
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry, 20 October 2022
Sec. Schizophrenia
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1005373
This article is part of the Research TopicTreatment Resistance in Psychotic DisordersView all 7 articles
Objective: This study surveyed clinicians in psychiatry in Hong Kong and Singapore to understand their familiarity and prescribing practices in treatment-resistant schizophrenia (TRS) and clozapine-resistant schizophrenia (CRS).
Materials and methods: All clinicians in psychiatry in both regions were invited through email to participate in an anonymous online survey. The survey collected information on the participants’ characteristics, their familiarity and experience with clozapine use, and their treatment practices in TRS and CRS. Data collection took place between September 2019 and February 2020 in Hong Kong and December 2018 and March 2019 in Singapore.
Results: 261 clinicians responded to the survey, with response rates of 19% (105 out of 556 participants) in Hong Kong and 50% (156 out of 309 participants) in Singapore. The majority of respondents (99.0% in Hong Kong; 87.9% in Singapore) were familiar with treatment guidelines for TRS. However, approximately half (54.2% in Hong Kong; 41.7% in Singapore) delayed the prescription of clozapine when indicated. In terms of alternatives to clozapine, approximately half or more of the clinicians in both regions would use high dose antipsychotics, long-acting injectable antipsychotics, antipsychotic polypharmacy, while the adjuvant use of mood stabilizers and electroconvulsive therapy differed between the two regions. In those with CRS, between 10 and 20% of the respondents added adjuvant mood stabilizers or antipsychotics, and 3-10% would use an antidepressant.
Conclusion: Clozapine delays occur in spite of clinicians’ familiarity with treatment guidelines. More research is needed to guide the use of augmentation strategies and the search for effective treatments beyond clozapine.
Schizophrenia afflicts close to 1% of the population (1). Approximately 15–30% of those with schizophrenia develop treatment-resistance (2–4), which is defined as the failure to respond at least two different antipsychotics of adequate dose and duration (5). Clozapine is the only antipsychotic indicated for use in treatment-resistant schizophrenia (TRS; 6). However, 40 to 70% of patients with TRS remain unwell on clozapine and develop clozapine-resistant schizophrenia (CRS; 7, 8).
The quality of life in patients with TRS was thought to be comparable to that of patients with stroke or end-stage renal failure on maintenance dialysis (9). TRS leads to a 10-fold increase in patients’ cost of hospitalizations, health resource utilization, and higher rates of serious co-morbidities (9). Patient with clozapine-resistance have even poorer clinical and functional outcomes than those with TRS (4).
In order to improve recovery outcomes, prompt and effective treatment with clozapine is needed (10). A retrospective chart review of patients with schizophrenia/schizoaffective diagnosis in Toronto, Canada, found that every one-year delay in clozapine initiation increased the odds of long-term clozapine-resistance by 6% (7). Delays in clozapine prescription was also found as a significant predictor of clozapine resistance in a 12-year follow-up study (4). A critical treatment window of 3 years from the onset of TRS was also described, after which the risk of clozapine resistance increases from 30.8 to 81.6% (11).
When clozapine fails, the navigation of treatment choices becomes a challenge due to the scarcity of robust evidence to guide clinicians’ choice beyond clozapine. Studies of clozapine augmentation strategies are often based on open-label trials and meta-analysis of trials that are of low quality (12–17). In today’s clinical practice, the treatment of clozapine-resistance is heterogeneous and determined by the clinician’s experience and the patient’s individual response to the offered intervention.
Understanding clinicians’ practice is the first step in elucidating the gaps that exist in the treatment of patients with TRS. Surveys of clinician attitude toward clozapine prescription have been conducted in various countries, including Denmark (18), India (19), Iran (20), Israel (21), Serbia (22), and the United Kingdom (UK; 23, 24). Most of these studies focused on describing the clinicians’ knowledge and attitudes toward clozapine and their perception of the barriers toward clozapine prescription. Only two of them (18, 19) have described the prescribing practices of the surveyed clinicians in detail. The current study aimed to survey clinicians in Hong Kong and Singapore to understand their practice of managing patients with treatment-resistant schizophrenia. Results from this study pertaining to the clinicians’ experience with clozapine initiation, their perceived barriers to clozapine initiation and factors that might improve clozapine use, were reported in a previous submission (25). This paper focused on understanding the clinicians’ familiarity with antipsychotic treatment guidelines for schizophrenia and explored in detail their treatment approaches in patients with TRS and CRS. Hong Kong and Singapore are both Asian city-states with high urban density that run on a mixed medical economy, where the majority of mental healthcare is delivered by the public sector (26).
