- Department of Psychology, Franciscan University of Steubenville, Steubenville, OH, United States
Background: Mental health issues have continued to rise globally, including among university students. The COVID-19 pandemic has exacerbated the previously existing and concerning problem. Given that coping mechanisms have been proposed to mediate the relationship between stressors and mental health, the aim of our cross-sectional study was to investigate the mediation of coping mechanisms on the relationship between the impact of the COVID-19 pandemic and mental health.
Methods: University students (≥18 years old; N = 676; 31% male, 69% female) were administered an anonymous survey addressing current demographics, COVID-19 pandemic-related demographics, personal experiences, sources of stress and perceived effect on mental health, politics, sources of news/information, and various pre-validated scales addressing mental health (DASS-21), the impact of the COVID-19 pandemic (IES-R) and coping strategies utilized (Brief COPE).
Results: Our results indicate a substantial proportion of our sample reporting scores in the severe and extremely severe DASS-21 categories, in addition to ~50% reporting a perceived deterioration in mental health relative to pre-COVID-19 pandemic. Moreover, a substantial proportion of students reported IES-R scores at levels where PTSD is of clinical concern. Alarmingly, a significant proportion of females (~15%) reported scores reflecting potential long-term PTSD-related implications. Females tended to be more severely impacted in all mental health measures. Mediation analysis indicated that while dysfunctional coping mediated the relationship between the impact of the event (COVID-19 pandemic) and all three mental health outcomes, overall, this was not the case with the positive coping strategies.
Conclusion: Our study appears to indicate a reduced buffering influence on negative mental health outcomes by the positive coping mechanisms investigated in relation to the COVID-19 pandemic and secondary interventions implemented. While the findings of this study pertain specifically to university students, they corroborate the existing extensive body of research (from physiological to behavioral, preclinical to clinical) pertaining to the response associated with major stressful events at every level of society. In this regard, the findings imply the necessity for health and other authorities, tasked with safeguarding public well-being, to avoid reactive interventions that do not appropriately balance the risks and benefits, potentially exacerbating pre-existing psychopathologies and compromising social order.
Introduction
Well-being is a concept that incorporates the physical, mental, and social aspects of health and does not simply indicate an absence of disease (1, 2). Mental health, also referred to as emotional well-being (3), “includes the presence of positive emotions and moods (e.g., contentment, happiness), the absence of negative emotions (e.g., depression, anxiety), satisfaction with life, fulfillment and positive functioning,” as well as the ability to maintain autonomy (2, 4). Globally, the past several decades have seen a significant decline in mental health in the general population (5, 6).
One group, which appears to be rather vulnerable to negative mental health and has been of special interest, most especially in the past 10 years, is the university student population (7–9). This is, in part, due to the significant and formative period of development (neurodevelopmental, social, etc.) experienced by this age group, with potential long-term implications into adulthood (10–13). This dynamic neurological, and thus behavioral, period of development is also characterized by an increased predisposition to the onset of various psychiatric disorders (14–16).
Psychological stress is defined as “a particular relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering his or her well-being” (17). Psychological stress can have a significant impact on the predisposition, development and expression of mental disorders (18) and, as such, it is necessary to have an understanding of the potential sources of stress in order to aid in finding potential remedies to alleviate the resulting negative consequences. Various stressors have been reported to relate to the mental health problems observed within the university student population, including academic performance, transition from high school, leaving home, changes in social relationships (e.g., new friendships), financial difficulties, post-graduation plans, problematic internet use, sleep, diet, and exercise (19–28). However, one unifying characteristic that identifies most of these stressors and their impact is that, in general, they reflect, with some variation, experiences faced, at varying periods of life, by a broad and significant proportion of the global population.
These challenges, however, bear a definite distinction from significant major external events over which the general population has little control, or those that have an impact not only at the personal level, but also at the local community, state, national and even international levels (e.g., natural disasters, pandemics, war) (29–34). One such event is the COVID-19 pandemic, a global event associated with the SARS-CoV-2 virus, resulting in numerous measures that directly and significantly impacted various aspects of human behavior. These include, but are not limited to, reduced freedom of movement, reduced access to essential needs, and restricted social interaction, purportedly directed to restrict the spread of a virus that was predicted to result in a significant excess in mortality (34–38). Such measures, impacting the very essence of humanity (39–42) and fundamental human behavior (e.g., social relationships, including within the family) also adversely and significantly impacted mental well-being (34, 42, 43).
The potential mental health impact of the COVID-19 pandemic is reflected in the significant increase, observed globally, in the volume of scientific literature addressing this subject, in various groups of the general population, including university students (44–54). Many factors associated with the COVID-19 pandemic, such as the fast spread of news on the internet, including social media, and its potential to induce fear (55), the presentation of the information related to the virus itself, the imposition of national and regional lockdowns, and the involvement of politics have been reported to produce detrimental effects, including in university-age students (42, 56–58). Such situations and conditions also have the potential to adversely impact other areas of life, including relationships (e.g., increased abuse within the family) (59–63) and the economy and finances (e.g., loss of job, loss of businesses) (64), which have also been shown to potentially contribute to decreased mental well-being (65, 66). In relation to university students specifically, this population also faced additional possible stressors related to education including, but not limited to, the transitioning of classes from in-person attendance to online formats and isolation from friends and peer support (36, 67–69). However, extensive research remains necessary to assist in providing a better comprehension of the magnitude of the impact of the COVID-19-related events on the emerging adult group and, more specifically, the university student population.
In times of stress, individuals often employ various coping mechanisms in order to counter or, at the very least, temper the impact of the stressors (70, 71). The stressor and the adopted coping mechanism ultimately impact psychological well-being. In fact, coping has been described as a mediator of emotion (72). Additionally, the relationship between the individual and their response (coping) and the environment from which the stress emanates is considered to be dynamic and bidirectional (17). Previous research further implicates coping as a mediator between mental health and a number of variables (e.g., resilience, psychological maltreatment, body image, locus of control, etc.) (73–78). Thus, the method of coping (e.g., emotion-focused or problem-focused), associated with how the stress is perceived, has the potential to influence the response, positively or negatively, with varying effects on an individual's mental health depending on the coping mechanisms utilized (74, 79–81).
While the impact of stress on mental health and the mediating role of coping mechanisms are substantially documented in the literature, they have not been addressed in regards to the COVID-19 pandemic and the university student population. Thus, given the above literature indicating that coping mechanisms can mediate mental health, and can potentially influence the impact of a stressful life event, in addition to the vulnerability of university students to negative mental health, the aim of this cross-sectional study was to test and verify the mediation of coping mechanisms (emotion-focused, problem-focused, dysfunctional coping) on the association between stress related to the ongoing COVID-19 pandemic and mental health in a sample of university students. It is proposed that the use of a cross-sectional study provides a unique point-in-time perspective of the impact of an event that could not be predicted (the pandemic). Additionally, the continued presence of an event has the potential to confound the measured parameters due to variable adaptation of the responses of the subjects being tested. Thus, according to the evidence provided in the above review, we proposed the following hypothesis: Coping strategies (emotion-focused, problem-focused, dysfunctional coping) have a mediating effect on the relationship between the impact of the COVID-19 pandemic (stressor) and mental health. It is expected that emotion-focused and problem-focused coping, considered to be positive coping strategies (82–86), would potentially aid in reducing the negative mental health impact, while dysfunctional coping would potentially have the opposite effect, that is, positively mediate (i.e., enhance) the negative impact of the event on mental health.
Materials and Methods
Study Design
In compliance with Federal Law, indicating that all researchers conducting testing on human participants must complete training on the protection of research subjects, all survey administrators completed the Protecting Human Research Participants Training Module provided by the NIH Office of Extramural Research. Certification is kept on file for documentation purposes. Prior to administration of the survey, Franciscan University of Steubenville Institutional Review Board (IRB) approval was obtained (#2020-08). Our cross-sectional study consisted of a convenience sample of university/college (undergraduate and graduate) students from Franciscan University of Steubenville, a small private Catholic university located in Steubenville, OH, United States. An anonymous survey was sent via the university student email address, to all students taking classes at Franciscan University, who were at least 18 years of age. Over the course of 4 weeks (August 31st to September 21st, 2020), the survey was administered through the online survey engine SurveyMonkey®. Prior to completing the survey, participants were directed to a consent form, which detailed the confidentiality and the nature of the study and explained that participation in the study implied consent to analyze and publish the overall results. Participants who did not provide consent were directed to the Disqualification Page. The projected time of completion of the survey was ~15–20 min. The instructions indicated to students that they should not spend too much time on any question and give their honest response. The final page of the survey included a link to enter an optional drawing for one (1) of 15 Amazon gift cards (5 of $20 and 10 of $10). The participants were informed that there was no possibility of linking the drawing information to that of the survey and that their information would remain confidential.
Exclusion Criteria
Exclusion criteria included any individual who: (1) was younger than 18 years of age (n = 1), (2) was not a student at Franciscan University of Steubenville (n = 2) or did not complete the question (n = 2), (3) responded “No” (n = 5) or did not complete the question regarding consent (n = 26), (4) did not complete the survey question regarding their age (n = 10), (5) did not provide a response to the Depression, Anxiety and Stress Scale (n = 94) and (6) provided an ambiguous demographic response (n = 1). The final number of participants whose responses met inclusion criteria was 676 (out of the original 817 total respondents, i.e., 83%).
Survey Structure
Demographic Questions
Demographic questions included: age, sex, class, number of semesters completed at Franciscan University, major, housing during the school year at the time of survey, and relationship status. Participants were also asked to indicate whether they were an online-only and/or a transfer student. If the participant indicated that they were a transfer student, they were asked to further indicate whether or not they transferred in the current semester.
Depression, Anxiety and Stress Scale (DASS-21)
The 21-question version of the DASS (87) was also included in the survey. This survey measures various core symptoms associated with depression (D; e.g., “I felt down-hearted and blue”), anxiety (A; e.g., “I felt I was close to panic”) and stress (S; e.g., “I found it difficult to relax”). Subjects were instructed to indicate how much each statement applied to them over the past week on a four-point Likert scale (from 0 = Did not apply to me at all to 3=Applied to me very much, or most of the time). The DASS-21 is not intended to diagnose disorders related to depression, anxiety or stress. The participants' total scores in the three criteria (D, A, and S) were categorized by severity as either “normal,” “mild,” “moderate,” “severe,” or “extremely severe,” as previously defined (88). The Cronbach's alpha for each of the three mental health parameters (depression, anxiety and stress) were α = 0.90, 0.82, and 0.86, respectively, indicating good to excellent internal consistency.
Questions on Pandemic-Related Sources of Stress and Perceived Effect of COVID-19 on Mental Health
Participants were asked to indicate the extent to which they believed their mental health changed relative to the time before the COVID-19 outbreak, as a result of the outbreak and its effects, on a five-point Likert scale (from Much worse to Much better). Additionally, participants were asked to indicate (on a five-point Likert scale from Not at all to Extremely) how significant a source of stress various items were in their lives relative to various factors associated with the COVID-19 pandemic, such as the possibility of contracting COVID-19, the closing of schools/universities, going to public places or a health care facility, etc.
Questions on Personal Experiences Surrounding COVID-19
Returning students (i.e., those who had previously attended Franciscan University) were asked questions regarding various aspects associated with the COVID-19 pandemic, including their level of satisfaction with the online classes at Franciscan University, their state of primary residence during the pandemic, and whether or not they returned home (i.e., place of primary residence during pandemic).
Freshmen, who would not have been attending a university during the initial outbreak of COVID-19, were asked equivalent questions in relation to their high school, as well as where they were living during the outbreak. Similarly, participants who transferred to Franciscan University the semester in which the survey was completed were asked similar questions in relation to the university from which they transferred (i.e., the university they were attending at the time of the COVID-19 outbreak).
Impact of Event Scale—Revised (IES-R)
The revised version of the Impact of Event Scale (89–91) was utilized to assess the participants' responses to a particular event (in this case, the COVID-19 pandemic). Individuals were asked to indicate on a five-point Likert scale (Not at all to Extremely) how distressing each item had been for them in the past seven days in relation to the COVID-19 pandemic. Total overall scores were calculated and categorized into the various levels of impact (89–91). Additionally, average scores were calculated for each of the following subscales: Intrusion (INT; e.g., “I had dreams about it”), Avoidance (AVD; e.g., “I tried not to think about it”), and Hyperarousal (HYP; e.g., “I was jumpy and easily startled”), for which reliability analysis indicated good internal consistency with Cronbach's alpha coefficients of α = 0.87, 0.85, and 0.81, respectively. The internal consistency for the total score, as calculated by Cronbach's alpha, showed a coefficient of α = 0.93.
