
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 03 December 2021
Sec. Sleep Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.791342
This article is part of the Research TopicSleep, Vigilance & Disruptive BehaviorsView all 15 articles
 Leila Karimi1†
Leila Karimi1† Farshid Rahimi-Bashar2†
Farshid Rahimi-Bashar2† Seyyede Momeneh Mohammadi3†
Seyyede Momeneh Mohammadi3† Mohsen Mollahadi4†
Mohsen Mollahadi4† Masoum Khosh-Fetrat5†
Masoum Khosh-Fetrat5† Amir Vahedian-Azimi6†
Amir Vahedian-Azimi6† Sara Ashtari7*†
Sara Ashtari7*†Using physical devices such as eye masks and earplugs to improve to the quality of sleep in intensive care units (ICUs) is a very important issue. This study was conducted to assess the efficacy of eye masks and earplugs for sleep promotion in critically ill adult patients in the ICU based on various sleep quality assessment tools. PubMed, Scopus, Web of Science, and ProQuest were systematically retrieved until May 2021. Both randomized and non-randomized experimental and quasi-experimental studies were included if they evaluated the efficacy of eye masks and earplugs interventions on sleep outcomes in critically ill patients. The methodological quality was assessed by the Joanna Briggs Institute (JBI) critical appraisal tool. For the main outcome (sleep quality), a mean difference (MD) and confidence intervals (CIs) of 95% were determined. A total of 2,687 participants from 35 studies met the inclusion criteria. Twenty one studies were included in meta-analysis and 14 studies were included in the qualitative analysis. According to the results based on sleep quality assessment tools; overall scores of Pittsburgh Sleep Quality Index (PSQI) and Richards-Campbell Sleep Questionnaire (RCSQ), eye mask and/or earplug interventions have a positive effect on sleep quality. Based on Verran-Snyder-Halpern Sleep Scale (VSHSS), sleep disturbance was significantly lower in the intervention groups. In terms of polysomnography, the use of eye masks and/or earplugs resulted in a significant increase in total sleep time, sleep efficiency, rapid eye movement (REM) time, significant reduction of awaking, and sleep arousals index. The results of the present study suggest that the use of earplugs or eye masks, separately or combined affects sleep improvement in critically ill patients.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=145830, PROSPERO: CRD42020145830.
Sleep in critical care settings was demonstrated to be of a poor quality, which is associated to both environmental-related factors (artificial light, ambient noise, alarms from monitoring devices, patient-care activities monitoring, diagnostic, and therapeutic procedures) and patients-related factors (old age, underlying diseases, pain, stress, psychosis, circadian rhythm disturbances, and organ dysfunction) (1, 2). Evidence suggests that the poor quality sleep in critically ill patients can cause both psychological and physiological consequences and also affect the recovery and treatment (3). Sleep disturbances may reduce immunodeficiency function, inspiratory muscle endurance, alter patients' weaning patterns, cardiorespiratory status, and increased pain scores in critically ill patients (4). In addition, it can leads to negative psychological states such as agitation, confusion and delirium (5, 6).
Sleep promotion interventions include both pharmacological and non-pharmacological treatments. Pharmacological agents that induce sleep provide sedation and analgesia and are commonly used in the ICU setting (7). However, pharmacological interventions can have negative side effects such as impaired cognitive function, the risk of tolerance or dependency, decreased ventilation, and a disruption in normal sleep physiology (8). Additionally, drug-induced sleep is contraindicated in certain patient groups, such as non-ventilated patients with hypercapnic lung disease (9). Therefore, today there is more emphasis and recommendation on non-pharmacological interventions. However, non-pharmacological interventions for improving sleep have been found to be less effective than pharmacological methods while posing no risk of drug-related tolerance or dependency (4, 10). Several non-pharmacological interventions including utilizing physical devices (eye masks and/or earplugs), relaxation techniques (massage and foot baths), music interventions, quiet time, acupuncture, and aromatherapy were attempt to improve to the quality of sleep in ICU (10).
Evidence shows that light and noise are the main cause of sleep disorders in the ICU (11, 12). Hence, it seems that the use of eye masks and earplugs as a low-cost intervention methods of noise reduction and light control can be superior to other interventions. Several studies found that the use of earplugs and eye masks improved sleep quality (13, 14). In addition, two systematic reviews by Alway et al. (15), and Locihova et al. (16), have highlighted benefits of earplugs and eye masks for improving sleep. But so far no meta-analysis has been done in this field. Therefore, we conducted this study to examine the efficacy of eye masks and earplugs for sleep promotion in critically ill patients based on various sleep quality assessment tools.
This study was carried out in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines and recommendation by the Cochrane Collaboration for programming and conducting systematic reviews and meta-analyses (17, 18). Ethical approval was obtained from the research ethics committee of Baqiyatallah University of Medical Sciences with the ethics code of IR.BMSU.REC.1398.175. In addition, this systematic review has also been registered in international prospective register of systematic reviews (PROSPERO) with the registry code of CRD42020145830. Extensive electronic search was done in the following databases and search engines: PubMed, Scopus, Web of Science, and ProQuest. Combination of medical subject heading (Mesh terms) or synonyms, “eye masks,” “earplugs,” and “sleep” were used for carrying out literature search until May 2021 without restrictions in date and countries. Relevant articles in the reference lists of all included published articles were also searched manually. The full search strategy is available in Supplementary Material 1.
Studies were eligible if they met all of the following inclusion criteria: (i) types of studies: randomized controlled trials (RCTs), randomized crossover studies, cluster randomized trials, and randomized or non-randomized quasi experimental (we included all studies, published or unpublished, in English and Persian language); (ii) types of participants: adult patients with stable hemodynamic condition who were admitted to ICUs, critical care units (CCUs), or in a simulated ICU conditions that is completely similar in terms of sound and light with no restrictions on gender or ethnicity; (iii) types of intervention: using eye mask and/or earplugs for improving sleep quality compare to routine standard care; (iv) outcome: the outcome measure sleep quality, which was measured by using standardized instruments including objective and/or subjective tools. Studies were excluded if they (i) enrolling participants who were diagnosed with obstructive sleep apnea or dementia or those who were terminally ill or required palliative care; (ii) conference articles, abstracts and protocols; (iii) examined a combination of other interventions (e.g., massage, foot baths, nursing interventions, valerian acupressure, and aromatherapy).
Two investigators (S.A, A.V-A) independently screened the full-text of the articles to select the studies satisfying the inclusion criteria. Then, the data and information were extracted according to the following study characteristics required for the current review; (a) general information: first author name, publication year and country; (b) method information: study design, study setting, study participants and sample size; (c) intervention: intervention type and assessment tools for sleep quality; (d) outcome: results of sleep quality. Any disagreements during this selection and extraction process were resolved either through consensus or consultation with third investigator (F.R-B).