An anonymous online survey was conducted among clinicians in psychiatry in Hong Kong and Singapore to understand their attitudes toward clozapine prescription. The respondents included trainees in psychiatry, resident physicians and psychiatry specialists in both regions. In Hong Kong, the survey invitations were sent through the Hong Kong College of Psychiatrists, the only professional organization for psychiatrists in Hong Kong. All trainees in psychiatry have to register with this organization prior to their specialist training. Therefore, the college has the email addresses of all practicing psychiatric trainees and specialists in Hong Kong. In Singapore, the eligible clinicians and their contact information were obtained from the Singapore Medical Council and National Psychiatry Residency Program, and crossed-checked against the email addresses of psychiatric departments in all restructured hospitals and available emails of private clinics and hospitals. At the time of the study, there were a total of 556 and 309 eligible participants, respectively, in Hong Kong and Singapore. Data collection took place between September 2019 and February 2020 in Hong Kong and December 2018 and March 2019 in Singapore.
Participants were invited via email to complete the survey on Questionpro, an online survey platform. The emails explained the purpose of the study and the anonymous and voluntary nature of study participation. Two reminder emails were sent to each participant at separate intervals to encourage their participation in the study.
The survey employed was adapted from Gee et al. (23) in their study of attitudes toward clozapine prescription in practitioners in South London and Maudsley NHS Foundation Trust (23). Participants were asked about their sociodemographic information, the proportion of patients with clozapine under their care, their familiarity with antipsychotic treatment guidelines, their prescribing practices in the treatment of those with TRS, including their threshold for prescribing clozapine as well as the alternatives to clozapine they would use, and their prescription patterns for CRS.
Ethics approval was granted by the relevant ethics review board, i.e., the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster in Hong Kong and the National Healthcare Group’s Domain Specific Review Board in Singapore.
The Statistical Package for Social Sciences (SPSS) version 23.0 was used for data analysis. Frequencies and percentages were calculated for categorical variables while mode, median and interquartile range were calculated for ordinal data. Comparisons were performed using corrected chi-square test and Mann-Whitney U test, respectively. Associations were tested using Spearman’s rank correlation. All statistically significant differences were evaluated at the 0.05 level using two-sided tests.
A total of 261 clinicians from both regions responded to the survey, giving response rates of 19% (105 out of 556 participants) in Hong Kong and 50% (156 out of 309 participants) in Singapore. Missing responses were noted in 1.3 and 0.3% of the total responses provided by the clinicians in Hong Kong and Singapore, respectively. The majority of respondents were male (59.4%), working as psychiatrists (67.4%) in both inpatient and outpatient settings (67.0%), with 6 to 11 years of experience in psychiatry (29.1%). The respondents from both regions had comparable sociodemographic characteristics, as shown in Table 1.
When asked to provide an estimate of the proportion of patients with clozapine under their care, 72.4% of respondents in Hong Kong and 53.2% of those in Singapore provided a response. Clinicians in both regions reported a median of 5.0% of patients on clozapine under their care (Hong Kong range = 0.3–40.0%, IQR = 3.0–10.0%; Singapore range = 0.0–90.0%, IQR = 1.0–10.0%).
In terms of familiarity with the antipsychotic treatment guidelines in schizophrenia, 1.0% of respondents in Hong Kong and none in Singapore were “not at all familiar” and 12.2% of respondents in Singapore and none in Hong Kong were “a little familiar” with the guidelines. A higher proportion of clinicians in Hong Kong reported being “fairly familiar” (51.4%) and “very familiar” (47.6%) with the guidelines compared to clinicians in Singapore (“fairly familiar” 63.5%, “very familiar” 24.4%; χ22,261 = 21.94, P < 0.001). The guidelines that the respondents consulted with were similar, including the NICE guidelines, local clinical guidelines and Maudsley Prescribing Guidelines in Psychiatry (in order of increasing familiarity).
Those with more years of practice in psychiatry in Singapore were more familiar with treatment guidelines for TRS (r = 0.34, P < 0.001). The same association was found in respondents in Hong Kong, but did not achieve statistical significance (r = 0.19, P = 0.053).
When asked about their threshold for clozapine initiation, 45.7% of respondents in Hong Kong and 57.7% of respondents in Singapore reported they would prescribe clozapine after the failure of two antipsychotics. One respondent from Singapore reported starting clozapine early (after one antipsychotic trial), while none of the respondents in Hong Kong would do so. The rest would delay the initiation of clozapine – after the failure of three antipsychotics in 39.0% and 31.4% of respondents in Hong Kong and Singapore, respectively, and after four or more antipsychotics in 15.2% and 10.3% of respondents in Hong Kong and Singapore, respectively.
Those who were more familiar with the treatment guidelines were less likely to delay the initiation of clozapine in both Hong Kong (r = –0.21, P = 0.03) and Singapore (r = –0.17, P = 0.03).