Questions on COVID-19 Testing
In relation to COVID-19 testing, participants were asked to indicate whether or not they had been tested for COVID-19 prior to or since coming to campus (for Fall 2020 semester) and whether or not they tested positive. Moreover, questions were asked in relation to whether a close/immediate family member or a close friend had been tested for COVID-19 and whether or not they tested positive or negative.
Questions on Changes in Work Resulting From the COVID-19 Pandemic
Various survey questions were asked to assess potential changes in work that the participant, as well as family members and/or close friends, may have experienced as a result of the pandemic. Questions were adapted from the Report on the Economic Well-Being of the U.S. Households in 2019 (64) and addressed whether or not the participant lost a job, experienced an increase or decrease in work hours (e.g., took paid leave, took unpaid leave, etc.) or applied for unemployment benefits since March 1, 2020 (the onset of the coronavirus outbreak in the United States). Equivalent questions were asked in regards to whether or not a close friend or a close/immediate family member had experienced the previously mentioned changes in work since March 1, 2020.
Additionally, participants were asked whether or not they were considered as a frontline/essential worker as defined by CISA (92) during the COVID-19 outbreak, as well as whether or not a close/immediate family member or a close friend fell under such a category.
Questions on Politics and Sources of News/Information
The survey also included questions assessing how much the participant depended on various sources of information pertaining to COVID-19 [e.g., CDC/WHO, Scientific sources (e.g., PubMed, PsycINFO, etc.), Social media, etc.] on a five-point Likert scale (Not at all to Extremely) and how often they watched/read various news sources on a six-point Likert scale (Every day to Never), as well as their rating of the trustworthiness of various news sources (e.g., CNN, Fox News, local newspaper, etc.) in regards to COVID-19 on a seven-point Likert scale (1 = Very untrustworthy to 7=Very trustworthy), with the possibility of indicating that they were not familiar with the news source. Questions were adapted from Dart et al. (93).
Additionally, a question was asked in regards to how the participant would describe themselves politically (Extremely Conservative to Extremely Liberal), as well as whether they think of themselves as Republican (Strong Republican, Moderate Republican, Leaning Republican), Democrat (Strong Democrat, Moderate Democrat, Leaning Democrat) or Independent.
Brief COPE
Our survey also included the Brief COPE (94), a shortened version of the original COPE, which assesses various coping mechanisms that individuals may utilize to cope with stress and deal with problems. Participants were instructed to rate each of the 28 items on a four-point Likert scale (from I haven't been doing this at all to I've been doing this a lot) relative to the COVID-19 pandemic. The 28 items of the Brief COPE are categorized into 14 different scales pertaining to different coping strategies (e.g., active coping, using emotional support, substance use, etc.) (94). Additionally, the 14 scales are then further categorized into Problem-focused (PF; e.g., “I've been thinking hard about what steps to take”), Emotion-focused (EF; e.g., “I've been looking for something good in what is happening”), and Dysfunctional coping (DC; e.g., “I've been giving up the attempt to cope”) (95) strategies. Reliability analysis indicated good internal consistency, as measured by Cronbach's alpha, for PF and DC (α = 0.82 and 0.81, respectively) and acceptable internal consistency for EF (α = 0.78).
Statistical Analysis
Analyses were conducted on all data remaining following the application of the exclusion criteria (n = 676) using R version 4.1.1, SigmaPlot version 14.0 (Systat Software, Inc.) and Jamovi version 2.2.2.0. Differences in proportions between the sexes for the DASS-21, IES-R, Brief COPE (14 subscales), perceived change in mental health and sources of stress relative to COVID-19, as well as within the sexes for perceived change in mental health were analyzed using Chi squared or Fisher's exact test, as appropriate. T-tests (two-tailed) were utilized in order to assess differences between sexes in the average scores of the DASS-21. Differences in the average IES-R subscale scores for those in a category of concern (i.e., score >23) were analyzed using a one-way repeated measures ANOVA, whereas the average Brief COPE subscale scores (three subscales) were analyzed using a two-way repeated measures ANOVA with one factor repetition (Brief COPE subscales) due to the inclusion of sex as a variable in the analysis. Two-way repeated measures ANOVA with one-factor repetition (Brief COPE subscale or EFA factor) was also used to assess differences in the average Brief COPE scores across subscales or average score of the EFA-identified factors between participants scoring below (Normal) or within a level of concern for PTSD (PTSD). Tukey post-hoc analysis was conducted where appropriate. In order to investigate the patterns within the various COVID-19-related sources of stress and uncover specific factors, exploratory factor analysis (EFA) was utilized in this study to explore such patterns rather than to confirm a specific hypothesis relating to the various variables presented to the participants. Bartlett's test of sphericity and the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy were utilized to determine the factorability of the data pertaining to the COVID-19-related sources of stress. Pearson correlations were utilized to assess the relationship between the DASS-21, IES-R, Brief COPE and perceived change in mental health. Given the correlations between the IES-R and DASS-21 subscales and previous literature indicating a relationship between stressful events and mental health, in addition to the reported mediation of such a relationship by various coping behaviors (see Figure 3A) (72), mediation analysis using Baron and Kenny's criteria (96) and using 1,000 bootstrapping replicates (97) was utilized to investigate the potential relationship between the impact of the COVID-19 pandemic (predictor) on the mental health of the participants (outcome) and the potential mediating effect of coping strategies (mediator) on such a relationship.
Results
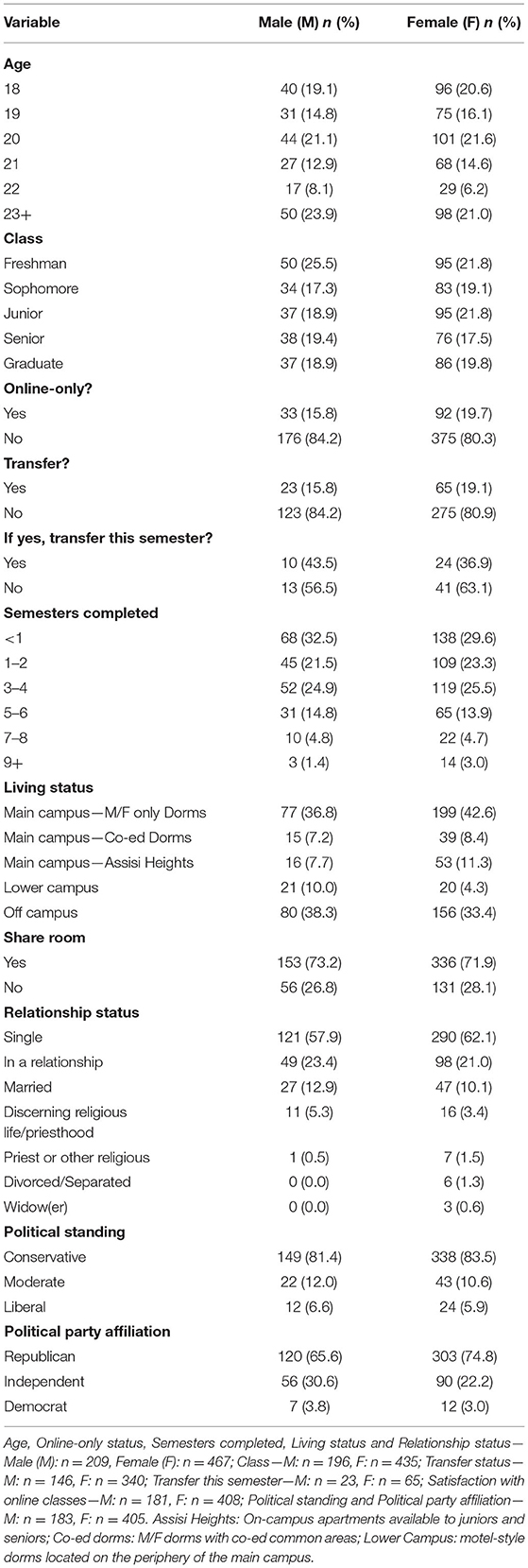
Current Demographics
The distribution of participants was 31% male and 69% female, which is relatively representative of the student population at Franciscan University of Steubenville. The demographic information pertaining to age, class, living status, relationship status, number of semesters completed at Franciscan University, online-only, transfer status, political standing and political party affiliation are presented in Table 1. Additionally, information pertaining to the frequency that participants accessed various sources of information for news and the perceived trustworthiness of various news sources are shown in Supplementary Figure 1 and Figure 2, respectively. This information represents the students during the semester in which the survey was conducted.
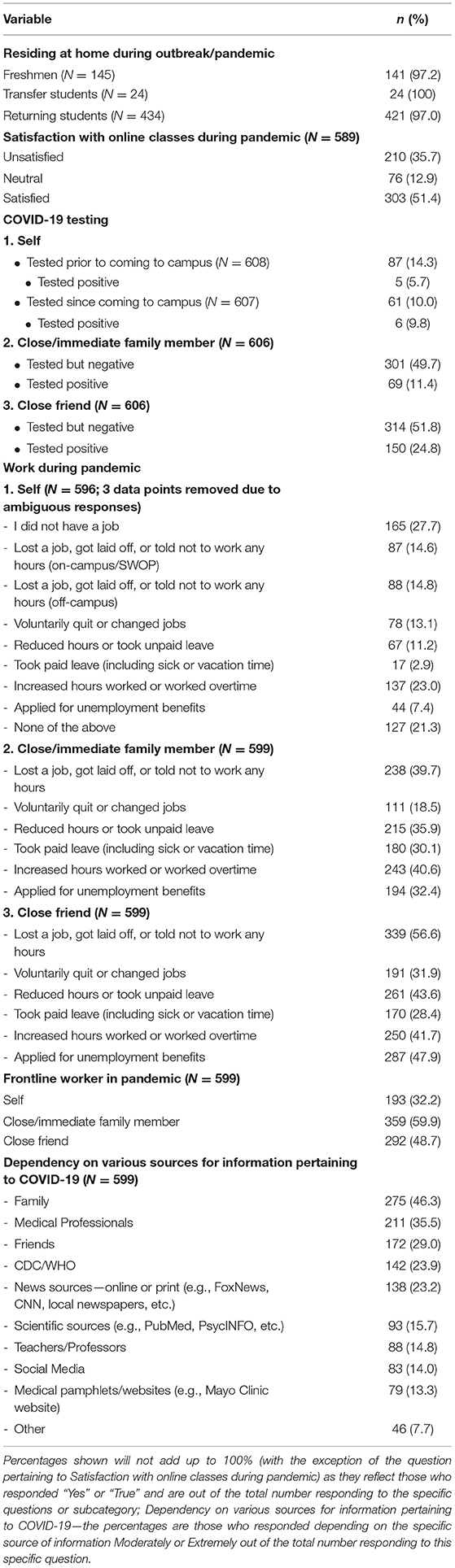
Pandemic-Related Demographics
The geographical distribution of the student sample (N = 617), excluding those who were not residing in the United States (n = 7) and those who provided ambiguous responses (n = 2) is shown in Figure 1. Additional demographics pertaining specifically to the outbreak of the pandemic, including place of residence, satisfaction with online classes, COVID-19 testing, work, frontline worker status and sources of information pertaining to COVID-19, are included in Table 2.
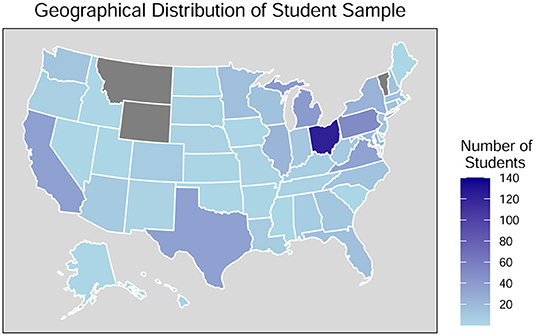
Figure 1. Geographical distribution of student sample during the COVID-19 outbreak (n = 617). Data excludes those who were not residing in the United States (n = 7). Gray-colored states reflect no representation in sample.