The quality assessment was performed by utilizing the Joanna Briggs Institute (JBI) critical appraisal tool (https://jbi.global/critical-appraisal-tools) for quasi-experimental and RCT studies, separately. Two reviewers independently assessed the risk of bias in each study. The RCT and quasi-experimental were evaluated based on 13 and nine criteria, respectively. All questions were answered as yes, no, not clear, or not applicable and assessed individually. Eligible studies were rated according to the dictionary and guidelines of the tool. After evaluating all the components of the study, the overall rating was determined using the criteria set out in the tool. Based on the number of “yes” responses, a rating of good = (≥10 yes), medium = (6–9 yes), and poor = (≤ 5 yes) was assigned to each RCT studies. For quasi-experimental studies, a rating of good = (≥7 yes), medium = (4–6), and poor = (≤ 3 yes) was assigned for nine questions (Supplementary Material 1).
The statistical analyses were conducted by STATA 16.0 (STATA Corp; College Station, Texas, USA) software. Included studies used different scales and instruments to measure sleep quality. Meta-analyses performed if outcomes from two or more studies with similar sleep quality assessment tool were available. To compare the use of earplugs or eye masks or both vs. no use of earplugs or eye masks, we used the mean difference (MD) with a 95% confidence interval (CI) for continuous data. Random effects models were performed to balance the effect quantity of each study. Statistical heterogeneity was assessed by I2, with I2 > 75% regarded as high heterogeneity. P < 0.05 was considered statistically significant. Moreover, to assess the publication bias, the Egger's (19) and Begg's (20) tests were conducted.
The literature search results and the screening process are summarized in Figure 1. The search strategy yielded 93 records. A total of 37 records were excluded because they did not meet all predefined inclusion criteria or were duplicated. Moreover, we reviewed the bibliographies of the retrieved articles and found three more relevant studies. Fifty-nine full-text articles were evaluated for eligibility. Twenty-four studies were excluded due to unclear methodology, involve the use of eye masks and earplugs as part of a multimodal intervention, and lack of adequate control group. Thus, 35 full-text articles with 2,678 participants were included in the study. Meta-analyses were performed if outcomes from two or more studies with similar scales and sleep quality assessment tool were available. Therefore, 21 studied were included in the meta-analysis and the others (14 studies) were included in the qualitative analysis.
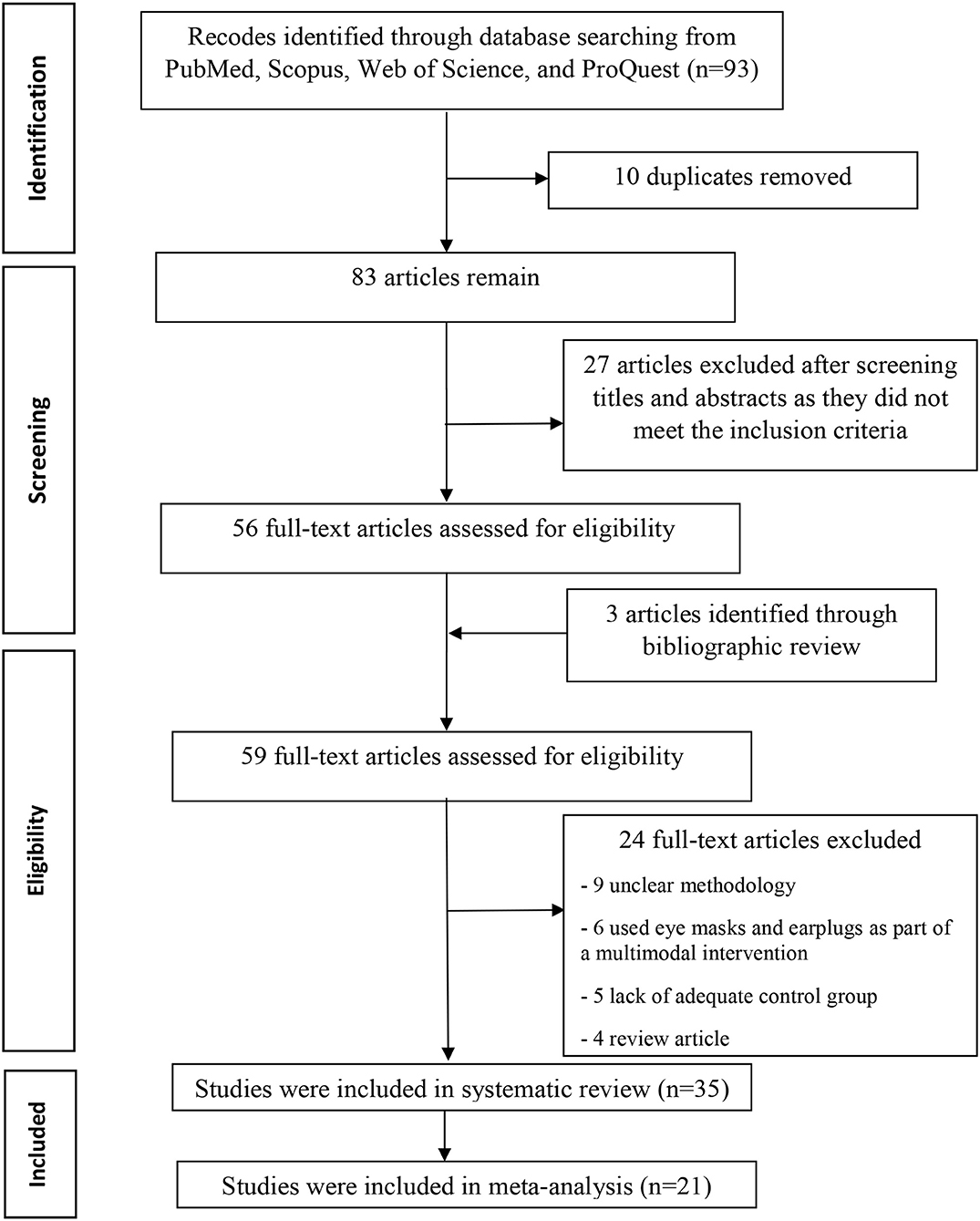
Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) flowchart detailing the disposition of screened, included, and excluded records.
The characteristics of selected studies are presented in Table 1. The studies were conducted in USA (14, 21, 36, 48, 50, 51), UK (13, 22, 43), Belgium (23), China (24, 25, 27, 38), Iran (26, 28–32, 35, 39, 42, 49), France (33, 34), India (37, 41, 46), Australia (40), Jordan (44), Canada (45), Turkey (47), Egypt (52), and Singapore (53). Twenty eligible studies were RCTs (23, 24, 26, 28, 29, 33–35, 37–43, 46, 48, 51–53), six were randomized quasi-experimental (3, 21, 25, 27, 30), four were pre-post studies (5, 22, 31, 47), two were randomized cross-over studies (32, 49), and three were non-randomized quasi-experimental (13, 14, 45). Twenty-four trials were conducted in ICU which including medical ICU (5, 41, 46), cardiac ICU (13), general ICU (22, 33, 37, 44, 53), surgical ICU (32, 40, 48, 51), mixed medical and surgical ICU (23, 43), mixed medical and cardiac ICU (14), mixed medical and general ICU (42, 45, 50), neurology ICU (47), cardiac surgery intensive care unit (CSICU) (24, 52), and post-anesthesia care units (PACUs) (34). Nine trials were conducted in coronary care unit (CCU) (26–31, 35, 39, 49), and three trials were conducted in simulated ICU environment among healthy subjects (21, 25, 38).
