
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 09 September 2022
Sec. Aging Psychiatry
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.1003810
This article is part of the Research Topic Epidemiology and Clinical Researches on Neuropsychiatric Disorders in Aging View all 10 articles
Background: Primary care represents an ideal setting for screening for and managing suicidal older adults but the clinical epidemiology of suicidal ideation in Chinese older primary care patients remains unclear. This study investigated the prevalence and correlates of suicidal ideation in older Chinese adults receiving primary care.
Methods: This multicenter cross-sectional survey included a total of 769 older adults (≥65 years) from seven urban and six rural primary care clinics in Wuhan, China. The presence of depressive symptoms and suicidal ideation was assessed with the Geriatric Depression Scale and a single-item question “In the past 12 months, did you think about ending your life?,” respectively.
Results: The 12-month prevalence of suicidal ideation in older primary care patients was 16.6%. Significant correlates of suicidal ideation were poor economic status (vs. good, OR = 2.80, P = 0.008), heart disease (OR = 2.48, P = 0.005), chronic gastric ulcer (OR = 3.55, P = 0.012), arthritis (OR = 2.10, P = 0.042), and depressive symptoms (OR = 11.29, P < 0.001).
Conclusions: Suicidal ideation is common among older adults attending Chinese primary care clinics. It is necessary to integrate psychological crisis intervention into primary care to prevent late-life suicide.
Despite the declining time-trend in national elderly suicide rates in recent decades, suicide in older adults remains a significant public health concern in China because of its higher elderly suicide rate compared to most major East Asian and Western countries/regions, largest number of older adults in the world, and rapid increase of aging population (1–6). Given the complexity of late-life suicide, a multi sectoral suicide prevention strategy is needed for effective suicide prevention in older adults (7–9).
In Western countries, Hong Kong SAR, and mainland China, as high as 60–80% of the older suicide completers visited their primary care physicians (PCPs) in the preceding month before committing suicide (10–13). Given the wide availability of primary care services and the frequent contacts between PCPs and older adults, primary care represents an ideal setting for screening for and managing suicidal older adults (14–16). Accordingly, one essential component of the national strategies for suicide prevention of most countries in the world, as recommended by the World Health Organization, is to provide and maintain gatekeeper training programs to PCPs to improve their capacity to identify persons who are at-risk of suicide and refer them to mental health specialists when necessary (7).
To facilitate the timely detection, suicide risk assessment, and early initiation of the intervention of suicidal older adults in primary care settings, it is necessary to understand the clinical epidemiology of suicidal behaviors in older primary care patients. Until now, suicidal behaviors, in particular suicidal ideation, have been extensively studied in older primary care adults in Western countries (17–23). These studies assessed the presence of suicidal ideation with various instruments (i.e., suicidality subscale of the Depressive Symptom Inventory and suicidal item of the nine-item Patient Health Questionnaire) and reported a wide range of prevalence estimates (0.7–23.3%) (18, 21, 23). A variety of factors were found to be significantly associated with suicidal ideation in this population, including male sex, living alone, financial strain, family history of suicide, depressive symptoms, pain, and poor physical health (17, 18, 23).
Findings from psychological autopsy studies in both Western countries and China have reported the greater risk of suicide in older adults with physical illnesses (24, 25); for example, congestive heart failure, chronic obstructive lung disease (COPD), seizure disorder, and urinary incontinence are associated with 1.7-, 1.6-, 3.0-, and 2.0-fold increases in odds of suicide in older adults, respectively. However, one significant knowledge gap of the above studies is that few data are available regarding the risk of suicidal behaviors in older primary care patients according to physical conditions, which may help the identification of high-risk subgroups in this physically ill population. In addition, accumulating empirical evidence has shown the important role of social disconnectedness-related factors in the etiology of later-life suicide, which are potentially modifiable and include lack of close friends, living alone, feelings of loneliness, no trusted friends, insufficient number family relatives, and inadequate social support (12, 26–30). Nevertheless, few prior studies have examined the contributions of these factors to suicidal behaviors in older primary care patients.