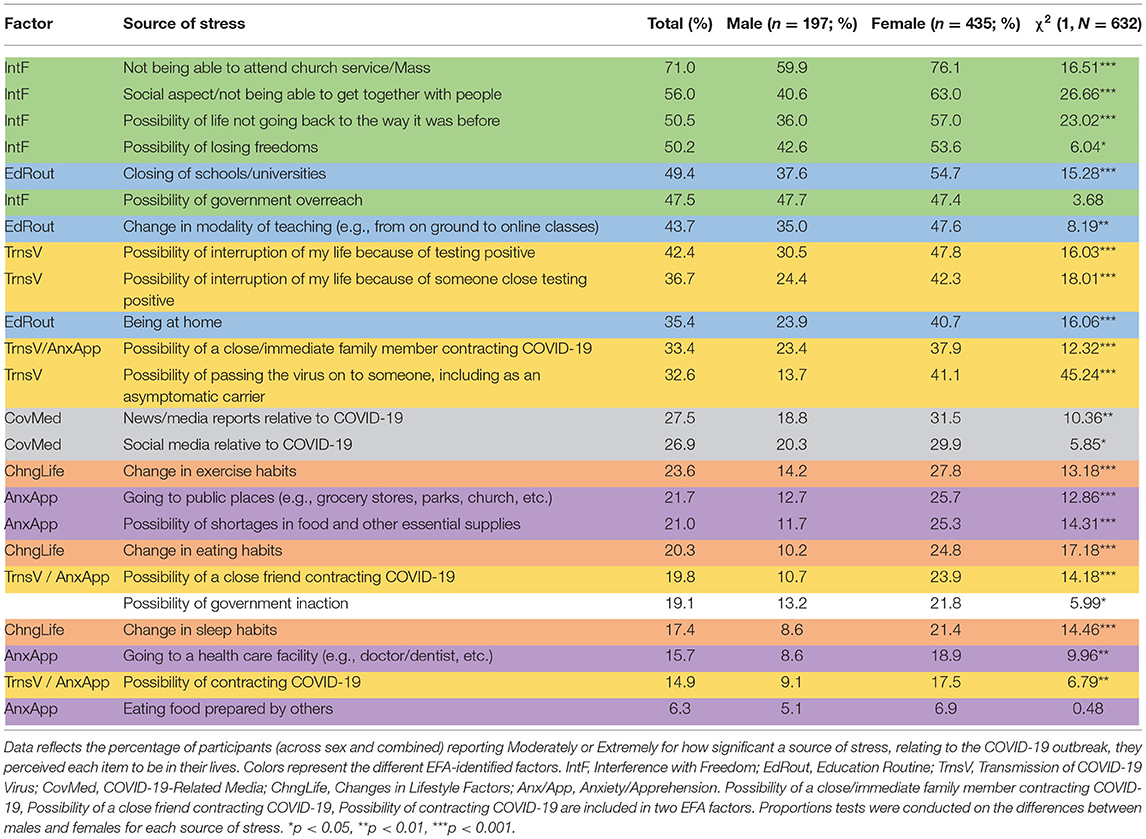
Sources of Stress Relative to COVID-19
The percentage of students (total, males and females) who reported that various potential sources of stress related to the COVID-19 pandemic were a moderate or extreme source of stress are shown in Table 3.
Exploratory Factor Analysis for the COVID-19-Related Sources of Stress
Exploratory factor analysis (EFA) using a principal-axis factor extraction (98, 99) was used to investigate the potential factors present within the sources of stress related to COVID-19 included in our survey. Parallel analysis (98, 99) recommended a six-factor solution (see Table 4). Given the high correlation of the items, a “promax” (oblique) rotation (98, 99) was utilized for interpretation of the six factors. This rotation had sums of squared loadings ranging from 1.67 to 2.90. The correlation coefficients between factors ranged from 0.168 to 0.665.
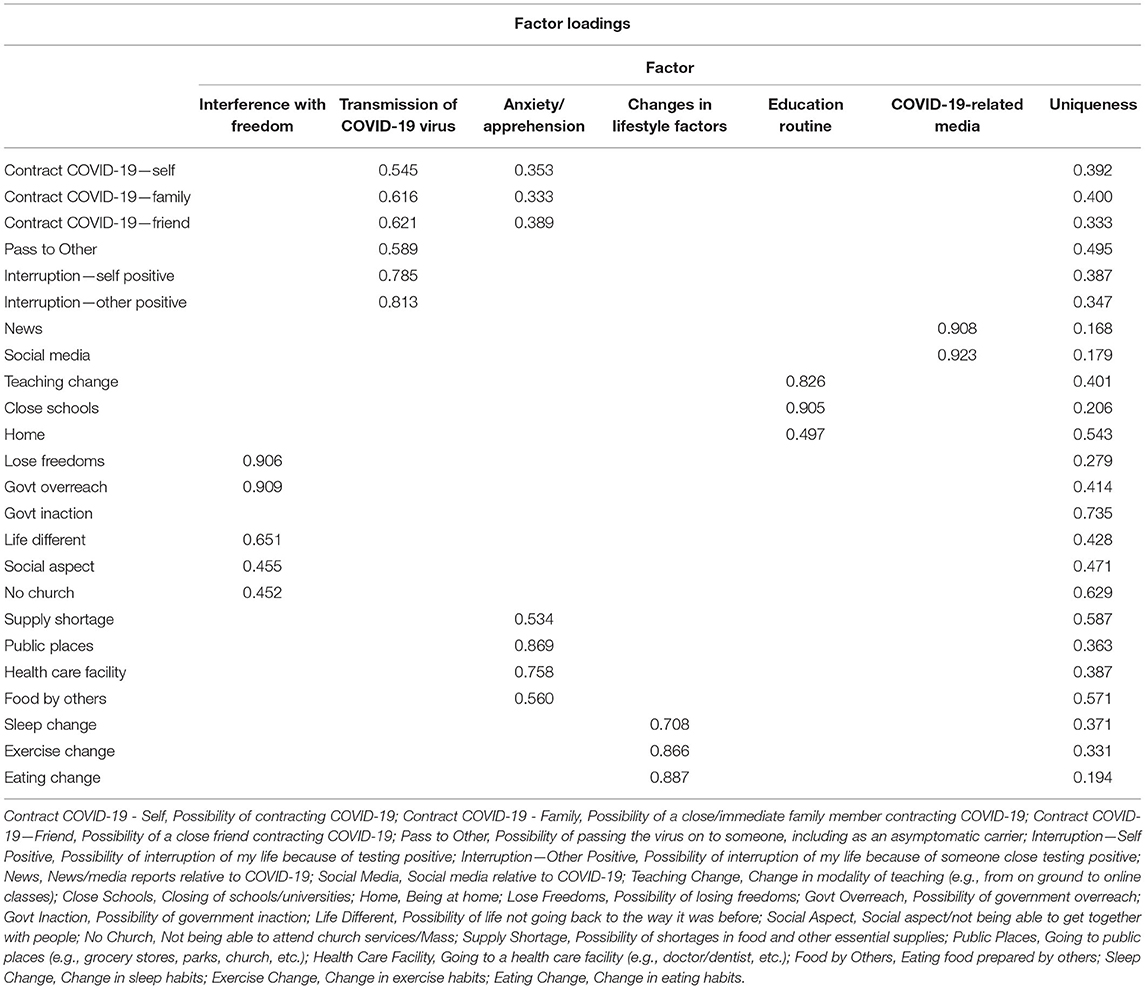
Table 4. Summary of exploratory factor analysis results pertaining to the items addressing COVID-19-related sources of stress, using the principal axis factoring extraction method in combination with a promax rotation (n = 632).
The first factor, identified as “Interference with Freedom” (IntF), included the possibility of losing freedoms (Lose Freedoms), the possibility of government overreach (Govt Overreach), the possibility of life not going back to the way it was before (Life Different), the social aspect and not being able to get together with people (Social Aspect), and not being able to attend church services/Mass (No Church). The second factor, labeled as “Transmission of COVID-19 Virus” (TrnsV), included the possibility of self (Contract COVID-19—Self), a close/immediate family member (Contract COVID-19—Family) or a close friend (Contract COVID-19—Friend) contracting COVID-19, the possibility of passing the virus on to someone, including as an asymptomatic carrier (Pass to Other), and the possibility of interruption of life due to self (Interruption—Self Positive) or someone close (Interruption—Other Positive) testing positive. The third factor, “Anxiety/Apprehension” (AnxApp), also included the possibility of self, a close/immediate family member or a close friend contracting COVID-19, as well as the possibility of shortages in food and other essential supplies (Supply Shortage), going to public places (e.g., grocery stores, parks, church, etc.) (Public Places), going to a health care facility (e.g., doctor/dentist, etc.) (Health Care Facility), and eating food prepared by others (Food by Others). The fourth factor, identified as “Changes in Lifestyle Factors” (ChngLife), included changes in sleep (Sleep Change), exercise (Exercise Change) and eating (Eating Change) habits, all factors involved in the overall health and well-being of the individual. The fifth factor, labeled as “Education Routine” (EdRout), included change in modality of teaching (e.g., from on ground to online classes) (Teaching Change), the closing of schools/universities (Close Schools) and being at home (Home). The final factor, “COVID-19-Related Media” (CovMed), included news/media reports (News) and social media (Social Media) relative to COVID-19. Of note, the possibility of government inaction (Govt Inaction) as a potential source of stress was not included in any factor following EFA.
Mental Health
DASS-21
Based on the scoring of the DASS-21 as previously described (87), from the participants who completed this section of the survey (N = 676), the overall percentages for each of the categories was as follows: Normal: 59.6, 62.1, and 67.5%; Mild: 12.1, 7.8, 9.2%; Moderate: 15.4, 14.5, 12.0%; Severe: 5.9, 6.5, 8.7%; Extremely Severe: 7.0, 9.0, 2.7% for depression, anxiety and stress, respectively. In relation to the average scores for each of the subscales, analysis revealed significantly higher average anxiety [t(674) = 4.894, p < 0.001, r2 = 0.034] and stress [t(674) = 5.124, p < 0.001, r2 = 0.037] scores in females relative to males, as well as a tendency toward significance [t(674) = 1.711, p = 0.088, r2 = 0.004] in average depression scores with females scoring higher than males. Additionally, the sex differences in relation to the proportions pertaining to the combined severe and extremely severe categories for each of the subscales are provided in Table 5.
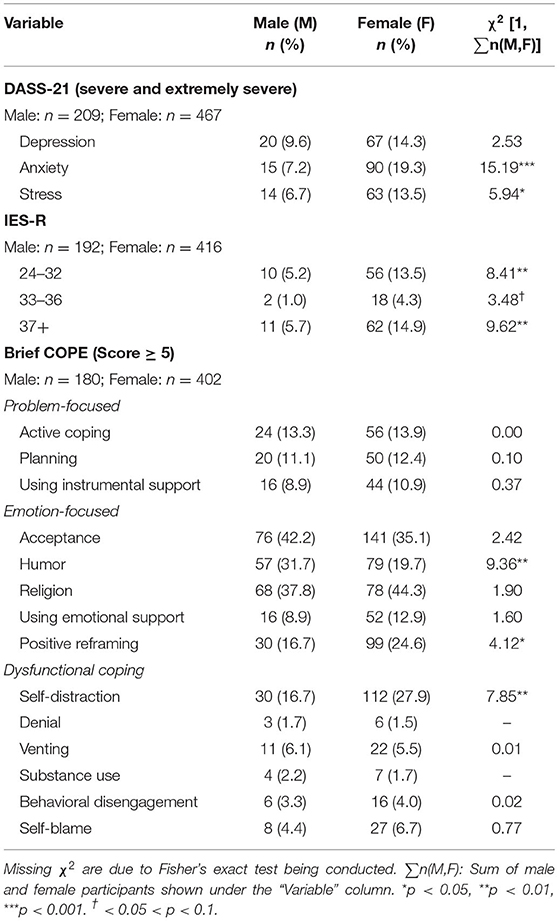
Table 5. Percentages and proportions test outputs between the sexes pertaining to the DASS-21, IES-R and Brief COPE survey scales.
Perceived Change in Mental Health as a Result of COVID-19
Analysis of the question assessing the extent that the participants believed their mental health changed relative to the time before the COVID-19 outbreak indicated a significantly higher proportion [χ2 (1, N = 632) = 9.30, p < 0.01] of females (53.6%) relative to males (40.1%) reporting worse (Somewhat worse or Much worse) mental health. Moreover, a significantly higher proportion of males relative to females reported perceiving their mental health to have remained About the same [χ2 (1, N = 632) = 7.03, p < 0.01; Males: 45.2%, Females: 33.8%]. Additionally, there was no significant difference between the proportion of males and females who reported that they believed their mental health was better (Somewhat better or Much better) [χ2 (1, N = 632) = 0.34, p > 0.05; Males: 14.7%, Females: 12.6%].