Several sleep assessment tools have been used in the reviewed studies. The majority of the publications used subjective tools, while only five of them employed the form of objective evaluation (21, 25, 33, 38, 46). Polysomnography (PSG) was the only form of objective method of assessment that used in these studies. Among the subjective tools for sleep evaluation, the Richards- Campbell Sleep Questionnaire (RCSQ) (5, 24, 44, 46–48, 51–54), and the Verran and Snyder-Halpern Sleep Scale (VSHSS) (14, 27, 31, 32, 37, 42, 45, 49) were the most frequently used in 11 and eight studies, respectively. Five trials used Pittsburgh sleep quality index (PSQI) as sleep assessment tool (26, 28, 29, 35, 39). Five studies (13, 22, 23, 41, 43), used their original sleep questionnaires. In addition, three studies used variable assessment tools such as Medical Outcomes Study Sleep (MOSS) score (34), Insomnia Severity Index (ISI) questionnaire (50), and Leeds Sleep Evaluation Questionnaire (LSEQ) (30).
Five studies (26, 28, 29, 35, 39) with 312 participants (156 patients in each control and treatment group), reported data on sleep outcomes using the PSQI scale. A study by Babaii et al. (35), reported the overall scale of PSQI via median (IQR), while the others reported by mean (SD). Thus, the meta-analysis was performed in the four studies (26, 28, 29, 39), and the qualitative analysis was conducted in the latter one study because the data of them could not be combined. A total PSQI score ranges from 0 to 21. A higher score suggests worse overall sleep quality, and a total cut-off PSQI score < 5 indicates good sleep (55). The meta-analysis of combined data conducted, showed a positive effect of used eye masks and/ or earplugs interventions on overall sleep quality based on PSQI score (MD= −5.02, 95% CI = −6.16 to −3.89, P < 0.001), with substantially heterogeneity among the studies (I2 = 59.01%, P = 0.07) (Figure 2A). The result revealed that the average PSQI score of the eye masks and/ or earplugs group was 5.02 points lower than that of the control group and indicating that the interventions might be beneficial to improve overall sleep quality. P-values of Egger and Begg tests indicated non-significant coefficient values for publication bias (Egger test: P = 0.635 and Begg test: P = 0.065) (Figure 2B). The PSQI scale consists of seven components including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medications, and daytime dysfunction. Three studies (26, 28, 29), provided the data on the PSQI components, thus the meta-analyses were conducted to explore the efficacy of eye masks and/or earplugs interventions on sleep components, as shown in Table 2. No significant results were obtained for sleep components based on PSQI score (P > 0.05) (Supplementary Figures 1–3).
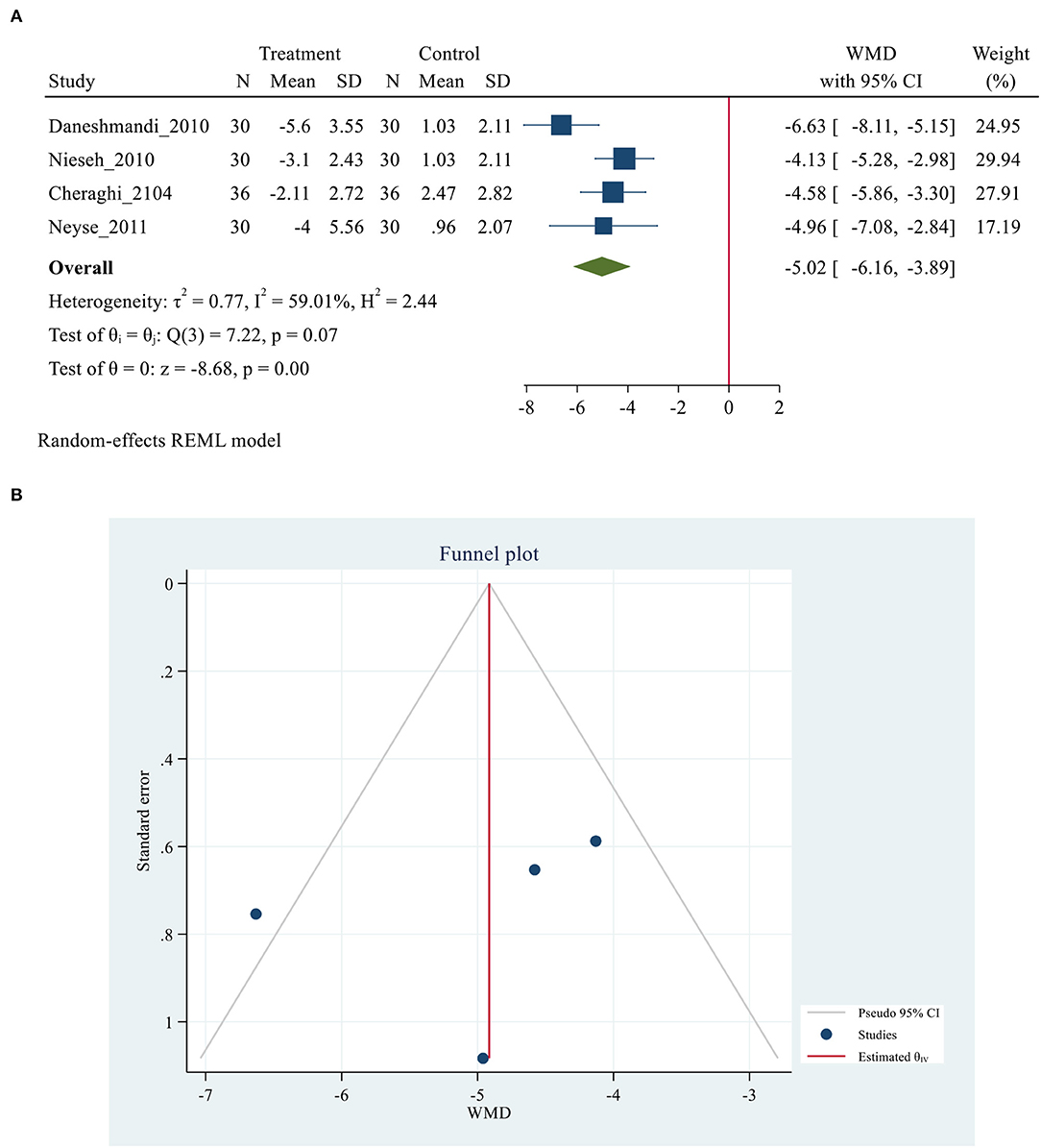
Figure 2. (A) Forest plot of mean difference (MD) for sleep quality based on PSQI between intervention and control groups. (B) Funnel plot showing publication bias on PSQI -based sleep quality.