As an alternative to clozapine for patients with TRS (see Tables 2, 3), approximately half of the respondents in both regions would ‘often’ or ‘always’ use high dose antipsychotics (55.2% in Hong Kong, 48.1% in Singapore, χ21,261 = 1.29, P = 0.26) and long-acting injectable antipsychotics (56.2% in Hong Kong, 50.3% in Singapore, χ21,260 = 0.87, P = 0.35). More clinicians in Hong Kong (70.5%) were inclined to ‘often’ or ‘always’ prescribe antipsychotic polypharmacy compared to those in Singapore (47.7%; χ21,260 = 13.19, P < 0.001). More clinicians in Hong Kong (49.5%) were also inclined to ‘often’ or ‘always’ prescribe adjuvant mood stabilizers compared to those in Singapore (33.5%; χ21,257 = 6.60, P = 0.01). In contrast, electroconvulsive therapy (ECT) was more commonly used by Singapore clinicians (56.2%) than those in Hong Kong (24.8%; χ21,260 = 25.06, P < 0.001).
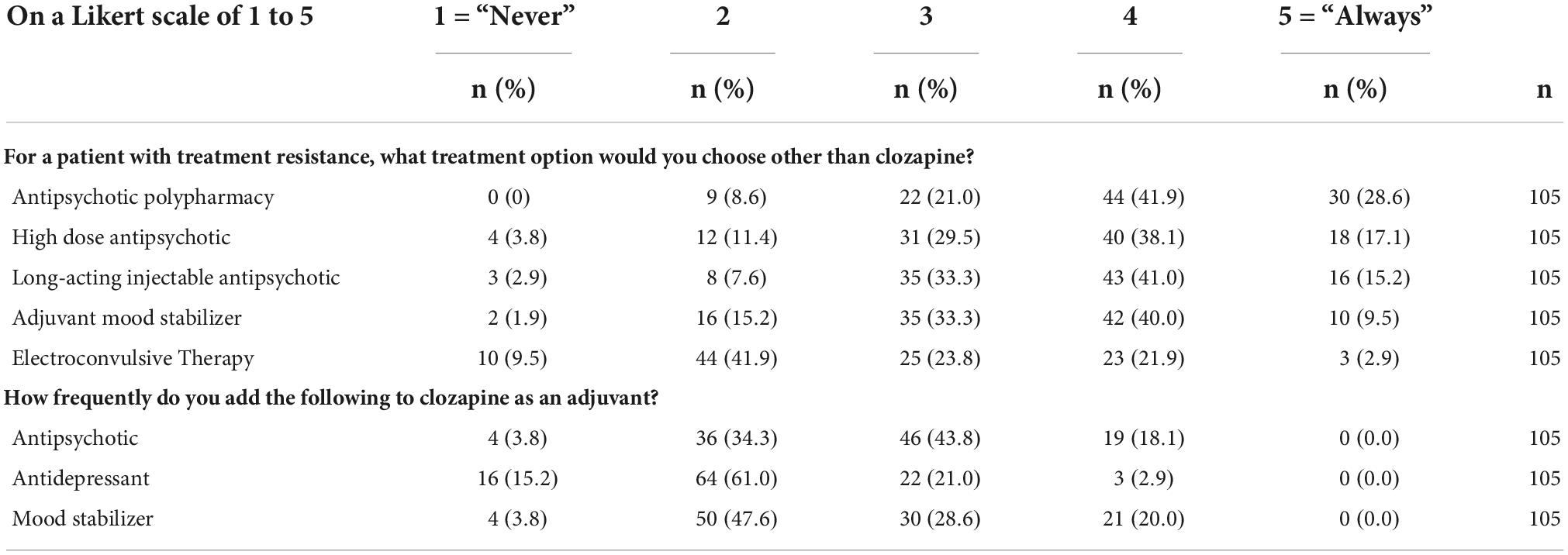
Table 2. Answers to questionnaire, shown as percentage of respondents who answered each question (Hong Kong).