Within the specific sexes, the greatest proportion of females reported worse followed by About the same and better mental health. All comparisons were significant (all p < 0.001) [χ2 (2, N = 435) = 163.94, p < 0.001]. Relative to males, a significantly higher proportion [χ2 (2, N = 197) = 47.21, p < 0.001] reported worse and About the same relative to better (both p < 0.001). However, unlike females, there was no significant difference between the proportion of males who reported worse and About the same (p > 0.05).
IES-R
A significantly [χ2 (1, N = 608) = 28.12, p < 0.001] higher proportion of females (32.7%) relative to males (12.0%) reported total IES-R scores within the published cutoff values for PTSD (100–102). The sex differences in relation to the proportions pertaining to each of the severity levels of PTSD symptoms (24–32, 33–36, 37+) are provided in Table 5. Moreover, within each category of severity of the IES-R total score, the average scores reported were not significantly different between the sexes (24–32—Females: M = 28.09, SEM = 0.34; Males: M = 27.40, SEM = 0.72; 33–36—Females: M = 34.39, SEM = 0.23; Males: M = 34.50, SEM = 0.50; and 37+—Females: M = 46.84, SEM = 1.13; Males: M = 45.73, SEM = 2.55; all p > 0.05).
The IES-R scores were sub-categorized into three subscales (intrusion, INT; avoidance, AVD; hyperarousal, HYP) according to Weiss (91). Given that the average INT, AVD and HYP scores were not significantly different between the sexes (all p > 0.05), the data for both sexes was combined and analyzed to assess the differences between the average scores for each subscale. This analysis indicated a significant difference between subscale scores, F(2,316) = 27.25, p < 0.001, η2 = 0.076. Post-hoc analysis indicated that the average AVD score (M = 1.97, SEM = 0.05) was significantly higher than both INT and HYP average scores (INT: M = 1.55, SEM = 0.05; HYP: M = 1.55, SEM = 0.06; both p < 0.001). There was no significant difference between the INT and HYP average scores (p > 0.05).
Brief COPE
In relation to coping strategies, as measured by the Brief COPE, the results indicated a significant effect of sex [F(1,1160) = 9.77, p < 0.01, η2= 0.008) and the subscales (emotion-focused, EF; problem-focused, PF; dysfunctional coping, DC; F(2,1160) = 451.28, p < 0.001, η2 = 0.215). However, there was no significant effect of the interaction between sex and Brief COPE subscales [F(2,1160) = 0.00, p > 0.05, η2 = 0.000). Post-hoc analysis indicated that the average EF score (Females: M = 1.60, SEM = 0.03; Males: M = 1.46, SEM = 0.04) was significantly higher than both PF (Females: M = 1.17, SEM = 0.03; Males: M = 1.04, SEM = 0.05) and DC (Females: M = 0.73, SEM = 0.02; Males: M = 0.60, SEM = 0.03) scores for both males and females. Additionally, PF was significantly higher than DC for both sexes (all p < 0.001). Moreover, females scored significantly higher than males in all three subscales (all p < 0.05).
The three subscales of the Brief COPE are further broken down into 14 subcategories addressing the frequency of utilization of specific coping mechanisms. The breakdown of the proportions for the sexes reporting a score ≥5 (at least one score indicating “I've been doing this a lot” and one score of “I've been doing this a medium amount,” or both scores indicating “I've been doing this a lot”) for each of the 14 categories of coping strategies, measured by the Brief COPE, are shown in Table 5.
In addition to the above relationships, we were also interested in how our results compared to the breakdown provided by Mohr, Delfino et al. (103, 104) addressing Activity (AC, activity-passivity) and Defeatism (DF, defeatism-resilience). Using the criteria addressed by Delfino et al. (104) defining “high defeatism” as being ≥1.3 standard deviations above the mean and reflecting insufficient coping behavior under chronic stress, our results indicate that 10.5% of the sample students met this criterion.
Correlation of DASS-21, IES-R, Brief COPE, and Perception of Mental Health Change Relative to COVID-19 Outbreak
Correlation analysis indicated various significant positive relationships (Figure 2) between the variables measured pertaining to mental health (DASS-21; D, A, S), the impact of the COVID-19 pandemic on the participant (IES-R; HYP, INT, AVD) and coping mechanisms (Brief COPE; EF, PF, DC). Moreover, various significant negative correlations were revealed between these measures and the question regarding the participant's perceived change in mental health relative to before the COVID-19 outbreak. Given the coding of the question pertaining to mental health change relative to the COVID-19 outbreak, with “much worse” coded as “0” to “much better” coded as “4,” a negative correlation indicates that the higher the score on the various scales (DASS-21, IES-R and Brief COPE), the worse (lower score) the participant perceived their mental health to be.
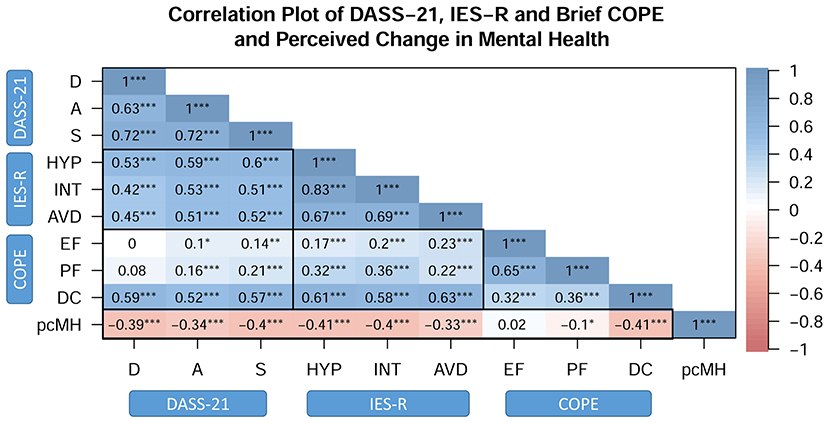
Figure 2. Correlation plot of mental health outcomes (DASS-21), the impact of the COVID-19 pandemic (IES-R), coping strategies (Brief COPE) and perceived change in mental health. DASS-21: D, depression; A, anxiety; S, stress; IES-R: HYP, hyperarousal; INT, intrusion; AVD, avoidance; COPE: Brief COPE, EF, emotion-focused coping; PF, problem-focused coping; DC, dysfunctional coping; pcMH: perceived change in mental health relative to before the COVID-19 outbreak. *p < 0.05, **p < 0.01, ***p < 0.001.
In relation to the breakdown of the Brief COPE provided by Mohr et al., and addressed above, our results indicated strong and significant relationships between dysfunctional coping and defeatism (r = 0.89, p < 0.001), as well as between both problem-focused and emotion-focused coping and activity (PF vs. AC: r = 0.88; EF vs. AC: r = 0.87; both p < 0.001). The relationships between DF and the mental health measures (DF vs. D: r = 0.50, A: r = 0.49 and S: r = 0.49; all p < 0.001) are similar to those reported for DC and the mental health measures.
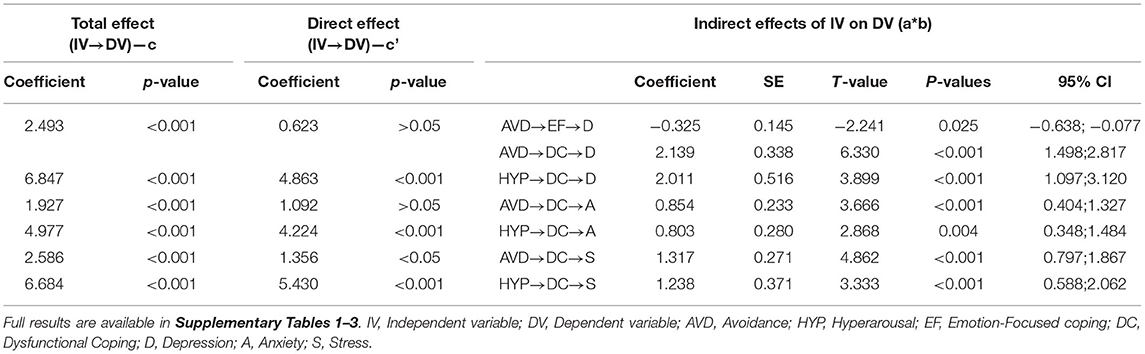
Mediation Analysis of DASS-21, IES-R, and Brief COPE
Mediation analysis was performed to assess the mediating role of coping strategies (M = Mediator; PF, EF, and DC) on the relationship between the stressful responses caused by the impact of an event (IV = independent variable; INT, AVD and HYP) and mental health (DV= dependent variable; D, A, and S). Figure 3 shows the hypothesized conceptual model (Figure 3A) along with the final models (Figures 3B–D) for each of the mental health parameters (D, A, and S, respectively). The significant mediation pathways, including the indirect relationships, addressed in Table 6 (full results shown in Supplementary Tables 1–3), revealed that the total effect of AVD, INT and HYP on Depression scores were significant (H1: β = 2.49, t = 4.43, p < 0.001; β = −2.11, t = −2.39, p < 0.05; β = 6.85, t = 8.14, p < 0.001, respectively). Moreover, both Anxiety and Stress revealed similar behaviors. The results indicated a significant total effect for both Anxiety and Stress in relation to AVD (H1: β = 1.93, t = 4.32, p < 0.001; β = 2.59, t = 5.00, p < 0.001, for Anxiety and Stress, respectively) and HYP (H1: β = 4.98, t =7.46, p < 0.001; β = 6.68, t =8.63, p < 0.001 for Anxiety and Stress, respectively). The total effect relating to INT was not significant in either Anxiety or Stress (H1: β = 0.17, t = 0.25, and β = −1.06, t = −1.30, respectively, both p > 0.05).
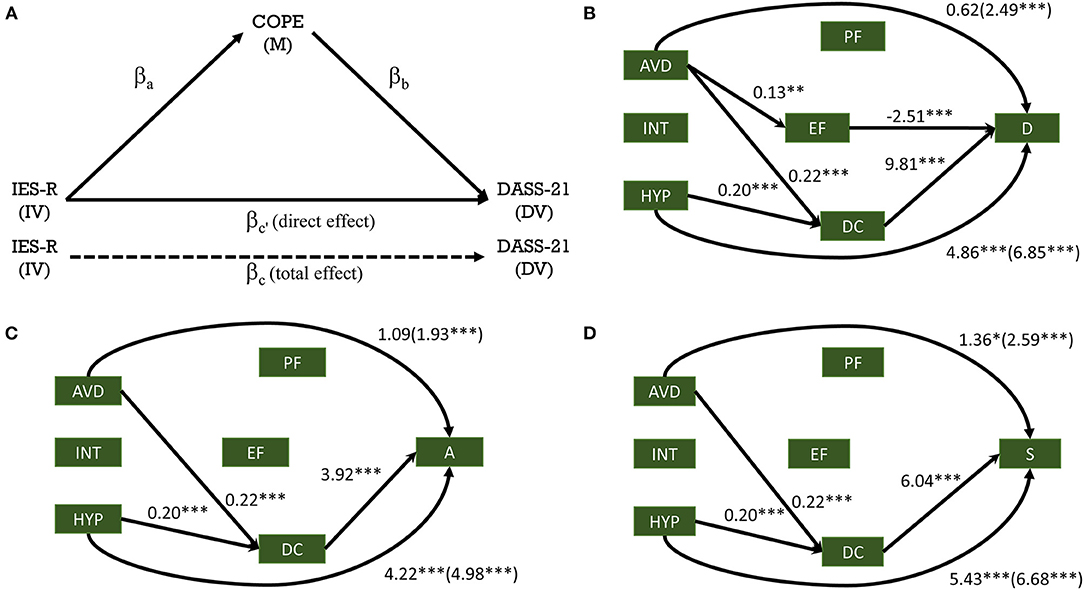
Figure 3. Mediation analysis of the impact of the COVID-19 pandemic on mental health, mediated through coping strategies. Hypothesized mediation model (A); Final mediation model for depression (B), anxiety (C) and stress (D). DASS-21: D, depression; A, anxiety; S, stress; IES-R: HYP, hyperarousal; INT, intrusion; AVD, avoidance; COPE: Brief COPE, EF, emotion-focused coping; PF, problem-focused coping; DC, dysfunctional coping. Data represents estimates/betas—direct (total). IV, independent variable; DV, dependent variable; M, mediator. *p < 0.05, **p < 0.01, ***p < 0.001.