Ten studies (3, 5, 24, 40, 46–48, 51–53), with 1,078 participants (568 and 510 patients in the intervention and control group, respectively), reported data on sleep outcomes using the RCSQ scale. RCSQ responses were graded on a 0–100 mm visual analog scale, with higher scores indicating better sleep. A score of 0–25 indicates poor sleep, while a score of 76–100 indicates good sleep (56). The RCSQ mean score of 11 studies for intervention groups was significantly higher than the mean score of the control groups (55.01 ± 15.43 vs. 40.15 ± 14.71, P = 0.007). The meta-analysis demonstrated a positive effect of using eye masks and/or earplugs on overall sleep quality based on RCSQ (MD = 11.46, 95% CI = 7.04–15.88, P < 0.001). However, substantial heterogeneity was also observed across the studies (I2 = 88.70%. P < 0.001). The results showing that the average RCSQ score of the treatment group was 11.46 points higher than that of the control group and indicating that the intervention might be beneficial to improve overall sleep quality based on RCSQ score in critically ill patients (Figure 3A). P-values of Egger and Begg tests indicated non-significant coefficient values for publication bias (Egger test: P = 0.269 and Begg test: P = 0.692) (Figure 3B). The RCSQ is a 5-item questionnaire that is used to assess sleep depth, latency, number of awakenings, efficiency, and sleep quality. Five studies (3, 24, 40, 48, 52), provided the data on the five-subdomain of RCSQ, thus the meta-analyses were conducted to explore the efficacy of eye masks and/or earplugs interventions on sleep subdomains based on RCSQ, as shown in Table 3. Significant results were obtained for all subdomains; sleep depth (MD = 9.88, 95% CI = 7.97–11.80, P < 0.001), sleep latency (MD = 13.17, 95% CI = 7.45–18.9, P < 0.001), number of awakenings (MD = 10.87, 95% CI = 8.90–12.84, P < 0.001), sleep efficiency (MD = 15.36, 95% CI = 7.27–23.46, P < 0.001), and sleep quality (MD = 12.59, 95% CI = 6.50–18.68, P < 0.001) (Supplementary Figures 4–6).
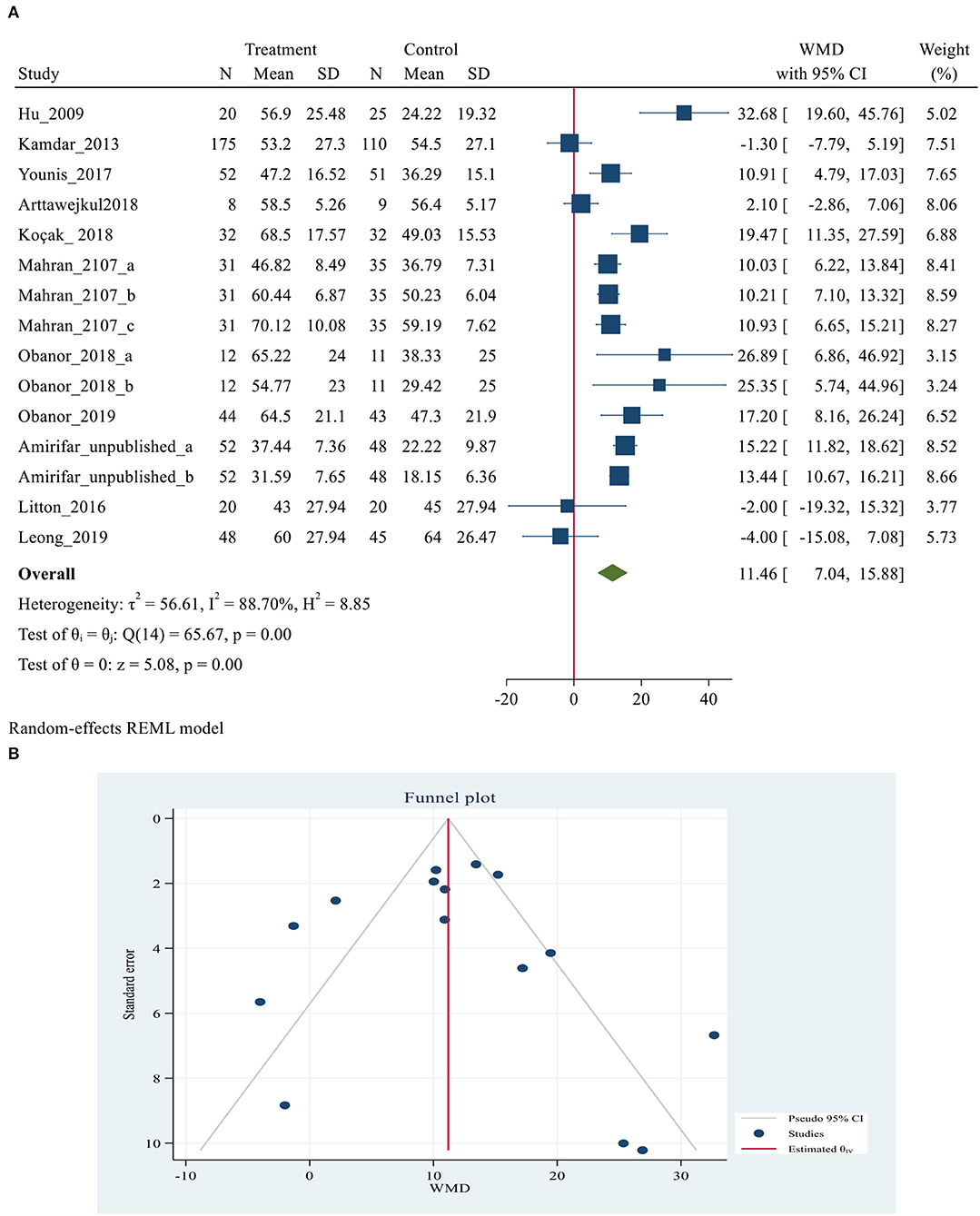
Figure 3. (A) Forest plot of mean difference (MD) for sleep quality based on RCSQ between intervention and control groups. (B) Funnel plot showing publication bias on RCSQ -based sleep quality.
Eight studies (14, 27, 31, 32, 37, 42, 45, 49), with 606 participants (307 and 299 patients in the intervention and control group, respectively), reported data on sleep outcomes using the VSHSS scale. Of these 8 studies, only three studies (31, 32, 49), were able to combine their data and implement meta-analysis on them. The VSHSS scale is a visual scale that evaluates the three domains of sleep disturbance (Seven items), effectiveness (Five items) and supplementary sleep (Four items) with separate scoring. Each item is answered by marking the samples on a graded vector with scores varies from 0 to 100 mm (57). Lower scores in sleep disturbance and supplementary sleep and higher scores in the effectiveness of sleep domains indicate a more satisfying sleep quality (57). Three trials reported the sleep disturbance and effectiveness sleep domains (31, 32, 49). However, only two trials reported the supplementary sleep domain via VSHSS (31, 49). The meta-analysis demonstrated a positive effect of using eye masks and/or earplugs on domains of sleep disturbance (MD = −19.82, 95% CI= −35.54−4.11, P < 0.001). However, substantial heterogeneity was also observed across the studies (I2 = 95.67%. P < 0.001). The result showing that the average of sleep disturbance of the treatment group was 19.82 points lower than that of the control group and indicating that the interventions might be beneficial to improve sleep disturbance in critically ill patients (Figure 4A). However, no significant differences were obtained for effectiveness and supplementary sleep domain between treatment and control groups (Figures 4B,C). P-values of Egger and Begg tests indicated non-significant coefficient values for publication bias for sleep disturbance (Egger test: P = 0.067 and Begg test: P = 0.111), effectiveness (Egger test: P = 0.052 and Begg test: P = 0.067), and supplementary sleep (Egger test: P = 0.063 and Begg test: P = 0.296).
