Schizophr Bull. (2020) 46:1126–43. doi: 10.1093/schbul/sbaa024
5. Kaskie RE, Graziano B, Ferrarelli F. Topographic deficits in sleep spindle density and duration point to frontal thalamo-cortical dysfunctions in first-episode psychosis. J Psychiatr Res. (2019) 113:39–44. doi: 10.1016/j.jpsychires.2019.03.009
6. Hayes JF, Marston L, Walters K, King MB, Osborn DP. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000–2014. Br J Psychiatry. (2017) 211:175–81. doi: 10.1192/bjp.bp.117.202606
7. Fekih-Romdhane F, Nefzi H, Sassi H, Cherif W, Cheour M. Sleep in first-episode schizophrenia patients, their unaffected siblings and healthy controls: a comparison. Early Interv Psychiatry. (2021) 15:1167–78. doi: 10.1111/eip.13058
8. Tan HY, Ang YG. First-episode psychosis in the military: a comparative study of prodromal symptoms. Aust N Z J Psychiatry. (2001) 35:512–9. doi: 10.1046/j.1440-1614.2001.00912.x
9. Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. (1996) 22:353–70. doi: 10.1093/schbul/22.2.353
10. Clarke L, Chisholm K, Cappuccio FP, Tang NKY, Miller MA, Elahi F, et al. Sleep disturbances and the At Risk Mental State: a systematic review and meta-analysis. Schizophr Res. (2021) 227:81–91. doi: 10.1016/j.schres.2020.06.027
11. Davies G, Haddock G, Yung AR, Mulligan LD, Kyle SD. A systematic review of the nature and correlates of sleep disturbance in early psychosis. Sleep Med Rev. (2017) 31:25–38. doi: 10.1016/j.smrv.2016.01.001
12. Lunsford-Avery JR, Orr JM, Gupta T, Pelletier-Baldelli A, Dean DJ, Smith Watts AK, et al. Sleep dysfunction and thalamic abnormalities in adolescents at ultra high-risk for psychosis. Schizophr Res. (2013) 151:148–53. doi: 10.1016/j.schres.2013.09.015
13. Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rössler A, Schultze-Lutter F, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. (2013) 70:107–20. doi: 10.1001/jamapsychiatry.2013.269
14. McGorry P. Prevention, innovation and implementation science in mental health: the next wave of reform. Br J Psychiatry. (2013) 202:s3–4. doi: 10.1192/bjp.bp.112.119222
15. McGorry P, Keshavan M, Goldstone S, Amminger P, Allott K, Berk M, et al. Biomarkers and clinical staging in psychiatry. World Psychiatry. (2014) 13:211–23. doi: 10.1002/wps.20144
16. Dondé C, Jaffiol A, Khouri C, Pouchon A, Tamisier R, Lejoyeux M, et al. Sleep disturbances in early clinical stages of psychotic and bipolar disorders: a meta-analysis. Aust N Z J Psychiatry. (2021) 56:1068–79. doi: 10.1177/00048674211068395
17. Lunsford-Avery JR, Damme KS, Vargas T, Sweitzer MM, Mittal VA. Psychotic-like experiences associated with sleep disturbance and brain volumes in youth: findings from the adolescent brain cognitive development study. JCPP Adv. (2021) 1:e12055. doi: 10.1002/jcv2.12055
18. Clarke S, Hanna D, Davidson S, Shannon C, Mulholland C. The association between sleep quality and attenuated psychotic symptoms. Early Interv Psychiatry. (2021) 15:837–48. doi: 10.1111/eip.13020
19. Nuzum E, Hammoud R, Spencer T, Akande I, Tognin S. No rest for the weary: prevalence, impact and nature of sleep problems among young people at risk of psychosis. Early Interv Psychiatry. (2022) 16:651–8. doi: 10.1111/eip.13210
20. Zaks N, Velikonja T, Parvaz MA, Zinberg J, Done M, Mathalon DH, et al. Sleep disturbance in individuals at clinical high risk for psychosis. Schizophr Bull. (2022) 48:111–21. doi: 10.1093/schbul/sbab104
21. Mayeli A, LaGoy A, Donati FL, Kaskie RE, Najibi SM, Ferrarelli F. Sleep abnormalities in individuals at clinical high risk for psychosis. J Psychiatr Res. (2021) 137:328–34. doi: 10.1016/j.jpsychires.2021.03.006
22. Ristanovic I, Haase CM, Lunsford-Avery JR, Mittal VA. The relationship between stress responding in family context and stress sensitivity with sleep dysfunction in individuals at clinical high-risk for psychosis. J Psychiatr Res. (2022) 149:194–200. doi: 10.1016/j.jpsychires.2022.02.038
23. Yung A, Phillips L, McGorry P, Ward J, Donovan K, Thompson K. Comprehensive Assessment of at-Risk Mental States (CAARMS). Melbourne, VIC, Australia: University of Melbourne, Department of Psychiatry, Personal Assessment and Crisis Evaluation Clinic (2002).
24. Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. (2003) 29:703–15. doi: 10.1093/oxfordjournals.schbul.a007040
25. Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the structured clinical interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother. (2011) 18:75–9. doi: 10.1002/cpp.693
26. Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
27. Grivel MM, Leong W, Masucci MD, Altschuler RA, Arndt LY, Redman SL, et al. Impact of lifetime traumatic experiences on suicidality and likelihood of conversion in a cohort of individuals at clinical high-risk for psychosis. Schizophr Res. (2018) 195:549–53. doi: 10.1016/j.schres.2017.09.006
28. Miller T, Zipursky R, Perkins D, Addington J, Woods S, Hawkins K, et al. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis: II. baseline characteristics of the “prodromal” sample. Schizophr Res. (2003) 61:19–30. doi: 10.1016/S0920-9964(02)00440-1
29. Tso IF, Taylor SF, Grove TB, Niendam T, Adelsheim S, Auther A, et al. Factor analysis of the S cale of P rodromal S ymptoms: data from the E arly D etection and I ntervention for the P revention of P sychosis P rogram. Early Interv Psychiatry. (2017) 11:14–22. doi: 10.1111/eip.12209
30. Poe S-L, Brucato G, Bruno N, Arndt LY, Ben-David S, Gill KE, et al. Sleep disturbances in individuals at clinical high risk for psychosis. Psychiatry Res. (2017) 249:240–3. doi: 10.1016/j.psychres.2016.12.029
31. Goines KB, LoPilato AM, Addington J, Bearden CE, Cadenhead KS, Cannon TD, et al. Sleep problems and attenuated psychotic symptoms in youth at clinical high-risk for psychosis. Psychiatry Res. (2019) 282:112492. doi: 10.1016/j.psychres.2019.112492
32. Zanini MA, Castro J, Cunha GR, Asevedo E, Pan PM, Bittencourt L, et al. Abnormalities in sleep patterns in individuals at risk for psychosis and bipolar disorder. Schizophr Res. (2015) 169:262–7. doi: 10.1016/j.schres.2015.08.023
33. Castro J, Zanini M, Gonçalves BdSB, Coelho FMS, Bressan R, Bittencourt L, et al. Circadian rest–activity rhythm in individuals at risk for psychosis and bipolar disorder. Schizophr Res. (2015) 168:50–5. doi: 10.1016/j.schres.2015.07.024
34. Lederman O, Rosenbaum S, Maloney C, Curtis J, Ward PB. Modifiable cardiometabolic risk factors in youth with at-risk mental states: a cross-sectional pilot study. Psychiatry Res. (2017) 257:424–30. doi: 10.1016/j.psychres.2017.08.034
35. Lunsford-Avery JR, LeBourgeois MK, Gupta T, Mittal VA. Actigraphic-measured sleep disturbance predicts increased positive symptoms in adolescents at ultra high-risk for psychosis: a longitudinal study. Schizophr Res. (2015) 164:15–20. doi: 10.1016/j.schres.2015.03.013
36. Michels F, Schilling C, Rausch F, Eifler S, Zink M, Meyer-Lindenberg A, et al. Nightmare frequency in schizophrenic patients, healthy relatives of schizophrenic patients, patients at high risk states for psychosis, healthy controls. Int J Dream Res. (2014) 7:9–13.
37. Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. (1976) 4:97–110. doi: 10.1037/t02254-000
38. Lunsford-Avery JR, Gonçalves BdSB, Brietzke E, Bressan RA, Gadelha A, Auerbach RP, et al. Adolescents at clinical-high risk for psychosis: circadian rhythm disturbances predict worsened prognosis at 1-year follow-up. Schizophr Res. (2017) 189:37–42. doi: 10.1016/j.schres.2017.01.051
39. Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. (2010) 67:241–51. doi: 10.1001/archgenpsychiatry.2009.206
40. Lindgren M, Manninen M, Kalska H, Mustonen U, Laajasalo T, Moilanen K, et al. Suicidality, self-harm and psychotic-like symptoms in a general adolescent psychiatric sample. Early Interv Psychiatry. (2017) 11:113–22. doi: 10.1111/eip.12218
41. Lunsford-Avery JR, Dean DJ, Mittal VA. Self-reported sleep disturbances associated with procedural learning impairment in adolescents at ultra-high risk for psychosis. Schizophr Res. (2017) 190:160–3. doi: 10.1016/j.schres.2017.03.025
42. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
43. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. (2000) 48:555–60. doi: 10.1016/S0022-3999(00)00095-7
44. Freeman D, Waite F, Startup H, Myers E, Lister R, McInerney J, et al. Efficacy of cognitive behavioural therapy for sleep improvement in patients with persistent delusions and hallucinations (BEST): a prospective, assessor-blind, randomised controlled pilot trial. Lancet Psychiatry. (2015) 2:975–83. doi: 10.1016/S2215-0366(15)00314-4
45. Freeman D, Pugh K, Vorontsova N, Southgate L. Insomnia and paranoia. Schizophr Res. (2009) 108:280–4. doi: 10.1016/j.schres.2008.12.001
46. Klingaman EA, Palmer-Bacon J, Bennett ME, Rowland LM. Sleep disorders among people with schizophrenia: emerging research. Curr Psychiatry Rep. (2015) 17:1–8. doi: 10.1007/s11920-015-0616-7
47. Mulligan LD, Haddock G, Emsley R, Neil ST, Kyle SD. High resolution examination of the role of sleep disturbance in predicting functioning and psychotic symptoms in schizophrenia: a novel experience sampling study. J Abnormal Psychol. (2016) 125:788. doi: 10.1037/abn0000180
48. Zanini M, Castro J, Coelho FM, Bittencourt L, Bressan RA, Tufik S, et al. Do sleep abnormalities and misaligned sleep/circadian rhythm patterns represent early clinical characteristics for developing psychosis in high risk populations? Neurosci Biobehav Rev. (2013) 37:2631–7. doi: 10.1016/j.neubiorev.2013.08.012
49. Reeve S, Sheaves B, Freeman D. The role of sleep dysfunction in the occurrence of delusions and hallucinations: a systematic review. Clin Psychol Rev. (2015) 42:96–115. doi: 10.1016/j.cpr.2015.09.001
50. Reeve S, Nickless A, Sheaves B, Hodgekins J, Stewart S, Gumley A, et al. Sleep duration and psychotic experiences in patients at risk of psychosis: a secondary analysis of the EDIE-2 trial. Schizophr Res. (2019) 204:326–33. doi: 10.1016/j.schres.2018.08.006
51. Waters F, Chiu V, Atkinson A, Blom JD. Severe sleep deprivation causes hallucinations and a gradual progression toward psychosis with increasing time awake. Front Psychiatry. (2018) 9:303. doi: 10.3389/fpsyt.2018.00303
52. Schlosser DA, Jacobson S, Chen Q, Sugar CA, Niendam TA, Li G, et al. Recovery from an at-risk state: clinical and functional outcomes of putatively prodromal youth who do not develop psychosis. Schizophr Bull. (2012) 38:1225–33. doi: 10.1093/schbul/sbr098
53. Addington J, Cornblatt BA, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, et al. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. (2011) 168:800–5. doi: 10.1176/appi.ajp.2011.10081191
54. Anderson KN, Bradley AJ. Sleep disturbance in mental health problems and neurodegenerative disease. Nat Sci Sleep. (2013) 5:61. doi: 10.2147/NSS.S34842
55. Dondé C, Laprévote V, Lavallé L, Haesebaert F, Fakra E, Brunelin J. Cognitive insight in individuals with an at-risk mental state for psychosis: a meta-analysis. Early Interv Psychiatry. (2021) 15:449–56. doi: 10.1111/eip.12993
56. Carrión RE, McLaughlin D, Goldberg TE, Auther AM, Olsen RH, Olvet DM, et al. Prediction of functional outcome in individuals at clinical high risk for psychosis. JAMA Psychiatry. (2013) 70:1133–42. doi: 10.1001/jamapsychiatry.2013.1909
57. Cosgrave J, Haines R, van Heugten-van der Kloet D, Purple R, Porcheret K, Foster R, et al. The interaction between subclinical psychotic experiences, insomnia and objective measures of sleep. Schizophr Res. (2018) 193:204–8. doi: 10.1016/j.schres.2017.06.058
58. Reeve S, Sheaves B, Freeman D. Sleep disorders in early psychosis: incidence, severity, and association with clinical symptoms. Schizophr Bull. (2019) 45:287–95. doi: 10.1093/schbul/sby129