With the inclusion of the mediating variables (PF, EF, DC), the impact of the independent variable (impact of event) was affected differentially between the three mental health outcomes (D, A, S). Specifically, the impact of HYP on D, A, and S was still found significant (β = 4.86, t = 5.03; β = 4.22, t = 4.24; β = 5.43, t = 6.15, respectively; all p < 0.001). However, the impact of INT and AVD on the depression scores (D), showed a tendency toward significance (INT: β = −1.87, t = −1.93, p = 0.054) or did not remain significant (AVD: β =0.62, t = 0.99, p > 0.05). In relation to A and S, the impact of INT and AVD was not significant (INT: β = 0.28, t = 0.32, p > 0.05; β = −1.18, t = −1.33, p > 0.05 for A and S, respectively) or showed a tendency toward significance for A in relation to AVD (β = 1.09, t = 1.86, p = 0.063). In relation to S, the impact of AVD was reduced but remained significant, β = 1.36, t = 2.04, p < 0.05.
The indirect effect of the impact of event as measured by HYP on Depression, Anxiety and Stress scores through DC was found significant (β = 2.01, t = 3.90, p < 0.001; β = 0.80, t = 2.87, p < 0.01; β = 1.24, t = 3.33, p < 0.001 for D, A, and S, respectively). In a similar fashion, the impact of event as measured by AVD on Depression, Anxiety and Stress scores through DC was found significant (β = 2.14, t = 6.33; β = 0.85, t = 3.67; β = 1.32, t = 4.86, all p < 0.001 for D, A, and S, respectively). The indirect effect of AVD on mental health through EF was only significant in the case of Depression (β = −0.33, t = −2.24, p < 0.05).
Thus, our findings indicate that the relationship between the impact of the event being addressed in this study (“with respect to the Coronavirus Disease 2019 (COVID-19) pandemic, which occurred starting around December 2019”) and mental health (D, A, and S) was primarily mediated by dysfunctional coping (DC) for all mental health measures, while depression was also mediated by emotion-focused (EF) coping.
Brief COPE and COVID-19-Related Sources of Stress Across IES-R Outcome
Pertaining to the Brief COPE subscales, when the IES-R scores were categorized as normal (<24, Normal) or of clinical concern for PTSD (≥24, PTSD), analysis indicated a significant difference across IES-R category [Normal vs. PTSD, F(1,1160) = 98.13, η2 = 0.068], coping strategy [EF, PF and DC, F(2,1160) = 343.04, η2 = 0.157] and the interaction of IES-R category x coping strategy, F(2,1160) = 23.48, η2 = 0.011, all p < 0.001. Post-hoc analysis indicated significant differences for all within and between factor comparisons (all p < 0.001), with those in the PTSD category scoring higher than the Normal category and with the EF coping strategy being higher than the PF, which in turn was higher than the DC coping strategy (Figure 4A).
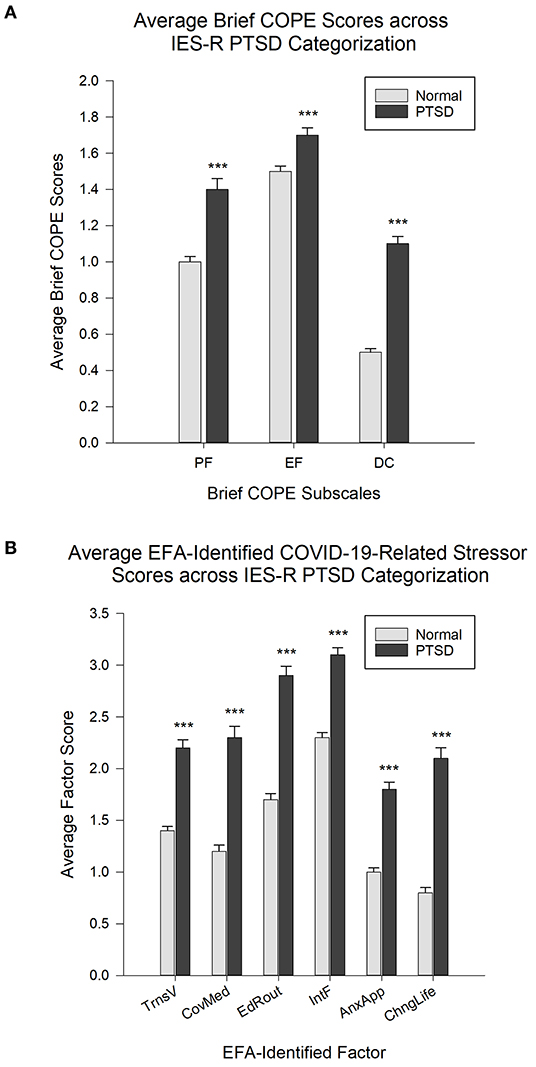
Figure 4. (A) Average Brief COPE scores for each subscale across IES-R categorization of scores falling within the normal range (<24, Normal) and those falling within the range of clinical concern for PTSD (≥24, PTSD). EF, emotion-focused coping; PF, problem-focused coping; DC, dysfunctional coping. N = 582; Normal: n = 426; PTSD: n =156. (B) Average factor scores, with higher scores interpreted as higher likelihood of perceiving the stressors as more stressful, across IES-R categorization of Normal (<24, Normal) and of clinical concern for PTSD (≥24, PTSD). N = 608; Normal: n = 449; PTSD: n = 159. ***p < 0.001 relative to the Normal group. Data is expressed as Mean ± SEM.
In regards to the average scores reported for the EFA-identified factors (TrnsV, CovMed, EdRout, IntF, AnxApp, and ChngLife) relating to COVID-19-related sources of stress, across IES-R category (Normal vs. PTSD), analysis indicated a significant difference across IES-R category [F(1,3030) = 272.80, η2 = 0.129], source of stress factor [F(5,3030) = 143.15, η2 = 0.104] and the interaction of IES-R category x stress factor, F(5,3030) = 6.02, η2 = 0.004, all p < 0.001. Post-hoc analysis indicated a significantly higher average score in the PTSD subgroup (interpreted as higher likelihood of perceiving the stressors as more stressful) relative to the Normal subgroup for all EFA-identified source of stress factors (all p < 0.001). In relation to the stress factors for the Normal IES-R category, all p < 0.001 except for TrnsV vs. CovMed and AnxApp vs. ChngLife, p < 0.01, while CovMed vs. AnxApp, p < 0.05. For the PTSD subgroup, both IntF and EdRout were significantly higher (all p < 0.001) than all other factors except relative to each other (p > 0.05), and both CovMed and TrnsV were significantly higher than AnxApp, p < 0.001 and p < 0.01, respectively. All other comparisons were not significant (p > 0.05) (Figure 4B).
Discussion
The relationship that exists between a stressful event and the resultant impact on the mental health of an individual is complex. The complexity stems from the nature of the stressful event itself, in addition to how the individual perceives the stress and its consequences (threat vs. challenge), and how they ultimately respond to the event (emotional vs. logical) (80, 105).
As indicated above, we proposed that based on previous findings, coping strategies (emotion-focused, problem-focused, dysfunctional coping) would have a mediating effect on the relationship between the impact of the COVID-19 pandemic (stressor) and mental health (outcome). In our study, this investigation was conducted utilizing a cross-sectional methodology. As addressed earlier, the use of a cross-sectional study provides an opportunity to investigate the potential effects when the event is still taking place or shortly after, avoiding the potential for recall bias (29).
COVID-19 Pandemic and Depression, Anxiety, and Stress
Our findings indicate a substantial proportion of students in the severe and extremely severe categories of the depression, anxiety and stress scales. In relation to the average scores, females scored higher than males in all mental health measures, significantly in anxiety and stress, and a tendency toward significance in depression. Additionally, a significant proportion of students (~50%) reported perceiving a deterioration in their mental health relative to before the onset of the COVID-19 pandemic, with the proportion of females being significantly higher than males.
COVID-19 Pandemic: Impact, Coping, and Mental Health
In relation to the impact of the COVID-19 pandemic, a substantial proportion of students reported scores within the previously established cutoff values for PTSD, with a significantly higher proportion of females scoring at a level where PTSD is a clinical concern (100–102). Alarmingly, a significant percentage of females (~15%) fell in the highest category, which has been described as potentially impacting the immune system long-term (100). This proportion was also significantly higher than the proportion of males in the same category. These results, indicating levels of potential clinical concern within our sample, appear to also correspond with previous reports describing COVID-19 as a traumatic stressor resulting in PTSD-like responses (51). Moreover, all three IES-R subscales (AVD, INT, HYP) were significantly positively correlated to the three mental health outcomes (D, A, S). Additionally, all three IES-R subscales were most strongly correlated to the dysfunctional coping strategy of the Brief COPE, which was also the coping strategy that was most strongly related to the three mental health measures. Mediation analysis indicated that dysfunctional coping mediated the relationship between both AVD and HYP, and all three mental health measures. Additionally, the only mediation involving positive coping strategies [PF, EF; (82–86)] was that of emotion-focused coping mediating the relationship between AVD and depression, corroborating previous findings (106, 107). This is despite the fact that both the average scores of the positive coping mechanisms and the number of respondents reporting utilizing these coping mechanisms were higher than the DC strategy.
Pertaining to EF and PF (positive coping strategies), in addition to the general absence of a positive influence of such coping mechanisms on mental health as indicated by the mediation analysis, small positive relationships were observed in relation to the anxiety and stress scores. This may result from the potential for even positive coping mechanisms (e.g., finding comfort in religion or spiritual beliefs) to be misused (e.g., misuse of humor, spiritual bypass, etc.) (108–111) with the potential for negative mental health consequences.
Taken in the context of the data pertaining to the impact of the event (IES-R) indicating that ~33% of our females and 12% of our males were in a category of concern for the IES-R, and the rather substantial correlations between the IES-R and mental health (DASS-21) scores addressed above, it appears that coping strategies, while playing a role in mediating negative mental health outcomes through dysfunctional coping strategies, were not influential in minimizing the impact of the event on mental health. This may be indicative of potential additional factors/variables that may influence mental health outcomes more potently than the buffering capacity of the coping strategies addressed in this study.
Chronic Stress: Physiology, Behavior, and Influence on Coping Responses
A potential major factor that may impact this dynamic between the stressor, the coping mechanism and the mental health outcome is chronic stress (as distinct from acute stress). Chronic stress is known to significantly influence physiology (112–114), including neurophysiology (115–117) and the immune system (118–120). As a result, it is to be expected that health in general will also be impacted. Additionally, and related, chronic stress contributes to the potential for an increased predisposition to psychiatric disorders such as depression and anxiety (121, 122). Ironically, it may also impact the efficacy of treatments (e.g., psychotropics, vaccinations, etc.) targeted toward the very same systems (e.g., central nervous system, immune system, etc.) affected by chronic stress (119, 123, 124).
Thus, given the complex impact of chronic stress, including at the neurophysiological level and its implication at the behavioral level (113, 116), it is reasonable to expect interference with the very behaviors that have the potential to be used to buffer the impact of stressful events. The response and coping strategies utilized in the presence of a stressor will vary and are dependent on the nature, duration and intensity of the stressor and the impact of the lingering stressor on the physiology. This dynamic may lead to a diversity of responses in the various systems (e.g., behavioral, endocrine) within the organism (125) that inform future responses. It is possible that part of this diversity of responses may involve a failure of healthy coping strategies (82) to positively impact mental health and the potential adoption of maladaptive coping strategies (126). This may potentially contribute to explaining the observations described above relating to the higher reported use of positive coping strategies in our sample with minimal impact on mental health outcomes.
Additionally, this may represent a physiological and psychological burnout that perpetuates further maladaptive coping and negative mental health (127, 128). This may reflect the observed relationship between dysfunctional coping and all three mental health parameters, in addition to the mediating role of dysfunctional coping in influencing the impact of the COVID-19 pandemic on mental health. Moreover, our results also indicate a substantial relationship between dysfunctional coping and what Mohr et al. refer to as defeatism (constituting a substantial portion of the dysfunctional coping questions of the Brief COPE). Defeatism, defined as consisting of such behaviors “like ‘giving up', ‘using alcohol' or ‘refusing to believe that this happened',” also reflects insufficient coping behavior in the presence of chronic stress (103, 104). In this regard, our data revealed a similar proportion of students displaying insufficient coping to those reported previously, cross-culturally, under chronic stress (104).