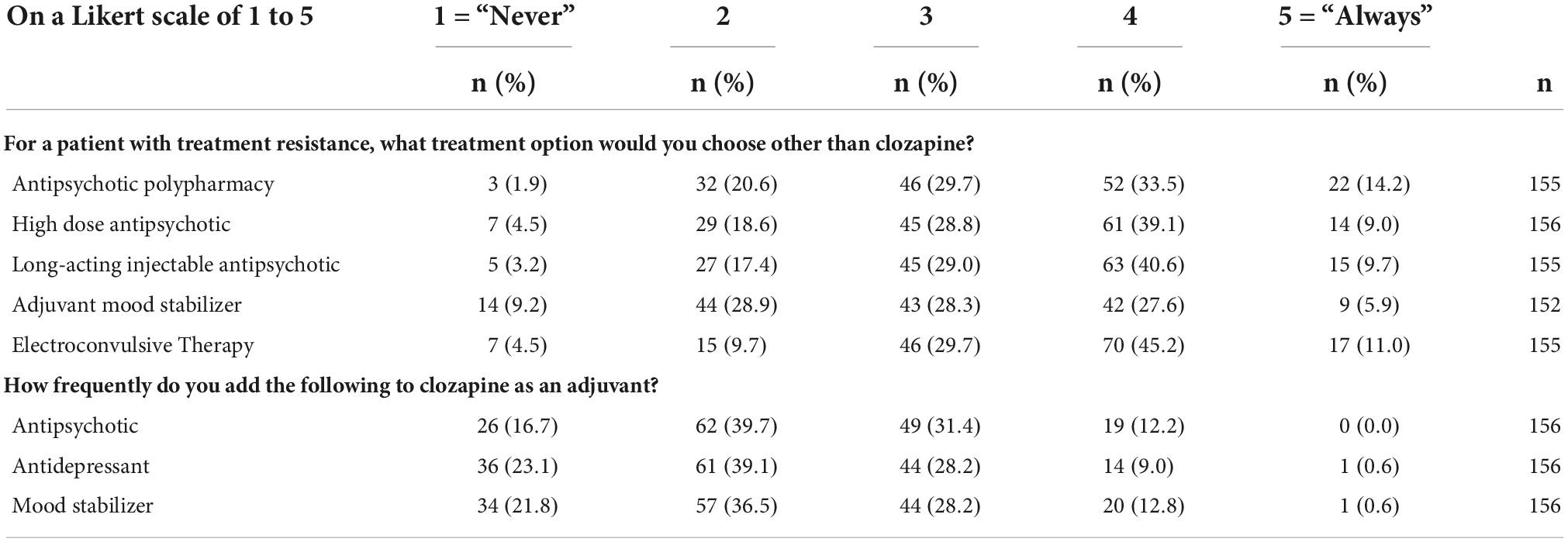
Table 3. Answers to questionnaire, shown as percentage of respondents who answered each question (Singapore).
When patients become clozapine-resistant, 20.0% of respondents in Hong Kong and 13.4% of respondents in Singapore may “often” or “always” add a mood stabilizer; 2.9% in Hong Kong and 9.6% in Singapore may “often” or “always” add an antidepressant; 18.1% in Hong Kong and 12.2% in Singapore may “often” or “always” add an antipsychotic (see Tables 2, 3). While the use of adjuvants was low in both regions, clinicians in Singapore were more inclined to add an antidepressant to augment clozapine compared to clinicians in Hong Kong (χ21,261 = 4.46, P = 0.04).
The prescribing practices of clinicians in Hong Kong and Singapore in the treatment of patients with TRS and CRS were described in this paper. The findings highlight the existence of clozapine delays in both regions in spite of clinicians’ familiarity with treatment guidelines. Clinicians in the study also have heterogeneous practices when it comes to the offering of non-clozapine alternatives to patients with TRS and their choice of treatment for CRS.
More respondents in Hong Kong (99.0%) and Singapore (87.9%) reported being “fairly” or “very” familiar with treatment guidelines compared to those in original study of practitioner attitudes toward clozapine prescription in South London and Maudsley NHS Foundation Trust (81%; 21). However, there was a longer delay to clozapine prescription by clinicians in our study. 54.2% of clinicians in Hong Kong and 41.7% of clinicians in Singapore would delay the prescription of clozapine. In contrast, close to 80% of practitioners in the London survey initiated clozapine after the failure of two antipsychotic trials as per the guidelines and only 17% of practitioners delayed clozapine initiation (23). Interestingly, the timely manner of clozapine prescription in the South London and Maudsley NHS Foundation Trust appeared to be an exception rather than the norm. The rates of clozapine delay reported in other similar surveys of clinicians’ attitude toward clozapine were closer to the findings of this study. A 2015 study in the UK by Tungaraza and Farooq (24) found that 40.5% of psychiatrists preferred to use several other antipsychotics before considering clozapine. 73% of psychiatrists in an Iranian study likewise preferred other strategies to clozapine when treatment fails with two or three antipsychotics (20). 61.3% of psychiatrists in India would use clozapine in patients who have failed 2 antipsychotics, 17.3% would prefer polypharmacy, 10% would use polypharmacy with clozapine as one of the agents (19). In Denmark, 44.9% of psychiatrists would initiate clozapine after two antipsychotics have failed while 30.6% and 18.4% would wait until three or more than three antipsychotics have failed (18). In Israel, 53.3% of respondents would initiate treatment with clozapine according to the guidelines, while 33% would delay clozapine initiation until the failure of three or more antipsychotics (21).
The delay in clozapine prescription is a common problem across various countries. The barriers to clozapine prescription are often complex and lie beyond a simple lack of knowledge. Our earlier publication (25) suggested that clinicians were deterred from prescribing clozapine due to the need for frequent blood monitoring and concerns about clozapine’s tolerability and its medical complications. Health system factors were also identified as a barrier and clinicians in Hong Kong and Singapore reported a greater need for outpatient resources in terms of clinic and administrative support to improve clozapine prescription (25). These findings were echoed by similar surveys of clinicians in other countries (18–23).