59. Laskemoen JF, Simonsen C, Büchmann C, Barrett EA, Bjella T, Lagerberg TV, et al. Sleep disturbances in schizophrenia spectrum and bipolar disorders–a transdiagnostic perspective. Compreh Psychiatry. (2019) 91:6–12. doi: 10.1016/j.comppsych.2019.02.006
60. Fusar-Poli P, Rutigliano G, Stahl D, Davies C, De Micheli A, Ramella-Cravaro V, et al. Long-term validity of the At Risk Mental State (ARMS) for predicting psychotic and non-psychotic mental disorders. Eur Psychiatry. (2017) 42:49–54. doi: 10.1016/j.eurpsy.2016.11.010
61. Piras S, Casu G, Casu MA, Orrù A, Ruiu S, Pilleri A, et al. Prediction and prevention of the first psychotic episode: new directions and opportunities. Ther Clin Risk Manag. (2014) 10:241–53. doi: 10.2147/TCRM.S55770
62. Reeve S, Bell V. Sleep disorders predict the 1-year onset, persistence, but not remission of psychotic experiences in preadolescence: a longitudinal analysis of the ABCD cohort data. Eur Child Adolesc Psychiatry. (2022) 1–11. doi: 10.1007/s00787-022-01966-z
63. Hennig T, Schlier B, Lincoln TM. Sleep and psychotic symptoms: an actigraphy and diary study with young adults with low and elevated psychosis proneness. Schizophr Res. (2020) 221:12–9. doi: 10.1016/j.schres.2019.09.012
64. Lunsford-Avery JR, Mittal VA. Sleep dysfunction prior to the onset of schizophrenia: a review and neurodevelopmental diathesis–stress conceptualization. Clin Psychol Sci Pract. (2013) 20:291. doi: 10.1111/cpsp.12041
65. Schwartz MD, Kilduff TS. The neurobiology of sleep and wakefulness. Psychiatr Clin. (2015) 38:615–44. doi: 10.1016/j.psc.2015.07.002
66. Shepherd AM, Laurens KR, Matheson SL, Carr VJ, Green MJ. Systematic meta-review and quality assessment of the structural brain alterations in schizophrenia. Neurosci Biobehav Rev. (2012) 36:1342–56. doi: 10.1016/j.neubiorev.2011.12.015
67. van Erp TG, Hibar DP, Rasmussen JM, Glahn DC, Pearlson GD, Andreassen OA, et al. Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol Psychiatry. (2016) 21:547–53. doi: 10.1038/mp.2015.63
68. Dietsche B, Kircher T, Falkenberg I. Structural brain changes in schizophrenia at different stages of the illness: a selective review of longitudinal magnetic resonance imaging studies. Austral New Zeal J Psychiatry. (2017) 51:500–8. doi: 10.1177/0004867417699473
69. Steullet P. Thalamus-related anomalies as candidate mechanism-based biomarkers for psychosis. Schizophr Res. (2020) 226:147–57. doi: 10.1016/j.schres.2019.05.027
70. Feinberg I. Schizophrenia: caused by a fault in programmed synaptic elimination during adolescence? J Psychiatr Res. (1982) 17:319–34. doi: 10.1016/0022-3956(82)90038-3
71. Waters F, Blom JD, Dang-Vu TT, Cheyne AJ, Alderson-Day B, Woodruff P, et al. What is the link between hallucinations, dreams, and hypnagogic-hypnopompic experiences? Schizophr Bull. (2016) 42:1098–109. doi: 10.1093/schbul/sbw076
72. Reeve S, Emsley R, Sheaves B, Freeman D. Disrupting sleep: the effects of sleep loss on psychotic experiences tested in an experimental study with mediation analysis. Schizophr Bull. (2018) 44:662–71. doi: 10.1093/schbul/sbx103
73. Reeve S, Nickless A, Sheaves B, Freeman D. Insomnia, negative affect, and psychotic experiences: modelling pathways over time in a clinical observational study. Psychiatry Res. (2018) 269:673–80. doi: 10.1016/j.psychres.2018.08.090
74. Freeman D, Stahl D, McManus S, Meltzer H, Brugha T, Wiles N, Bebbington P. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1195–203. doi: 10.1007/s00127-011-0433-1
75. Cullen AE, Fisher HL, Gullet N, Fraser ER, Roberts RE, Zahid U, et al. Cortisol levels in childhood associated with emergence of attenuated psychotic symptoms in early adulthood. Biol Psychiatry. (2022) 91:226–35. doi: 10.1016/j.biopsych.2021.08.009
76. Kater MJ, Werner A, Schlarb AA, Lohaus A. Stress reactivity in salivary cortisol and electrocardiogram in adolescents: investigating sleep disturbances and insomnia. J Sleep Res. (2022) e13591. doi: 10.1111/jsr.13591
77. Karanikas E, Manganaris S, Ntouros E, Floros G, Antoniadis D, Garyfallos G. Cytokines, cortisol and IGF-1 in first episode psychosis and ultra high risk males. Evidence for TNF-α, IFN-γ, TNF-β, IL-4 deviation. Asian J Psychiatry. (2017) 26:99–103. doi: 10.1016/j.ajp.2017.01.026
78. Pérez de Heredia F, Garaulet M, Gómez-Martínez S, Díaz LE, Wärnberg J, Androutsos O, et al. Self-reported sleep duration, white blood cell counts and cytokine profiles in European adolescents: the HELENA study. Sleep Med. (2014) 15:1251–8. doi: 10.1016/j.sleep.2014.04.010
79. Waite F, Sheaves B, Isham L, Reeve S, Freeman D. Sleep and schizophrenia: from epiphenomenon to treatable causal target. Schizophr Res. (2020) 221:44–56. doi: 10.1016/j.schres.2019.11.014
80. Freeman D, Sheaves B, Goodwin GM, Yu L-M, Nickless A, Harrison PJ, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. (2017) 4:749–58. doi: 10.1016/S2215-0366(17)30328-0