COVID-19-Related Interventions and Impact
In relation to the COVID-19 pandemic, implemented secondary measures seeking to putatively address the pandemic (e.g., lockdowns, isolation, etc.) and the resulting consequences have the potential to influence how the event itself impacts the dynamic described above in relation to chronic stress, coping and mental health and the magnitude of such an impact. Such consequences have been reported extensively in other reports including, but not limited to, increased substance use to cope with the pandemic (46, 129), increased numbers of reported drug overdoses and related deaths (130–133), increased reports of suicidal ideation/thoughts/consideration of suicide (46, 47), loss of work/increased unemployment (134), financial hardships (135), loss of essential social interaction (40, 135, 136), physical health disturbances [e.g., sleep, exercise, eating habits; (47, 137–141)] and disruption of education (142).
Our results indicate that university students were not immune or exempt from the impact of the secondary measures implemented and discussed above. This is of special concern given that university students are within the age range (mid-teens to mid-20's) when a majority of mental disorders manifest themselves (143). Students are not shielded entirely from the realities of the events taking place around them, such as steps taken by various authorities (e.g., federal and local governments, school administrations etc.), and recognize the potential impact that such events have on their personal lives and the lives of those close to them (e.g., situations of unemployment). These experiences assist them in forming schemas informing their interpretation and perception of the same events.
In this regard, interestingly, pertaining to the secondary measures implemented in relation to COVID-19, the top 10 stressors reported by the student sample (sexes combined) reflected all the variables identified within the Interference with Freedom and Education Routine factors, in addition to two variables within the Transmission of COVID-19 Virus factor, specifically the “Possibility of interruption of my life because of testing positive” and the “Possibility of interruption of my life because of someone close testing positive.” All of these variables reflect an interruption of life by the measures implemented, rather than concerns directly relating to the actual SARS-CoV-2 virus itself, including the potential for contracting it.
Limitations and Future Research
Given the complexity of the events that have occurred since the outbreak of COVID-19, the global nature of the event, the complexity of human behavior and the potential uniqueness of the sample involving students from a single location, caution is necessary, as is in fact with all human studies, in extrapolating and generalizing the findings and subsequent implications. Related is the complication associated with more localized restrictions, at the state, the city and even at the institutional level. Moreover, the findings of this study need to be interpreted in the context of the large body of research that continues to accumulate addressing the indirect impact of the COVID-19 pandemic associated with the measures taken. However, consideration also needs to be given to the consistencies of our results with cross-cultural, cross-age and cross-sex findings reported in both national and international studies. A limitation of our work is the potential for survey fatigue due to the length of the survey. Associated with this limitation is the logistical constraint present in any survey research on the number of topics investigated within a single survey. Additionally, in relation to coping strategies, while the 14 Brief COPE subscales addressed a number of coping mechanisms (e.g., the use of religion/faith for emotion-focused coping) constituting the three principal categories (EF, PF, and DC), they were limited in their capacity to address these in great depth, e.g., positive vs. negative religious coping. Our study also did not provide an opportunity for the participants to report how they personally appraised the event. Future research should take into consideration these limitations in addition to considering addressing in greater depth the potential for differential impacts on mental health of the various interventions implemented in different institutions, localities, states and countries.
Conclusion
In conclusion, our study appears to reflect a minimal impact of the positive coping mechanisms investigated (emotion-focused, problem-focused) in minimizing the negative mental health outcomes in the context of the COVID-19 pandemic. This was evident in the higher levels of reported use of such strategies, but with minimal mediation of any of the mental health parameters. Conversely, while the use of dysfunctional coping mediated the relationship between the impact of the event and mental health, this was also the coping mechanism reported to be used least by the students. Given (1) the absence of an impact of the positive coping mechanisms investigated, which have been previously reported to positively influence mental health, (2) the higher prevalence of the utilization of positive coping mechanisms relative to the dysfunctional coping strategy, (3) the perceived worsening of mental health relative to prior to the pandemic, (4) the reported significant COVID-19-related stressors, and (5) previous non-COVID-19-related research [e.g., (82)] indicating the potential that emotion- and problem-focused strategies are effective in “benign” but not “severe” events, our study appears to highlight an influence of external factors that may override the capacity/efficacy of certain coping mechanisms (e.g., those measured in this study) to positively impact mental health in the presence of a significant chronic stressor. Our results cannot be interpreted as concluding that other positive coping mechanisms may not potentially play a role in mediating the stress imposed by the implemented measures and restrictions during the COVID-19 pandemic. Rather, the implication is that, in light of the reviewed literature indicating the specific positive coping strategies addressed as mediators in this study (EF and PF) in reducing the impact of various stressors on mental health, it appears, and it should be of concern, that the stress resulting from the putative mitigation efforts significantly overwhelmed the mediating capacity of these specific coping measures. Moreover, our results appear to corroborate previous literature indicating the potential exacerbation of negative mental health issues, including PTSD-like reactions, by the COVID-19 pandemic (51) and show a similarity in impact on mental health to those observed in previous major events (e.g., SARS-CoV-1, September 11, 2001 terrorist attacks in the US), as well as other reports relating to the current COVID-19 pandemic, reflecting significant negative mental health consequences in the general population, including in university students (29–31, 33, 34, 51, 144–147).
Our research indicates the necessity for continued surveillance of mental health in relation to the ongoing COVID-19 pandemic and the associated interventions within the university student population. This includes the need for efforts to reduce the impact of influences that may contribute to propagating a sense of despondency (55), potentially amplifying behaviors that may result from or increase the predisposition to negative mental health outcomes, such as alcohol consumption, drug abuse, suicidal ideation, etc. (47, 53, 131–133, 148). Efforts should also target measures that ensure the presence of sufficient supporting elements (e.g., counseling centers and staff), in addition to educational efforts that develop and facilitate personality traits that build strength in character. These would, in turn, support the development of positive mental health characteristics and the ability to look beyond the perceived threat and recognize and utilize stressful events/adversity as a challenge enabling growth. Such efforts would assist in potentially avoiding the implications of the response to major stressful events being primarily controlled by fear with minimal involvement of reason (logical response) [17, 80, 104]. However, there is a major caveat to this, that is very pertinent to the current COVID-19 pandemic, in regard to how successful and beneficial the above measures could be based on the personal appraisal (challenge vs. threat) of the event by an individual. As previously reported, events that are “high in personal significance and low in controllability” are considered as being a threat (149), and events perceived as a threat may lead to a dysfunctional response. This becomes a grave concern when a significant body of literature pertaining to the impact of the COVID-19 pandemic at the psychological level (including our findings in university students) appears to indicate a predominant global appraisal of the COVID-19 pandemic and related interventions as a threat.
Thus, while this study specifically pertained to the university student population and the COVID-19 pandemic, the implications potentially impact the broader population and events other than the COVID-19 pandemic. Given the lack of a role of positive coping, attention needs to be given to the factors that are outside the individual's control, and the potential role that the factors may play in being sources of stress. Our findings appear to highlight the need for a more integrated psycho-neuro-endocrinological approach that considers the broader well-being of society and avoids the potential significant detrimental ramifications of a reactionary myopic approach to events such as the COVID-19 pandemic, in order to truly and best serve the common good of humanity.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Ethics Statement
The studies involving human participants were reviewed and approved by Franciscan University of Steubenville Institutional Review Board (IRB; #2020-08). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SS supervised the study. SS and CC contributed to the conception, design of the study, conducting of the study, and contributed to manuscript revision. SS, CC, CF, and KO'B performed the statistical analyses and contributed to the writing of the first draft of the manuscript. All authors read and approved the submitted version.
Funding
Funding for this study was provided by Franciscan University of Steubenville. The funders had no role in study design, data collection and analysis, interpretation of results, decision to publish or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.801859/full#supplementary-material
References
2. Centers for Disease Control and Prevention (CDC). Well-Being Concepts [Online]. Centers for Disease Control and Prevention (2018). Available online at: https://www.cdc.gov/hrqol/wellbeing.htm (accessed June 28, 2021).
3. O'Connor CA, Dyson J, Cowdell F, Watson R. Do universal school-based mental health promotion programmes improve the mental health and emotional wellbeing of young people? A literature review. J Clin Nurs. (2018) 27:e412–26. doi: 10.1111/jocn.14078
4. National Institute for Health and Care Excellence (NICE). Early Years: Promoting Health and Wellbeing in Under-5s: QS128 (2016).
5. Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. (2016) 138:e20161878. doi: 10.1542/peds.2016-1878
6. Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. (2019) 128:185–99. doi: 10.1037/abn0000410
7. Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. (2010) 46:3–10. doi: 10.1016/j.jadohealth.2009.08.008
8. Twenge JM, Gentile B, Dewall CN, Ma D, Lacefield K, Schurtz DR. Birth cohort increases in psychopathology among young Americans, 1938-2007: a cross-temporal meta-analysis of the MMPI. Clin Psychol Rev. (2010) 30:145–54. doi: 10.1016/j.cpr,0.2009.10.005
9. Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. College students: 10-year population-level trends (2007-2017). Psychiatr Serv. (2019) 70:60–3. doi: 10.1176/appi.ps.201800332
10. Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. (2004) 101:8174–9. doi: 10.1073/pnas.0402680101
11. Olsson CA, Mcgee R, Nada-Raja S, Williams SM. A 32-year longitudinal study of child and adolescent pathways to well-being in adulthood. J Happiness Stud. (2012) 14:1069–83. doi: 10.1007/s10902-012-9369-8
12. Sarma MS, Kuo PX, Bechayda SA, Kuzawa CW, Gettler LT. Exploring the links between early life and young adulthood social experiences and men's later life psychobiology as fathers. Physiol Behav. (2018) 193:82–9. doi: 10.1016/j.physbeh.2017.11.029
13. Granger TA, Cook PF, Ramos G. Adolescent peer and parent relationships into emerging adulthood. West J Nurs Res. (2020) 42:90–6. doi: 10.1177/0193945919848439
14. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
15. Sussman S, Arnett JJ. Emerging adulthood: developmental period facilitative of the addictions. Eval Health Prof. (2014) 37:147–55. doi: 10.1177/0163278714521812
16. Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO World Mental Health Surveys International College Student Project: prevalence and distribution of mental disorders. J Abnorm Psychol. (2018) 127:623–38. doi: 10.1037/abn0000362
18. Esch T, Stefano GB, Fricchione GL, Benson H. The role of stress in neurodegenerative diseases and mental disorders. Neuro Endocrinol Lett. (2002) 23:199–208.