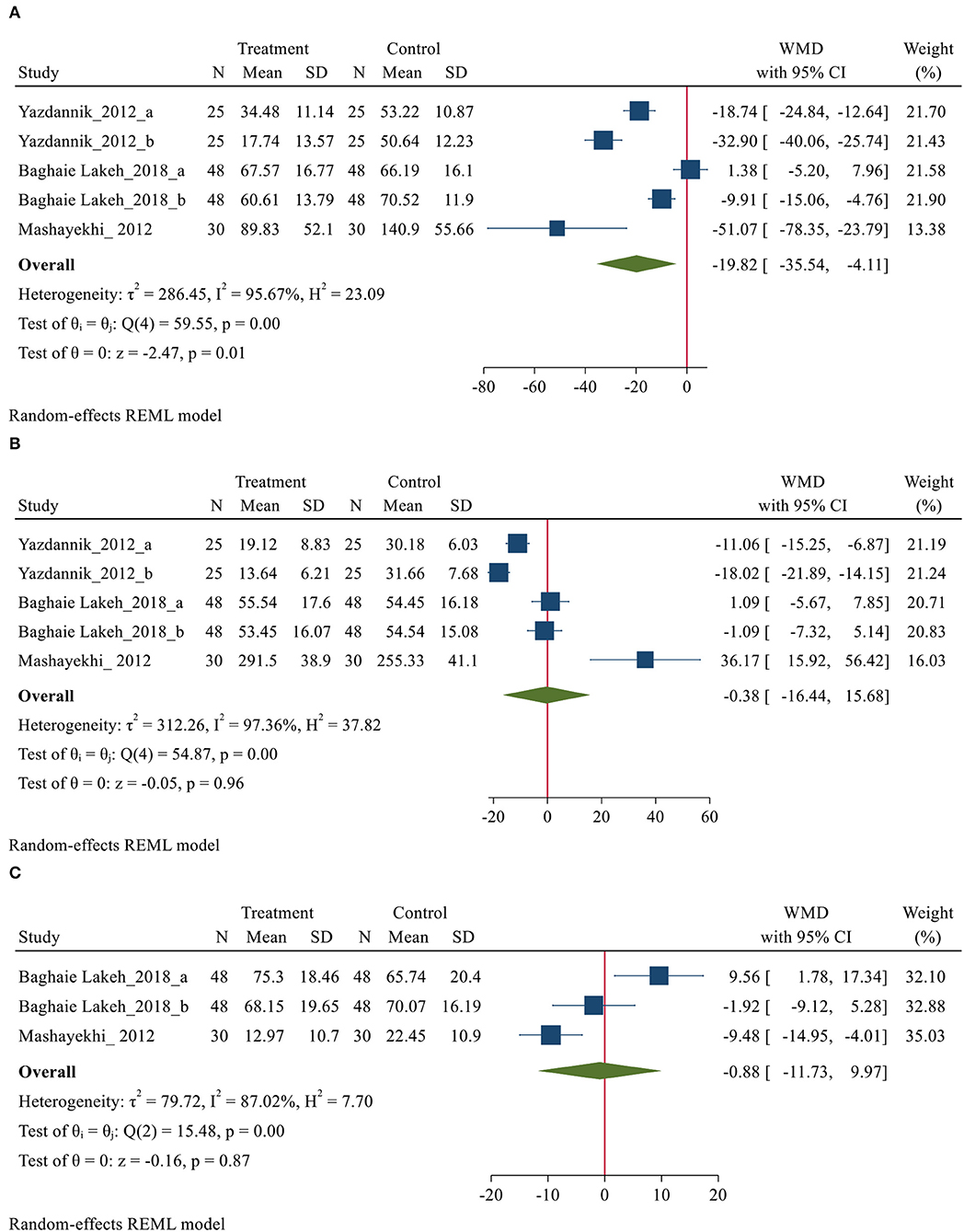
Figure 4. Forest plot of mean difference (MD) for sleep quality domains based on VSHSS between intervention and control groups, (A) disturbance; (B) effectiveness and (C) supplementary.
Five studies (21, 25, 33, 38, 46), with 128 participants (61 and 67 subjects in the intervention and control group, respectively), reported data on sleep outcomes using PSG. Three studies were performed in simulated ICU environment among healthy individuals and reported the outcomes on the mean (SD) scale (21, 25, 38). While two other studies have been done in the ICU and reported the results at different scales (33, 46). Therefore, meta-analysis was performed in three studies that could combine data (21, 25, 38). According to the results of these studies, sleep in simulated ICU environment was shown to be significantly fragmented, with prolonged sleep latencies, frequent arousals, a reduction or absence of rapid eye movement (REM) stage of sleep, an increase in stage 2 of non-REM sleep, and a reduction or absence of deep or slow-wave stage 3 of non-REM sleep. The pooled analyses were conducted to explore the efficacy of eye masks and/or earplugs interventions on sleep quality based on PSG, as shown in Table 4. Meta-analysis findings showed that the use of eye masks and/or earplugs resulted in a significant increase in total sleep time (MD = 25.47, 95% CI = 8.05–42.90, P < 0.001), sleep efficiency (MD = 0.06, 95% CI = 0.01–0.1, P = 0.01), REM (MD = 4.66, 95% CI = 2.7–6.62, P < 0.001), and a significant reduction of awaking (MD = −8.40, 95% CI = −10.15−6.64, P < 0.001), and sleep arousals index (MD = −5.17, 95% CI = −6.58−3.75, P < 0.001) (Supplementary Figures 7–10).