Although suicidal ideation is less prevalent in old age-group than younger age-groups, older adults, once they have suicidal thoughts, are more likely to commit suicide with greater suicidal intention and by using more immediately lethal means (1, 31–34). These data suggest that screening for suicidal ideation is the first essential step toward effective prevention of late-life suicide. However, to the best of our knowledge, few studies have investigated the clinical epidemiology of suicidal ideation in older adults undergoing primary care services in China. This study filled the above-mentioned knowledge gaps by investigating the prevalence of suicidal ideation and its associated factors in older primary care patients in Wuhan, the largest city in Hubei province and the most populous city in Central China (35). Factors to be examined included major medical conditions and some social disconnectedness-related factors.
Subjects were 791 older adults who were consecutively recruited from 13 district-center public primary care clinics (seven urban and six rural) in Wuhan, 65 years old or over, receiving outpatient treatment at these selected clinics during the survey period from October 2015 to November 2016, and voluntary to participate in this study. Details of the sampling and subject inclusion have been described elsewhere (14, 36–38). Wuhan has 13 districts: seven urban and six rural. Considering the geographic representativeness of the study sample, we purposively selected one primary care clinic from each district, which was located in or nearest to the center of the most populous area of the district.
Prior to the formal study, the survey protocol was approved by the Institutional Review Board of Wuhan Mental Health Center (approval number: WMHC-IRB-S065). All subjects and their guardians (if necessary) provided informed consent before the interview.
Trained PCPs collected the questionnaire data via face-to-face interviews with the older primary care patients. Demographic factors in the questionnaire included sex, age, educational attainment, marital status, self-rated economic status (good, fair, poor), main occupation engaged in before the older adulthood (physical vs. mental), and current residence place (urban vs. rural).
Lifestyle factors included currently smoking and the habit of regular physical activity (36). We used a checklist to assess the presence of 11 major medical conditions and two sensory impairments: hypertension, diabetes, heart diseases, stroke and other cerebrovascular diseases, COPD, tuberculosis, chronic gastric ulcer, Parkinson's disease, anemia, hepatitis cirrhosis, arthritis, hearing impairment, and vision impairment. Hearing impairment was present if the interviewer must speak more loudly than normal to let the patients know what the interviewer was saying, while vision impairment was present if the patient endorsed having difficulties in watching movies or TV shows (32, 36).
Social disconnectedness-related factors included number of living adult children, the status of living alone, feelings of loneliness, self-rated relationship with family members (good, fair, poor), and self-rated relationship with non-family associates (good, fair, poor). A single-item question was used to assess feelings of loneliness: “How often do you feel lonely?” with five response options: always, often, sometimes, seldom, and never. Respondents who reported felt lonely at least sometimes were those having feelings of loneliness (38).
Depressive symptoms were evaluated with validated Chinese version of the Geriatric Depression Scale with a total score of five or greater denoting clinically significant depressive symptoms (37, 39). One-year suicidal ideation was assessed with a single question “In the past 12 months, did you think about ending your life?”(40).
Prevalence of suicidal ideation was calculated. Chi-square test was used to compare rates of suicidal ideation between/across subgroups according to demographic and other characteristics. Unconditional binary logistic regression was used to identify correlates of suicidal ideation, which included all significant factors from the Chi-square test as the independent variables and employed backward elimination to select the final set of correlates. Associations between correlates and suicidal ideation were measured by using Odds Ratios (ORs) and their 95% confidence intervals (95% CIs). SPSS software, version 16.0, was used for analyzing the data. A two-sided P < 0.05 was defined as statistically significant.
In total, 791 older primary care adults were invited to join the study and 769 completed the survey questionnaire. Reasons for non-completion of the survey included: refusal to join in the survey (n = 10), very severe cognitive impairment (n = 5), the withdrawal of informed consent (n = 6), and missing data on variables of interest (n = 1). The average age of the study sample was 72.9 years (standard deviation = 6.1, range = 65–97) and 414 (53.8%) were women. Table 1 displays the characteristics of the survey sample and prevalence rates of suicidal ideation by sample characteristics.