19. Sadeh A, Keinan G, Daon K. Effects of stress on sleep: the moderating role of coping style. Health Psychol. (2004) 23:542–5. doi: 10.1037/0278-6133.23.5.542
20. Verger P, Guagliardo V, Gilbert F, Rouillon F, Kovess-Masfety V. Psychiatric disorders in students in six French universities: 12-month prevalence, comorbidity, impairment and help-seeking. Soc Psychiatry Psychiatr Epidemiol. (2010) 45:189–99. doi: 10.1007/s00127-009-0055-z
21. Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. (2014) 44:81–121. doi: 10.1007/s40279-013-0090-5
22. Andreassen CS. Online social network site addiction: a comprehensive review. Curr Addict Rep. (2015) 2:175–84. doi: 10.1007/s40429-015-0056-9
23. Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. (2015) 173:90–6. doi: 10.1016/j.jad.2014.10.054
24. Dissing AS, Jorgensen TB, Gerds TA, Rod NH, Lund R. High perceived stress and social interaction behaviour among young adults. A study based on objective measures of face-to-face and smartphone interaction.s PLoS ONE. (2019) 14:e0218429. doi: 10.1371/journal.pone.0218429
25. Bremner JD, Moazzami K, Wittbrodt MT, Nye JA, Lima BB, Gillespie CF, et al. Diet, stress and mental health. Nutrients. (2020) 12:2428. doi: 10.3390/nu12082428
26. Mamun MA, Hossain MS, Moonajilin MS, Masud MT, Misti JM, Griffiths MD. Does loneliness, self-esteem and psychological distress correlate with problematic internet use? A Bangladeshi survey study. Asia Pac Psychiatry. (2020) 12:e12386. doi: 10.1111/appy.12386
27. Stevens C, Zhang E, Cherkerzian S, Chen JA, Liu CH. Problematic internet use/computer gaming among US college students: prevalence and correlates with mental health symptoms. Depress Anxiety. (2020) 37:1127–36. doi: 10.1002/da.23094
28. Vall-Roque H, Andres A, Saldana C. The impact of COVID-19 lockdown on social network sites use, body image disturbances and self-esteem among adolescent and young women. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 110:110293. doi: 10.1016/j.pnpbp.2021.110293
29. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. (2004) 10:1206–12. doi: 10.3201/eid1007.030703
30. Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. (2012) 53:15–23. doi: 10.1016/j.comppsych.2011.02.003
31. Rousseau C, Jamil U, Bhui K, Boudjarane M. Consequences of 9/11 and the war on terror on children's and young adult's mental health: a systematic review of the past 10 years. Clin Child Psychol Psychiatry. (2015) 20:173–93. doi: 10.1177/1359104513503354
32. Shultz JM, Cela T, Marcelin LH, Espinola M, Heitmann I, Sanchez C, et al. The trauma signature of 2016 Hurricane Matthew and the psychosocial impact on Haiti. Disaster Health. (2016) 3:121–38. doi: 10.1080/21665044.2016.1263538
33. Cruz J, White PCL, Bell A, Coventry PA. Effect of extreme weather events on mental health: a narrative synthesis and meta-analysis for the UK. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17228581
34. Ganesan B, Al-Jumaily A, Fong KNK, Prasad P, Meena SK, Tong RK. Impact of Coronavirus Disease 2019 (COVID-19) outbreak quarantine, isolation, and lockdown policies on mental health and suicide. Front Psychiatry. (2021) 12:565190. doi: 10.3389/fpsyt.2021.565190
35. Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. (2020) 29:2047–9. doi: 10.1111/jocn.15296
36. Mheidly N, Fares MY, Fares J. Coping with stress and burnout associated with telecommunication and online learning. Front Public Health. (2020) 8:574969. doi: 10.3389/fpubh.2020.574969
37. Pan Y, Darzi A, Kabiri A, Zhao G, Luo W, Xiong C, et al. Quantifying human mobility behaviour changes during the COVID-19 outbreak in the United States. Sci Rep. (2020) 10:20742. doi: 10.1038/s41598-020-77751-2
38. Bembich S, Tripani A, Mastromarino S, Di Risio G, Castelpietra E, Risso FM. Parents experiencing NICU visit restrictions due to COVID-19 pandemic. Acta Paediatr. (2021) 110:940–1. doi: 10.1111/apa.15620
39. Moehring F, Cowie AM, Menzel AD, Weyer AD, Grzybowski M, Arzua T, et al. Keratinocytes mediate innocuous and noxious touch via ATP-P2X4 signaling. Elife. (2018) 7. doi: 10.7554/eLife.31684
40. Capozzo AV. Dying Alone Due to COVID-19: Do the needs of the many outweigh the rights of the few-or the one? Front Public Health. (2020) 8:593464. doi: 10.3389/fpubh.2020.593464
41. Danilovich MK, Norrick CR, Hill KC, Conroy DE. Nursing home resident weight loss during coronavirus disease 2019 restrictions. J Am Med Dir Assoc. (2020) 21:1568–9. doi: 10.1016/j.jamda.2020.08.032
42. Marroquin B, Vine V, Morgan R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. (2020) 293:113419. doi: 10.1016/j.psychres.2020.113419
43. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–39.e1213. doi: 10.1016/j.jaac.2020.05.009
44. Cortes-Alvarez NY, Pineiro-Lamas R, Vuelvas-Olmos CR. psychological effects and associated factors of COVID-19 in a Mexican sample. Disaster Med Public Health Prep. (2020) 14:413–24. doi: 10.1017/dmp.2020.215
45. Cosic K, Popovic S, Sarlija M, Kesedzic I. Impact of human disasters and COVID-19 pandemic on mental health: potential of digital psychiatry. Psychiatr Danub. (2020) 32:25–31. doi: 10.24869/psyd.2020.25
46. Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1049–57. doi: 10.15585/mmwr.mm6932a1
47. Fiorillo A, Sampogna G, Giallonardo V, Del Vecchio V, Luciano M, Albert U, et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: results from the COMET collaborative network. Eur Psychiatry. (2020) 63:e87. doi: 10.1192/j.eurpsy.2020.89
48. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. (2020) 291:113264. doi: 10.1016/j.psychres.2020.113264
49. Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. (2020) 277:379–91. doi: 10.1016/j.jad.2020.08.043
50. Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. (2020) 66:317–20. doi: 10.1177/0020764020915212
51. Bridgland VME, Moeck EK, Green DM, Swain TL, Nayda DM, Matson LA, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE. (2021) 16:e0240146. doi: 10.1371/journal.pone.0240146
52. El-Monshed AH, El-Adl AA, Ali AS, Loutfy A. University students under lockdown, the psychosocial effects and coping strategies during COVID-19 pandemic: a cross sectional study in Egypt. J Am Coll Health. (2021) 1–12. doi: 10.1080/07448481.2021.1891086
53. Horigian VE, Schmidt RD, Feaster DJ. Loneliness, mental health, and substance use among US young adults during COVID-19. J Psychoactive Drugs. (2021) 53:1–9. doi: 10.1080/02791072.2020.1836435
54. Pretorius T, Padmanabhanunni A. A looming mental health pandemic in the time of COVID-19? Role of fortitude in the interrelationship between loneliness, anxiety, and life satisfaction among young adults. South Afr J Psychol. (2021) 51:256–68. doi: 10.1177/0081246321991030
55. Sacerdote B, Sehgal R, Cook M. Why is all COVID-19 news bad news? NBER. (2020). doi: 10.3386/w28110
56. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. (2020) 4:421. doi: 10.1016/S2352-4642(20)30109-7
57. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
58. Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. (2020) 289:113098. doi: 10.1016/j.psychres.2020.113098
59. Brown SM, Doom JR, Lechuga-Pena S, Watamura SE, Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. (2020) 110:104699. doi: 10.1016/j.chiabu.2020.104699
60. Erdei C, Liu CH. The downstream effects of COVID-19: a call for supporting family wellbeing in the NICU. J Perinatol. (2020) 40:1283–5. doi: 10.1038/s41372-020-0745-7
61. Mazza M, Marano G, Lai C, Janiri L, Sani G. Danger in danger: interpersonal violence during COVID-19 quarantine. Psychiatry Res. (2020) 289:113046. doi: 10.1016/j.psychres.2020.113046
62. Pieh C, T OR, Budimir S, Probst T. Relationship quality and mental health during COVID-19 lockdown. PLoS ONE. (2020) 15:e0238906. doi: 10.1371/journal.pone.0238906
63. Stamu-O'Brien C, Carniciu S, Halvorsen E, Jafferany M. Psychological aspects of COVID-19. J Cosmet Dermatol. (2020) 19:2169–73. doi: 10.1111/jocd.13601
64. Board of Governors of the Federal Reserve System. Report on the Economic Well-Being of U.S. Households in 2019, Featuring Supplemental Data from April 2020 (2020).
65. Barbaglia MG, Ten Have M, Dorsselaer S, Alonso J, De Graaf R. Negative socioeconomic changes and mental disorders: a longitudinal study. J Epidemiol Community Health. (2015) 69:55–62. doi: 10.1136/jech-2014-204184
66. Drydakis N. The effect of unemployment on self-reported health and mental health in Greece from 2008 to 2013: a longitudinal study before and during the financial crisis. Soc Sci Med. (2015) 128:43–51. doi: 10.1016/j.socscimed.2014.12.025
67. Radu MC, Schnakovszky C, Herghelegiu E, Ciubotariu VA, Cristea I. The impact of the COVID-19 pandemic on the quality of educational process: a student survey. Int J Environ Res Public Health. (2020) 17:7770. doi: 10.3390/ijerph17217770
68. Fyllos A, Kanellopoulos A, Kitixis P, Cojocari DV, Markou A, Raoulis V, et al. University students perception of online education: is engagement enough? Acta Inform Med. (2021) 29:4–9. doi: 10.5455/aim.2021.29.4-9
69. Pasion R, Dias-Oliveira E, Camacho A, Morais C, Franco RC. Impact of COVID-19 on undergraduate business students: a longitudinal study on academic motivation, engagement and attachment to university. Account Res J. (2021) 34:246–57. doi: 10.1108/ARJ-09-2020-0286
70. Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol. (2007) 3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520
71. Stanislawski K. The coping circumplex model: an integrative model of the structure of coping with stress. Front Psychol. (2019) 10:694. doi: 10.3389/fpsyg.2019.00694
72. Folkman S, Lazarus RS. Coping as a mediator of emotion. J Pers Soc Psychol. (1988) 54:466–75. doi: 10.1037/0022-3514.54.3.466
73. McMahon EM, Corcoran P, Mcauliffe C, Keeley H, Perry IJ, Arensman E. Mediating effects of coping style on associations between mental health factors and self-harm among adolescents. Crisis. (2013) 34:242–50. doi: 10.1027/0227-5910/a000188
74. Gloria CT, Steinhardt MA. Relationships among positive emotions, coping, resilience and mental health. Stress Health. (2016) 32:145–56. doi: 10.1002/smi.2589
75. Arslan G. Psychological maltreatment, coping strategies, and mental health problems: a brief and effective measure of psychological maltreatment in adolescents. Child Abuse Negl. (2017) 68:96–106. doi: 10.1016/j.chiabu.2017.03.023
76. Groth N, Schnyder N, Kaess M, Markovic A, Rietschel L, Moser S, et al. Coping as a mediator between locus of control, competence beliefs, and mental health: a systematic review and structural equation modelling meta-analysis. Behav Res Ther. (2019) 121:103442. doi: 10.1016/j.brat.2019.103442
77. Xu N, Liu Y. Coping strategy mediates the relationship between body image evaluation and mental health: a study with Chinese college students with disabilities. Disabil Health J. (2020) 13:100830. doi: 10.1016/j.dhjo.2019.100830
78. Arslan G, Yildirim M. Meaning-based coping and spirituality during the COVID-19 pandemic: mediating effects on subjective well-being. Front Psychol. (2021) 12:646572. doi: 10.3389/fpsyg.2021.646572
79. Folkman S, Lazarus RS, Dunkel-Schetter C, Delongis A, Gruen RJ. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. (1986) 50:992–1003. doi: 10.1037/0022-3514.50.5.992
80. Rom O, Reznick AZ. The stress reaction: a historical perspective. In: Pokorski M, editor. Respiratory Contagion. Cham: Springer International Publishing (2016). p. 1–4. doi: 10.1007/5584_2015_195
81. Iida M, Gleason M, Green-Rapaport AS, Bolger N, Shrout PE. The influence of daily coping on anxiety under examination stress: a model of interindividual differences in intraindividual change. Pers Soc Psychol Bull. (2017) 43:907–23. doi: 10.1177/0146167217700605
82. Gidron Y, Nyklicek I. Experimentally testing Taylor's stress, coping and adaptation framework. Anxiety Stress Coping. (2009) 22:525–35. doi: 10.1080/10615800902755536
83. Kopp CB. Emotion-focused coping in young children: self and self-regulatory processes. New Dir Child Adolesc Dev. (2009) 2009:33–46. doi: 10.1002/cd.241
84. Lloyd J, Muers J, Patterson TG, Marczak M. Self-compassion, coping strategies, and caregiver burden in caregivers of people with dementia. Clin Gerontol. (2018) 42:47–59. doi: 10.1080/07317115.2018.1461162
85. Anzaldi K, Shifren K. Optimism, pessimism, coping, and depression: a study on individuals with Parkinson's disease. Int J Aging Hum Dev. (2019) 88:231–49. doi: 10.1177/0091415018763401
86. Al-Yateem N, Subu MA, Al-Shujairi A, Alrimawi I, Ali HM, Hasan K, et al. Coping among adolescents with long-term health conditions: a mixed-methods study. Br J Nurs. (2020) 29:762–9. doi: 10.12968/bjon.2020.29.13.762
87. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Psychology Foundation Monograph (2004).
88. Lovibond PF, Lovibond SH. The structure of negative emotional states - comparison of the Depression Anxiety Stress Scales (Dass) with the beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
89. Weiss DS, Marmar CR. The impact of event scale – revised. In: Wilson JP, Keane TM. Assessing Psychological Trauma and PTSD. New York, NY: Guilford Press (1997). p. 399–411.
90. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. (2007) 52:233–40. doi: 10.1177/070674370705200405
91. Weiss DS. The impact of event scale-revised. In: Wilson JP, Keane TM. Assessing Psychological Trauma and PTSD: A Practitioner's Handbook. 2nd ed. New York, NY: Guildford Press (2007). p. 168–89.
92. U. S., and Department of Homeland Security CISA. Guidance on the Essential Critical Infrastructure Workforce: Ensuring Community and National Resilience in COVID-19 Response Version 2.0. (2020).
93. Dart J, Gallois C, Yellowlees P. Community health information sources–a survey in three disparate communities. Aust Health Rev. (2008) 32:186–96. doi: 10.1071/AH080186
94. Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
95. Cooper C, Katona C, Livingston G. Validity and reliability of the brief COPE in carers of people with dementia: the LASER-AD Study. J Nerv Ment Dis. (2008) 196:838–43. doi: 10.1097/NMD.0b013e31818b504c
96. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
97. Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. (2002) 7:422–45. doi: 10.1037/1082-989X.7.4.422
98. Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. In: Practical Assessment Research and Evaluation. (2005). p. 10. Available online at: http://pareonline.net/getvn.asp?v=10andn=7 (accessed September 24, 2021).
99. Baglin J. Improving your exploratory factor analysis for ordinal data: a demonstration using FACTOR. In: Practical Assessment Research and Evaluation. (2014). p. 19. Available online at: http://pareonline.net/getvn.asp?v=19andn=5 (accessed September 24, 2021).
100. Kawamura N, Kim Y, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry. (2001) 158:484–6. doi: 10.1176/appi.ajp.158.3.484
101. Asukai N, Kato H, Kawamura N, Kim Y, Yamamoto K, Kishimoto J, et al. Reliability and validity of the Japanese-language version of the impact of event scale-revised (IES-R-J): four studies of different traumatic events. J Nerv Ment Dis. (2002) 190:175–82. doi: 10.1097/00005053-200203000-00006
102. Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - revised. Behav Res Ther. (2003) 41:1489–96. doi: 10.1016/j.brat.2003.07.010
103. Mohr C, Braun S, Bridler R, Chmetz F, Delfino JP, Kluckner VJ, et al. Insufficient coping behavior under chronic stress and vulnerability to psychiatric disorders. Psychopathology. (2014) 47:235–43. doi: 10.1159/000356398
104. Delfino JP, Barragan E, Botella C, Braun S, Bridler R, Camussi E, et al. Quantifying insufficient coping behavior under chronic stress: a cross-cultural study of 1,303 students from Italy, Spain and Argentina. Psychopathology. (2015) 48:230–9. doi: 10.1159/000381400
105. Lazarus RS. The psychology of stress and coping. Issues Ment Health Nurs. (1985) 7:399–418. doi: 10.3109/01612848509009463
106. Viana Machado A, Volchan E, Figueira I, Aguiar C, Xavier M, Souza GGL, et al. Association between habitual use of coping strategies and posttraumatic stress symptoms in a non-clinical sample of college students: a Bayesian approach. PLoS ONE. (2020) 15:e0228661. doi: 10.1371/journal.pone.0228661
107. Yildirim M, Arslan G, Alkahtani AM. Do fear of COVID-19 and religious coping predict depression, anxiety, and stress among the Arab population during health crisis? Death Stud. (2021) 1–7. doi: 10.1080/07481187.2021.1882617
108. Welwood J. Principles of inner work - psychological and spiritual. J Transpers Psychol. (1984) 16:63–73.
109. Dimmer SA, Carroll JL, Wyatt GK. Uses of humor in psychotherapy. Psychol Rep. (1990) 66:795–801. doi: 10.2466/pr0.1990.66.3.795
110. Olson MM, Trevino DB, Geske JA, Vanderpool H. Religious coping and mental health outcomes: an exploratory study of socioeconomically disadvantaged patients. Explore. (2012) 8:172–6. doi: 10.1016/j.explore.2012.02.005
111. Parenteau SC. Religious coping and substance use: the moderating role of sex. J Relig Health. (2017) 56:380–7. doi: 10.1007/s10943-015-0166-7
112. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. (2007) 87:873–904. doi: 10.1152/physrev.00041.2006
113. McEwen BS. Neurobiological and systemic effects of chronic stress. Chronic Stress. (2017) 1:2470547017692328. doi: 10.1177/2470547017692328
114. Koob GF, Schulkin J. Addiction and stress: an allostatic view. Neurosci Biobehav Rev. (2019) 106:245–62. doi: 10.1016/j.neubiorev.2018.09.008
115. Keay KA, Bandler R. Parallel circuits mediating distinct emotional coping reactions to different types of stress. Neurosci Biobehav Rev. (2001) 25:669–78. doi: 10.1016/S0149-7634(01)00049-5
116. Fee C, Prevot T, Misquitta K, Banasr M, Sibille E. Chronic stress-induced behaviors correlate with exacerbated acute stress-induced cingulate cortex and ventral hippocampus activation. Neuroscience. (2020) 440:113–29. doi: 10.1016/j.neuroscience.2020.05.034
117. Hu P, Liu J, Maita I, Kwok C, Gu E, Gergues MM, et al. Chronic stress induces maladaptive behaviors by activating corticotropin-releasing hormone signaling in the mouse oval bed nucleus of the stria terminalis. J Neurosci. (2020) 40:2519–37. doi: 10.1523/JNEUROSCI.2410-19.2020
118. Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. (2004) 130:601–30. doi: 10.1037/0033-2909.130.4.601
119. Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation. (2009) 16:300–17. doi: 10.1159/000216188
120. Raony I, De Figueiredo CS, Pandolfo P, Giestal-De-Araujo E, Oliveira-Silva Bomfim P, Savino W. Psycho-neuroendocrine-immune interactions in COVID-19: potential impacts on mental health. Front Immunol. (2020) 11:1170. doi: 10.3389/fimmu.2020.01170
121. Hammen C, Kim EY, Eberhart NK, Brennan PA. Chronic and acute stress and the prediction of major depression in women. Depress Anxiety. (2009) 26:718–23. doi: 10.1002/da.20571
122. McEwen BS, Eiland L, Hunter RG, Miller MM. Stress and anxiety: structural plasticity and epigenetic regulation as a consequence of stress. Neuropharmacology. (2012) 62:3–12. doi: 10.1016/j.neuropharm.2011.07.014
123. Sommershof A, Scheuermann L, Koerner J, Groettrup M. Chronic stress suppresses anti-tumor TCD8+ responses and tumor regression following cancer immunotherapy in a mouse model of melanoma. Brain Behav Immun. (2017) 65:140–9. doi: 10.1016/j.bbi.2017.04.021
124. Madison AA, Shrout MR, Renna ME, Kiecolt-Glaser JK. Psychological and behavioral predictors of vaccine efficacy: considerations for COVID-19. Perspect Psychol Sci. (2021) 16:191–203. doi: 10.1177/1745691621989243
125. Helmreich DL, Tylee D, Christianson JP, Kubala KH, Govindarajan ST, O'Neill WE, et al. Active behavioral coping alters the behavioral but not the endocrine response to stress. Psychoneuroendocrinology. (2012) 37:1941–8. doi: 10.1016/j.psyneuen.2012.04.005
126. Wadsworth ME. Development of maladaptive coping: a functional adaptation to chronic, uncontrollable stress. Child Dev Perspect. (2015) 9:96–100. doi: 10.1111/cdep.12112
127. Grossi G, Perski A, Evengård B, Blomkvist V, Orth-Gomér K. Physiological correlates of burnout among women. J Psychosom Res. (2003) 55:309–16. doi: 10.1016/S0022-3999(02)00633-5
128. McCain RS, McKinley N, Dempster M, Campbell WJ, Kirk SJ. A study of the relationship between resilience, burnout and coping strategies in doctors. Postgrad Med J. (2017). doi: 10.1136/postgradmedj-2016-134683
129. Esterwood E, Saeed SA. Past Epidemics, Natural Disasters, COVID19, and mental health: learning from history as we deal with the present and prepare for the future. Psychiatr Q. (2020) 91:1121–33. doi: 10.1007/s11126-020-09808-4
131. Glober N, Mohler G, Huynh P, Arkins T, O'Donnell D, Carter J, et al. Impact of COVID-19 pandemic on drug overdoses in indianapolis. J Urban Health. (2020) 97:802–7. doi: 10.1007/s11524-020-00484-0
132. Haley DF, Saitz R. The opioid epidemic during the COVID-19 pandemic. JAMA. (2020) 324:1615–7. doi: 10.1001/jama.2020.18543
133. Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. (2020) 214:108176. doi: 10.1016/j.drugalcdep.2020.108176
134. Janaskie A, Earle PC. The Devastating Economic Impact of Covid-19 Shutdowns. American Institute for Economic Research (2020). Available online at: https://www.aier.org/article/the-devastating-economic-impact-of-covid-19-shutdowns/
135. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
136. Gismero-Gonzalez E, Bermejo-Toro L, Cagigal V, Roldan A, Martinez-Beltran MJ, Halty L. Emotional impact of COVID-19 lockdown among the Spanish population. Front Psychol. (2020) 11:616978. doi: 10.3389/fpsyg.2020.616978
137. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. (2020) 12:1583. doi: 10.3390/nu12061583
138. Schwendinger F, Pocecco E. Counteracting physical inactivity during the COVID-19 pandemic: evidence-based recommendations for home-based exercise. Int J Environ Res Public Health. (2020) 17:3909. doi: 10.3390/ijerph17113909
139. Sepulveda-Loyola W, Rodriguez-Sanchez I, Perez-Rodriguez P, Ganz F, Torralba R, Oliveira DV, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging. (2020) 24:938–47. doi: 10.1007/s12603-020-1500-7
140. Mandelkorn U, Genzer S, Choshen-Hillel S, Reiter J, Meira ECM, Hochner H, et al. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. (2021) 17:45–53. doi: 10.5664/jcsm.8800
141. Morin CM, Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med. (2021) 77:346–7. doi: 10.1016/j.sleep.2020.06.005
142. Giubilini A, Gupta S, Heneghan C. A focused protection vaccination strategy: why we should not target children with COVID-19 vaccination policies. J Med Ethics. (2021) 47:565–6. doi: 10.1136/medethics-2021-107700
143. Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. (2007) 20:359–64. doi: 10.1097/YCO.0b013e32816ebc8c
144. Maria AN, Ahmmed SU. Graduating into a pandemic: exploring the factors influencing the anxiety level of the university finalists. Shanlax Int J Educ. (2020) 9:68–75. doi: 10.34293/education.v9i1.3508
145. Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students' mental health in the united states: interview survey study. J Med Internet Res. (2020) 22:e21279. doi: 10.2196/21279
146. Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2020) 22:e22817. doi: 10.2196/22817
147. Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2025591. doi: 10.1001/jamanetworkopen.2020.25591
148. Jacob L, Smith L, Armstrong NC, Yakkundi A, Barnett Y, Butler L, et al. Alcohol use and mental health during COVID-19 lockdown: a cross-sectional study in a sample of UK adults. Drug Alcohol Depend. (2021) 219:108488. doi: 10.1016/j.drugalcdep.2020.108488
Keywords: COVID-19, mental health, depression, anxiety, stress, coping, impact of event, university students
Citation: Camilleri C, Fogle CS, O'Brien KG and Sammut S (2022) The Impact of COVID-19 and Associated Interventions on Mental Health: A Cross-Sectional Study in a Sample of University Students. Front. Psychiatry 12:801859. doi: 10.3389/fpsyt.2021.801859
Received: 25 October 2021; Accepted: 27 December 2021;
Published: 26 January 2022.
Edited by:
Christos Theleritis, National and Kapodistrian University of Athens, GreeceReviewed by:
Walter Schumm, Kansas State University, United StatesFrancisco Manuel Morales Rodríguez, University of Granada, Spain
Copyright © 2022 Camilleri, Fogle, O'Brien and Sammut. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephen Sammut, c3NhbW11dEBmcmFuY2lzY2FuLmVkdQ==
†These authors have contributed equally to this work
 Christina Camilleri
Christina Camilleri Cole S. Fogle
Cole S. Fogle Kathryn G. O'Brien
Kathryn G. O'Brien Stephen Sammut
Stephen Sammut