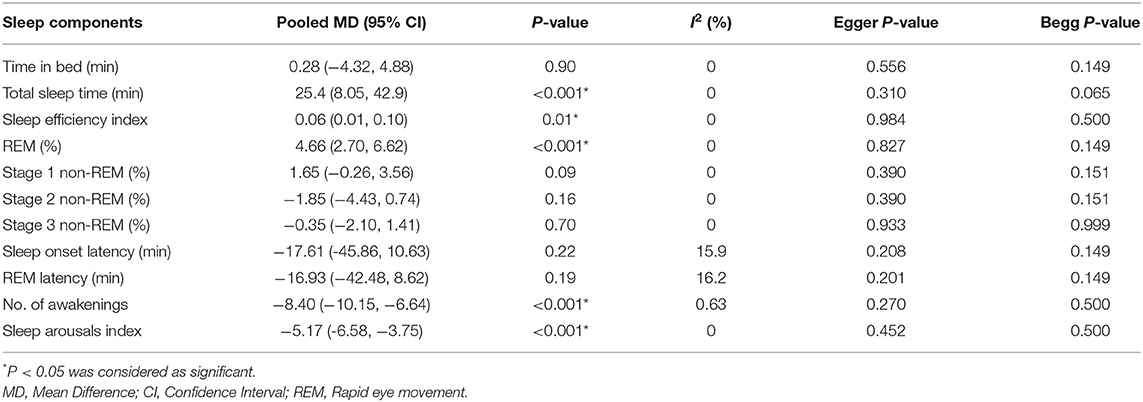
Table 4. Efficacy of eye masks and/or earplugs interventions for sleep quality based on polysomnography.
In the study, the effect of using eye masks and/or earplugs on quality of sleep was investigated in critical care setting and simulated environment of intensive care. Our study systematically reviewed 36 available studies, and 21 studies were included in the meta-analyses based on various sleep quality assessment tools. The results indicated that eye masks and/or earplugs interventions might have a positive effect on the sleep quality in critically ill patients. According to the overall PSQI sleep quality score, the eye masks and/or earplugs interventions had a positive effect on the sleep quality (26, 28, 29, 39). However, no significant difference was identified for sleep components based on PSQI score (26, 28, 29). Eleven studies reported the efficacy of eye masks and/or earplugs interventions on the overall sleep quality of critically ill patients using the RCSQ, and statistical significance in meta-analyses was observed, especially with respect to sleep depth, sleep latency, number of awakenings, sleep efficiency, and sleep quality (3, 5, 24, 40, 46–48, 51–53). Based on three studies, a positive effect of using eye masks and/or earplugs on domains of sleep disturbance via VSHSS was observed (31, 32, 49). Three studies measured sleep variables objectively by using PSG in a simulated critical care environment (21, 25, 38). Because of these similar conditions, we used these three studies. However, the results of these studies are not generalizable and should be interpreted with caution. The pooled results for the intervention groups showed beneficial impact (P < 0.05) for increased sleep period, sleep efficiency, REM sleep and decreased awaking and sleep arousals index. But the results should be treated with caution because of the studies were conducted in a simulated ICU environment with healthy adults and small sample sizes.
Eight studies used various instruments to evaluate the effectiveness of eye masks and earplugs on the sleep quality of ICU patients. One author, Le Guen et al. (34), used the Medical Outcome Study Scale (MOSS) and the Spiegel Scale (SS) and confirmed a statistically significant improvement after the intervention (P = 0.006). A non-randomized controlled trial study by Ho et al. (50), used the Insomnia Severity Index (ISI) questionnaire and they did not find any statistical significant difference between the intervention and control groups. In an experimental study by Baghaei et al. (30), 40 eligible patients were randomly assigned to control and eye mask groups and the Leeds Sleep Evaluation Questionnaire (LSEQ) was used to assess the effect of eye masks on nighttime sleep in CCU patients. According to the findings of this study, the use of eye masks improves sleep. Other authors; Richardson et al. (13), Jones et al. (22), Van Rompaey et al. (23), Sweity et al. (43), and Chaudhary et al. (41), employed their original questionnaires, which included a varied amount of items with different content focus. Due to the significant variety or lack of further details of questionnaires, these studies were not included in the meta-analysis. However, all of them had consensus on the positive effect of using eye masks and earplugs on the subjective quality of sleep.
In a review of 11 studies by Xie et al. (58), showed that noise was the most important cause of sleep disorders in critical care setting. The most disturbing noise sources were staff conversations and alarms, especially those with high frequencies. In addition to reducing noise by earplugs, this improvement of the sleep pattern via using eye masks can be explained by the relation between sleep wakefulness rhythm and the light-dark cycle. In this context, it is known that in the suprachiasmatic nucleus, the connections of the retina orient the nervous system about the existence of the light, which, being absent, stimulates the secretion of melatonin through the pineal gland (59). In a number of studies (13, 22, 25), the convenience of interventions was assessed based on patients' feedback. Many subjects reported that these interventions were comfortable and tolerable, and overall the rankings show that the products were very comfortable, very helpful, and very easy to use. However, it is important to note that earplugs and eye masks are only recommended for patients who are alert enough to cooperate and agree to these measures. Despite the evidence, the use of eye masks and earplugs may be considered invasive, especially if the patient is unable to remove them without assistance.
To our knowledge, this is the first systematic review and meta-analysis to observe the efficacy of eye masks and earplugs interventions on sleep quality in critically ill patients. Consistent with previous review studies (15, 16) on the effects of eye masks and /or earplug interventions on sleep quality in intensive care patients. The difference is that there was no meta-analysis in this area based on sleep quality assessment tools. However, there still exist several limitations in our research. The main limitation of this study was that due to the heterogeneity of studies on participants' demographic and clinical characteristics, methodological limitations, as well as measures and expression of outcomes, many of them did not enter the meta-analysis. In addition, small sample size, short evaluation period, different mental and objective sleep assessment techniques, and other methodological problems, such as lack of double blindness, and the use of simulation environment were other limitations of this study. Due to these limitations, the results of these studies are not generalizable and should be interpreted with caution. In addition, further high-quality research is needed to strengthen the evidence base.
According to the data presented in the study, non-invasive and low-cost sound- and light-masking interventions like as earplugs and eye masks may improve objective sleep characteristics aswell as subjective sleep experiences of patients in critical care settings.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
AV-A, FR-B, and MK-F designed the study. AV-A, SA, and SM contributed to the concept of the review and meta-analysis, acquisition of data, analysis and interpretation of data, and drafting the article. All authors edited and revised manuscript, and approved final version of manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Thanks to guidance and advice from the Clinical Research Development Unit of Baqiyatallah Hospital.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.791342/full#supplementary-material
1. Naik RD, Gupta K, Soneja M, Elavarasi A, Sreenivas V, Sinha S. Sleep quality and quantity in intensive care unit patients: a cross-sectional study. Indian J Crit Care Med. (2018) 22:408–14. doi: 10.4103/ijccm.IJCCM_65_18
2. Medrzycka-Dabrowska W, Lewandowska K, Kwiecień-Jaguś K, Czyz-Szypenbajl K. Sleep deprivation in intensive care unit - systematic review. Open Med. (2018) 13:384–93. doi: 10.1515/med-2018-0057
3. Bani Younis M, Hayajneh FA. Quality of sleep among intensive care unit patients: a literature review. Crit Care Nurs Q. (2018) 41:170–7. doi: 10.1097/CNQ.0000000000000196
4. Hu RF, Jiang XY, Chen J, Zeng Z, Chen XY, Li Y, et al. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst Rev. (2015) 2015:Cd008808. doi: 10.1002/14651858.CD008808.pub2
5. Kamdar BB, Martin JL, Needham DM, Ong MK. Promoting sleep to improve delirium in the ICU. Crit Care Med. (2016) 44:2290–1. doi: 10.1097/CCM.0000000000001982
6. Kamdar BB, Needham DM, Collop NA. Sleep deprivation in critical illness: its role in physical and psychological recovery. J Intensive Care Med. (2012) 27:97–111. doi: 10.1177/0885066610394322
7. Abad VC, Guilleminault C. Pharmacological treatment of sleep disorders and its relationship with neuroplasticity. Current Top Behav Neurosci. (2015) 25:503–53. doi: 10.1007/7854_2014_365
8. Mistraletti G, Carloni E, Cigada M, Zambrelli E, Taverna M, Sabbatini G, et al. Sleep and delirium in the intensive care unit. Minerva anestesiologica. (2008) 74:329–33.