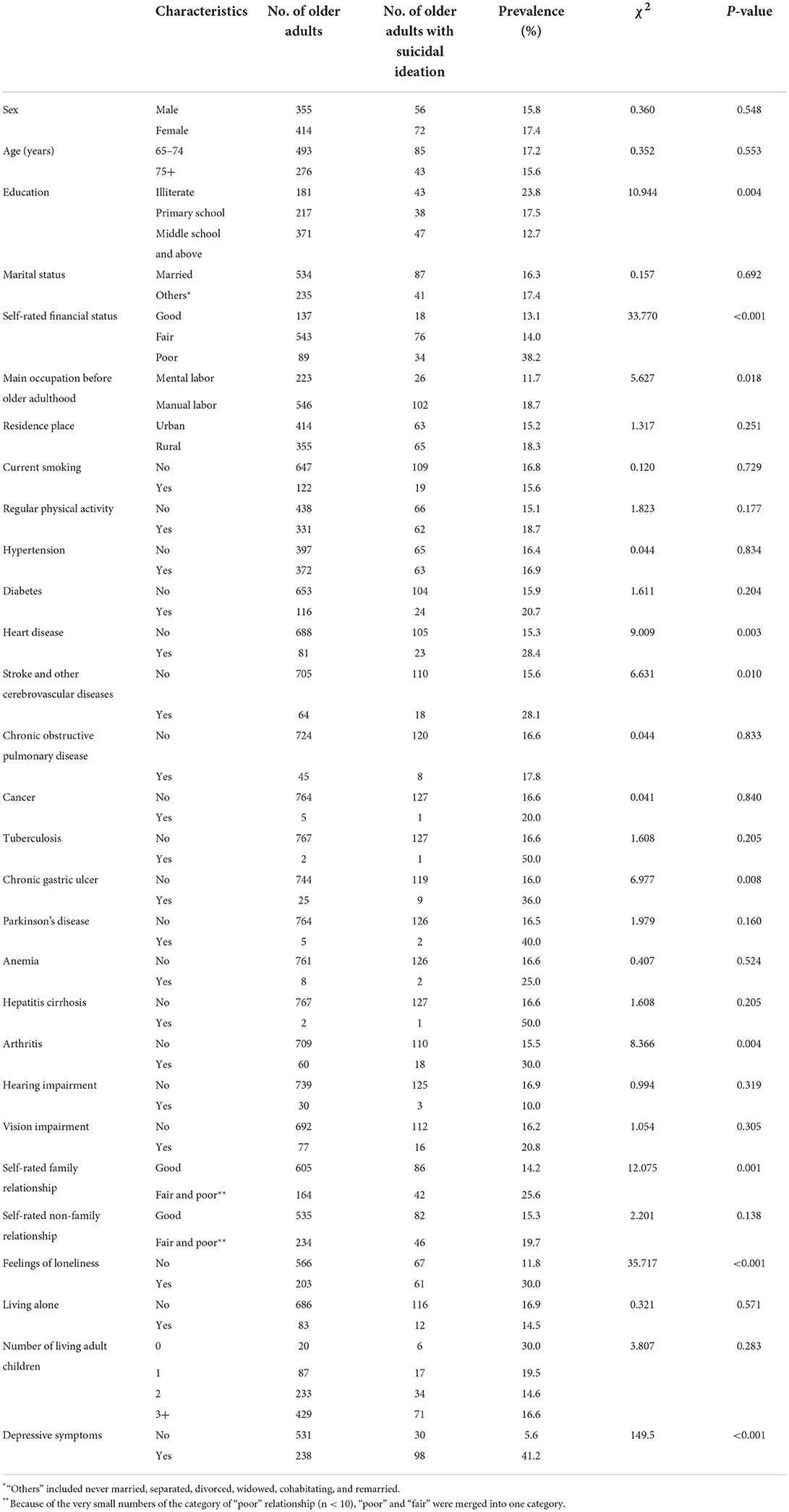
Table 1. Characteristics of the sample of older primary care patients and prevalence rates of suicidal ideation by sample characteristics.
Altogether, 128 older adults endorsed suicidal ideation during the past year and the corresponding 1-year prevalence of suicidal ideation was 16.6%.
Results from Chi-square test (Table 1) show that significantly higher rates of suicidal ideation were observed in illiterate respondents (vs. middle school and above), in respondents with poor economic status (vs. good), in respondents who engaged in physical labor (vs. mental labor) before the older adulthood, in respondents suffering heart disease (vs. no), in respondents suffering stroke and other cerebrovascular diseases (vs. no), in respondents suffering chronic gastric ulcer (vs. no), in respondents suffering arthritis (vs. no), in respondents with fair and poor family relationship (vs. good), in respondents having feelings of loneliness (vs. no), and in respondents having depressive symptoms (vs. no).