Some patients with TRS may refuse clozapine or fail to tolerate it. In such instances, alternatives to clozapine may be considered. In our study, approximately half of the clinicians in both regions supported the use of long-acting injectable antipsychotics and the use of high dose antipsychotics. The former has been recommended in instances where pseudo-resistance due to non-adherence to antipsychotics is suspected (5). The latter is less grounded in evidence; multiple guidelines have cautioned against the use of supratherapeutic doses of antipsychotics given the higher risk of side effects and little evidence of benefits (27, 28).
Augmentation strategies were commonly adopted by clinicians in both regions. Antipsychotic polypharmacy was prescribed by close to three quarters of clinicians in Hong Kong and half in Singapore, in comparison to the range of 15.9–64.7% reported in other studies (5, 18, 19). Studies that demonstrated the superiority of antipsychotic polypharmacy over antipsychotic monotherapy tended to be open-label trials and low-quality trials, with no superiority showed in double-blinded and high-quality trials (13). Nonetheless, a recent large nationwide cohort study found that those on antipsychotic polypharmacy had an approximately 10% lower relative risk of psychiatric rehospitalization than those on antipsychotic monotherapy, with some antipsychotic combinations working better than others (29).
Approximately half of the clinicians in Hong Kong and one-third in Singapore also employed the use of adjuvant mood stabilizers as an alternative to clozapine monotherapy. A meta-analysis that studied the efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia found significant effect sizes favoring the addition of mood stabilizers, such as lithium and lamotrigine (15). However, the addition of mood stabilizers was ultimately not recommended as the evidence was generally informed by small, short-term trials with poorly reported data (15, 30, 31).
Electroconvulsive therapy (ECT) as an alternative to clozapine was adopted more strongly by clinicians in Singapore than those in Hong Kong. This is in line with the common use of ECT for schizophrenia in Singapore. The Institute of Mental Health is the sole tertiary psychiatric institute in Singapore and sees the majority of patients who are severely psychotic or aggressive in the country (32). It is also the largest center for ECT in Singapore with half of all the performed ECT sessions indicated for schizophrenia (33). Overall, one-third of all ECT sessions in Singapore were indicated for schizophrenia (33). This approach is backed by moderate quality evidence that suggest that ECT augmentation to of a non-clozapine antipsychotic monotherapy is superior to antipsychotic monotherapy alone in the treatment of TRS (34–36).
In our study, only 10–20% of clinicians would opt to use combination antipsychotics or adjuvant “mood stabilizers” with clozapine. An even smaller number would consider adjuvant antidepressants. In contrast, 76.3% of psychiatrists in a survey in India would combine clozapine with another antipsychotic, with amisulpride being one of the three most preferred agents, followed by risperidone, aripiprazole and haloperidol (19). In a Danish study, when treating resistant-positive symptoms, 39.8% would increase the clozapine dose, 29.6% of respondents would add an atypical antipsychotic, 23.9% would add a conventional antipsychotic, and 4.6% would add a mood stabilizer; when negative symptoms are resistant, 9.5% would increase the clozapine dose, 77.0% would add an atypical antipsychotic, 8.1% an antidepressant and 2.6% a mood stabilizer (18).
In existing literature, the recommendations on augmentation strategies for clozapine non-response have varied across different guidelines (27). This is perhaps a reflection of the lack of robust evidence to support one strategy over the other. The TRRIP Working Group (37) offered the following recommendations on the basis of international expert consensus: Combining clozapine with an antipsychotic, specifically amisulpride or aripiprazole, was suggested for patients who have persistent positive or mixed symptoms or persistent aggression. The combination of clozapine and aripiprazole was found in the earlier-mentioned nationwide cohort study on antipsychotic polypharmacy versus monotherapy to have the best outcome in reducing the risk of rehospitalization, in comparison to clozapine monotherapy as well as other antipsychotic combinations (29). The TRRIP Working Group also recommended the use of adjuvant mood stabilizers (namely, lithium, and lamotrigine) in patients with persistent aggression and/or suicidal ideation, and adjuvant antidepressants in patients with persistent negative symptoms or suicidal ideation (37). While the use of ECT in CRS was not studied in our survey, ECT shows promise and was mentioned by the TRRIP Working Group as a possible treatment for those with persistent positive symptoms, mixed symptoms or suicidal ideation (36–38).
This is the first survey that described the insights on experience, familiarity and prescribing practices in the treatment of patients with TRS and CRS in clinicians from Hong Kong and Singapore. The response rates of 19% and 50% in Singapore in Hong Kong were comparable to the average response rates in previous survey studies from the same regions (39, 40). There was a good completion of the survey questions by the respondents, with missing responses in 1.3% and 0.3% of the total responses in Hong Kong and Singapore, respectively. The similar sociodemographic characteristics of respondents in both regions also allowed for a more meaningful comparison of the survey responses. However, the small sample size for the Hong Kong participants might have led to false negatives in some of the results. The management approach of TRS in this study was limited to the use of pharmacotherapy and ECT, and did not include the use of psychological interventions such as cognitive behavioral therapy for psychosis. Psychological interventions are gaining ground as complementary treatment in psychosis, though the evidence-base for their use remains limited and more research in this field is still needed (12, 41–43). Other limitations of this study include the possibility of recall bias and social desirability bias due to the self-reporting nature of the survey. Selection bias may also be present as the respondents were more likely to be clinicians who were experienced in the use of clozapine and those who were concerned about its underutilization.