9. Shilo L, Dagan Y, Smorjik Y, Weinberg U, Dolev S, Komptel B, et al. Patients in the intensive care unit suffer from severe lack of sleep associated with loss of normal melatonin secretion pattern. Am J Med Sci. (1999) 317:278–81. doi: 10.1016/S0002-9629(15)40528-2
10. Brito RA, do Nascimento Rebouças Viana SM, Beltrão BA, de Araújo Magalhães CB, de Bruin VMS, de Bruin PFC. Pharmacological and non-pharmacological interventions to promote sleep in intensive care units: a critical review. Sleep Breath. (2020) 24:25–35. doi: 10.1007/s11325-019-01902-7
11. Matthews EE. Sleep disturbances and fatigue in critically ill patients. AACN Adv Crit Care. (2011) 22:204–24. doi: 10.4037/NCI.0b013e31822052cb
12. Bion V, Lowe AS, Puthucheary Z, Montgomery H. Reducing sound and light exposure to improve sleep on the adult intensive care unit: an inclusive narrative review. J Intensive Care Soc. (2018) 19:138–46. doi: 10.1177/1751143717740803
13. Richardson A, Allsop M, Coghill E, Turnock C. Earplugs and eye masks: do they improve critical care patients' sleep? Nurs Crit Care. (2007) 12:278–86. doi: 10.1111/j.1478-5153.2007.00243.x
14. Scotto CJ, McClusky C, Spillan S, Kimmel J. Earplugs improve patients' subjective experience of sleep in critical care. Nurs Crit Care. (2009) 14:180–4. doi: 10.1111/j.1478-5153.2009.00344.x
15. Alway A, Halm MA, Shilhanek M, St Pierre J. Do earplugs and eye masks affect sleep and delirium outcomes in the critically ill? Am Crit Care. (2013) 22:357–60. doi: 10.4037/ajcc2013545
16. Locihova H, Axmann K, Padysakova H, Fejfar J. Effect of the use of earplugs and eye mask on the quality of sleep in intensive care patients: a systematic review. J Sleep Res. (2018) 27:e12607. doi: 10.1111/jsr.12607
17. Moher D, Liberati A, Tetzlaff J, Altman DG. Reprint–preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. (2009) 89:873–80. doi: 10.1093/ptj/89.9.873
18. Higgins JPT, Green S, Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions, Cochrane Book Series. Chichester; Hoboken: Wiley-Blackwell. (2008). p. 649. doi: 10.1002/9780470712184
19. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
20. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
21. Wallace CJ, Robins J, Alvord LS, Walker JM. The effect of earplugs on sleep measures during exposure to simulated intensive care unit noise. Am J Crit Care. (1999) 8:210–9. doi: 10.4037/ajcc1999.8.4.210
22. Jones C, Dawson D. Eye masks and earplugs improve patient's perception of sleep. Nurs Crit Care. (2012) 17:247–54. doi: 10.1111/j.1478-5153.2012.00501.x
23. Van Rompaey B, Elseviers MM, Van Drom W, Fromont V, Jorens PG. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care. (2012) 16:R73. doi: 10.1186/cc11330
24. Hu RF, Jiang XY, Hegadoren KM, Zhang YH. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Critical Care. (2015) 19:115. doi: 10.1186/s13054-015-0855-3
25. Hu RF, Jiang XY, Zeng YM, Chen XY, Zhang YH. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. Crit Care. (2010) 14:R66. doi: 10.1186/cc8965
26. Daneshmandi M, Neiseh F, SadeghiShermeh M, Ebadi A. Effect of eye mask on sleep quality in patients with acute coronary syndrome. J Caring Sci. (2012) 1:135–43. doi: 10.5681/jcs.2012.020
27. Ryu MJ, Park JS, Park H. Effect of sleep-inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. J Clin Nurs. (2012) 21:728–35. doi: 10.1111/j.1365-2702.2011.03876.x
28. Neiseh F, Daneshmandi M, Sadeghi Sharme M, Ebadi A. The effects of ear and eue protect device applicatio on quality of sleep of CCU patients with acute coronary syndrome (Hospital Military). J Mil Psychol. (2011) 2:67–80.
29. Neiseh F, Daneshmandi M, Sadeghi Sharme M, Ebadi A. The effect of earplugs on sleep quality in patients with acute coronary syndrome. IJCCN. (2011) 4:127–34.
30. Baghaei R, Feizi A, Ghaderi C. The effect of eye masks on nocturnal sleep in patients hospitalized in the Intensive Cardiac Care Units. Nurs Midwifery J. (2014) 12:800–6.
31. Mashayekhi F, Arab M, Pilevarzadeh M, Amiri M, Rafiei H. The effect of eye mask on sleep quality in patients of coronary care unit. Sleep Sci. (2013) 6:108–11.
32. Yazdannik AR, Zareie A, Hasanpour M, Kashefi P. The effect of earplugs and eye mask on patients' perceived sleep quality in intensive care unit. Iranian J Nurs Midwifery Res. (2014) 19:673−8.
33. Demoule A, Carreira S, Lavault S, Pallanca O, Morawiec E, Mayaux J, et al. Impact of earplugs and eye mask on sleep in critically ill patients: a prospective randomized study. Crit Care. (2017) 21:284. doi: 10.1186/s13054-017-1865-0
34. Le Guen M, Nicolas-Robin A, Lebard C, Arnulf I, Langeron O. Earplugs and eye masks vs routine care prevent sleep impairment in post-anaesthesia care unit: a randomized study. Br J Anaesth. (2014) 112:89–95. doi: 10.1093/bja/aet304
35. Babaii A, Adib-Hajbaghery M, Hajibagheri A. Effect of using eye mask on sleep quality in cardiac patients: a randomized controlled trial. Nurs Midwifery Stud. (2015) 4:e28332. doi: 10.17795/nmsjournal28332
36. Kamdar BB, King LM, Collop NA, Sakamuri S, Colantuoni E, Neufeld KJ, et al. The effect of a quality improvement intervention on perceived sleep quality and cognition in a medical ICU. Critical Care Med. (2013) 41:800–9. doi: 10.1097/CCM.0b013e3182746442
37. Bajwa N, Saini P, Kaur H, Kalra S, Kaur J. Effect of ear plugs and eye mask on sleep among ICU patients: a randomized control trial. Int J Curr Res. (2015) 7:741–5.