Multiple logistic regression analysis identified five factors significantly associated with suicidal ideation in older primary care patients (Table 2): poor economic status (vs. good, OR = 2.80, P = 0.008), heart disease (OR = 2.48, P = 0.005), chronic gastric ulcer (OR = 3.55, P = 0.012), arthritis (OR = 2.10, P = 0.042), and depressive symptoms (OR = 11.29, P < 0.001).
Given the limited mental health service and crisis intervention resources in China, empirical data on the clinical epidemiology of suicidal ideation in older primary care patients would inform the development of late-life suicide prevention programs in Chinese primary care settings. To the best of our knowledge, this is the first study in China that examined the prevalence and correlates of suicidal ideation among older Chinese adults receiving primary care. The main findings of this study are the 16.6% prevalence of 1-year suicidal ideation and its significant associations with poor economic status, heart disease, chronic gastric ulcer, arthritis, and depressive symptoms.
Compared to the 2.6 and 5.7% prevalence of 1-year suicidal ideation in urban and rural community-residing older Chinese adults, respectively (41, 42), our study found a much higher prevalence of suicidal ideation in older primary care adults in China. The high risk of suicidal ideation in older Chinese adults attending primary care clinics should be primarily due to their prevailing physical health problems, because poor physical health has been associated with poor mental health, i.e., acute stress caused by the fracture and post-stroke depression, which in turn results in the elevated risk of suicidal behaviors (1, 14, 24, 25). Further, there is evidence that the treatment rate of major depression in older adults receiving primary care in China is extremely low, <1% (43). Therefore, the much higher prevalence of suicidal ideation might be the result of untreated late-life depression in primary care settings in China.
In line with earlier studies (17, 18, 23, 40, 44), we confirmed significant associations between poor financial status, depressive symptoms, and suicidal ideation in Chinese older primary care patients. Nevertheless, this study did not find significant associations of suicidal ideation with disconnectedness-related factors in the final step of multiple logistic regression model despite significant associations between fair and poor family relationship and feelings of loneliness and suicidal ideation in the Chi-square test. We speculate that this does not indicate that disconnectedness-related factors did not contribute to suicidal ideation; rather, the effects of these factors may be relative weak and be masked by the prevailing physical health problems of this population.
The elevated risk of suicidal ideation in individuals with heart disease, peptic ulcers, and arthritis in the general population has been previously reported (45–47). Because depression can be viewed as an antecedent for suicidal ideation and these chronic diseases have been associated with depression (45, 48, 49), our findings on the three major medical conditions as significant correlates of suicidal ideation are expected. Nevertheless, it seems that depression is not the only bridge that links major medical conditions and suicidal ideation together because both depressive symptoms and major medical conditions were significant and independent correlates in the final regression model. We speculated that major medical conditions might increase the risk of suicidal ideation via other pathways such as pain and psychological distress.
The main limitation of this study is the methodology of cross-sectional survey, which cannot ascertain the causality between identified correlates and suicidal ideation. The second limitation is no assessment of the mental health-help seeking behaviors of suicidal older adults, which is essential for the planning of crisis intervention in primary care settings in China. Third, some modifiable factors that are potentially associated with suicidal ideation in older adults such as pain and social support were not measured in this study.
In summary, in Chinese primary care settings, suicidal ideation is common among older patients. Given the potentially high risk of suicide in suicidal older adults, it is necessary to integrate psychological crisis intervention into primary care to prevent late-life suicide. Services in primary care settings in China should include routinely screening for older adults at-risk of suicide, suicide risk assessment, psychosocial support, antidepressant treatment, and referral to mental health specialists when necessary. In addition, the elevated risk of suicidal ideation in older adults with several major medical conditions suggests that effective management of major medical conditions should be considered as a component of the late-life suicide prevention strategy in primary care settings.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Review Board of Wuhan Mental Health Center (approval number WMHC-IRB-S065). The patients/participants provided their written informed consent to participate in this study.