Clozapine is the only evidence-based treatment in patients with TRS. However, its initiation across the world is often delayed and this delay in turn leads to higher incidences of clozapine-resistance and poorer outcomes for patients (4). There is a need to examine and address the factors that are preventing the timely prescription of clozapine in order to facilitate its earlier adoption. More research into the biological mechanisms that underpin treatment-resistance and clozapine-resistance in schizophrenia is needed in order to guide the search for effective treatments beyond clozapine.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by The Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster in Hong Kong and the National Healthcare Group’s Domain Specific Review Board in Singapore. The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
This research was supported by the Singapore FY18 NHG-LKCMedicine Clinician-Scientist Preparatory Program (Reference code: CSPP-18001) and the Singapore Ministry of Health’s National Medical Research Council under the Centre Grant Program (Grant No: NMRC/CG/M002/2017_IMH). The sponsor had no role in the design, analysis, interpretation, or publication of this study.
We thank the University of Hong Kong, the Hong Kong College of Psychiatrists, the Institute of Mental Health, Singapore, and all the participants from Hong Kong and Singapore for their support of this study. We thank Ms. Veronica Hei Yan Chan, M.Sc. (The University of Hong Kong, Hong Kong) for coordinating the recruitment of participants in Hong Kong, and Ms. See Yuen Mei, PgDip (Institute of Mental Health, Singapore) for coordinating the administration of this study in Singapore and managing the overall database. We also extend our gratitude to Ms. Siobhan Gee, Ph.D. (South London and the Maudsley NHS Foundation Trust, King’s College London, the United Kingdom) for sharing the survey tool. Ms. Chan, Ms. See, and Ms. Gee have no conflicts of interest to declare.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. He H, Liu Q, Li N, Guo L, Gao F, Bai L, et al. Trends in the incidence and DALYs of schizophrenia at the global, regional and national levels: results from the global burden of disease study 2017. Epidemiol Psychiatr Sci. (2019) 29:e91. doi: 10.1017/S2045796019000891
2. Agid O, Arenovich T, Sajeev G, Zipursky RB, Kapur S, Foussias G, et al. An algorithm-based approach to first-episode schizophrenia: response rates over 3 prospective antipsychotic trials with a retrospective data analysis. J Clin Psychiatry. (2011) 72:1439–44. doi: 10.4088/JCP.09m05785yel
3. Siskind D, Orr S, Sinha S, Yu O, Brijball B, Warren N, et al. Rates of treatment-resistant schizophrenia from first-episode cohorts: systematic review and meta-analysis. Br J Psychiatry. (2021) 220:1–6. doi: 10.1192/bjp.2021.61
4. Chan SKW, Chan HYV, Honer WG, Bastiampillai T, Suen YN, Yeung WS, et al. Predictors of treatment-resistant and clozapine-resistant schizophrenia: a 12-year follow-up study of first-episode schizophrenia-spectrum disorders. Schizophr Bull. (2021) 47:485–94. doi: 10.1093/schbul/sbaa145
5. Kane JM, Agid O, Baldwin ML, Howes O, Lindenmayer JP, Marder S, et al. Clinical guidance on the identification and management of treatment-resistant schizophrenia. J Clin Psychiatry. (2019) 80:18com12123. doi: 10.4088/JCP.18com12123
6. Warnez S, Alessi-Severini S. Clozapine: a review of clinical practice guidelines and prescribing trends. BMC Psychiatry. (2014) 14:102. doi: 10.1186/1471-244X-14-102
7. Shah P, Iwata Y, Brown EE, Kim J, Sanches M, Takeuchi H, et al. Clozapine response trajectories and predictors of non-response in treatment-resistant schizophrenia: a chart review study. Eur Arch Psychiatry Clin Neurosci. (2020) 270:11–22. doi: 10.1007/s00406-019-01053-6
8. Siskind D, Siskind V, Kisely S. Clozapine response rates among people with treatment-resistant schizophrenia: data from a systematic review and meta-analysis. Can J Psychiatry. (2017) 62:772–7. doi: 10.1177/0706743717718167
9. Kennedy JL, Altar CA, Taylor DL, Degtiar I, Hornberger JC. The social and economic burden of treatment-resistant schizophrenia: a systematic literature review. Int Clin Psychopharmacol. (2014) 29:63–76. doi: 10.1097/YIC.0b013e32836508e6