81. Edition F. Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc. (2013) 21:591–643.
82. Bradley J, Freeman D, Chadwick E, Harvey AG, Mullins B, Johns L, et al. Treating sleep problems in young people at ultra-high risk of psychosis: a feasibility case series. Behav Cogn Psychother. (2018) 46:276–91. doi: 10.1017/S1352465817000601
83. Keshavan MS, Diwadkar VA, Montrose DM, Stanley JA, Pettegrew JW. Premorbid characterization in schizophrenia: the Pittsburgh high risk study. World Psychiatry. (2004) 3:163.
84. O'Sullivan M, Rahim M, Hall C. The prevalence and management of poor sleep quality in a secondary care mental health population. J Clin Sleep Med. (2015) 11:111–6. doi: 10.5664/jcsm.4452
85. Rehman A, Waite F, Sheaves B, Biello S, Freeman D, Gumley A. Clinician perceptions of sleep problems, their treatment. in patients with non-affective psychosis. Psychosis. (2017) 9:129–39. doi: 10.1080/17522439.2016.1206955
86. Griffiths C, Hina F, Pollard L, Jugon S, Sam M, Kelbrick M. A qualitative study of Early Intervention Psychosis (EIP) service patient's experience of sleep, exercise, sleep hygiene advice and fitbit wearable activity and sleep tracker. Open J Psychiatry. (2021) 11:91–106. doi: 10.4236/ojpsych.2021.112009
87. Myers E, Startup H, Freeman D. Cognitive behavioural treatment of insomnia in individuals with persistent persecutory delusions: a pilot trial. J Behav Ther Exp Psychiatry. (2011) 42:330–6. doi: 10.1016/j.jbtep.2011.02.004
88. Henry AL, Miller CB, Emsley R, Sheaves B, Freeman D, Luik AI, et al. Insomnia as a mediating therapeutic target for depressive symptoms: a sub-analysis of participant data from two large randomized controlled trials of a digital sleep intervention. J Sleep Res. (2021) 30:e13140. doi: 10.1111/jsr.13140
89. Waite F, Kabir T, Johns L, Mollison J, Tsiachristas A, Petit A, et al. Treating sleep problems in young people at ultra-high-risk of psychosis: study protocol for a single-blind parallel group randomised controlled feasibility trial (SleepWell). BMJ Open. (2020) 10:e045235. doi: 10.1136/bmjopen-2020-045235
Keywords: sleep, UHR, at-risk mental state, psychosis, early intervention
Citation: Fekih-Romdhane F, Hallit S, Cheour M and Jahrami H (2022) The nature, consequences, mechanisms, and management of sleep disturbances in individuals at-risk for psychosis. Front. Psychiatry 13:1011963. doi: 10.3389/fpsyt.2022.1011963
Received: 04 August 2022; Accepted: 05 September 2022;
Published: 20 September 2022.
Edited by:
Sunao Uchida, Waseda University, JapanReviewed by:
Genichi Sugihara, Tokyo Medical and Dental University, JapanCopyright © 2022 Fekih-Romdhane, Hallit, Cheour and Jahrami. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feten Fekih-Romdhane, ZmV0ZW4uZmVraWhAZ21haWwuY29t; Haitham Jahrami, aGphaHJhbWlAaGVhbHRoLmdvdi5iaA==
 Feten Fekih-Romdhane
Feten Fekih-Romdhane Souheil Hallit
Souheil Hallit Majda Cheour1,2
Majda Cheour1,2 Haitham Jahrami
Haitham Jahrami