X-MZ acquisition and analysis of data for the study, drafting the paper, and interpretation of data for the study. Y-MX and Z-QW design and acquisition of data for the study. X-MZ and B-LZ drafting the paper, revising the paper for important intellectual content, and interpretation of data for the study. All authors contributed to the article and approved the submitted version.
This work was supported by National Natural Science Foundation of China (grant number: 71774060), 2015 Irma and Paul Milstein Program for Senior Health Awards from the Milstein Medical Asian American Partnership Foundation, Wuhan Health and Family Planning Commission (grant numbers: WX17Q30, WG16A02, and WG14C24), and Suzhou Medical Talents Program from Suzhou Health Commission (grant number: GSWS2021052).
The authors thank all the research staff for their team collaboration work and all the older adults and primary healthcare physicians involved in this study for their co-operation and support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liang YJ, Deng F, Liang P, Zhong BL. Suicidal ideation and mental health help-seeking behaviors among older Chinese adults during the COVID-19 pandemic. J Geriatr Psychiatry Neurol. (2022) 35:245–51. doi: 10.1177/08919887221078568
2. Hua R, Ma Y, Li C, Zhong B, Xie W. Low levels of low-density lipoprotein cholesterol and cognitive decline. Sci Bull. (2021) 66:1684–90. doi: 10.1016/j.scib.2021.02.018
3. Zhong BL, Chen SL, Tu X, Conwell Y. Loneliness and cognitive function in older adults: findings from the Chinese longitudinal healthy longevity survey. J Gerontol B Psychol Sci Soc Sci. (2017) 72:120–8. doi: 10.1093/geronb/gbw037
4. Zhong BL, Chiu HF, Conwell Y. Rates and characteristics of elderly suicide in China, 2013–14. J Affect Disord. (2016) 206:273–9. doi: 10.1016/j.jad.2016.09.003
5. Zhong BL, Chiu HF, Conwell Y. Elderly suicide trends in the context of transforming China, 1987–2014. Sci Rep. (2016) 6:37724. doi: 10.1038/srep37724
6. Chen WC, Chen SJ, Zhong BL. Sense of alienation and its associations with depressive symptoms and poor sleep quality in older adults who experienced the lockdown in Wuhan, China, during the COVID-19 pandemic. J Geriatr Psychiatry Neurol. (2022) 35:215–22. doi: 10.1177/08919887221078564
8. Diego DL. Late-life suicide in an aging world. Nat Aging. (2022) 2:7–12. doi: 10.1038/s43587-021-00160-1
9. Chattun MR, Amdanee N, Zhang X, Yao Z. Suicidality in the geriatric population. Asian J Psychiatr. (2022) 75:103213. doi: 10.1016/j.ajp.2022.103213
10. Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. (2002) 159:909–16. doi: 10.1176/appi.ajp.159.6.909
11. Chiu HF, Yip PS, Chi I, Chan S, Tsoh J, Kwan CW, et al. Elderly suicide in Hong Kong–a case-controlled psychological autopsy study. Acta Psychiatr Scand. (2004) 109:299–305. doi: 10.1046/j.1600-0447.2003.00263.x
12. Zhou L, Wang G, Jia C, Ma Z. Being left-behind, mental disorder, and elderly suicide in rural China: a case-control psychological autopsy study. Psychol Med. (2019) 49:458–64. doi: 10.1017/S003329171800106X
13. Soriano Barcelo J, Portes Cruz J, Cornes Iglesias JM, Portela Traba B, Brenlla Gonzalez J, Mateos Alvarez R. Health care contact prior to suicide attempts in older adults. a field study in Galicia, Spain. Actas Esp Psiquiatr. (2020) 48:106–15.