10. Shah P, Iwata Y, Plitman E, Brown EE, Caravaggio F, Kim J, et al. The impact of delay in clozapine initiation on treatment outcomes in patients with treatment-resistant schizophrenia: a systematic review. Psychiatry Res. (2018) 268:114–22. doi: 10.1016/j.psychres.2018.06.070
11. Yoshimura B, Yada Y, So R, Takaki M, Yamada N. The critical treatment window of clozapine in treatment-resistant schizophrenia: secondary analysis of an observational study. Psychiatry Res. (2017) 250:65–70. doi: 10.1016/j.psychres.2017.01.064
12. Keepers GA, Fochtmann LJ, Anzia JM, Benjamin S, Lyness JM, Mojtabai R, et al. The American psychiatric association practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. (2020) 177:868–72. doi: 10.1176/appi.ajp.2020.177901
13. Galling B, Roldán A, Hagi K, Rietschel L, Walyzada F, Zheng W, et al. Antipsychotic augmentation vs. monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry. (2017) 16:77–89. doi: 10.1002/wps.20387
14. Barber S, Olotu U, Corsi M, Cipriani A. Clozapine combined with different antipsychotic drugs for treatment-resistant schizophrenia. Cochrane Database Syst Rev. (2017) 2017:CD006324. doi: 10.1002/14651858.CD006324.pub3
15. Correll CU, Rubio JM, Inczedy-Farkas G, Birnbaum ML, Kane JM, Leucht S. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry. (2017) 74:675–84. doi: 10.1001/jamapsychiatry.2017.0624
16. Siskind DJ, Lee M, Ravindran A, Zhang Q, Ma E, Motamarri B, et al. Augmentation strategies for clozapine refractory schizophrenia: a systematic review and meta-analysis. Aust N Z J Psychiatry. (2018) 52:751–67. doi: 10.1177/0004867418772351
17. Wagner E, Löhrs L, Siskind D, Honer WG, Falkai P, Hasan A. Clozapine augmentation strategies – a systematic meta-review of available evidence. treatment options for clozapine resistance. J Psychopharmacol. (2019) 33:423–35. doi: 10.1177/0269881118822171
18. Nielsen J, Dahm M, Lublin H, Taylor D. Psychiatrists attitude towards and knowledge of clozapine treatment. J Psychopharmacol. (2010) 24:965–71. doi: 10.1177/0269881108100320
19. Grover S, Balachander S, Chakarabarti S, Avasthi A. Prescription practices and attitude of psychiatrists towards clozapine: a survey of psychiatrists from India. Asian J Psychiatr. (2015) 18:57–65. doi: 10.1016/j.ajp.2015.09.013
20. Rezaie L, Nazari A, Safari-Faramani R, Shohaimi S, Khazaie H. Iranian psychiatrists’ attitude towards clozapine use for patients with treatment-resistant schizophrenia: a nationwide survey. BMC Psychiatry. (2022) 22:534. doi: 10.1186/s12888-022-04179-5
21. Daod E, Krivoy A, Shoval G, Zubedat S, Lally J, Vadas L, et al. Psychiatrists’ attitude towards the use of clozapine in the treatment of refractory schizophrenia: a nationwide survey. Psychiatry Res. (2019) 275:155–61. doi: 10.1016/j.psychres.2019.03.029
22. Ignjatovic Ristic D, Cohen D, Ristic I. Prescription attitudes and practices regarding clozapine among Serbian psychiatrists: results of a nationwide survey. Ther Adv Psychopharmacol. (2021) 11:20451253211020236. doi: 10.1177/20451253211020235
23. Gee S, Vergunst F, Howes O, Taylor D. Practitioner attitudes to clozapine initiation. Acta Psychiatr Scand. (2014) 130:16–24. doi: 10.1111/acps.12193
24. Tungaraza TE, Farooq S. Clozapine prescribing in the UK: views and experience of consultant psychiatrists. Ther Adv Psychopharmacol. (2015) 5:88–96. doi: 10.1177/2045125314566808
25. Zheng S, Lee J, Chan SKW. Utility and barriers to clozapine use: a joint study of clinicians’ attitudes from Singapore and Hong Kong. J Clin Psychiatry. (2022) 83:21m14231. doi: 10.4088/JCP.21m14231
26. Cheung EFC, Lam LCW, Hung S. Mental health in Hong Kong: transition from hospital-based service to personalised care. Int Psychiatry. (2010) 7:62–4. doi: 10.1192/s1749367600005865
27. Shimomura Y, Kikuchi Y, Suzuki T, Uchida H, Mimura M, Takeuchi H. Antipsychotic treatment strategies for acute phase and treatment resistance in schizophrenia: a systematic review of the guidelines and algorithms. Schizophr Res. (2021) 236:142–55. doi: 10.1016/j.schres.2021.07.040
28. Dold M, Fugger G, Aigner M, Lanzenberger R, Kasper S. Dose escalation of antipsychotic drugs in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Res. (2015) 166:187–93. doi: 10.1016/j.schres.2015.04.024