38. Huang HW, Zheng BL, Jiang L, Lin ZT, Zhang GB, Shen L, et al. Effect of oral melatonin and wearing earplugs and eye masks on nocturnal sleep in healthy subjects in a simulated intensive care unit environment: which might be a more promising strategy for ICU sleep deprivation? Critical Care. (2015) 19:124. doi: 10.1186/s13054-015-0842-8
39. Cheraghi Ma, Akbari K, Bahramnezhad F, Haghani H. The effect of earplug on the sleep of patients hospitalized in the coronary care unit. Complement Med J. (2018) 8:2293–303. Available online at: http://cmja.arakmu.ac.ir/article-1-386-en.html
40. Litton E, Elliott R, Ferrier J, Webb SAR. Quality sleep using earplugs in the intensive care unit: the QUIET pilot randomised controlled trial. Crit Care Resusc. (2017) 19:128–33.
41. Chaudhary A, Kumari V, Neetu N. Sleep promotion among critically ill patients: earplugs/eye mask versus ocean sound-a randomized controlled trial study. Crit Care Res Pract. (2020) 2020:8898172. doi: 10.1155/2020/8898172
42. Sharafi S, Hajiabadi F, Razi M, Bahrami M. The effect of simultaneously using earplug and eye mask on quality of sleep in intensive care unit patients: a randomized clinical trial study. J Crit Care Nurs. (2018) 11:27–34. Available online at: http://jccnursing.com/article-1-439-en.html
43. Sweity S, Finlay A, Lees C, Monk A, Sherpa T, Wade D. SleepSure: a pilot randomized-controlled trial to assess the effects of eye masks and earplugs on the quality of sleep for patients in hospital. Clin Rehabil. (2019) 33:253–61. doi: 10.1177/0269215518806041
44. Bani Younis MK, Hayajneh FA, Alduraidi H. Effectiveness of using eye mask and earplugs on sleep length and quality among intensive care patients: a quasi-experimental study. Int J Nurs Pract. (2019) 25:e12740. doi: 10.1111/ijn.12740
45. Dobing S, Dey A, McAlister F, Ringrose J. Non-pharmacologic interventions to improve sleep of medicine inpatients: a controlled study. J Community Hosp Int Med Perspect. (2017) 7:287–95. doi: 10.1080/20009666.2017.1379845
46. Arttawejkul P, Reutrakul S, Muntham D, Chirakalwasan N. Effect of nighttime earplugs and eye masks on sleep quality in intensive care unit patients. Indian J Crit Care Med. (2020) 24:6–10. doi: 10.5005/jp-journals-10071-23321
47. Kocak AT, Arslan S. The effect of using eye masks and earplugs on intensive care patients quality of sleep and vital signs. J Neurosci Nurs. (2021) 53:29–33. doi: 10.1097/JNN.0000000000000562
48. Obanor O, McBroom M, Elia J, Sasaki J, Murphy K, Chalk S, et al. Preliminary analysis of impact of earplugs and eye masks on sleep quality for patients in a SICU. Crit Care Med. (2019) 47:619. doi: 10.1097/01.ccm.0000552029.58235.0e
49. Lakeh MB, Lakeh MB, Mohammadi TK, Leyli EKN. The effect of use of earplugs on sleep quality in coronary care units patients. J Holistic Nurs Midwifery. (2018) 28:93–100. doi: 10.29252/hnmj.28.2.93
50. Ho AT, Waldhorn RE, Joshi A, Thapaliya S, Hunt T, Diamond M, et al. A Pilot non-randomized control trial of providing quiet time, ear plugs, eye masks, reducing noise and light in improving sleep for patients in general medical wards. Am J Respir Crit Care Med. (2019) 199:A1388. doi: 10.1186/ISRCTN15393303
51. Obanor OO, McBroom MM, Elia JM, Ahmed F, Sasaki JD, Murphy KM, et al. The impact of earplugs and eye masks on sleep quality in surgical ICU patients at risk for frequent awakenings. Crit Care Med. (2021) 49:e822–32. doi: 10.1097/CCM.0000000000005031
52. Mahran GS, Leach MJ, Abbas MS, Abbas AM, Ghoneim AM. Effect of eye masks on pain and sleep quality in patients undergoing cardiac surgery: a randomized controlled trial. Crit Care Nurse. (2020) 40:27–35. doi: 10.4037/ccn2020709
53. Leong RW, Davies LJ, Fook-Chong S, Ng SY, Lee YL. Effect of the use of earplugs and eye masks on the quality of sleep after major abdominal surgery: a randomised controlled trial. Anaesthesia. (2021) 76:1482–91. doi: 10.1111/anae.15468
54. Litton E, Carnegie V, Elliott R, Webb SA. The efficacy of earplugs as a sleep hygiene strategy for reducing delirium in the ICU: a systematic review and meta-analysis. Crit Care Med. (2016) 44:992–9. doi: 10.1097/CCM.0000000000001557
55. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
56. Richards K. Techniques for measurement of sleep in critical care. Focus Critical Care. (1987) 14:34–40.
57. Snyder-Halpern R, Verran JA. Instrumentation to describe subjective sleep characteristics in healthy subjects. Res Nurs Health. (1987) 10:155–63. doi: 10.1002/nur.4770100307
58. Xie H, Kang J, Mills GH. Clinical review: the impact of noise on patients' sleep and the effectiveness of noise reduction strategies in intensive care units. Crit Care. (2009) 13:208. doi: 10.1186/cc7154
Keywords: earplugs, eye mask, quality of sleep, intensive care unit, meta-analysis
Citation: Karimi L, Rahimi-Bashar F, Mohammadi SM, Mollahadi M, Khosh-Fetrat M, Vahedian-Azimi A and Ashtari S (2021) The Efficacy of Eye Masks and Earplugs Interventions for Sleep Promotion in Critically Ill Patients: A Systematic Review and Meta-Analysis. Front. Psychiatry 12:791342. doi: 10.3389/fpsyt.2021.791342
Received: 08 October 2021; Accepted: 10 November 2021;
Published: 03 December 2021.
Edited by:
Rosalia Cesarea Silvestri, University of Messina, ItalyReviewed by:
Brian K. Gehlbach, The University of Iowa, United StatesCopyright © 2021 Karimi, Rahimi-Bashar, Mohammadi, Mollahadi, Khosh-Fetrat, Vahedian-Azimi and Ashtari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Ashtari, c2FyYV9hc2h0YXJpQHlhaG9vLmNvbQ==
†ORCID: Leila Karimi orcid.org/0000-0001-8928-8220
Farshid Rahimi-Bashar orcid.org/0000-0001-8276-1425
Seyyede Momeneh Mohammadi orcid.org/0000-0001-5190-7209
Mohsen Mollahadi orcid.org/0000-0002-1134-9115
Masoum Khosh-Fetrat orcid.org/0000-0003-0346-9114
Amir Vahedian-Azimi orcid.org/0000-0002-1678-7608
Sara Ashtari orcid.org/0000-0003-1108-664X
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.