14. Zhong BL, Ruan YF, Xu YM, Chen WC, Liu LF. Prevalence and recognition of depressive disorders among Chinese older adults receiving primary care: a multi-center cross-sectional study. J Affect Disord. (2020) 260:26–31. doi: 10.1016/j.jad.2019.09.011
15. O'Connor E, Gaynes BN, Burda BU, Soh C, Whitlock EP. Screening for and treatment of suicide risk relevant to primary care: a systematic review for the US preventive services task force. Ann Intern Med. (2013) 158:741–54. doi: 10.7326/0003-4819-158-10-201305210-00642
16. de Mendonca Lima CA, De Leo D, Ivbijaro G, Svab I. Suicide prevention in older adults. Asia Pac Psychiatry. (2021) 13:e12473. doi: 10.1111/appy.12473
17. Almeida OP, Draper B, Snowdon J, Lautenschlager NT, Pirkis J, Byrne G, et al. Factors associated with suicidal thoughts in a large community study of older adults. Br J Psychiatry. (2012) 201:466–72. doi: 10.1192/bjp.bp.112.110130
18. Cohen A, Chapman BP, Gilman SE, Delmerico AM, Wieczorek W, Duberstein PR, et al. Social inequalities in the occurrence of suicidal ideation among older primary care patients. Am J Geriatr Psychiatry. (2010) 18:1146–54. doi: 10.1097/JGP.0b013e3181dd1e55
19. Heisel MJ, Duberstein PR, Lyness JM, Feldman MD. Screening for suicide ideation among older primary care patients. J Am Board Fam Med. (2010) 23:260–9. doi: 10.3122/jabfm.2010.02.080163
20. Hirsch JK, Duberstein PR, Chapman B, Lyness JM. Positive affect and suicide ideation in older adult primary care patients. Psychol Aging. (2007) 22:380–5. doi: 10.1037/0882-7974.22.2.380
21. Callahan CM, Hendrie HC, Nienaber NA, Tierney WM. Suicidal ideation among older primary care patients. J Am Geriatr Soc. (1996) 44:1205–9. doi: 10.1111/j.1532-5415.1996.tb01370.x
22. Ruckert-Eheberg IM, Lukaschek K, Brenk-Franz K, Strauss B, Gensichen J. Association of adult attachment and suicidal ideation in primary care patients with multiple chronic conditions. J Affect Disord. (2019) 246:121–5. doi: 10.1016/j.jad.2018.12.029
23. Gilman SE, Bruce ML, Ten Have T, Alexopoulos GS, Mulsant BH, Reynolds CF 3rd, et al. Social inequalities in depression and suicidal ideation among older primary care patients. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:59–69. doi: 10.1007/s00127-012-0575-9
24. Zhou Y, Ma Z, Jia CX, Zhou L. Relationship between impulsivity and suicide among the rural elderly in China: a case-control psychological autopsy study. PeerJ. (2021) 9:e11801. doi: 10.7717/peerj.11801
25. Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med. (2004) 164:1179–84. doi: 10.1001/archinte.164.11.1179
26. Miller M. A psychological autopsy of a geriatric suicide. J Geriatr Psychiatry. (1977) 10:229–42.
27. Niu L, Jia C, Ma Z, Wang G, Sun B, Zhang D, et al. Loneliness, hopelessness and suicide in later life: a case-control psychological autopsy study in rural China. Epidemiol Psychiatr Sci. (2020) 29:e119. doi: 10.1017/S2045796020000335
28. Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. (2002) 10:398–406. doi: 10.1097/00019442-200207000-00006
29. Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. (2004) 34:1331–7. doi: 10.1017/S0033291704002600
30. Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. (2011) 34:451–68. doi: 10.1016/j.psc.2011.02.002
31. Conwell Y. Suicide later in life: challenges and priorities for prevention. Am J Prev Med. (2014) 47(3 Suppl 2):S244–50. doi: 10.1016/j.amepre.2014.05.040
32. Luo W, Zhong BL, Chiu HF. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2021) 30:e31. doi: 10.1017/S2045796021000202
33. Wang S, Chen O, Zhao M, Wu F, Wang Y, Wang K. The prevalence of suicide ideation among the Chinese elderly: a meta-analysis. Chin Nurs Res. (2020) 34:806–13. doi: 10.12102/j.issn.1009-6493.2020.05.018
34. Zou G, Lv J, Qiao X. A meta-analysis of detection rate of suicidal ideation in middle school students in China. Chin Ment Health J. (2021) 35:643–50. doi: 10.3969/j.issn.1000-6729.2021.08.006
35. Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG, Li WT, et al. Knowledge, attitudes, and practices toward COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. (2020) 16:1745–52. doi: 10.7150/ijbs.45221
36. Zhong BL, Xu YM, Xie WX, Liu XJ. Quality of life of older Chinese adults receiving primary care in Wuhan, China: a multi-center study. PeerJ. (2019) 7:e6860. doi: 10.7717/peerj.6860
37. Zhong BL, Xu YM, Xie WX, Liu XJ, Huang ZW. Depressive symptoms in elderly Chinese primary care patients: prevalence and sociodemographic and clinical correlates. J Geriatr Psych Neur. (2019) 32:312–8. doi: 10.1177/0891988719862620
38. Zhong BL, Liu XJ, Chen WC, Chiu HF, Conwell Y. Loneliness in Chinese older adults in primary care: prevalence and correlates. Psychogeriatrics. (2018) 18:334–42. doi: 10.1111/psyg.12325
39. Cao H, Zhang J, Guo R, Ye X. Comparison of reliability and validity of two scales in the evaluation of depression status in elderly patients with type 2 diabetes. J Neurosci Ment Heal. (2017) 17:721–6. doi: 10.3969/j.issn.1009-6574.2017.10.010
40. Zhong BL, Chan SSM, Liu TB, Chiu HF. Nonfatal suicidal behaviors of Chinese rural-to-urban migrant workers: attitude toward suicide matters. Suicide Life Threat Behav. (2019) 49:1199–208. doi: 10.1111/sltb.12519
41. Liu Y, Li N, Gao J. Suicide ideation and related factors among elderly people in Beijing. Injur Med. (2014) 3:35–8. doi: 10.3868/j.issn.2095-1566.2014.01.006
42. Luo M, Li J, He Y. Research on suicide ideation of elderly people. Sci Res Age. (2015) 3:41–57. doi: 10.3969/j.issn.2095-5898.2015.07.006
43. Chen S, Conwell Y, Vanorden K, Lu N, Fang Y, Ma Y, et al. Prevalence and natural course of late-life depression in China primary care: a population based study from an urban community. J Affect Disord. (2012) 141:86–93. doi: 10.1016/j.jad.2012.02.027
44. Dai J, Zhong BL, Xiang YT, Chiu HF, Chan SS, Yu X, et al. Internal migration, mental health, and suicidal behaviors in young rural Chinese. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:621–31. doi: 10.1007/s00127-014-0985-y
45. Lehmann M, Kohlmann S, Gierk B, Murray AM, Lowe B. Suicidal ideation in patients with coronary heart disease and hypertension: baseline results from the DEPSCREEN-INFO clinical trial. Clin Psychol Psychother. (2018) 25:754–64. doi: 10.1002/cpp.2305
46. Lee YB, Yu J, Choi HH, Jeon BS, Kim HK, Kim SW, et al. The association between peptic ulcer diseases and mental health problems: a population-based study: a STROBE compliant article. Medicine. (2017) 96:e7828. doi: 10.1097/MD.0000000000007828
47. Huh Y, Kim SM, Lee JH, Nam GE. Associations between the type and number of chronic diseases and suicidal thoughts among Korean adults. Psychiatry Res. (2021) 296:113694. doi: 10.1016/j.psychres.2020.113694
48. Yan Z, Gu M, Zhong B, Wang C, Tang H, Ling Y, et al. Prevalence, risk factors and recognition rates of depressive disorders among inpatients of tertiary general hospitals in Shanghai, China. J Psychosom Res. (2013) 75:65–71. doi: 10.1016/j.jpsychores.2013.03.003
Keywords: older adults, primary care, suicidal ideation, cross-sectional survey, China
Citation: Zhu X-M, Xu Y-M, Wang Z-Q and Zhong B-L (2022) Prevalence and correlates of suicidal ideation among older adults attending primary care clinics in Wuhan, China: A multicenter cross-sectional study. Front. Psychiatry 13:1003810. doi: 10.3389/fpsyt.2022.1003810
Received: 26 July 2022; Accepted: 23 August 2022;
Published: 09 September 2022.
Edited by:
Wenjie Duan, East China University of Science and Technology, ChinaReviewed by:
Xiaomei Zhong, Guangzhou Medical University, ChinaCopyright © 2022 Zhu, Xu, Wang and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bao-Liang Zhong, aGFpemhpbGFuQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.