29. Tiihonen J, Taipale H, Mehtälä J, Vattulainen P, Correll CU, Tanskanen A. Association of antipsychotic polypharmacy vs monotherapy with psychiatric rehospitalization among adults with schizophrenia. JAMA Psychiatry. (2019) 76:499–507. doi: 10.1001/jamapsychiatry.2018.4320
30. Leucht S, Helfer B, Dold M, Kissling W, Mcgrath JJ. Lithium for schizophrenia. Cochrane Database Syst Rev. (2015) 2015:CD003834. doi: 10.1002/14651858.CD003834.pub3
31. Premkumar TS, Pick J. Lamotrigine for schizophrenia. Cochrane Database Syst Rev. (2006) 4:CD005962. doi: 10.1002/14651858.CD005962.pub2
32. Ho CSH, Ho RCM, Mahendran R. The evolving mental health landscape in Singapore. Adv Psychiatr Treat. (2014) 20:293–4. doi: 10.1192/apt.bp.113.011445
33. Tor PC, Gálvez V, Ang A, Fam J, Chan HN, Tan SN, et al. Electroconvulsive practice in Singapore: a cross-sectional national survey. Singapore Med J. (2019) 60:590–5. doi: 10.11622/smedj.2019064
34. Sinclair DJM, Zhao S, Qi F, Nyakyoma K, Kwong JSW, Adams CE. Electroconvulsive therapy for treatment-resistant schizophrenia. Cochrane Database Syst Rev. (2019) 3:CD011847. doi: 10.1002/14651858.CD011847.pub2
35. Zheng W, Cao XL, Ungvari GS, Xiang YQ, Guo T, Liu ZR, et al. Electroconvulsive therapy added to non-clozapine antipsychotic medication for treatment resistant schizophrenia: meta-analysis of randomized controlled trials. PLoS One. (2016) 11:e0156510. doi: 10.1371/journal.pone.0156510
36. Chan CYW, Abdin E, Seow E, Subramaniam M, Liu J, Peh CX, et al. Clinical effectiveness and speed of response of electroconvulsive therapy in treatment-resistant schizophrenia. Psychiatry Clin Neurosci. (2019) 73:416–22. doi: 10.1111/pcn.12855
37. Wagner E, Kane JM, Correll CU, Howes O, Siskind D, Honer WG, et al. Clozapine combination and augmentation strategies in patients with schizophrenia – recommendations from an international expert survey among the treatment response and resistance in psychosis (TRRIP) working group. Schizophr Bull. (2020) 46:1459–70. doi: 10.1093/schbul/sbaa060
38. Petrides G, Malur C, Braga RJ, Bailine SH, Schooler NR, Malhotra AK, et al. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: a prospective, randomized study. Am J Psychiatry. (2015) 172:52–8. doi: 10.1176/appi.ajp.2014.13060787
39. Chan CYW, Chua BY, Subramaniam M, Suen ELK, Lee J. Clinicians’ perceptions of pharmacogenomics use in psychiatry. Pharmacogenomics. (2017) 18:531–8. doi: 10.2217/pgs-2016-0164
40. Hui CLM, Wong AKH, Leung WWT, Lee EHM, Chan SKW, Chang WC, et al. Psychiatrists’ opinion towards medication discontinuation in remitted first-episode psychosis: a multi-site study of the Asian Network for Early Psychosis. Early Interv Psychiatry. (2019) 13:1329–37. doi: 10.1111/eip.12765
41. Jones C, Hacker D, Meaden A, Cormac I, Irving CB, Xia J, et al. Cognitive behavioural therapy plus standard care versus standard care plus other psychosocial treatments for people with schizophrenia. Cochrane Database Syst Rev. (2018) 2018:CD008712.
42. Jones C, Hacker D, Xia J, Meaden A, Irving CBB, Zhao S, et al. Cognitive behavioural therapy plus standard care versus standard care for people with schizophrenia. Cochrane Database Syst Rev. (2018) 2018:CD008712. doi: 10.1002/14651858.CD008712.pub3
43. Polese D, Fornaro M, Palermo M, De Luca V, De Bartolomeis A. Treatment-resistant to antipsychotics: a resistance to everything? psychotherapy in treatment-resistant schizophrenia and nonaffective psychosis: a 25-year systematic review and exploratory meta-analysis. Front Psychiatry. (2019) 10:210. doi: 10.3389/fpsyt.2019.00210
Keywords: clozapine, treatment resistance, schizophrenia, ECT, clozapine resistance
Citation: Zheng S, Chan SKW and Lee J (2022) Managing treatment resistance in schizophrenia: A joint study in Hong Kong and Singapore. Front. Psychiatry 13:1005373. doi: 10.3389/fpsyt.2022.1005373
Received: 28 July 2022; Accepted: 04 October 2022;
Published: 20 October 2022.
Edited by:
Eugenia Kravariti, King’s College London, United KingdomReviewed by:
Marcin Siwek, Jagiellonian University Medical College, PolandCopyright © 2022 Zheng, Chan and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shushan Zheng, c2h1c2hhbl96aGVuZ0BpbWguY29tLnNn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.